Introduction
It has been nearly five years since Coronavirus disease 2019 (COVID-19) was first reported in Wuhan, China, in The so-called "COVID-19 crisis," during which COVID-19 dominated societal concerns, persisted for some time. However, since the reclassification of COVID-19 to Category 5 under Japan's Infectious Disease Control Law in May 2023, public interest in the virus appears to have waned, and society seems to have regained a sense of normalcy. Mask usage has declined, and the public now regards the "COVID-19 crisis" as largely a matter of the past. The author is very pleased to see that society has finally returned to a more normal state.
On the other hand, COVID-19 vaccination efforts will continue in the fall of 2024, with vaccines available to high-risk groups, including adults over 65 and individuals aged 60 to 64 who have certain underlying conditions (such as heart, kidney, or respiratory dysfunctions that significantly impair daily life, immune dysfunction caused by HIV). These groups have been made eligible for routine vaccination [1].
In response, the Japanese Society of Infectious Diseases, together with the Japanese Respiratory Society and the Japanese Society for Vaccinology, has issued a "Position Paper on Routine COVID-19 Vaccination in 2024," strongly recommending routine vaccination with the COVID-19 vaccine in Fall/Winter 2024, as COVID-19 is considered more severe and has a worse prognosis than influenza [2]. Additionally, the Japan Pediatric Society recommends vaccination for all children between 6 months and 17 years of age, including initial and booster doses at appropriate intervals [3]. The Pharmaceuticals and Medical Devices Agency (PMDA) also emphasizes the efficacy and safety of the COVID-19 vaccine [4].
However, as vaccination is now voluntary and individuals bear most of the cost—though some local government subsidies are available—there are concerns. Past vaccinations led to unexpectedly severe reactions, such as fever, and some individuals have experienced lasting side effects. Moreover, with the perception that COVID-19 itself has become less severe and that infections typically result in mild symptoms, the number of people expected to receive the COVID-19 vaccine in Japan in Fall/Winter 2024 may be significantly lower than anticipated.
Hybrid Immunity and Its Implications for Public Health Policy
A survey conducted using residual blood samples from blood donors to assess Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) antibody prevalence found that as of March 31, 2024, the prevalence of anti-N (nucleocapsid) antibodies, which indicates previous SARS-CoV-2 infection, was 64.5% (64.2% among males and 64.7% among females) [5]. This prevalence exceeds 80% among individuals aged 16–19 and generally decreases with age, though a majority of those aged 60–69 still possess these antibodies. Given that COVID-19 was also prevalent during the summer of 2024, the current antibody prevalence is likely even higher. Considering the anticipated recurrent waves of COVID-19 in the coming summers and winters, this prevalence is expected to approach nearly 100% over the next several years.
The combination of vaccination and natural SARS-CoV-2 infection, referred to as “hybrid immunity,” is known to elicit a particularly robust immune response, significantly increasing antibody titers [6,7,8,9,10]. To monitor IgG antibody responses to the receptor-binding domain (RBD) of the S1 subunit of the SARS-CoV-2 spike protein, we employed the Abbott Architect SARS-CoV-2 IgG II Quant chemiluminescent microparticle immunoassay (Abbott Laboratories, Chicago, IL, USA) in a limited cohort of outpatients. In cases of natural infection following vaccination (commonly termed breakthrough infection), hybrid immunity led to a notable increase in RBD antibodies [11,12,13]. During a one-year follow-up period, we observed that antibody titers remained elevated, although they gradually attenuated over time [14]. Additionally, in cases of natural infection occurring in the summer of 2023 after five vaccine doses, antibody titers rose to over 80,000 AU/mL, exceeding the assay’s measurable limit, with some individuals maintaining titers in the tens of thousands of AU/mL for over six months.
Since most individuals previously infected with COVID-19 in Japan experienced breakthrough infections after receiving two or more vaccine doses, and with more than 80% of the Japanese population having received at least two vaccine doses, it is estimated that a significant portion (likely a majority) of the population has acquired hybrid immunity and sustains high antibody titers. Consequently, the necessity of frequent additional vaccinations, as recommended in Japan through 2023, warrants further consideration.
In the United States, a comprehensive study of beneficiaries within the U.S. Military Health System was conducted to identify predictors of vaccine immunogenicity. This study demonstrated that, compared with vaccine-only or infection-only immunization, hybrid immunity was associated with sustained antibody titers six months post-infection. The researchers reported that antibody titers remained elevated for at least six months following hybrid immunization, potentially informing optimal vaccination timing strategies. Studies involving New York City residents similarly indicated that the rate of antibody titer decline over time was slower among those with hybrid immunity [16]. More recently, a study in China revealed a gradual decline in anti-SARS-CoV-2 IgG antibodies following breakthrough infections, indicating that vaccination efficacy persists for over one year [17].
