Submitted:
05 June 2024
Posted:
07 June 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Methods
2.1. Study Design
2.2. Intervention
2.3. Clinical-Epidemiological Variables
2.4. Analytical Variables
2.5. PCR Study of HPV and Anal and Cervical Cytology
2.6. High-Resolution Anoscopy
2.7. Gynecological Examination
2.8. Nonavalent HPV Vaccine
2.9. Antibodies against the 9-HPV Genotypes of the Vaccine
2.10. Statistical Analysis
2.10.1. Sample Size
2.10.2. Data Analysis
3. Results
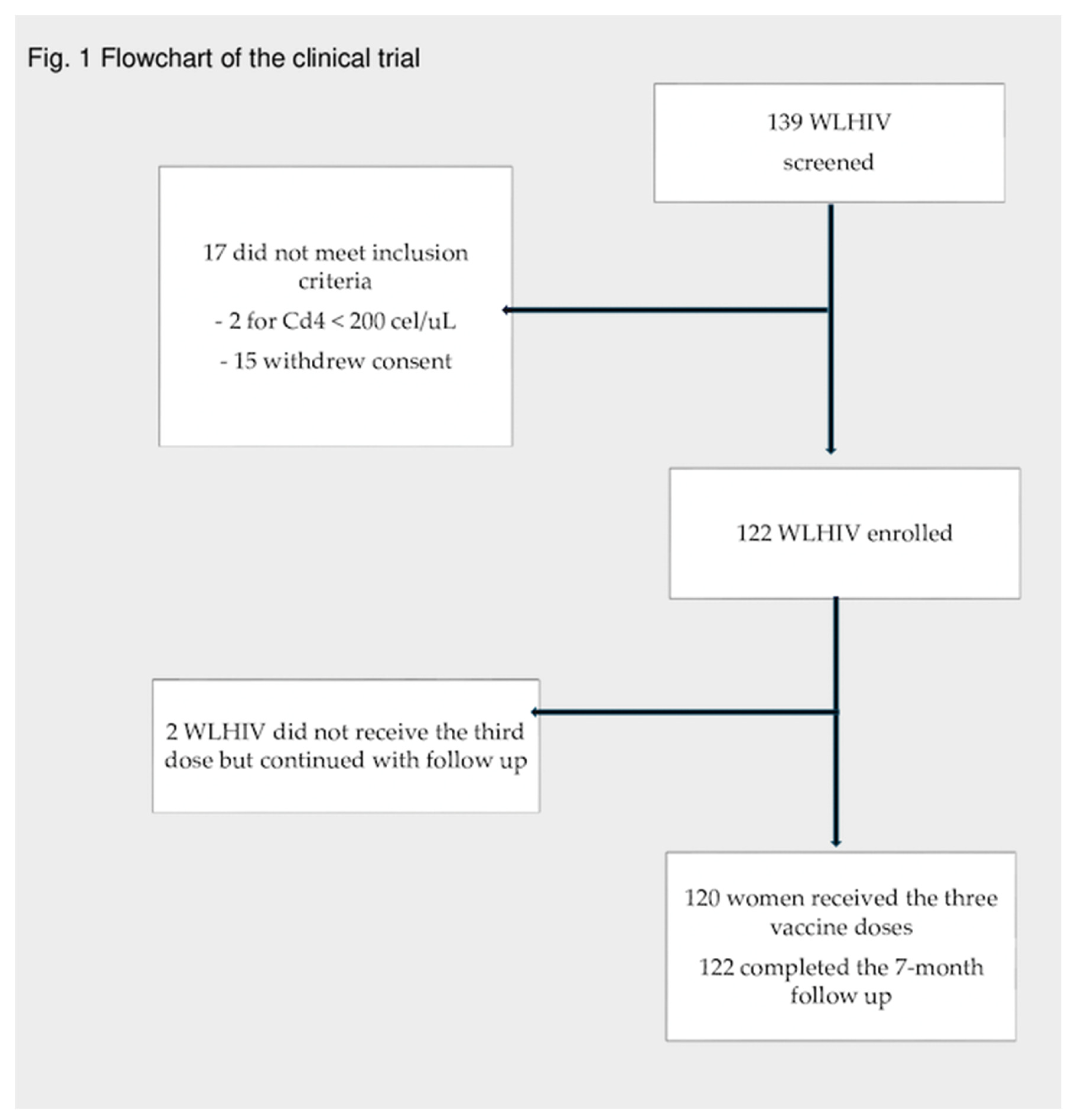
3.1. Study Population
3.2. HPV PCR and Anal Cytology
3.3. Cytology and Cervical HPV PCR
3.4. Adverse Effects
3.5. Immunogenicity
3.6. Risk Factors of Anal Infection by HR-HPV
4. Discussion
Conflicts of Interests:
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgements
References
- Silverberg, M.J.; Lau, B.; Justice, A.C.; Engels, E.; Gill, M.J.; Goedert, J.J.; Kirk, G.D.; D’souza, G.; Bosch, R.J.; Brooks, J.T.; et al. Risk of Anal Cancer in HIV-Infected and HIV-Uninfected Individuals in North America. Clin. Infect. Dis. 2012, 54, 1026–1034. [Google Scholar] [CrossRef] [PubMed]
- Stier, E.A.; Sebring, M.C.; Mendez, A.E.; Ba, F.S.; Trimble, D.D.; Chiao, E.Y. Prevalence of anal human papillomavirus infection and anal HPV-related disorders in women: a systematic review. Am. J. Obstet. Gynecol. 2015, 213, 278–309. [Google Scholar] [CrossRef]
- Jemal A, Simard EP, Dorell C, Noone AM, Markowitz LE, Kohler B, et al. Annual report to the nation on the status of cancer, 1975-2009, featuring the burden and trends in human papillomavirus (HPV)-associated cancers and HPV vaccination coverage levels. J Natl Cancer Inst 2013; 105: 175–201.
- Firnhaber, C.; Westreich, D.; Schulze, D.; Williams, S.; Siminya, M.; Michelow, P.; Levin, S.; Faesen, M.; Smith, J.S. Highly active antiretroviral therapy and cervical dysplasia in HIV-positive women in South Africa. J. Int. AIDS Soc. 2012, 15, 17382. [Google Scholar] [CrossRef]
- Piketty, C.; Selinger-Leneman, H.; Grabar, S.; Duvivier, C.; Bonmarchand, M.; Abramowitz, L.; Costagliola, D.; Mary-Krause, M. Marked increase in the incidence of invasive anal cancer among HIV-infected patients despite treatment with combination antiretroviral therapy. AIDS 2008, 22, 1203–1211. [Google Scholar] [CrossRef] [PubMed]
