Submitted:
11 September 2024
Posted:
12 September 2024
You are already at the latest version
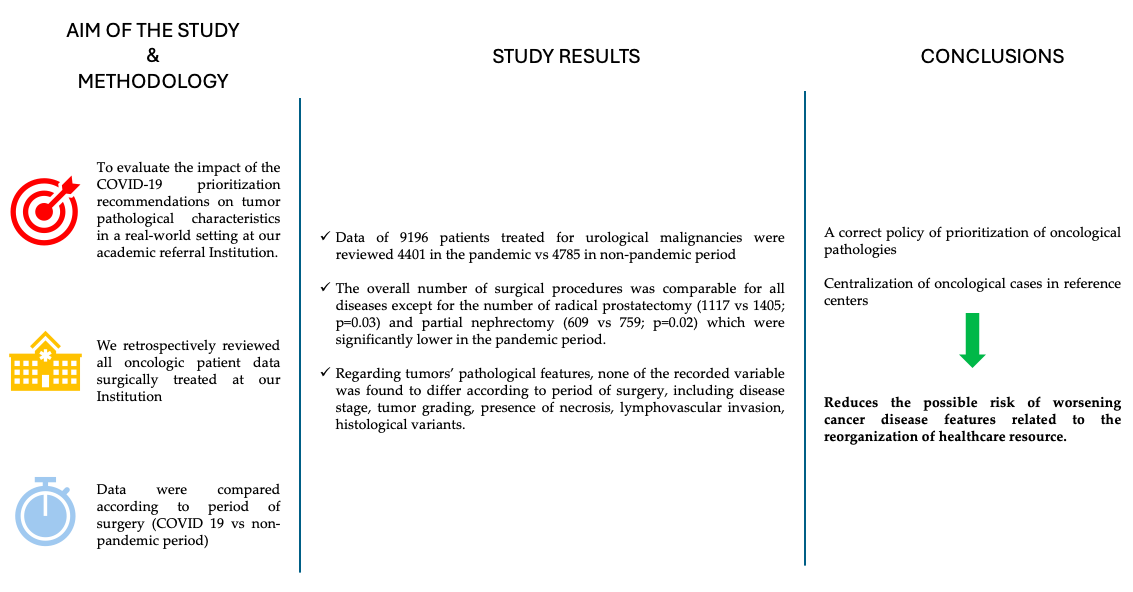
Abstract
Keywords:
1. Introduction
2. Materials and Methods
2.1. Patient Data and Data Collection
2.2. Statistical Analysis
3. Results
| Pandemic period (2020 – 2021) n = 4401 |
Non Pandemic period (2022 – 2023) n = 4785 |
p-value | |||
| 1117 | 1405 | 0.03 | |||
| PROSTATECTOMY (n = 2522) |
Age, median (IQR); years | 66 (60 - 71) | 68 (60 - 71) | 0.11 | |
| ASA score, median (IQR) | 2 (2 - 2) | 2 (2 - 3) | 0.06 | ||
| CCI score, median (IQR) | 3 (3 - 4) | 3 (3 - 4) | 0.09 | ||
| PSA serum level, median (IQR); ng/mL | 10 (6 - 14) | 7 (5 - 13) | 0.02 | ||
| 1861 | 1890 | 0.21 | |||
| TURBT (n = 3751) |
Gender, n. (%) | Male | 1144 (61.5) | 1192 (63.1) | 0.21 |
| Female | 717 (38.5) | 698 (36.9) | |||
| Age, median (IQR); years | 71 (64 – 78) | 70 (65 -77) | 0.28 | ||
| ASA score, median (IQR) | 2 (2 - 3) | 2 (2 - 3) | 0.11 | ||
| CCI score, median (IQR) | 4 (3 - 4) | 4 (3 - 4) | 0.24 | ||
| 252 | 246 | 0.18 | |||
| CISTECTOMY (n = 508) |
Gender, n. (%) | Male | 173 (68.7) | 163 (66.4) | 0.33 |
| Female | 79 (31.3) | 83 (33.6) | |||
| Age, median (IQR); years | 73 (66 – 78) | 74 (66 – 78) | 0.18 | ||
| ASA score, median (IQR) | 2 (2 - 3) | 2 (2 - 3) | 0.11 | ||
| CCI score, median (IQR) | 4 (3 - 4) | 4 (3 - 4) | 0.24 | ||
| 170 | 185 | 0.34 | |||
| NEPHROURETERECTOMY (n = 355) |
Gender, n. (%) | Male | 121 (71.4) | 127 (68.8) | 0.57 |
| Female | 49 (28.6) | 58 (31.2) | |||
| Age, median (IQR); years | 70 (62 – 70) | 70 (60 – 68) | 0.43 | ||
| ASA score, median (IQR) | 2 (2 - 3) | 2 (2 - 3) | 0.48 | ||
| CCI score, median (IQR) | 2 (2 - 3) | 2 (2 - 3) | 0.33 | ||
| Hydronephrosis, n. % | 89 (52.5) | 93 (50.1) | 0.17 | ||
| 190 | 201 | 0.24 | |||
| RADICAL NEPHRECTOMY (n = 391) |
Gender, n. (%) | Male | 113 (59.5) | 116 (58.0) | 0.33 |
| Female | 77 (40.5) | 85 (42.0) | |||
| Age, median (IQR); years | 60 (52 - 68) | 61 (52 - 68) | 0.41 | ||
| ASA score, median (IQR) | 2 (2 - 3) | 2 (2 - 3) | 0.38 | ||
| CCI score, median (IQR) | 3 (3 - 4) | 3 (3 - 4) | 0.22 | ||
| Symtomps, n. (%) | 44 (23.2) | 38 (19.1) | 0.07 | ||
| 609 | 759 | 0.02 | |||
| PARTIAL NEPHRECTOMY (n = 1468) |
Gender, n. (%) | Male | 352 (57.7) | 447 (59.0) | 0.51 |
