Submitted:
18 November 2024
Posted:
20 November 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Statistical Analysis
2.3. Ethical Statement
3. Results
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kim KM, Arghami A, Habib R, et al. The Society of Thoracic Surgeons Adult Cardiac Surgery Database: 2022 Update on Outcomes and Research. Ann Thorac Surg. Published online 2023.
- Wu J, Cong X, Lou Z, Zhang M. Trend and Impact of Concomitant CABG and Multiple-Valve Procedure on In-hospital Outcomes of SAVR Patients. Front Cardiovasc Med. 2021;8(740084). [CrossRef]
- Melly L, Torregrossa G, Lee T, Jansens JL, Puskas JD. Fifty years of coronary artery bypass grafting. J Thorac Dis. 2018;10(3):1960-1967. [CrossRef]
- Ma WG, Hou B, Abdurusul A. Dysfunction of mechanical heart valve prosthesis: experience with surgical management in 48 patients. J Thorac Dis. 2015;7(12):2321-2329. [CrossRef]
- Maribas P. Management of prosthetic heart valve obstruction: Speech for the surgery? Arch Cardiovasc Dis. 2009;102:255-257.
- Harik L, Perezgrovas-Olaria R, G S Jr. Graft thrombosis after coronary artery bypass surgery and current practice for prevention. Front Cardiovasc Med. 2023;10(1125126). [CrossRef]
- Aschacher T, Baranyi U, Aschacher O, Eichmair E, Messner B, Zimpfer D. A novel endothelial damage inhibitor reduces oxidative stress and improves cellular integrity in radial artery grafts for coronary artery bypass. Front Cardiovasc Med. 2021;8(736503). [CrossRef]
- Ali MR, Nacer H, Lawson CA, Khunti K. Racial and Ethnic Disparities in Primary Prevention of Cardiovascular Disease. Can J Cardiol Published online February. 2024;2. [CrossRef]
- Javed Z, Haisum Maqsood M, Yahya T. Race, Racism, and Cardiovascular Health: Applying a Social Determinants of Health Framework to Racial/Ethnic Disparities in Cardiovascular Disease. Circ Cardiovasc Qual Outcomes. 2022;15(1). [CrossRef]
- Mehtsun WT, Figueroa JF, Zheng J, Orav EJ, Jha AK. Racial disparities in surgical mortality: the gap appears to have narrowed. Health Aff (Millwood. 2017;36:1057-1064.
- Khera R, Vaughan-Sarrazin M, Rosenthal GE, Girotra S. Racial disparities in outcome after cardiac surgery: the role of hospital quality. Curr Cardiol Rep. 2015;17(29).
- Shah NS, Lloyd-Jones DM, O’Flaherty M. Trends in Cardiometabolic Mortality in the United States, 1999-2017 [published correction appears in JAMA. JAMA. 2019;2019;322(8):780-782. [CrossRef]
- Woodruff RC, Tong X, Khan SS. Trends in Cardiovascular Disease Mortality Rates and Excess Deaths, 2010-2022. Am J Prev Med. 2024;66(4):582-589. [CrossRef]
- Scott SS, Gouchoe DA, Azap L, et al. Racial and Ethnic Disparities in Peri-and Post-operative Cardiac Surgery. Curr Cardiovasc Risk Rep. 2024;18(7):95-113. [CrossRef]
- Rangrass G, Ghaferi AA, Dimick JB. Explaining racial disparities in outcomes after cardiac surgery: the role of hospital quality. JAMA Surg. 2014;149(3):223-227. [CrossRef]
- Mehta RH, Shahian DM, Sheng S, et al. Association of Hospital and Physician Characteristics and Care Processes With Racial Disparities in Procedural Outcomes Among Contemporary Patients Undergoing Coronary Artery Bypass Grafting Surgery. Circulation. 2016;133(2):124-130. [CrossRef]
- Trivedi AN, Sequist TD, Ayanian JZ. Impact of Hospital Volume on Racial Disparities in Cardiovascular Procedure Mortality. Journal of the American College of Cardiology. 2006;47(2):417-424. [CrossRef]
- Castellanos LR, Normand SLT, Ayanian JZ. Racial and Ethnic Disparities in Access to Higher and Lower Quality Cardiac Surgeons for Coronary Artery Bypass Grafting. The American Journal of Cardiology. 2009;103(12):1682-1686. [CrossRef]
- Berger A, MacCarthy PA, Siebert U, et al. Long-Term Patency of Internal Mammary Artery Bypass Grafts: Relationship With Preoperative Severity of the Native Coronary Artery Stenosis. Circulation. 2004;110(11_suppl_1). [CrossRef]
- Ruel M, Rubens FD, Masters RG, Pipe AL, Bédard P, Mesana TG. Late incidence and predictors of persistent or recurrent heart failure in patients with mitral prosthetic valves. J Thorac Cardiovasc Surg. 2004;128(2):278-283. [CrossRef]
- Zaouter C, Oses P, Assatourian S, Labrousse L, Rémy A, Ouattara A. Reduced Length of Hospital Stay for Cardiac Surgery-Implementing an Optimized Perioperative Pathway: Prospective Evaluation of an Enhanced Recovery After Surgery Program Designed for Mini-Invasive Aortic Valve Replacement. J Cardiothorac Vasc Anesth. Published online 2019.
