1. Introduction
The importance of effective, innovative leadership in healthcare is well recognized as a driving source for successful operation of organizations [
1,
2]. Successful leaders have improved quality and integration of care [
3], influenced patient outcomes [
4], organizational performance [
5,
6], and contributed to reduced adverse events [
7]. Effective leadership has impacted morbidity and mortality [
8], and can enable their growth, development, and advancement as professionals [
6,
9]. In addition, the relationship of leadership and the reduction of adverse effects is critically related to lower patient mortality, staff satisfaction, and may affect employee attitudes which then can impact retention [
10,
11].
The triad of leadership strategies, skills, and practices in healthcare settings extends well beyond clinical expertise to include authentic and quality leadership attributes which contribute to the expected standards of a healthy workplace [
12] and employee well-being [
13]. Clinical nurses want to have visible, value-driven leaders with effective communication skills that listen to and include them in decision-making [
14]. Leaders are needed who will advocate for and support staff’s growth and development, as well as recognize and reward staff accomplishments [
15].
Currently, the forecast for the nursing shortage worldwide is to exceed 9 million by 2030 [
16], and HRSA predicts a shortage of 78,610 full-time RNs in 2025 and 63,720 in 2030 [
17]. While nursing shortages have risen and fallen over the years, it is known that nursing retention is an issue influenced by satisfaction, burnout, moral distress and many other reasons, all impacted by leadership [
18]. The Covid-19 pandemic severely exacerbated the nursing shortage and retention crisis, revealed challenges for leadership, and required innovative solutions [
19]. Surveys show nearly 1 in 5 RNs left their positions in 2022-2023, disengaged nurses are 2.2 times more likely to leave their positions, and when nurses have ineffective leaders, they are 1.5 times more likely to leave their positions [
20]. The relationship of leadership to retention and impacting the nursing shortage is directly correlated, thus further supporting the need for focused and practical leadership education.
In a study by Aydogdu [
21], BSN nursing students reported awareness of the importance of nursing leadership, yet they also reported not having sufficient or any classes on leadership as well feeling unprepared for leadership positions. Faculty in both undergraduate and graduate nursing programs are charged with educating students on multiple theories, styles of leadership, attributes, and behaviors to prepare them for the complexities of healthcare environments. The critical need for exemplary nursing leaders who will promote high quality patient care [
22], presents multiple challenges for nursing education programs to prepare graduates with knowledge and practical tools to embrace the challenge. Leadership education begins at entry level in preparing new graduates, and progresses to higher levels of complexity and skills development with each advanced degree program.
Styles and Attributes of Leadership
Numerous styles of leadership have been shown to be directly related to promoting and achieving positive outcomes, to include influencing professional relationships [
11]. Effective leadership strategies support and contribute to a positive work environment resulting in organizational success and increase employee morale and retention [
23,
24]. Nursing leadership curricula must include exposure to multiple styles of leadership to provide choices for how to adapt to different situations, and to help students to identify their own strengths, leadership styles, and attributes. Three commonly used and referenced styles of leadership are described here: transformational [
3], relational [
25], and authentic [
14].
Relational Leadership
Relational leadership theory (RLT) focuses on social interconnectivity and the contextual dynamics of relationships between leader and team members [
25]. Elements of RLT include respect, inclusion, empowerment, purposefulness, and team processes. Two leadership studies by Raso et al. [
14,
15] provided empirical evidence supporting the connection of relational leadership to positive outcomes, including employee engagement leading to a more positive workforce, a healthier work environment, all of which are correlated with improved patient outcomes. Relational leadership traits are based on optimism, integrity, positive emotions, and employee growth and development, which in nursing leadership is demonstrated by ethical choices, positive change, purpose, growth, and social connections. By prioritizing the human interconnectivity inherent within the healthcare team, RLT enables collaborations, increased productivity, positive social capital, and provides an effective balance to the heavy influence of technology in healthcare environments and in nursing roles. Given the presence of incivility at various levels of healthcare, relational leadership promotes a foundation for creating positive relationships to foster inclusion and support retention [
25]. The emphasis of the need to proactively prevent incivility yet address it when present, is an essential part of leadership education at all levels [
28].
Authentic Leadership
Authentic nursing leadership (ANL) embraces nursing values, which resonates strongly with many clinical nurses. Several constructs of ANL include self-awareness, balanced processing, and personal integrity, which embraces moral and ethical courage. Raso, Fitzpatrick, and Masick found that nurses value ANL, which correlated moderately to healthy work environments [
14]. Alilyyani (2022) found positive effects of ANL and trust in managers, however, did not find relationships between ANL and job performance[
29]. Building trust is positively correlated with higher levels of engagement, satisfaction, and relational improved work environments. This style is more likely to be threaded throughout the nursing curriculum, at all levels, in didactic coursework to reflect the nursing decisions necessary in clinical practice.
Effective Leadership Traits
There are distinct and different characteristics in the plethora of leadership styles that motivate, influence, and direct followers. Nevertheless, threaded through the various leadership styles are also common traits that embody effective and successful leadership practice. Reynolds (2021) suggests acquiring the soft skills of leadership such as effective communication, enthusiasm, emotional intelligence, and interpersonal skills as the positive strategies to influence human capital [
30]. Successful nurse leaders and managers are open and responsive to nursing staff suggestions about decision making in the workplace, promote autonomy, and collaborative team engagement that results in safe and effective patient outcomes. Additional positive approaches include seeking regular feedback and promoting recognition, performance improvement, and advocacy for staff nurses. Nurse leaders and managers must be visible and actively engaged at whatever level their role may be in the healthcare organization. Staff retention and satisfaction, both essential elements for a successful organization, are achieved by enhancing leadership team behaviors. This includes understanding and recognizing the different generational needs regarding staffing, family, and social life [
31]. Healthcare environments now have multi-generational personnel, with some distinct approaches to the “how-to” of working. These approaches should be included in nursing leadership course content, to provide students with the desired attributes and behaviors for future transitions into leadership roles.