- D'Souza, G.; Wiley, D.J.; Li, X.M.; Chmiel, J.S.; Margolick, J.B.; Cranston, R.D.M.; Jacobson, L.P. Incidence and Epidemiology of Anal Cancer in the Multicenter AIDS Cohort Study. Am. J. Ther. 2008, 48, 491–499. [Google Scholar] [CrossRef]
- Diamond, C.; Taylor, T.H.; Aboumrad, T.; Bringman, D.; Anton-Culver, H. Increased Incidence of Squamous Cell Anal Cancer Among Men With AIDS in the Era of Highly Active Antiretroviral Therapy. Sex. Transm. Dis. 2005, 32, 314–320. [Google Scholar] [CrossRef]
- Silverberg, M.J.; Lau, B.; Justice, A.C.; Engels, E.; Gill, M.J.; Goedert, J.J.; et al. and North American AIDS Cohort Collaboration on Research and Design (NA-ACCORD) of IeDEA. Risk of anal cancer in HIV-infected and HIV-uninfected individuals in North America. Clin Infect Dis. 2012, 54, 1026–1034. [Google Scholar] [CrossRef] [PubMed]
- Franceschi, S.; the Swiss HIV Cohort Study; Lise, M. ; Clifford, G.M.; Rickenbach, M.; Levi, F.; Maspoli, M.; Bouchardy, C.; Dehler, S.; Jundt, G.; et al. Changing patterns of cancer incidence in the early- and late-HAART periods: the Swiss HIV Cohort Study. Br. J. Cancer 2010, 103, 416–422. [Google Scholar] [CrossRef]
- van der Snoek, E.M.; van der Ende, M.E.; Hollander, J.C.D.; Schutten, M.; Neumann, H.A.M.; van Doornum, G.J.J. Use of Highly Active Antiretroviral Therapy Is Associated With Lower Prevalence of Anal Intraepithelial Neoplastic Lesions and Lower Prevalence of Human Papillomavirus in HIV-Infected Men Who Have Sex With Men. Sex. Transm. Dis. 2012, 39, 495–500. [Google Scholar] [CrossRef]
- Hidalgo-Tenorio, C.; Rivero-Rodriguez, M.; Gil-Anguita, C.; De Hierro, M.L.; Palma, P.; Ramírez-Taboada, J.; Esquivias, J.; López-Ruz, M.A.; Javier-Martínez, R.; Pasquau-Liaño, J. Antiretroviral Therapy as a Factor Protective against Anal Dysplasia in HIV-Infected Males Who Have Sex with Males. PLOS ONE 2014, 9, e92376. [Google Scholar] [CrossRef] [PubMed]
- Hidalgo-Tenorio, C.; de Jesus, S.E.; Esquivias, J.; Pasquau, J. High prevalence and incidence of HPV-related anal cancer precursor lesions in HIV-positive women in the late HAART era. Enfermedades Infecc. y Microbiol. Clin. (English ed.) 2018, 36, 555–562. [Google Scholar] [CrossRef]
- Panel de expertos del Grupo de Estudio de Sida (GESIDA). Documento de consenso sobre diagnóstico y tratamiento de las infecciones de transmisión sexual en adultos, niños y adolescentes (ACTUALIZACIÓN MARZO 2017). Available online: http://www.gesida-seimc.org.
