1. Introduction
Achieving acceptable stability and retention with mandibular complete dentures presents significant challenges. Specific issues such as high tongue mobility, insufficient residual ridge height, movable retromolar pads, and anatomical structures that change size when the patient opens or closes their mouth complicate the use of mandibular dentures [
1,
2].
Definitive impressions for complete dentures play a crucial role in treatment success and can be classified into techniques such as neutral zone, mucostatic, mucocompressive, selective pressure, and functional [
3,
4,
5].
In 1999, Abe introduced an innovative functional impression technique and new concepts regarding the correct extension of the prosthesis that revolutionized denture fitting by ensuring a peripheral seal even with mobile soft tissues at the denture’s base. This method, known for its high predictability, enabled mandibular dentures to restore function and masticatory capacity, significantly improving patients’ quality of life, all without requiring surgical procedures [
6].
Advancements in technology have significantly transformed the fabrication of complete dentures, offering more efficient and precise methods than traditional approaches. The integration of computer-aided design (CAD) and computer-aided manufacturing (CAM) has enabled the creation of digital complete dentures with a high degree of accuracy and repeatability [
7]. The use of intraoral scanners (IOS) has significantly improved the patient experience by eliminating the need for physical impressions, which can be uncomfortable and less accurate [
8].
The purpose of this report is to describe a technique for fabricating mandibular dentures with increased retention, utilizing a single-step scanning technique combined with Abe’s concepts for both the intraoral scanning process and the design of the prosthesis extension.
2. Materials and Methods