Ineffective Leadership Traits
Education must be reality-based; thus it is crucial to include content about ineffective leadership traits and practices that can increase or exacerbate challenges within healthcare environments. While impossible to prepare for every situation, common challenges are inherent in healthcare leadership with recognized strategies that may prevent or intentionally address them.
Lepez (2024) identifies ten challenges in healthcare leadership, focusing on self-awareness, communication, empathy, resistance to change, delegation, overconfidence, accountability, cognitive biases, time management, and issues influenced by pride and ego [
32]. One type of ineffective leadership, labeled toxic leadership, is a decidedly negative style with systematic or even destructive behaviors. This may include attitudes and actions that demean, threaten, belittle, ignore, denigrate, micromanage, and may be abusive in nature [
33]. Labrague, Nwafor and Tsaras (2020) identified toxic leadership as a predictor related to decreased job satisfaction, absenteeism, psychological distress, and intention to leave nursing. They surveyed 770 RNs across the Philippines, to self-report on transformational vs. toxic leadership styles [
34]. Nurses working with leaders who exhibited toxic leadership behaviors reported lower satisfaction, higher job-related stress and absenteeism, as well as higher intent to leave the nursing profession. Areas of leadership concerns that can contribute to staff and leader disengagement include lack of presence, communication, recognition, follow-through, and collaborative decision-making [
15]. Students must learn about both effective and toxic leadership styles, attributes, and behaviors in order to build their own toolkit for success and be prepared for the reality of the workplace.
Nursing Education Opportunities
Nurse educators and leaders understand the need for preparation not only for their own roles, but also for those working together with leaders in units and in executive positions. While the need for high-quality, compassionate, and diverse leadership is clear and a global concern, the educational blueprint and journey towards leadership development is less developed [
35]. As healthcare delivery evolves continuously and at a rapid pace, educators may ask many questions, including: What makes a nurse leader or executive effective through the eyes of students or those starting out in leadership roles? What do our students hope for and expect are important styles, attributes, and behaviors in leaders, now and in the future, to enable healthy work environments? This study was based upon reflective leadership assignments for baccalaureate and master’s nursing students that included a comprehensive self-assessment of their own knowledge, understanding, and perceptions of leadership approaches and roles.
2. Materials and Methods
This mixed-methods study collected, analyzed, and compared data from leadership assignments that were completed by two groups of nursing students, in undergraduate (RN-BSN) and graduate (MS in Nursing Administration) programs within a public university located in upstate New York. Both nursing programs are fully online, with asynchronous learning activities and assessments. The American Organization for Nursing Leadership (AONL), the premier nursing organization for nursing leaders, was used as the framework for this study. “The AONL Nurse Leader Executive Nurse Competencies provide the framework for the knowledge, skills, and abilities associated with effective leadership--from first time leaders to experienced executives. The overarching competencies encompass the breadth and depth of the nursing leadership specialty, across health care settings and leadership roles” [
36]. Nursing believes that adherence to professional standards is foundational and helps to ensure high quality performance, whether in practice or in non-practice areas, such as education or leadership. The AONL competencies are the professional standards used to prepare competent nurse leaders, which ultimately will improve the health and well-being of populations [
37].
The study sample was drawn from student enrollment in the undergraduate and graduate programs. There were a total of 112 student submissions in archived courses; sixty RN-BSN (post-licensure) and fifty-two MS in nursing administration students identified tips for success for leaders in the current healthcare environment, which represented their perceived leadership priorities. Data were collected retrospectively from a portion of an assignment within one course each from the RN-BSN (henceforth referred to as “BSN”) and the MS in Nursing Administration programs, during the Fall and Spring semesters from 2020-2023. The BSN course was Leadership and Management in Nursing, an upper-level leadership course that includes a hands-on clinical leadership practicum occurring within a healthcare setting. The data were collected from a graded presentation created by students that included audio-narrated slides that focused on leadership skills. Voice-over presentations are used extensively in online programs to enable asynchronous interaction with presentation slides that may include written documents, photos, videos, or other media. The final reflective assignment provided a synthesis of the course learning activities. For the final slide the BSN students were asked the question: “Discuss one tip or advice you would give to a new nurse leader/manager to help them to be successful.” The MS in Nursing Administration course in Strategic Management was the final didactic course preceding two intense immersion executive leadership practicum experiences. Students were asked the question: “What tips would you give to future nurse leaders to help them be successful, while managing a strategic process?”
Students’ comments to these questions were analyzed using qualitative concept analysis. Data were collected from each presentation after student names had been removed by the research team and were not publicly accessible to anyone aside from the researchers. The researcher who collected the student’s data transcribed the comments and assigned the comments a number. The relevant content on the slide and the comments on the audio file were transcribed verbatim onto a table. Each comment was then analyzed for alignment with the domains, competencies, and behaviors of the AONL Nurse Executive Competencies [
36].
The quantitative descriptive data was created by tabulation of the total responses per domain, demonstrating alignment to the AONL Competencies. The data were then compared for which behaviors and competencies were specific to each level of nursing program or which were common. The final step for the qualitative research analysis was verification by the investigators of each other’s results. This included a full review of all components: the data and identification of leadership behaviors, alignment with the AONL Competencies, and a full recount of the descriptive data. This verification process confirmed the interpretation of participants' comments, alignment to standards, and the descriptive data, which assured both qualitative and quantitative rigor.
