Submitted:
10 September 2024
Posted:
11 September 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
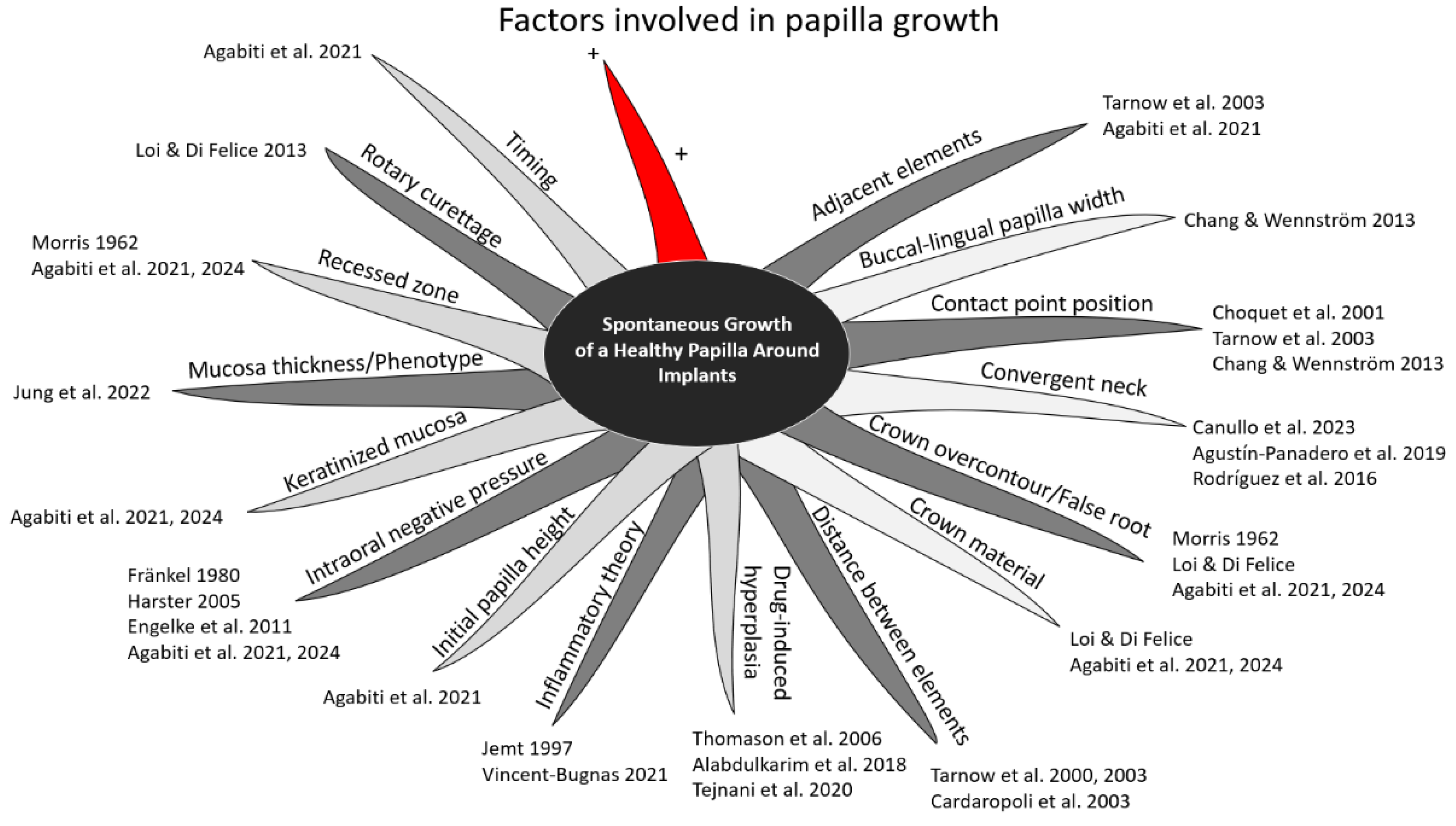
2.1. Factors Evaluated
- Buccal-lingual papilla width: The likelihood of a fully filled papilla is greatly influenced by the bucco-lingual width of the papilla's base [7].
- Initial papilla height: A post-hoc analysis of the data of an already published article was planned to evaluate the influence of the initial height of the papilla on the outcome [1].
