Submitted:
13 May 2024
Posted:
14 May 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Results
2.1. Demorphraphic and Biologic Characteristics of Participants
2.2. Hypertension Prevalence in Relation to Cd Burden
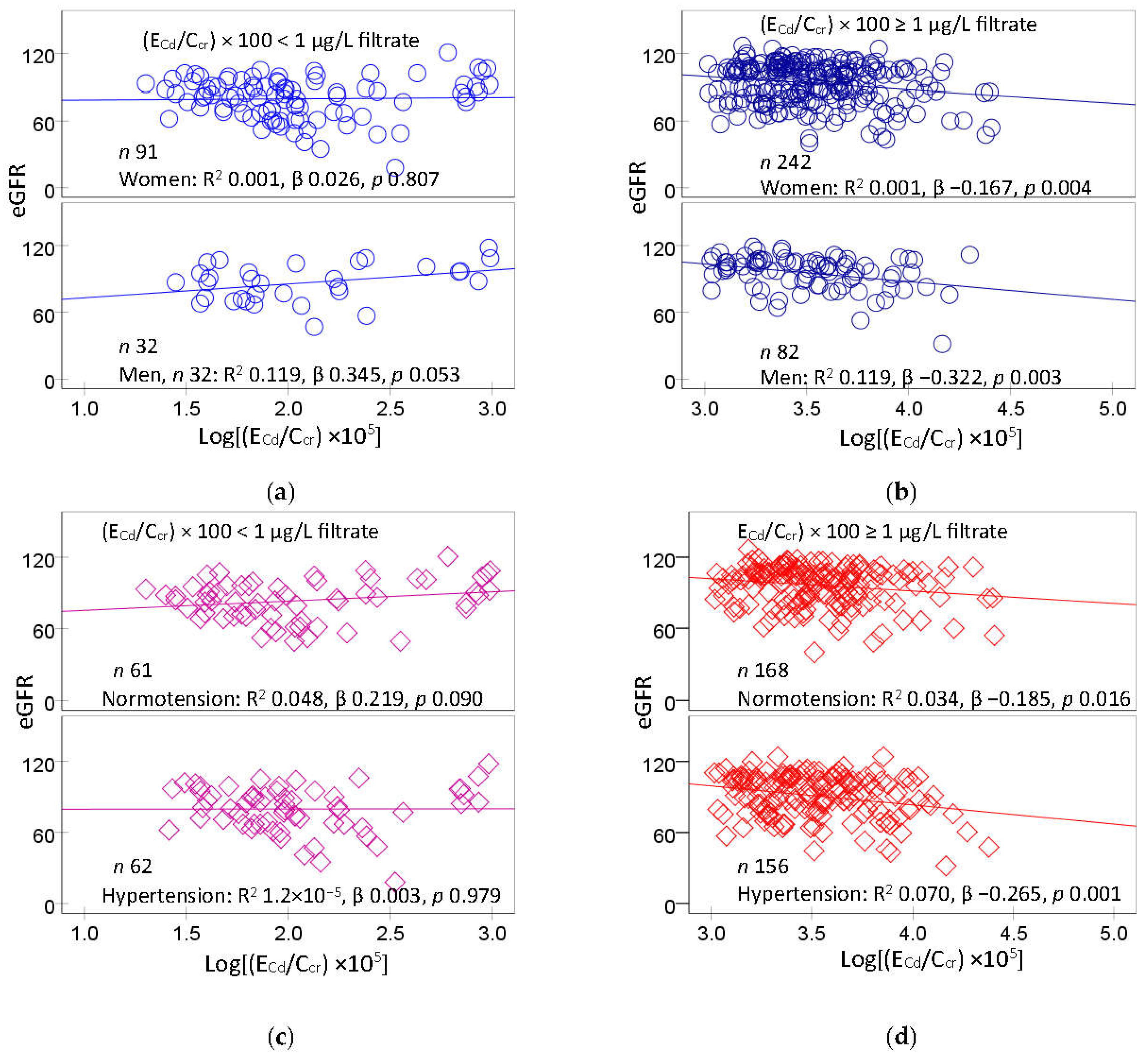
