Introduction
Motor vehicle collisions (MVCs) remain a leading cause of traumatic injury and mortality worldwide [
1], presenting a critical public health challenge. Despite significant advancements in vehicle safety, urban infrastructure, and traffic regulations, the complexity and severity of injuries from motor vehicle collisions continue to strain trauma centers, especially in densely populated urban areas. New York City, known for being one of America’s most walkable cities, faces unique challenges, with over 60% of commuters walking or using public transportation as of 2016 [
2]. Previous studies have investigated the epidemiology and outcomes of injuries related to MVCs. However, in-depth analyses still need to focus on specific types of transportation, such as pedestrians, motorcyclists, bicyclists, and vehicle occupants. Each group displays unique injury patterns and clinical outcomes, which can help shape targeted prevention strategies and optimize resource allocation within trauma care systems.
This study aims to examine the injury patterns and clinical outcomes associated with MVCs among patients presenting to a level I trauma center in New York City. By analyzing data from various transportation modalities, the research provides valuable insights into how different forms of transportation affect the type and severity of trauma, as well as patient outcomes. The findings will help guide future injury prevention efforts and improve patient care. This analysis is intended to inform trauma care protocols, public health strategies, and injury prevention initiatives, particularly in urban areas with high traffic density and pedestrian activity. This retrospective study was approved by the IRB at Elmhurst Hospital Center (EHC) on October 24, 2024, with IRB number 24-12-380-05G. Informed consent was waived due to the retrospective nature of this study.
Methods
This retrospective, single-center study analyzed patients who sustained trauma from MVCs between January 1, 2016, and December 31, 2023, at a level I trauma center in New York City. Patients were identified from the National Trauma Registry of the American College of Surgeons (NTRACS) and data were collected from electronic health records (EHR) in the study center. Patients were identified based on the International Classification of Diseases (ICD) injury codes and the Abbreviated Injury Severity (AIS) for body region involvement. Eligible patients were those who presented to the hospital following an MVC and had documented injuries that met the trauma activation criteria outlined in the center’s guidelines. Key demographic information, injury patterns, and severity, as well as clinical outcomes, were recorded.
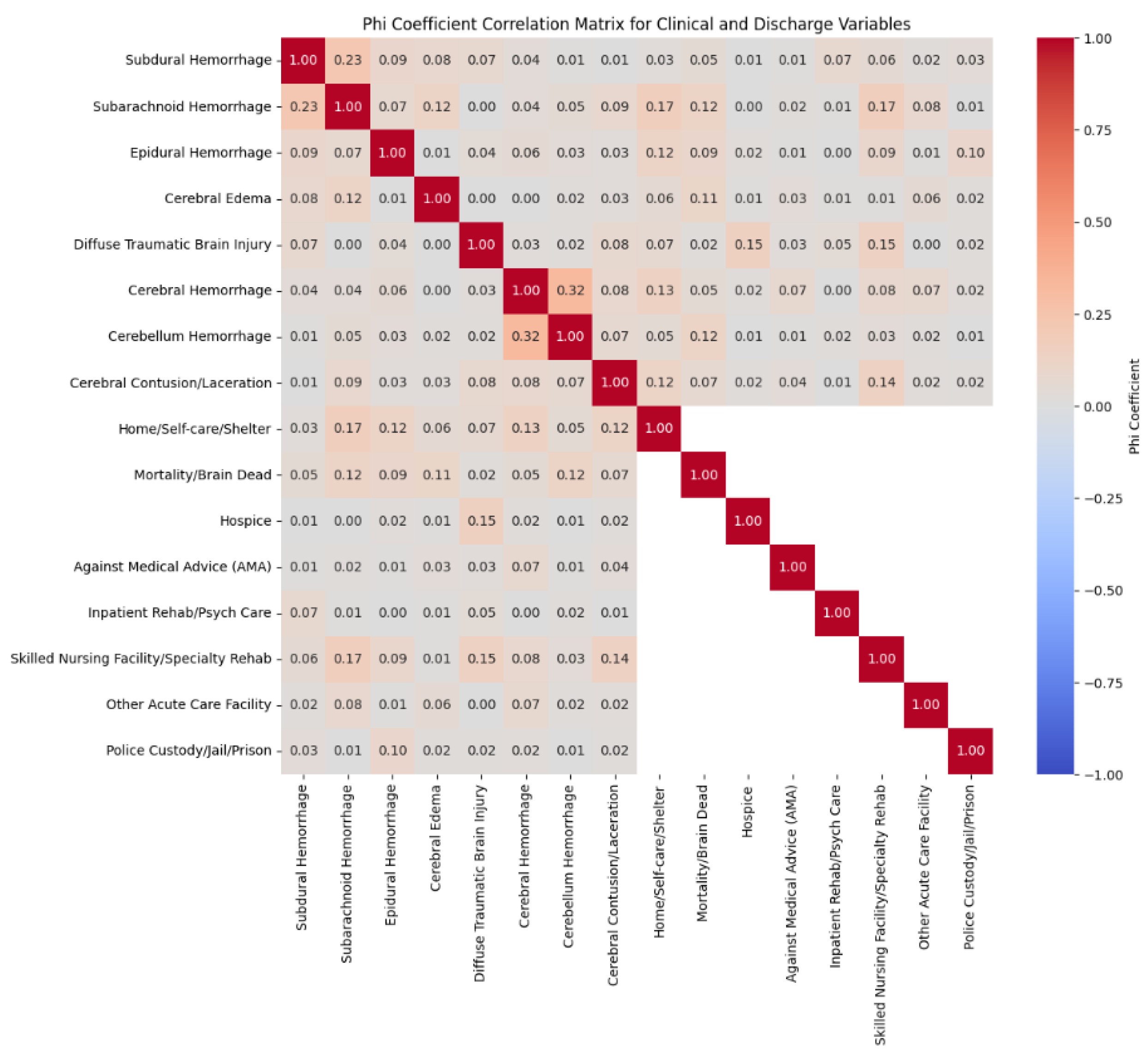
