Submitted:
13 August 2024
Posted:
14 August 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Sphingolipids: Fundamentals of Biology and Metabolism
2.1. Sphingolipid Biosynthesis, Metabolism, and Catabolism
2.1.1. Sphingoid Bases
2.1.2. Ceramides
2.1.3. Sphingomyelin
2.1.4. Glycosphingolipids
2.1.5. Ceramide-1-Phosphate
2.1.6. Sphingosine-1-Phosphate
2.2. Physiological Roles of Sphingolipids
2.2.1. Sphingoid Bases
2.2.2. Ceramides
2.2.3. Sphingomyelin
2.2.4. Glycosphingolipids
2.2.5. Ceramide-1-Phosphate
2.2.6. Sphingosine-1-Phosphate
3. Sphingolipids and Vascular Disease
3.1. Sphingolipids and Atherosclerosis
3.2. Sphingolipids and Aneurysmal Disease
3.3. Sphingolipids and Stroke
4. Sphingolipids and Myocardial Disease
4.1. Sphingolipids and Heart Failure
4.2. Sphingolipids and Atrial Fibrillation
5. Sphingolipids and Metabolic Disease
6. Sphingolipids as a Therapeutic Target
6.1. Weight loss and Exercise
6.2. Dietary Interventions
6.2.1. Oleic Acid
6.2.2. Milk Polar Lipids
6.2.3. Ginseng
6.2.4. Low-Fat and Low-Carbohydrate Diet
6.3. Pharmacological Treatments
6.3.1. Fingolimod
6.3.2. Statins
6.3.3. Glucagon-like Peptide-1 Receptor (GLP-1R) Agonists
6.3.4. Sodium Glucose Transporter 2 (SGLT-2) Inhibitors
6.3.5. Amitriptyline
6.3.6. Desipramine
6.3.7. N-acetylcysteine
6.3.8. SPT Inhibitors
6.3.9. SphK inhibitors
6.3.10. UDP-Glucose Ceramide Glucosyltransferase (UGCG) Inhibitors
6.3.11. Dihydroceramide Desaturase Inhibitors
7. Conclusion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Vaduganathan M, Mensah GA, Turco JV, Fuster V, Roth GA. The Global Burden of Cardiovascular Diseases and Risk: A Compass for Future Health. Journal of the American College of Cardiology. 2022, 80, 2361–2371. [CrossRef]
- Sarwar N, Gao P, Seshasai SRK, Gobin R, Kaptoge S, Di Angelantonio E, et al. Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: a collaborative meta-analysis of 102 prospective studies. Lancet (London, England). 2010, 375, 2215–2222. [CrossRef]
- Choi RH, Tatum SM, Symons JD, Summers SA, Holland WL. Ceramides and other sphingolipids as drivers of cardiovascular disease. Nature Reviews Cardiology. 2021, 18, 701–711, Available online: https://www.nature.com/articles/s41569-021-00536-1 (accessed on 27 December 2023). [CrossRef]
- Merrill AH, Schmelz EM, Dillehay DL, Spiegel S, Shayman JA, Schroeder JJ, et al. Sphingolipids--the enigmatic lipid class: biochemistry, physiology, and pathophysiology. Toxicology and Applied Pharmacology. 1997, 142, 208–225. [CrossRef]
- Hannun YA, Obeid LM. Sphingolipids and their metabolism in physiology and disease. Nature Reviews. Molecular Cell Biology. 2018, 19, 175–191. [CrossRef]
- Merrill, AH. Lipids Carbohydrates Membranes and Membrane Proteins - Sphingolipid Biosynthesis. Encyclopedia of Biological Chemistry. 2nd ed. Atlanta, GA, USA: Elsevier; 2013. pp. 281–286.
- Gault CR, Obeid LM, Hannun YA. An overview of sphingolipid metabolism: from synthesis to breakdown. Advances in experimental medicine and biology. 2010. 6881-23. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3069696/ (accessed on 27 December 2023).
- Karlsson, K. On the chemistry and occurrence of sphingolipid long-chain bases - ScienceDirect. Chemistry and Physics of Lipids. 1970, 5, 6–43, Available online: https://www.sciencedirect.com/science/article/pii/0009308470900083 (accessed on 27 December 2023). [Google Scholar] [CrossRef]
- Maccioni HJF, Quiroga R, Ferrari ML. Cellular and molecular biology of glycosphingolipid glycosylation. Journal of Neurochemistry. 2011, 117, 589–602. [CrossRef]
- Canals D, Salamone S, Hannun YA. Visualizing Bioactive Ceramides. Chemistry and physics of lipids. 2018, 216142-151. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6233321/ (accessed on 27 December 2023). [CrossRef]
- Quinville BM, Deschenes NM, Ryckman AE, Walia JS. A Comprehensive Review: Sphingolipid Metabolism and Implications of Disruption in Sphingolipid Homeostasis. International Journal of Molecular Sciences. 2021, 22, 5793. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8198874/ (accessed on 27 December 2023). [CrossRef]
- Zheng W, Kollmeyer J, Symolon H, Momin A, Munter E, Wang E, et al. Ceramides and other bioactive sphingolipid backbones in health and disease: lipidomic analysis, metabolism and roles in membrane structure, dynamics, signaling and autophagy. Biochimica Et Biophysica Acta. 2006, 1758, 1864–1884. [CrossRef]
- Pruett ST, Bushnev A, Hagedorn K, Adiga M, Haynes CA, Sullards MC, et al. Thematic Review Series: Sphingolipids. Biodiversity of sphingoid bases (“sphingosines”) and related amino alcohols. Journal of Lipid Research. 2008, 49, 1621–1639, Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2444003/ (accessed on 27 December 2023). [CrossRef]
- Merrill AH, Williams RD. Utilization of different fatty acyl-CoA thioesters by serine palmitoyltransferase from rat brain. Journal of Lipid Research. 1984, 25, 185–188.
- Farwanah H, Pierstorff B, Schmelzer CEH, Raith K, Neubert RHH, Kolter T, et al. Separation and mass spectrometric characterization of covalently bound skin ceramides using LC/APCI-MS and Nano-ESI-MS/MS. Journal of Chromatography. B, Analytical Technologies in the Biomedical and Life Sciences. 2007;852(1-2): 562-570. [CrossRef]
- Liu Q, Chan AKN, Chang W, Yang L, Pokharel SP, Miyashita K, et al. 3-Ketodihydrosphingosine reductase maintains ER homeostasis and unfolded protein response in leukemia. Leukemia. 2022, 36, 100–110, Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8732298/ (accessed on 27 December 2023). [CrossRef]
- Stith JL, Velazquez FN, Obeid LM. Advances in determining signaling mechanisms of ceramide and role in disease. Journal of Lipid Research. 2019, 60, 913–918, Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6495170/ (accessed on 28 December 2023). [CrossRef]
- Hannun YA, Obeid LM. Principles of bioactive lipid signalling: lessons from sphingolipids. Nature Reviews. Molecular Cell Biology. 2008, 9, 139–150. [CrossRef]
- Bikman BT, Summers SA. Ceramides as modulators of cellular and whole-body metabolism. The Journal of Clinical Investigation. 2011, 121, 4222–4230, Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3204836/ (accessed on 28 December 2023). [CrossRef]
- Yamaji T, Hanada K. Sphingolipid metabolism and interorganellar transport: localization of sphingolipid enzymes and lipid transfer proteins. Traffic (Copenhagen, Denmark). 2015, 16, 101–122. [CrossRef]
- Wegner M, Schiffmann S, Parnham MJ, Geisslinger G, Grösch S. The enigma of ceramide synthase regulation in mammalian cells. Progress in Lipid Research. 2016, 6393–119. [CrossRef]
- Michel C, van Echten-Deckert G, Rother J, Sandhoff K, Wang E, Merrill AH. Characterization of ceramide synthesis. A dihydroceramide desaturase introduces the 4,5-trans-double bond of sphingosine at the level of dihydroceramide. The Journal of Biological Chemistry. 1997, 272, 22432–22437. [CrossRef]
- Hanada, K. Co-evolution of sphingomyelin and the ceramide transport protein CERT. Biochimica Et Biophysica Acta. 2014, 1841, 704–719. [Google Scholar] [CrossRef]
- Merrill, AH. Sphingolipid and Glycosphingolipid Metabolic Pathways in the Era of Sphingolipidomics. Chemical Reviews. 2011, 111, 6387–6422, Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3191729/ (accessed on 27 December 2023). [Google Scholar] [CrossRef]
- Shayman JA, Abe A. Sphingolipid Catabolism. In: Lennarz WJ, Lane D. (eds.) Encyclopedia of Biological Chemistry. 2nd ed. Elsevier; 2013. pp. 287–292.
- Zeidan YH, Hannun YA. The acid sphingomyelinase/ceramide pathway: biomedical significance and mechanisms of regulation. Current Molecular Medicine. 2010, 10, 454–466. [CrossRef]
- Boer DEC, van Smeden J, Bouwstra JA, Aerts JMFG. Glucocerebrosidase: Functions in and Beyond the Lysosome. Journal of Clinical Medicine. 2020, 9, 736. [CrossRef]
- Kitatani K, Idkowiak-Baldys J, Hannun YA. The sphingolipid salvage pathway in ceramide metabolism and signaling. Cellular Signalling. 2008, 20, 1010–1018. [CrossRef]
- Villani M, Subathra M, Im Y, Choi Y, Signorelli P, Del Poeta M, et al. Sphingomyelin synthases regulate production of diacylglycerol at the Golgi. The Biochemical Journal. 2008, 414, 31–41. [CrossRef]
- Huitema K, van den Dikkenberg J, Brouwers JFHM, Holthuis JCM. Identification of a family of animal sphingomyelin synthases. The EMBO journal. 2004, 23, 33–44. [CrossRef]
- Merrill AH, Jones DD. An update of the enzymology and regulation of sphingomyelin metabolism. Biochimica Et Biophysica Acta. 1990, 1044, 1–12. [CrossRef]
- Varki A, Cummings R, Esko J, Freeze H, Hart G, Marth J. Chapter 9: Glycosphingolipids. Essentials of Glycobiology. Cold Spring Harbor (NY), United States: Cold Spring Harbor Laboratory Press; 1999.
- D'Angelo G, Polishchuk E, Di Tullio G, Santoro M, Di Campli A, Godi A, et al. Glycosphingolipid synthesis requires FAPP2 transfer of glucosylceramide. Nature. 2007, 449, 62–67. [CrossRef]
- Sprong H, Kruithof B, Leijendekker R, Slot JW, van Meer G, van der Sluijs P. UDP-galactose:ceramide galactosyltransferase is a class I integral membrane protein of the endoplasmic reticulum. The Journal of Biological Chemistry. 1998, 273, 25880–25888. [CrossRef]
- Sugiura M, Kono K, Liu H, Shimizugawa T, Minekura H, Spiegel S, et al. Ceramide kinase, a novel lipid kinase. Molecular cloning and functional characterization. The Journal of Biological Chemistry. 2002, 277, 23294–23300. [CrossRef]
- Simanshu DK, Kamlekar RK, Wijesinghe DS, Zou X, Zhai X, Mishra SK, et al. Non-vesicular trafficking by a ceramide-1-phosphate transfer protein regulates eicosanoids. Nature. 2013, 500, 463–467. [CrossRef]
- Gomez-Larrauri A, Ouro A, Trueba M, Gomez-Muñoz A. Regulation of cell growth, survival and migration by ceramide 1-phosphate - implications in lung cancer progression and inflammation. Cellular Signalling. 2021;83109980. [CrossRef]
- Shinghal R, Scheller RH, Bajjalieh SM. Ceramide 1-phosphate phosphatase activity in brain. Journal of Neurochemistry. 1993, 61, 2279–2285. [CrossRef]
- Waggoner DW, Gómez-Muñoz A, Dewald J, Brindley DN. Phosphatidate phosphohydrolase catalyzes the hydrolysis of ceramide 1-phosphate, lysophosphatidate, and sphingosine 1-phosphate. The Journal of Biological Chemistry. 1996, 271, 16506–16509. [CrossRef]
- Yatomi Y, Ozaki Y, Ohmori T, Igarashi Y. Sphingosine 1-phosphate: synthesis and release. Prostaglandins & Other Lipid Mediators. 2001, 64, 107–122. [CrossRef]
- Spiegel, S. Sphingosine 1-phosphate: a prototype of a new class of second messengers. Journal of Leukocyte Biology. 1999, 65, 341–344. [Google Scholar] [CrossRef]
- Jiang Z, Delaney TL, Zanin MP, Haberberger RV, Pitson SM, Huang J, et al. Extracellular and intracellular sphingosine-1-phosphate distinctly regulates exocytosis in chromaffin cells. Journal of Neurochemistry. 2019, 149, 729–746. [CrossRef]
- Strub GM, Maceyka M, Hait NC, Milstien S, Spiegel S. Extracellular and intracellular actions of sphingosine-1-phosphate. Advances in Experimental Medicine and Biology. 2010, 688, 141–155. [CrossRef]
- Venkataraman K, Thangada S, Michaud J, Oo ML, Ai Y, Lee Y, et al. Extracellular export of sphingosine kinase-1a contributes to the vascular S1P gradient. The Biochemical Journal. 2006, 397, 461–471. [CrossRef]
- Yatomi Y, Ozaki Y, Ohmori T, Igarashi Y. Sphingosine 1-phosphate: synthesis and release. Prostaglandins & Other Lipid Mediators. 2001, 64, 107–122. [CrossRef]
- Kikkawa U, Takai Y, Minakuchi R, Inohara S, Nishizuka Y. Calcium-activated, phospholipid-dependent protein kinase from rat brain. Subcellular distribution, purification, and properties. The Journal of Biological Chemistry. 1982, 257, 13341–13348.