| Female | 257 (42.3) | 312 (41.0) | |||
| Age, median (IQR); years | 61 (50 – 67) | 63 (52 – 68) | 0.24 | ||
| ASA score, median (IQR) | 2 (2 – 2) | 2 (2 – 2) | 0.31 | ||
| CCI score, median (IQR) | 2 (2 - 3) | 2 (2 - 3) | 0.32 | ||
| PADUA score, median (IQR) | 8 (7 – 9) | 8 (7 – 9) | 0.29 | ||
| 86 | 89 | 0.33 | |||
| ORCHIECTOMY (n = 175) |
Age, median (IQR); years | 34 (25 - 42) | 36 (26 - 44) | 0.41 | |
| ASA score, median (IQR) | 1 (1 – 1) | 1 (1 – 1) | 0.28 | ||
| CCI score, median (IQR) | 0 (0 – 0) | 0 (0 – 0) | 0.24 | ||
| Tumor diameter, median (IQR); mm | 2.1 (0.8 – 2.8) | 1.9 (0.6 – 2.8) | 0.33 | ||
| 16 | 10 | 0.28 | |||
| PENECTOMY (n = 26) |
Age, median (IQR); years | 75 (72 – 78) | 76 (68 – 77) | 0.18 | |
| ASA score, median (IQR) | 3 (2 – 3) | 3 (2 – 3) | 0.22 | ||
| CCI score, median (IQR) | 4 (3 - 4) | 4 (3 - 4) | 0.28 | ||
| Pandemic period (2020 – 2021) n = 4401 |
Non Pandemic period (2022 – 2023) n = 4785 |
p-value | ||||
| 1117 | 1405 | 0.03 | ||||
| PROSTATECTOMY (n = 2522) |
pT stage, n. (%) | pT2 | 424 (37.9) | 542 (38.5) | 0.18 | |
| pT3a | 511 (45.7) | 602 (43.0) | ||||
| pT3b | 177 (16.0) | 254 (18.0) | ||||
| pT4 | 5 (0.4) | 7 (0.5) | ||||
| pN+, n. (%) | 159 (14.2) | 210 (14.9) | 0.24 | |||
| ISUP grade, median (IQR) | 3 (2 – 4) | 3 (2 – 4) | 0.33 | |||
| 1861 | 1890 | 0.21 | ||||
| TURBT (n = 3751) |
pT stage, n. (%) | pTis | 53 (2.8) | 58 (3.1) | 0.14 | |
| pTa | 786 (42.2) | 776 (41.1) | ||||
| pT1 | 893 (47.9) | 871 (46.0) | ||||
| pT2 | 129 (7.1) | 185 (9.8) | ||||
| Tumor Grade, n. (%) | Low | 998 (53.6) | 1022 (54.0) | 0.38 | ||
| High | 863 (46,4) | 868 (46.0) | ||||
| Concomitant CIS, n. (%) | 241 (12.9) | 205 (10.8) | 0.29 | |||
| 252 | 246 | 0.18 | ||||
| CISTECTOMY (n = 508) |
pT stage, n. (%) | pT2 | 105 (41.6) | 111 (45.1) | 0.41 | |
| pT3a | 95 (37.6) | 89 (36.1) | ||||
| pT3b | 45 (18.1) | 37 (15.2) | ||||
| pT4 | 7 (2.7) | 9 (3.6) | ||||
| pN+, n. (%) | 41 (16.2) | 38 (15.4) | 0.38 | |||
| Histology variant, n. (%) | 32 (12.6) | 32 (13.0) | 0.28 | |||
| 170 | 185 | 0.34 | ||||
| NEPHROURETERECTOMY (n = 355) |
pT stage, n. (%) | pT1 | 43 (25.2) | 39 (21.0) | 0.17 | |
| pT2 | 96 (56.4) | 109 (58.9) | ||||
| pT3 | 29 (17.0) | 33 (18.0) | ||||
| pT4 | 2 (1.4) | 4 (2.1) | ||||
| pN+, n. (%) | 25 (14.7) | 31 (16.7) | 0.24 | |||