We utilized Phi coefficient analysis to assess the association between binary variables, specifically to examine the relationships between various clinical conditions and discharge outcomes. As a measure of association for categorical data, the Phi coefficient is particularly suitable for binary variables because it quantifies the strength of association on a scale from -1 (perfect negative association) to +1 (perfect positive association), with values close to zero indicating little or no association. This makes it an ideal choice for exploring the relationships within a dataset where outcomes are represented as binary variables. By utilizing the Phi coefficient, we can evaluate the association between patterns of traumatic brain injury and discharge disposition variables in a statistically sound and interpretable manner, offering insights into these patterns without making assumptions about causality.
While the Chi-square test is commonly used to assess the independence of categorical variables, it only indicates whether an association is statistically significant and does not measure the strength of that association. In contrast, the Phi coefficient indicates the presence of an association and quantifies its strength, which is valuable in understanding the degree of relationship between variables in this study. Additionally, Chi-square testing alone is less informative for our purpose, as we are not solely interested in whether a relationship exists but in how strongly traumatic brain injury patterns are associated with specific discharge outcomes. Thus, the Phi coefficient analysis offers a more comprehensive view of these relationships by combining significance and strength, making it a better fit for our research objectives.
Results
-
i.)
Association between Demographics and the mode of transportation
A total of 536 patients met the inclusion criteria. These patients were further differentiated based on the mode of transportation associated with their injury. It was found that pedestrian injuries were most prevalent with 251 patients (46.8%), followed by motorcycle drivers (135, 25.2%), bicyclists (100, 18.7%), and motor vehicle drivers (50, 9.3%). The average age of patients was 37.86, 34.53, 37.85, 49.14 (bicyclists, motorcyclists, motor vehicle occupants, and pedestrians, respectively), and the male-to-female ratio was higher for bicyclists and motorcyclists (13.7:1 and 11.9:1, respectively) compared to motor vehicle occupants and pedestrians (2.3:1 and 1.5:1, respectively). Racial demographics and ethnicity varied among the different modes of transportation. For a full summary of patient demographic information, see
Table 1.
-
ii.)
Injury Patterns
The majority of patients (99.63%) sustained blunt trauma, while only a small fraction (0.37%) experienced penetrating trauma. In the majority of cases, the head had the highest AIS score with a mean of 3.7, and the median ISS was 20 (interquartile range 14). 80.4% of patients had multi-body region injuries, with 431 occurrences, while single-body region injuries accounted for 19.6%, totaling 105 occurrences.