- European AIDS Clinical Society. Guidelines. 2023: 28. (versión 12).
- Hidalgo-Tenorio C, Rivero-Rodriguez M, Gil-Anguita C, Esquivias J, López-Castro R, Ramírez-Taboada J, et al. The role of polymerase chain reaction of high-risk human papilloma virus in the screening of high-grade squamous intraepithelial lesions in the anal mucosa of human immunodeficiency virus-positive males having sex with males. PLoS ONE 2015, 10, e0123590. [Google Scholar]
- E Salit, I.; Lytwyn, A.; Raboud, J.; Sano, M.; Chong, S.; Diong, C.; Chapman, W.; Mahony, J.B.; Tinmouth, J. The role of cytology (Pap tests) and human papillomavirus testing in anal cancer screening. AIDS 2011, 24, 1307–1313. [Google Scholar] [CrossRef] [PubMed]
- Padilla-España L, Repiso-Jiménez B, Fernández-Sánchez F, Frieyro-Elicegui M, Fernández-Morano T, Pereda T, et al. Usefulness of human papillomavirus testing in anal intraepithelial neoplasia screening in a risk behaviour population. Enferm Infecc Microbiol Clin. 2014 Jun 4. pii: S0213-005X (14)00136-0.
- Palefsky, J.M.; Lee, J.Y.; Jay, N.; Goldstone, S.E.; Darragh, T.M.; Dunlevy, H.A.; Rosa-Cunha, I.; Arons, A.; Pugliese, J.C.; Vena, D.; et al. Treatment of Anal High-Grade Squamous Intraepithelial Lesions to Prevent Anal Cancer. New Engl. J. Med. 2022, 386, 2273–2282. [Google Scholar] [CrossRef] [PubMed]
- Park, I.U.; Palefsky, J.M. Evaluation and Management of Anal Intraepithelial Neoplasia in HIV-Negative and HIV-Positive Men Who Have Sex with Men. Curr. Infect. Dis. Rep. 2010, 12, 126–133. [Google Scholar] [CrossRef] [PubMed]
- E Salit, I.; Lytwyn, A.; Raboud, J.; Sano, M.; Chong, S.; Diong, C.; Chapman, W.; Mahony, J.B.; Tinmouth, J. The role of cytology (Pap tests) and human papillomavirus testing in anal cancer screening. AIDS 2010, 24, 1307–1313. [Google Scholar] [CrossRef] [PubMed]
- Kenneth SH, Cranston Rd. Anal Cytology screening in HIV-positive men who have sex with men: what’s new and what´s now?. Current Opinion in Infectious Disease 2010; 23: 21-25.