3. Results
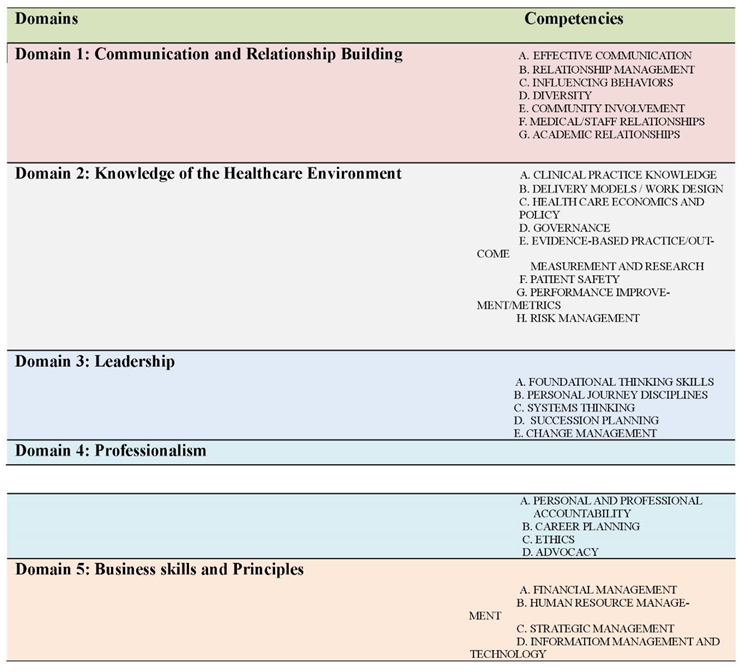
The AONL Nurse Executive Competencies consist of five domains, with each one divided into competencies (
Appendix A), and then further divided into behaviors [
36]. The number of behaviors that reflect the competencies within the standards document exceeds the scope of this report, however a selection of the domain specific behaviors has been provided that align with the data in order to demonstrate how the domain and competencies may be enacted. Each domain is presented with the associated data alignment with the competencies.
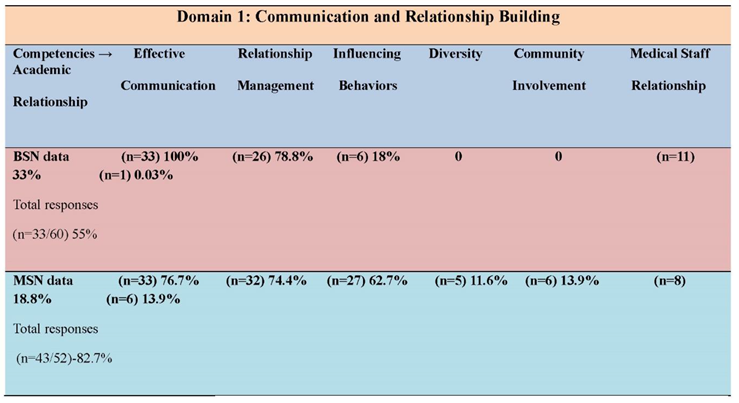
Domain 1: Communication and Relationship Building
Seven competencies are associated with Domain 1: Communication and Relationship Building are listed below in
Table 1 with the students’ response rates. Students in both programs expressed the importance of effective communication skills. BSN students (55%) addressed this domain in their tips for leaders, while MS in nursing administration students (87.7%) spoke of the importance of communication.
Table 1.
Domain 1: Communication and Relationship Building.
Table 1.
Domain 1: Communication and Relationship Building.
The BSN students suggest a micro focus:
Have open and honest communication with staff.
Listen to all members of the team.
Practice active listening. Employees like to be heard.
The MS students suggest a macro focus, emphasizing the executive leadership role:
Be visionary, lead with passion, and harness emotional intelligence. Be adaptable and nimble. Establish a culture of positivity, teamwork, collaboration, and accountability and be knowledgeable about industry trends seeking cost effective and efficient solutions for organization success.
Culture is key. Establish a culture of trust where employees can speak up and give critical feedback where everyone is committed to organizational success. The leader sets the tone and must model these behaviors to set the culture.
Strategic management requires just the right touch. You do not want to overmanage or under manage. Be innovative. Set the tone and the culture and empower staff to make their own decisions. Be a visionary, keep the big picture and do not get lost in the weeds. Be able to adapt and change direction as necessary.
There are 40 behaviors identified by the AONL Competencies for Domain 1. A sample of these behaviors reflect connection to the students’ comments, and include the following: Demonstrate skill in interpersonal communication, create a trusting environment by engaging staff and others in decision making, facilitate consensus building, create a shared vision, establish cultural competency in the workforce, and inspire desired behaviors and manage undesired behaviors.
Effective communication and relations management competencies were identified as priorities for both the BSN and MS students. Nursing students learn that the importance of active listening is emphasized to maintain conversations to be positive and engaging, and to have the other person feel valued. Effective communication can build relationships, enhance the patient experience and support the goals of nursing leadership [
30]. The ability of the nurse to lead and be seen as trustworthy through written and oral communication skills is practiced in nursing education. The recent Covid-19 pandemic had a detrimental effect on communication with healthcare workers, with the prevention of full facial communication and the effects upon relationships in clinical settings [
38]. The results of Domain 1 indicate the importance students placed on the competencies of effective communication and relationship management. This represents the ongoing need for efforts to return to pre-COVID communication protocols, and to build and maintain relationships through face-to-face communication strategies, whenever possible. Reverting to a more personalized communication style can be a positive force to help staff to achieve common goals and build a shared vision.
The BSN students did not prioritize the competencies of diversity (n=0), community involvement (n=0), and/or academic relationships (n=1). BSN programs promote diversity and cultural awareness, as students are taught to treat everyone with fairness, empathy, and respect, and there are current expectations for diversity, equity and inclusion (DEI) content throughout nursing education. The students know this content; however they did not prioritize it for leadership. The focus at this level of education is hospital-based patient centered safe care and the results are reflecting more basic clinical practices.