An 87-year-old male presented to a private dental clinic with the chief complaint that his current lower complete denture lacked retention and stability, making it difficult for him to eat and speak. The patient’s medical history was non-contributory, with no contraindications for dental treatment.
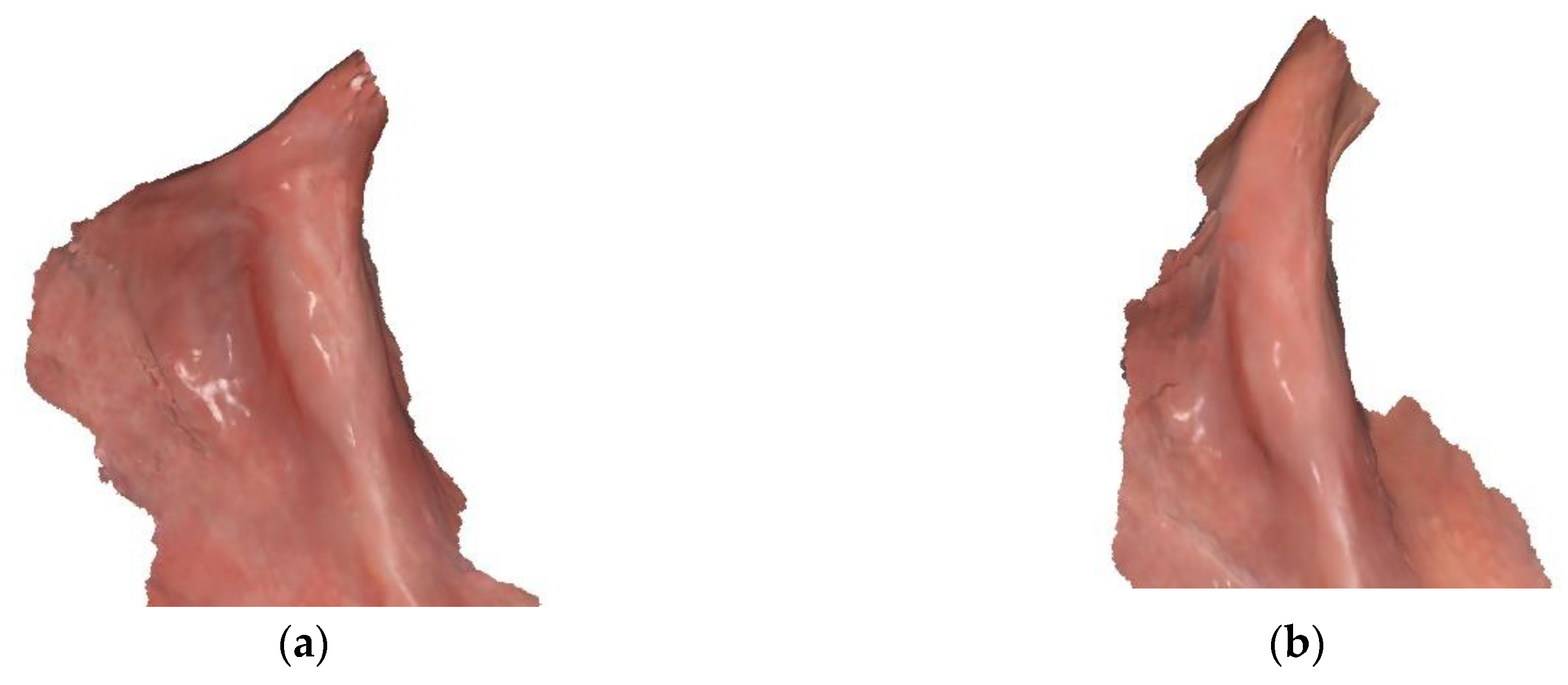
Intraoral examination revealed a severely resorbed mandibular edentulous ridge with movable retromolar pads and a prominent spongy lingual area (
Figure 1). The existing denture exhibited excessive movement of the mandibular base during functional activities, with teeth positioned in suboptimal locations.
The patient was presented with several treatment options, including implant overdentures, implant-supported fixed prostheses, and new complete dentures. However, he opted for a new mandibular complete denture, emphasizing his preference for a design closely resembling his current prosthesis and expressing his intention to use it temporarily while deciding whether to pursue implant treatment at a later date.
During the first appointment, an intraoral scanner (Aoralscan 3, Shining 3D, Hangzhou, China) was used to scan the patient’s existing dentures in occlusion. This process facilitated the capture of not only the antagonist but also the patient’s vertical dimension of occlusion as a reference.
To perform the mandibular scan, an intraoral retractor for edentulous arches (Lo Russo Retractors, Italy) was employed. The patient was instructed to keep their mandible slightly closed, in a resting position, while the scan was performed following a specific strategy: starting posteriorly and proceeding along the occlusal aspect of the ridge to the opposite side, subsequently returning along the palatal or lingual aspect, and finally scanning the buccal aspect (
Figure 2).
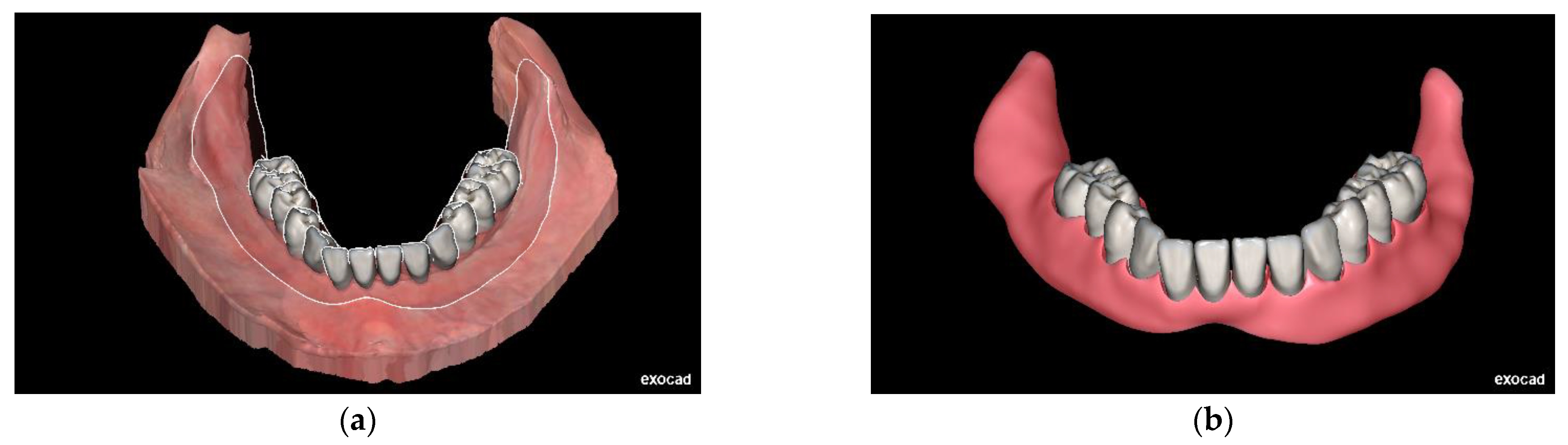
Once the mandibular scan was completed, the scanner software automatically aligned the scan with the reference of the patient’s existing dentures. The scan files were subsequently exported to design software (DentalCAD, Exocad GmbH, Darmstadt, Germany)) to create the prosthesis.
