1. Introduction
1.1. Background and Rationale
Chronic ischemic cardiovascular disease (CICD) is one of the most common conditions worldwide, and a frequent cause of hospitalization in patients 65y.o., with significant differences observed between men and women. It is also a critical comorbidity, influencing both the length of hospital stay and patient mortality. [
1]
CICD originates from impaired coronary circulation, typically caused by the formation of atherosclerotic plaques in the coronary arteries. [
2] A transient mismatch causing reversible myocardial ischemia is its dominant feature; CICD is also characterized by stable symptoms over a period of months, years, or even decades. Stable angina is CICD most frequent presentation; other clinical presentations are microvascular angina, vasospastic angina, and ischemic cardiomyopathy. [
3] Several risk factors are linked to CICD, including hypertension, diabetes mellitus, dyslipidemia, chronic obstructive pulmonary disease, smoking, and genetic predisposition. Adopting a healthy lifestyle, managing risk factors, and regular monitoring are all crucial for CICD prevention. [
4]
The staples of CICD treatment are myocardial perfusion improvement, symptoms alleviation, and prevention of complications. Therapeutic options include risk factors management, pharmacological therapy, revascularization procedures such as coronary angioplasty, surgical interventions such as coronary artery bypass grafting, and cardiac rehabilitation. [
5]
The prognosis of CICD depends on the severity of the disease and the effectiveness of the treatment. Proper management can enhance quality of life, reduce the risk of cardiac events, and prolong survival. However, CICD requires long-term monitoring and continuous management to prevent disease progression. [
6]
The direct costs of hospitalization for CICD can vary significantly depending on various factors, including geographic region, hospital infrastructure, disease severity, length of stay, and specific treatments administered. The patient population admitted to Internal Medicine departments, which largely consists of elderly individuals with multiple coexisting chronic conditions—often exacerbated and accompanied by critical episodes of clinical instability and functional organ deficits—means that real-life cases are often excluded from the guidelines designed for individual pathologies, as these do not reflect the evidence of large clinical trials. [
7]
1.2. Study Objectives
Especially after COVID-19 pandemic, whose toll was heavy on both territorial care and acute hospital facilities, the importance and role of Internal Medicine adequate management has been strengthened. [
8,
9,
10] Since cardiovascular diseases represent a worldwide leading cause of death, and are preventable through lifestyle modifications, we decided to focus on their economic and organizational impact. [
11]
Objective of this study is to describe the epidemiology of patients with Chronic Ischemic Cardiovascular Disease (CICD) admitted to internal medicine departments that manage this condition (Internal Medicine, Cardiology, Geriatrics), assessing potential discrepancies in terms of comorbidities, length of hospitalization, and epidemiological characteristics. In particular, comorbidities and age and gender differences were analyzed as they were previously linked with differences in treatment and outcome of cardiovascular diseases. [
12]
Since the main focus is on inpatients management, this study does not consider the impact on emergency services, including the activities carried out in the Emergency Department that do not result in acute care hospital admissions, nor does it cover outpatient, day-care, or home-based services.
2. Materials and Methods
2.1. Study Design, Population and Data Sources
This is a retrospective ecological study, conducted using an existing national administrative database. The data used pertains to all hospital admissions in the designated departments (Internal Medicine, Geriatrics, Cardiology) of public and private healthcare facilities across Italy in the year 2019.
The data was collected anonymously from the Hospital Discharge Records (Schede di Dimissione Ospedaliera, SDO) database managed by the Italian Ministry of Health. SDO database system was established by the Ministerial Decree of December 28, 1991, as a standard for gathering information on every discharged patient, from either public or private healthcare institutions, across the entire national territory. As Italian National Healthcare service is a Beveridge system, the SDO database is based on the ICD-9-CM classification system, coupled with the Diagnosis-Related Group (DRG) coding system.
The collected data includes demographic characteristics of the patients (age, gender, residence, education level), hospitalization details (institution and specialty at discharge, admission type, discharge method), and clinical characteristics (primary diagnosis, comorbidities, diagnostic or therapeutic procedures).