Across the total patient population, the most prevalent injuries were head injuries and fractures. By overall injury category, fractures were the most common with 1125 occurrences, followed by hemorrhage with 695 occurrences, laceration with 311 occurrences, contusion with 242 occurrences, and abrasion with 104 occurrences. More detailed analysis revealed skull fractures had the highest number of occurrences within the dataset (390), followed by subdural and subarachnoid hemorrhages (302 and 252, respectively), fracture of other facial bones (248), and cervical/thoracic/lumbar fracture (122).
More specifically, subdural hemorrhage with loss of consciousness had the highest prevalence, occurring in 169 cases, followed by fractures of the vault of the skull in 156 cases, subarachnoid hemorrhage with loss of consciousness in 141 cases, and fractures of the base of the skull with 110 cases. 72 patients had multiple rib fractures, 69 patients had scalp lacerations 53 had scalp contusions, and 60 had lung contusions. Overall, injury patterns among the different modes of transportation showed that brain injuries were the most prevalent, followed closely by fractures, then lacerations, concussions/contusions, and other injuries, including hemothorax/pneumothorax, and dislocations. Pedestrians were the only ones to experience amputations with 5 occurrences.
Table 2.
It illustrates various patterns of brain injuries and fractures related to the mode of transportation in patients with trauma from motor vehicle collisions (MVCs).
Table 2.
It illustrates various patterns of brain injuries and fractures related to the mode of transportation in patients with trauma from motor vehicle collisions (MVCs).
| |
Count (%) |
| Injury * |
Total
n=536
|
Bicyclist
n=103
|
Motorcyclist
n=129
|
Motor Vehicle
n=46
|
Pedestrian
n=258
|
| Brain Injury Patterns |
|
|
|
|
|
| Subdural Hemorrhage (SDH) |
299 (55.8%) |
60 (58.2%) |
65 (50.4%) |
27 (58.7%) |
147 (57.0%) |
| Epidural Hemorrhage (EDH) |
69 (12.9%) |
15 (14.6%) |
19 (14.7%) |
3 (6.5%) |
32 (12.4%) |
| Subarachnoid Hemorrhage (SAH) |
252 (47.0%) |
45 (43.7%) |
58 (45.0%) |
20 (43.5%) |
129 (50.0%) |
| Brain Stem Hemorrhage |
9 (1.7%) |
1 (0.97%) |
4 (3.1%) |
1 (2.2%) |
3 (1.2%) |
| Diffuse Traumatic Brain Injury |
20 (3.7%) |
1 (0.97%) |
9 (7.0%) |
2 (4.3%) |
8 (3.1%) |
| Other Intracranial Injuries/Hemorrhage of cerebrum, others |
63 (11.8%) |
15 (14.6%) |
18 (14.0%) |
6 (13.0%) |
24 (9.3%) |
| Major Fracture Patterns |
|
|
|
|
|
| Long Bone Fractures (Tib-Fib, Femur, Radius, Ulna, Humerus, Trimalleolar) |
92 (17.2%) |
8 (7.8%) |
19 (14.7%) |
6 (13.0%) |
59 (22.9%) |
| Hand/Foot Fractures (Metatarsal, Metacarpal, Phalanges, Talus, Calcaneus) |
16 (3.0%) |
2 (1.9%) |
1 (0.78%) |
1 (2.2%) |
12 (4.7%) |
| Facial (Nasal, Mandible, Orbit, Maxilla, Zygomatic) & Skull (Vault, Sphenoid, Parietal, Temporal, Occipital) Fractures |
320 (59.7%) |
63 (61.2%) |
88 (68.2%) |
20 (43.5%) |
149 (57.8%) |
| Other Fractures (Ribs, Pelvis, Hip) |
68 (12.7%) |
14 (13.6%) |
10 (7.8%) |
10 (21.7%) |
34 (13.1%) |
-
iii.)
Clinical Outcomes
The analysis of clinical outcomes in patients involved in MVCs reveals significant variations based on the mode of transportation used. Among the different groups, pedestrians had the highest overall mortality rate of 24%. In comparison, bicyclists had a lower mortality rate of 8.7%, motorcyclists had a rate of 13.1%, and motor vehicle occupants had a rate of 10.9%. This indicates that pedestrians are more vulnerable to such injuries. Lack of protective gear may be one of the reasons for this vulnerability.