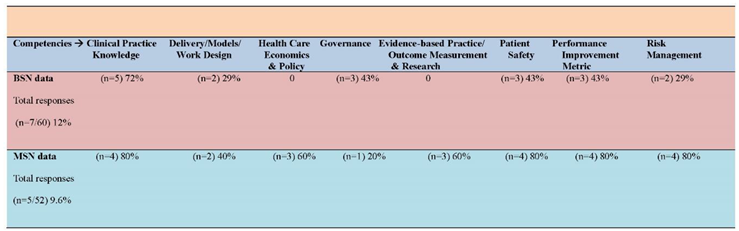
Domain 2: Knowledge of the Healthcare Environment
The eight competencies that are associated with Domain 2: Knowledge of the Healthcare Environment are listed below in
Table 2 with the students’ response rates.
The BSN student response comments reflected on lifelong learning strategies:
Never stop evaluating your skills
Focus on innovation. Apply ideas to new methods of care.
Share your knowledge with your staff.
The MS student response comments focused on the pursuit of excellence:
Focus on service, patient & staff satisfaction, quality and measuring safety, encourage growth of staff and organization, review business plans and make changes as needed.
Embrace change, innovate. Analyze situations to eliminate the gap between current and desired state. Use high reliability concepts and evidence-based metrics in decision-making.
Having a background in nursing knowledge is important but merging it with administrative skills that include business and financial skills can help future nurse leaders be successful in their roles as they would have the knowledge to drive the business of care delivery while understanding the importance of quality patient- centered care as it impacts the nursing workforce and the organization.
Table 2.
Domain 2: Knowledge of the HealthCare Environment.
Table 2.
Domain 2: Knowledge of the HealthCare Environment.
There are 49 behaviors identified by the AONL Competencies for Domain 2. A sample of these behaviors reflect connection to the students’ comments, and include the following: Demonstrate knowledge of current nursing practice and the roles and functions of patient care team members, communicate patient care standards as established by accreditation, regulation, and quality agencies, participate in strategic planning and quality initiatives with the governing body, support the development of an organization-wide patient safety program, and use data and other resources of evidence to inform decision making.
Neither student group (RN- BSN, n= 7 and MS n=5) identified knowledge as a priority tip to share with leaders. Based on the low response rates, BSN (n= 7) students identified governance and patient safety as priorities, while economics, policy, research and outcome measurement were scored as zero. Their responses (n=7) focused on clinical knowledge issues to include patient safety delivery model, performance improvement and risk management, which are all competencies that a basic level nursing student and an entry level nurse deal with regularly. A score of zero was tabulated for research and evidence-based practice/outcome measurements. This presents an opportunity to revise the BSN curriculum to further emphasize research and evidence-based practice/measurement outcomes. This content is included in the curriculum and reinforced, but these results indicate it was not felt to be a leadership priority. The MS students and MS, (n=5), prioritized 7 out of the 8 competencies scoring them from 40% (n= 2) to 80% (n=4). The low response rates may be reflective of the students already acquiring clinical knowledge and skill sets, through advanced nursing education and clinical expertise. Governance received the lowest score of 20% (n=1). The issue of governance overlaps with team building in the Domain 3: Leadership. This presents an opportunity to revise the graduate curriculum to further emphasize the importance of shared governance and team building. The sample for this domain is low, therefore representing the need for a larger sample to make more evidence-based conclusions from the analysis.
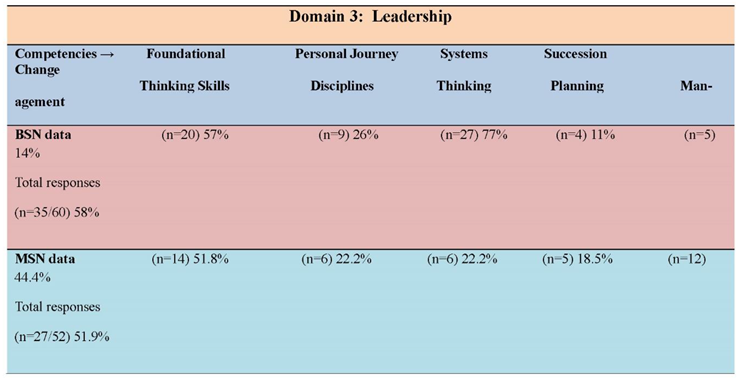
Domain 3: Leadership
The five competencies that are associated with Domain 3: Leadership are listed below in
Table 3 with the students’ response rates. Leadership was the focus of both the BSN (n=35) and the MS (n=27) students in this assignment. More than 50% of each student group included leadership tips in their assignment responses.
Table 3.
Domain 3: Leadership.
Table 3.
Domain 3: Leadership.
BSN response comments emphasized team building strategies:
Focus on the work climate the leader creates. Show respect for your staff. Be consistent and fair. Engage staff in decision-making. Hire carefully. Invest in staff’s professional development and strengths. Have a team approach.
Teamwork is important.
Be honest. Promote teamwork. Advocate for your team and this will promote happier staff and better patient outcomes.
MS student response comments had a broader perspective and included strategies reflective of executive practice:
Embrace change, innovate. Analyze situations to eliminate the gap between current and desired state. Use high reliability concepts and evidence-based metrics in decision-making.
Lead through transition periods, this requires transformational leadership. Creating strategies of a shared vision. Implementing the strategies with clear communication. Empower others to lead and ensure access to the resources needed to provide quality care and inspire people to meet the demands of the future.
Monitor and control strategic momentum. Effective communication to provide guidance to the nursing staff through organizational change. Leadership should implement the culture of nursing into the strategic planning process.
There are 21 behaviors identified by the AONL Competencies for Domain 3. A sample of these behaviors reflect connection to the students’ comments, and include the following: maintain curiosity and an eagerness to explore new knowledge and ideas, provide visionary thinking on issues that impact the healthcare organization, establish mechanisms that provide for early identification and mentoring of staff with leadership potential, and serve as a change leader.