Case Studies of Antibody Responses Following Vaccination and Infection
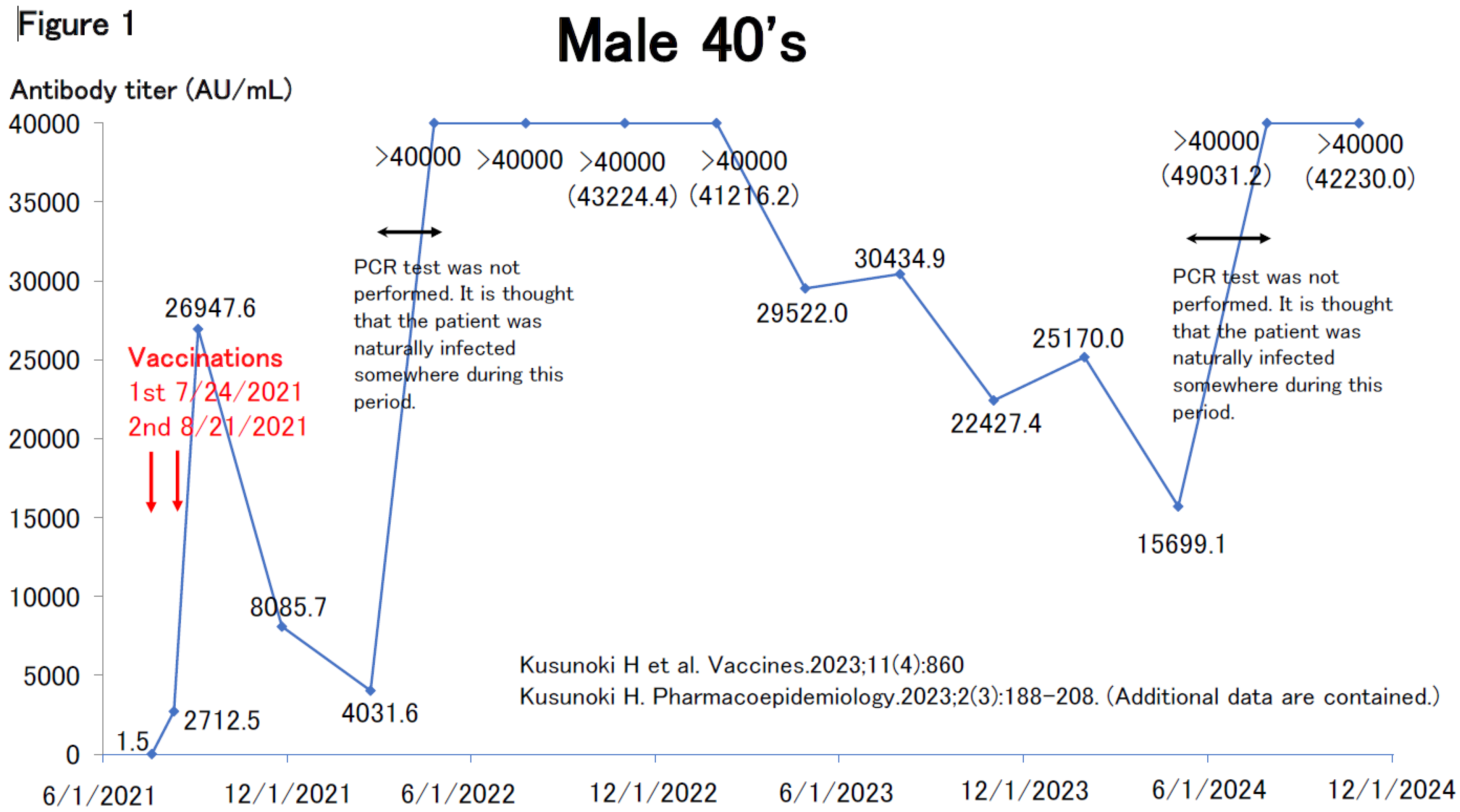
Figure 1 illustrates the antibody response of a man in his 40s. Before his initial vaccine dose in July 2021, he tested negative for antibodies and had no prior suspected COVID-19 infection. After receiving his second dose, his antibody levels surged to nearly 27,000 AU/mL but decreased to approximately 4,000 AU/mL over the following six months. In April 2022, while considering a third vaccine dose, his antibody titers unexpectedly rose above 40,000 AU/mL—well beyond measurable limits. This suggests he was likely infected with COVID-19 between February and March 2022, although no PCR test was performed, and he was not documented as a COVID-19 case [11,13]. The antibody levels gradually declined but spiked again to around 40,000 AU/mL between May and July 2024, likely due to another infection. Throughout this period, he experienced no symptoms such as fever and remained untested, indicating a probable asymptomatic infection.
