Submitted:
21 July 2024
Posted:
23 July 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
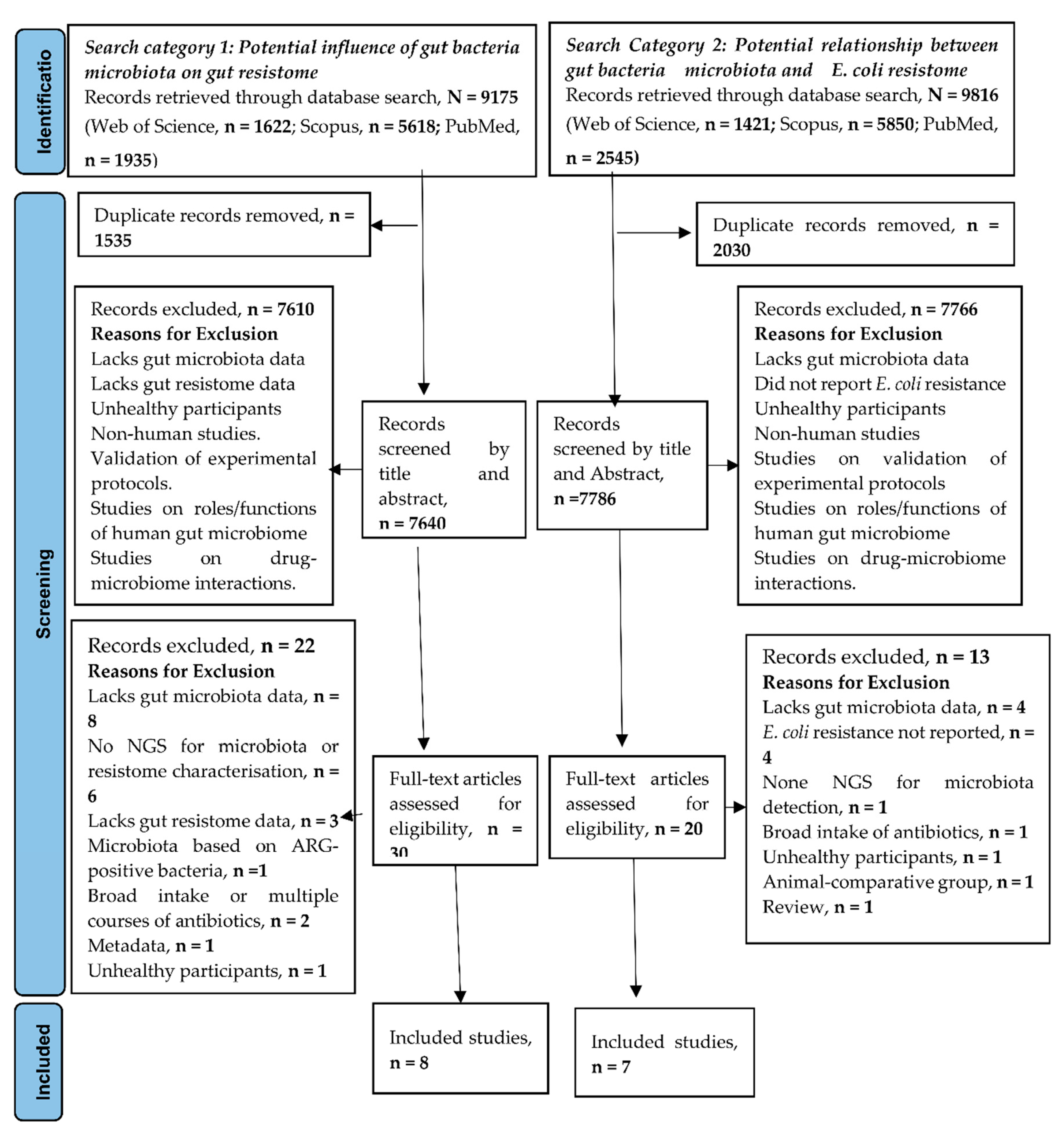
2. Methodology
2.1. Search Strategy
2.2. Selection of Studies
2.3. Data Extraction and Synthesis
2.4. Outcome Measures
2.5. Risk of Assessment Bias and Critical Appraisal of Eligible Studies
3. Results
3.1. Characteristics of Studies Included in the Analysis
| S/N | Country of Study | Study Design | Study Objective/Hypothesis | Age of Participant and Study Time Points | Sample Size | DNA Extraction and Quantification | Sequencing Technology and Platform | Database and Bioinformatic Pipelines for Microbiota and ARG Detection | Reference | |
|---|---|---|---|---|---|---|---|---|---|---|
| 1ab | Norway | Longitudinal | Determine resistome and mobilome across gestational ages and microbiota-modifying treatment. | 7days, 28days, 120days, 365days. |
10 | NorDiag Arrow Stool DNA Extraction kit (+bead beating) Qubit +nanodrop |
Shotgun Illumina Miseq |
Bowtie 2 MetaPhlAn3 (based on CHOCOPhlAn) MetaSPAdes and MetaQUAST (from QUAST) ShortBRED based on CARD NanoARG HUMAnN |
[26] | |
| 2ab | USA | Longitudinal | Determine factors associated with early life resistome development. | 6weeks & 1year. | 195 | Fecal DNA extraction kit Qubit |
Shotgun | MetaPhlAn PanPhlAn HUMANn2 ShotBRED based on CARD |
[27] | |
| 3ab | USA | Longitudinal | Determine potential sources of infant and maternal ARGs. | Mother-child 1month, 6months. |
10 | InviMag® Stool DNA Kit Qubit, Nanodrop |
Shotgun Illumina NextSeq |
Bowtie2 MetaPhlan2 CARD RestFinder PlasmidFinder |
[28] | |
| 4ab | Denmark | Longitudinal | Characterise the ARGs acquired during the first year of life and assess the impacts of diverse environmental exposures on ARG load. | 1 year 1 week 1 month 1 year 4 years 5 years |
|
662- shotgun 660-16S rRNA |
PowerMagSoil DNA isolation kit | Shotgun Illumina NovaSeq 16SrRNA sequencing- Illumina Miseq |
SPAdes Humann2 MetaPhlAn MetaWRAP MetaBAT2 Bowtie2 QllME2 CARD |
[29] |
| 5a | China | Longitudinal | To understand the characteristics of the gut microbial composition | 18-69 years (Mean= 28.6) |
7 followed for 1 year (12 time points) | QIAamp Fast DNA stool minikit |
Shotgun Illumina HiSeq |
HUMAnN3, UniRef 90, KEGG, Kraken2.0, ResFinder and SPAdes | [30] | |
| 6a | Vietnam | Cross-sectional | Healthy human gut in Vietnam is a source of ARGs transferable to gut pathogens. | 0-23months 2-5years > 18yrs, |
42 | FastDNA soil kit | Shotgun Illumina |
Bowtie2 Kraken2 Bracken ARGANNOT database |
[31] | |
| 7a | USA | Cross-sectional | To characterise the microbiome and resistome of dairy workers | Mean age dairy workers, 38.4 community controls, 49.5 |