- Brindley DN, Xu J, Jasinska R, Waggoner DW. Analysis of ceramide 1-phosphate and sphingosine-1-phosphate phosphatase activities. Methods in Enzymology. 2000, 311233-244. [CrossRef]
- Ikeda M, Kihara A, Igarashi Y. Sphingosine-1-phosphate lyase SPL is an endoplasmic reticulum-resident, integral membrane protein with the pyridoxal 5'-phosphate binding domain exposed to the cytosol. Biochemical and Biophysical Research Communications. 2004, 325, 338–343. [CrossRef]
- Carreira AC, Santos TC, Lone MA, Zupančič E, Lloyd-Evans E, de Almeida RFM, et al. Mammalian sphingoid bases: Biophysical, physiological and pathological properties. Progress in Lipid Research. 2019, 100995. [CrossRef]
- Kõiv A, Mustonen P, Kinnunen PK. Influence of sphingosine on the thermal phase behaviour of neutral and acidic phospholipid liposomes. Chemistry and Physics of Lipids. 1993, 66, 123–134. [CrossRef]
- Zheng W, Kollmeyer J, Symolon H, Momin A, Munter E, Wang E, et al. Ceramides and other bioactive sphingolipid backbones in health and disease: lipidomic analysis, metabolism and roles in membrane structure, dynamics, signaling and autophagy. Biochimica Et Biophysica Acta. 2006, 1758, 1864–1884. [CrossRef]
- Carreira AC, de Almeida RFM, Silva LC. Development of lysosome-mimicking vesicles to study the effect of abnormal accumulation of sphingosine on membrane properties. Scientific Reports. 2017, 7, 3949. [CrossRef]
- Lima S, Milstien S, Spiegel S. Sphingosine and Sphingosine Kinase 1 Involvement in Endocytic Membrane Trafficking. The Journal of Biological Chemistry. 2017, 292, 3074–3088. [CrossRef]
- Hannun YA, Bell RM. Lysosphingolipids inhibit protein kinase C: implications for the sphingolipidoses. Science (New York, N.Y.). 1987, 235, 670–674. [CrossRef]
- Miao L, Pan D, Shi J, Du J, Chen P, Gao J, et al. Role and Mechanism of PKC-δ for Cardiovascular Disease: Current Status and Perspective. Frontiers in Cardiovascular Medicine. 2022, 9816369. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8885814/ (accessed on 4 January 2024). [CrossRef]
- Zeidan YH, Hannun YA. Activation of acid sphingomyelinase by protein kinase Cdelta-mediated phosphorylation. The Journal of Biological Chemistry. 2007, 282, 11549–11561. [CrossRef]
- Arnold RS, Newton AC. Inhibition of the insulin receptor tyrosine kinase by sphingosine. Biochemistry. 1991, 30, 7747–7754. [CrossRef]
- Aji G, Huang Y, Ng ML, Wang W, Lan T, Li M, et al. Regulation of hepatic insulin signaling and glucose homeostasis by sphingosine kinase 2. Proceedings of the National Academy of Sciences of the United States of America. 2020, 117, 24434–24442. [CrossRef]
- Akoumianakis I, Badi I, Douglas G, Chuaiphichai S, Herdman L, Akawi N, et al. Insulin-induced vascular redox dysregulation in human atherosclerosis is ameliorated by dipeptidyl peptidase 4 inhibition. Science Translational Medicine. 2020, 12, eaav8824. [CrossRef]
- Woodcock, J. Sphingosine and ceramide signalling in apoptosis. IUBMB life. 2006, 58, 462–466. [Google Scholar] [CrossRef]
- Summers SA, Garza LA, Zhou H, Birnbaum MJ. Regulation of insulin-stimulated glucose transporter GLUT4 translocation and Akt kinase activity by ceramide. Molecular and Cellular Biology. 1998, 18, 5457–5464. [CrossRef]
- Guenther GG, Peralta ER, Rosales KR, Wong SY, Siskind LJ, Edinger AL. Ceramide starves cells to death by downregulating nutrient transporter proteins. Proceedings of the National Academy of Sciences of the United States of America. 2008, 105, 17402–17407. [CrossRef]
- Siskind, LJ. Mitochondrial Ceramide and the Induction of Apoptosis. Journal of bioenergetics and biomembranes. 2005, 37, 143–153, Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2246044/ (accessed on 5 January 2024). [Google Scholar] [CrossRef]
- Vasudevan KM, Garraway LA. AKT signaling in physiology and disease. Current Topics in Microbiology and Immunology. 2010, 347105–133. [CrossRef]
- Stoica BA, Movsesyan VA, Lea PM, Faden AI. Ceramide-induced neuronal apoptosis is associated with dephosphorylation of Akt, BAD, FKHR, GSK-3beta, and induction of the mitochondrial-dependent intrinsic caspase pathway. Molecular and Cellular Neurosciences. 2003, 22, 365–382. [CrossRef]
- Ruvolo PP, Deng X, Ito T, Carr BK, May WS. Ceramide induces Bcl2 dephosphorylation via a mechanism involving mitochondrial PP2A. The Journal of Biological Chemistry. 1999, 274, 20296–20300. [CrossRef]
- Young MM, Kester M, Wang H. Sphingolipids: regulators of crosstalk between apoptosis and autophagy. Journal of Lipid Research. 2013, 54, 5–19. [CrossRef]
- Siddique MM, Li Y, Chaurasia B, Kaddai VA, Summers SA. Dihydroceramides: From Bit Players to Lead Actors. The Journal of Biological Chemistry. 2015, 290, 15371–15379, Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4505450/ (accessed on 5 January 2024). [CrossRef]
- Casasampere M, Ordóñez YF, Casas J, Fabrias G. Dihydroceramide desaturase inhibitors induce autophagy via dihydroceramide-dependent and independent mechanisms. Biochimica Et Biophysica Acta. General Subjects. 2017, 1861, 264–275. [CrossRef]
- Bielawska A, Crane HM, Liotta D, Obeid LM, Hannun YA. Selectivity of ceramide-mediated biology. Lack of activity of erythro-dihydroceramide. The Journal of Biological Chemistry. 1993, 268, 26226–26232.
- Siskind LJ, Colombini M. The lipids C2- and C16-ceramide form large stable channels. Implications for apoptosis. The Journal of Biological Chemistry. 2000, 275, 38640–38644. [CrossRef]
- Gagliostro V, Casas J, Caretti A, Abad JL, Tagliavacca L, Ghidoni R, et al. Dihydroceramide delays cell cycle G1/S transition via activation of ER stress and induction of autophagy. The International Journal of Biochemistry & Cell Biology. 2012, 44, 2135–2143. [CrossRef]
- Coderch L, López O, de la Maza A, Parra JL. Ceramides and skin function. American Journal of Clinical Dermatology. 2003, 4, 107–129. [CrossRef]
- Hachem, JP. The two compartment model of the stratum corneum: biochemical aspects and pathophysiological implications. Verhandelingen - Koninklijke Academie Voor Geneeskunde Van Belgie. 2006, 68, 287–317. [Google Scholar] [PubMed]
- Jennemann R, Sandhoff R, Langbein L, Kaden S, Rothermel U, Gallala H, et al. Integrity and barrier function of the epidermis critically depend on glucosylceramide synthesis. The Journal of Biological Chemistry. 2007, 282, 3083–3094. [CrossRef]
- Holleran WM, Man MQ, Gao WN, Menon GK, Elias PM, Feingold KR. Sphingolipids are required for mammalian epidermal barrier function. Inhibition of sphingolipid synthesis delays barrier recovery after acute perturbation. The Journal of Clinical Investigation. 1991, 88, 1338–1345. [CrossRef]
- Taniguchi M, Okazaki T. The role of sphingomyelin and sphingomyelin synthases in cell death, proliferation and migration-from cell and animal models to human disorders. Biochimica Et Biophysica Acta. 2014, 1841, 692–703. [CrossRef]
- Goñi, FM. Sphingomyelin: What is it good for? Biochemical and Biophysical Research Communications. 2022, 63323–25. [Google Scholar] [CrossRef] [PubMed]
- Subathra M, Qureshi A, Luberto C. Sphingomyelin synthases regulate protein trafficking and secretion. PloS One. 2011, 6, e23644. [CrossRef]
- Romanenko EB, Alessenko AV, Vanyushin BF. Effect of sphingomyelin and antioxidants on the in vitro and in vivo DNA methylation. Biochemistry and Molecular Biology International. 1995, 35, 87–94.
- Albi E, Lazzarini A, Lazzarini R, Floridi A, Damaskopoulou E, Curcio F, et al. Nuclear Lipid Microdomain as Place of Interaction between Sphingomyelin and DNA during Liver Regeneration. International Journal of Molecular Sciences. 2013, 14, 6529–6541, Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3645652/ (accessed on 7 January 2024). [CrossRef]
- Tafesse FG, Huitema K, Hermansson M, van der Poel S, van den Dikkenberg J, Uphoff A, et al. Both sphingomyelin synthases SMS1 and SMS2 are required for sphingomyelin homeostasis and growth in human HeLa cells. The Journal of Biological Chemistry. 2007, 282, 17537–17547. [CrossRef]
- Hidari KIPJ n, Ichikawa S, Fujita T, Sakiyama H, Hirabayashi Y. Complete removal of sphingolipids from the plasma membrane disrupts cell to substratum adhesion of mouse melanoma cells. The Journal of Biological Chemistry. 1996, 271, 14636–14641. [CrossRef]
- Poitelon Y, Kopec AM, Belin S. Myelin Fat Facts: An Overview of Lipids and Fatty Acid Metabolism. Cells. 2020, 9, 812, Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7226731/ (accessed on 7 January 2024). [CrossRef]
- Thompson TE, Tillack TW. Organization of glycosphingolipids in bilayers and plasma membranes of mammalian cells. Annual Review of Biophysics and Biophysical Chemistry. 1985;14361-386. [CrossRef]
- Skotland T, Sandvig K. The role of PS 18:0/18:1 in membrane function. Nature Communications. 2019, 10, 2752. [CrossRef]
- Sillence DJ, Puri V, Marks DL, Butters TD, Dwek RA, Pagano RE, et al. Glucosylceramide modulates membrane traffic along the endocytic pathway. Journal of Lipid Research. 2002, 43, 1837–1845. [CrossRef]
- Aida J, Higuchi S, Hasegawa Y, Nagano-Ito M, Hirabayashi Y, Banba A, et al. Up-regulation of ceramide glucosyltransferase during the differentiation of U937 cells. Journal of Biochemistry. 2011, 150, 303–310. [CrossRef]
- Lalazar G, Ya'acov AB, Livovsky DM, El Haj M, Pappo O, Preston S, et al. β-Glycoglycosphingolipid-Induced Alterations of the STAT Signaling Pathways Are Dependent on CD1d and the Lipid Raft Protein Flotillin-2. The American Journal of Pathology. 2009, 174, 1390–1399, Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2671370/ (accessed on 6 January 2024). [CrossRef]
- Zigmond E, Preston S, Pappo O, Lalazar G, Margalit M, Shalev Z, et al. Beta-glucosylceramide: a novel method for enhancement of natural killer T lymphoycte plasticity in murine models of immune-mediated disorders. Gut. 2007, 56, 82–89. [CrossRef]
- Deguchi H, Fernández JA, Pabinger I, Heit JA, Griffin JH. Plasma glucosylceramide deficiency as potential risk factor for venous thrombosis and modulator of anticoagulant protein C pathway. Blood. 2001, 97, 1907–1914. [CrossRef]
- Lavie Y, Cao H, Bursten SL, Giuliano AE, Cabot MC. Accumulation of glucosylceramides in multidrug-resistant cancer cells. The Journal of Biological Chemistry. 1996, 271, 19530–19536. [CrossRef]
- Messner MC, Cabot MC. Glucosylceramide in Humans. Sphingolipids as Signaling and Regulatory Molecules. New York: Springer New York; 2011. pp. 156–164.