Additionally, only 43.8% of pedestrians were discharged home, while 19% required sub-acute or inpatient rehabilitation, reflecting the severity of their injuries. A small percentage, 2.6%, met the criteria for brain death, with slightly higher rates noted among motorcyclists and pedestrians. Discharges to skilled nursing facilities and other acute care settings were also more common for pedestrians, highlighting their increased need for care after hospitalization.
In contrast, bicyclists had the best outcomes overall, evidenced by the highest discharge rate to home at 68.9%. These findings underscore the importance of implementing targeted preventive measures and tailored post-trauma care strategies, especially for pedestrians who face the most significant risk of severe and prolonged injuries following MVCs.
Overall mortality was 17.4%, with an additional 14 patients (2.6%) meeting brain death criteria. Between the different transportation modalities, pedestrians had the highest mortality rate at 24.0%, followed by motorcyclists (13.1%), motor vehicle occupants (10.9%), and bicyclists (8.7%). Pedestrians were also the least likely to be discharged to home/shelter at 43.8%, compared to bicyclists at 68.9%, motorcyclists at 62.8%, and motor vehicle occupants at 54.3%. A complete summary of clinical outcomes is represented in
Table 3.
Figure 1 of this paper provides insights into the relationships between various traumatic injuries and discharge outcomes while accounting for the mutual exclusivity of discharge destinations. In this adjusted heatmap, we focused on meaningful associations between Brain-specific injuries (such as Subdural Hemorrhage, Subarachnoid Hemorrhage, Epidural Hemorrhage, etc.) and individual discharge outcomes (e.g., home/self-care, mortality, hospice, specialty rehab) without creating artificial correlations between discharge outcomes that cannot occur simultaneously.
Most observed Phi values are relatively low, suggesting weak associations between most clinical and discharge variables. This finding indicates that no single clinical condition strongly predicts a specific discharge destination in this dataset, implying that a broader set of clinical, demographic, or social factors likely influences discharge decisions. However, a few moderate associations are noteworthy. For example, Cerebral Hemorrhage has a moderate correlation with Hospice (Phi = 0.32), suggesting that patients with cerebral hemorrhage may have an increased likelihood of being discharged to hospice care, likely due to the severe nature of this condition. Additionally, Skilled Nursing Facility/Specialty Rehab shows a moderate association with Cerebral Hemorrhage (Phi = 0.15), indicating that patients with severe brain injury might require specialized rehabilitation.
The Phi coefficient analysis also highlights the relationship between Cerebral Hemorrhage and Cerebellum Hemorrhage, which shows a moderate positive association (Phi = 0.32). This suggests that cases involving cerebral hemorrhage are somewhat likely to be associated with cases of cerebellar hemorrhage within the same patient population. This relationship may indicate overlapping risk factors or a tendency for multiple areas of the brain to be affected in cases with severe or widespread hemorrhaging. This finding could reflect a clinical pattern where patients with one type of brain hemorrhage may have a predisposition or a higher likelihood of experiencing hemorrhage in another area of the brain. Further exploration into these commonalities may provide insights into risk factors or clinical characteristics contributing to concurrent or multi-regional brain hemorrhages, which could be valuable for targeted intervention and management strategies.
Overall, this analysis shows that while certain traumatic injuries might be moderately associated with specific discharge outcomes, most associations are weak, underscoring the complexity of discharge planning and the potential role of additional, unmeasured factors. Excluding correlations among mutually exclusive discharge outcomes can provide a clearer and more accurate understanding of the true relationships between traumatic injuries and patient discharge destinations.
Discussion
This retrospective analysis of patients involved in MVCs from 2016 to 2023 provides critical insights into the injury patterns and clinical outcomes associated with various transportation modalities. By examining 536 patients, this study offers a detailed understanding of the distribution of head injuries, fractures, and associated trauma across four primary transportation groups: pedestrians, bicyclists, motorcyclists, and motor vehicle occupants.
Almost half of MVC trauma patients were pedestrians, one-quarter were motorcyclists, 19.4% were bicyclists, and 8.6% were motor vehicle occupants. This is not similar to previous literature which found pedestrians were 10.5-28% of MVC patients, motorcyclists 21-60.8%, bicyclists 0.7%, and motor vehicle occupants 28.7-51%, depending on the study [
3,
4,
5]. This variation shows that transportation varies widely by location, and as such, preventative measures should be tailored to the individual needs of that location. In the case of this study, measures that protect pedestrians would likely be most beneficial, especially as pedestrians had the highest mortality rate.
