Submitted:
20 June 2024
Posted:
24 June 2024
You are already at the latest version
Abstract
Keywords:
Introduction
Methods
Case Series Presentation
Discussion
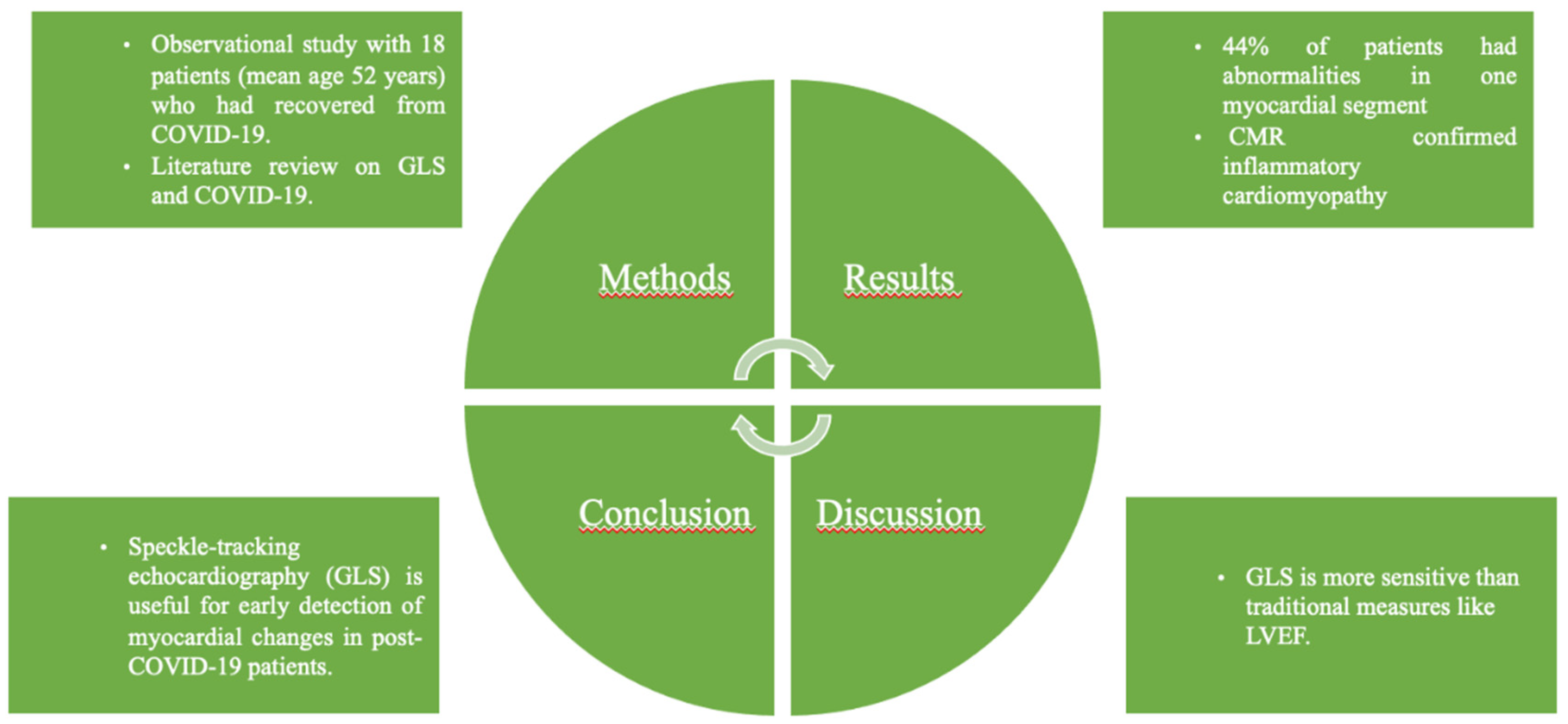
Conclusion
References
- Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, Zhao X, Huang B, Shi W, Lu R, Niu P. A novel coronavirus from patients with pneumonia in China, 2019. New England journal of medicine. 2020 Feb 20;382(8):727-33.