- Giuliano, A.R.; Palefsky, J.M.; Goldstone, S.; Moreira, E.D.J.; Penny, M.E.; Aranda, C.; Vardas, E.; Moi, H.; Jessen, H.; Hillman, R.; et al. Efficacy of Quadrivalent HPV Vaccine against HPV Infection and Disease in Males. New Engl. J. Med. 2011, 364, 401–411. [Google Scholar] [CrossRef]
- Wilkin, T.; Lee, J.Y.; Lensing, S.Y.; Stier, E.A.; Goldstone, S.E.; Berry, J.M.; Jay, N.; Aboulafia, D.; Cohn, D.L.; Einstein, M.H.; et al. Safety and Immunogenicity of the Quadrivalent Human Papillomavirus Vaccine in HIV-1–Infected Men. J. Infect. Dis. 2010, 202, 1246–1253. [Google Scholar] [CrossRef] [PubMed]
- Hidalgo-Tenorio, C.; Ramírez-Taboada, J.; Gil-Anguita, C.; Esquivias, J.; Omar-Mohamed-Balgahata, M.; SamPedro, A.; Lopez-Ruz, M.; Pasquau, J. Safety and immunogenicity of the quadrivalent human papillomavirus (qHPV) vaccine in HIV-positive Spanish men who have sex with men (MSM). AIDS Res. Ther. 2017, 14, 34–34. [Google Scholar] [CrossRef] [PubMed]
- Wilkin, T.J.; Chen, H.; Cespedes, M.S.; Leon-Cruz, J.T.; Godfrey, C.; Chiao, E.Y.; Bastow, B.; Webster-Cyriaque, J.; Feng, Q.; Dragavon, J.; et al. A Randomized, Placebo-Controlled Trial of the Quadrivalent Human Papillomavirus Vaccine in Human Immunodeficiency Virus-Infected Adults Aged 27 Years or Older: AIDS Clinical Trials Group Protocol A5298. Clin. Infect. Dis. 2018, 67, 1339–1346. [Google Scholar] [CrossRef] [PubMed]
- Muñoz, N.; Bosch, F.X.; De Sanjosé, S.; Herrero, R.; Castellsagué, X.; Shah, K.V.; Snijders, P.J.F.; Meijer, C.J.L.M. Epidemiologic Classification of Human Papillomavirus Types Associated with Cervical Cancer. N. Engl. J. Med. 2003, 348, 518–527. [Google Scholar] [CrossRef] [PubMed]
- Solomon, D.; Davey, D.; Kurman, R.; Moriarty, A.; O’connor, D.; Prey, M.; Raab, S.; Sherman, M.; Wilbur, D.; Wright, T. The 2001 Bethesda System: Terminology for Reporting Results of Cervical Cytology. Obstet. Gynecol. Surv. 2002, 57, 505–507. [Google Scholar] [CrossRef]
- Darragh, T.M.; Colgan, T.J.; Cox, J.T.; Heller, D.S.; Henry, M.R.; Luff, R.D.; McCalmont, T.; Nayar, R.; Palefsky, J.M.; Stoler, M.H.; et al. The Lower Anogenital Squamous Terminology Standardization Project for HPV-Associated Lesions: Background and Consensus Recommendations from the College of American Pathologists and the American Society for Colposcopy and Cervical Pathology. Arch. Pathol. Lab. Med. 2012, 136, 1266–1297. [Google Scholar] [CrossRef]
- Perez, S.; Iñarrea, A.; Pérez-Tanoira, R.; Gil, M.; López-Díez, E.; Valenzuela, O.; Porto, M.; Alberte-Lista, L.; Peteiro-Cancelo, M.A.; Treinta, A.; et al. Fraction of high-grade cervical intraepithelial lesions attributable to genotypes targeted by a nonavalent HPV vaccine in Galicia, Spain. Virol. J. 2017, 14, 214. [Google Scholar] [CrossRef] [PubMed]