16(10 dairy workers and 6 nondairy workers | MoBio DNeasy PowerLyzer PowerSoil Kit | Shotgun Illunina HiSeq |
MetaPhlAn3, ChocoPhlAn, Anvio, Centrifuge, MEGAHIT, ABRicate, MetaCherchant, Kraken2, CARD | [32] | |
| 8a | China | Cross-sectional. | Determine antibiotic resistome shared between chicken farms and Life poultry markets workers and those with no contact with life poultry markets. | NR | 36 (18 life poultry market workers & 18 non-workers) | DNeasy PowerSoil Pro Kit agarose gel electrophoresis Qubit dsDNA assay kit |
Shotgun Illumina NovaSeq PE150. |
MEGAHIT MetaGeneMark MetaPhlAn2 CARD, ResFinder |
[33] | |
| 9b | Malaysia | Cross-sectional | Profile the gut resistome of Malaysians and investigate its association with demographic and lifestyle variables. | ≤ 90 yrs Lower boundary NR |
200 | QIAamp PowerFecal Pro DNA Kit | Shotgun Illumina NovaSeq |
BioBakery3 KneadData MetaPhlAn3 ARGs-OAP |
[34] | |
| 10b | USA | Cross-sectional | Characterise fecal, oral, and skin bacterial microbiome and resistome of the Yanomami Amerindians with no previous contact with Western people. | 4- 50yrs old | 12 | Powersoil DNA isolation kit | V4 region of the 16SrRNA Illumina HiSeq |
PICRUSt STAMP KEGG CONCOCT PARFuMS Resfams |
[35] | |
| 11b | Saudi Arabia | Cross-sectional | To assess pregnancy induced gut microbiome composition and antimicrobial resistome in Saudi females. | Mean age NP 39.1±7.7 First trimester 25.4±4.1 Third trimester 33.3±7.3 |
24 (8 NP 8 first trimester 8 third trimester) |
QIAamp Fast DNA Stool Mini Kit | 16S rRNA Illumina MiSeq |
NR | [36] | |
3.2. The Potential Influence of the Gut Microbiome on Gut Resistome
3.3. The Potential Association between Gut Microbiota and E. coli Resistome
4. Discussion
4.1. Conclusion and Future Directives
4.1. Strengths and Limitations of the Study
Author Contributions
Funding
Data availability statement
Acknowledgments
Conflicts of Interest
References
- World Health Organisation. Antibiotic resistance. WHO, 2023a. Available online: https://www.who.int/news-room/fact-sheets/detail/antibioticresistance#:~:text=Bacteria%2C%20not%20humans%20or%20animals,hospital%20stays%2C%20and%20increased%20mortality (accessed on 18 September 2023).
- World Health Organisation. Proportion of bloodstream infection due to Escherichia coli resistant to third generation cephalosporins. WHO, 2023b. Available online: https://www.who.int/data/gho/data/indicators/indicator-details/GHO/sdg-3.d.2--proportion-of-bloodstream-infections-due-to-selected-antimicrobial-resistant-organisms--median- (accessed on 3 November 2023).