The data was extracted by distinguishing between the primary diagnosis (the main cause for admission) and secondary diagnoses (conditions present that were not the direct cause of hospitalization but potentially contributed to clinical and/or organizational complexity).
SDO data was used to extract data related to cardiovascular diagnoses from Internal Medicine, Cardiology, and Geriatrics departments. Data from other departments was excluded, as the focus of this study is the evaluation of complex patients. According to the definition adopted by the Agency for Healthcare Research and Quality (AHRQ), a complex patient is a person suffering from two or more chronic diseases, in which each of the morbid conditions present is able to influence the outcome of the treatments of the other co-existing ones. This may happen through various modalities: limitation of life expectancy, increased intercurrent morbidity, interactions between pharmacological therapies , impossibility of full use of adequate treatments due to contraindications. [
13]
2.2. Statistical Analysis
Data related to hospitalization episodes across the three ward types were presented in aggregated form, categorized by department type, the proportion of patients with Chronic Ischemic Cardiovascular Disease (CICD), and by gender. Mean values and percentages were reported as appropriate. The economic output generated by the DRG (Diagnosis-Related Groups) was calculated using the reimbursement rates provided by the National Health System for each hospital admission episode.
Results were processed and presented descriptively; since data from the entire population was available, no inferential analysis was required.
3. Results
3.1. Hospitaliztions
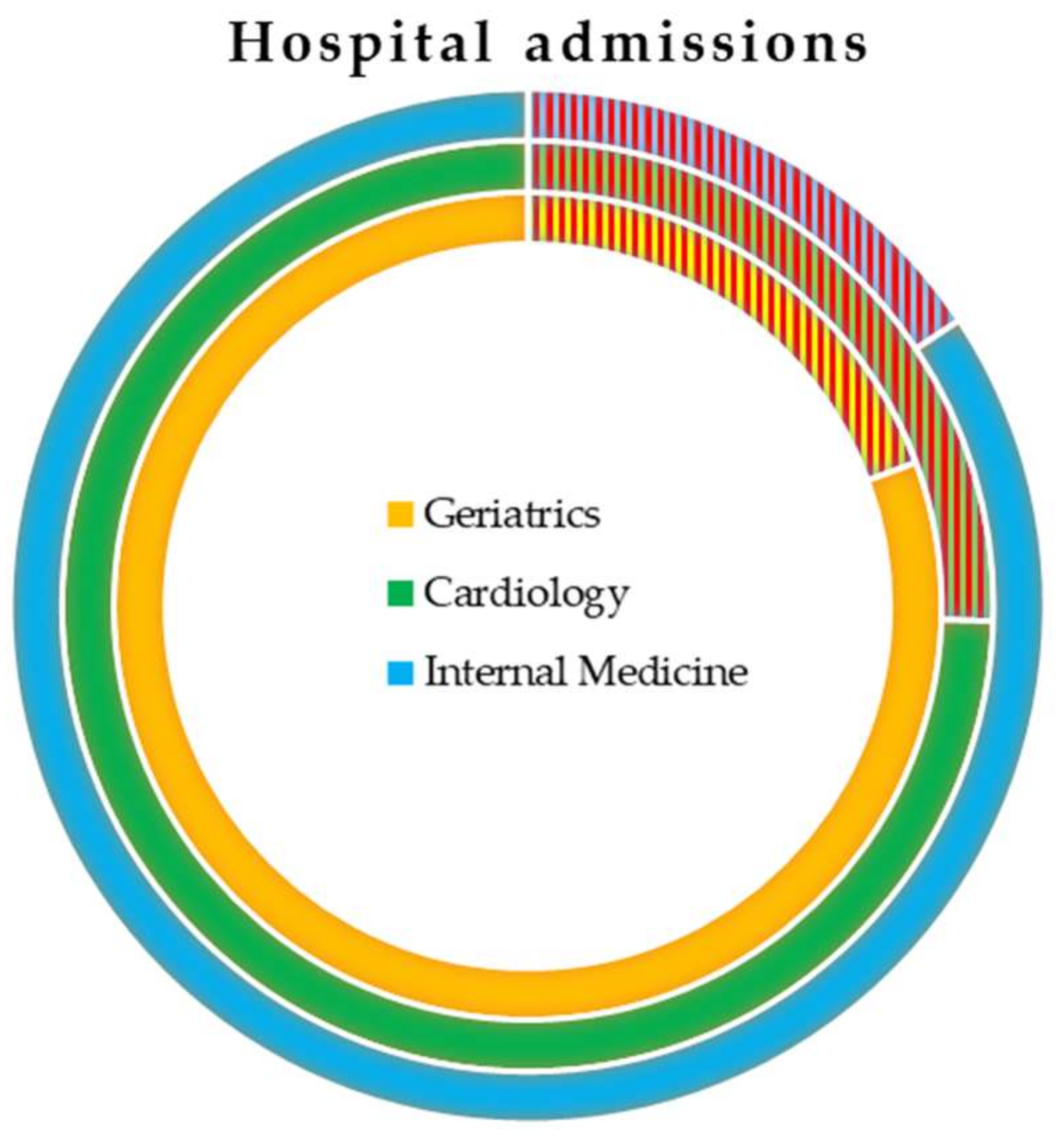
In 2019, the Internal Medicine, Cardiology, and Geriatrics wards generated 1,593,446 hospital admissions. Of these, 18.8% had a diagnosis of CICD (
Figure 1).
