1. Introduction
Herpes Simplex type 1 (HSV-1), Herpes Simples type 2 (HSV-2), and Varicella Zoster Virus (VZV) are double-stranded DNA viruses classified in the same subfamily of alphaviruses [
1]. Alphaviruses also belong to the superfamily of Herpesviridae [
1]. Usually, HSV-1 is the aetiological agent of oro-labial herpes and HSV-2 of genital herpes [
2]. Infections of these two Herpes viruses are amongst the most common viral infections with ulcers in the symptomatic phase in a high-risk group categorized as patients with sexually transmitted disease (STD) posing considerable morbidity and health economic inconvenience. A large majority of people worldwide have antibodies for the herpes simplex virus (HSV), with about 80% of them being unaware that they have been infected, as most infections occur without showing any symptoms. In 2016, the global seroprevalence of HSV-1 was around 67%, and HSV-2 was around 13% [
3,
4]. Transmission of both viruses occurs through close contact and results in a lifelong infection. Generally, people acquire HSV-1 early in life through the orolabial mucosal contact with the virus in sores or saliva. Nevertheless, oral-genital contact to cause genital herpes due to HSV-1 cannot be ignored. Conversely, HSV-2 infection occurs at a later stage of life through sexual contact. Virions are produced in the lytic replication phase due to an orchestrated expression of viral genes. Transmission of viruses from one host to another occurs in the lytic phase of HSV-1 and HSV-2 viruses [
5]. Nevertheless, a higher risk of transmission prevails when there are active sores [
6]. Alphaviruses primarily infect muco-epithelial cells. After primary infection these viruses establish latency with reactivation in mucosa time to time. During latency, there is limited gene expression and no production of viral particles [
7]. The reactivation of latent Herpesviruses is spontaneous or due to an external stinulii and highly dependent on the immune status of an individual. Oral risk habits introduce inflammatory and carcinogenic chemicals to oral mucosa [
8] thus, smoking, betel quid chewing, areca nut chewing and alcohol abuse are considered as environmental factors causing ecological stress on normal subgingival microbiome [
9] breaking the delicate balance between the host’s physiology and innate immune mechanisms. Anatomical pathology of oral fibroepithelial polyps (FEP)s appears as hyperplastic parakeratinized stratified squamous epithelium with arcading pattern and mixed inflammatory cell infiltrate lymphocytes predominantly and plasma cells [
10,
11] in haematoxylin and eosin (H&E) stain. Fibroepitheial polyps are not uncommon in the oral cavity at sites where there could be chronic irritation [
12]. The common modality of treatment becomes excision and usually sent for hisyopathological diagnosis. As this group of patients practiced risk habits such as betel quid chewing, it is reasonable to argue for the possibility of mucosal irritation which could predispose to occurrence of fibroepithelial polyps.
There is paucity of information on the association between oral risk habits and reactivation of HSV in oral mucosa among Sri Lankan patients. Thus, this retrospective study aimed to find co-variation between oral risk habits and HSV status in a cohort of Sri Lankan male patients presented with oral fibroepithelial polyps.
2. Material and Methods
2.1. Present Study
Present study was an additional component of the study aimed at assessing the oral microbiome of oral squamous cell carcinoma tiissues of a group of male patients in Sri Lanka The microbiome study comprised 25 Sinhala males with histologically confirmed OSCC involving the buccal mucosa or tongue (cases) to represents the over whelming majority and 27 Sinhala males with FEP as controls from the same anatomical sites of a large unmatched case control study conducted in selected 9, Oral and Maxillo-Facial (OMF) Units, located in 6 provinces namely, Western, Southern, Sabaragamuwa, North Western, Uva and Central in the Democartic Socialist Republic of Sri Lanka as described previously [
13].
2.2. Sample Size Calculation
The main sample consisted included 134 OSCC cases and 134 FEP controls and other benign mucosal lesion controls. Thus, the sample size was calculated using the formula described by Kelsey et al. [
14] The present study was based on 25 FEP patients.