- Falcaro, M.; Castañon, A.; Ndlela, B.; Checchi, M.; Soldan, K.; Lopez-Bernal, J.; Elliss-Brookes, L.; Sasieni, P. The effects of the national HPV vaccination programme in England, UK, on cervical cancer and grade 3 cervical intraepithelial neoplasia incidence: a register-based observational study. Lancet 2021, 398, 2084–2092. [Google Scholar] [CrossRef]
- Ghelardi, A.; Parazzini, F.; Martella, F.; Pieralli, A.; Bay, P.; Tonetti, A.; Svelato, A.; Bertacca, G.; Lombardi, S.; Joura, E.A. SPERANZA project: HPV vaccination after treatment for CIN2+. Gynecol. Oncol. 2018, 151, 229–234. [Google Scholar] [CrossRef]
- Hidalgo-Tenorio, C.; Pasquau, J.; Omar-Mohamed, M.; Sampedro, A.; López-Ruz, M.A.; Hidalgo, J.L.; Ramírez-Taboada, J. Effectiveness of the Quadrivalent HPV Vaccine in Preventing Anal ≥ HSILs in a Spanish Population of HIV+ MSM Aged > 26 Years. Viruses 2021, 13, 144. [Google Scholar] [CrossRef]
- Staadegaard, L.; Rönn, M.M.; Soni, N.; Bellerose, M.E.; Bloem, P.; Brisson, M.; Maheu-Giroux, M.; Barnabas, R.V.; Drolet, M.; Mayaud, P.; et al. Immunogenicity, safety, and efficacy of the HPV vaccines among people living with HIV: A systematic review and meta-analysis. EClinicalMedicine 2022, 52, 101585. [Google Scholar] [CrossRef] [PubMed]
- Zizza, A.; Banchelli, F.; Guido, M.; Marotta, C.; Di Gennaro, F.; Mazzucco, W.; Pistotti, V.; D’amico, R. Efficacy and safety of human papillomavirus vaccination in HIV-infected patients: a systematic review and meta-analysis. Sci. Rep. 2021, 11, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Zayats, R.; Murooka, T.T.; McKinnon, L.R. HPV and the Risk of HIV Acquisition in Women. Front. Cell. Infect. Microbiol. 2022, 12, 814948. [Google Scholar] [CrossRef] [PubMed]
| Variables | n = 122 |
|---|---|
| Age, years; mean (±SD) | 49.62 (±9.51) |
| Spanish nationality, n (%) University education, n (%) |
87 (71.3) 10 (8.2) |
| Partners in the previous 12 months, median (IQR) Life-time partners number, median (IQR) Months of sexual activity, median (IQR) History of sex worker, n (%) Sex worker currently, n (%) |
1 (0-1) 5 (3-12) 390 (288-456) 20 (16.4) 2 (1.6) |
| Condom use, n (%) | 53 (43.4) |
| Perianal/genital condylomas at screening, n (%) | 5 (4.1) |
| History of anal/genital condylomas, n (%) History of gynaecologic dysplasia CIN1/VIN1/VAIN1 CIN2/CIN3/VIN2/3/VAIN2/3 Cervical/Vaginal/Vulvar Cancer History of anal dysplasia AIN1 AIN2/3 Anal cancer |
13 (10.7) 28 (22.9) 9 (7.4) 15 (12.2) 2 (1.6) 33 (27) 24 (19.7) 7 (5.7) 2 (1.6) |
| Duration of HIV, mean years (IQR) | 19 (8-24) |
| History of AIDS, n (%) | 58 (47.5) |
| CD4 mean nadir, cells/µL, (± SD) | 226.9 (178.3) |
| CD4 mean, cells/µL (± SD) | 809.3 (367.4) |
| CD8 mean, cells/µL (± SD) CD8/CD4 ratio, mean (± SD) |
794.3 (458.2) 1.2 (0.7) |
| VL of HIV log10, copies/mL (± SD) VL < 50 copies/mL, n (%) |