The majority of patients in the study were male (75%), which is consistent with prior studies [
4,
6]. This was even more pronounced in the bicyclist and motorcyclist groups, which were 93.2% and 92.2% male, respectively, also consistent with prior studies [
7,
8]. Of note, Liasidis et al. found that 81.4% of motorcycle passengers, specifically female, [
9], compared to drivers, who were majority male. Regardless, this suggests that males have a much higher risk than females of being involved in MVCs causing traumatic injuries, especially bicyclists and motorcyclists. Yan et al. suggest a possible reason for this difference, finding male bicyclists were more likely to be involved in crashes caused by a failure to obey traffic signals [
10].
Almost all patients experienced injuries from blunt trauma and most had multi-body region injuries. The median ISS was found to be 20. Brain injuries were found to be the most common injury pattern across all modalities (subdural hemorrhage > subarachnoid hemorrhage > epidural hemorrhage), followed by fractures, which varied in prevalence depending on the mode of transportation. This overall trend is similar to a previous study, which found that head and external injuries were present in over 60% of patients who experienced motor vehicle trauma [
3]. However, when looked at individually, our findings for each mode of transportation are not consistent with prior studies. Generally, brain injuries and facial/skull fractures were much more prevalent in this study compared with prior findings of extremity injuries.
For bicyclists, the most common injury was facial/skull fractures (61.2%), followed by SDH (58.2%), SAH (43.7%), and EDH/another intracranial injury (both 14.6%). In contrast, Kale et al. found long bone fractures to be the most prevalent at 56% [
11]; in this study, they only accounted for 7.8% of injuries.
Similarly, injury prevalence for motorcyclists was facial/skull fracture (68.2%), SDH (50.4%), SAH (45.0%), and EDH (14.7%). The prevalence of long bone fractures was slightly increased (also 14.7%) compared to bicyclists. Takalkar et. al. specifically studied head injury patterns in motorcyclists and found similar findings, with SDH and SAH being the most prevalent [
8]. Other studies varied in their findings; while one found most injuries were sustained to the head/skull [
7], others found extremity fractures [
9] and contusions [
5] to be the most common injuries. One study showed that head injuries and facial fractures were least prevalent in motorcyclists compared to other transportation modalities [
3]. In contrast, this study found that motorcyclists had the highest prevalence of facial/skull fractures, and while SDH was lowest in motorcyclists, other brain injuries like SAH and EDH were increased compared to other modalities.
Motor vehicle occupants were the only mode of transportation to have SDH as the most common injury (58.7%), followed by SAH tied with facial/skull fracture (43.5%), and torso/pelvis fracture (21.7%), which had the highest prevalence compared to other modes of transportation. Likewise, Parkinson et al. showed that motor vehicle occupants were more likely to have intra-abdominal injuries compared to pedestrians [
12]. These injuries are consistent with those commonly caused by seatbelts, which can explain their increased frequency in this population.
Pedestrians again had similar injury patterns; facial/skull fracture (57.8%), followed by SDH (57.0%), SAH (50.0%), long bone fracture (22.9%), and torso/pelvis fracture (13.1%). Again, this is inconsistent with previous literature, which found lower extremity (specifically tibia-fibula and femur), pelvic, and vertebral fractures to be the most prevalent [
11,
12,
13]. There were similarities though when comparing pedestrian injury to the other transportation modalities; pedestrians were more likely to have long bone fractures including lower limb (tibia-fibula), clavicle, and radio-ulnar fractures [
12].
Mortality overall was 17.4% with an additional 2.6% meeting brain death criteria. This is increased compared to other studies that had mortality rates of around 3-5% [
6,
7,
12]. Pedestrians had the highest mortality rate at 24.0% and were the most likely to be discharged to sub-acute/inpatient rehabilitation (19.0%) and the least likely to be discharged home (43.8%). This suggests that pedestrians experience more severe and life-altering injuries compared to other transportation groups, necessitating extended care in sub-acute rehabilitation or skilled nursing facilities. Previous studies also found that pedestrian mortality was increased compared to motorcyclists and motor vehicle occupants, with rates ranging from 20-38.4% [
3,
13,
14]. This presents a unique problem to try to solve. While other transport modalities utilize features to minimize or decrease injury (airbags and seatbelts in motor vehicles, helmets, and protective clothing for bicyclists and motorcyclists), pedestrians have limited protection options against injury in MVCs. Analysis of the environment is needed to determine specific risk factors for this pedestrian population. This may include specific location (intersection/street), time of day, and vehicle type/speed at impact, among other factors.