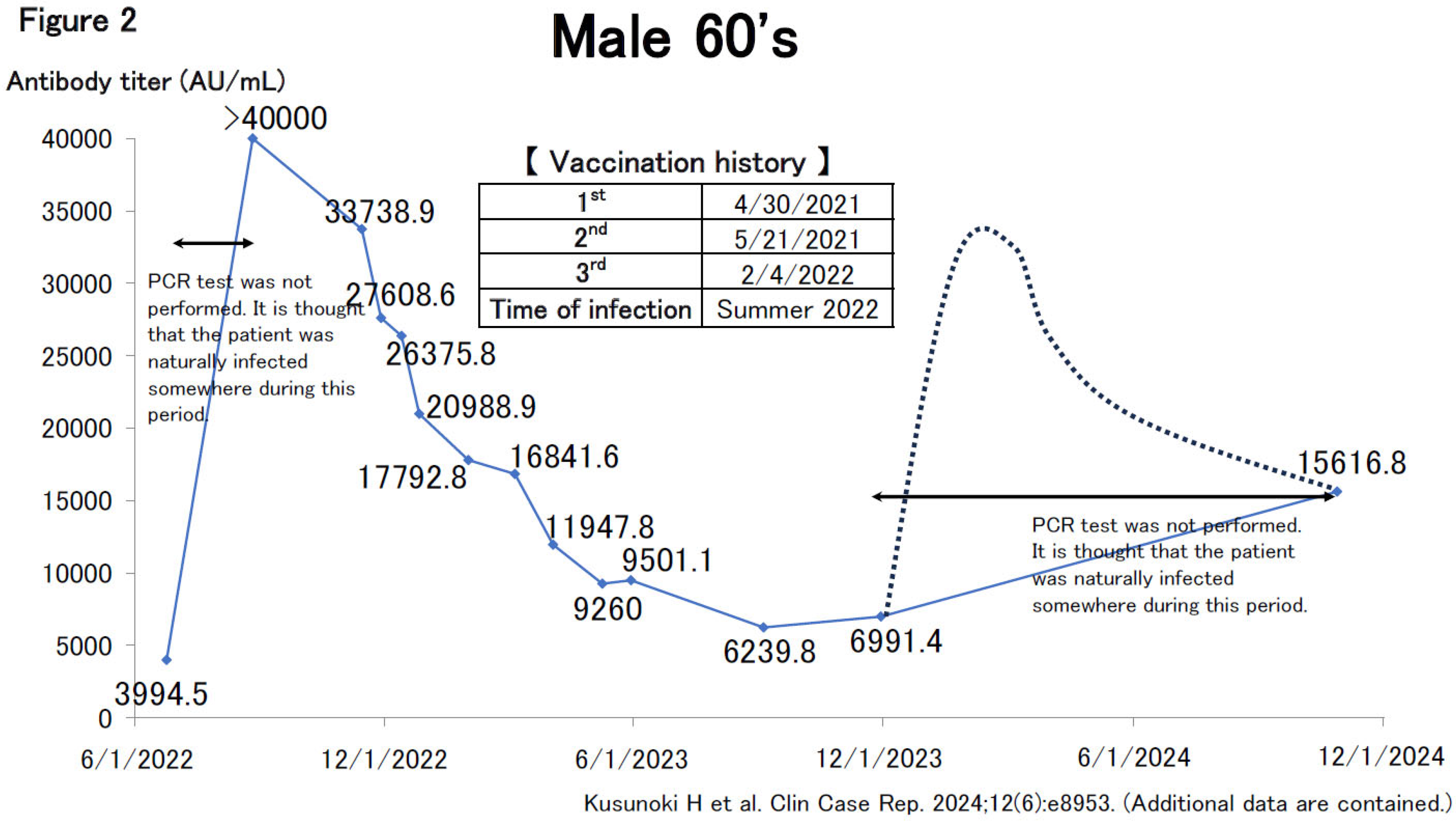
Figure 2 depicts a man in his 60s who likely contracted COVID-19 spontaneously in the summer of 2022, resulting in an antibody titer increase to >40,000 AU/mL (the upper limit of our facility’s measurements at that time). Subsequent antibody measurements revealed a non-linear decline, following an exponential decay pattern, f(x)=e-x. Although titers decreased over time, they reached a plateau, remaining within the 6,000–7,000 AU/mL range, comparable to levels observed immediately after his second or third vaccination. This level of antibody retention indicates that titers resulting from hybrid immunity remain impressively high.
In October 2024, antibody titers were reassessed for the first time in nearly a year, showing an increase to around 15,000 AU/mL, suggesting at least one natural infection during Given his history of reaching >40,000 AU/mL post-infection, it is possible that his antibody levels had initially risen significantly before stabilizing at 15,000 AU/mL, as indicated by the dotted line in Figure Cases like his, with asymptomatic or mild infections and no confirmatory tests, are likely contributing to community transmission. Due to such instances, COVID-19 transmission surges twice yearly, in summer and winter, making it virtually impossible to contain the virus’s spread during these periods [14].
Epidemiological Trends in Antibody Titers and Vaccine Efficacy
Our study, based on a small number of cases, highlights the need for a large-scale study in Japan to investigate trends in COVID-19 antibody titers over time, particularly in post-vaccination breakthrough cases, which now comprise the majority of COVID-19 infections in Japan.
An epidemiological study in Bizen City, Okayama Prefecture, conducted by Okayama University, revealed that antibody titers were sustained longer in individuals with prior SARS-CoV-2 infection compared to uninfected individuals following booster doses [18,19]. This study, which also measured antibodies against the RBD of the spike protein as we did, analyzed the relationship between antibody titer levels and infection risk. The non-linear correlation observed indicated that infection risk decreased with increasing antibody titers, although the slope of risk reduction flattened around the 10,000 AU/mL mark [20,21].