CICD accounted for 15% of hospitalizations in Internal Medicine, 19.4% in Geriatrics, and 25% in Cardiology. The highest number of patients was admitted to Internal Medicine (157,000), compared to 118,000 in Cardiology and 25,000 in Geriatrics. In Cardiology, CICD was recorded as the primary diagnosis in almost half of cases; in Internal Medicine and Geriatrics, this figure was close to one third (
Table 1).
While the highest proportion of CICD hospitalizations was observed in Cardiology departments, followed by Geriatrics, the largest volume of cases occurred in Internal Medicine. The average length of stay for CICD patients slightly exceeded the overall departmental averages: 10.5 days compared to 10.0 in Internal Medicine, and 6.8 days versus 5.9 in Cardiology. The average length of stay was longer in Geriatrics and Internal Medicine departments, particularly in cases where CICD was not the primary diagnosis but rather a comorbidity.
Patients with CICD tended to be older than the average patient in these departments. In Internal Medicine, CICD patients had an average age of 81 years, compared to a departmental average of 75; in Cardiology, the average age was 72 years compared to 69; and in Geriatrics, CICD patients had an average age of 85 years, compared to a departmental average of 84 (
Table 1).
Internal Medicine and Geriatrics wards had a similar pattern of comorbidities, with the most frequently observed condition being Acute Respiratory Failure (12.8% of cases), followed by Atrial Fibrillation (10.3%), Pneumonia and Bronchopneumonia (6.6%), Chronic Acute Respiratory Failure (4.7%), Exacerbated COPD (3.4%), and Chronic Renal Failure (2.9%). In contrast, Cardiology hospitalizations exhibited a different pattern of comorbidities, with the most common being Atrial Fibrillation (10.9%), Left Heart Failure (6.2%), Coronary Atherosclerosis (6.1%), Benign Essential Hypertension (6.0%), and Diabetes (5.3%).
3.2. Economic Impact
The average cost per admission for patients with CICD is aligned with the overall ward averages in Internal Medicine (€3,527 vs €3,505) and Geriatrics (€3,640 vs €3,650). In Cardiology, however, the average cost per admission is higher, both in absolute terms and relative to the department’s average (€5,760 vs €5,280) (
Table 2).