- Liu Y, Han TY, Yu JY, Bitterman A, Le A, Giuliano AE, et al. Oligonucleotides blocking glucosylceramide synthase expression selectively reverse drug resistance in cancer cells. Journal of Lipid Research. 2004, 45, 933–940. [CrossRef]
- Chavez JA, Siddique MM, Wang ST, Ching J, Shayman JA, Summers SA. Ceramides and glucosylceramides are independent antagonists of insulin signaling. The Journal of Biological Chemistry. 2014, 289, 723–734. [CrossRef]
- Jackman N, Ishii A, Bansal R. Oligodendrocyte development and myelin biogenesis: parsing out the roles of glycosphingolipids. Physiology (Bethesda, Md.). 2009, 24, 290–297. [CrossRef]
- Boggs, JM. Role of galactosylceramide and sulfatide in oligodendrocytes and CNS myelin: formation of a glycosynapse. Advances in Neurobiology. 2014, 9, 263–291. [Google Scholar] [CrossRef]
- Van Kaer, L. alpha-Galactosylceramide therapy for autoimmune diseases: prospects and obstacles. Nature Reviews. Immunology. 2005, 5, 31–42. [Google Scholar] [CrossRef] [PubMed]
- Hoeferlin LA, Wijesinghe DS, Chalfant CE. The Role of Ceramide-1-Phosphate in Biological Functions. Handbook of experimental pharmacology. 2013, 215, 153–166, Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5598467/ (accessed on 8 January 2024). [CrossRef]
- Gómez-Muñoz A, Kong JY, Salh B, Steinbrecher UP. Ceramide-1-phosphate blocks apoptosis through inhibition of acid sphingomyelinase in macrophages. Journal of Lipid Research. 2004, 45, 99–105. [CrossRef]
- Gomez-Muñoz A, Frago LM, Alvarez L, Varela-Nieto I. Stimulation of DNA synthesis by natural ceramide 1-phosphate. The Biochemical Journal. 1997, 325 Pt 2, 435-440. [CrossRef]
- Gangoiti P, Granado MH, Wang SW, Kong JY, Steinbrecher UP, Gómez-Muñoz A. Ceramide 1-phosphate stimulates macrophage proliferation through activation of the PI3-kinase/PKB, JNK and ERK1/2 pathways. Cellular Signalling. 2008, 20, 726–736. [CrossRef]
- Granado MH, Gangoiti P, Ouro A, Arana L, González M, Trueba M, et al. Ceramide 1-phosphate (C1P) promotes cell migration Involvement of a specific C1P receptor. Cellular Signalling. 2009, 21, 405–412. [CrossRef]
- Pettus BJ, Bielawska A, Subramanian P, Wijesinghe DS, Maceyka M, Leslie CC, et al. Ceramide 1-phosphate is a direct activator of cytosolic phospholipase A2. The Journal of Biological Chemistry. 2004, 279, 11320–11326. [CrossRef]
- Lamour NF, Wijesinghe DS, Mietla JA, Ward KE, Stahelin RV, Chalfant CE. Ceramide kinase regulates the production of tumor necrosis factor α (TNFα) via inhibition of TNFα-converting enzyme. The Journal of Biological Chemistry. 2011, 286, 42808–42817. [CrossRef]
- Rutherford C, Childs S, Ohotski J, McGlynn L, Riddick M, MacFarlane S, et al. Regulation of cell survival by sphingosine-1-phosphate receptor S1P1 via reciprocal ERK-dependent suppression of Bim and PI-3-kinase/protein kinase C-mediated upregulation of Mcl-1. Cell Death & Disease. 2013, 4, e927–e927, Available online: https://www.nature.com/articles/cddis2013455 (accessed on 10 January 2024). [CrossRef]
- Xiao S, Peng K, Li C, Long Y, Yu Q. The role of sphingosine-1-phosphate in autophagy and related disorders. Cell Death Discovery. 2023, 9, 1–14, Available online: https://www.nature.com/articles/s41420-023-01681-x (accessed on 10 January 2024). [CrossRef]
- Cyster JG, Schwab SR. Sphingosine-1-phosphate and lymphocyte egress from lymphoid organs. Annual Review of Immunology. 2012, 30, 69–94. [CrossRef]
- Hla T, Dannenberg AJ. Sphingolipid signaling in metabolic disorders. Cell metabolism. 2012, 16, 420–434, Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3466368/ (accessed on 17 October 2023). [CrossRef]
- Blaho VA, Hla T. Regulation of mammalian physiology, development, and disease by the sphingosine 1-phosphate and lysophosphatidic acid receptors. Chemical reviews. 2011, 111, 6299–6320, Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3216694/ (accessed on 17 October 2023). [CrossRef]
- Cyster JG, Schwab SR. Sphingosine-1-phosphate and lymphocyte egress from lymphoid organs. Annual Review of Immunology. 2012;3069-94. [CrossRef]
- Tiper IV, East JE, Subrahmanyam PB, Webb TJ. Sphingosine 1-phosphate signaling impacts lymphocyte migration, inflammation and infection. Pathogens and Disease. 2016, 74, ftw063, Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5985508/ (accessed on 8 January 2024). [CrossRef]
- Pappu R, Schwab SR, Cornelissen I, Pereira JP, Regard JB, Xu Y, et al. Promotion of lymphocyte egress into blood and lymph by distinct sources of sphingosine-1-phosphate. Science (New York, N.Y.). 2007, 316, 295–298. [CrossRef]
- Schwab SR, Pereira JP, Matloubian M, Xu Y, Huang Y, Cyster JG. Lymphocyte sequestration through S1P lyase inhibition and disruption of S1P gradients. Science (New York, N.Y.). 2005, 309, 1735–1739. [CrossRef]
- Murata N, Sato K, Kon J, Tomura H, Yanagita M, Kuwabara A, et al. Interaction of sphingosine 1-phosphate with plasma components, including lipoproteins, regulates the lipid receptor-mediated actions. The Biochemical Journal. 2000, 352 Pt 3, 809-815.
- Gaengel K, Niaudet C, Hagikura K, Laviña B, Muhl L, Hofmann JJ, et al. The sphingosine-1-phosphate receptor S1PR1 restricts sprouting angiogenesis by regulating the interplay between VE-cadherin and VEGFR2. Developmental Cell. 2012, 23, 587–599. [CrossRef]
- Ragunathrao VAB, Anwar M, Akhter MZ, Chavez A, Mao DY, Natarajan V, et al. Sphingosine-1-Phosphate Receptor 1 Activity Promotes Tumor Growth by Amplifying VEGF-VEGFR2 Angiogenic Signaling. Cell reports. 2019, 29, 3472–3487, Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6927555/ (accessed on 23 January 2024). [CrossRef]
- LaMontagne K, Littlewood-Evans A, Schnell C, O'Reilly T, Wyder L, Sanchez T, et al. Antagonism of sphingosine-1-phosphate receptors by FTY720 inhibits angiogenesis and tumor vascularization. Cancer Research. 2006, 66, 221–231. [CrossRef]
- Sarkisyan G, Gay LJ, Nguyen N, Felding BH, Rosen H. Host endothelial S1PR1 regulation of vascular permeability modulates tumor growth. American Journal of Physiology - Cell Physiology. 2014, 307, C14–C24, Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4080184/ (accessed on 23 January 2024). [CrossRef]
- Jozefczuk E, Guzik TJ, Siedlinski M. Significance of sphingosine-1-phosphate in cardiovascular physiology and pathology. Pharmacological Research. 2020;156104793. [CrossRef]
- Lee MJ, Thangada S, Claffey KP, Ancellin N, Liu CH, Kluk M, et al. Vascular endothelial cell adherens junction assembly and morphogenesis induced by sphingosine-1-phosphate. Cell. 1999, 99, 301–312. [CrossRef]
- Zeng Y, Adamson RH, Curry FE, Tarbell JM. Sphingosine-1-phosphate protects endothelial glycocalyx by inhibiting syndecan-1 shedding. American Journal of Physiology. Heart and Circulatory Physiology. 2014, 306, 363. [CrossRef]
- Camerer E, Regard JB, Cornelissen I, Srinivasan Y, Duong DN, Palmer D, et al. Sphingosine-1-phosphate in the plasma compartment regulates basal and inflammation-induced vascular leak in mice. The Journal of Clinical Investigation. 2009, 119, 1871–1879. [CrossRef]
- Liu Y, Wada R, Yamashita T, Mi Y, Deng CX, Hobson JP, et al. Edg-1, the G protein-coupled receptor for sphingosine-1-phosphate, is essential for vascular maturation. The Journal of Clinical Investigation. 2000, 106, 951–961. [CrossRef]
- Allende ML, Yamashita T, Proia RL. G-protein-coupled receptor S1P1 acts within endothelial cells to regulate vascular maturation. Blood. 2003, 102, 3665–3667. [CrossRef]
- Obinata H, Hla T. Sphingosine 1-phosphate and inflammation. International Immunology. 2019, 31, 617–625. [CrossRef]
- Galvani S, Sanson M, Blaho VA, Swendeman SL, Obinata H, Conger H, et al. HDL-bound sphingosine 1-phosphate acts as a biased agonist for the endothelial cell receptor S1P1 to limit vascular inflammation. Science Signaling. 2015, 8, ra79. [CrossRef]
- Tong X, Lv P, Mathew AV, Liu D, Niu C, Wang Y, et al. The compensatory enrichment of sphingosine -1- phosphate harbored on glycated high-density lipoprotein restores endothelial protective function in type 2 diabetes mellitus. Cardiovascular Diabetology. 2014, 1382. [CrossRef]
- Jebari-Benslaiman S, Galicia-García U, Larrea-Sebal A, Olaetxea JR, Alloza I, Vandenbroeck K, et al. Pathophysiology of Atherosclerosis. International Journal of Molecular Sciences. 2022, 23, 3346, Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8954705/ (accessed on 23 January 2024). [CrossRef]
- Akhiyat N, Vasile V, Ahmad A, Sara JD, Nardi V, Lerman LO, et al. Plasma Ceramide Levels Are Elevated in Patients With Early Coronary Atherosclerosis and Endothelial Dysfunction. Journal of the American Heart Association. 2022, 11, e022852. [CrossRef]
- Othman A, Saely CH, Muendlein A, Vonbank A, Drexel H, von Eckardstein A, et al. Plasma C20-Sphingolipids predict cardiovascular events independently from conventional cardiovascular risk factors in patients undergoing coronary angiography. Atherosclerosis. 2015, 240, 216–221. [CrossRef]
- Edsfeldt A, Dunér P, Ståhlman M, Mollet IG, Asciutto G, Grufman H, et al. Sphingolipids Contribute to Human Atherosclerotic Plaque Inflammation. Arteriosclerosis, Thrombosis, and Vascular Biology. 2016, 36, 1132–1140. [CrossRef]
- Laaksonen R, Ekroos K, Sysi-Aho M, Hilvo M, Vihervaara T, Kauhanen D, et al. Plasma ceramides predict cardiovascular death in patients with stable coronary artery disease and acute coronary syndromes beyond LDL-cholesterol. European Heart Journal. 2016, 37, 1967–1976, Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4929378/ (accessed on 3 November 2023). [CrossRef]
- Lallemand T, Rouahi M, Swiader A, Grazide M, Geoffre N, Alayrac P, et al. nSMase2 (Type 2-Neutral Sphingomyelinase) Deficiency or Inhibition by GW4869 Reduces Inflammation and Atherosclerosis in Apoe−/− Mice. Arteriosclerosis, Thrombosis, and Vascular Biology. 2018, 38, 1479–1492, Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6039418/ (accessed on 3 November 2023). [CrossRef]
- Piccoli M, Cirillo F, Ghiroldi A, Rota P, Coviello S, Tarantino A, et al. Sphingolipids and Atherosclerosis: The Dual Role of Ceramide and Sphingosine-1-Phosphate. Antioxidants (Basel, Switzerland). 2023, 12, 143. [CrossRef]
- Li P, Zhang Y. Cross talk between ceramide and redox signaling: implications for endothelial dysfunction and renal disease. Handbook of Experimental Pharmacology. 2013, 216, 171–197. [CrossRef]
- Vos M, Dulovic-Mahlow M, Mandik F, Frese L, Kanana Y, Haissatou Diaw S, et al. Ceramide accumulation induces mitophagy and impairs β-oxidation in PINK1 deficiency. Proceedings of the National Academy of Sciences of the United States of America. 2021, 118, e2025347118, Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8639384/ (accessed on 13 April 2024). [CrossRef]
- Li X, Becker KA, Zhang Y. Ceramide in redox signaling and cardiovascular diseases. Cellular Physiology and Biochemistry: International Journal of Experimental Cellular Physiology, Biochemistry, and Pharmacology. 2010, 26, 41–48. [CrossRef]
- Ji Y, Chen J, Pang L, Chen C, Ye J, Liu H, et al. The Acid Sphingomyelinase Inhibitor Amitriptyline Ameliorates TNF-α-Induced Endothelial Dysfunction. Cardiovascular Drugs and Therapy. 2022. [CrossRef]