This finding is particularly significant, as epidemiological data in Japan suggest that once antibody titers surpass 10,000 AU/mL, additional vaccination has minimal benefit in further reducing infection risk. In other words, for individuals who have achieved antibody titers in the tens of thousands of AU/mL through hybrid immunity, additional vaccination may have limited value and could pose more risk than benefit when considering adverse reactions, such as fever or thrombotic risk. Given that a large portion of the Japanese population has already attained high antibody levels through hybrid immunity, a uniform recommendation for additional vaccinations is highly questionable. Going forward, vaccination timing may need to be adjusted more flexibly, considering factors such as age, underlying health conditions, antibody titer levels, and timing of prior infections.
In fact, many countries outside Japan have ceased offering additional vaccinations after For instance, the VIVALDI study, a prospective cohort study in long-term care facilities in England, showed that while successive booster doses provided short-term protection against COVID-19-related mortality, there was no added long-term benefit from fourth or fifth doses relative to the third booster dose [22]. This underscores that additional vaccinations beyond the third dose may not always be beneficial.
Analysis of Vaccine Recommendations by Japanese Medical Societies
In their Position Paper on Routine Vaccination with COVID-19 in 2024, the Japanese Society of Infectious Diseases and other academic organizations strongly recommend routine COVID-19 vaccination for older adults in the fall and winter of They reference a study claiming that the vaccine has prevented 14.4 million COVID-19-related deaths worldwide [23]. However, this study provides a one-year estimate beginning in December 2020, when mRNA vaccines were first introduced, and may not reflect current conditions. Many studies cited as evidence for the vaccine’s effectiveness tend to describe its impact from when it was initially launched. Additionally, the organizations argue that COVID-19 remains more severe and fatal than influenza, claiming that COVID-19 deaths are approximately three times those from influenza. An online article with the headline "COVID-19 deaths are about 15 times more common than flu deaths" has also fueled public perception [24].
While influenza peaks in the winter, COVID-19 circulates year-round, with notable surges in summer and winter. SARS-CoV-2 has largely replaced previous coronaviruses that caused common colds before the pandemic. With frequent SARS-CoV-2 antigen testing for common colds and fevers, many cases with typical cold symptoms are now diagnosed as COVID-Even when COVID-19 is not the primary cause of death, a positive test result may still classify the death as COVID-19-related, potentially contributing to an apparent increase in COVID-19 deaths. Therefore, it is not possible to simply compare the risks of the two.
Another cited reason for strongly recommending vaccination is the risk of post-acute sequelae (Long COVID). Among people aged 70 and older, 15.7% reported symptoms lasting over three months that disrupted daily life [25]. However, these post-COVID symptoms were self-reported, and objective measures were not used in assessments. In a cross-sectional study utilizing questionnaires and electronic health records, over half of patients reported persistent COVID-19 symptoms of various severities one year post-infection [26]. Participant enrollment for this study occurred in 2020, at an early pandemic stage when COVID-19 symptoms were likely different from those associated with the Omicron variant. The study authors also note that selection bias and recall bias could have influenced participants’ willingness to engage in the study, possibly resulting in an overestimation of Long COVID prevalence, as those experiencing prolonged symptoms were more inclined to participate. Given that 60-70% of the population has now been infected with COVID-19, it seems unlikely that the true prevalence of Long COVID is as high as some studies suggest. Thus, current estimates of Long COVID rates may be inflated.
Public Perception and Skepticism Toward COVID-19 Vaccines
The vaccine effectiveness real-time surveillance for SARS-CoV-2 (VERSUS) study, primarily conducted by Nagasaki University—recognized as a leader in infectious disease research in Japan—has sent a significantly larger number of board members to the Japanese Society of Infectious Diseases than other universities. However, there are opinions suggesting that the VERSUS study may include or exclude cases arbitrarily to suit its own purposes [27]. According to the findings, while the effectiveness of additional vaccination in preventing severe disease was significant, the effectiveness in preventing the onset of disease was not as pronounced [28,29].
If the efficacy of preventing the development of Long COVID is not substantial, even in the presence of a high incidence of Long COVID, the recommendation for additional vaccinations may be less justified in terms of their effectiveness against this condition.
Some may argue that individuals who have been infected in the past might exhibit a weak immune response to the current epidemic strain, necessitating vaccination against the latest variant. Indeed, if more than a year has passed since a person's prior infection, their protection against the current pandemic strain may be inadequate. In such cases, additional vaccination could be beneficial. However, individuals who were naturally infected in the summer of 2024 are likely to have developed sufficient immunity to the updated strain of the virus, which diminishes the significance of further vaccination for them.
Reflecting on Japan’s Response: Successes, Challenges, and Public Trust
It has been pointed out that many people in Japan believe that "COVID-19 was brought under control due to the proper advice of experts, the hard work of medical personnel, and the leadership of politicians. Above all, the citizens were very cooperative in implementing infection control measures, including masks and vaccines. The vaccine was also immensely effective, saving many lives" [30].
Considering that Japan has spent over 300 trillion yen in total on COVID-19 countermeasures, and that the Japanese population has had to bear significant economic and mental burdens due to self-restraint and other measures, leading to immense sacrifices across various areas, the author finds himself inclined to agree with this sentiment.