- Sutton TS, McKay RG, Mather J, et al. Enhanced Recovery After Surgery Is Associated With Improved Outcomes and Reduced Racial and Ethnic Disparities After Isolated Coronary Artery Bypass Surgery: A Retrospective Analysis With Propensity-Score Matching. Journal of Cardiothoracic and Vascular Anesthesia. 2022;36(8):2418-2431. [CrossRef]
- Mehaffey JH, Hawkins RB, Charles EJ, et al. Distressed communities are associated with worse outcomes after coronary artery bypass surgery. The Journal of Thoracic and Cardiovascular Surgery. 2020;160(2):425-432.e9. [CrossRef]
- Hannan EL, Wu Y, Cozzens K, et al. The Association of Socioeconomic Factors With Outcomes for Coronary Artery Bypass Surgery. The Annals of Thoracic Surgery. 2022;114(4):1318-1325. [CrossRef]
- Connolly TM, White RS, Sastow DL, Gaber-Baylis LK, Turnbull ZA, Rong LQ. The Disparities of Coronary Artery Bypass Grafting Surgery Outcomes by Insurance Status: A Retrospective Cohort Study, 2007–2014. World j surg. 2018;42(10):3240-3249. [CrossRef]
- Cohen BD, Zeymo A, Bouchard M, et al. Increased Access to Cardiac Surgery Did Not Improve Outcomes: Early Look Into Medicaid Expansion. The Annals of Thoracic Surgery. 2022;114(5):1637-1644. [CrossRef]
- Bach PB, Pham HH, Schrag D, Tate RC, Hargraves JL. Primary Care Physicians Who Treat Blacks and Whites. N Engl J Med. 2004;351(6):575-584. [CrossRef]
- Brennan JM, Bryant A, Boero I, et al. RACE AND SEX-BASED DISPARITIES PERSIST IN THE TREATMENT OF PATIENTS WITH SEVERE, SYMPTOMATIC AORTIC VALVE STENOSIS. Journal of the American College of Cardiology. 2019;73(9):1207. [CrossRef]
- Cruz Rodriguez B, Acharya P, Salazar-Fields C, Horne A. Comparison of Frequency of Referral to Cardiothoracic Surgery for Aortic Valve Disease in Blacks, Hispanics, and Whites. Am J Cardiol. 2017;120(3):450-455. [CrossRef]
- Sleder A, Tackett S, Cerasale M, et al. Socioeconomic and Racial Disparities: a Case-Control Study of Patients Receiving Transcatheter Aortic Valve Replacement for Severe Aortic Stenosis. J Racial and Ethnic Health Disparities. 2017;4(6):1189-1194. [CrossRef]
- Nathan AS, Yang L, Yang N, et al. Racial, Ethnic, and Socioeconomic Disparities in Access to Transcatheter Aortic Valve Replacement Within Major Metropolitan Areas. JAMA Cardiol. 2022;7(2):150. [CrossRef]
- Gupta A, Mori M, Wang Y, et al. Racial/Ethnic Disparities in Aortic Valve Replacement Among Medicare Beneficiaries in the United States, 2012-2019. Am J Med. 2024;137(4):321-330.e7. [CrossRef]
- Milam AJ, Ogunniyi MO, Faloye AO, et al. Racial and Ethnic Disparities in Perioperative Health Care Among Patients Undergoing Cardiac Surgery. Journal of the American College of Cardiology. 2024;83(4):530-545. [CrossRef]
- Aragam KG, Dai D, Neely ML, et al. Gaps in referral to cardiac rehabilitation of patients undergoing percutaneous coronary intervention in the United States. J Am Coll Cardiol. 2015;65(19):2079-2088. [CrossRef]
- Chindhy S, Taub PR, Lavie CJ, Shen J. Current challenges in cardiac rehabilitation: strategies to overcome social factors and attendance barriers. Expert Rev Cardiovasc Ther. 2020;18(11):777-789. [CrossRef]
- Garfein J, Guhl EN, Swabe G, et al. Racial and Ethnic Differences in Cardiac Rehabilitation Participation: Effect Modification by Household Income. J Am Heart Assoc. 2022;11(13):e025591. [CrossRef]
- Ritchey MD, Maresh S, McNeely J, et al. Tracking Cardiac Rehabilitation Participation and Completion Among Medicare Beneficiaries to Inform the Efforts of a National Initiative. Circ Cardiovasc Qual Outcomes. 2020;13(1):e005902. [CrossRef]
- Roudaut R, Lafitte S, Roudaut MF. Management of prosthetic heart valve obstruction: fibrinolysis versus surgery. Early results and long-term follow-up in a single-centre study of 263 cases. Arch Cardiovasc Dis. 2009;102:269-277.