2.3. Patients and Samples
Excissional biopsies from Sinhala males ≥ 40yrs with Fibro- Epithelial Polyps in buccial mucosa or tongue who were indulged in practicing at least one of betel quid chewing,smoking and alcohol consumption but not on antibiotics for the past two months as described previously [
13].
2.4. Data Collection
A structured pre-tested interviewer administered questioner was used to collect data on sociodemography and oral risk habits. Each participant provided written informed consent [
13].
2.5. Tissue Sampling, Genomic DNA Extraction and Quality Assessment
Deep tissue samples (~100 mg each) were dissected from frozen (stored at -80°C) excisional biopsies to prevent contamination from the tumour surface. Genomic DNA was then extracted using the Gentra Puregene Tissue kit (Qiagen) according to the manufacturer's protocol for solid tissue [Cat no. 158689] as described previously [
13,
15]. The concentration and purity of extracted genomic DNA were assessed by the nanodrop spectrophotometry. The quality assessment on the intergrity and absence of PCR inhibitors was done by GAPDH (human housekeeping gene) using β-globin PCR with the primers PCO3 and PCO4 as described previously. [
13].
2.6. Real Time PCR for HSV-1 and HSV-2 DNA
The real time PCR assay for HSV-1 and HSV-2 were set up separately using primer sequences as standardized, validated and published previously [
14].
Primers used for HSV rt PCR assay
| HSV-1-wield-F |
CGGCGTGTGACACTATCG |
HSV-1-wied-R |
GGCGTGTGACACTATCG |
| Watz-HSV2-F |
CGCCAAATACGCCTTAGCA |
HSV2-R |
GAAGGTTCTTCCCGCGAAAT |
Positive Controls: Extracted DNA from saliva from a patients known to be HSV-1and HSV -2 positive respectively.
Negative Controls: Extracted DNA from saliva from a patients known to be HSV-1and HSV -2 negative respectively.
Then, the real time PCR was performed on a Quant Studio 6- real -time machine with an initial step of hold stage of polymerase activation step at 950 C for 5 minutes, followed by 45 cycles of amplication (5 seconds denaturation at 950 C for 5 minutes; 30 seconds annealing (TM)/extension at 550 C) and melt curve stage of 3 steps (950 C for 10 minutes, 500 C for 10 minutes and 950 C for 15 minutes). Overall run duration was 73 minutes and 24 seconds. Positivity was determined via qPCR screening and melt curve analysis. If the melt curve temperature does not equal that of the calibration curve, that sample is reported virus-negative. Data entering and analysis were performed by the SPSS-21 Statistical Package. The statistical significance of qualitative and quantitative data was obtained by descriptive and inferential statistics. Among inferential statistics, the Chi-Square test was used to assess the relationship between categorical variables and Fisher’s exact for comparing groups (where cell counts were < 5).
3. Results
After confirming suitability through real-time PCR data analysis, HSV data of clinically diagnosed FEP subjectswere presented using figures. Cross tabulation was done to find out satistically significant co-variations between HSV positivity/negativity and oral risk habits.