For this design, the outline was carefully extended to fully cover the retromolar pad, avoid interference with Someya’s sinew string, reach the deepest point of the buccal shelf, relieve pressure on the buccal frenum, and extend two millimeters beyond the mylohyoid ridge. The teeth were positioned based on the patient’s request, using the previous denture as a reference (
Figure 3).
The final denture base was printed using pink base resin (Denture Base Resin, Formlabs, Somerville, MA, USA), and the teeth were printed with denture teeth resin (Denture Teeth Resin A2, Formlabs, Somerville, MA, USA). The prosthesis was then assembled, finished, and polished (
Figure 4).
At the second appointment, the patient received the final denture, which fit well and restored his masticatory function. He reported satisfaction with the comfort, stability, and esthetics of the new denture (
Figure 5).
3. Discussion
The advent of digital technologies in dentistry has significantly transformed the fabrication of complete dentures, introducing more efficient and precise methods compared to traditional techniques [
9]. Conventional impression methods have long been considered the gold standard for obtaining accurate anatomical records; however, they present limitations such as patient discomfort, potential for tissue distortion, and challenges in capturing dynamic anatomical structures—especially in the mandibular arch [
10].
Intraoral scanners (IOS) have emerged as valuable alternatives, offering efficient and reproducible means of capturing oral anatomy while enhancing patient comfort. Studies have demonstrated that digital scans obtained via IOS can capture fine anatomical details without the distortion associated with conventional impression materials, a critical factor for achieving optimal fit in mandibular complete dentures, particularly in patients with compromised residual ridges or mobile soft tissues [
11].
Despite these advantages, achieving an effective peripheral seal—a crucial element for the retention and stability of complete dentures—remains a challenge with digital impressions. The development of refined scanning protocols and techniques has addressed many of these obstacles, improving clinical predictability [
12]. Utilizing IOS as a primary record before definitive impressions allows for precise planning and iterative adjustments of prosthetic designs, reducing clinical time and the number of appointments required [
13]. The implementation of specific scanning strategies is essential to ensure accurate and functional digital impressions [
14,
15,
16,
17]. Techniques such as employing intraoral retractors to stabilize soft tissues and systematically capturing critical anatomical landmarks—such as the retromolar pad and buccal shelf—have enhanced the quality and clinical utility of digital records [
18].
Jiro Abe’s Suction Effective Mandibular Complete Denture (SEMCD) technique revolutionized the concept of achieving a peripheral seal in mandibular dentures by accounting for the dynamic nature of soft tissues. The key concepts of SEMCD involve capturing tissue dynamics by recognizing the dimensional changes in the retromolar area when the mouth opens or closes. Abe emphasized taking impressions with the mouth closed to ensure that the prosthesis aligns accurately with the tissues during function, as impressions taken with the mouth open can lead to discrepancies between the prosthesis and posterior tissues, compromising the peripheral seal and suction effectiveness. Additionally, extending the denture 2 to 3 mm beyond the mylohyoid ridge increases stability during functional movements by engaging additional tissue support. Relieving pressure in the area of Someya’s string—a tendinous structure in the floor of the mouth—is crucial, as failure to relieve this area can cause discomfort and lead to prosthesis dislodgement during mastication.