- Schweitzer KS, Hatoum H, Brown MB, Gupta M, Justice MJ, Beteck B, et al. Mechanisms of lung endothelial barrier disruption induced by cigarette smoke: role of oxidative stress and ceramides. American Journal of Physiology. Lung Cellular and Molecular Physiology. 2011, 301, 836. [CrossRef]
- Akoumianakis I, Badi I, Douglas G, Chuaiphichai S, Herdman L, Akawi N, et al. Insulin-induced vascular redox dysregulation in human atherosclerosis is ameliorated by dipeptidyl peptidase 4 inhibition. Science translational medicine. 2020, 12, eaav8824, Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7212010/ (accessed on 13 April 2024). [CrossRef]
- Zhang Q, Holland WL, Wilson L, Tanner JM, Kearns D, Cahoon JM, et al. Ceramide Mediates Vascular Dysfunction in Diet-Induced Obesity by PP2A-Mediated Dephosphorylation of the eNOS-Akt Complex. Diabetes. 2012, 61, 1848–1859, Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3379648/ (accessed on 13 April 2024). [CrossRef]
- Cantalupo A, Sasset L, Gargiulo A, Rubinelli L, Del Gaudio I, Benvenuto D, et al. Endothelial Sphingolipid De Novo Synthesis Controls Blood Pressure by Regulating Signal Transduction and NO via Ceramide. Hypertension (Dallas, Tex.: 1979). 2020, 75, 1279–1288. [CrossRef]
- Jernigan PL, Makley AT, Hoehn RS, Edwards MJ, Pritts TA. The role of sphingolipids in endothelial barrier function. Biological Chemistry. 2015, 396, 681–691. [CrossRef]
- Li H, Junk P, Huwiler A, Burkhardt C, Wallerath T, Pfeilschifter J, et al. Dual effect of ceramide on human endothelial cells: induction of oxidative stress and transcriptional upregulation of endothelial nitric oxide synthase. Circulation. 2002, 106, 2250–2256. [CrossRef]
- Walters MJ, Wrenn SP. Effect of sphingomyelinase-mediated generation of ceramide on aggregation of low-density lipoprotein. Langmuir: the ACS journal of surfaces and colloids. 2008, 24, 9642–9647. [CrossRef]
- Sneck M, Nguyen SD, Pihlajamaa T, Yohannes G, Riekkola M, Milne R, et al. Conformational changes of apoB-100 in SMase-modified LDL mediate formation of large aggregates at acidic pH. Journal of Lipid Research. 2012, 53, 1832–1839. [CrossRef]
- Ruuth M, Nguyen SD, Vihervaara T, Hilvo M, Laajala TD, Kondadi PK, et al. Susceptibility of low-density lipoprotein particles to aggregate depends on particle lipidome, is modifiable, and associates with future cardiovascular deaths. European Heart Journal. 2018, 39, 2562–2573. [CrossRef]
- Li W, Yang X, Xing S, Bian F, Yao W, Bai X, et al. Endogenous ceramide contributes to the transcytosis of oxLDL across endothelial cells and promotes its subendothelial retention in vascular wall. Oxidative Medicine and Cellular Longevity. 2014;2014823071. [CrossRef]
- Eckhardt ERM, Wang DQ-, Donovan JM, Carey MC. Dietary sphingomyelin suppresses intestinal cholesterol absorption by decreasing thermodynamic activity of cholesterol monomers. Gastroenterology. 2002, 122, 948–956. [CrossRef]
- Gao D, Pararasa C, Dunston CR, Bailey CJ, Griffiths HR. Palmitate promotes monocyte atherogenicity via de novo ceramide synthesis. Free Radical Biology & Medicine. 2012, 53, 796–806. [CrossRef]
- Alewijnse AE, Peters SLM. Sphingolipid signalling in the cardiovascular system: good, bad or both? European Journal of Pharmacology. 2008, 585, 292–302. [CrossRef]
- Lai Y, Tian Y, You X, Du J, Huang J. Effects of sphingolipid metabolism disorders on endothelial cells. Lipids in Health and Disease. 2022, 21, 101. [CrossRef]
- Kerage D, Brindley DN, Hemmings DG. Review: novel insights into the regulation of vascular tone by sphingosine 1-phosphate. Placenta. 2014;35 Suppl86. [CrossRef]
- Liu W, Liu B, Liu S, Zhang J, Lin S. Sphingosine-1-phosphate receptor 2 mediates endothelial cells dysfunction by PI3K-Akt pathway under high glucose condition. European Journal of Pharmacology. 2016;77619-25. [CrossRef]
- Galvani S, Sanson M, Blaho VA, Swendeman SL, Obinata H, Conger H, et al. HDL-bound sphingosine 1-phosphate acts as a biased agonist for the endothelial cell receptor S1P1 to limit vascular inflammation. Science signaling. 2015, 8, ra79, Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4768813/ (accessed on 7 November 2023). [CrossRef]
- Xu M, Waters CL, Hu C, Wysolmerski RB, Vincent PA, Minnear FL. Sphingosine 1-phosphate rapidly increases endothelial barrier function independently of VE-cadherin but requires cell spreading and Rho kinase. American Journal of Physiology. Cell Physiology. 2007, 293, 1309. [CrossRef]
- Dennhardt S, Finke KR, Huwiler A, Coldewey SM. Sphingosine-1-phosphate promotes barrier-stabilizing effects in human microvascular endothelial cells via AMPK-dependent mechanisms. Biochimica Et Biophysica Acta. Molecular Basis of Disease. 2019, 1865, 774–781. [CrossRef]
- Kim T, Kang Y, Lim Y, Lee H, Bae K, Lee Y, et al. Ceramide 1-phosphate induces neointimal formation via cell proliferation and cell cycle progression upstream of ERK1/2 in vascular smooth muscle cells. Experimental Cell Research. 2011, 317, 2041–2051. [CrossRef]
- Dawson G, Kruski AW, Scanu AM. Distribution of glycosphingolipids in the serum lipoproteins of normal human subjects and patients with hypo- and hyperlipidemias. Journal of Lipid Research. 1976, 17, 125–131.
- Bietrix F, Lombardo E, van Roomen CPAA, Ottenhoff R, Vos M, Rensen PCN, et al. Inhibition of glycosphingolipid synthesis induces a profound reduction of plasma cholesterol and inhibits atherosclerosis development in APOE*3 Leiden and low-density lipoprotein receptor-/- mice. Arteriosclerosis, Thrombosis, and Vascular Biology. 2010, 30, 931–937. [CrossRef]
- Arai T, Bhunia AK, Chatterjee S, Bulkley GB. Lactosylceramide stimulates human neutrophils to upregulate Mac-1, adhere to endothelium, and generate reactive oxygen metabolites in vitro. Circulation Research. 1998, 82, 540–547. [CrossRef]
- Deguchi H, Navarro S, Payne AB, Elias DJ, Dowling NF, Austin HD, et al. Low level of the plasma sphingolipid, glucosylceramide, is associated with thrombotic diseases. Research and Practice in Thrombosis and Haemostasis. 2017, 1, 33–40. [CrossRef]
- Chatterjee SB, Dey S, Shi WY, Thomas K, Hutchins GM. Accumulation of glycosphingolipids in human atherosclerotic plaque and unaffected aorta tissues. Glycobiology. 1997, 7, 57–65. [CrossRef]
- Chatterjee S, Clarke KS, Kwiterovich PO. Regulation of synthesis of lactosylceramide and long chain bases in normal and familial hypercholesterolemic cultured proximal tubular cells. The Journal of Biological Chemistry. 1986, 261, 13474–13479.
- Okrzeja J, Karwowska A, Błachnio-Zabielska A. The Role of Obesity, Inflammation and Sphingolipids in the Development of an Abdominal Aortic Aneurysm. Nutrients. 2022, 14, 2438. [CrossRef]
- Folkesson M, Vorkapic E, Gulbins E, Japtok L, Kleuser B, Welander M, et al. Inflammatory cells, ceramides, and expression of proteases in perivascular adipose tissue adjacent to human abdominal aortic aneurysms. Journal of Vascular Surgery. 2017, 65, 1171–1179.e1. [CrossRef]
- Xu J, Yeh CH, Chen S, He L, Sensi SL, Canzoniero LM, et al. Involvement of de novo ceramide biosynthesis in tumor necrosis factor-alpha/cycloheximide-induced cerebral endothelial cell death. The Journal of Biological Chemistry. 1998, 273, 16521–16526. [CrossRef]
- Pilane CM, LaBelle EF. NO induced apoptosis of vascular smooth muscle cells accompanied by ceramide increase. Journal of Cellular Physiology. 2004, 199, 310–315. [CrossRef]
- Kasumov T, Li L, Li M, Gulshan K, Kirwan JP, Liu X, et al. Ceramide as a mediator of non-alcoholic Fatty liver disease and associated atherosclerosis. PloS One. 2015, 10, e0126910. [CrossRef]
- Baudiß K, Ayata CK, Lazar Z, Cicko S, Beckert J, Meyer A, et al. Ceramide-1-phosphate inhibits cigarette smoke-induced airway inflammation. The European Respiratory Journal. 2015, 45, 1669–1680. [CrossRef]
- Goodall S, Crowther M, Hemingway DM, Bell PR, Thompson MM. Ubiquitous elevation of matrix metalloproteinase-2 expression in the vasculature of patients with abdominal aneurysms. Circulation. 2001, 104, 304–309. [CrossRef]
- Moxon JV, Liu D, Wong G, Weir JM, Behl-Gilhotra R, Bradshaw B, et al. Comparison of the serum lipidome in patients with abdominal aortic aneurysm and peripheral artery disease. Circulation. Cardiovascular Genetics. 2014, 7, 71–79. [CrossRef]
- Krishna SM, Seto SW, Moxon JV, Rush C, Walker PJ, Norman PE, et al. Fenofibrate increases high-density lipoprotein and sphingosine 1 phosphate concentrations limiting abdominal aortic aneurysm progression in a mouse model. The American Journal of Pathology. 2012, 181, 706–718. [CrossRef]
- Damirin A, Tomura H, Komachi M, Tobo M, Sato K, Mogi C, et al. Sphingosine 1-phosphate receptors mediate the lipid-induced cAMP accumulation through cyclooxygenase-2/prostaglandin I2 pathway in human coronary artery smooth muscle cells. Molecular Pharmacology. 2005, 67, 1177–1185. [CrossRef]
- Qu Z, Cheuk BLY, Cheng SWK. Differential expression of sphingosine-1-phosphate receptors in abdominal aortic aneurysms. Mediators of Inflammation. 2012;2012643609. [CrossRef]
- Campbell BCV, Khatri P. Stroke. Lancet (London, England). 2020, 396, 129–142. [CrossRef]
- Fiedorowicz A, Kozak-Sykała A, Bobak Ł, Kałas W, Strządała L. Ceramides and sphingosine-1-phosphate as potential markers in diagnosis of ischaemic stroke. Neurologia I Neurochirurgia Polska. 2019, 53, 484–491. [CrossRef]
- Takahashi K, Ginis I, Nishioka R, Klimanis D, Barone FC, White RF, et al. Glucosylceramide synthase activity and ceramide levels are modulated during cerebral ischemia after ischemic preconditioning. Journal of Cerebral Blood Flow and Metabolism: Official Journal of the International Society of Cerebral Blood Flow and Metabolism. 2004, 24, 623–627. [CrossRef]
- Brunkhorst R, Friedlaender F, Ferreirós N, Schwalm S, Koch A, Grammatikos G, et al. Alterations of the Ceramide Metabolism in the Peri-Infarct Cortex Are Independent of the Sphingomyelinase Pathway and Not Influenced by the Acid Sphingomyelinase Inhibitor Fluoxetine. Neural Plasticity. 2015;2015503079. [CrossRef]
- Kang MS, Ahn KH, Kim SK, Jeon HJ, Ji JE, Choi JM, et al. Hypoxia-induced neuronal apoptosis is mediated by de novo synthesis of ceramide through activation of serine palmitoyltransferase. Cellular Signalling. 2010, 22, 610–618. [CrossRef]
- Wang T, Zhang J, Yang M, Guo J, Li D, Li Y. Lipidomics Analysis Reveals a Protective Effect of Myriocin on Cerebral Ischemia/Reperfusion Model Rats. Journal of molecular neuroscience: MN. 2022, 72, 1846–1858. [CrossRef]
- Altura BM, Carella A, Gebrewold A, Shah NC, Altura BT, Resnick LM, et al. Why there is an Increased Risk of Cardiac Failure, Widening of Pulse Pressure.
- and Hemorrhagic Stroke in Type 2 Diabetics Over Age 60: Roles of Unrecognized.
- Hypomagnesemia and Epigenetics Coupled with Increased Levels of Ceramides,.
- Cytokines, ROS, 4-HNE and Platelet-Activating Factor. Journal of Clinical Case Studies. 2020, 5. Available online: https://www.sciforschenonline.org/journals/clinical-case-studies/article-data/JCCS198/JCCS198.pdf (accessed on 6 November 2023).