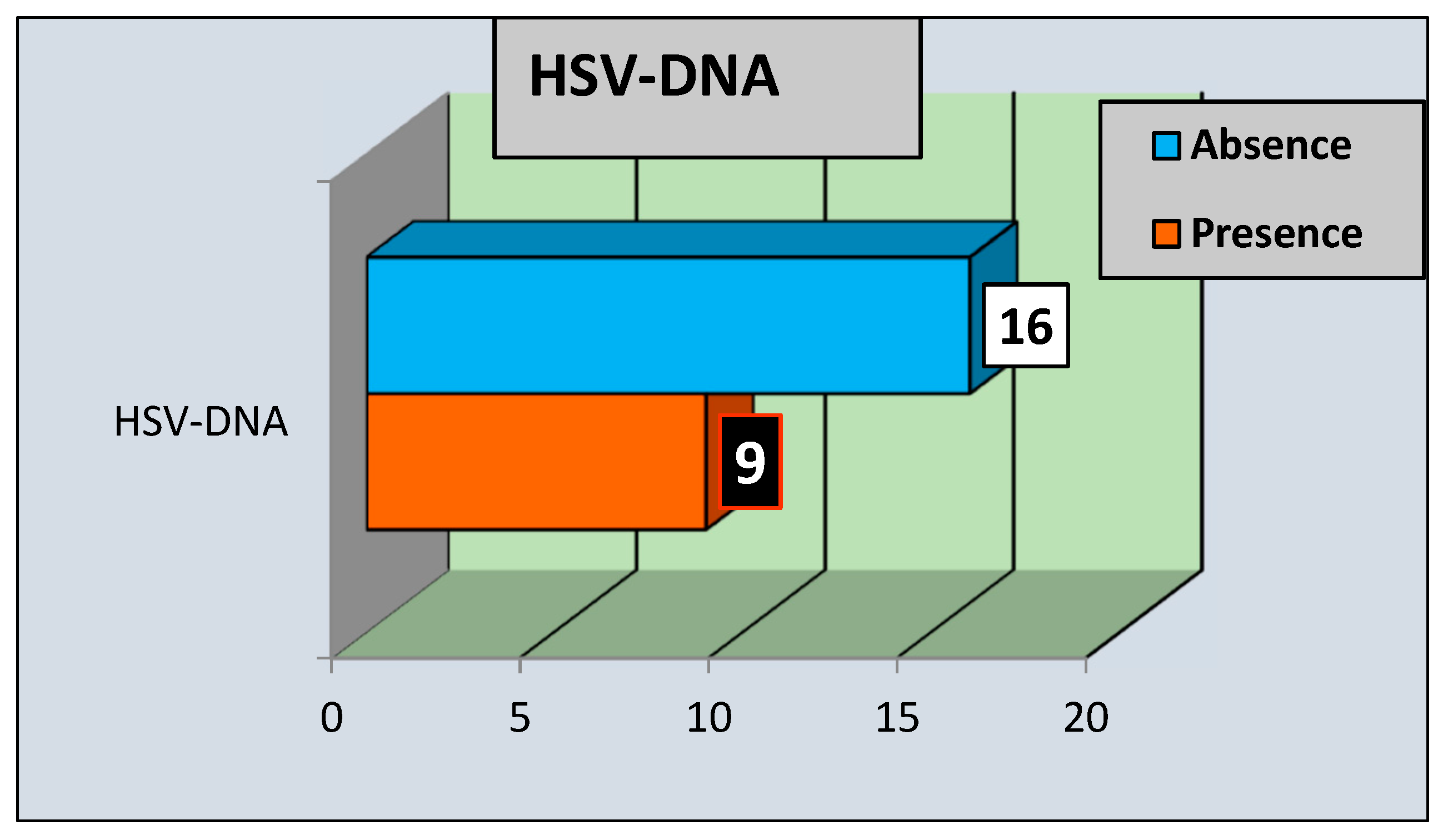
3.1. HSV-DNA Status in FEP Tissues
Of 25 tissues, HSV-DNA was present in 9 (44%) and absent in 16 (66 %) of FEP tissue sample as delineated in
Figure 1.