In the present case, Abe’s SEMCD principles were integrated into a digital workflow. The intraoral scan was performed with the patient maintaining a mandibular resting position, allowing for the functional dimensions of the soft tissues to be captured and improving the accuracy of the digital impression (
Figure 6). Extending the digital prosthesis design beyond the mylohyoid ridge and relieving the area of Someya’s string replicated the functional extensions described by Abe, optimizing prosthetic stability and retention in the final denture [
19].
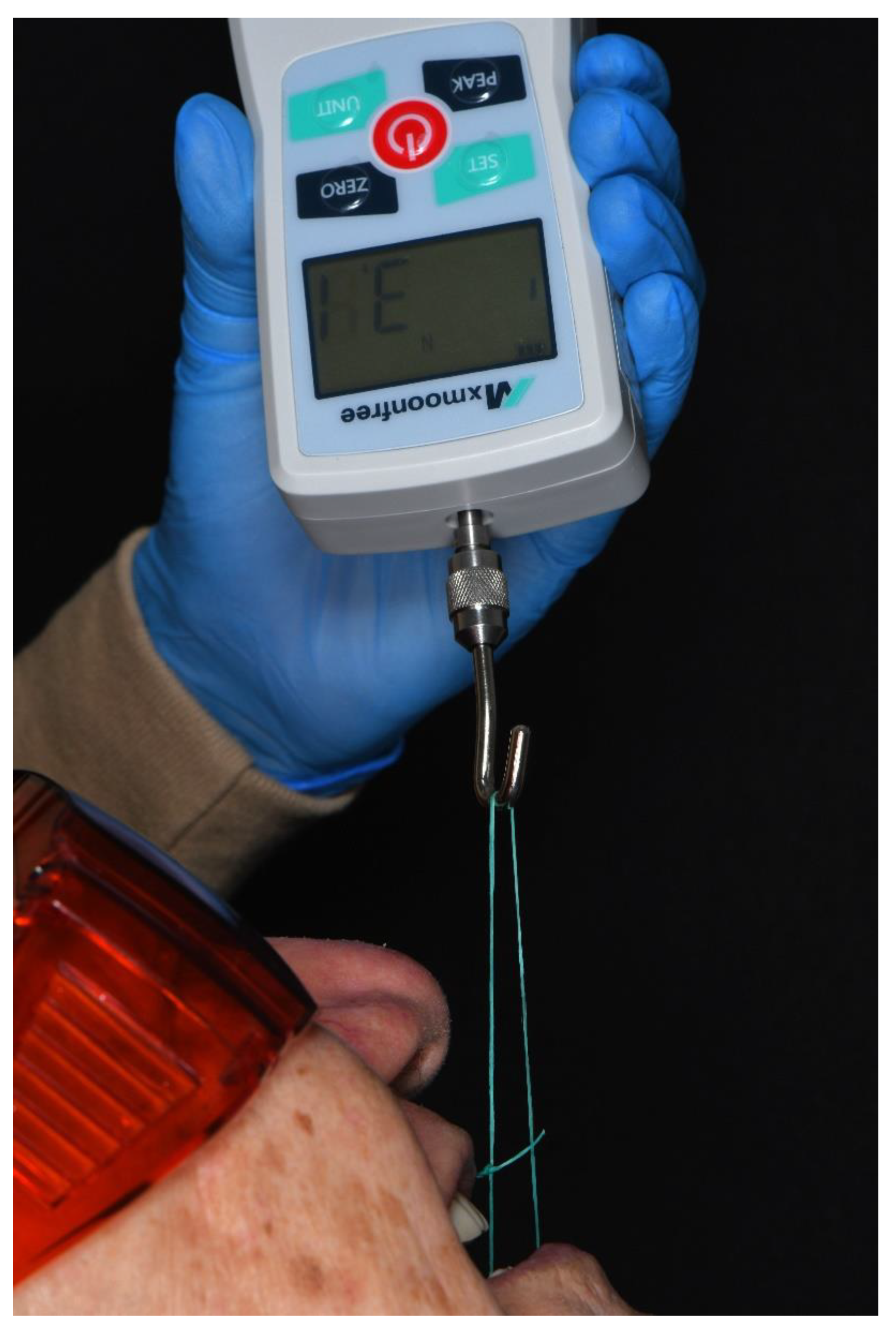
Retention is a critical factor in the success of mandibular dentures. Studies comparing the force required to dislodge mandibular overdentures have shown that ball attachments require approximately 0.655 kg, implant bar attachments require 1.677 kg, and magnet attachments require 0.370 kg for removal [
20]. In this case, the digitally fabricated mandibular complete denture required 0.31 kg of force to be dislodged (
Figure 7). Although the retention force achieved is slightly lower than that of some attachment systems, this approach offers a viable treatment option for edentulous patients.
Incorporating SEMCD concepts into a digital workflow is both feasible and beneficial. The digital replication of functional extensions allows for high precision in prosthesis fabrication, potentially leading to improved clinical outcomes. Moreover, this method eliminates the need for physical impressions and models, streamlining the fabrication process and enhancing patient comfort.
4. Conclusions
The integration of Abe’s principles into a digital workflow enhances the retention and stability of mandibular complete dentures while minimizing the number of clinical steps involved. The results of this study demonstrate that digital technologies can effectively replicate established functional concepts, providing a precise and efficient solution for the rehabilitation of edentulous patients.
Author Contributions
Conceptualization, E.G.; methodology, E.G. and S.J.; software, E.G.; validation, E.G. and S.J.; resources, E.G.; data curation, E.G.; writing—original draft preparation, E.G.; writing—review and editing, S.J.; visualization, E.G. and S.J.; supervision, E.G.; project administration, E.G.; funding acquisition, E.G. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Informed consent was obtained from the subject involved in this study.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Jacobson, T.E.; Krol, A.J. A contemporary review of the factors involved in complete denture retention, stability, and support. Part I: Retention. J. Prosthet. Dent. 1983, 49, 5–15. [Google Scholar] [CrossRef] [PubMed]