- Rizzoli G, Guglielmi C, Toscano G. Reoperations for acute prosthetic thrombosis and pannus: an assessment of rates, relationship and risk. Eur J Cardiothorac Surg. 1999;16:74-80.
- Essien UR, Holmes DN, Jackson LR, et al. Association of Race/Ethnicity With Oral Anticoagulant Use in Patients With Atrial Fibrillation: Findings From the Outcomes Registry for Better Informed Treatment of Atrial Fibrillation II. JAMA Cardiol. 2018;3(12):1174-1182. [CrossRef]
- Schauer DP, Johnston JA, Moomaw CJ, Wess M, Eckman MH. Racial disparities in the filling of warfarin prescriptions for nonvalvular atrial fibrillation. Am J Med Sci. 2007;333(2):67-73. [CrossRef]
- Nathan AS, Geng Z, Dayoub EJ. Racial, Ethnic, and Socioeconomic Inequities in the Prescription of Direct Oral Anticoagulants in Patients With Venous Thromboembolism in the United States. Circ Cardiovasc Qual Outcomes. 2019;12(4). [CrossRef]
- Reynolds KR, Khosrow-Khavar F, Dave CV. Racial and Ethnic Disparities in Initiation of Direct Oral Anticoagulants Among Medicare Beneficiaries. JAMA Network Open. 2024;2024;7(5):e249465. [CrossRef]
- Stevens SM, Woller SC, Baumann Kreuziger L. Executive Summary: Antithrombotic Therapy for VTE Disease: Second Update of the CHEST Guideline and Expert Panel Report. Chest. 2021;160(6):2247-2259. [CrossRef]
- Meschia JF, Merrill P, Soliman EZ. Racial disparities in awareness and treatment of atrial fibrillation: the REasons for Geographic and Racial Differences in Stroke (REGARDS) study. Stroke. 2010;41(4):581-587. [CrossRef]
- Essien UR, Kim N, Magnani JW. Association of Race and Ethnicity and Anticoagulation in Patients With Atrial Fibrillation Dually Enrolled in Veterans Health Administration and Medicare: Effects of Medicare Part D on Prescribing Disparities. Circ Cardiovasc Qual Outcomes. 2022;15(2). [CrossRef]
- Jha AK, Epstein AM. A survey of board chairs of English hospitals shows greater attention to quality of care than among their US counterparts. Health Aff (Millwood. 2013;32(4):677-685. [CrossRef]
- Revankar S, Agarwala A. Stepping Away from the Monolith: The Disaggregation of Asian Cardiovascular Data. Am J Cardiol. 2024;219:120-122. [CrossRef]
- Min LY, Islam RB, Gandrakota N, Shah MK. The social determinants of health associated with cardiometabolic diseases among Asian American subgroups: a systematic review. BMC Health Serv Res. 2022;2022;22(1):257. [CrossRef]
- Ghisi GLM, Chaves GSDS, Britto RR, Oh P. Health literacy and coronary artery disease: A systematic review. Patient Educ Couns. 2018;101(2):177-184. [CrossRef]
- Marcolino M, Sales T, Rios D, et al. Health Literacy, Patient Knowledge and Adherence to Oral Anticoagulation in Primary Care. International Journal of Cardiovascular Sciences. 2023;36:10 36660 20220158.