- The United Nations. The Sustainable Development Goal Report, 2023. UN 2023. Available online: https://unstats.un.org/sdgs/report/2023/The-Sustainable-Development-Goals-Report-2023.pdf. (accessed on 3 November 2023).
- Million, M.; Diallo, A.; and Raoult, D. Gut microbiota and malnutrition. Microb pathog 2017, 106, 127–138. [Google Scholar] [CrossRef] [PubMed]
- Nath, A.; Bhattacharjee, R.; Nandi, A.; Sinha, A.; Kar, S.; Manoharan, N.; Mitra, S.; Mojumdar, A.; Panda, P.K.; Patro, S.; Dutt, A. Phage delivered CRISPR-Cas system to combat multidrug-resistant pathogens in gut microbiome. Biomed. Pharmacother. 2022, 151, 113122. [Google Scholar] [CrossRef] [PubMed]
- Priadko, K.; Romano, L.; Olivieri, S.; Romeo, M.; Barone, B.; Sciorio, C.; Spirito, L.; Morelli, M.; Crocetto, F.; Arcaniolo, D.; Mirone, V. Intestinal microbiota, intestinal permeability and the urogenital tract: is there a pathophysiological link? J. Physiol. Pharmacol 2022, 73. [Google Scholar]
- Moore, A.M.; Patel, S.; Forsberg, K.J.; Wang, B.; Bentley, G.; Razia, Y.; Qin, X.; Tarr, P.I.; Dantas, G. Pediatric fecal microbiota harbor diverse and novel antibiotic resistance genes. PloS one 2013, 8, e78822. [Google Scholar] [CrossRef] [PubMed]
- Purkait, D.; Hameed, S.; Fatima, Z. Gut microbiome: Current development, challenges, and perspectives. New and Future Developments in Microbial Biotechnology and Bioengineering, Gupta V.K Ed. Elsevier: Amsterdam, Netherlands, 2020; pp.227-241.
- Penders, J.; Stobberingh, E.E.; Savelkoul, P.H.; Wolffs, P.F. The human microbiome as a reservoir of antimicrobial resistance. Front. in Microbiol. 2013, 4, 87. [Google Scholar] [CrossRef] [PubMed]
- von Wintersdorff, C.J.; Wolffs, P.F.; van Niekerk, J.M.; Beuken, E.; van Alphen, L.B.; Stobberingh, E.E.; Oude Lashof, A.M.; Hoebe, C.J.; Savelkoul, P.H.; Penders, J. Detection of the plasmid-mediated colistin-resistance gene mcr-1 in faecal metagenomes of Dutch travellers. J. Antimicrob. Chemother. 2016, 71, 3416–3419. [Google Scholar] [CrossRef] [PubMed]
- Jiang, X.; Ellabaan, M.M.H.; Charusanti, P.; Munck, C.; Blin, K.; Tong, Y.; Weber, T.; Sommer, M.O.A.; Lee, S.Y. Dissemination of antibiotic resistance genes from antibiotic producers to pathogens. Nat. Commun 2017, 8, 15784. [Google Scholar] [CrossRef] [PubMed]
- DeFrancesco, A.S.; Tanih, N.F.; Samie, A.; Guerrant, R.L.; Bessong, P.O. Antibiotic resistance patterns and beta-lactamase identification in Escherichia coli isolated from young children in rural Limpopo Province, South Africa: The MAL-ED cohort. S. Afr. Med. J. 2017, 107, 205–214. [Google Scholar] [CrossRef] [PubMed]
- Feng, J.; Li, B.; Jiang, X.; Yang, Y.; Wells, G.F.; Zhang, T.; Li, X. Antibiotic resistome in a large-scale healthy human gut microbiota deciphered by metagenomic and network analyses. Environ. Microbiol. 2018, 20, 355–368. [Google Scholar] [CrossRef] [PubMed]
- Gasparrini, A.J.; Wang, B.; Sun, X.; Kennedy, E.A.; Hernandez-Leyva, A.; Ndao, I.M.; Tarr, P.I.; Warner, B.B.; Dantas, G. Persistent metagenomic signatures of early-life hospitalisation and antibiotic treatment in the infant gut microbiota and resistome. Nat. Microbiol. 2019, 4, 2285–2297. [Google Scholar] [CrossRef]
- Chong, C.W.; Alkatheeri, A.H.S.; Ali, N.; Tay, Z.H.; Lee, Y.L.; Paramasivam, S.J.; Jeevaratnam, K.; Low, W.Y.; Lim, S.H.E. Association of antimicrobial resistance and gut microbiota composition in human and non-human primates at an urban ecotourism site. Gut pathogens 2020, 12, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Carvalho, M.J.; Sands, K.; Thomson, K.; Portal, E.; Mathias, J.; Milton, R.; Gillespie, D.; Dyer, C.; Akpulu, C.; Boostrom, I.; Hogan, P. Antibiotic resistance genes in the gut microbiota of mothers and linked neonates with or without sepsis from low-and middle-income countries. Nat. Microbiol. 2022, 7, 1337–1347. [Google Scholar] [CrossRef] [PubMed]
- Narayan, S.; Nayak, A.; King, C. L. Inflammatory pseudotumor of the liver with Escherichia coli in the sputum. Case Reports in Medicine 2015, 1, 249210. [Google Scholar]