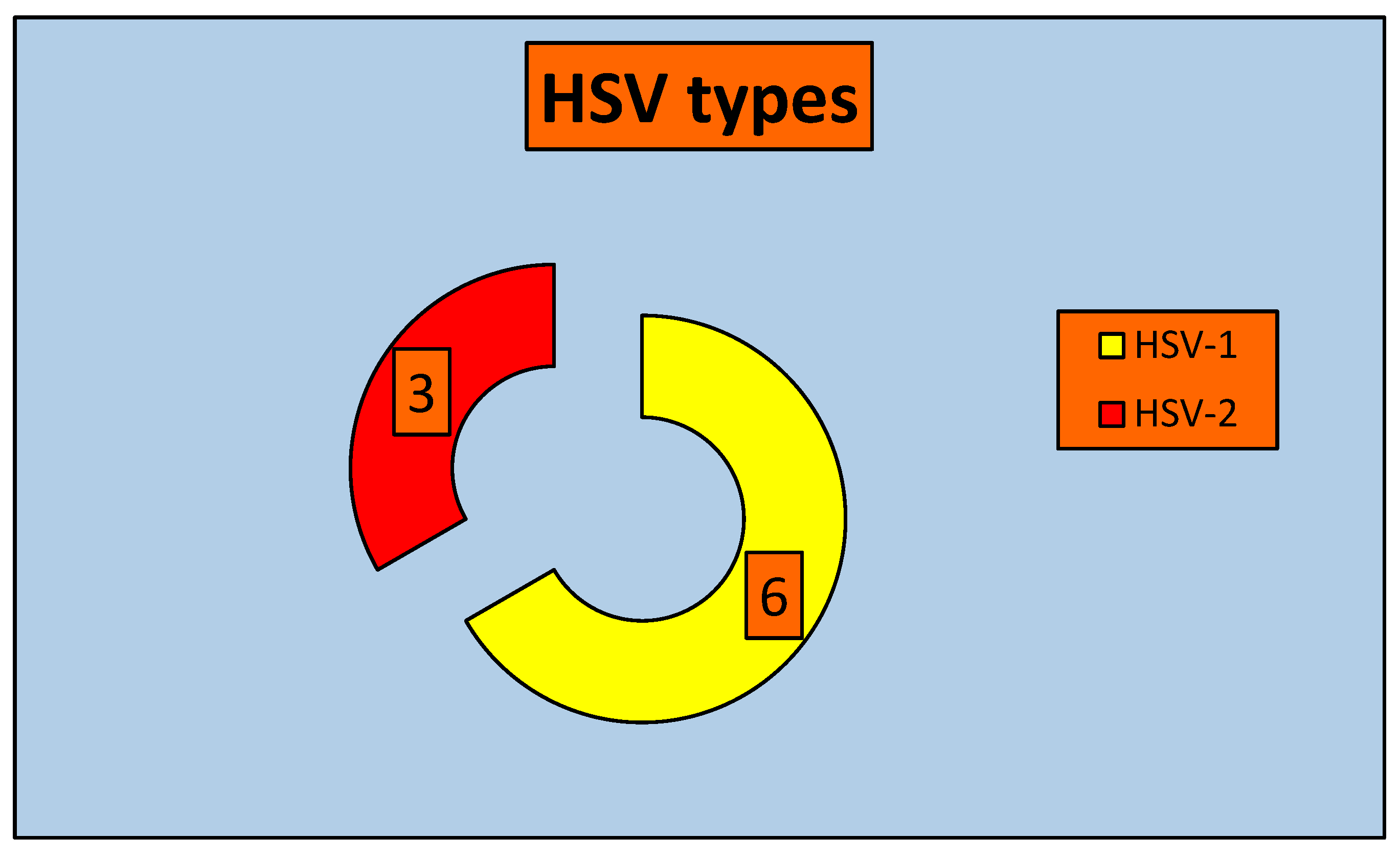
3.2. HSV Types in FEP Tissues
Among the HSV positives, 6 (66.67%) and 3 (33.33%) were HSV-1 and HSV-2 respectively as delineated in the
Figure 2.
3.3. HSV Status by Oral Risk Habits
Each two by two (bi-variate) table was used to present the data on co=variations between HSV status and the oral risk habit.
Table 1.
Distribution of HSV positivity and negativity by betel quid chewing habit.
Table 1.
Distribution of HSV positivity and negativity by betel quid chewing habit.