The strong results are evidence of the fact that the data were collected from the last assignment in leadership courses where most of the competencies are currently or already have been discussed in previous courses. Succession planning is not discussed in the BSN and the MS courses and should be considered as a topic in the future. Change management is discussed and a basis for an assignment in both leadership courses in this study. MS students (n=12) identified this as an important competency for leader success. BSN students focus on change at a micro (unit) level where change is implemented, rather than strategized. While MS students focus on change at the mezzo (departmental) and macro (organizational) levels where change is strategized and planned. This presents the opportunity for nurse leaders and leadership students to embrace the importance of shared governance and team building to encourage collaboration throughout the organization. The BSN students (n=27) recognized the importance of a systems thinking approach to problem solving versus the MS students (n=6). Systems thinking is a complex approach that connects the relationship and interactions between organizational functions [
39]. Systems thinking is taught in both the BSN and MS leadership courses. This is new content for the BSN students studying change management and a foundational concept woven through the graduate level courses.
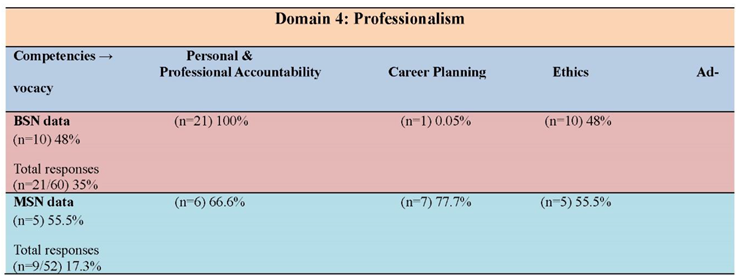
Domain 4: Professionalism
The four competencies that are associated with Domain 4: Professionalism are listed below in
Table 4 with the students’ response rates.
Table 4.
Domain 4: Professionalism.
Table 4.
Domain 4: Professionalism.
BSN student response comments reflected on self-improvement strategies:
Seek and give timely feedback.
Be open to constructive criticism. Treat others as you would like to be treated.
Have confidence in yourself.
MS response comments also reflected on self-improvement strategies that demonstrated greater in depth thought processes:
Remain open minded, always welcome feedback and continuously seek opportunities to teach by example. Always seek to learn.
Embrace change and innovation and seek learning opportunities throughout one’s career.
Take a break between moments of efficiency, take a breath and enjoy the successes.
There are 20 behaviors identified by the AONL Competencies for Domain 4. A sample of these behaviors reflect connection to the students’ comments, and include the following: Seek input and mentorship from others in career planning and development, act on feedback about personal strengths and weaknesses, develop a personal and professional career plan and measure progress, and achieve and maintain professional certification for self.
Thirty-five percent of the BSN students (n=21) prioritized personal and professional accountability as a key for leader success and half of these students (n= 10) recognized ethics and advocacy as significant traits for nurse leaders to have. Career planning was mentioned by only one student (0.05%). Most of the students enrolled in an RN-BSN program are already working in New York State where a BSN degree is required for continued employment ten years post-licensure. It is evident that their current focus is maintaining their current position rather than embarking on career advancement at this time. A small number (n=9) of MS students identified that aspects of professionalism were needed for leadership success. Across the board the score for the MS students the four competencies were scored between 56% and 78%. Unlike their BSN counterparts, the MS students prioritized the importance of career planning. This is supported by their enrollment in a master’s program that provides specific nursing role preparation and opportunities for career advancement. It is expected that the concepts of accountability, ethics, and advocacy are recognized and valued by both BSN and MS students, as these concepts are foundational to the professionalism of nursing. The students in this study are all licensed Registered Nurses and most are employed, thus their responses reflect their experience with and dedication to responsible, safe, and ethical practice.
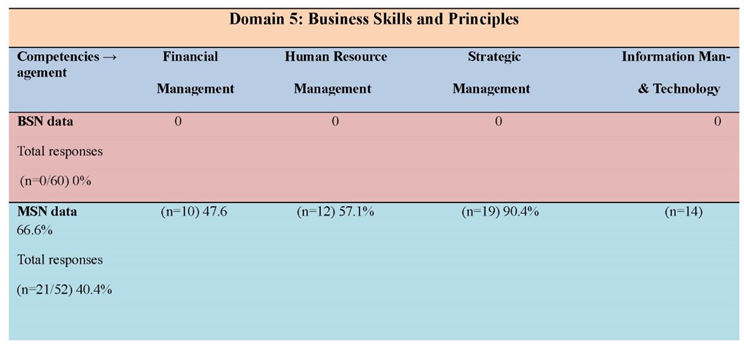
Domain 5: Business Skills and Principles
The four competencies that are associated with Domain 5: Business Skills and Principles are listed below in
Table 5 with the students’ response rates. Collectively, the BSN students offered no response tips related to business skills and principles.
The MS student response comments revolved around the strategic management process:
Engage all stakeholders, demonstrate the value of strategies to all stakeholders, make sure all stakeholders understand their role in the strategic plan.
Be flexible, be able to adapt and change, foresight and monitor market research.
Being adaptable to change, remaining informed on the internal and external environment, trying to be proactive and one step ahead. Transparency.
Table 5.
Domain 5: Business Skills and Principles.
Table 5.
Domain 5: Business Skills and Principles.
There are 39 behaviors identified by the AONL Competencies for Domain 5. A sample of these behaviors reflect connection to the students’ comments, and include the following: use business models for health care organizations and apply fundamental concepts of economics, create the operational objectives, goals and specific strategies required to achieve the strategic outcomes, identify marketing opportunities, conduct SWOT and Gap analyses, and analyze market data in relation to supply and demand. Throughout this analysis the data demonstrated that BSN students focus on unit-based activities; the data represents the knowledge and skills from one upper-level course. Despite some inclusion of business concepts in their course, none of the BSN students identified this knowledge as an important skill for leadership. The BSN students learn basics of capital and operational budget, balanced scorecard, strategic planning, SWOT analysis, and change theory. Their discussion includes an analysis of healthcare finance at the micro level, to include topics on productivity, cost containment, and impact on nursing. All nurses, whether managerial or staff, should have a basic understanding of finance and economic principles. Healthcare is a business; therefore, an understanding of finance is essential to better equip nurses to deal with cost challenges, allocate resources, staffing, and patient advocacy. Staff nurses' voices should be part of the unit budget process to ensure stakeholder buy-in.