In terms of total annual production generated by Internal Medicine, amounting to €3,516,982,171, the portion attributed to CICD hospitalizations is 15% (€555,264,058). Most of this expenditure incurred for patients with CICD as a secondary diagnosis (€411,301,495). Similarly, in Geriatrics, with a total production of €462,241,085, the share related to patients with CICD as the primary diagnosis was much smaller (5%) compared to those with CICD as a secondary diagnosis (14.3%). Overall, the expenditure for CICD amounted to €89,282,223. In Cardiology, however, with a total production of €2,447,596,863, the distribution of costs between patients with CICD as the primary and secondary diagnosis was more balanced (12.3% vs 15.5%), with a total expenditure of €681,416,923 for CICD.
3.3. Organizative Impact on Healthcare Facilities
The progressive aging of Italian population will likely lead to an increase in the volume of healthcare services related to both acute and chronic cardiovascular illnesses. However, in recent years, Italy has adopted health policies aimed at reducing behaviors which are known risk factors for ischemic heart disease, such as smoking, physical inactivity, alcohol consumption, and unbalanced diets. These factors still persist in the country, with significant North-South disparities and a notable impact on the younger population. [
14]
Compared to the pre-pandemic period, there has been a gradual reduction in hospital admissions due to Acute Myocardial Infarction. Similarly, the number of coronary artery bypass graft surgeries has decreased, although mortality rates have remained stable. Conversely, evidence of a shift toward a population with a higher prevalence of chronic conditions is reflected in the increasing number of valvuloplasty or valve replacement procedures, except during the pandemic period (2020-2021), likely due to the reprioritization of resources in healthcare facilities. [
15] In Italy, despite significant improvements in the emergency care system, the reduction in the number of hospital beds over the last 30 years, and the increase in the number of fragile patients have led to an increase in ED attendance, a significant proportion of which are inappropriate. [
16]. This means that many chronically ill patients get directed towards services that are structured to provide for acute care, but end up being clogged by patients whose health necessities are not otherwise provided, such as Emergency Departments. [
17] These inappropriate attendances drive up costs and increase system inefficiency. [
18,
19]
The current high prevalence of chronic ischemic heart disease in the Italian population, driven not only by the absolute rise in incidence due to aging but also by improved diagnostic and therapeutic capabilities that allow patients to survive acute phases, places a significant burden on healthcare facilities. Beyond the increased hospitalizations in medical wards, the impact on surgical activities should not be overlooked, with the potential need to upgrade service delivery settings for patients with chronic ischemic heart disease. Additionally, there is the potential for discharge challenges, as patients may require transfer to intermediate care facilities equipped to manage complex cases, necessitating an integrated care approach. [
20]
3.4. Gender Inequalities
According to the AHA Scientific Statement 2016, from 1979 to 2011, ischemic heart disease mortality was higher in women than in men, in line with European data, where cardiovascular disease prevalence is greater in women (51%) compared to men (42%). [
21] This trend is also evident in Italy, although with slightly lower percentages.
Acute Myocardial Infarction (AMI) is the leading cause of death in women worldwide, significantly worsening quality of life and leading to a high degree of morbidity due to heart failure. The clinical and instrumental approach to AMI and CICD is heavily influenced by studies conducted on male populations, with their findings indiscriminately applied to females. This approach fails to account for sex- and gender-specific differences that significantly influence the pathophysiology and clinical presentation of these conditions.
In Italy, we found that in Cardiology wards, women over 65 with a diagnosis of CICD represent about half the number of men over 65 (27,893 vs. 58,049), a situation that does not occur in Internal Medicine and Geriatrics. In Internal Medicine, there are 70,256 women over 65 compared to 75,120 men, while in Geriatrics, there are 12,893 women and 11,420 men. For patients under 65, women are consistently fewer than men, representing half the number of men in Internal Medicine and Geriatrics, and only about one-fifth in Cardiology (
Table 3).