However, as we have mentioned, the necessity of frequent booster vaccinations is highly questionable regarding the cost-effectiveness of additional doses. It may be necessary to reconsider whether aggressive recommendations are truly appropriate, especially for young people and healthy adults. In some instances, excessive infection control measures and booster recommendations proposed by certain experts have caused confusion. The author has previously noted the widespread distrust of infectious disease specialists among the general public [14]. Negative opinions about infectious disease experts, infection control measures, and additional vaccinations tend to be particularly pronounced in online spaces such as Yahoo! Comments. While this stream of comments does not necessarily reflect the views of the public as a whole, it is true that a significant number of people are skeptical of the infection control measures and vaccines promoted by infectious disease specialists.
Conversely, while politicians often face criticism, their leadership in organizing the Tokyo Olympics without spectators, allowing individuals to decide whether to wear masks, and classifying COVID-19 as a class 5 disease—despite the reluctance of infectious disease experts—should perhaps be more highly regarded. Had they adhered strictly to the recommendations of Dr. Shigeru Omi and his colleagues, the infectious disease experts central to Japan's COVID-19 response, the economic and social disruptions would likely have been even greater. Moreover, the fact that many citizens cooperated in wearing masks and receiving vaccinations may have been due to strong social pressure and a sense of collective responsibility among their peers, rather than a high level of public awareness.
It has been noted that Japan has experienced a population decline since the COVID-19 pandemic [31], with a particular increase in excess deaths becoming a topic of discussion. Some have suggested that the COVID-19 vaccine may be associated with this increase in excess deaths [13,17,32]. In an interview in September 2024, Dr. Shigeru Omi stated, “Unfortunately, Japan does not have a system in place to obtain detailed data on vaccine-induced damage and deaths. The situation is such that we hardly know whether the cause of the deaths was the vaccine or something else, meaning we cannot draw any conclusions at this time. I believe Japan should quickly establish a monitoring system for close scrutiny” [33,34]. Dr. Omi's words and actions have been described as somewhat cowardly [35]. While establishing such a monitoring system now would be challenging due to budgetary constraints and the risk of arbitrary data manipulation, it is possible to investigate and publish data on the incidence, severity of illness, and mortality rates relative to the number of vaccine doses administered, even through retrospective studies. This should be pursued as soon as possible.
Employees of vaccine manufacturing companies actively publish studies to emphasize the efficacy and safety of vaccines while advocating for higher vaccination rates. In Japan, a study conducted by Pfizer employees estimated COVID-19-related symptoms, hospitalizations, deaths, as well as both vaccine- and non-vaccine-related medical costs and productivity losses at vaccination rates of 50%, 90%, and 10%. The study found that, even with increased vaccine-related costs, overall medical expenses and productivity losses exceeded those costs. It concluded that non-vaccine-related medical costs and productivity losses could be significantly reduced, thereby lowering overall costs and underscoring the importance of maintaining high vaccination coverage among elderly and at-risk populations [37]. However, further validation of these estimates is essential, as results may vary considerably depending on the assumptions and premises of the models employed.
Additionally, a review article by a Moderna employee in the U.S. highlighted the low rate of additional COVID-19 vaccinations in the U.S. and recommended that all individuals aged 6 months and older receive further vaccinations. The article emphasized the importance of integrating vaccination into routine medical care and establishing consistent vaccination guidelines from healthcare providers to encourage COVID-19 vaccination [37]. The reasons cited for the low uptake of additional vaccinations include, primarily, a lack of long-term safety data and efficacy information, a decreased sense of urgency for COVID-19 vaccination compared to the pandemic's early stages, and insufficient communication about the need for additional doses and updates to vaccination schedules from healthcare providers and the general public. However, there is minimal discussion on the lack of scientific evidence supporting the necessity and frequency of additional vaccinations.
Fundamentally, since vaccine manufacturers have direct economic interests in increasing vaccination rates, the fairness and objectivity of studies published by their employees are questionable, and some may argue that these studies are disingenuous in terms of conflict of interest.
The Role of Replicon Vaccines: New Developments and Controversies
The COVID-19 vaccination for 2024 commenced in October, with significant attention focused on a replicon-type (self-amplifying) mRNA vaccine developed by Arcturus Therapeutics in the United States and Meiji Seika Pharma in Japan. This replicon vaccine has been shown to induce higher neutralizing antibody titers than conventional mRNA vaccines [38] and offers the advantage of a longer duration of neutralizing antibodies [39,40].
However, widespread skepticism emerged, particularly among those already doubtful of existing COVID-19 vaccines, regarding why this vaccine was approved solely in Japan while not receiving approval in the U.S. or Vietnam, where clinical trials were conducted. Additionally, Meiji Seika Pharma employees published a book revealing the inner workings of the pharmaceutical company [41]. The theory that recipients of the replicon vaccine could shed the virus and infect others gained traction, leading to frequent bans on replicon vaccine recipients from entering doctors' offices, beauty salons, and other venues. Meiji Seika Pharma is currently preparing to sue a member of the Diet who has repeatedly made negative remarks about the replicon vaccine, accusing him of “inciting public anxiety by misrepresenting facts and raising issues not grounded in scientific knowledge” [42].