| Lymphovascular invasion, n. (%) | 53 (25.2) | 46 (24.8) | 0.28 | |||
| Histology variant, n. (%) | 19 (11.1) | 17 (9.1) | 0.45 | |||
| 190 | 201 | 0.24 | ||||
| RADICAL NEPHRECTOMY (n = 391) |
pT stage, n. (%) | pT1b | 24 (12.6) | 27 (13.4) | 0.19 | |
| pT2 | 69 (36.3) | 70 (34.8) | ||||
| pT3a | 81 (42.6) | 89 (44.2) | ||||
| pT3b/c | 10 (5.2) | 13 (6.4) | ||||
| pT4 | 6 (3.3) | 2 (1.2) | ||||
| pN+, n. (%) | 40 (21.0) | 38 (18.9) | 0.31 | |||
| Nuclear grade, median (IQR) | 3 (3 – 4) | 3 (3 – 4) | ||||
| Necrosis, n. (%) | 64 (33.6) | 72 (35.8) | 0.22 | |||
| 609 | 759 | 0.02 | ||||
| PARTIAL NEPHRECTOMY (n = 1468) |
pT stage, n. (%) | pT1a | 339 (55.6) | 401 (52.8) | 0.44 | |
| pT1b | 158 (25.9) | 221 (29.1) | ||||
| pT2 | 28 (4.5) | 36 (4.8) | ||||
| pT3a | 84 (14.0) | 101 (13.3) | ||||
| Nuclear grade, median (IQR) | 2 (1 – 3) | 2 (1 – 3) | 0.19 | |||
| Necrosis, n. (%) | 93 (13.1) | 101 (13.3) | 0.56 | |||
| 86 | 89 | 0.33 | ||||
| ORCHIECTOMY (n = 175) |
Disease Stage, n. (%) | Ia | 19 (22.0) | 17 (19.1) | 0.26 | |
| Ib | 18 (22.1) | 22 (24.7) | ||||
| Is | 20 (23.2) | 15 (16.8) | ||||
| II | 21 (23.4) | 26 (29.3) | ||||
| III | 8 (9.3) | 9 (10.1) | ||||
| Lymphovascular invasion, n. (%) | 15 (17.4) | 17 (19.1) | 0.19 | |||
| Non-seminomatous germ cell tumours, n. (%) | 39 (45.3) | 38 (42.6) | 0.22 | |||
| 16 | 10 | 0.28 | ||||
| PENECTOMY (n = 26) |
Disease Stage, n. (%) | I | 4 (25.0) | 3 (30.0) | 0.37 | |
| IIa | 5 (31.2) | 4 (40.0) | ||||
| IIb | 3 (18.7) | 2 (20.0) | ||||
| IIIa | 3 (18.7) | 1 (10.0) | ||||
| IIIb | 1 (6.4) | 0 (0.0) | ||||
| IV | 0 | 0 (0.0) | ||||
| Histopathological Grading, median, (IQR) | 2 (1 - 3) | 2 (1 – 3) | 0.22 | |||
4. Discussion
5. Conclusion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Campi R, Tellini R, Grosso AA, Amparore D, Mari A, Viola L, et al. Deferring Elective Urologic Surgery During the COVID-19 Pandemic: The Patients’ Perspective. Urology. 2021 Jan;147:21-26. [CrossRef]
- Amparore D, Campi R, Checcucci E, Piana A, Sica M, Grosso AA, et al. Patients’ perspective on the use of telemedicine for outpatient urological visits: Learning from the COVID-19 outbreak. Actas Urol Esp (Engl Ed). 2020 Nov;44(9):637-638. English, Spanish. [CrossRef]
- Naspro R, Da Pozzo LF. Urology in the time of corona. Nat Rev Urol. 2020 May;17(5):251-253. [CrossRef]