It appears, therefore, that women undergo fewer revascularization procedures, which typically lead to hospitalization in Cardiology, despite having similar comorbidity profiles to men. This disparity could be attributed to scientific evidence and, consequently, clinical guidelines and recommendations that are primarily based on studies involving predominantly male subjects.
Regardless of age or sex, heart failure is treated predominantly and at twice the frequency in Internal Medicine and Geriatrics departments compared to Cardiology.
In Cardiology, the length of hospital stay for women over 65 is, on average, one day longer than for men, and 1.5 days longer in the under-65 age group, with an additional cost of approximately €500. These gender-based differences in length of stay are not observed in Geriatrics or Internal Medicine, where the average hospital stay for patients over 65 does not show significant gender disparities.
4. Discussion
4.1. Strengths and Limitations
This study uses data from a comprehensive national administrative database, providing a robust and representative dataset of hospital admissions across Italy for patients with CICD. This enhances the significance and generalizability of our findings, allowing to derive insights into the clinical and economic impacts of CICD across the different medical specialty wards. Furthermore, the study design facilitates an exploration of gender disparities in hospitalizations and treatments, a critical area that remains under-researched in the context of cardiovascular disease. The retrospective nature of the study, coupled with rigorous data collection methods, contributes to the accuracy and reliability of the reported hospitalization patterns and associated costs.
This study presents, however, some limitations. As a retrospective ecological study, the data primarily reflects historical practices and outcomes, which may not fully capture future evolution of clinical practices. Additionally, while the use of the SDO database ensures a broad coverage of hospital admissions, it may lack detailed clinical information regarding the severity of CICD and its comorbidities, potentially leading to an underestimation of the complexity associated with these patients. Finally, the reliance on administrative data may introduce coding inaccuracies, which could affect the interpretation of the results.
4.2. Interpretation and Generalizability
Management of chronic conditions is an ever-evolving challenge, especially in acute care settings and internal medicine wards. While many efforts are being directed in effective management of acute conditions, emphasizing both organizational and technological solutions, impact of chronic conditions on Health Systems as a whole is ever increasing, with difficulties in providing adequate care, especially in overburdened facilities. [
22,
23,
24]
On the other hand, the best of care to be provided is routinely established by evidence-based elements, and as such, the problem of gender bias in research may affect the day-to-day clinical practice. [
7] In patients with cardiovascular diseases, timely identification and evaluation are fundamental for adequate treatment based on gender, severity, state of illness and for risk reduction. [
12]
Nowadays, the typical profile of a medical patient with CICD is characterized by advanced age (average age 80 years), significant comorbidities, and an extended average length of stay (10.5 days). The average hospitalization value for CICD aligns closely with the average values in Internal Medicine and Geriatrics; however, in Cardiology, this average is significantly higher. CICD has a substantial impact on Internal Medicine, Cardiology, and Geriatrics, accounting for between 15% and 25% of both the number of hospitalizations and the economic value of activities. The total hospitalization costs amount to €1.3 billion, with over 40% (€555 million) occurring in Internal Medicine.
In Cardiology, women over 65 with a diagnosis of CICD represent about half the number of men over 65, a pattern not observed in Internal Medicine and Geriatrics. This disparity may suggest that existing guidelines are influenced by studies predominantly conducted on male samples, leading to fewer recommendations for interventional procedures in females.
5. Conclusions
CICD is still a major presence among patients in medical wards. It disproportionately affects elderly patients, leading to increase in hospital length of stay, complications during admission, and increased direct and indirect costs. Although fewer CICD cases are treated in Cardiology compared to other ward types, the costs there are significantly higher, particularly for patients undergoing advanced interventional procedures; this suggests that patients who necessitate a cardiology admission necessitate of a higher amount of resources. This may be due to their clinical presentation being more complex ab initio, or because Cardiology wards are more likely to treat acute exacerbations of CICD, whereas chronic complication of CICD ends up being admitted elsewhere; this is coherent with the proportions of primary and secondary diagnoses of CICD among the investigated wards. Therefore, especially considering the aging of population (in Italy, but also in the whole western world and even in Asia), the need for a sustainable healthcare system, able to effectively manage chronic illnesses both inside and outside the hospital setting, is paramount.