MS in Nursing Administration students completed five leadership courses prior to this assignment: Leadership and Quality Improvement in Healthcare, Finance and Economics, Human Resource (HR) Management, and Strategic Management. These courses expanded their worldview of nursing leadership from manager to that of the nurse executive, consistent with the focus of their graduate program. Their comments (41%) demonstrate the importance they prioritized on the four competencies within this domain. The analysis indicates scores of 48%-90% with strategic management as the most important for leadership success. The strategic management process incorporates knowledge of finance, HR, and technology/information management. The MS students’ results validate the IOM (2010) report findings for the need for formal leadership education and demonstrate that nurses can recognize and prioritize business skills as foundational for leader success.
4. Discussion
Assessment and evaluation of leadership development is necessary to be tracked in nursing curricula. There are numerous worthy pedagogical strategies available for teaching application of leadership styles, attributes and behaviors, including simulation([
40], case studies [
41], group projects [
42], and reflection [
43]. Our nursing faculty value reflections as a method for students to increase their self-awareness, be creative, and synthesize their learning. In addition to teaching pedagogy, reflections are also recognized as an important skill for nurse executives, to increase self-care and professional growth, which may contribute to promoting caring cultures and resiliency [
43]. Leadership styles are an essential component of the theoretical foundation for the reflection assignments at both levels of our program. The BSN student responses are basic and correlate with unit leaders and managers. Creating a positive work culture with collaboration and effective communication is essential for quality patient care as well as staff retention. Starting the inclusion of leadership skills at the BSN level can provide the opportunity to spread strength and optimism, in order to attract and retain committed nurses [
44]. The BSN results validate the IOM report [
1] and National Academies of Science, Engineering, and Medicine [
2] report findings that formal leadership education is necessary to cultivate well-prepared, resourceful leaders. The IOM report reveals the underrepresentation of nurses on hospital boards, executive teams, and in key leadership roles where healthcare decision making occurs. Clinical nurses may be nurse leaders in a variety of capacities, and as such should be familiar with the business aspects of managing a nursing unit. Understanding profitability and financial viability is an integral part of operational and strategic planning to maintain and grow organizations. This provides direction for the need to expand BSN leadership curriculum content to include basic finance and economics topics, and design learning activities in order to provide students the practice skills needed to allocate resources efficiently and address budgeting challenges. Also, an ongoing mandatory financial education plan is needed for clinical and managerial nursing staff to understand cost challenges and the fundamental economic concepts that drive the strategies to maintain a financially sustainable organization.
The MS student leadership education is based on executive practice, a macro level focus (departmental and/or organizational). The students’ responses are sophisticated, demonstrate higher critical thought, a broader understanding of organizational issues, and are more reflective of executive leadership. To advance the way nursing is delivered and received, nursing leaders need to be willing to change the status quo and have the conversations to advance our future [
45]. Based on this study’s results, additional topics for master’s in leadership curricula may build upon the basic foundation of professionalism to include governance, advocacy, and succession planning. Some of our master’s students are already in administrative and executive positions, thus their responses reflect their own professional experiences, in addition to their didactic knowledge.
Communication, the how, what, when, and with whom, is the most common behavior identified by the majority of BSN and MS participants. Nursing education and professional development activities highlight the importance of effective communication skills and yet nurse leaders still struggle with this. Connecting with staff is a strategy for developing trust, boosting morale, and improving organizational performance. For example, leaders can schedule time to attend morning and change of shift reports to enhance connections with nursing staff. This provides an opportunity to recognize staff accomplishments and present organizational changes and gives the staff an opportunity to voice their views and be actively heard by leadership [
46]. In addition, it is suggested human resource management topics be included in BSN and MS curricula, appropriate to program level, to learn strategies to support positive organizational and nursing service goals to include staff satisfaction, workforce diversity, and the strength of collaborative partnerships.
Limitations of the study include the use of two different questions for the analysis, each pertinent to the level of the nursing program. Thus, variances in responses between the levels of students were expected from the start, however the data still identified common domains and competencies. In addition, the BSN students were in an RN-BSN program, thus post-licensure. Their prior work experiences in nursing roles may have influenced their responses, however while these results may not be fully generalizable to a generic BSN program, there are accepted standards of practice pertinent to all baccalaureate nursing education programs. The 2015 Nurse Executive Competencies [
36] document was used for this study because at the time of this research this document was the current one in circulation and used in our curriculum. These competencies were later revised to be the AONL Nurse Leader Core Competencies (2022) [
36,
47]. The updated competencies are similar, thus the data from this study remains valid and usable. Lastly, due to the anonymity of the data and retrospective design, there are no demographics of age, gender, race, ethnicity, or prior leadership experience, thus limiting generalizations related to demographics and diversity.
5. Conclusions
This study demonstrated results that are specific to micro, mezzo, and macro levels of leadership, yet showed common areas that students internalized and believe to be essential leadership competencies. The implications for leadership strategies and practices may be generalized to both baccalaureate and graduate-level programs to guide curriculum planning. This data provides an opportunity for nurse educators to assess their leadership course content and outcomes, and provide realistic, learning activities that are appropriate to the level of leadership in the workforce that is aligned with the degree program. Educators can assist and facilitate students to identify and evaluate creative and innovative leadership strategies from an educational and practice perspective to improve the work environment and enhance quality patient care [
37]. Further research is encouraged to assess students’ in-depth perceptions of their own leadership competencies, including areas of confidence, growth, and areas for improvement as they move forward to assume leadership roles in the healthcare setting. Studies can assess other pedagogies for leadership education, and can also be focused on refining leadership priorities that are being shaped by the Generation Y and Z nurses, who are the current and upcoming leaders in nursing.