- Cucinotta D, Vanelli M. WHO declares COVID-19 a pandemic. Acta bio medica: Atenei parmensis. 2020;91(1):157.
- Cheng VC, Lau SK, Woo PC, Yuen KY. Severe acute respiratory syndrome coronavirus as an agent of emerging and reemerging infection. Clinical microbiology reviews. 2007 Oct;20(4):660-94.
- Zaki AM, Van Boheemen S, Bestebroer TM, Osterhaus AD, Fouchier RA. Isolation of a novel coronavirus from a man with pneumonia in Saudi Arabia. New England Journal of Medicine. 2012 Nov 8;367(19):1814-20.
- Anthony SJ, Johnson CK, Greig DJ, Kramer S, Che X, Wells H, Hicks AL, Joly DO, Wolfe ND, Daszak P, Karesh W. Global patterns in coronavirus diversity. Virus evolution. 2017 Jan;3(1):vex012.
- Sharma A, Ahmad Farouk I, Lal SK. COVID-19: a review on the novel coronavirus disease evolution, transmission, detection, control and prevention. Viruses. 2021 Jan 29;13(2):202.
- Ochani R, Asad A, Yasmin F, Shaikh S, Khalid H, Batra S, Sohail MR, Mahmood SF, Ochani R, Hussham Arshad M, Kumar A. COVID-19 pandemic: from origins to outcomes. A comprehensive review of viral pathogenesis, clinical manifestations, diagnostic evaluation, and management. Infez Med. 2021 Mar 1;29(1):20-36.
- Sarker R, Roknuzzaman AS, Hossain MJ, Bhuiyan MA, Islam MR. The WHO declares COVID-19 is no longer a public health emergency of international concern: benefits, challenges, and necessary precautions to come back to normal life. International Journal of Surgery. 2023 Sep 1;109(9):2851-2.
- Parasher, A. COVID-19: Current understanding of its Pathophysiology, Clinical presentation and Treatment. Postgraduate medical journal. 2021 May;97(1147):312-20.
- Yuki K, Fujiogi M, Koutsogiannaki S. COVID-19 pathophysiology: A review. Clinical immunology. 2020 Jun 1;215:108427.
- Guo, T., Fan, Y., Chen, M., Wu, X., Zhang, L., He, T., ... & Wang, H. (2020). Cardiovascular Implications of Fatal Outcomes of Patients With Coronavirus Disease 2019 (COVID-19). JAMA Cardiology, 5(7), 811-818. [CrossRef]
- Zhou, F., Yu, T., Du, R., Fan, G., Liu, Y., Liu, Z., ... & Cao, B. (2020). Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. The Lancet, 395(10229), 1054-1062. [CrossRef]
- Bavishi, C., Maddox, T. M., & Messerli, F. H. (2020). Coronavirus Disease 2019 (COVID-19) Infection and Renin Angiotensin System Blockers. JAMA Cardiology, 5(7), 745-747. [CrossRef]
- Clerkin, K. J., Fried, J. A., Raikhelkar, J., Sayer, G., Griffin, J. M., Masoumi, A., ... & Schwartz, A. (2020). COVID-19 and Cardiovascular Disease. Circulation, 141(20), 1648-1655. [CrossRef]
- Dweck, M. R., Bularga, A., Hahn, R. T., Bing, R., Lee, K. K., Chapman, A. R., ... & Newby, D. E. (2020). Global evaluation of echocardiography in patients with COVID-19. European Heart Journal - Cardiovascular Imaging, 21(9), 949-958. [CrossRef]