Variable
HSV status
|
Betelquid Never
n % |
chewing habit
Past
n % |
Sometimes
n % |
Daily
n % |
Total
n %
|
p value |
| Positive |
2 (22.2) |
0 (0.0) |
4 (44.4) |
3 (33.4) |
9 (44) |
*0.32 (p>0.05) |
| Negative |
2 (12.5) |
2 (12.5) |
3 (18.7) |
9 (56.3) |
16 (66) |
|
| Total |
4 (16.0) |
2 (8.0) |
7 (28.0) |
12 (48.0) |
25 (100) |
|
Accordingly, the majority of (44.4%) HSV positive subjects were some times betel quid chewrs, In contrast, the preponderance of HSV negatives were (56.3%) were daily betel quid chewers. Furthermore, (22.2%) of HSV positive, (12.5%) of HSV negative subjects were never betel quid chewers. Among HSV positivity and negativity, (33.4%) and (56.3%) respectively were daily betel quid chewers. However, these differences among HSV positives and negatives were not statistically significant (p<0.05).
Table 2.
Distribution of HSV positive and negative subjects by smoking habit.
Table 2.
Distribution of HSV positive and negative subjects by smoking habit.
Variable
HSV status |
Smoking habit
Never
n % |
One year back
n % |
Sometimes
n % |
Daily
n % |
Total
n %
|
p value |
| Positive |
4 (44.4) |
3 (33.3) |
2 (22.2) |
0 (0.0) |
9 (44) |
*0.05 (p =0.05) |
| Negative |
4 (25.0) |
3 (18.8) |
3 (18.8) |
6 (37.5) |
16 (66) |
|
| Total |
8 (32.0) |
6 (24.0) |
5 (20.0) |
6 (24.0) |
25 (100) |
|
Therefore, the highest percentage (44.4%) of HSV-positive subjects were never smokers. There was not even a single HSV-positive subject who was also a daily smoker. Moreover, HSV positives (22.2%) and HSV negatives (18.8%) were sometimes smokers. These differences were closer to being significant. Nevertheless, there was no statistically significant association (p<0.05) between HSV-DNA positive/negative difference and smoking pattern.
Table 3.
Distribution of presence or absence HSV-DNA by alcohol consumption .
Table 3.
Distribution of presence or absence HSV-DNA by alcohol consumption .
Variable
HSV status |
Smoking habit
Never
n % |
One year back
n % |
Sometimes
n % |
Daily
n % |
Total
n %
|
p value |
| Positive |
1 (11.1) |
1 (11.1) |
5 (55.6) |
2 (22.2) |
9 (44) |
*0.16 (p>0.05) |
| Negative |
2 (12.5) |
1 (6.3) |
11 (68.8) |
2 (12.5) |
16 (66) |
|
| Total |
3(12.0) |
2 (8.0) |
16 (64.0) |
4 (16.0) |
25 (100) |
|
Thus, the majority (55.6%) of HSV-positives and the preponderance (68.8%) of HSV-negatives were “sometimes” alcohol consumers. HSV positives (22.2%) but HSV negatives (12.5%) were daily alcohol drinkers. Among HSV positives, lesser percentage (11.1%) consumed alcohol one year ago. In contrast, the least of HSV negatives (6.3%) followed the same alcohol-consuming pattern. Moreover, the percentage of HSV positives and HSV negatives who were never drinkers were (11.1%) and (12.5%) respectively. Nonetheless, these differences were not statistically significant (p<0.05).
4. Discussion
Intelligible with the accidental finding of the overall rate of HSV-2 seropositivity (26%) amongst non-high-risk adult males ≥ 45 years with the highest HSV-2 seroprevalence (20%) in male blood donors previously [
14], we obtained consistent findings demonstrating HSV-2 DNA (33.33 %) among oral FEP patients from OMF units representing 6 out 9 Provinces in Sri Lanka. They were not clinically suspected patients for HSV infection. In another study, HSV-1 seroprevalence (82%) included Sri Lankan males and females ≥ 45 years. However, in the present study 66.67% of males ≥ 45yrs were found to contain HSV-1 DNA in their oral firo epithelial polyps. Our finding is much higher than the seroprevalence (HSV-1 IgG positive) of 4% and 12 % of Sri Lankan older adults 50 years and>50 years respectively [
15].Transmission of the highly contagious HSV is possible
particularly when a person is asymptomatic
because shedding occurs predominantly in the absence of symptoms. Once infected, this viral infection is incurable and lasts a lifetime with periods of latency in trigeminal or lumbosacral ganglia and reactivation and [
16] multiplication in epithelial cells [
17]. HSV infection can also be fatal, Alarmingly, especially in neonates and immune suppressed persons [
17].