- Kobayashi, T.; Ikeda, M.; Okada, Y.; Higurashi, Y.; Okugawa, S.; Moriya, K. Clinical and microbiological characteristics of recurrent Escherichia coli bacteremia. Microbiol. Spectr. 2021, 9, e01399–21. [Google Scholar] [CrossRef] [PubMed]
- Geurtsen, J.; de Been, M.; Weerdenburg, E.; Zomer, A.; McNally, A.; Poolman, J. Genomics and pathotypes of the many faces of Escherichia coli. FEMS Microbiol. Rev. 2022, 46, fuac031. [Google Scholar] [CrossRef] [PubMed]
- Mohsin, A.S.; Alsakini, A.H.; Ali, M.R. Outbreak of drug resistance Escherichia coli phylogenetic F group associated urinary tract infection. Iran J Microbiol 2022, 14, 341–350. [Google Scholar] [CrossRef] [PubMed]
- Abdullah, R.N.; Juboory, Y.H.O.; Noomi, B.S. Antibiotic Susceptibility Profile and Virulence Factors Profile of E. coli Isolated from Otitis Media. Ann. Romanian Soc. Cell Biol. 2023, 27, 105–111. [Google Scholar]
- Ryan (2023). Escherichia coli (E. coli) Infections Medication. MedScape, Drugs and diseases. Available online: https://emedicine.medscape.com/article/217485-medication?form=fpf. (accessed on 3 June 2023).
- Campbell, T.P.; Sun, X.; Patel, V.H.; Sanz, C.; Morgan, D.; Dantas, G. The microbiome and resistome of chimpanzees, gorillas, and humans across host lifestyle and geography. The ISME journal 2020, 14, 1584–1599. [Google Scholar] [CrossRef] [PubMed]
- Melo, R.T.; Oliveira, R.P.; Silva, B.F.; Monteiro, G.P.; Saut, J..PE., Costa, L.R.M., Dias, S.D.C., Rossi, D.A. Phylogeny and Virulence Factors of Escherichia coli Isolated from Dogs with Pyometra. Vet Sci, 2022, 9,158.
- Sajeev, S.; Hamza, M.; Rajan, V.; Vijayan, A.; Sivaraman, G.K.; Shome, B.R.; Holmes, M.A. Resistance profiles and genotyping of extended-spectrum beta-lactamase (ESBL)-producing and non-ESBL-producing E. coli and Klebsiella from retail market fishes. Infect. Genet. Evol. 2023, 112, 105446. [Google Scholar] [CrossRef] [PubMed]
- Bargheet, A.; Klingenberg, C.; Esaiassen, E.; Hjerde, E.; Cavanagh, J.P.; Bengtsson-Palme, J.; Pettersen, V.K. Development of early life gut resistome and mobilome across gestational ages and microbiota-modifying treatments. EBioMedicine 2023, 92. [Google Scholar] [CrossRef] [PubMed]
- Lebeaux, R.M.; Coker, M.O.; Dade, E.F.; Palys, T.J.; Morrison, H.G.; Ross, B.D.; Baker, E.R.; Karagas, M.R.; Madan, J.C.; Hoen, A.G. The infant gut resistome is associated with E. coli and early-life exposures. BMC Microbiol. 2021, 21, 201. [Google Scholar] [CrossRef] [PubMed]
- Pärnänen, K.; Karkman, A.; Hultman, J.; Lyra, C.; Bengtsson-Palme, J.; Larsson, D.J.; Rautava, S.; Isolauri, E.; Salminen, S.; Kumar, H.; Satokari, R. Maternal gut and breast milk microbiota affect infant gut antibiotic resistome and mobile genetic elements. Nat. commun. 2018, 9, 3891. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Stokholm, J.; Brejnrod, A.; Vestergaard, G.A.; Russel, J.; Trivedi, U.; Thorsen, J.; Gupta, S.; Hjelmsø, M.H.; Shah, S.A.; Rasmussen, M.A. The infant gut resistome associates with E. coli, environmental exposures, gut microbiome maturity, and asthma-associated bacterial composition. Cell Host & Microbe 2021, 29, 975–987. [Google Scholar]
- Zhang, W.; Han, N.; Zhang, T.; Qiang, Y.; Peng, X.; Li, X.; Kan, B. The spatial features and temporalchanges in the gut microbiota of a healthy Chinese population. Microbiol. Spectr. 2022, 10, pp.e01310-22.
- Pereira-Dias, J.; Nguyen Ngoc Minh, C.; Tran Thi Hong, C.; Nguyen Thi Nguyen, T.; Ha Thanh, T.; Zellmer, C.; Chung The, H.; Pike, L.; Higginson, E.E.; Baker, S. The gut microbiome of healthy Vietnamese adults and children is a major reservoir for resistance genes against critical antimicrobials. J. Infect. Dis. 2021, 224 (Supplement_7), S840–S847. [Google Scholar] [CrossRef] [PubMed]
- Trinh, P.; Roberts, M.C.; Rabinowitz, P.M.; Willis, A.D. Differences in gut metagenomes between dairy workers and community controls: a cross-sectional study. bioRxiv. 2023 (Preprint).