- Szekely, Y., Lichter, Y., Taieb, P., Banai, A., Hochstadt, A., Merdler, I., ... & Topilsky, Y. (2020). Spectrum of Cardiac Manifestations in COVID-19. Circulation, 142(4), 342-353. [CrossRef]
- Fried, J. A., Ramasubbu, K., Bhatt, R., Topkara, V. K., Clerkin, K. J., Horn, E., ... & Leon, M. B. (2020). The Variety of Cardiovascular Presentations of COVID-19. Circulation, 141(23), 1930-1936. [CrossRef]
- Jensen, J., Ma, L. P., Fu, M., & Røsjø, H. (2020). Prognostic Value of Echocardiography and Speckle-Tracking Echocardiography in COVID-19. JACC: Cardiovascular Imaging, 13(11), 2472-2474. [CrossRef]
- Li, Y., Li, H., Zhu, S., Xie, Y., Wang, B., He, L., ... & Cao, B. (2020). Prognostic Value of Right Ventricular Longitudinal Strain in COVID-19 Patients. JACC: Cardiovascular Imaging, 13(11), 2287-2299. [CrossRef]
- Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, Flachskampf FA, Foster E, Goldstein SA, Kuznetsova T, Lancellotti P, Muraru D, Picard MH, Rietzschel ER, Rudski L, Spencer KT, Tsang W, Voigt JU. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2015 Jan;28(1):1-39.e14. [CrossRef] [PubMed]
- Lairez O, Blanchard V, Houard V, Vardon-Bounes F, Lemasle M, Cariou E, Lavie-Badie Y, Ruiz S, Cazalbou S, Delmas C, Georges B, Galinier M, Carrié D, Conil JM, Minville V. Cardiac imaging phenotype in patients with coronavirus disease 2019 (COVID-19): results of the cocarde study. Int J Cardiovasc Imaging. 2021 Feb;37(2):449-457. [CrossRef] [PubMed]
- Guan, W., Ni, Z., Hu, Y., Liang, W., Ou, C., He, J., & Zhong, N. (2020). Clinical characteristics of coronavirus disease 2019 in China. New England Journal of Medicine, 382(18), 1708-1720. [CrossRef]
- Zhu, N., Zhang, D., Wang, W., Li, X., Yang, B., Song, J., & Tan, W. (2020). A novel coronavirus from patients with pneumonia in China, 2019. New England Journal of Medicine, 382(8), 727-733. [CrossRef]
- Lewnard, J. A., Hong, V. X., Patel, M. M., Kahn, R., Lipsitch, M., Tartof, S. Y., & Jodar, L. (2022). Clinical outcomes among patients infected with Omicron (B.1.1.529) SARS-CoV-2 variant in southern California. Nature Medicine, 28(7), 1463-1472. [CrossRef]
- Sah P, Fitzpatrick MC, Zimmer CF, Abdollahi E, Juden-Kelly L, Moghadas SM, Singer BH, Galvani AP. Asymptomatic SARS-CoV-2 infection: A systematic review and meta-analysis. Proceedings of the National Academy of Sciences. 2021 Aug 24;118(34):e2109229118.
- Surveillances V. The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19)—China, 2020. China CDC weekly. 2020 Apr;2(8):113-22.
- Bielecka-Dąbrowa A, Cichocka-Radwan A, Lewek J, Pawliczak F, Maciejewski M, Banach M. Cardiac manifestations of COVID-19. Reviews in cardiovascular medicine. 2021;22(2).