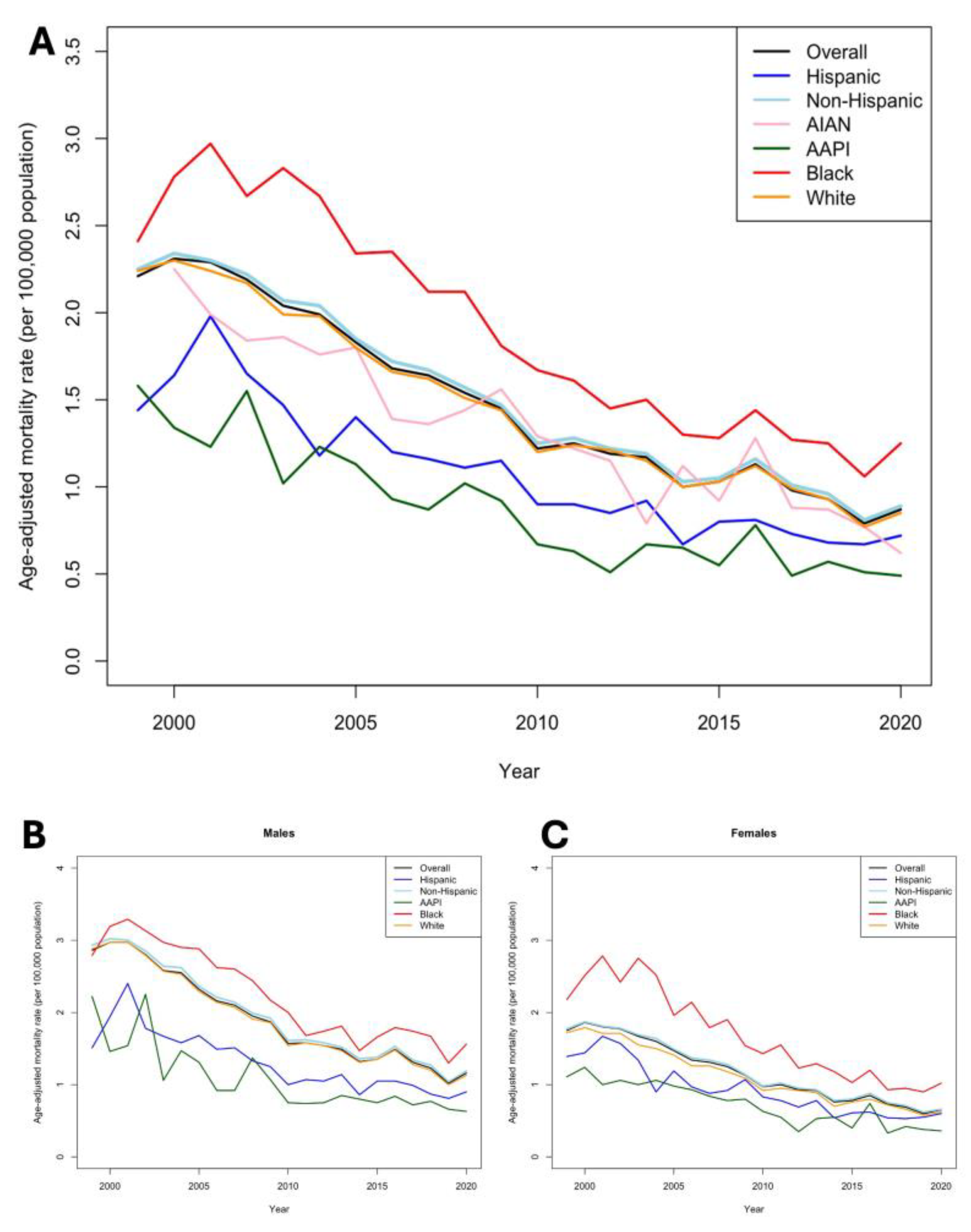
| AGE-ADJUSTED MORTALITY RATE PER 100,000 (95% CI) | RELATIVE PERCENT CHANGE (95% CI) |
ANNUAl AVERAGE PERCENT CHANGE (P-VALUE) | ||
|---|---|---|---|---|
| 1999 | 2020 | |||
| TOTAL | 2.21 (2.16-2.27) | 0.88 (1.05-0.88) | -60.18 (51.39-61.23) | -9.5 (p<0.03) |
| RACE AND ETHNIC GROUP | ||||
| WHITE | 2.26 (2.2-2.32) | 0.83 (0.8-0.86) | -63.27 (62.93-63.63) | -9.7 (p<0.001) |
| BLACK | 2.45 (2.24-2.64) | 1.31 (1.2-1.42) | -46.53 (46.21-46.62) | -11.3 (p<0.001) |
| HISPANIC | 1.44 (1.24-1.64) | 0.72 (0.63-0.8) | -50.00 (49.19-51.22) | -6.8 (p<0.03) |