- Wang, Y.; Lyu, N.; Liu, F.; Liu, W.J.; Bi, Y.; Zhang, Z.; Ma, S.; Cao, J.; Song, X.; Wang, A.; Zhang, G. More diversified antibiotic resistance genes in chickens and workers of the live poultry markets. Environ. Int. 2021, 153, 106534. [Google Scholar] [CrossRef] [PubMed]
- Dwiyanto, J.; Huët, M.A.L.; Hussain, M.H.; Su, T.T.; Tan, J.B.L.; Toh, K.Y.; Lee, J.W.J.; Rahman, S.; Chong, C.W. Social demographics determinants for resistome and microbiome variation of a multiethnic community in Southern Malaysia. npj Biofilms and Microbiomes 2023, 9, 55. [Google Scholar] [CrossRef]
- Clemente, J.C.; Pehrsson, E.C.; Blaser, M.J.; Sandhu, K.; Gao, Z.; Wang, B.; Magris, M.; Hidalgo, G.; Contreras, M.; Noya-Alarcón, Ó.; Lander, O. The microbiome of uncontacted Amerindians. Sci. Adv. 2015, 1, e1500183. [Google Scholar] [CrossRef] [PubMed]
- Khan, I.; Yasir, M.; Farman, M.; Kumosani, T.; AlBasri, S.F.; Bajouh, O.S.; Azhar, E.I. Evaluation of gut bacterial community composition and antimicrobial resistome in pregnant and non-pregnant women from Saudi population. Infect. drug Res. 2019, pp.1749-1761.
- Arumugam, M.; Raes, J.; Pelletier, E.; Le Paslier, D.; Yamada, T.; Mende, D.R.; Fernandes, G.R.; Tap, J.; Bruls, T.; Batto, J.M.; Bertalan, M. Enterotypes of the human gut microbiome. Nature 2011, 473, 174–180. [Google Scholar] [CrossRef] [PubMed]
- Siezen, R.J.; Kleerebezem, M. The human gut microbiome: are we our enterotypes? Microb. Biotechnol. 2011, 4, 550. [Google Scholar] [CrossRef]
- Lozupone, C.A, Stombaugh, J.I, Gordon, J.I, Jansson, J.K.; Knight, R. Diversity, stability and resilience of the human gut microbiota. Nature 2012, 489, 220-30.
- Shin, N.R.; Whon, T.W.; Bae, J.W. Proteobacteria: microbial signature of dysbiosis in gut microbiota. Trends Biotechnol. 2015, 33, 496–503. [Google Scholar] [CrossRef] [PubMed]
- Jiang, X.; Ellabaan, M.M.H.; Charusanti, P.; Munck, C.; Blin, K.; Tong, Y.; Weber, T.; Sommer, M.O.A.; Lee, S.Y. Dissemination of antibiotic resistance genes from antibiotic producers to pathogens. Nat. Commun 2017, 8, 15784. [Google Scholar] [CrossRef] [PubMed]
- Murray, C.J.; Ikuta, K.S.; Sharara, F.; Swetschinski, L.; Aguilar, G.R.; Gray, A.; Han, C.; Bisignano, C.; Rao, P.; Wool, E.; Johnson, S.C. Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis. The Lancet 2022, 399, 629–655. [Google Scholar] [CrossRef] [PubMed]
- Hu, Y.; Yang, X.; Lu, N.; Zhu, B. The abundance of antibiotic resistance genes in human guts has correlation to the consumption of antibiotics in animal. Gut microbes 2014, 5, 245–249. [Google Scholar] [CrossRef] [PubMed]
- Afridi, O.K.; Ali, J.; Chang, J.H. Fecal microbiome and Resistome profiling of healthy and diseased Pakistani individuals using next-generation sequencing. Microorganisms 2021, 9, 616. [Google Scholar] [CrossRef] [PubMed]
- Eckburg, P. B.; Bik, E. M.; Bernstein, C. N.; Purdom, E.; Dethlefsen, L.; Sargent, M.; Gill, S.R.; Nelson, K.E.; Relman, D. A. Diversity of the human intestinal microbial flora. Science 2005, 308, 1635–1638. [Google Scholar] [CrossRef] [PubMed]
- Sun, S.; Luo, L.; Liang, W.; Yin, Q.; Guo, J.; Rush, A.M.; Lv, Z.; Liang, Q.; Fischbach, M.A.; Sonnenburg, J.L.; Dodd, D. Bifidobacterium alters the gut microbiota and modulates the functional metabolism of T regulatory cells in the context of immune checkpoint blockade. PNAS 2020, 117, 27509–27515. [Google Scholar] [CrossRef] [PubMed]
- Mitsuoka, T. Bifidobacteria and their role in human health. J. Ind. Microbiol. 1990, 6, 263–267. [Google Scholar] [CrossRef]