- Hezzy Shmueli, Maulin Shah, Joseph E. Ebinger. Left ventricular global longitudinal strain in identifying subclinical myocardial dysfunction among patients hospitalized with COVID-19. [CrossRef]
- Valentina, O. Puntmann, M. Ludovica Carerj, Imke Wieters. Outcomes of Cardiovascular Magnetic Resonance Imaging in Patients Recently Recovered From Coronavirus Disease 2019 (COVID-19). [CrossRef]
- Jin Joo Park, Jun-Bean Park, Jae-Hyeong Park. Global Longitudinal Strain to Predict Mortality in Patients With Acute Heart Failure. [CrossRef]
- Rui Li, Hong Wang, Fei Ma. Widespread myocardial dysfunction in COVID-19 patients detected by myocardial strain imaging using 2-D speckle-tracking echocardiography. [CrossRef]
- Hosseiny, M., Kooraki, S., Gholamrezanezhad, A., Reddy, S., Myers, L., & Hajighasemi, F. (2020). Clinical characteristics of hospitalized patients with SARS-CoV-2 infection: A single arm meta-analysis. Journal of Medical Virology, 92(6), 612–617. [CrossRef]
| Patient No. | Age (years) | LVEF (%) | LV GLS (%) | ANT-SEPT LS (%) | ANT LS (%) | ANT-LAT LS (%) | INF-LAT LS (%) | INF LS (%) | INF-SEPT LS (%) |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 63 | 70 | -21.2 | -23 | -15 | -12 | -22 | -16 | -15 |
| 2 | 50 | 54 | -17.2 | -16 | -22 | -13 | -17 | -14 | -11 |
| 3 | 55 | 62 | -19.6 | -16 | -21 | -15 | -16 | -18 | -15 |
| 4 | 69 | 67 | -22.5 | -20 | -22 | -19 | -26 | -11 | -8 |
| 5 | 53 | 69 | -21.1 | -16 | -20 | -23 | -22 | -14 | -17 |
| 6 | 46 | 55 | -18.3 | -7 | -15 | -14 | -17 | -22 | -7 |
| 7 | 50 | 55 | -19.2 | -17 | -19 | -23 | -19 | -14 | -12 |
| 8 | 48 | 29 | -8.9 | -8 | -12 | -7 | -7 | -7 | -6 |
| 9 | 59 | 42 | -14.9 | -15 | -14 | -14 | -13 | -12 | -12 |
| 10 | 44 | 59 | -17 | -8 | -16 | -19 | -12 | -11 | -13 |
| 11 | 47 | 55 | -16.9 | -15 | -10 | -12 | -18 | -14 | -10 |
| 12 | 49 | 59 | -22 | -17 | -28 | -20 | -24 | -19 | -12 |
| 13 | 58 | 60 | -18.5 | -17 | -18 | -18 | -20 | -12 | -18 |
| 14 | 45 | 60 | -18.8 | -13 | -20 | -15 | -16 | -16 | -12 |
| 15 | 71 | 63 | -21.1 | -17 | -22 | -19 | -18 | -20 | -13 |
| 16 | 44 | 61 | -24.8 | ||||||
| 17 | 47 | 49 | -15.2 | -14 | -20 | -15 | -15 | -13 | -14 |
| 18 | 28 | 66 | -19.4 |
| Variable | Values |
| N | 18 |
| Male (%) | 50 |
| Female (%) | 50 |
| Age (years) | 52 ± 10 |
| LVEF (%) | 57.5 ± 9.986 |
| ANT-SEPT LS (%) | 18.22± 4.84 |
| ANT LS (%) | 17.83± 4.86 |
| ANT-LAT LS (%) | 15.91±4,68 |
| INF LS (%) | 14.33±3.85 |
| INF-SEPT LS (%) | 11.5 ± 3.20 |
| INF-LAT (%) | 17.75± 5.16 |
| LV GLS (%) | 18.7 ± 3.54 |
| Asymptomatic | COVID nucleic acid test positive. Without any clinical symptoms and signs and the chest imaging is normal. |
| Mild | Symptoms of acute upper respiratory tract infection (fever, fatigue, myalgia, cough, sore throat, runny nose, sneezing) or digestive symptoms (nausea, vomiting, abdominal pain, diarrhea). |
| Moderate | Pneumonia (frequent fever, cough) with no obvious hypoxemia, chest CT with lesions. |
| Severe | Pneumonia with hypoxemia (Peripheral oxygen saturation < 92%). |
| Critical | Acute respiratory distress syndrome (ARDS), may have shock, encephalopathy, myocardial injury, heart failure, coagulation dysfunction and acute kidney injury. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