- Mucosa thickness/phenotype: In a recent Consensus report it was concluded that the presence of a thick mucosa provides a tendency of better esthetic outcomes [26].
- Timing: It has been shown that most of the height gain occur in the first year after prosthetic delivering [1].
2.2. Tools used for Evaluation
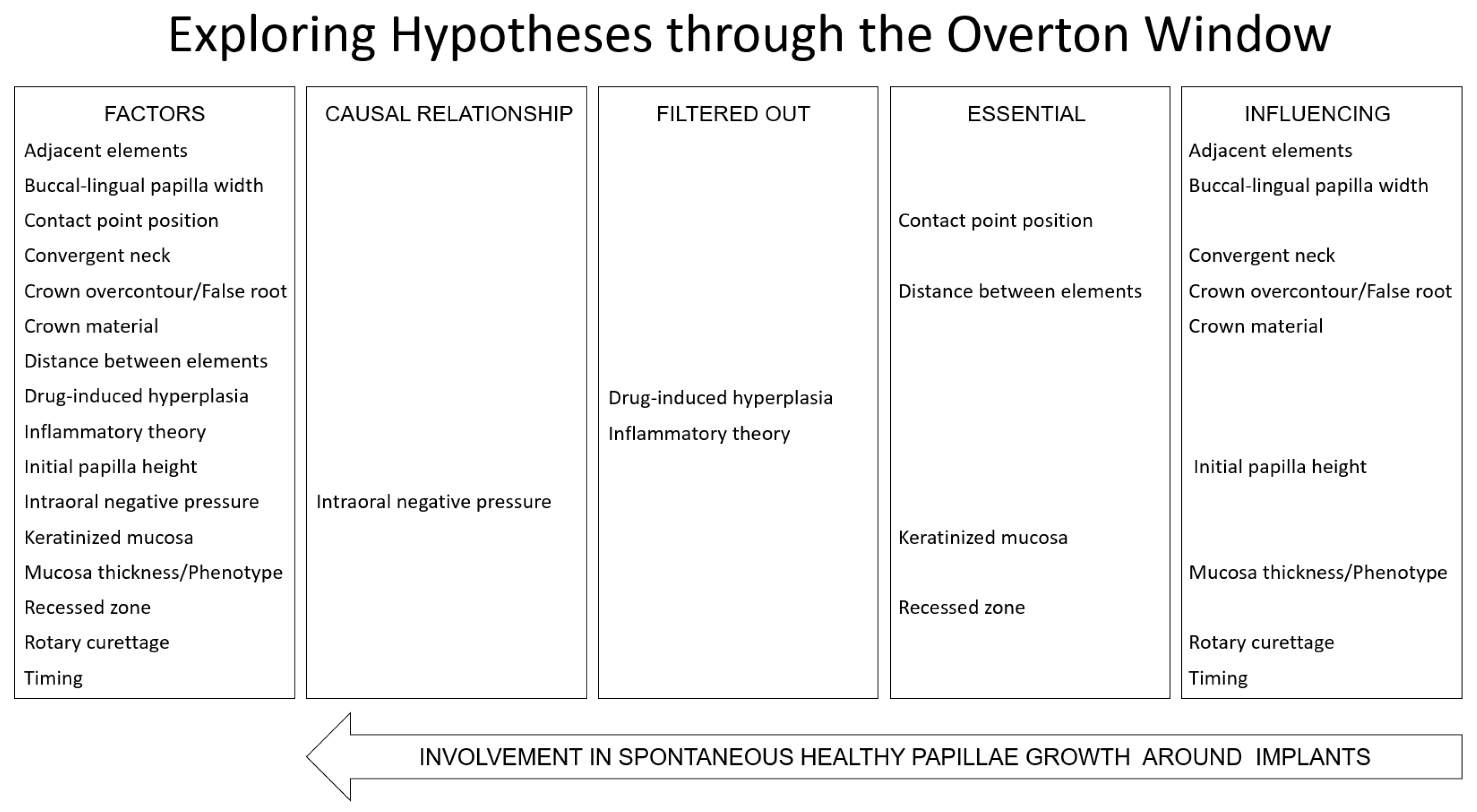
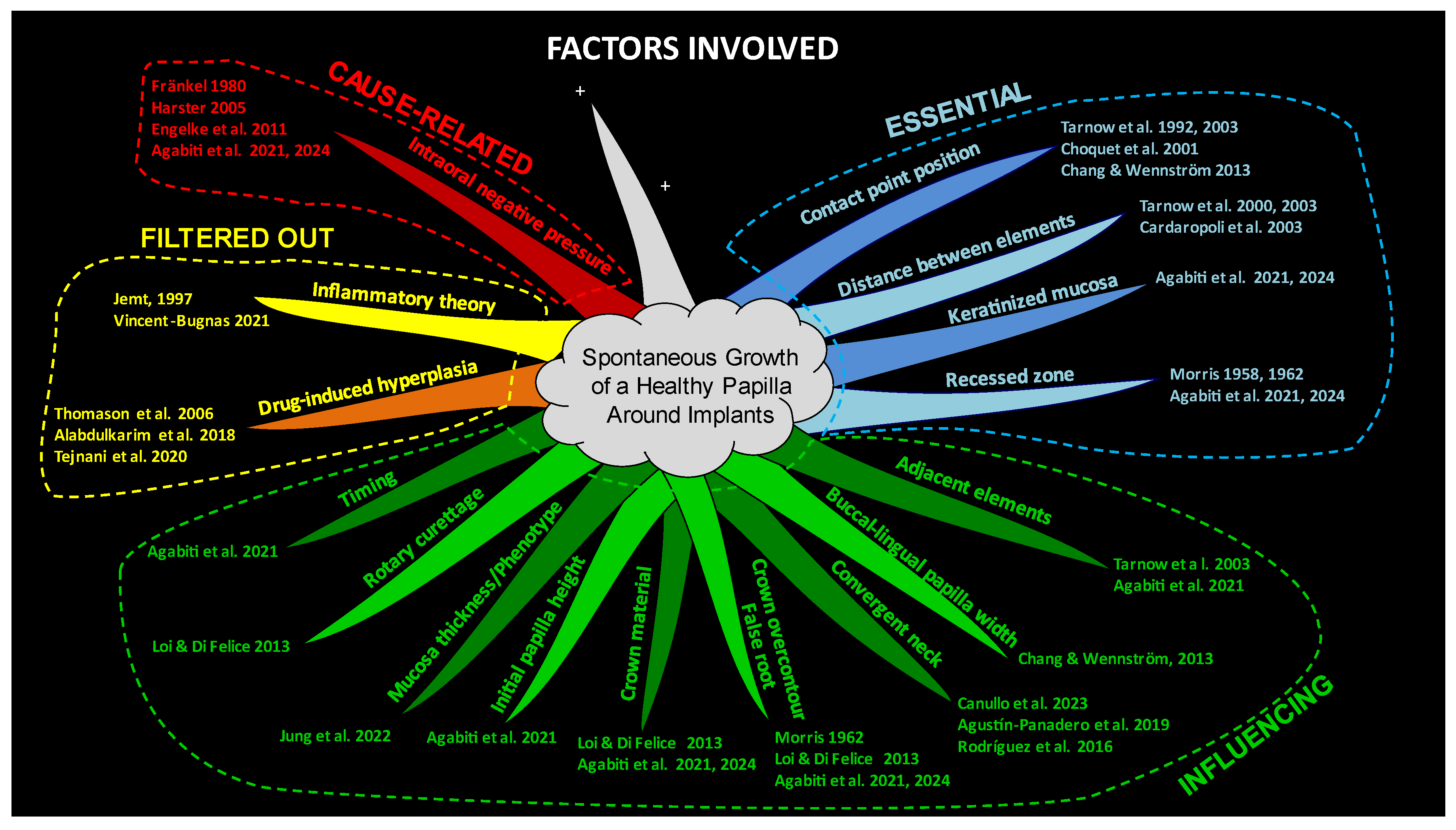
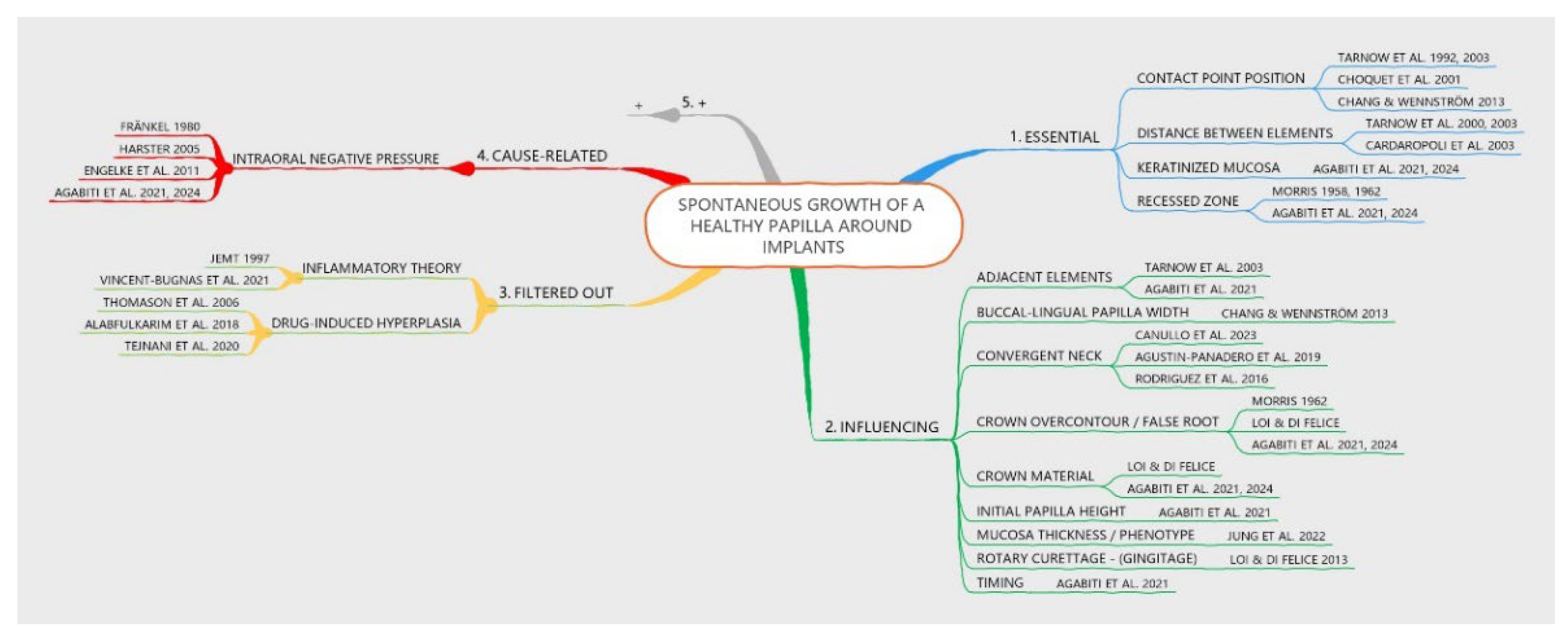
- Causal Relationship Factor - Identified when a potential cause-and-effect relationship with papilla growth is observed.
- Filtered Out Factor - Factors that exhibit a cause-and-effect relationship with papilla growth but whose effects are attributable to inflammation or drug influences, and therefore should not be associated with healthy tissue. This classification may also be applied to factors that are neither essential nor influential.
- Essential Factor - Determined as critical for papilla growth. Papilla growth cannot occur in the absence of this factor, despite no direct cause-and-effect relationship being observed.
- Influencing Factor - Recognized as having an impact on papilla growth, although not essential for it. No direct cause-and-effect relationship is observed with papilla growth.
3. Results
- Buccal-lingual papilla width: No cause-related relationship was found. The buccal-lingual width was considered to influence papilla growth [7].
- Inflammatory theory: The inflammatory theory presented a causal relationship with papilla growth. However, an inflammatory condition that causes edema and inflammatory infiltrate, leading to tissue growth, cannot be considered healthy [3]. The biofilm theory was invoked primarily in the context of orthodontic treatment, given the noticeable papilla growth despite the absence of significant plaque accumulation [23].
- Initial papilla height: A post-hoc analysis of data from a previously published study1 revealed that a lower initial height of the papilla was associated with a greater increase in papilla score (Table 1). No cause-related relationship was found. This factor was considered to influence papilla growth [1].
- Mucosa thickness/phenotype: No cause-related relationship was found. The mucosa thickness was considered to influence papilla growth [24].
- Timing: No cause-related relationship was found. The timing was considered influencing papilla growth [1].