To the best of the author’s knowledge, this is the first attempt to assess the association of HSV prevalence with risk habits among Sri Lankan male patients with fibroepithelial polyps. Despite inability to find significant associations, present findings should inspire researchers in the same field to explore the predisposing factors of asymptomatic reactivation of latent HSV in low-risk populations. As per risk habits, HSV status did not statistically significantly associated with the pattern of betel chewing habits in our study. There are no comparative and contrasting findings for and against this study respectively. Interestingly, in vitro evaluation of the
Areca catechu aqueous extract against HSV-1 demonstrated promising results lessening UL46 and US6 genes expression, probably due to interruption in HSV-1 binding to Vero cells or inhibition of the intermediate genes expression and late virus genes expression [
18].
In the current study, there was a marginal association between HSV (herpes simplex virus) positivity and negativity with smoking habits (p=0.05). However, this finding did not definitively support the conclusion that the use of tobacco products is primarily linked to HSV-2 infection and co-infection with HSV-1/HSV-2, as reported in a study on socio-demographic and behavioural factors associated with herpes simplex virus type 1 and 2 infections among adults in the USA [
16]. Previous studies have shown that tobacco smoking is associated with various sexually transmitted diseases, including HSV-2 [
20,
21]. In a cross-sectional study, it was found that there was a connection between alcohol consumption and the risk of HSV-2 infection [
22]. According to multivariate logistic regression models in the same study, both former and current drinkers showed a higher risk of HSV-2 infection compared to individuals who had never consumed alcohol. Eight studies in the latest systematic review [
23] found statistically significant associations between alcohol use, particularly heavy drinking occasions, and STIs. However, it was inconclusive whether alcohol increases the risk of STIs through risky sexual behaviour due to quality issues of the studies, which often relied on self-reported data for both exposure and outcomes [
24].
The present study did not find significant correlations between the status of Herpes Simplex Virus and oral risk habits in a group of Sri Lankan male oral fibroepithelial polyp patients. This study group belonged to the low risk group of STIs including HSV infections. No previous research has explored these areas. Additionally, the study found that 44% of oral FEP patients had asymptomatic HSV-DNA presence. Inflammation in older adults [
25] and induced social psycological stress in mice [
26] have been linked with reactivation of latent Herpesviruses and HSV-1 respectively. Further, despite asymptomatic colonization of HSV on fibroepithelial polyps there could be the possibility of ulceration. These findings provide rationale to hypothesize that chronic inflammation induced by substance abuse may affect the reactivation of latent HSV-1 and HSV-2 in this population, but further research is warranted to generate more conclusive evidence. The study has limitations, such as a small sample size, the presence of PCR inhibitors in a few samples which were not included, and the inability of surface sterilization using 70% alcohol to prevent surface contamination by salivary HSV.
It is estimated to affect around 2−3% of golobal pregnant women [27]. Vertical transmission during pregnancy is rare happening in less than 1% of cases but for those with active lesions or shedding the virus asymptomatically the risk of vertical transmission intrapartum is elevated. Neonatal HSV infection causes serious morbidity and mortality and leaves many survivors with permanent sequelae [25]. HSV-1/HSV-2 infection and co-infection demonstrate geographic and population specificity for acquiring sexually transmitted diseases (STDs) with sociodemographic, additives, recreational drugs and behavioural risk factors [
18].