3.38 (4.41) 113 (92.6) |
| Virological failure, n (%) | 1 (0.8) |
| Median duration of ART, years (IQR) Number of lines of ART, median (IQR) |
15 (8-21.2) 4 (3-6) |
| Antibodies of HPV, n (%) | 7 (5.7) |
| Syphilis treated, n (%) Other STD, n (%) |
6 (4.9) 9 (7.3) |
| Latent tuberculosis treated, n (%) | 17 (13.9) |
| Chronic HCV infection not treated, n (%) | 1 (0.8) |
| Chronic active HCV infection (AgHBs), n (%) Smoking, n (%) Smoking, packets/year, median (IQR) Ex-smoking, n (%), (n=42) Ex-IVDA, n (%) Alcohol (SUA), median (IQR) |
2 (1.6) 66 (55.1) 10 (1.5-23) 15 (12.3) 27 (22.1) 0 (0-0) |
| Variables | n = 122 |
|---|---|
| PCR of HPV, n (%) LR-HPV, n (%) |
42 (34.4) |
| HR-HPV, n (%) | 47 (38.5) |
| HR and LR HPV, n (%) | 30 (24.6) |
| Number of HR-HPV (IQR) | 0 (0-1) |
| Number of LR-HPV (IQR) | 0 (0-1) |
| HPV Genotypes, n (%) | |
| Vaccine HPV genotypes HPV 6 HPV11 HPV16 HPV18 HPV 31 HPV 33 HPV 45 HPV 52 HPV 58 |
9 (7.4) 1 (0.8) 13 (10.7) 2 (1.6) 1 (0.8) 4 (3.3) 6 (4.9) 6 (4.9) 6 (4.9) |
| Another HPV genotypes HPV 32 HPV 35 HPV 39 HPV 40 HPV 42 HPV 43 HPV 44/55 HPV 51 HPV 53 HPV 54 HPV 56 HPV 59 HPV 61 HPV 62 HPV 62/81 HPV 66 HPV 67 HPV 68 HPV 70 HPV 71 HPV 72 HPV 73 HPV 81 HPV 82 HPV 84 |
1 (0.8) 6 (4.9) 3 (2.5) 1 (0.8) 7 (5.7) 2 (1.6) 8 (6.5) 10 (8.2) 3 (2.5) 1 (0.8) 5 (4.1) 3 (2.5) 6 (4.9) 1 (0.8) 9 (7.4) 5 (4.1) 2 (1.6) 9 (7.4) 5 (4.1) 2 (1.6) 1 (0.8) 4 (3.3) 1 (0.8) 1 (0.8) 1 (0.8) |
| Cytology, n (%) Normal LSIL HSIL ASCUS ASCUS-H Invalid results |
122 (100) 80 (65.6) 21 (17.2) 0 (0) 19 (15.6) 0 2 (1.4) |
| HRA, n (%) Normal LSIL (AIN1) |
96 (78.7) 76 (80.8) 18 (19.1) |
| Variables | n = 122 |
|---|---|
| PCR of HPV | |
| LR-HPV, n (%) | 31 (25.4) |
| HR-HPV, n (%) | 32 (26.2) |
| HR and LR HPV, n (%) | 13 (10.7) |
| Number of HR-HPV (IQR) | 0 (0-1) |
| Number of LR-HPV (IQR) | 0 (0-1) |
| HPV Genotypes, n (%) | |
| Vaccine HPV genotypes HPV6 HPV11 HPV16 HPV18 HPV 31 HPV 33 HPV 45 HPV 52 HPV 58 |
8 (6.6) 0 (0) 9 (7.4) 0 (0) 2 (1.6) 2 (1.6) 1 (0.8) 1 (0.8) 2 (1.6) |
| Another HPV genotypes HPV 19 HPV 35 HPV 39 HPV 40 HPV 42 HPV 43 HPV 44 HPV 51 HPV 53 HPV 56 HPV 61 HPV 62 HPV 62/81 HPV 64 HPV 66 HPV 68 HPV 70 HPV 72 HPV 73 HPV 81 HPV 84 |
1(0.8) 1 (0.8) 2 (1.6) 2 (1.6) 8 (6.6) 1 (0.8) 6 (4.9) 3 (2.5) 1 (0.8) 2 (1.6) 4 (3.3) 2 (1.6) 9 (7.4) 1 (0.8) 3 (2.5) 3 (2.5) 2 (1.6) 4 (3.3) 6 (4.9) 2 (1.6) 1 (0.8) |
| Cytology, n (%) Normal LSIL HSIL ASC/ASC-H Invalid result |
122 (100) 111 (91) 4 (3.3) 1 (0.8) 0 (0) 1 (0.8) |
| Colposcopy, n (%) Normal CIN1 CIN2 CIN3 Cervical cancer |
64 (52.5) 60 (93.8) 2 (3.1) 2 (3.1) 0 (0) 0 (0) |
| Adverse events | V1 n=122 |
V2, n=122 |
p* (V1-V2) | V3 n=120 |
p* (V1-V3) |
| Total AE, n (%) | 81 (66.4) | 64 (52.4) | 0.07 | 58 (48.3) | 0.05 |
| Injection-site pain VAS (0-10), median (IQR) |