Author Contributions
Conceptualization, B.A.D. and B.B.; methodology, B.A.D., B.B., and C.G.L.; validation, B.A.D. and B.B; formal analysis, B.A.D. and B.B, investigation, B.A.D. and B.B; resources, B.A.D. and B.B.; writing —original draft preparation: C.G.L., B.A.D., and B.B.; writing—review and editing, C.G.L.; B.A.D., and B.B., supervision, B.A.D..; project administration, B.A.D. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board of the State University of New York, Delhi College of Technology,(protocol code: 0086-001) and date of approval: 01/23/2023.
Informed Consent Statement
Informed consent was waived due to the data being retrospective and without having any impact on student records or connection to student names.
Data Availability Statement
Data supporting results can be requested from the corresponding authors (B.A.D. and B.B).
Acknowledgments
The authors acknowledge the assistance of Nancy Winters PhD, RN, FNP-BC, ANP for her review of the final draft of the manuscript.
Conflicts of Interest
The authors declare no conflicts of interest. The authors did not have any outside assistance with the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
Public Involvement Statement
No public involvement in any aspect of this research.
Guidelines and Standards Statement
This manuscript was drafted against The American Organization for Nursing Leadership (AONL) Nurse Executive Competencies (2015). Reporting Qualitative Research (SRQR) guideline for qualitative research. O'Brien BC, Harris IB, Beckman TJ, Reed DA, Cook DA. Standards for reporting qualitative research: a synthesis of recommendations. Academic Medicine, Vol. 89, No. 9 / Sept 2014 doi:10.1097/ACM.0000000000000388 389.
Use of Artificial Intelligence
AI or AI-assisted tools were not used in drafting any aspect of this manuscript.
Appendix A
Association of Nurse Leaders
Nurse Executive Competencies Domains and Competencies (2015).
References
- Institute of Medicine. The Future of Nursing: Leading Change, Advancing Health; The National Academies Press: Washington, DC, USA, 2011. [CrossRef]
- National Academies of Science, Engineering, and Medicine. Assessing progress on the Institute of Medicine Report:The Future of Nursing; The National Academies Press Washington, DC, USA, 2011. [CrossRef]
- Sfantou, D. F.; Laliotis, A.; Patelarou, A. E.; Sifaki-Pistolla, D.; Matalliotakis, M.; Patelarou, E. Importance of leadership style towards quality of care measures in healthcare settings: A systematic review. Healthcare 2017, 5(4), 73. [CrossRef]
- Ferreira, T.; Mesquita, R.; Melo, C.; Oliveira S.; Bucci, F.; Porcari, A.; Teles, G.; Altafini, J.; Dias, F.; Gasparino, R. The influence of nursing leadership styles on the outcomes of patients, professionals and institutions: An integrative review. J.Nurs.Manag 2022, 30(4), 936–953. [CrossRef]
- Lesandrini, J.; Lecleric, L. Fostering excellence in healthcare: The imperative for ethical leadership training for nurse leaders. Nurs Leader 2024, 22(3), 273- 278. [CrossRef]
- Alsadaan, N.; Salameh, B.;Reshia, F. A. A. E.; Alruwaili, M.; Ali, S. A. A.; Alruwali, A.N.;Hefnawy, G. R.;lshammari, M. S. S.; Alrumayh, A. G. R.; Alruwali, A., O.; Jones, L. K. Impact of nurse leaders’ behaviors on nursing staff performance: A systematic review of literature. Inquiry 2023, 60,1-16. [CrossRef]
- Labrague, L.L. Relationship between transformational leadership, adverse patient events, and nurse-assessed quality of care in emergency units: The mediating role of work satisfaction. Australas Emergency Care 2024, 27(1), 49-56. [CrossRef]
- Wong, C. A. Connecting nursing leadership and patient outcomes: State of the science. J. Nurs. Manag. 2015,23, 275-278. [CrossRef]
- Mabona, J.F.; van Rooyen, D.: ten Ham-Baloyi, W. Best practice recommendations for healthy work environments for nurses: An integrative literature review. Health SA 2022, 27, (1788). [CrossRef]
- Wong, C. A.; Cummings, G. G. The relationship between nursing leadership and patient outcomes: A systematic review. J. Nurs. Manag. 2013, 15, 508–521. [CrossRef]
- Ehrnrooth, M.; Barner, R. W.; Koveshnikov, A.; Törnroos, M. A new look at the relationships between transformational leadership and employee attitudes—Does a high-performance work system substitute and/or enhance these relationships? Hum. Resour. Manag. J. 2021, 60(3), 377–398. [CrossRef]
- Vidman, A.; Stromberg, A. Leadership for a healthy work environment – a question about who, what and how. LHS 2020, 34(1), 1-15. DOI:10.1108/LHS-06-2020-0041.
- Arnold, K.A. Transformational leadership and employee psychological well-being: A review and directions for future research. J.Occup.Health Psychol 2017, 22(3), 381-393. [CrossRef]
- Raso, R.; Fitzpatrick, J.; Masick, K. Clinical nurses' perceptions of authentic nurse leadership and healthy work environment. J Nurs. Adm 2020, 50(9), 489-494. [CrossRef]
- Raso, R.; Fitzpatrick, J. How leadership matters: Clinical nurses’ perceptions of leadership behaviors affecting their work environment. Nurs Manag 2021, 52(10), 16-22. [CrossRef]
- Pressley, C.; Garside, J. Safeguarding the retention of nurses: A systematic review on determinants of nurse's intentions to stay. Nurs Open 2023, 10(5). 2842-2858. [CrossRef]
- American Association of Colleges of Nursing. Fact sheet: Nursing shortage. 2024 https://https://www.aacnnursing.org/Portals/0/PDFs/Fact-Sheets/Nursing-Shortage-Factsheet.pdf.