- Jacobson, T.E.; Krol, A.J. A contemporary review of the factors involved in complete dentures. Part II: Stability. J. Prosthet. Dent. 1983, 49, 165–172. [Google Scholar] [CrossRef] [PubMed]
- Freeman, S.P. Impressions for complete dentures. J. Am. Dent. Assoc. 1969, 79, 1173–1178. [Google Scholar] [CrossRef] [PubMed]
- Boucher, C.O. Complete denture impressions based upon the anatomy of the mouth. J. Am. Dent. Assoc. 1944, 31, 1174–1181. [Google Scholar] [CrossRef]
- Boucher, C.O. A critical analysis of mid-century impression techniques for full dentures. J. Prosthet. Dent. 1951, 1, 472–491. [Google Scholar] [CrossRef] [PubMed]
- Abe, J. Clinical denture fabrication to achieve an effective suction of the mandibular complete denture: Enhancement of the posterior end border seal around the retromolar pad. Ann. Jpn. Prosthodont. Soc. 2011, 3, 220–230. [Google Scholar] [CrossRef]
- Zandinejad, A.; Floriani, F.; Lin, W.S.; Naimi-Akbar, A. Clinical outcomes of milled, 3D-printed, and conventional complete dentures in edentulous patients: A systematic review and meta-analysis. J. Prosthodont. 2024, 33, 736–747. [Google Scholar] [CrossRef] [PubMed]
- Lo Russo, L.; Salamini, A.; Troiano, G.; Guida, L. Digital dentures: A protocol based on intraoral scans. J. Prosthet. Dent. 2021, 125, 597–602. [Google Scholar] [CrossRef] [PubMed]
- Lo Russo, L.; Salamini, A. Removable complete digital dentures: A workflow that integrates open technologies. J. Prosthet. Dent. 2018, 119, 727–732. [Google Scholar] [CrossRef] [PubMed]
- Tripathi, A.; Singh, S.V.; Aggarwal, H.; Gupta, A. Effect of mucostatic and selective pressure impression techniques on residual ridge resorption in individuals with different bone mineral densities: A prospective clinical pilot study. J. Prosthet. Dent. 2019, 121, 90–94. [Google Scholar] [CrossRef] [PubMed]
- LoRusso, L.; Caradonna, G.; Troiano, G.; Salamini, A.; Guida, L.; Ciavarella, D. Three-dimensional differences between intraoral scans and conven tional impressions of edentulous jaws: A clinical study. J. Prosthet. Dent. 2020, 123, 264–268. [Google Scholar] [CrossRef] [PubMed]