66 (54.1) 1 (0-4.5) |
54 (44.3) 0 (0-3) |
0.109 | 47 (38.5) 0 (0-3) |
0.008 |
| Local itching | 6 (4.9) | 4 (3.3) | 0.066 | 3 (2.5) | 0.102 |
| Injection site nodule | 7 (5.7) | 5 (4.1) | 0.56 | 5 (4.1) | 0.782 |
| Dizziness | 2 (1.6) | 1 (0.8) | 0.32 | 3 (2.5) | 0.157 |
| AE leading to treatment discontinuation, n (%) | 0 (0) | 0 (0) | 0 (0) | ||
| Deaths, n (%) | 0 (0) | 0 (0) | 0 (0) | ||
| Serious AE, n (%) | 0 (0) | 0 (0) | 0 (0) | ||
| Grade 3 or 4 abnormalities related to nHPV vaccine, n (%) | 0 (0) | 0 (0) | 0 (0) |
| Variables | Baseline (B) | 2m | 6m | 7m | P* B-7m |
| CD4, cel/ul, mean (±SD) CD8, cel/ul, mean (±SD) CD4/CD8 ratio, mean (±SD) VL, log10, mean (±SD) |
809 (226.8) 790.59 (460.44) 1.2 (0.7) 3.38 (4.41) |
831.47 (366.68) 818.35 (527.77) 5.49 (34.92) 0.97(1.39) |
811.51 (370.02) 817 (666.44) 4.33 (33.12) 1.13(1.77) |
792.35 (349.95) 809.61 (521.71) 3.21 (14.98) 1.62(2.55) |
0.357 0.534 0.348 0.125 |
| SGOT, mean (±SD) SGPT, mean (±SD) GGT, mean (±SD) AP, mean (±SD) Bilirubin, mean (±SD) Creatinine, mean (±SD) |
21.24 (7.82) 20.76 (10.41) 39.56 (120.12) 77.85 (47.03) 0.71 (1.01) 0.81 (0.19) |
22.28 (8.51) 20.84 (8.69) 37.34 (110.53) 79.06 (58.88) 1.16 (5.84) 0.84 (0.48) |
22.39 (9.98) 22.31 (11.20) 48.13 (218.51) 79.15 (52.32) 0.56 (0.27) 0.84 (0.51) |
23.63 (16.85) 23.84 (21.23) 49.62 (189.40) 83.45 (56.18) 0.57 (0.25) 1.49 (±6.81) |
0.051 0.012 0.060 0.191 0.036 0.64 |
| Anti-HPV Ab, nm, median (IQR) Anti-HPV Ab positive, n (%) |
0 (0-0) 10 (8.2) |
1 (1-1) 72 (59) |
1 (1-1) 109 (89.3) |
7.63 (3.46-19.7) 118 (96.7) |
0.0001 0.0001 |
| WLHIV without HR-HPV N=73 |
WLHIV with HR-HPV N= 48 |
P* | HR; (95% CI) | |
|---|---|---|---|---|
| Age; mean years (±SD) | 50.5 (7.6) | 48.2 (11.8) | 0.19 | 1.02 (0.93-1.11) |
| Educational level, n (%) Illiterate Elementary High school University education |
11 (15.1) 35 (47.9) 22 (30.1) 5 (6.8) |
9 (19.1) 21 (44.7) 12 (25.5) 5 (10.6) |
0.79 |
1.71 (0.27-10.58) |
| Sex in the previous 12 months, n (%) Anal sex previous 12 months, n (%) Sex worker Partners in the previous 12 months; median (IQR) Life-time partners; median (IQR) Time since commencement of sexual activity (years); median (IQR) |
52 (71.2) 12 (16.4) 12 (16.4) 1 (0-1) 3 (2-9) 33 (27-37) |
31 (64.6) 9 (18.8) 8 (16.7) 1 (0-1) 6 (4-14) 30 (18-41) |
0.44 0.74 0.97 0.96 0.04 0.96 |
1.09 (0.19-6.15) 1 (0.999-1.001) |
| Condom use, n (%) Rate of use condom; median (IQR) |
33 (45.2) 0 (0-100) |
19 (39.6) 0 (0-100) |
0.86 0.87 |
1.21(0.28-5.2) |
| Retired | 16 (21.9) | 13 (28.3) | 0.38 | |
| Polypharmacy | 14 (19.2) | 11 (22.9) | 0.62 | |
| Perianal/genital warts, n (%) | 1 (1.4) | 4 (8.7) | 0.71 | |
| History of anal/genital warts, n (%) History of syphilis, n (%) History others STD CMV IgG positive, n (%) |
9 (12.3) 4 (5.5) 8 (11.3) 53 (72.6) |