| NON-HISPANIC | 2.26 (2.2-2.32) | 0.89 (0.85-0.92) | -60.62 (60.34-61.36) | -9.3 (p<0.001) |
| AIAN | 2.37 (1.61-3.36) | 0.95 (0.61-1.42) | -59.92 (57.74-62.11) | -9.2 (p<0.001) |
| AAPI | 1.58 (1.26-1.9) | 0.48 (0.39-0.57) | -69.62 (69.05-70.00) | -6.2 (p<0.04) |
| SEX | ||||
| FEMALE | 1.75 (1.69-1.82) | 0.65 (0.61-0.68) | -62.86 (62.64-63.91) |
-6.2 (p<0.04) |
| MALE | 2.86 (2.76-2.96) | 1.16 (1.11-1.21) | -59.44 (59.12-59.78) |
-8.9 (p<0.01) |
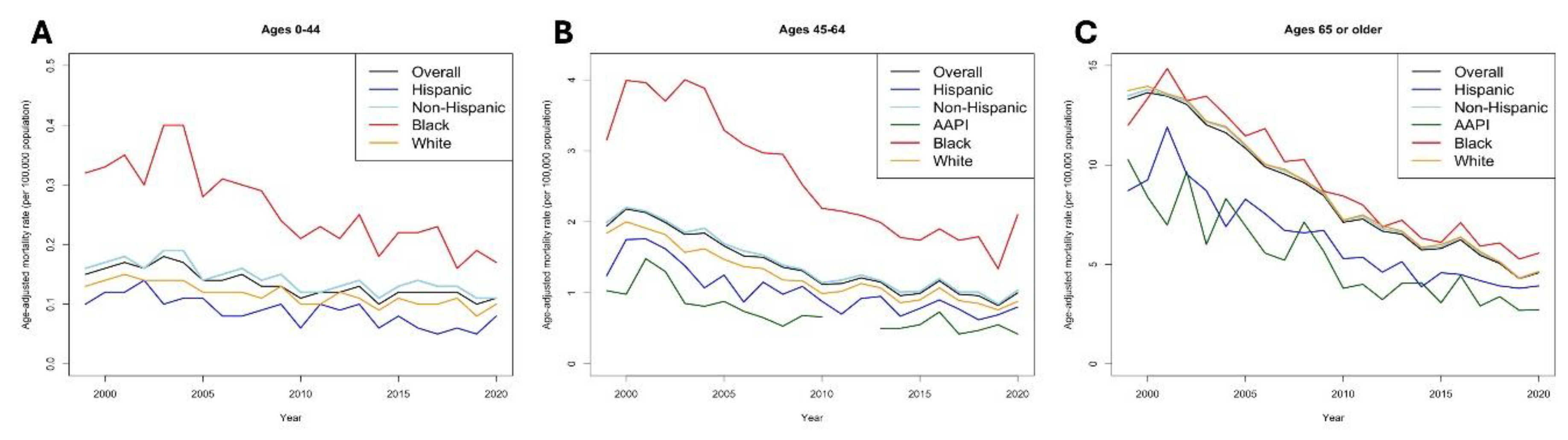
| AGE GROUP (YEARS) | ||||
| 0-44 | 0.15 (0.13-0.17) | 0.1 (0.09-0.12) | -33.33 (29.41-33.76) | -1.2 (p=0.55) |