Finally, our work puts evidence on the gender inequalities still present in healthcare. While CICD prevalence and risk factors are the same among men and women, the latter are less likely to receive interventional procedures than men; this suggest the presence of potential gender bias among existing treatment guidelines, as they are mostly written with the bulk of evidence coming from men-dominated clinical trials.
Author Contributions
Conceptualization, FP, FR, FS, CC, DdA and AV; methodology, FS, DdA.; software, CC.; validation, CC, AV, and FR.; formal analysis, FS.; investigation, FS, CC, FP, AV, DdA.; resources, FS, AV, FR.; data curation, CC.; writing—original draft preparation, FP, AV, FR.; writing—review and editing, AV.; visualization, CC.; supervision, FS.; project administration, FS, AV, FR.; funding acquisition, FS, AV. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The datasets presented in this article are not readily available because are estracted by the national SDO Data that are available only after special permission. Requests to access the datasets should be directed to CREA Sanità, prof. Feedrico Spandonaro.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Komajda M, Weidinger F, Kerneis M, Cosentino F, Cremonesi A, Ferrari R, et al. EURObservational Research Programme: the Chronic Ischaemic Cardiovascular Disease Registry: Pilot phase (CICD-PILOT). Eur Heart J. 2016;37: 152–160. [CrossRef]
- Wang R, Zhou C, Parry M. Health locus of control and self-management behaviours among individuals with ischaemic heart disease: protocol for a scoping review. BMJ Open. 2023;13: e075277. [CrossRef]
- Crea F, Camici PG, De Caterina R, Lanza GA. Chronic Ischaemic Heart Disease. 2nd ed. In: Camm AJ, Lüscher TF, Serruys PW, editors. The ESC Textbook of Cardiovascular Medicine. 2nd ed. Oxford University PressOxford; 2009. pp. 597–664. [CrossRef]
- Siriwardhana C, Carrazana E, Liow K, Chen JJ. Racial/Ethnic Disparities in the Alzheimer’s Disease Link with Cardio and Cerebrovascular Diseases, Based on Hawaii Medicare Data. J Alzheimers Dis Rep. 2023;7: 1103–1120. [CrossRef]
- Komajda M, Cosentino F, Ferrari R, Kerneis M, Kosmachova E, Laroche C, et al. Profile and treatment of chronic coronary syndromes in European Society of Cardiology member countries: The ESC EORP CICD-LT registry. Eur J Prev Cardiol. 2021;28: 432–445. [CrossRef]
- Kerneis M, Cosentino F, Ferrari R, Georges J-L, Kosmachova E, Laroche C, et al. Impact of chronic coronary syndromes on cardiovascular hospitalization and mortality: the ESC-EORP CICD-LT registry. Eur J Prev Cardiol. 2022;29: 1945–1954. [CrossRef]
- Chilet-Rosell, E. Gender bias in clinical research, pharmaceutical marketing, and the prescription of drugs. Glob Health Action. 2014;7: 25484. [CrossRef]
- Vinci A, Pasquarella A, Corradi MP, Chatzichristou P, D’Agostino G, Iannazzo S, et al. Emergency Medical Services Calls Analysis for Trend Prediction during Epidemic Outbreaks: Interrupted Time Series Analysis on 2020–2021 COVID-19 Epidemic in Lazio, Italy. Int J Environ Res Public Health. 2022;19: 5951. [CrossRef]
- Ferron R, Agarwal G, Cooper R, Munkley D. The effect of COVID-19 on emergency medical service call volumes and patient acuity: a cross-sectional study in Niagara, Ontario. BMC Emerg Med. 2021;21: 39. [CrossRef]