- Lee T, Cheng C, Chao H, Lee C, Kuo C, Tang S, et al. Plasma ceramides are associated with outcomes in acute ischemic stroke patients. Journal of the Formosan Medical Association = Taiwan Yi Zhi. 2022;121(1 Pt 1): 43-50. [CrossRef]
- Spijkers LJA, van den Akker RFP, Janssen BJA, Debets JJ, De Mey JGR, Stroes ESG, et al. Hypertension is associated with marked alterations in sphingolipid biology: a potential role for ceramide. PloS One. 2011, 6, e21817. [CrossRef]
- Ramirez MR, Muraro F, Zylbersztejn DS, Abel CR, Arteni NS, Lavinsky D, et al. Neonatal hypoxia-ischemia reduces ganglioside, phospholipid and cholesterol contents in the rat hippocampus. Neuroscience Research. 2003, 46, 339–347. [CrossRef]
- Whitehead SN, Chan KHN, Gangaraju S, Slinn J, Li J, Hou ST. Imaging mass spectrometry detection of gangliosides species in the mouse brain following transient focal cerebral ischemia and long-term recovery. PloS One. 2011, 6, e20808. [CrossRef]
- Caughlin S, Hepburn J, Liu Q, Wang L, Yeung KK-, Cechetto DF, et al. Chloroquine Restores Ganglioside Homeostasis and Improves Pathological and Behavioral Outcomes Post-stroke in the Rat. Molecular Neurobiology. 2019, 56, 3552–3562. [CrossRef]
- Hisaki H, Okazaki T, Kubota M, Nakane M, Fujimaki T, Nakayama H, et al. L-PDMP improves glucosylceramide synthesis and behavior in rats with focal ischemia. Neurological Research. 2008, 30, 979–984. [CrossRef]
- Su D, Ma J, Yang J, Kang Y, Lv M, Li Y. Monosialotetrahexosy-1 ganglioside attenuates diabetes-associated cerebral ischemia/reperfusion injury through suppression of the endoplasmic reticulum stress-induced apoptosis. Journal of Clinical Neuroscience: Official Journal of the Neurosurgical Society of Australasia. 2017;4154-59. [CrossRef]
- Katajamäki TT, Koivula M, Hilvo M, Lääperi MTA, Salminen MJ, Viljanen AM, et al. Ceramides and Phosphatidylcholines Associate with Cardiovascular Diseases in the Elderly. Clinical Chemistry. 2022, 68, 1502–1508. [CrossRef]
- Lee T, Cheng C, Lee C, Kuo C, Tang S, Jeng J. Investigating sphingolipids as biomarkers for the outcomes of acute ischemic stroke patients receiving endovascular treatment. Journal of the Formosan Medical Association = Taiwan Yi Zhi. 2023, 122, 19–28. [CrossRef]
- McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Böhm M, et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. European Heart Journal. 2021, 42, 3599–3726. [CrossRef]
- Kovilakath A, Wohlford G, Cowart LA. Circulating sphingolipids in heart failure. Frontiers in Cardiovascular Medicine. 2023;101154447. [CrossRef]
- Choi RH, Tatum SM, Symons JD, Summers SA, Holland WL. Ceramides and other sphingolipids as drivers of cardiovascular disease. Nature Reviews. Cardiology. 2021, 18, 701–711. [CrossRef]
- Borodzicz-Jażdżyk S, Jażdżyk P, Łysik W, Cudnoch-Jȩdrzejewska A, Czarzasta K. Sphingolipid metabolism and signaling in cardiovascular diseases. Frontiers in Cardiovascular Medicine. 2022;9915961. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9471951/ (accessed on 3 November 2023). [CrossRef]
- Wittenbecher C, Eichelmann F, Toledo E, Guasch-Ferré M, Ruiz-Canela M, Li J, et al. Lipid Profiles and Heart Failure Risk: Results From Two Prospective Studies. Circulation Research. 2021, 128, 309–320. [CrossRef]
- Knapp M, Baranowski M, Lisowska A, Musiał W. Decreased free sphingoid base concentration in the plasma of patients with chronic systolic heart failure. Advances in Medical Sciences. 2012, 57, 100–105. [CrossRef]
- Lemaitre RN, Jensen PN, Hoofnagle A, McKnight B, Fretts AM, King IB, et al. Plasma Ceramides and Sphingomyelins in Relation to Heart Failure Risk. Circulation. Heart Failure. 2019, 12, e005708. [CrossRef]
- Yin W, Li F, Tan X, Wang H, Jiang W, Wang X, et al. Plasma Ceramides and Cardiovascular Events in Hypertensive Patients at High Cardiovascular Risk. American Journal of Hypertension. 2021, 34, 1209–1216. [CrossRef]
- Javaheri A, Allegood JC, Cowart LA, Chirinos JA. Circulating Ceramide 16:0 in Heart Failure With Preserved Ejection Fraction. Journal of the American College of Cardiology. 2020, 75, 2273–2275. [CrossRef]
- Ji R, Akashi H, Drosatos K, Liao X, Jiang H, Kennel PJ, et al. Increased de novo ceramide synthesis and accumulation in failing myocardium. JCI insight. 2017, 2, e96203–96203. [CrossRef]
- Chokshi A, Drosatos K, Cheema FH, Ji R, Khawaja T, Yu S, et al. Ventricular assist device implantation corrects myocardial lipotoxicity, reverses insulin resistance, and normalizes cardiac metabolism in patients with advanced heart failure. Circulation. 2012, 125, 2844–2853. [CrossRef]
- Dong S, Ma W, Hao B, Hu F, Yan L, Yan X, et al. microRNA-21 promotes cardiac fibrosis and development of heart failure with preserved left ventricular ejection fraction by up-regulating Bcl-2. International Journal of Clinical and Experimental Pathology. 2014, 7, 565–574.
- de Mello VDF, Lankinen M, Schwab U, Kolehmainen M, Lehto S, Seppänen-Laakso T, et al. Link between plasma ceramides, inflammation and insulin resistance: association with serum IL-6 concentration in patients with coronary heart disease. Diabetologia. 2009, 52, 2612–2615. [CrossRef]
- Hadas Y, Vincek AS, Youssef E, Żak MM, Chepurko E, Sultana N, et al. Altering Sphingolipid Metabolism Attenuates Cell Death and Inflammatory Response After Myocardial Infarction. Circulation. 2020, 141, 916–930. [CrossRef]
- B Gowda S, Gowda D, Kain V, Chiba H, Hui S, Chalfant CE, et al. Sphingosine-1-phosphate interactions in the spleen and heart reflect extent of cardiac repair in mice and failing human hearts. American Journal of Physiology. Heart and Circulatory Physiology. 2021, 321, H599–H611. [CrossRef]
- Liu J, Liu X, Luo Y, Huang F, Xie Y, Zheng S, et al. Sphingolipids: drivers of cardiac fibrosis and atrial fibrillation. Journal of Molecular Medicine (Berlin, Germany). 2024, 102, 149–165. [CrossRef]
- Jensen PN, Fretts AM, Hoofnagle AN, Sitlani CM, McKnight B, King IB, et al. Plasma Ceramides and Sphingomyelins in Relation to Atrial Fibrillation Risk: The Cardiovascular Health Study. Journal of the American Heart Association: Cardiovascular and Cerebrovascular Disease. 2020, 9, e012853, Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7070192/ (accessed on 3 November 2023). [CrossRef]
- Holzwirth E, Fischer-Schaepmann T, Obradovic D, von Lucadou M, Schwedhelm E, Daum G, et al. Anti-inflammatory HDL effects are impaired in atrial fibrillation. Heart and Vessels. 2022, 37, 161–171. [CrossRef]
- Takuwa N, Ohkura S, Takashima S, Ohtani K, Okamoto Y, Tanaka T, et al. S1P3-mediated cardiac fibrosis in sphingosine kinase 1 transgenic mice involves reactive oxygen species. Cardiovascular Research. 2010, 85, 484–493. [CrossRef]
- Cencetti F, Bernacchioni C, Nincheri P, Donati C, Bruni P. Transforming growth factor-beta1 induces transdifferentiation of myoblasts into myofibroblasts via up-regulation of sphingosine kinase-1/S1P3 axis. Molecular Biology of the Cell. 2010, 21, 1111–1124. [CrossRef]
- Wilkerson JL, Basu SK, Stiles MA, Prislovsky A, Grambergs RC, Nicholas SE, et al. Ablation of Sphingosine Kinase 1 Protects Cornea from Neovascularization in a Mouse Corneal Injury Model. Cells. 2022, 11, 2914. [CrossRef]
- Trappe K, Thomas D, Bikou O, Kelemen K, Lugenbiel P, Voss F, et al. Suppression of persistent atrial fibrillation by genetic knockdown of caspase 3: a pre-clinical pilot study. European Heart Journal. 2013, 34, 147–157. [CrossRef]
- Li Y, Gong Z, Sheng L, Gong Y, Tan X, Li W, et al. Anti-apoptotic effects of a calpain inhibitor on cardiomyocytes in a canine rapid atrial fibrillation model. Cardiovascular Drugs and Therapy. 2009, 23, 361–368. [CrossRef]
- Himmel HM, Meyer Zu Heringdorf D, Graf E, Dobrev D, Kortner A, Schüler S, et al. Evidence for Edg-3 receptor-mediated activation of I(K.ACh) by sphingosine-1-phosphate in human atrial cardiomyocytes. Molecular Pharmacology. 2000, 58, 449–454. [CrossRef]
- Berkowitz L, Salazar C, Ryff CD, Coe CL, Rigotti A. Serum sphingolipid profiling as a novel biomarker for metabolic syndrome characterization. Frontiers in Cardiovascular Medicine. 2022, 9, 1092331. [CrossRef]
- Samad F, Hester KD, Yang G, Hannun YA, Bielawski J. Altered adipose and plasma sphingolipid metabolism in obesity: a potential mechanism for cardiovascular and metabolic risk. Diabetes. 2006, 55, 2579–2587. [CrossRef]
- Majumdar I, Mastrandrea LD. Serum sphingolipids and inflammatory mediators in adolescents at risk for metabolic syndrome. Endocrine. 2012, 41, 442–449. [CrossRef]
- Samad F, Badeanlou L, Shah C, Yang G. Adipose tissue and ceramide biosynthesis in the pathogenesis of obesity. Advances in Experimental Medicine and Biology. 2011;72167-86. [CrossRef]
- Holland WL, Miller RA, Wang ZV, Sun K, Barth BM, Bui HH, et al. Receptor-mediated activation of ceramidase activity initiates the pleiotropic actions of adiponectin. Nature Medicine. 2011, 17, 55–63. [CrossRef]
- Haus JM, Kashyap SR, Kasumov T, Zhang R, Kelly KR, Defronzo RA, et al. Plasma ceramides are elevated in obese subjects with type 2 diabetes and correlate with the severity of insulin resistance. Diabetes. 2009, 58, 337–343. [CrossRef]
- Holland WL, Brozinick JT, Wang L, Hawkins ED, Sargent KM, Liu Y, et al. Inhibition of ceramide synthesis ameliorates glucocorticoid-, saturated-fat-, and obesity-induced insulin resistance. Cell Metabolism. 2007, 5, 167–179. [CrossRef]
- Bikman BT, Guan Y, Shui G, Siddique MM, Holland WL, Kim JY, et al. Fenretinide Prevents Lipid-induced Insulin Resistance by Blocking Ceramide Biosynthesis. The Journal of Biological Chemistry. 2012, 287, 17426–17437, Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3366851/ (accessed on 18 October 2023). [CrossRef]