Disseminating unsubstantiated information in an emotional and sensational manner is undeniably problematic. Nevertheless, it is understandable that many individuals express concerns about the replicon vaccine, given that it represents a novel vaccine type not yet approved in other countries. Additionally, negative opinions from critics of the replicon vaccine have emerged in various online articles [43].
Regarding “unnecessarily inflaming public fears,” it is worth noting that the words and actions of infectious disease experts in the early stages of the pandemic contributed to public anxiety. A prominent infectious disease expert's announcement in 2020 that over 420,000 people could die without intervention unnecessarily heightened public anxiety. Since the results of such large-scale estimates are sensitive to even slight changes in assumptions, a thorough verification of these assumptions and reassessment based on multiple scenarios should have been conducted, with findings made accessible to the general public. Furthermore, questioning the credibility and realistic applicability of such figures is reasonable, as they may be perceived as disconnected from the experiences of the general public and clinicians. Experts also estimated that without the introduction of the new COVID-19 vaccine, the number of cases and deaths would have been 13.5 times and 36.4 times higher, respectively, than those reported from February to November 2021 [44]. This data also seems far removed from the perceptions of many citizens and clinicians, and some presentations have raised questions about the validity of these findings [45,46,47].
Similar episodes have occurred elsewhere. Nobel Prize laureate Dr. Shinya Yamanaka noted not only the efforts of Japanese health authorities and the public's self-restraint in reducing outings, as well as decreased close contact through practices like handshaking and kissing compared to Western cultures, but also pointed to public health programs such as childhood BCG vaccinations against tuberculosis. He suggested the possibility that Japanese people might possess genetic resistance to SARS-CoV-2 or have already acquired such resistance through infections with similar viruses. Collectively, these factors were referred to as “Factor X,” sparking considerable controversy [48]. Some specialists have argued that the idea of Japanese resistance to COVID-19 is merely an illusion [49] and that Factor X does not exist [50,51].
Concerns may have arisen regarding the risk that “Factor X” could provide the public with a false sense of security, leading to neglect of other essential infection prevention measures. These specialists may have asserted that “Factor X” was an illusion, lacking scientific basis and evidence. However, stating that “Factor X” is an illusion might have left the public with the impression that “biological differences” attributed to “Factor X” are impossible, which may reflect a lack of prudence on the part of scientists regarding unnecessary public anxiety.
Despite aggressive recommendations from academic societies and vaccine manufacturers for vaccination, demand for the COVID-19 vaccine is expected to decline in Fall/Winter Many individuals, including the elderly, are likely to refrain from receiving the COVID-19 vaccine, partly due to reductions in public subsidies for the vaccine and the proliferation of various negative perceptions. With a large supply of vaccine already available (over 30 million doses), significant surplus will likely need to be disposed of. Furthermore, it is unlikely that individuals who have already declined vaccination will reconsider their decision in the future, even beyond Fall/Winter Although this situation poses challenges for vaccine manufacturers, who have made substantial capital investments anticipating high demand for COVID-19 vaccines, it would be prudent to order a realistic number of vaccines post-2025 based on the projected vaccination population for 2024.
Opinions on COVID-19 vaccines and infection control measures are sharply divided between proponents and opponents, often resulting in irreconcilable arguments. This dichotomy frequently leads to sterile disputes that emphasize differences rather than deepen the discussion. While both sides may deny each other's claims, it is essential to respect the coexistence of differing opinions and promote an approach that values individual choices in policy decisions. Both sides present reasonable arguments, but there are also emotional, aggressive, and excessive aspects, as well as points that raise doubts. In discussions surrounding the COVID-19 vaccine, even mild criticism of the vaccine tends to label individuals as “anti-vaccine” or conspiracy theorists, while information that is slightly negative about the vaccine is often dismissed as misinformation.
Concluding Thoughts on COVID-19 Vaccination Policies and Future Directions
The author believes that the COVID-19 vaccine represents an excellent technological advancement, as significant increases in antibody titers can be achieved with the first two doses, particularly when combined with spontaneous infection. In healthy individuals, the risk of severe illness is minimal, and the author does not wholly dismiss the efficacy of the COVID-19 vaccine. It is acknowledged that there was a positive impact during the initial vaccination period in 2021, and in some cases, the benefits of additional vaccinations may still outweigh the risks.
Furthermore, the author respects the autonomy of patients and healthcare providers who choose to receive additional vaccinations and does not advocate against their decision. This choice reflects a form of personal freedom that should be honored. However, it is essential that those who opt for additional vaccinations do not criticize or pressure individuals who are hesitant or unwilling to receive them. As for-profit entities, vaccine manufacturers have the right to promote their products actively.
Nonetheless, it has been a painful experience for the author to be labeled "anti-vaccine" by those around them, including family members, merely for questioning the need for additional vaccinations. In Japanese culture, there is a tendency to act based on societal expectations and peer pressure rather than on rational judgment. Moving forward, it is crucial to develop policies that respect individual values and choices regarding vaccination.
Conclusions
The COVID-19 pandemic has profoundly impacted Japan’s healthcare system, societal norms, and public policy. With the development of hybrid immunity across a significant portion of the population, there is a compelling need to re-evaluate the blanket approach to booster vaccinations. Evidence from both domestic and international studies suggests that hybrid immunity confers strong and lasting protection, potentially reducing the necessity for frequent additional vaccinations. Given this, vaccination strategies should be adapted to consider individual immune status, including antibody levels and infection history, to promote a more targeted and cost-effective approach.