- Gagnon, M.; Kheadr, E.E.; Le Blay, G.; Fliss, I. In vitro inhibition of Escherichia coli O157: H7 by bifidobacterial strains of human origin. nt. J. Food Microbiol 2004, 92, 69–78. [Google Scholar] [CrossRef] [PubMed]
- Piddock, L.J. Clinically relevant chromosomally encoded multidrug resistance efflux pumps in bacteria. Clin. Microbiol. Rev. 2006, 19, 382–402. [Google Scholar] [CrossRef] [PubMed]
- Nishino, K.; Yamasaki, S.; Nakashima, R.; Zwama, M.; Hayashi-Nishino, M. Function and inhibitory mechanisms of multidrug efflux pumps. Front. Microbiol. 2021, 12, 737288. [Google Scholar] [CrossRef] [PubMed]
- Nuonming, P.; Khemthong, S.; Dokpikul, T.; Sukchawalit, R.; Mongkolsuk, S. Characterization and regulation of AcrABR, a RND-type multidrug efflux system, in Agrobacterium tumefaciens C58. Microbiol. Res. 2018, 214, 146–155. [Google Scholar] [CrossRef] [PubMed]
- World Health Organisation. Global research agenda for antimicrobial resistance in human health. Policy brief. June 2023. WHO 2023c. Available online: https://cdn.who.int/media/docs/default-source/antimicrobial-resistance/amr-spc-npm/who-global-research-agenda-for-amr-in-human-health---policy-brief.pdf?sfvrsn=f86aa073_4&download=true (accessed on 4 November 2023).
- Barba, M.; Czosnek, H.; Hadidi, A. Historical perspective, development and applications of next-generation sequencing in plant virology. Viruses 2014, 6, 106–136. [Google Scholar] [CrossRef] [PubMed]
- Marchant, J. When antibiotics turn toxic. Nature 2018, 555, 431–433. [Google Scholar] [CrossRef]
- Naylor, N.R.; Pouwels, K.B.; Hope, R.; Green, N.; Henderson, K.L.; Knight, G.M.; Atun, R.; Robotham, J.V.; Deeny, S.R. The health and cost burden of antibiotic resistant and susceptible Escherichia coli bacteraemia in the English hospital setting: A national retrospective cohort study. PloS one 2019, 14, e0221944. [Google Scholar] [CrossRef] [PubMed]
- Peters, L.; Olson, L.; Khu, D.T.; Linnros, S.; Le, N.K.; Hanberger, H.; Hoang, N.T.; Tran, D.M.; Larsson, M. Multiple antibiotic resistance as a risk factor for mortality and prolonged hospital stay: a cohort study among neonatal intensive care patients with hospital-acquired infections caused by gram-negative bacteria in Vietnam. PloS one, 2019, 14, e0215666. [Google Scholar] [CrossRef]
- Collado, M.C., Gueimonde, M. and Salminen, S. Probiotics in adhesion of pathogens: mechanisms of action. In Bioactive foods in promoting health Academic Press. 2010, 353–370.
- Bermudez-Brito, M.; Plaza-Díaz, J.; Muñoz-Quezada, S.; Gómez-Llorente,, C.; Gil, A. Probiotic mechanisms of action. Annals of Nutrition and Metabolism, 2012, 61, 160–174. [Google Scholar] [CrossRef] [PubMed]
- Elshaghabee, F.M. and Rokana, N., 2021. Dietary management by probiotics, prebiotics and synbiotics for the prevention of antimicrobial resistance. Sustainable Agriculture Reviews 49: Mitigation of Antimicrobial Resistance Vol 2. Natural and Synthetic Approaches, pp.33-56.
- Nataraj, B.H. and Mallappa, R.H., 2021. Antibiotic resistance crisis: an update on antagonistic interactions between probiotics and methicillin-resistant staphylococcus aureus (MRSA). Current microbiology, 78(6), pp.2194-2211.
- Mazziotta, C., Tognon, M., Martini, F., Torreggiani, E. and Rotondo, J.C., 2023. Probiotics mechanism of action on immune cells and beneficial effects on human health. Cells, 12(1), p.184.
- Pot, B. and Vandenplas, Y., 2021. Factors that influence clinical efficacy of live biotherapeutic products. European Journal of Medical Research, 26(1), pp.1-10.