- Keppley LJW, Walker SJ, Gademsey AN, Smith JP, Keller SR, Kester M, et al. Nervonic acid limits weight gain in a mouse model of diet-induced obesity. FASEB journal : official publication of the Federation of American Societies for Experimental Biology. 2020, 34, 15314–15326, Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8183615/ (accessed on 25 June 2024). [CrossRef]
- Park J, Park W, Kuperman Y, Boura-Halfon S, Pewzner-Jung Y, Futerman AH. Ablation of very long acyl chain sphingolipids causes hepatic insulin resistance in mice due to altered detergent-resistant membranes. Hepatology (Baltimore, Md.). 2013, 57, 525–532. [CrossRef]
- Straczkowski M, Kowalska I, Baranowski M, Nikolajuk A, Otziomek E, Zabielski P, et al. Increased skeletal muscle ceramide level in men at risk of developing type 2 diabetes. Diabetologia. 2007, 50, 2366–2373. [CrossRef]
- Luo C, Liu H, Wang X, Xia L, Huang H, Peng X, et al. The associations between individual plasma SFAs, serine palmitoyl-transferase long-chain base subunit 3 gene rs680379 polymorphism, and type 2 diabetes among Chinese adults. The American Journal of Clinical Nutrition. 2021, 114, 704–712. [CrossRef]
- Tagami S, Inokuchi Ji J, Kabayama K, Yoshimura H, Kitamura F, Uemura S, et al. Ganglioside GM3 participates in the pathological conditions of insulin resistance. The Journal of Biological Chemistry. 2002, 277, 3085–3092. [CrossRef]
- Chaurasia B, Summers SA. Ceramides - Lipotoxic Inducers of Metabolic Disorders. Trends in endocrinology and metabolism: TEM. 2015, 26, 538–550. [CrossRef]
- Holland WL, Adams AC, Brozinick JT, Bui HH, Miyauchi Y, Kusminski CM, et al. An FGF21-adiponectin-ceramide axis controls energy expenditure and insulin action in mice. Cell Metabolism. 2013, 17, 790–797. [CrossRef]
- Aerts JM, Ottenhoff R, Powlson AS, Grefhorst A, van Eijk M, Dubbelhuis PF, et al. Pharmacological inhibition of glucosylceramide synthase enhances insulin sensitivity. Diabetes. 2007, 56, 1341–1349. [CrossRef]
- Eizirik DL, Pasquali L, Cnop M. Pancreatic β-cells in type 1 and type 2 diabetes mellitus: different pathways to failure. Nature Reviews. Endocrinology. 2020, 16, 349–362. [CrossRef]
- Hahn C, Tyka K, Saba JD, Lenzen S, Gurgul-Convey E. Overexpression of sphingosine-1-phosphate lyase protects insulin-secreting cells against cytokine toxicity. The Journal of Biological Chemistry. 2017, 292, 20292–20304, Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5724014/ (accessed on 12 May 2024). [CrossRef]
- Green CD, Maceyka M, Cowart LA, Spiegel S. Sphingolipids in Metabolic Disease: The Good, the Bad, and the Unknown. Cell metabolism. 2021, 33, 1293–1306, Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8269961/ (accessed on 25 June 2024). [CrossRef]
- Jörns A, Akin M, Arndt T, Terbish T, Zu Vilsendorf AM, Wedekind D, et al. Anti-TCR therapy combined with fingolimod for reversal of diabetic hyperglycemia by β cell regeneration in the LEW.1AR1-iddm rat model of type 1 diabetes. Journal of Molecular Medicine (Berlin, Germany). 2014, 92, 743–755. [CrossRef]
- Rütti S, Ehses JA, Sibler RA, Prazak R, Rohrer L, Georgopoulos S, et al. Low- and high-density lipoproteins modulate function, apoptosis, and proliferation of primary human and murine pancreatic beta-cells. Endocrinology. 2009, 150, 4521–4530. [CrossRef]
- Anderson AK, Lambert JM, Montefusco DJ, Tran BN, Roddy P, Holland WL, et al. Depletion of adipocyte sphingosine kinase 1 leads to cell hypertrophy, impaired lipolysis, and nonalcoholic fatty liver disease. Journal of Lipid Research. 2020, 61, 1328–1340. [CrossRef]
- Kitada Y, Kajita K, Taguchi K, Mori I, Yamauchi M, Ikeda T, et al. Blockade of Sphingosine 1-Phosphate Receptor 2 Signaling Attenuates High-Fat Diet-Induced Adipocyte Hypertrophy and Systemic Glucose Intolerance in Mice. Endocrinology. 2016, 157, 1839–1851, Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4870879/ (accessed on 26 June 2024). [CrossRef]
- Dubé JJ, Amati F, Toledo FGS, Stefanovic-Racic M, Rossi A, Coen P, et al. Effects of weight loss and exercise on insulin resistance, and intramyocellular triacylglycerol, diacylglycerol and ceramide. Diabetologia. 2011, 54, 1147–1156, Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3804898/ (accessed on 3 November 2023). [CrossRef]
- Kasumov T, Solomon TPJ, Hwang C, Huang H, Haus JM, Zhang R, et al. Improved insulin sensitivity after exercise training is linked to reduced plasma C14:0 ceramide in obesity and type 2 diabetes. Obesity (Silver Spring, Md.). 2015, 23, 1414–1421. [CrossRef]
- Kayser BD, Prifti E, Lhomme M, Belda E, Dao M, Aron-Wisnewsky J, et al. Elevated serum ceramides are linked with obesity-associated gut dysbiosis and impaired glucose metabolism. Metabolomics: Official Journal of the Metabolomic Society. 2019, 15, 140. [CrossRef]
- Promrat K, Longato L, Wands JR, de la Monte SM. Weight loss amelioration of non-alcoholic steatohepatitis linked to shifts in hepatic ceramide expression and serum ceramide levels. Hepatology Research: The Official Journal of the Japan Society of Hepatology. 2011, 41, 754–762. [CrossRef]
- Kayser BD, Lhomme M, Dao MC, Ichou F, Bouillot J-, Prifti E, et al. Serum lipidomics reveals early differential effects of gastric bypass compared with banding on phospholipids and sphingolipids independent of differences in weight loss. International Journal of Obesity (2005). 2017, 41, 917–925. [CrossRef]
- Özer H, Aslan İ, Oruç MT, Çöpelci Y, Afşar E, Kaya S, et al. Early postoperative changes of sphingomyelins and ceramides after laparoscopic sleeve gastrectomy. Lipids in Health and Disease. 2018, 17, 269. [CrossRef]
- Mikhalkova D, Holman SR, Jiang H, Saghir M, Novak E, Coggan AR, et al. Bariatric Surgery-Induced Cardiac and Lipidomic Changes in Obesity-Related Heart Failure with Preserved Ejection Fraction. Obesity (Silver Spring, Md.). 2018, 26, 284–290. [CrossRef]
- Huang H, Kasumov T, Gatmaitan P, Heneghan HM, Kashyap SR, Schauer PR, et al. Gastric bypass surgery reduces plasma ceramide subspecies and improves insulin sensitivity in severely obese patients. Obesity (Silver Spring, Md.). 2011, 19, 2235–2240. [CrossRef]
- Heneghan HM, Huang H, Kashyap SR, Gornik HL, McCullough AJ, Schauer PR, et al. Reduced cardiovascular risk after bariatric surgery is linked to plasma ceramides, apolipoprotein-B100, and ApoB100/A1 ratio. Surgery for Obesity and Related Diseases: Official Journal of the American Society for Bariatric Surgery. 2013, 9, 100–107. [CrossRef]
- Graessler J, Bornstein TD, Goel D, Bhalla VP, Lohmann T, Wolf T, et al. Lipidomic profiling before and after Roux-en-Y gastric bypass in obese patients with diabetes. The Pharmacogenomics Journal. 2014, 14, 201–207. [CrossRef]
- Coen PM, Menshikova EV, Distefano G, Zheng D, Tanner CJ, Standley RA, et al. Exercise and Weight Loss Improve Muscle Mitochondrial Respiration, Lipid Partitioning, and Insulin Sensitivity After Gastric Bypass Surgery. Diabetes. 2015, 64, 3737–3750. [CrossRef]
- Hu W, Ross J, Geng T, Brice SE, Cowart LA. Differential regulation of dihydroceramide desaturase by palmitate versus monounsaturated fatty acids: implications for insulin resistance. The Journal of Biological Chemistry. 2011, 286, 16596–16605. [CrossRef]
- Kien CL, Bunn JY, Poynter ME, Stevens R, Bain J, Ikayeva O, et al. A lipidomics analysis of the relationship between dietary fatty acid composition and insulin sensitivity in young adults. Diabetes. 2013, 62, 1054–1063. [CrossRef]
- Norris GH, Milard M, Michalski M, Blesso CN. Protective properties of milk sphingomyelin against dysfunctional lipid metabolism, gut dysbiosis, and inflammation. The Journal of Nutritional Biochemistry. 2019;73108224. [CrossRef]
- Noh SK, Koo SI. Milk sphingomyelin is more effective than egg sphingomyelin in inhibiting intestinal absorption of cholesterol and fat in rats. The Journal of Nutrition. 2004, 134, 2611–2616. [CrossRef]
- Kamili A, Wat E, Chung RW, Tandy S, Weir JM, Meikle PJ, et al. Hepatic accumulation of intestinal cholesterol is decreased and fecal cholesterol excretion is increased in mice fed a high-fat diet supplemented with milk phospholipids. Nutrition & Metabolism. 2010;790. [CrossRef]
- Wat E, Tandy S, Kapera E, Kamili A, Chung RWS, Brown A, et al. Dietary phospholipid-rich dairy milk extract reduces hepatomegaly, hepatic steatosis and hyperlipidemia in mice fed a high-fat diet. Atherosclerosis. 2009, 205, 144–150. [CrossRef]
- Norris GH, Jiang C, Ryan J, Porter CM, Blesso CN. Milk sphingomyelin improves lipid metabolism and alters gut microbiota in high fat diet-fed mice. The Journal of Nutritional Biochemistry. 2016;3093-101. [CrossRef]
- Le Barz M, Vors C, Combe E, Joumard-Cubizolles L, Lecomte M, Joffre F, et al. Milk polar lipids favorably alter circulating and intestinal ceramide and sphingomyelin species in postmenopausal women. JCI insight. 2021, 6, e146161–146161. [CrossRef]
- Ramprasath VR, Jones PJ, Buckley DD, Woollett LA, Heubi JE. Effect of dietary sphingomyelin on absorption and fractional synthetic rate of cholesterol and serum lipid profile in humans. Lipids in Health and Disease. 2013;12125. [CrossRef]
- Li C, Wu L, Zhu C, Du H, Chen G, Yang F. The impacts of dietary sphingomyelin supplementation on metabolic parameters of healthy adults: a systematic review and meta-analysis of randomized controlled trials. Frontiers in Nutrition. 2024;111363077. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10922005/ (accessed on 17 May 2024). [CrossRef]
- Weiland A, Bub A, Barth SW, Schrezenmeir J, Pfeuffer M. Effects of dietary milk- and soya-phospholipids on lipid-parameters and other risk indicators for cardiovascular diseases in overweight or obese men – two double-blind, randomised, controlled, clinical trials. Journal of Nutritional Science. 2016;5e21. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4891556/ (accessed on 17 May 2024). [CrossRef]