4 (8.5) 2 (4.2) 4 (8.7) 40 (87) |
0,55 1 0.76 0.06 |
1.88 (0.35-10) |
| Smoking, n (%) Smoking, packets/year; median (IQR) Ex-UDI, n (%) |
38 (52.1) 9(0-26) 16 (21.9) |
27(56.3) 2.7 (0-14) 11 (22.9) |
0.65 0.2 0.89 |
1.25 (0.28-5.5) |
| Duration of HIV (year); median (IQR) | 22.7 (14.3-27) | 12.2(5.4-20.1) | 0.03 | 0.99 (0.98-1.008) |
| CD4 mean nadir (cells/µL); mean (± SD) | 226.4 (178) | 221.1 (178.3) | 0.9 | 1.002 (0.996-1.008) |
| Treatment naïve, n (%) | 0 | 1(2.1) | 0.39 | |
| VL of HIV, log10; mean (± SD) VL < 50 copies/mL, n (%) Virological failure |
1.85 (2.7) 70 (94.6) 0 |
3.8 (4.6) 42 (87.5) 1 (2.1) |
0.33 0.153 0.39 |
3.22 (0.25-40.84) |
| CD4 mean; cells/µL, mean (± SD) | 854.6 (351.2) | 725.1 (369.4) | 0.054 | 0.99 (0.99-1.001) |
| CD8 mean; cells/µL, mean (± SD) | 755.4 (310.4) | 835.8 (625.1) | 0.412 | |
| CD4/CD8 ratio | 1.3 (0.6) | 1.1 (0.77) | 0.25 | |
| History AIDS-defining illnesses; n (%) | 36 (50) | 22 (46.8) | 0.73 | 0.81 (0.14-4.76) |
| Median duration of ART (year), (IQR) Triple therapy, n (%) Dual therapy, n (%) Monotherapy (DRV/cob), n (%) Number of TAR, median (IQR) Median duration of current ART (months), (IQR) BIC/FTC/TAF DRV/cob/FTC/TAF DTG/ABC /3TC DTG/3TC DTG/RPV DRV/cob |
16.3 (12.3-24) 32 (43.8) 35 (47.9) 6 (8.2) 4(4-6) 21.5 (7.5-34.5) 25 (34.2) 4 (5.5) 1 (1.4) 11 (15.1) 12 (16.4) 15 (20.5) |
11.5 (4.3-19.5) 21 (43.8) 22 (45.8) 4 (8.3) 4 (2-5.5) 16 (6-35.5) 9 (18.8) 6 (12.6) 2 (4.2) 10 (21.8) 6 (12.5) 12 (25) |
0.54 0.99 0.82 1 0.06 0.537 0.06 0.19 0.56 0.41 0.55 0.56 |
0.995 (0.985-1.006) 0.92 (0.64-1.3) 0.26(0.05-1.2) |
| Active chronic HCV infection, n (%) Cured HCV infection, n (%) |
1 (1.4) 19 (26) |
0 12 (25) |
1 1 |
|
| Active chronic HBV infection (positive surface Ag), n (%) | 2 (2.7) | 0 | 0.52 | |
| History of cervical dysplasia, n (%) -CIN 1 -CIN 2 -CIN 3 -Cancer History of vulvar dysplasia, n (%) History of cervical HR-HPV infection, n (%) |
16 (22.9) 6 4 (5.5) 5 (7.1) 1 (1.4) 1 (1.4) 3 (4.8) |
11 (24.4) 3 4 (8.9) 4 (8.9) 1 (2.2) 1 (2.2) 5 (12.5) |
0.85 1 0.7 0.74 1 1 0.26 |
1.93 (0.47-7.98) |
| Anal LR-HPV, n (%) Median of anal LR-HPV genotypes, IQR |
13 (18.1) 0 (0-0) |
30 (62.5) 1 (0-1) |
0.0001 0.0001 |
2.6 (0.46-14.5) |
| Gynaecologic Infection by HR-HPV, n (%) Median of HR-HPV genotypes, IQR |
10 (13.7) 0 (0-0) |
21 (43.8) 1(0-1) |
0.0001 0.0001 |
5.027 (1.009-25.042) |
| Gynaecologic infection by LR-HPV, n (%) Median of LR-HPV genotypes, IQR Gynaecologic due to HR and LR-HPV |
12 (16.4) 0 (0-0) 4 (5.5) |
19 (39.6) 0 (0-1) 8 (16.7) |
0.004 0.02 0.06 |
1.8(0.22-15.3) 0.71(0.02-20.26) |
| Gynaecologic dysplasia, n (%) -CIN 1 -CIN 2 |
0 1 (2.6) |
2 (8) 1 (4) |
0.15 1 |
|
| Antibodies against HPV positive, n (%) | 7 (9.6) | 3 (6.3) | 0.704 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