- Kelly, L.A.; Gee, P.M.; Butler, R.J. Impact of nurse burnout on organizational and position turnover. Nurs Outlook 2021, 69(1),96-102. [CrossRef]
- Hand, M.W.; Alexander, C.; Lyman, B.; Parchment, J.; Joseph, M.L.; Chipps, E. Filling the knowledge gap for nurse leaders: Next steps following COVID-19. Nurs Leader 2021, 19(6), 616-621. [CrossRef]
-
2023: The state of workforce engagement. info.pressganey.com. https://info.pressganey.com/e-books-research/2023-state-of-workforce-engagement.
- Aydogdu, A.L. Perceptions of nursing students about leadership: A qualitative study. Nurse Educ Today 2023, 128. [CrossRef]
- Hallock, A. A case for leadership development in nursing practice. NNJ 2019, 46(3), 325-328.
- Bell, U. Healthcare leadership practices: How to conquer nursing shortage by improving engagement and retention; Higgins Publishing, Cedar Hill, Texas, USA. 2022. pp. 143-145.
- Kouzes, J.M.; Posner, Z. The leadership challenge, 7th ed.; John Wiley & Sons; Hoboken, New Jersey, USA, 2023. pp.193-196.
- Maritsa, E.; Goula, A.; Psychogios, A.; Pierrakos. (2022). Leadership development: Exploring relational leadership implications in healthcare Organizations. Int J Environ Public Health 2022, 19(23), 15971. [CrossRef]
- Collins, E.; Owen, P.; Digan, J.; Dunn, F. Applying transformational leadership in nursing practice. Nurs Stand 2020, 35(5), 59-66. [CrossRef]
- Iqbal, K.; Fatima, T.; Naveed, M. The impact of transformational leadership on nurses’ organizational commitment: A multiple mediation model. Eur J Investig Psychol Educ 2019, 10(1), 262-275. [CrossRef]
- Cahyadi, A.;Hendryadi, H.; Mappadang, A. Workplace and classroom incivility and learning engagement: The moderating role of locus of control. Int J Educ Integr 2021,17, 4. [CrossRef]
- Alilyyani, B. The effect of authentic leadership on nurses’ trust in managers and job performance: A cross-sectional study. Nurs Rep 2022, 12(4), 993-1003. [CrossRef]
- Reynolds, S.S. How to win friends and influence people- As a nurse leader. Nurs Leader 2021, 19(1), 87-89. [CrossRef]
- Juntitila, K.; Heikkita, A.; Heikkila, A.; Koivunen, M.; Lechtikunnas, T.; Mattila, E.; Merilainen, M.; Peltokoski, J.; Sneck, S.; Tervo-Heikkinen, T. The impact of leadership in the autonomy and engagement of nurses: A cross-sectional multicenter study among nurses outside the United States. JONA 2023, 53(1),19-26. [CrossRef]
- Lepez, C.O. Invisible challenges in healthcare leadership. Health Leadership and Quality of Life 2024, 2, 35. DOI: . [CrossRef]
- Abdelaliem, S. M F.; Zeid, M. A. G. A. The relationship between toxic leadership and organizational performance: The mediating effect of nurses’ silence. BMS Nurs 2023, 22(4). [CrossRef]
- Labrague, L.; Nwafor, C. E.; Tsaras, K. Influence of toxic and transformational leadership practices on nurses' job satisfaction, job stress, absenteeism and turnover intention: A cross-sectional study. J.Nurs.Manag 2020, 28(5), 1104-1113. [CrossRef]
- Hewison, A. Leading nursing beyond 2020 - the challenge and the opportunity. J.Nurs.Manag 2020, 28(4), 767-770. [CrossRef]
- American Organization for Nursing Leadership. The AONL Nurse Executive Competencies. 2015. AONL. https://https://www.aonl.org/sites/default/files/aone/nec.pdf.
- Morse, V.; Warshawsky. N. (2021). Nursing leader competencies: Today and tomorrow. Nurs Admin Quart 2021,45(1), 65-70. [CrossRef]
- Díaz-Agea, J. L.; Orcajada-Muñoz, I.; Leal-Costa, C.; Adánez-Martínez, M. G.; De Souza Oliveira, A. C.; Rojo-Rojo, A. How did the pandemic affect communication in clinical settings? A qualitative study with critical and emergency care nurses. Healthcare, 2022. 10(2), 373. [CrossRef]
- Coffey, A.M.; Powis, I.; Mullenix, A.; Rivero, V.; Evans, S.; Fatima, H.; Fleming, W. O.; Lich, K. H.; Orton, S.; Cilenti, D.; Margolis. L. Enhancing Title V workforce capacity to address complex challenges: Impact of the national maternal and child health workforce development center. Maternal & Child Health Journal 2022, 26, 51–59. [CrossRef]
- Labrague, L. J. Use of simulation in teaching nursing leadership and management course. SQUMJ 2021, 21(3), 344-353. [CrossRef]
- Englund, H. Using unfolding case studies to develop critical thinking skills in baccalaureate nursing students: A pilot study. Nurs Educ Today 2020, 93. [CrossRef]
- Lee, C.J.; Ahonen, K.; Navarette, E.; Frisch, K. Successful student group projects: Perspectives and strategies. Teaching and Learning in Nursing 2015, 10(4), 186-191. [CrossRef]
- Prestia, A.S. Reflection: A powerful leadership tool. Nurse Leader 2019, 17(5), 465-467. [CrossRef]
- Kerfoot, K.M. Leadership and the great reset: Rethinking possibilities for the future of nursing. Nurs Econ 2022,40(1), 38-41.
- Kurosaka, A. T. Challenging our current norms to succeed. NNJ 2022,49(5), 395. [CrossRef]
- Blake, P. G.; Bacon, C. T. Structured rounding to improve staff nurse satisfaction with leadership. Nurs Leader 2020, 18(5). [CrossRef]
- American Organization for Nursing Leadership. The AONL Nurse Leader Core Competencies. 2022, Association of Nurse Leaders. https://www.aonl.org/system/files/media/file/2022/10/AONL_CCDocument_101822_PRO.pd.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).