- Milard M, Laugerette F, Durand A, Buisson C, Meugnier E, Loizon E, et al. Milk Polar Lipids in a High-Fat Diet Can Prevent Body Weight Gain: Modulated Abundance of Gut Bacteria in Relation with Fecal Loss of Specific Fatty Acids. Molecular Nutrition & Food Research. 2019, 63, e1801078. [CrossRef]
- Lecomte M, Couëdelo L, Meugnier E, Plaisancié P, Létisse M, Benoit B, et al. Dietary emulsifiers from milk and soybean differently impact adiposity and inflammation in association with modulation of colonic goblet cells in high-fat fed mice. Molecular Nutrition & Food Research. 2016, 60, 609–620. [CrossRef]
- Vors C, Joumard-Cubizolles L, Lecomte M, Combe E, Ouchchane L, Drai J, et al. Milk polar lipids reduce lipid cardiovascular risk factors in overweight postmenopausal women: towards a gut sphingomyelin-cholesterol interplay. Gut. 2020, 69, 487–501, Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7034342/ (accessed on 17 May 2024). [CrossRef]
- Fumeron F, Nicolas A, Bastard J-, Fellahi S, Wigger L, Ibberson M, et al. Dairy consumption is associated with lower plasma dihydroceramides in women from the D.E.S.I.R. cohort. Diabetes & Metabolism. 2020, 46, 144–149. [CrossRef]
- Meikle PJ, Barlow CK, Mellett NA, Mundra PA, Bonham MP, Larsen A, et al. Postprandial Plasma Phospholipids in Men Are Influenced by the Source of Dietary Fat. The Journal of Nutrition. 2015, 145, 2012–2018. [CrossRef]
- Alexander DD, Bylsma LC, Vargas AJ, Cohen SS, Doucette A, Mohamed M, et al. Dairy consumption and CVD: a systematic review and meta-analysis - CORRIGENDUM. The British Journal of Nutrition. 2016, 115, 2268. [CrossRef]
- de Goede J, Soedamah-Muthu SS, Pan A, Gijsbers L, Geleijnse JM. Dairy Consumption and Risk of Stroke: A Systematic Review and Updated Dose-Response Meta-Analysis of Prospective Cohort Studies. Journal of the American Heart Association. 2016, 5, e002787. [CrossRef]
- Chen G, Wang Y, Tong X, Szeto IMY, Smit G, Li Z, et al. Cheese consumption and risk of cardiovascular disease: a meta-analysis of prospective studies. European Journal of Nutrition. 2017, 56, 2565–2575. [CrossRef]
- Mishali M, Prizant-Passal S, Avrech T, Shoenfeld Y. Association between dairy intake and the risk of contracting type 2 diabetes and cardiovascular diseases: a systematic review and meta-analysis with subgroup analysis of men versus women. Nutrition Reviews. 2019, 77, 417–429. [CrossRef]
- Zhang K, Chen X, Zhang L, Deng Z. Fermented dairy foods intake and risk of cardiovascular diseases: A meta-analysis of cohort studies. Critical Reviews in Food Science and Nutrition. 2020, 60, 1189–1194. [CrossRef]
- Chen Z, Ahmed M, Ha V, Jefferson K, Malik V, Ribeiro PAB, et al. Dairy Product Consumption and Cardiovascular Health: A Systematic Review and Meta-analysis of Prospective Cohort Studies. Advances in Nutrition (Bethesda, Md.). 2022, 13, 439–454. [CrossRef]
- Jakobsen MU, Trolle E, Outzen M, Mejborn H, Grønberg MG, Lyndgaard CB, et al. Intake of dairy products and associations with major atherosclerotic cardiovascular diseases: a systematic review and meta-analysis of cohort studies. Scientific Reports. 2021, 11, 1303. [CrossRef]
- Bechthold A, Boeing H, Schwedhelm C, Hoffmann G, Knüppel S, Iqbal K, et al. Food groups and risk of coronary heart disease, stroke and heart failure: A systematic review and dose-response meta-analysis of prospective studies. Critical Reviews in Food Science and Nutrition. 2019, 59, 1071–1090. [CrossRef]
- Guo J, Astrup A, Lovegrove JA, Gijsbers L, Givens DI, Soedamah-Muthu SS. Milk and dairy consumption and risk of cardiovascular diseases and all-cause mortality: dose-response meta-analysis of prospective cohort studies. European Journal of Epidemiology. 2017, 32, 269–287. [CrossRef]
- Shin K, Seo C, Cho H, Oh S, Hong S, Yoo H, et al. Ginsenoside compound K inhibits angiogenesis via regulation of sphingosine kinase-1 in human umbilical vein endothelial cells. Archives of Pharmacal Research. 2014, 37, 1183–1192. [CrossRef]
- Meng Y, Du Z, Li Y, Wang L, Gao P, Gao X, et al. Integration of Metabolomics With Pharmacodynamics to Elucidate the Anti-myocardial Ischemia Effects of Combination of Notoginseng Total Saponins and Safflower Total Flavonoids. Frontiers in Pharmacology. 2018, 9, 667. [CrossRef]
- Wu F, Lai S, Fu D, Liu J, Wang C, Feng H, et al. Neuroprotective Effects and Metabolomics Study of Protopanaxatriol (PPT) on Cerebral Ischemia/Reperfusion Injury In Vitro and In Vivo. International Journal of Molecular Sciences. 2023, 24, 1789. [CrossRef]
- Kwon Y, Lee G, Liu K, Jung D. Effect of Korean Red Ginseng on Plasma Ceramide Levels in Postmenopausal Women with Hypercholesterolemia: A Pilot Randomized Controlled Trial. Metabolites. 2021, 11, 417. [CrossRef]
- Dai T, Yan F, Gong J, Liu S. Anti-heart failure mechanism of saponin extract of black ginseng based on metabolomics. Journal of Pharmaceutical and Biomedical Analysis. 2023, 236, 115738. [CrossRef]
- Tian X, Chen X, Jiang Q, Sun Q, Liu T, Hong Y, et al. Notoginsenoside R1 Ameliorates Cardiac Lipotoxicity Through AMPK Signaling Pathway. Frontiers in Pharmacology. 2022;13864326. [CrossRef]
- Tang M, Zhao S, Li R, Hou W. Therapeutic mechanisms of ginseng in coronary heart disease. Frontiers in Pharmacology. 2023, 14, 1271029. [CrossRef]
- Lankinen M, Schwab U, Kolehmainen M, Paananen J, Nygren H, Seppänen-Laakso T, et al. A Healthy Nordic Diet Alters the Plasma Lipidomic Profile in Adults with Features of Metabolic Syndrome in a Multicenter Randomized Dietary Intervention. The Journal of Nutrition. 2015, 146, 662–672. [CrossRef]
- Mathews AT, Famodu OA, Olfert MD, Murray PJ, Cuff CF, Downes MT, et al. Efficacy of nutritional interventions to lower circulating ceramides in young adults: FRUVEDomic pilot study. Physiological Reports. 2017, 5, e13329. [CrossRef]
- Seah JYH, Chew WS, Torta F, Khoo CM, Wenk MR, Herr DR, et al. Dietary Fat and Protein Intake in Relation to Plasma Sphingolipids as Determined by a Large-Scale Lipidomic Analysis. Metabolites. 2021, 11, 93. [CrossRef]
- Luukkonen PK, Sädevirta S, Zhou Y, Kayser B, Ali A, Ahonen L, et al. Saturated Fat Is More Metabolically Harmful for the Human Liver Than Unsaturated Fat or Simple Sugars. Diabetes Care. 2018, 41, 1732–1739. [CrossRef]
- Rosqvist F, Kullberg J, Ståhlman M, Cedernaes J, Heurling K, Johansson H, et al. Overeating Saturated Fat Promotes Fatty Liver and Ceramides Compared With Polyunsaturated Fat: A Randomized Trial. The Journal of Clinical Endocrinology and Metabolism. 2019, 104, 6207–6219. [CrossRef]
- Holland WL, Bikman BT, Wang L, Yuguang G, Sargent KM, Bulchand S, et al. Lipid-induced insulin resistance mediated by the proinflammatory receptor TLR4 requires saturated fatty acid-induced ceramide biosynthesis in mice. The Journal of Clinical Investigation. 2011, 121, 1858–1870. [CrossRef]
- Chavez JA, Summers SA. Characterizing the effects of saturated fatty acids on insulin signaling and ceramide and diacylglycerol accumulation in 3T3-L1 adipocytes and C2C12 myotubes. Archives of Biochemistry and Biophysics. 2003, 419, 101–109. [CrossRef]
- Lahiri S, Park H, Laviad EL, Lu X, Bittman R, Futerman AH. Ceramide synthesis is modulated by the sphingosine analog FTY720 via a mixture of uncompetitive and noncompetitive inhibition in an Acyl-CoA chain length-dependent manner. The Journal of Biological Chemistry. 2009, 284, 16090–16098. [CrossRef]
- Dawson G, Qin J. Gilenya (FTY720) inhibits acid sphingomyelinase by a mechanism similar to tricyclic antidepressants. Biochemical and Biophysical Research Communications. 2011, 404, 321–323. [CrossRef]
- Lim KG, Tonelli F, Li Z, Lu X, Bittman R, Pyne S, et al. FTY720 analogues as sphingosine kinase 1 inhibitors: enzyme inhibition kinetics, allosterism, proteasomal degradation, and actin rearrangement in MCF-7 breast cancer cells. The Journal of Biological Chemistry. 2011, 286, 18633–18640. [CrossRef]
- Chun J, Hartung H. Mechanism of action of oral fingolimod (FTY720) in multiple sclerosis. Clinical Neuropharmacology. 2010, 33, 91–101. [CrossRef]
- Cohen JA, Barkhof F, Comi G, Hartung H, Khatri BO, Montalban X, et al. Oral fingolimod or intramuscular interferon for relapsing multiple sclerosis. The New England Journal of Medicine. 2010, 362, 402–415. [CrossRef]
- Kappos L, Radue E, O'Connor P, Polman C, Hohlfeld R, Calabresi P, et al. A placebo-controlled trial of oral fingolimod in relapsing multiple sclerosis. The New England Journal of Medicine. 2010, 362, 387–401. [CrossRef]
- Nofer J, Bot M, Brodde M, Taylor PJ, Salm P, Brinkmann V, et al. FTY720, a synthetic sphingosine 1 phosphate analogue, inhibits development of atherosclerosis in low-density lipoprotein receptor-deficient mice. Circulation. 2007, 115, 501–508. [CrossRef]
- Santos-Gallego CG, Vahl TP, Goliasch G, Picatoste B, Arias T, Ishikawa K, et al. Sphingosine-1-Phosphate Receptor Agonist Fingolimod Increases Myocardial Salvage and Decreases Adverse Postinfarction Left Ventricular Remodeling in a Porcine Model of Ischemia/Reperfusion. Circulation. 2016, 133, 954–966. [CrossRef]
- Egom EEA, Ke Y, Musa H, Mohamed TMA, Wang T, Cartwright E, et al. FTY720 prevents ischemia/reperfusion injury-associated arrhythmias in an ex vivo rat heart model via activation of Pak1/Akt signaling. Journal of Molecular and Cellular Cardiology. 2010, 48, 406–414. [CrossRef]
- Liu W, Zi M, Naumann R, Ulm S, Jin J, Taglieri DM, et al. Pak1 as a novel therapeutic target for antihypertrophic treatment in the heart. Circulation. 2011, 124, 2702–2715. [CrossRef]
- Ng TWK, Ooi EMM, Watts GF, Chan DC, Weir JM, Meikle PJ, et al. Dose-dependent effects of rosuvastatin on the plasma sphingolipidome and phospholipidome in the metabolic syndrome. The Journal of Clinical Endocrinology and Metabolism. 2014, 99, 2335. [CrossRef]