5. Conclusions and Recommendations
The study found no significant relationship between the presence of Herpes Simplex Viral DNA and oral risk habits in a group of male oral fibroepithelial polyp patients in Sri Lanka. Thus, It is important to conduct more comprehensive case-control studies with larger sample sizes, controlling for potential confounding factors, to determine significant relationships and associations between different types of Herpes Simplex Virus and oral risk habits. The study indicates a need for more solid evidence to prevent and control the transmission of Herpes Simplex Virus (HSV) from a asymptomatic individual with oral habits. It also suggests that immune suppression, possibly combined with inflammatory compounds found in certain substances, may reactivate the virus. This theory should be investigated using an appropriate animal model. However, the present study strongly recommends interventions to change oral habits to prevent the development of FEPs due to chronic irritation of the oral tissue caused by these habits.
Author Contributions
Manosha Perera: Conceptualization; experimenta design; laboratory analysis; interpretation of results obtained by laboratory and statistical analysis; writing the original draft. Irosha Perera: Conceptualization; study design; sample size calculation; performing excisional biopsies; followed patients and revision; statistical analysis; revision of the manuscript.
Ethics Statement
The microbiome profile of oral squamous cell carcinoma tissues in a group of Sri Lankan male patients which received ethical approval from the Faculty Research Committee, Faculty of Dental Sciences, University of Peradeniya, Sri Lanka (FRC/ FDS/UOP/E/2014/32) and Griffith University Human Research Ethics Committee, Australia (DOH/18/14/ HREC).
Conflicts of Interest
The authors declare no conflict of interest.
References
- Dheerasekara WKH, Attanayake WPDS, Raziya MS, Jayawardhana BDS, Rajamanthri RGLS, et al. Alpha herpes virus infections in a group of patients clinically suspected of central nervous system infections in Sri Lanka. A brief laboratory report. Sri Lankan Journal of Infectious Diseases. 2020; Vol.10 (1):72-75.
- Nahmias AJ, Lee FK, Beckman-Nahmias S. Sero-epidemiological and-sociological patterns of herpes simplex virus infection in the world.Sc and J Infect Dis 1990;69:19–36.
- Bloom DC. Alphaherpesvirus latency: a dynamic state of transcription and reactivation. Adv Virus Res. 2016;94:53–80.
- Zhu S and Viejo-Borbolla A. Pathogenesis and virulence of herpes simplex virus.VIRULENCE 2021, VOL. 12, NO. 1, 2670–2702.
- Bloom DC. Alphaherpesvirus latency: a dynamic state of transcription and reactivation. Adv Virus Res. 2016;94:53–80.
- Knipe DM, Howley P. Field’s virology. Sixth. Vol. 2. 2013.
- Textoris J, Mallet F. Immunosuppression and herpes viral reactivation in intensive care unit patients: one size does not fit all. Crit Care. 2017; Aug 26;21(1):230. PMCID: PMC5574101. [CrossRef] [PubMed]
- Perera, M., Perera, I., & Tilakaratne, W. M.Oral Microbiome and Oral Cancer. Immunology for Dentistry. 2020; 79-99.
- Perera L and Perera I. Revisiting For Resolving: The Ecological Perspective of Periodontal Bacteriome for Prevention and Control of Periodontitis in COVID-19 Era. J Dental Sci . 2020, 5(5): 0 0 0 275.
- Vijayakumar T, Vinoth PK, Kiruthika D, Krishnaraj S, Kiruthika Met al. (2021) Fibroepithelial polyp: A pediatric case report withclinicopathologic overview. SRM J Res Dent Sci. 2021; 12: 41-43.
- Manosha Lakmali Perera and Irosha Rukmali Perera. Insight Into Versatility of Bacteriome Dominated by Rothia Mucilaginosa in Oral Fibro Epithelial Polyps. Biomed J Sci & Tech Res. 2022; 47(4). BJSTR. MS.ID.007527.
- Lees TFA, Bogdashich L, Godden D. Conserving resources in the diagnosis of intraoral fibroepithelial polyps. Br J Oral Maxillofac Surg. 2021 Jan;59(1):e9-e12. Epub 2020 Jun 6. [CrossRef] [PubMed]
- Perera, M. L. The microbiome profile of oral squamous cell carcinoma tissues in a group of Sri Lankan male patients. Griffith University, Queensland, Australia. 2017; 10.25904/1912/3833.