- Amparore D, Campi R, Checcucci E, Sessa F, Pecoraro A, Minervini A, et al. Forecasting the Future of Urology Practice: A Comprehensive Review of the Recommendations by International and European Associations on Priority Procedures During the COVID-19 Pandemic. Eur Urol Focus. 2020 Sep 15;6(5):1032-1048. [CrossRef]
- Stensland KD, Morgan TM, Moinzadeh A, Lee CT, Briganti A, Catto JWF, et al. Considerations in the Triage of Urologic Surgeries During the COVID-19 Pandemic. Eur Urol. 2020 Jun;77(6):663-666. [CrossRef]
- Ribal MJ, Cornford P, Briganti A, Knoll T, Gravas S, Babjuk M, et al. EAU Section Offices and the EAU Guidelines Panels. European Association of Urology Guidelines Office Rapid Reaction Group: An Organisation-wide Collaborative Effort to Adapt the European Association of Urology Guidelines Recommendations to the Coronavirus Disease 2019 Era. Eur Urol. 2020 Jul;78(1):21-28. doi: 10.1016/j.eururo.2020.04.056 Quan H, Li B, Couris CM, Fushimi K, Graham P, Hider P, et al. Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am J Epidemiol. 2011 Mar 15;173(6):676-82. [CrossRef]
- Knuf KM, Maani CV, Cummings AK. Clinical agreement in the American Society of Anesthesiologists physical status classification. Perioper Med (Lond). 2018 Jun 19;7:14. [CrossRef]
- Quan H, Li B, Couris CM, Fushimi K, Graham P, Hider P, et al. Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am J Epidemiol. 2011 Mar 15;173(6):676-82. [CrossRef]
- Amin MB, Greene FL, Edge SB, Compton CC, Gershenwald JE, Brookland RK, et al. The Eighth Edition AJCC Cancer Staging Manual: Continuing to build a bridge from a population-based to a more “personalized” approach to cancer staging. CA Cancer J Clin. 2017 Mar;67(2):93-99. [CrossRef]
- Epstein JI, Egevad L, Amin MB, Delahunt B, Srigley JR, Humphrey PA; Grading Committee. The 2014 International Society of Urological Pathology (ISUP) Consensus Conference on Gleason Grading of Prostatic Carcinoma: Definition of Grading Patterns and Proposal for a New Grading System. Am J Surg Pathol. 2016 Feb;40(2):244-52. [CrossRef]
- WHO Classification of Tumours Editorial Board. WHO Classification of Tumours. Urinary and male genital tumours. International Agency for Research on Cancer 5th Edn.; Vol 8. 2022. https://publications.iarc.fr/610.