- Tarasov K, Ekroos K, Suoniemi M, Kauhanen D, Sylvänne T, Hurme R, et al. Molecular lipids identify cardiovascular risk and are efficiently lowered by simvastatin and PCSK9 deficiency. The Journal of Clinical Endocrinology and Metabolism. 2014, 99, 45. [CrossRef]
- Zhao M, You B, Wang X, Huang J, Zhou M, Shi R, et al. Desipramine enhances the stability of atherosclerotic plaque in rabbits monitored with molecular imaging. PLOS ONE. 2023, 18, e0283612, Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10062573/ (accessed on 4 November 2023). [CrossRef]
- Akawi N, Checa A, Antonopoulos AS, Akoumianakis I, Daskalaki E, Kotanidis CP, et al. Fat-Secreted Ceramides Regulate Vascular Redox State and Influence Outcomes in Patients With Cardiovascular Disease. Journal of the American College of Cardiology. 2021, 77, 2494–2513. [CrossRef]
- Denimal D, Bergas V, Pais-de-Barros J, Simoneau I, Demizieux L, Passilly-Degrace P, et al. Liraglutide reduces plasma dihydroceramide levels in patients with type 2 diabetes. Cardiovascular Diabetology. 2023, 22, 104. [CrossRef]
- Leonardini A, D'Oria R, Incalza MA, Caccioppoli C, Andrulli Buccheri V, Cignarelli A, et al. GLP-1 Receptor Activation Inhibits Palmitate-Induced Apoptosis via Ceramide in Human Cardiac Progenitor Cells. The Journal of Clinical Endocrinology and Metabolism. 2017, 102, 4136–4147. [CrossRef]
- Aragón-Herrera A, Feijóo-Bandín S, Otero Santiago M, Barral L, Campos-Toimil M, Gil-Longo J, et al. Empagliflozin reduces the levels of CD36 and cardiotoxic lipids while improving autophagy in the hearts of Zucker diabetic fatty rats. Biochemical Pharmacology. 2019, 170, 113677. [CrossRef]
- Beckmann N, Sharma D, Gulbins E, Becker KA, Edelmann B. Inhibition of acid sphingomyelinase by tricyclic antidepressants and analogons. Frontiers in Physiology. 2014, 5, 331, Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4151525/ (accessed on 2 November 2023). [CrossRef]
- Gulbins E, Palmada M, Reichel M, Lüth A, Böhmer C, Amato D, et al. Acid sphingomyelinase-ceramide system mediates effects of antidepressant drugs. Nature Medicine. 2013, 19, 934–938. [CrossRef]
- Usta E, Mustafi M, Artunc F, Walker T, Voth V, Aebert H, et al. The challenge to verify ceramide's role of apoptosis induction in human cardiomyocytes--a pilot study. Journal of Cardiothoracic Surgery. 2011, 638. [CrossRef]
- Lu Z, Li Y, Syn W, Wang Z, Lopes-Virella MF, Lyons TJ, et al. Amitriptyline inhibits nonalcoholic steatohepatitis and atherosclerosis induced by high-fat diet and LPS through modulation of sphingolipid metabolism. American Journal of Physiology - Endocrinology and Metabolism. 2020, 318, E131–E144, Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7052581/ (accessed on 2 November 2023). [CrossRef]
- Ji Y, Chen J, Pang L, Chen C, Ye J, Liu H, et al. The Acid Sphingomyelinase Inhibitor Amitriptyline Ameliorates TNF-α-Induced Endothelial Dysfunction. Cardiovascular Drugs and Therapy. 2022. [CrossRef]
- Guan Y, Li X, Umetani M, Boini KM, Li P, Zhang Y. Tricyclic antidepressant amitriptyline inhibits autophagic flux and prevents tube formation in vascular endothelial cells. Basic & clinical pharmacology & toxicology. 2019, 124, 370–384, Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6226027/ (accessed on 2 November 2023). [CrossRef]
- Jiang M, Huang S, Duan W, Liu Q, Lei M. Inhibition of acid sphingomyelinase activity ameliorates endothelial dysfunction in db/db mice. Bioscience Reports. 2019, 39, BSR20182144. [CrossRef]
- Cui J, Engelman RM, Maulik N, Das DK. Role of ceramide in ischemic preconditioning. Journal of the American College of Surgeons. 2004, 198, 770–777. [CrossRef]
- Chung H, Kollmey AS, Schrepper A, Kohl M, Bläss MF, Stehr SN, et al. Adjustment of Dysregulated Ceramide Metabolism in a Murine Model of Sepsis-Induced Cardiac Dysfunction. International Journal of Molecular Sciences. 2017, 18, 839. [CrossRef]
- Mohamud Yusuf A, Hagemann N, Zhang X, Zafar M, Hussner T, Bromkamp C, et al. Acid sphingomyelinase deactivation post-ischemia promotes brain angiogenesis and remodeling by small extracellular vesicles. Basic Research in Cardiology. 2022, 117, 43. [CrossRef]
- Hodun K, Sztolsztener K, Chabowski A. Antioxidants Supplementation Reduces Ceramide Synthesis Improving the Cardiac Insulin Transduction Pathway in a Rodent Model of Obesity. Nutrients. 2021, 13, 3413. [CrossRef]
- Adamy C, Mulder P, Khouzami L, Andrieu-abadie N, Defer N, Candiani G, et al. Neutral sphingomyelinase inhibition participates to the benefits of N-acetylcysteine treatment in post-myocardial infarction failing heart rats. Journal of Molecular and Cellular Cardiology. 2007, 43, 344–353. [CrossRef]
- Bourraindeloup M, Adamy C, Candiani G, Cailleret M, Bourin M, Badoual T, et al. N-acetylcysteine treatment normalizes serum tumor necrosis factor-alpha level and hinders the progression of cardiac injury in hypertensive rats. Circulation. 2004, 110, 2003–2009. [CrossRef]
- Liu B, Andrieu-Abadie N, Levade T, Zhang P, Obeid LM, Hannun YA. Glutathione regulation of neutral sphingomyelinase in tumor necrosis factor-alpha-induced cell death. The Journal of Biological Chemistry. 1998, 273, 11313–11320. [CrossRef]
- Liu B, Hannun YA. Inhibition of the neutral magnesium-dependent sphingomyelinase by glutathione. The Journal of Biological Chemistry. 1997, 272, 16281–16287. [CrossRef]
- Yang G, Badeanlou L, Bielawski J, Roberts AJ, Hannun YA, Samad F. Central role of ceramide biosynthesis in body weight regulation, energy metabolism, and the metabolic syndrome. American Journal of Physiology - Endocrinology and Metabolism. 2009, 297, E211–E224, Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2711669/ (accessed on 4 January 2024). [CrossRef]
- Ussher JR, Koves TR, Cadete VJJ, Zhang L, Jaswal JS, Swyrd SJ, et al. Inhibition of de novo ceramide synthesis reverses diet-induced insulin resistance and enhances whole-body oxygen consumption. Diabetes. 2010, 59, 2453–2464. [CrossRef]
- Park T, Panek RL, Mueller SB, Hanselman JC, Rosebury WS, Robertson AW, et al. Inhibition of sphingomyelin synthesis reduces atherogenesis in apolipoprotein E-knockout mice. Circulation. 2004, 110, 3465–3471. [CrossRef]
- Park T, Rosebury W, Kindt EK, Kowala MC, Panek RL. Serine palmitoyltransferase inhibitor myriocin induces the regression of atherosclerotic plaques in hyperlipidemic ApoE-deficient mice. Pharmacological Research. 2008, 58, 45–51. [CrossRef]
- Cantalupo A, Zhang Y, Kothiya M, Galvani S, Obinata H, Bucci M, et al. Nogo-B regulates endothelial sphingolipid homeostasis to control vascular function and blood pressure. Nature Medicine. 2015, 21, 1028–1037. [CrossRef]
- Hojjati MR, Li Z, Zhou H, Tang S, Huan C, Ooi E, et al. Effect of myriocin on plasma sphingolipid metabolism and atherosclerosis in apoE-deficient mice. The Journal of Biological Chemistry. 2005, 280, 10284–10289. [CrossRef]
- Ji R, Akashi H, Drosatos K, Liao X, Jiang H, Kennel PJ, et al. Increased de novo ceramide synthesis and accumulation in failing myocardium. JCI Insight. 2, e82922. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5414571/ (accessed on 16 June 2024). [CrossRef]
- Józefczuk E, Nosalski R, Saju B, Crespo E, Szczepaniak P, Guzik TJ, et al. Cardiovascular Effects of Pharmacological Targeting of Sphingosine Kinase 1. Hypertension (Dallas, Tex. : 1979). 2020, 75, 383–392, Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7055939/ (accessed on 17 October 2023). [CrossRef]
- Meissner A, Miro F, Jiménez-Altayó F, Jurado A, Vila E, Planas AM. Sphingosine-1-phosphate signalling-a key player in the pathogenesis of Angiotensin II-induced hypertension. Cardiovascular Research. 2017, 113, 123–133. [CrossRef]
- Chatterjee S, Bedja D, Mishra S, Amuzie C, Avolio A, Kass DA, et al. Inhibition of glycosphingolipid synthesis ameliorates atherosclerosis and arterial stiffness in apolipoprotein E-/- mice and rabbits fed a high-fat and -cholesterol diet. Circulation. 2014, 129, 2403–2413. [CrossRef]
- Mishra S, Bedja D, Amuzie C, Avolio A, Chatterjee S. Prevention of cardiac hypertrophy by the use of a glycosphingolipid synthesis inhibitor in ApoE-/- mice. Biochemical and Biophysical Research Communications. 2015, 465, 159–164. [CrossRef]
- Mishra S, Bedja D, Amuzie C, Foss CA, Pomper MG, Bhattacharya R, et al. Improved intervention of atherosclerosis and cardiac hypertrophy through biodegradable polymer-encapsulated delivery of glycosphingolipid inhibitor. Biomaterials. 2015, 64, 125–135. [CrossRef]
- Chatterjee S, Zheng L, Ma S, Bedja D, Bandaru VVR, Kim G, et al. Management of metabolic syndrome and reduction in body weight in type II diabetic mice by inhibiting glycosphingolipid synthesis. Biochemical and Biophysical Research Communications. 2020, 525, 455–461. [CrossRef]
- Bhunia AK, Han H, Snowden A, Chatterjee S. Redox-regulated signaling by lactosylceramide in the proliferation of human aortic smooth muscle cells. The Journal of Biological Chemistry. 1997, 272, 15642–15649. [CrossRef]
- Yang Q, Graham TE, Mody N, Preitner F, Peroni OD, Zabolotny JM, et al. Serum retinol binding protein 4 contributes to insulin resistance in obesity and type 2 diabetes. Nature. 2005, 436, 356–362. [CrossRef]
- Thompson D, Mahmood S, Morrice N, Kamli-Salino S, Dekeryte R, Hoffmann PA, et al. Fenretinide inhibits obesity and fatty liver disease but induces Smpd3 to increase serum ceramides and worsen atherosclerosis in LDLR-/- mice. Scientific Reports. 2023, 13, 3937. [CrossRef]
- Koh I, Jun H, Choi JS, Lim JH, Kim WH, Yoon JB, et al. Fenretinide ameliorates insulin resistance and fatty liver in obese mice. Biological & Pharmaceutical Bulletin. 2012, 35, 369–375. [CrossRef]
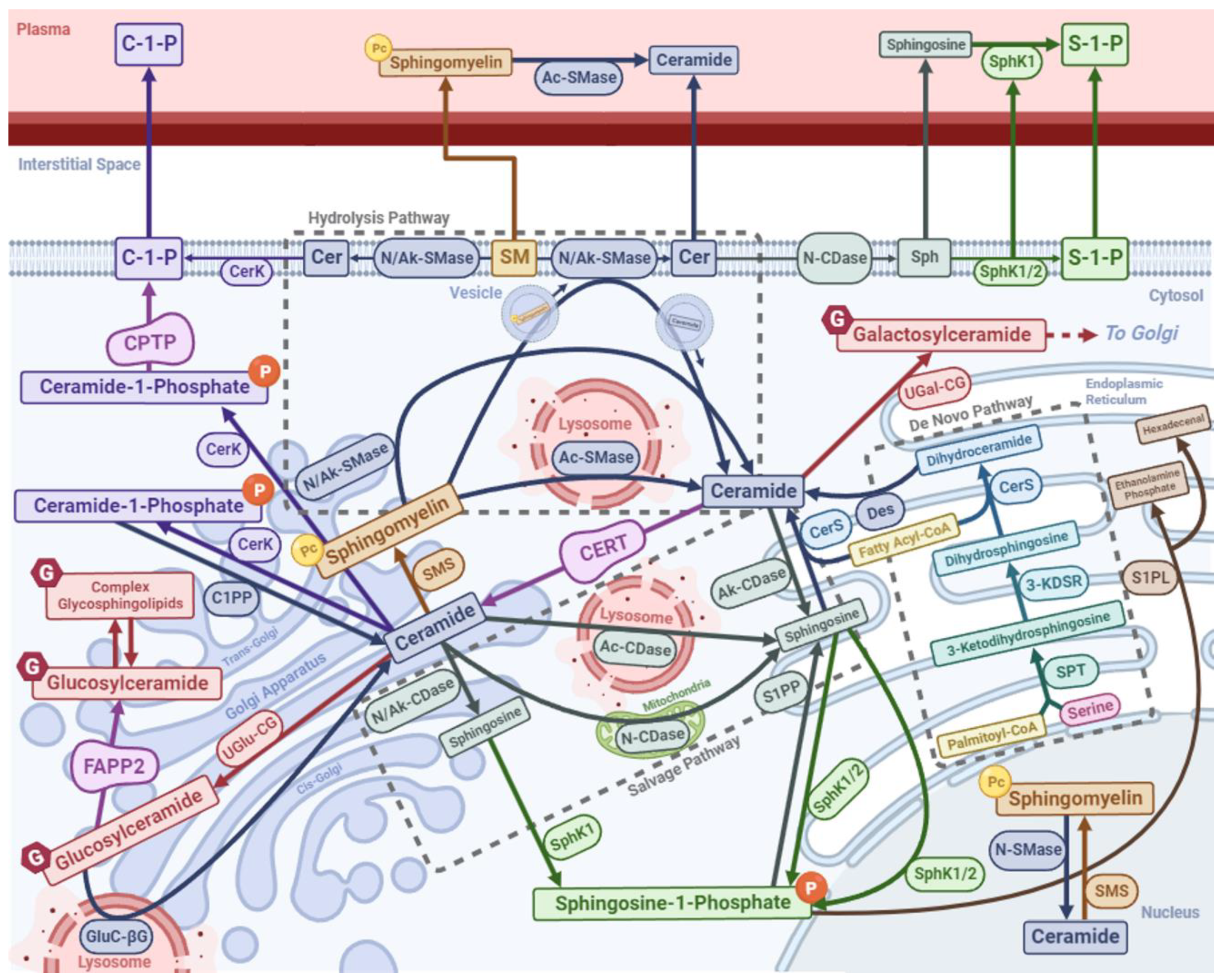
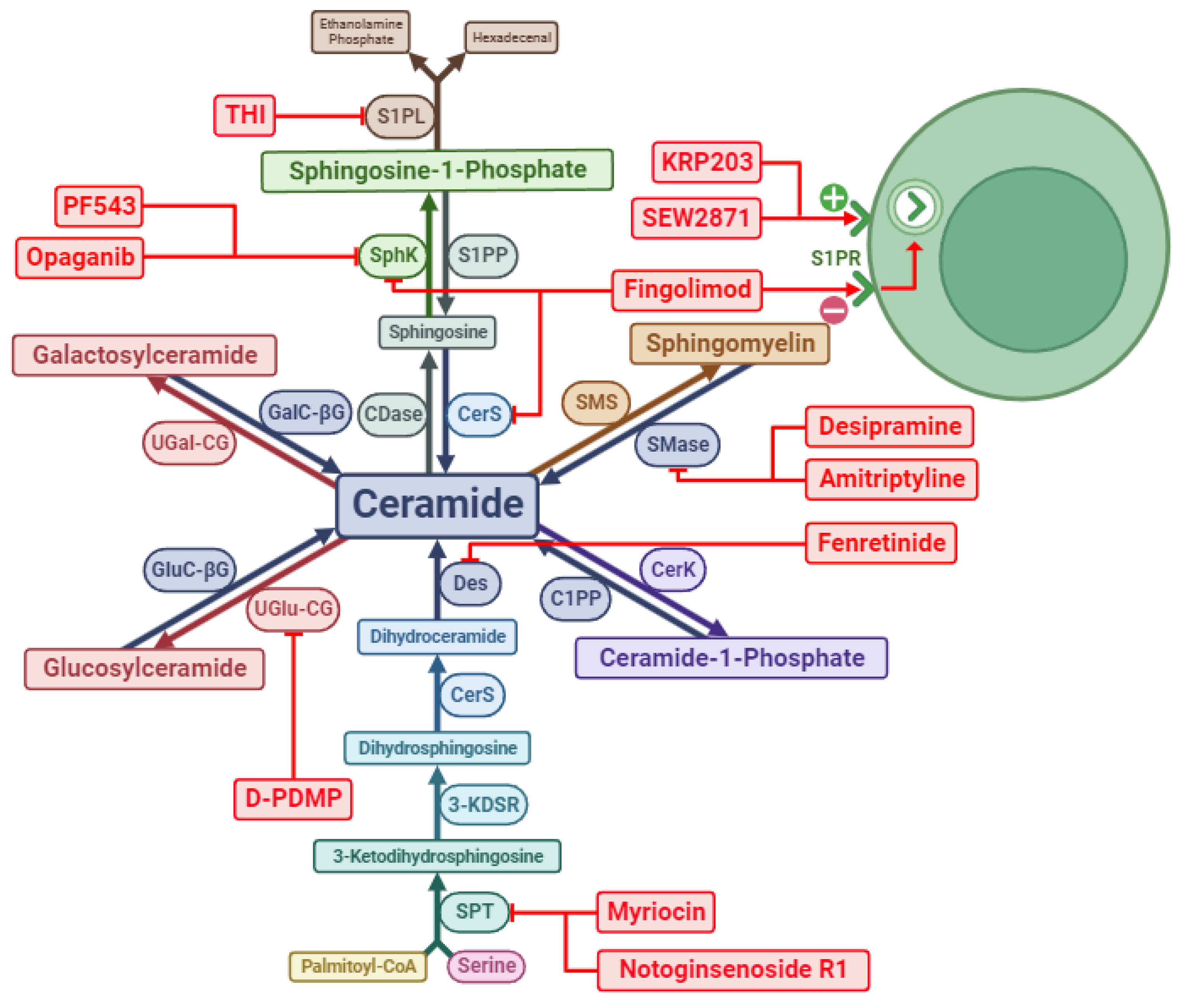
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).