Motorcyclist mortality was 13.1%, which is increased compared to prior studies that had mortality rates of 0-4.4% [
3,
9,
14]. This suggests there are specific risk factors in this population that are leading to increased mortality. Further study is needed to determine if this is related to the lack of use of protective gear such as helmets or another cause to determine the best way to decrease mortality.
Interestingly, motor vehicle occupants had a relatively low mortality rate (10.9%) and made up the smallest proportion of occurrences (8.6%). Other studies had increased occurrences (28.7-51%) [
3,
4,
5] and had varying mortality rates (3-29.2%) [
3,
7,
14]. This finding highlights the effectiveness of safety features such as seatbelts, airbags, and advanced vehicle crumple zones in reducing mortality among vehicle occupants. However, the comparatively low discharge-to-home rate (54.3%) indicates that many motor vehicle occupants still experience significant injuries that require prolonged rehabilitation. One explanation for this finding is that the majority of motor vehicle occupants involved in crashes receive minor injuries that do not meet trauma activation requirements, which is why the number of occurrences is low. Those that do meet trauma activation requirements, however, tend to have more severe injuries, resulting in the need for more long-term care.
Strength
This study is notable compared to previous research on MVC-related trauma because it provides a detailed analysis of specific injury patterns across various transportation modes, including pedestrians, bicyclists, motorcyclists, and vehicle occupants, within a densely populated urban area. Previous studies provide a general overview of MVC injuries but do not examine the specific patterns linked to each mode of transportation. This research offers a more detailed understanding of how different transportation modes influence injury type and severity.
The research spans over seven years, resulting in a robust dataset that enhances the reliability of the observed trends and injury associations. Additionally, the study utilizes Phi coefficient analysis, which is more informative than traditional Chi-square tests. This method quantifies the strength of associations between injury types and discharge outcomes, offering a clearer perspective on the relationships involved. Such methodological advancements facilitate a more precise and actionable understanding of MVC injuries, essential for developing targeted preventive measures and improving trauma care protocols specific to each transportation mode.
Limitations
This study is limited by its retrospective nature and reliance on data from a single trauma center. As such, the findings may not be generalizable to other regions with different transportation patterns or trauma care systems. The study also relies on the accuracy of ICD codes and EHR documentation, which may introduce coding errors or misclassification of injury types. Additionally, this study only included patients who met trauma activation criteria after arriving at the hospital, excluding both patients with more minor injuries and those who died at the scene. Future studies should consider prospective designs and multi-center collaborations to provide a more comprehensive understanding of injury patterns across different settings.
Conclusions
In conclusion, this study provides valuable insights into the patterns of injury and clinical outcomes among trauma patients involved in MVCs at a level I trauma center in New York City. Our findings highlight significant differences in injury severity, brain injuries, and fracture patterns across various transportation modalities, with pedestrians, motorcyclists, and bicyclists experiencing more severe and life-threatening injuries compared to motor vehicle occupants. Pedestrians, in particular, exhibited the highest mortality rates and were more likely to require long-term rehabilitation.
Overall, these findings suggest that tailored preventive strategies and safety improvements are critical for each transportation group. For pedestrians, enhanced urban planning and traffic control measures could help reduce injury risk, while increased awareness and adherence to safety practices for motorcyclists and bicyclists may lower the incidence of severe trauma. Future research should focus on identifying specific environmental risk factors and developing targeted interventions to minimize the severity of injury and improve clinical outcomes associated with MVC-related trauma. By addressing these factors, we can move toward safer urban transportation systems and more effective trauma care.
Author Contributions
Conceptualization- BS; writing—original draft preparation- BS and SK; writing—review and editing- BS, AA, KT, NDB, GA, JD, JM, ZS, and JW; figures and table, BS and AA; supervision- BS; project administration- BS
Funding
There is no grant support or financial relationship for this manuscript.