- Moch H, Cubilla AL, Humphrey PA, Reuter VE, Ulbright TM. The 2016 WHO Classification of Tumours of the Urinary System and Male Genital Organs-Part A: Renal, Penile, and Testicular Tumours. Eur Urol. 2016 Jul;70(1):93-105. [CrossRef]
- Rutter MD, Brookes M, Lee TJ, Rogers P, Sharp LJG. Impact of the COVID-19 pandemic on UK endoscopic activity and cancer detection: a National Endoscopy Database Analysis. Gut . 2021;70(3):537–543 .
- Jacob L, Loosen SH, Kalder M, Luedde T, Roderburg C, Kostev KJC. Impact of the COVID-19 pandemic on cancer diagnoses in general and specialized practices in Germany. Cancers . 2021;13(3):408.
- Wang J, Vahid S, Eberg M, Milroy S, Milkovich J, Wright FC, et al. Clearing the surgical backlog caused by COVID-19 in Ontario: a time series modelling study. CMAJ. 2020 Nov 2;192(44):E1347-E1356.
- Uimonen M, Kuitunen I, Paloneva J, Launonen AP, Ponkilainen V, Mattila VM. The impact of the COVID-19 pandemic on waiting times for elective surgery patients: A multicenter study. PLoS One. 2021 Jul 6;16(7):e0253875.
- Oderda M, Soria F, Rosi F, Calleris G, Mazzoli S, Giordano A, et al. COVID-19 pandemic impact on uro-oncological disease outcomes at an Italian tertiary referral center. World J Urol. 2022 Jan;40(1):263-269.
- Tachibana I, Ferguson EL, Mahenthiran A, Natarajan JP, Masterson TA, Bahler CD, et al. Delaying Cancer Cases in Urology during COVID-19: Review of the Literature. J Urol. 2020 Nov;204(5):926-933.
- Chan VW, Tan WS, Asif A, Ng A, Gbolahan O, Dinneen E, et al. Effects of Delayed Radical Prostatectomy and Active Surveillance on Localised Prostate Cancer-A Systematic Review and Meta-Analysis. Cancers (Basel). 2021 Jun 30;13(13):3274.
- Campi R, Amparore D, Capitanio U, Checcucci E, Salonia A, Fiori C, et al. Assessing the Burden of Nondeferrable Major Uro-oncologic Surgery to Guide Prioritisation Strategies During the COVID-19 Pandemic: Insights from Three Italian High-volume Referral Centres. Eur Urol. 2020 Jul;78(1):11-15.
- Campi R, Tellini R, Grosso AA, Pecoraro A, Mari A, Raspollini MR, et al. Exploring the Diversity and Predictors of Histopathological Findings Across the European Association of Urology Guidelines Office Rapid Reaction Group Priority Groups for Patients with Renal Tumors: Implications for Individualized Prioritization of Renal Cancer Care. Eur Urol Open Sci. 2021 Oct 28;34:5-9.
- Tandogdu Z, Collins J, Shaw G, Rohn J, Koves B, Sachdeva A, et al. Management of patients who opt for radical prostatectomy during the coronavirus disease 2019 (COVID-19) pandemic: an international accelerated consensus statement. BJU Int. 2021 Jun;127(6):729-741.
- Cakir OO, Castiglione F, Tandogdu Z, Collins J, Alnajjar HM, Akers C, et al. Management of penile cancer patients during the COVID-19 pandemic: An eUROGEN accelerated Delphi consensus study. Urol Oncol. 2021 Mar;39(3):197.e9-197.e17.
- Taheri D, Jahanshahi F, Khajavi A, Kafi F, Pouramini A, Farsani RM, et al. The Impact of Covid-19 Pandemic on Genitourinary Cancers Stage and Grade. Clin Genitourin Cancer. 2023 Feb;21(1):84-90.
- Diamand R, Ploussard G, Roumiguié M, Oderda M, Benamran D, Fiard G, et al. Timing and delay of radical prostatectomy do not lead to adverse oncologic outcomes: results from a large European cohort at the times of COVID-19 pandemic. World J Urol. 2021 Jun;39(6):1789-1796.
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