- Pietrantonio F, Vinci A, Rosiello F, Alessi E, Pascucci M, Rainone M, et al. Green Line Hospital-Territory Study: A Single-Blind Randomized Clinical Trial for Evaluation of Technological Challenges of Continuous Wireless Monitoring in Internal Medicine, Preliminary Results. Int J Environ Res Public Health. 2021;18: 10328. [CrossRef]
- Kaminsky LA, German C, Imboden M, Ozemek C, Peterman JE, Brubaker PH. The importance of healthy lifestyle behaviors in the prevention of cardiovascular disease. Prog Cardiovasc Dis. 2022;70: 8–15. [CrossRef]
- Pietrantonio F, Ciamei A, Vinci A, Ciarambino T, Alessi E, Pascucci M, et al. Polypharmacy Management in a Gender Perspective: At the Heart of the Problem: Analysis of Major Cardiac Diseases, SARS-CoV-2 Affection and Gender Distribution in a Cohort of Patients in Internal Medicine Ward. Int J Environ Res Public Health. 2023;20: 5711. [CrossRef]
- Nardi R, Fabbri T, Belmonte G, Leandri P, Mazzetti M, Pasquale A, et al. Medicina interna, paziente complesso, evidence based medicine e le non evidenze. Ital J Med. 2009;3: 191–200. [CrossRef]
- Melchiorre MG, Socci M, Quattrini S, Lamura G, D’Amen B. Frail Older People Ageing in Place in Italy: Use of Health Services and Relationship with General Practitioner. Int J Environ Res Public Health. 2022;19: 9063. [CrossRef]
- AGENAS. Report PNE 2020. Ministero Della Salute. Available online: https://www.agenas.gov.it/images/agenas/In%20primo%20piano/PNE/2020/Agenas_Report_PNE_2020.pdf.
- di Bella E, Gandullia L, Leporatti L, Locatelli W, Montefiori M, Persico L, et al. Frequent use of emergency departments and chronic conditions in ageing societies: a retrospective analysis based in Italy. Popul Health Metr. 2020;18: 29. [CrossRef]
- Furia G, Vinci A, Colamesta V, Papini P, Grossi A, Cammalleri V, et al. Appropriateness of frequent use of emergency departments: A retrospective analysis in Rome, Italy. Front Public Health. 2023;11: 1150511. [CrossRef]
- Giulio de Belvis A, Meregaglia M, Morsella A, Adduci A, Perilli A, Cascini F, et al. Italy: Health System Review. Health Syst Transit. 2022;24: 1–236.
- McDonagh MS, Smith DH, Goddard M. Measuring appropriate use of acute beds. A systematic review of methods and results. Health Policy Amst Neth. 2000;53: 157–184. [CrossRef]
- Boccardi V, Mecocci P. Intermediate Care in Italy: Addressing the Challenges and Opportunities for Person-Tailored Care. Geriatr Basel Switz. 2023;8: 59. [CrossRef]
- Mehta LS, Beckie TM, DeVon HA, Grines CL, Krumholz HM, Johnson MN, et al. Acute Myocardial Infarction in Women: A Scientific Statement From the American Heart Association. Circulation. 2016;133: 916–947. [CrossRef]
- Pietrantonio F, Vinci A, Maurici M, Ciarambino T, Galli B, Signorini A, et al. Intra- and Extra-Hospitalization Monitoring of Vital Signs—Two Sides of the Same Coin: Perspectives from LIMS and Greenline-HT Study Operators. Sensors. 2023;23: 5408. [CrossRef]
- Onen-Dumlu Z, Harper AL, Forte PG, Powell AL, Pitt M, Vasilakis C, et al. Optimising the balance of acute and intermediate care capacity for the complex discharge pathway: Computer modelling study during COVID-19 recovery in England. Pietrantonio F, editor. PLOS ONE. 2022;17: e0268837. [CrossRef]
- Vinci A, Furia G, Cammalleri V, Colamesta V, Chierchini P, Corrado O, et al. Burden of delayed discharge on acute hospital medical wards: A retrospective ecological study in Rome, Italy. PloS One. 2024;19: e0294785. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).