Acknowledgment
Not Applicable
Institutional Review Board (IRB) Statement
This retrospective study was approved by the IRB at Elmhurst Hospital Center (EHC) on October 24, 2024, with IRB number 24-12-380-05G.
Conflicts of Interest
The authors have no competing interests to declare.
References
- World Health Organization. Global Status Report on Road Safety 2015. 2015. https://iris.who.int/handle/10665/189242 (accessed 2024-10-17).
- New York Metropolitan Transportation Council. Regional Transportation Statistical Report. https://www.nymtc.org/LinkClick.aspx?fileticket=-gwiEIwYwYg=&portalid=0 (accessed 2024-10-17).
- Civil, I. D. Patterns of Injury in Motor Vehicle Trauma. New Zealand Medical Journal 1986, 99 (814), 905–906.
- Markogiannakis, H.; Sanidas, E.; Messaris, E.; Koutentakis, D.; Alpantaki, K.; Kafetzakis, A.; Tsiftsis, D. Motor Vehicle Trauma: Analysis of Injury Profiles by Road-User Category. Emergency Medicine Journal 2006, 23 (1), 27–31. [CrossRef]
- Ferrando, J.; Plasència, A.; Ricart, I.; Canaleta, X.; Seguí-Gómez , M. Motor-Vehicle Injury Patterns in Emergency-Department Patients in a South-European Urban Setting. Association for the Advancement of Automotive Medicine 2000, 44, 445–458.
- Nutbeam, T.; Weekes, L.; Heidari, S.; Fenwick, R.; Bouamra, O.; Smith, J.; Stassen, W. Sex-Disaggregated Analysis of the Injury Patterns, Outcome Data and Trapped Status of Major Trauma Patients Injured in Motor Vehicle Collisions: A Prespecified Analysis of the UK Trauma Registry (Tarn). BMJ Open 2022, 12 (5). [CrossRef]
- Hasan, O.; Sheikh, S.; Fatima, A.; Abbas, A.; Zahid, N.; Baloch, N. Motor-Vehicle Crash Patient Injury Patterns from a Level One Trauma Center in a Metropolitan City: A Cross-Sectional Study. Cureus 2019, 11 (2), e4073. [CrossRef]
- Takalkar, Y.; Vashist, K.; Chakravarthy, V.; Shinde, P. A Prospective Study of Head Injury Patterns in Motorcycle Riders Wearing/Not Wearing Helmets. Polish Journal of Surgery 2022, 95 (1), 30–34. [CrossRef]
- Liasidis, P.; Benjamin, E.; Jakob, D.; Lewis, M.; Demetriades, D. Injury Patterns and Outcomes in Motorcycle Passengers. European Journal of Trauma and Emergency Surgery 2023, 49 (6), 2447–2457. [CrossRef]
- Yan, X.; Ma, M.; Huang, H.; Abdel-Aty, M.; Wu, C. Motor Vehicle–Bicycle Crashes in Beijing: Irregular Maneuvers, Crash Patterns, and Injury Severity. Accident Analysis & Prevention 2011, 43 (5), 1751–1758. [CrossRef]
- Kale, N. N.; Lavorgna, T.; Vemulapalli, K. C.; Ierulli, V.; Mulcahey, M. K. Traumatic Orthopaedic Motor Vehicle Injuries: Are There Age and Sex Differences in Pedestrian and Cyclist Accidents in a Major Urban Center? Injury 2023, 54 (6), 1484–1491. [CrossRef]
- Parkinson, F.; Kent, S.; Aldous, C.; Oosthuizen, G.; Clarke, D. L. Patterns of Injury Seen in Road Crash Victims in a South African Trauma Centre. South African Journal of Surgery 2013, 51 (4), 131. [CrossRef]
- Brainard, B. J.; Slauterbeck, J.; Benjamin, J. B.; Hagaman, R. M.; Higie, S. Injury Profiles in Pedestrian Motor Vehicle Trauma. Annals of Emergency Medicine 1989, 18 (8), 881–883. [CrossRef]
- Al-Habib, A.; A-shail, A.; Alaqeel, A.; Zamakhshary, M.; Al-bedah, K.; AlQunai, M.; Al-enazi, S. Causes and Patterns of Adult Traumatic Head Injuries in Saudi Arabia: Implications for Injury Prevention. Annals of Saudi Medicine 2013, 33 (4), 351–355. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).