Public skepticism toward continued vaccination highlights a broader need for transparent communication from healthcare authorities. Vaccine manufacturers and policymakers must recognize the importance of public trust and address concerns around vaccine safety, cost, and effectiveness. Furthermore, Japan’s experience underscores the importance of balancing expert guidance with flexibility in public health policy to foster resilience against future health crises.
In moving forward, a policy framework that respects individual choices and is informed by ongoing scientific data will be crucial. By embracing a nuanced approach that considers the diverse immunity profiles of the population, Japan can optimize its COVID-19 strategy, ensuring that public health measures are both scientifically grounded and publicly supported.
References
- https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/vaccine_00184.
- https://www.kansensho.or.jp/uploads/files/news/gakkai/gakkai_covid19_241031.
- https://www.jpeds.or.jp/uploads/files/20241028_2024-2025_corona.
- https://www.pmda.go.jp/int-activities/int-harmony/icmra/0029.
- https://www.mhlw.go.jp/content/001251912.
- https://www.science.org/doi/10.1126/science. 2258.
- Shrestha NK, Burke PC, Nowacki AS, et al. Necessity of Coronavirus Disease 2019 (COVID-19) Vaccination in Persons Who Have Already Had COVID-Clin Infect Dis. 2022 Aug 24;75(1):e662-e671. [CrossRef]
- Desmecht S, Tashkeev A, El Moussaoui M, et al. Kinetics and Persistence of the Cellular and Humoral Immune Responses to BNT162b2 mRNA Vaccine in SARS-CoV-2-Naive and -Experienced Subjects: Impact of Booster Dose and Breakthrough Infections. Front Immunol. 2022 ;13:863554. 31 May. [CrossRef]
- Sarrigeorgiou I, Moschandreou D, Dimitriadis A, et al. Labropoulou S, Escriou N, Pouliakis A, Giannopoulou G, Gaitanarou E, Lazaridis K, Mentis A, Mamalaki A, Grouzi E, Lymberi P. Combined monitoring of IgG and IgA anti-Spike and anti-Receptor binding domain long term responses following BNT162b2 mRNA vaccination in Greek healthcare workers. PLoS One. 2022 Nov 21;17(11):e0277827. eCollection 2022. [CrossRef]
- Walls AC, Sprouse KR, Bowen JE, et al. SARS-CoV-2 breakthrough infections elicit potent, broad, and durable neutralizing antibody responses. Cell. 2022 Mar 3;185(5):872-880.e3. [CrossRef]
- Kusunoki H, Ohkusa M, Iida R, et al. Longitudinal Changes in IgG-Type SARS-CoV-2 Antibody Titers after COVID-19 Vaccination and a Prominent Increase in Antibody Titers When Infected after Vaccination.Vaccines (Basel). 2023 Apr 17;11(4):860. [CrossRef]
- Kusunoki H, Ekawa K, Ekawa M, et al. Trends in Antibody Titers after SARS-CoV-2 Vaccination-Insights from Self-Paid Tests at a General Internal Medicine Clinic. Medicines (Basel). 2023 Apr 20;10(4):27. [CrossRef]
- Kusunoki, H. COVID-19 and the COVID-19 vaccine in Japan—a review from a general physician's perspective. Pharmacoepidemiology. 2023;2(3):188-208. [CrossRef]
- Kusunoki H, Ohkusa M, Iida R, et al. Increase in antibody titer and change over time associated with severe acute respiratory syndrome coronavirus 2 infection after mRNA vaccination: Consideration of the significance of additional vaccination. Clin Case Rep. 2024 ;12(6):e8953. 27 May. [CrossRef]
- Epsi NJ, Richard SA, Lindholm DA, et al. Understanding “hybrid immunity”: comparison and predictors of humoral immune responses to severe acute respiratory syndrome coronavirus 2 infection (SARS-CoV-2) and coronavirus disease 2019 (COVID-19) vaccines. Clin Infect Dis. 2023;76(3):e439-e449.
- Srivastava K, Carreño JM, Gleason C, et al. SARS-CoV-2-infection- and vaccine-induced antibody responses are long lasting with an initial waning phase followed by a stabilization phase.Immunity. 2024 Mar 12;57(3):587-599.e4. [CrossRef]
- Yan X, Zhao X, Du Y, et al. Dynamics of anti-SARS-CoV-2 IgG antibody responses following breakthrough infection and the predicted protective efficacy: a longitudinal community-based population study in China. Int J Infect Dis. 2024;30:107075. [CrossRef]
- Matsumoto N, Sasaki A, Kadowaki T,et al. Longitudinal antibody dynamics after COVID-19 vaccine boosters based on prior infection status and booster doses. Sci Rep. 2024 Feb 25;14(1):4564. [CrossRef]
- Matsumoto N, Sasaki A, Kadowaki T,et al. Kinetics of SARS-CoV-2 antibody titers after booster vaccinations during an Omicron surge in Japan. Vaccine. 2024 Aug 30;42(21):126156. [CrossRef]
- Sasaki A, Kadowaki T, Matsumoto N,et al. Antibody levels and the risk of SARS-CoV-2 infection during the Omicron surge. GHM Open. 2024; 4(1):52-53.