| Groups | Metric | Microbiota Diversity | Taxonomic Abundance | ARGs Diversity | ARG Abundance | Significant Associations and Prediction between Microbiota and Resistome | Other Comments | Ref. |
|---|---|---|---|---|---|---|---|---|
| Full-term infants at 7 days, vs 28days, vs 120days, vs 365days |
α, Shannon Diversity |
lowest at 7 days and increases to 365 days. | Based on various time points, Bifidobacterium is highest at 28 days old > 120 > 7 > 365. Escherichia; 7 days > 120 > 28. Bacteroides: 365 days> lower time points. Klebsiella: highest in 7 days similar to 120days > 28days and least in 365days. |
NA | Higher ARGs of full-term infants at 28 days compared to 120 days. Median 7days > 28 days > 120 days. |
Escherichia coli was associated with the highest number of ARGs, followed by Klebsiella pneumoniae and Klebsiella aerogenes. |
[26] | |
| 6weeks vs 1yr | α, Shannon & Simpson | NR | NR | More even distribution of unique ARGs at 6 weeks, compared to 1-year samples, which were more dominated by one or two specific ARGs. | Higher | Positive correlation of compositional relative abundance of Proteobacteria with resistome composition Amongst the Proteobacteria, there was a strong positive correlation between E. coli relative abundance and resistome load. |
[27]. | |
| 0- 23m vs 2-5yrs | α, Shannon | Lower | Proteobacteria and Actinobacteria are > in children than adults. Bacteroides and Firmicutes A is > in adults than children. |
ARG encoding Tetracycline resistance had the greatest diversity. | Higher | NR | Although more diverse, there was a significant overlap of microbial signatures between 0-23 months and 2-5 years. |
[31] |
| 0- 23m vs > 18 | α, Shannon | lower | NR | Higher | ||||
| Infant 1month vs Mother and infant at 6month vs mother. |
α, Simpson | Lower diversity in infants than mothers. | Higher Gammaproteobacteria. Higher E. coli |
Higher | Higher in 1month infants compared to mother. Higher in 6 months infants compared to mother. |
Strong correlation between microbiome struc- ture and ARGs (r M, ≥ 0.5, p ≤ 0.001). Strong positive correlation between Gammaproteobacteria and resistome load. Strong positive correlation between E. coli and overall resistance gene load. E. coli was reliably indicated as the strongest predictor of ARGs in infants. Negative correlation between Bifidobacterium with resistance load. |
The most abundant ARGs in mothers and infants were those encoding tetracycline resistance. All resistant gene classes, except tetracycline, MLS and trimethoprim resistance, were more abundant in infants compared to mothers. |
[28] |
| NA | OTU richness For E. coli |
NR | Higher mean Relative abundance of E. coli from one week, lowering to 1yr | NR | Higher in the first year of life and lowers towards an equilibrium. | Higher in Proteobacteria. Higher in Enterobacteriaceae. Highest in E. coli |
Gut E. coli Abundance was associated with gut microbiome immaturity (High gut E. coli abundance was associated with low gut maturity and vice versa). |
[29] |
| 18-69 years olds chinese vs HMP data set |
α, Shannon | Higher | NR | NR | Higher (91% of total ARGs in were detected in Bacteriodetes, Proteobacteria and Firmicutes) |
. | Diffrence in gut microbiota were observed in samples from diffent region, location, individuals and time points. ARGs encoding tetracyclines were the most abundnant. ARGs encoding fosfomycin (9 genes) and quinolone ARGs (5 genes) were only identified in the Proteobacteria family. | [30] |
| Poultry vs. non-poultry workers |
α, Simpson | Lower | NR | Higher | Higher | LPM workers were enriched with beta-lactam and lincosamide resistance genes. Antibiotic inactivation mechanisms were higher in LPM workers. Microbiota of LPM workers was significantly different from the control group. |
[33] | |
| Dairy vs. non-dairy workers | α, Shannon | NR | No significant difference |
NR | Lower (probably due to lower sequencing depth in this group) |
Higher abundance of tetracycline and cephamycin genes in poultry workers. Evidence of commensal bacteria association with plasmid-mediated tetracycline resistance genes in both groups (including Faecalibacterium prausnitzii, Ligilactobacillus animalis, and Simiaoa sunii | [32] |
| Characteristics of the Group Considered | Microbiota Composition |
E. coli Resistome Profile | Comments | Ref. |
|---|---|---|---|---|
| 7-day old full-term infants |
Bifidobacterium breve* Bifidobacterium longum Escherichia coli Bifidobacterium bifidum Klebsiella pneumoniae Vellionella parvula Bacteroides dorei Klebsiella veriicola Bacteroides fragilis Enterococcus faecalis, Staphylococcus epidermis Klebsiella pneumoniae |
acrA acrD acrE acrF ampH bacA EC.15 emrA eptA evgA gadW gadX marA mdtE mdtF mdtG mdtH mdtO OmpA pmrF tolC yoji |
[26] | |
| 6weeks to 1year old healthy infants |