| 45-64 | 1.96 (1.85-2.08) | 1.05 (0.98-1.12) | -46.43 (46.15-47.03) | -3.5 (p<0.04) |
| >65 | 13.31 (12.92-13.69) | 4.58 (4.4-4.76) | -65.59 (65.23-65.94) | -11.7 (p<0.001) |
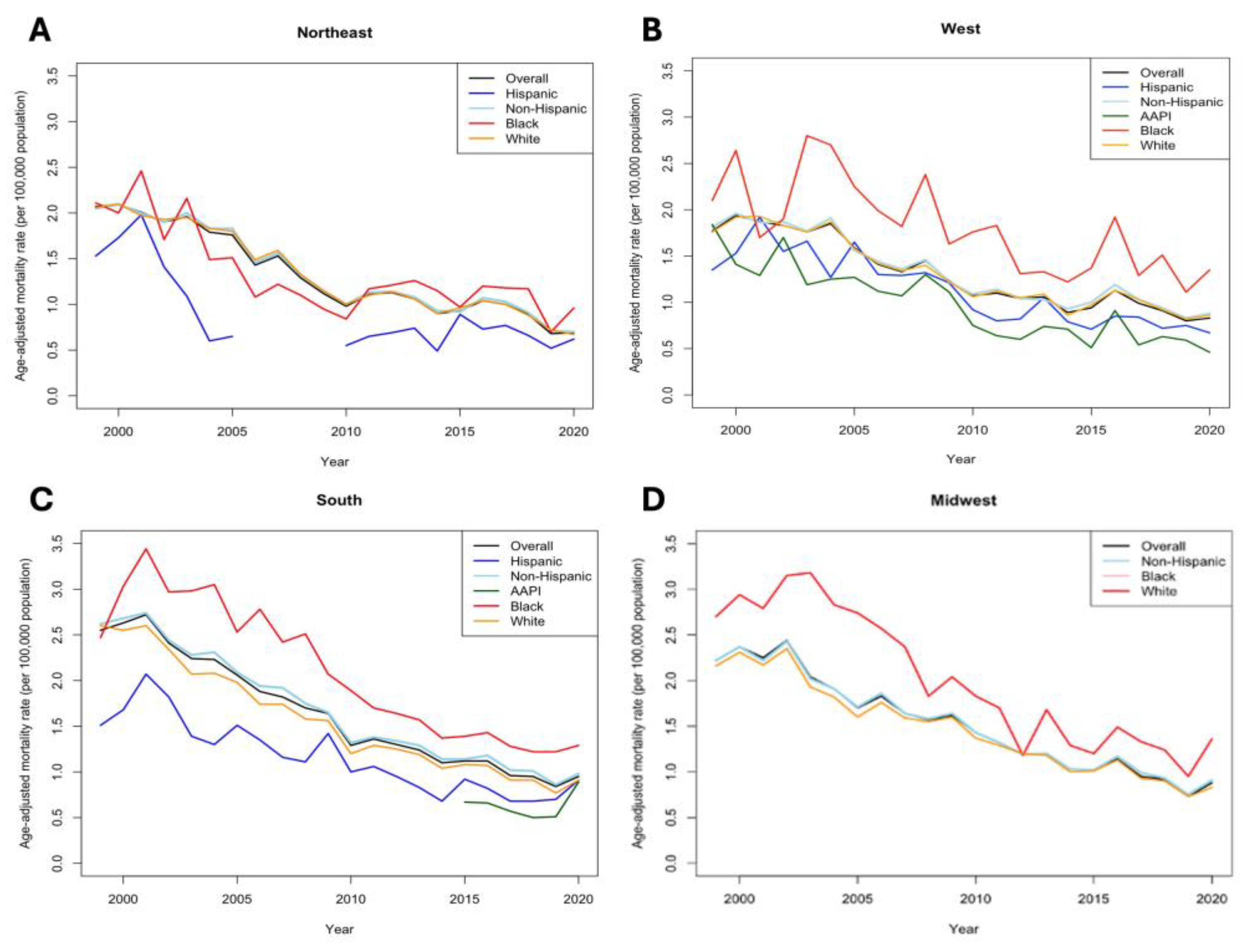
| US CENSUS REGIONS | ||||
| NORTHEAST | 2.07 (1.95-2.18) | 0.69 (0.63-0.76) | -66.67 (65.14-67.69) | -8.9 (p<0.001) |
| MIDWEST | 2.22 (2.11-2.34) | 0.88 (0.82-0.94) | -60.36 (59.83-61.14) | -2.1 (p=0.53) |
| SOUTH | 2.55 (2.45-2.65) | 0.95 (0.9-1.0) | -62.75 (62.26-63.27) | -10.2 (p<0.001) |
| WEST | 1.77 (1.66-1.88) | 0.83 (0.77-0.89) | -53.11 (52.66-53.61) | -6.3 (p<0.04) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