- Kadowaki T, Sasaki A, Matsumoto N,et al.Antibody Titers and the Risk of Infection During the SARS-CoV-2 Omicron Phase in Bizen City, Japan. J Infect Dis. 2024 Sep 23;230(3):662-669. [CrossRef]
- Stirrup O, Shrotri M, Adams NL,et al. Effectiveness of successive booster vaccine doses against SARS-CoV-2 related mortality in residents of long-term care facilities in the VIVALDI study. Age Ageing. 2023 Aug 1;52(8):afad141. [CrossRef]
- Watson OJ, Barnsley G, Toor J,et al. Global impact of the first year of COVID-19 vaccination: a mathematical modelling study. Lancet Infect Dis. 2022 Sep;22(9):1293-1302. [CrossRef]
- https://www.tokyo-np.co. 3623.
- Sugiyama A, Takafuta T, Sato T,et al. Natural course of post-COVID symptoms in adults and children. Sci Rep. 2024 Feb 16;14(1):3884. [CrossRef]
- Imoto W, Yamada K, Kawai R,et al. A cross-sectional, multicenter survey of the prevalence and risk factors for Long COVID. Sci Rep. 2022 Dec 27;12(1):22413. [CrossRef]
- https://www.youtube.com/watch?
- https://www.tm.nagasaki-u.ac.jp/versus/results/20240524.
- Maeda H, Saito N, Igarashi A,et al. Effectiveness of primary series, first, and second booster vaccination of monovalent mRNA COVID-19 vaccines against symptomatic SARS-CoV-2 infections and severe diseases during the SARS-CoV-2 omicron BA.5 epidemic in Japan: vaccine effectiveness real-time surveillance for SARS-CoV-2 (VERSUS). Expert Rev Vaccines. 2024 Jan-Dec;23(1):213-225. [CrossRef]
- https://wowma. 7120.
- Kaneda Y, Yamashita E, Kaneda U,et al. Japan's Demographic Dilemma: Navigating the Postpandemic Population Decline.JMA J. 2024 Jul 16;7(3):403-405. [CrossRef]
- Saiag E,Gamzu R,Padova H,et al.Antibody Response After a Fifth Dose (Third Booster) of BNT162b2 mRNA COVID-19 Vaccine in Healthcare Workers. J.Clin.Med. 2024. [CrossRef]
- https://news.yahoo.co.jp/articles/c6a3e1d3112ed3695c9e87127e81085e0207306d?
- https://video.yahoo.co. 4041.
- https://x. 1849.
- Nagano M, Tanabe K, Kamei K,et al. Public Health and Economic Impact of Periodic COVID-19 Vaccination with BNT162b2 for Old Adults and High-Risk Patients in an Illustrative Prefecture of Japan: A Budget Impact Analysis. Infect Dis Ther. 2024 Oct;13(10):2155-2177. [CrossRef]
- Mansi JA, Hensler HR, Dawson R,et al. Navigating the Evolving Landscape of COVID-19: Strategies to Increase Vaccine Confidence and Improve Vaccination Rates in the United States. Vaccines (Basel). 2024 Sep 19;12(9):1072. [CrossRef]
- Hồ NT, Hughes SG, Ta VT,et al. Safety, immunogenicity and efficacy of the self-amplifying mRNA ARCT-154 COVID-19 vaccine: pooled phase 1, 2, 3a and 3b randomized, controlled trials. Nat Commun. 2024 ;15(1):4081. 14 May. [CrossRef]
- Oda Y, Kumagai Y, Kanai M,et al. Persistence of immune responses of a self-amplifying RNA COVID-19 vaccine (ARCT-154) versus BNT162bLancet Infect Dis. 2024 Apr;24(4):341-343. [CrossRef]
- Oda Y, Kumagai Y, Kanai M, et al. 12-month persistence of immune responses to self-amplifying mRNA COVID-19 vaccines: ARCT-154 versus BNT162b2 vaccine. Lancet Infect Dis. 2024 Oct 7:S1473-3099(24)00615-7. [CrossRef]
- https://hojosha.co. 1052.
- https ://www.meiji-seika-pharma.co.jp/pdf/notice/notice_01.
- https://news.yahoo.co. 5151.
- Kayano T, Ko Y, Otani K, et al. Evaluating the COVID-19 vaccination program in Japan, 2021 using the counterfactual reproduction number. Sci Rep. 2023 Oct 18;13(1):17762. [CrossRef]
- Kakeya H, Itoh M, Kamijima Y, et al. Unreliability in simulations of COVID-19 cases and deaths based on transmission models. medRxiv. 2024. [CrossRef]
- https://www.youtube.com/watch? 3111.
- https://www.youtube.com/watch?
- https://asia.nikkei.
- Weekly Bunshun; Shūkan Bunshun: Tokyo, Japan, 2020; Aug. 13 issue; pp. 148–153. https://cir.nii.ac. 1523.
- https://www.jmedj.co.jp/journal/paper/detail.php? 1537.
- https://bunshun. 4215.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).