EF-Tu rpoB UhpT SoxR murA folP SoxS GlpT gyrB emrE acrR marR mdfA ompF nfSA |
The genes encode resistance to Pulvomycin Rifampicin Fosfomycin Sulfonamides Aminocoumarin Multidrug antibiotic resistance Nitrofurantoin Betalactams Resistome abundance was correlated with Proteobacteria (78.9%) and E. coli (62.2%) |
[27] | |
| 1 month and 6months olds | 1month Bifidobacterium* Escherichia Lactobacillus Bacteroides Streptococcus Staphylococcus Blautia 6months Bifidobacterium* Escherichia Blautia Bacteroides Lactobacillus Eubacterium Akkermansia Subdoligranulum |
E. coli was the highest predictor of ARG abundance | The strong correlation between the presence of E. coli and total ARG abundance in 1-month and six months olds | [28] |
| 1year – 5years |
Based on highest abundance of ARGs Escherichia coli Citrobacter werkmanii Klebsiella pneumoniae Enterobacter himalayensis Klebsiella oxytoca Citrobacter sp001037495 Enterobacter cloacae Bacteroides fragilis Bacteroides dorei Faecalibacterium prausnitzii Ruminococcus bromii Bifidobacterium longum Bifidobacterium breve Haemophilus parainfluenzae Morganella morganii Faecalicatena gnavus Tyzzerella nexilis Blautia wexlerae Ruminococcus bicirculans Flavonifractor plautii Veillonella seminalis Erysipelatoclostridium ramosum (Thomasclavelia ramosa) Agathobacter rectalis Staphylococcus epidermidis Collinsella sp003487125 Bifidobacterium pseudocatenulatum Bacteroides uniformis Bacteroides ovatus Bacteroides thetaiotaomicron Parabacteroides distasonis Alistipes putredinis Prevotella buccae |
68 out of 133 unique types of ARGs in Proteobacteria came from E. coli | Bacteria microbiota is based on the relative abundance of ARG-containing species. | [29] |
| ≤ 90 yrs |
20 most abundant Bifidobacterium adolescentis Prevotella copri Bifidobacterium longum Collinsella aerofaciens Bifidobacterium bifidum Eubacterium rectale Ruminococcus bromii Escherichia coli Bifidobacterium pseudocatenulatum Lactobacillus ruminis Faecalibacterium prausnitzii Blautia obeum Bacteroides vulgatus Bacteroides uniformis Fusicatenibacter saccharivorans Roseburia faecis Dorea longicatena Alistipes putredinis Blautia wexlerae Eubacterium hallii |
(not exclusive) mdfA emrE ampC ß-lactamase |
E. coli positively correlated with 36 ARGs. A strong association between E. coli and the Shannon resistome diversity |
[34] |
| 4-50yrs |
Prevotella* Ruminococcus Clostridaceae Bacteroides Succinovibrio Bacteroideles S24-7 Oscillospira Phascolarctobacterium Ruminobacter Desulfovibrio Helicobacter Oxalobacter formigenes |
Functional E. coli ARG detection ampC* mdfA bcr mdlB mdlA SoxS Classes Beta-lactam* ABC-transporter MFS -transporter AraC-family transcriptional regulator |
Antibiotics used for functional selection were Penicillin Piperacillin Piperacillin-tazobactam Cefotaxime Ceftazidime Cefepime Meropenem Aztreonam Chloramphenicol Tetracycline Tigecycline Gentamicin Ciprofloxacin Colistin |
[35] |
|
Non Pregnant (NP) Pregnant 1st-Trim (P1) Pregnant 3rd-Trim (P3) |
Based on 16S metagenomics Lower species diversity in pregnant compared to NP Phylum Bacteroidetes* Firmicutes Proteobacteria Actinobacteria Firmicutes* Bacteroidetes Proteobacteria Actinobacteria Firmicutes* Bacteroidetes Actinobacteria Proteobacteria |
E. coli was the most prevalent AR species E. coli isolates were resistant to Kanamycin Gentamicin Metronidazole Oxytetracycline Cycloserine Chloramphenicol Cefixime Trimethoprim/sulfamethoxazole Azithromycin Ampicillin Amoxicillin |
Majority of ARG containing species belonged to Proteobacteria in NP and Firmicutes in pregnant women. ARG rich families were Enterobacteriaceae, Enterococcaceae, and Streptococcaceae. |
[36] |
| Infant Groups | Adult-Dominated Group | ||
|---|---|---|---|
| 7-Day Old | 1 Month | 6 Months | < 11years (2%) 11-20years (22%) 20-90years (76%) |
| BifidobacteriumA | BifidobacteriumA | BifidobacteriumA | BifidobacteriumA |
| EscherichiaP | EscherichiaP | EscherichiaP | PrevotellaA |
| KlebsiellaP | LactobacillusF | BlautiaBa | CollinsellaB |
| VellionellaBa | BacteroidesB | BacteroidesB | EubacteriumF |
| BacteroidesB | StreptococcusF | LactobacillusF | RuminococcusF |
| EnterococcusF | StaphylococcusF | EubacteriumP | EscherichiaP |
| StaphylococcusF | BlautiaBa | AkkermansiaV | LactobacilluF |
| Antibiotic Class | ARGs |
|---|---|
| MDR-Efflux pump system |
acrA, acrD, acrE, acrF, acrR, mdfA ,mdtE, mdtF, mdtG, mdtH, mdtO, emrA, emrE mdfA, marA, marR, gadW, gadX, SoxS, SoxR, tolC, |
| Betalactam | ompA, ompF, ampH |
| Polypeptide | BacA, eptA, evgA, pmrF |
| Fosfomycins | murA, glpT, UhpT |
| Rifampicin | RpoB |
| Nitrofurans | nfSA |
| Aminocoumarins | GyrB |
| Beta-lactam | EC-15 |
| Folate pathway antagonists | FolP |
| Peptides | Yojl |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