- Sunil-Chandra N., Wijesooriya L., Kumaratunga J., Jayasinghe A. Brown D Burden of Infection with Herpes Simplex Virus Type 2 amongst Low Risk Populations in the Western Province of Sri Lanka 2015: https://www.researchgate.net/publication/320386428.
- Fernando MAY, Mahanama AIK, Zulficar Ahamed FA, Hettigoda GM, Wimalarathna WKGI, Abeynayake JI. Sero-prevalence of type-specific Herpes Simplex virus infection: retrospective analysis among clinically suspected patients. Sri Lanka College of Microbiologists Bulletin. 2018;16 (1).
- Madavaraju K, Koganti R, Volety I, Yadavalli T, Shuk-la D. Herpes simplex virus cell entry mechanisms: Anupdate. Front Cell Infect Microbiol 2021; 10: 617578.
- Beydoun HA, Dail J, Ugwu B, Boueiz A, Beydoun MA. Socio-demographic and behavioral correlates of herpes simplex virus type 1 and 2 infections and co-infections among adults in the USA. Int J Infect Dis. 2010 Sep;14 Suppl 3:e154-60. Epub 2010 Apr 24. PMCID: PMC2921001. [CrossRef] [PubMed]
- Zamanian M, Asgari E, Afaridoon S, Akbarzadeh T, Sharifi Z, Saeedi M. Iranian Journal of Microbiology.Volume 16 Number 2 ; 251-257; Volume 16 Number 2 : 2024; 251-257.
- Beydoun HA, Dail J, Ugwu B, Boueiz A, Beydoun MA. Socio-demographic and behavioral correlates of herpes simplex virus type 1 and 2 infections and co-infections among adults in the USA. Int J Infect Dis. 2010 Sep;14 Suppl 3:e154-60. Epub 2010 Apr 24. PMCID: PMC2921001. [CrossRef] [PubMed]
- Cherpes TL, Meyn LA, Krohn MA, Hillier SL. Risk factors for infection with herpes simplex virus type 2: role of smoking, douching, uncircumcised males, and vaginal flora. Sex Transm Dis 2003;30:405–10. [PubMed: 12916131].
- Fatahzadeh M, Schwartz R. Human herpes simplex virus infections: epidemiology, pathogenesis, symptomatology, diagnosis, and management. J Am Acad Dermatol 2007;57:737–63. [PubMed:17939933].
- Shi Y, Zhang J, Wang Z, Shan F. The association between alcohol consumption and herpes simplex virus type 2: A cross-sectional from national health and nutrition examination survey 2009–2016. PLoS ONE. 2024; 19(7):e0307702. [CrossRef]
- Llamosas-Falcón L, Hasan OSM, Shuper PA, Rehm J. A systematic review on the impact of alcohol use on sexually transmitted infections. Int J Alcohol Drug Res. 2023 Jun;11(1):3-12. Epub 2023 Mar 31. PMCID: PMC10270666. [CrossRef] [PubMed]
- Padgett DA, Sheridan JF, Dorne J, Berntson GG, Candelora J, Glaser R. Social stress and the reactivation of latent herpes simplex virus type 1. Proc Natl Acad Sci U S A. 1998 Jun 9;95(12):7231-5. Erratum in: Proc Natl Acad Sci U S A 1998 Sep 29;95(20):12070. PMCID: PMC22787. [CrossRef] [PubMed]
- Jeanette M. Bennett, Ronald Glaser, William B. Malarkey, David Q. Beversdorf, Juan Peng, Janice K. Kiecolt-Glaser,Inflammation and reactivation of latent herpesviruses in older adults,Brain, Behavior, and Immunity,Volume 26, Issue 5,2012.
- Wafaa Ali Belail Hammad, Justin C. Konje,Herpes simplex virus infection in pregnancy An update,European Journal of Obstetrics & Gynecology and Reproductive Biology,Volume 259,2021, Pages 38-4.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).