- Thu, K.M.; Molinero-Mourelle, P.; Yeung, A.W.K.; Abou-Ayash, S.; Lam, W.Y.H. Which clinical and laboratory procedures should be used to fab ricate digital complete dentures? A systematic review. J. Prosthet. Dent. 2024, 132, 922–938. [Google Scholar] [CrossRef] [PubMed]
- Lo Russo, L.; Guida, L.; Ronsivalle, V.; Ercoli, C. Digital denture with mucostatic base and functional borders: A cast-free digital technique. J. Prosthodont. [CrossRef]
- Jamjoom, F.Z.; Aldghim, A.; Aldibasi, O.; Yilmaz, B. Impact of intraoral scanner, scanning strategy, and scanned arch on the scan accuracy of edentulous arches: An in vitro study. J. Prosthet. Dent. 2024, 131, 1218–1225. [Google Scholar] [CrossRef] [PubMed]
- Al Hamad, K.Q.; Al-Kaff, F.T. Trueness of intraoral scanning of edentulous arches: A comparative clinical study. J. Prosthodont. 2023, 32, 26–31. [Google Scholar] [CrossRef] [PubMed]
- Zarone, F.; Ruggiero, G.; Ferrari, M.; Mangano, F.; Joda, T.; Sorrentino, R. Accuracy of a chairside intraoral scanner compared with a laboratory scanner for the completely edentulous maxilla: An in vitro 3-dimensional comparative analysis. J. Prosthet. Dent. 2020, 124, 761.e1–761.e7. [Google Scholar] [CrossRef] [PubMed]
- Sorrentino, R.; Ruggiero, G.; Leone, R.; Irene Di Mauro, M.; Cagidiaco, E.F.; Joda, T.; Lo Russo, L.; Zarone, F. Influence of different palatal morphologies on the accuracy of intraoral scanning of the edentulous maxilla: A three-dimensional analysis. J. Prosthodont. Res. 2024, 68, 634–642. [Google Scholar] [CrossRef] [PubMed]
- Lo Russo, L.; Sorrentino, R.; Esperouz, F.; Zarone, F.; Ercoli, C.; Guida, L. Assessment of distortion of intraoral scans of edentulous mandibular arch made with a 2-step scanning strategy: A clinical study. J. Prosthet. Dent. [CrossRef]
- Abe, J.; Kokubo, K.; Sato, D. Mandibular suction-effective denture: The professional. Quintessence Publishing: Tokyo, Japan, 2012.
- Naert, I.; Gizani, S.; Vuylsteke, M.; Van Steenberghe, D. A 5-year prospective randomized clinical trial on the influence of splinted and unsplinted oral implants retaining a mandibular overdenture: Prosthetic aspects and patient satisfaction. J. Oral. Rehabil. 1999, 26, 195–202. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).