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Agabiti I, Apaza Alccayhuaman KA, Nakajima Y, Botticelli D. An enigmatic soft tissue creeping phenomenon: The spontaneous peri-implant mucosa margin and papilla growth. A retrospective clinical study. Clin Exp Dent Res. 2021, 7, 474–483. [CrossRef] [PubMed] [PubMed Central]
- Agabiti I, Apaza Alccayhuaman KA, Taniguchi Z, Kuwano K, Botticelli D. An Enigmatic Soft-Tissue Creeping Phenomenon: The Spontaneous Peri-Implant Mucosa Margin and Papilla Growth, Part Two-A Scientifically Supported Hypothesis Article. Dent J (Basel). 2024, 12, 216. [CrossRef] [PubMed] [PubMed Central]
- Jemt, T. Regeneration of gingival papillae after single-implant treatment. Int J Periodontics Restorative Dent. 1997, 17, 326–33. [Google Scholar] [PubMed]
- Harster, P. Tissue modeling: the oral pump. Quintessence Int. 2005, 36, 633–640. [Google Scholar]
- Tarnow DP, Magner AW, Fletcher P. The effect of the distance from the contact point to the crest of bone on the presence or absence of the interproximal dental papilla. J Periodontol. 1992, 63, 995–6. [CrossRef] [PubMed]
- Tarnow D, Elian N, Fletcher P, et al. Vertical distance from the crest of bone to the height of the interproximal papilla between adjacent implants. J Periodontol. 2003, 74, 1785–1788. [CrossRef]
- Chang M, Wennström JL. Soft tissue topography and dimensions lateral to single implant-supported restorations. a cross-sectional study. Clin Oral Implants Res. 2013, 24, 556–562. [CrossRef]
- Tarnow DP, Cho SC, Wallace SS. The effect of inter-implant distance on the height of inter-implant bone crest. J Periodontol. 2000, 71, 546–549. [CrossRef]
- Cardaropoli G, Wennström JL, Lekholm U. Peri-implant bone alterations in relation to inter-unit distances. A 3-year retrospective study. Clin Oral Implants Res. 2003, 14, 430–6. [CrossRef] [PubMed]
- Weber, M. (1949). The Methodology of the Social Sciences. Free Press.
- Strand, M. , & Lizardo, O. Chance, Orientation, and Interpretation: Max Weber’s Neglected Probabilism and the Future of Social Theory. Sociological Theory 2022, 40, 149–169. [Google Scholar] [CrossRef]
- Choquet V, Hermans M, Adriaenssens P, Daelemans P, Tarnow DP, Malevez C. Clinical and radiographic evaluation of the papilla level adjacent to single-tooth dental implants. A retrospective study in the maxillary anterior region. J Periodontol. 2001, 72, 1364–71. [CrossRef] [PubMed]
- Canullo L, Giuliani A, Furlani M, Menini M, Piattelli A, Iezzi G. Influence of abutment macro- and micro-geometry on morphologic and morphometric features of peri-implant connective tissue. Clin Oral Implants Res. 2023, 34, 920–933. [CrossRef] [PubMed]
- Agustín-Panadero R, Martínez-Martínez N, Fernandez-Estevan L, Faus-López J, Solá-Ruíz MF. Influence of Transmucosal Area Morphology on Peri-Implant Bone Loss in Tissue-Level Implants. Int J Oral Maxillofac Implants. 2019, 34, 947–952. [CrossRef]
- Rodríguez X, Navajas A, Vela X, Fortuño A, Jimenez J, Nevins M. Arrangement of Peri-implant Connective Tissue Fibers Around Platform-Switching Implants with Conical Abutments and Its Relationship to the Underlying Bone: A Human Histologic Study. Int J Periodontics Restorative Dent. 2016, 36, 533–540. [CrossRef]
- Morris, ML. Artificial crown contours and gingival health. J. Prosthet Dent 1962, 12, 1146–1156. [Google Scholar] [CrossRef]
- Loi I, Di Felice A. Biologically oriented preparation technique (BOPT): a new approach for prosthetic restoration of periodontically healthy teeth. Eur J Esthet Dent. 2013, 8, 10–23 PMID: 23390618. [PubMed]
- Thomason, J.M.; Seymour, R. A. Phenytoin-induced gingival overgrowth: a review of the molecular, immune, and inflammatory features. Journal of Clinical Periodontology 2006, 33, 739–744. [Google Scholar]
- Alabdulkarim, M.; Bukhari, H.M.; Sheikh, S.A. Drug-induced gingival overgrowth: A comprehensive review. International Journal of Health Sciences 2018, 12, 82–89. [Google Scholar]
- Tejnani, A.; Diwan, A.; Sajjan, P. Drug-Induced Gingival Overgrowth: A Review. Cureus 2020, 12, e9307. [Google Scholar]
- Ingraham R, Sochat P, Hansing FJ. Rotary gingival curettage: A technique for tooth preparation and management of the gingival sulcus for impression taking. Int J Periodont Rest Dent 1981, 1, 9–33.
- Thorburn, W.M. The Myth of Occam's Razor. Mind 1918, 27, 345–353. [Google Scholar] [CrossRef]
- Vincent-Bugnas, S.; Borsa, L.; Gruss, A.; Lupi, L. Prioritization of predisposing factors of gingival hyperplasia during orthodontic treatment: The role of amount of biofilm. BMC Oral Health 2021, 21, 84. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Fränkel, R. A functional approach to orofacial orthopaedics. Br J Orthod. 1980, 7, 41–51. [Google Scholar] [CrossRef] [PubMed]
- Engelke W, Jung K, Knosel M. Intra-oral compartment pressures: a biofunctional model and experimental measurements under different conditions of posture. Clin Oral Investig. 2011, 15, 165–176.
- Jung RE, Becker K, Bienz SP, Dahlin C, Donos N, Hammächer C, Iglhaut G, Liñares A, Ortiz-Vigón A, Sanchez N, Sanz-Sánchez I, Thoma DS, Valles C, Weng D, Nart J. Effect of peri-implant mucosal thickness on esthetic outcomes and the efficacy of soft tissue augmentation procedures: Consensus report of group 2 of the SEPA/DGI/OF workshop. Clin Oral Implants Res. 2022, 33 (Suppl. 23), 100–108. [CrossRef] [PubMed]
- Mackinac Center for Public Policy. (2010). An introduction to the Overton window of political possibilities. Mackinac Center for Public Policy. Retrieved from https://www.mackinac.org/OvertonWindow.
- The Ultimate Book of Mind Maps – Tony Buzan - HarperThorsons, imprint of HarperCollins Publishers - New York City - New York, USA.
- Buzan, T. (1974). Use Your Head. London: BBC.
- Sober, E. (2015). Ockham's Razors: A User's Manual. Cambridge: Cambridge University Press.
- Peirce, C. S. Deduction, Induction, and Hypothesis. Popular Science Monthly 1878, 13, 470–482. [Google Scholar]
- Anderson, Douglas R. The evolution of Peirce’s concept of abduction. Transactions of the Charles S. Peirce Society 1986, 22, 145–164.
- Koffka, K. (1935). Principles of Gestalt Psychology. London: Routledge and Kegan Paul.
- Berglundh T, Lindhe J, Ericsson I, Marinello CP, Liljenberg B, Thomsen P. The soft tissue barrier at implants and teeth. Clin Oral Implants Res. 1991, 2, 81–90. [CrossRef] [PubMed]
- Lear, C.S.; Flanagan, J.B.; Moorrees, C.F. The frequency of deglutition in man. Archives of Oral Biology 1965, 10, 83–100. [Google Scholar] [CrossRef]
- Cao, H.; Li, X.; Liu, J. An updated review of the efficacy of cupping therapy. PLoS One 2012, 7, e31793. [Google Scholar] [CrossRef]
- Al-Bedah, A.M.; Elsubai, I.S.; Qureshi, N.A.; Aboushanab, T.S.; Ali, G.I.; El-Olemy, A.T.; Khalil, A.A. The medical perspective of cupping therapy: Effects and mechanisms of action. Journal of Traditional and Complementary Medicine 2019, 9, 90–97. [Google Scholar] [CrossRef]
| Mesial aspect | Distal aspect | ||
|---|---|---|---|
| Initial score | Gain | Initial score | Gain |
| 0 | 2.1 | 0 | 1.8 |
| 1 | 1.0 | 1 | 1.0 |
| 2 | 0.5 | 2 | 0.7 |
| The following Jemt`s score3 was adopted: 0, absence of papilla; 1, less than half of interdental embrasure height; 2, more than half of interdental embrasure height; 3, fully papilla filled interdental embrasure. | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