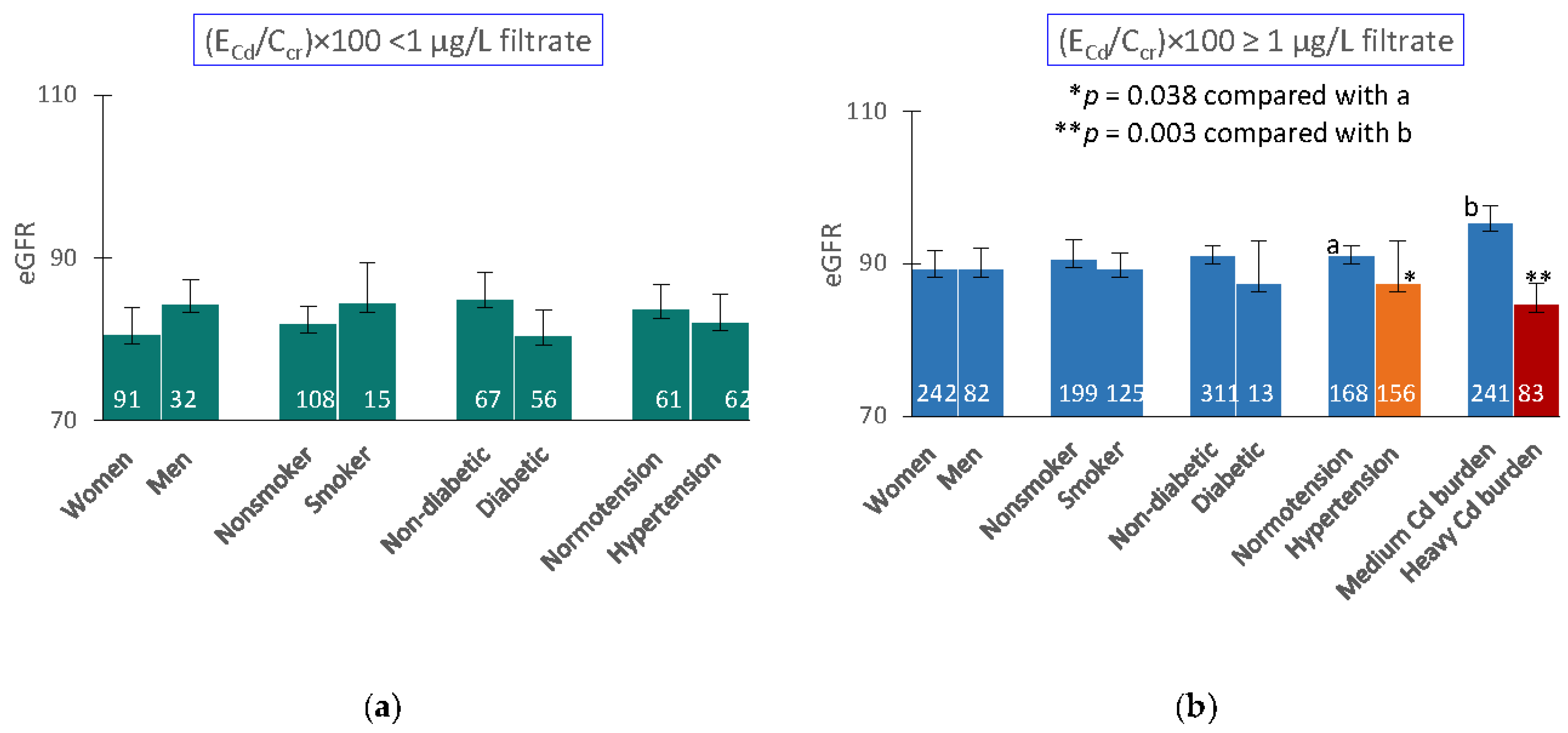
2.3. Cd-Induced eGFR Reduction
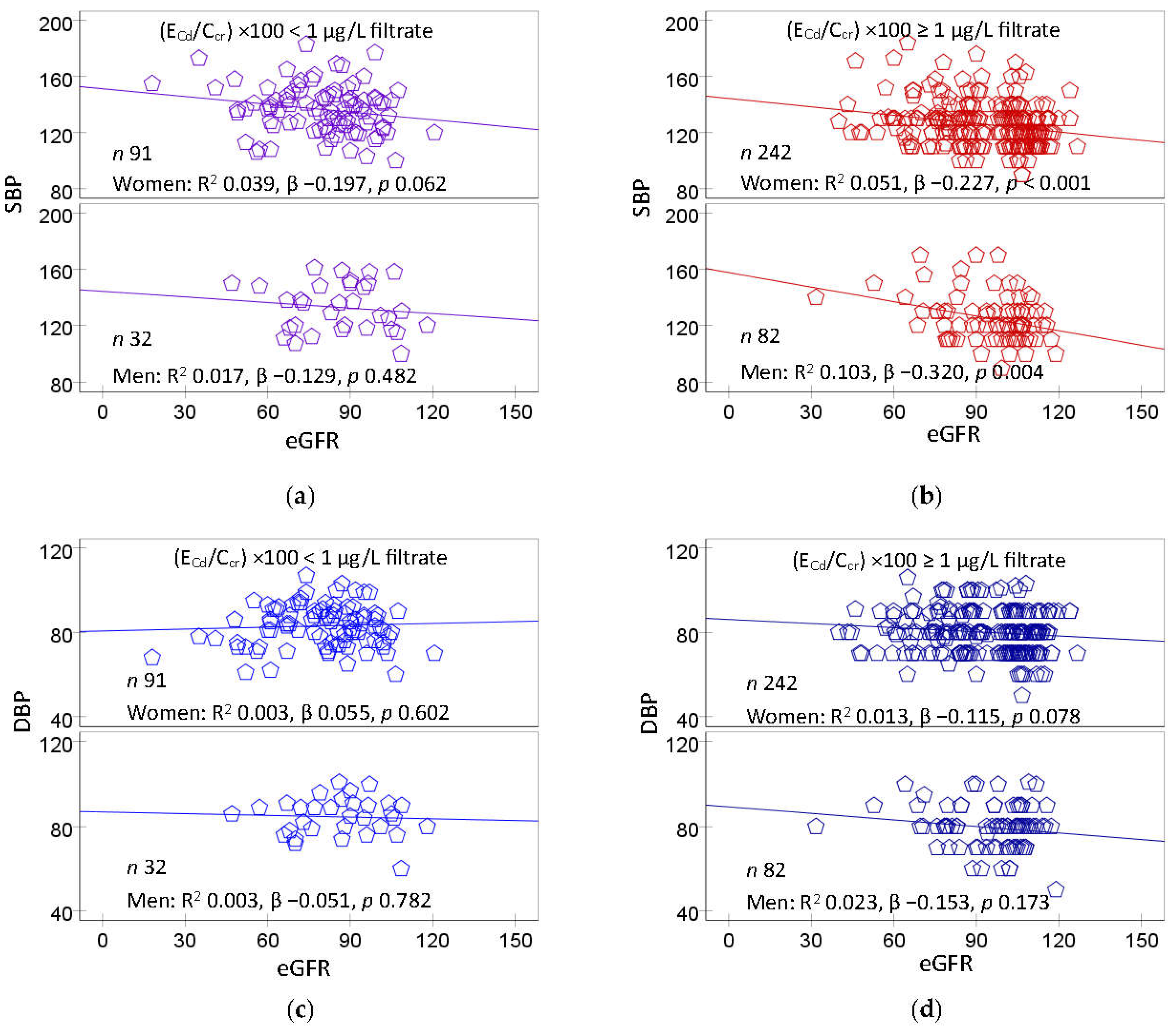
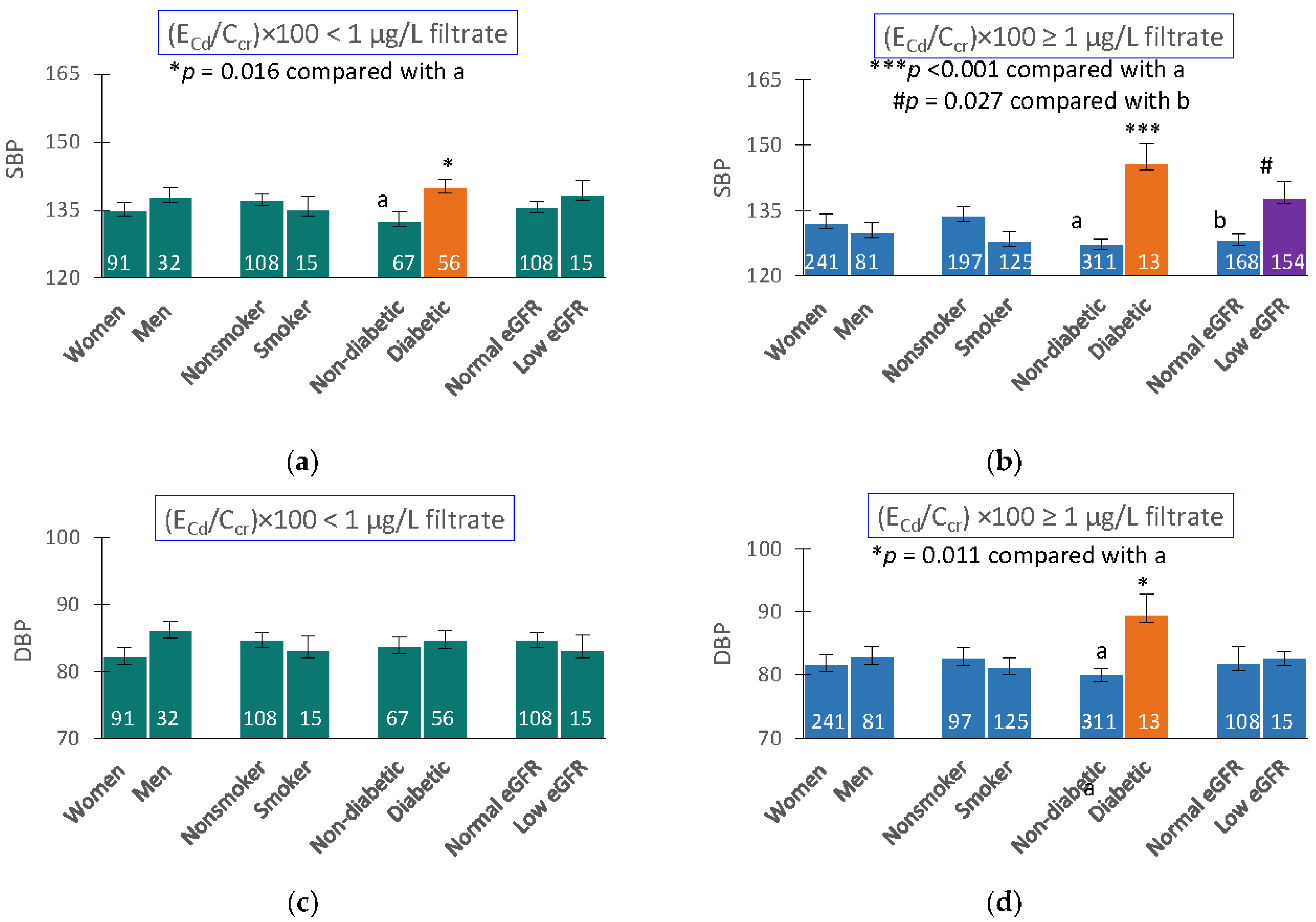
2.4. Inverse Relationships between Blood Pressure and eGFR
2.5. Regression Analysis of Blood Pressure Increment
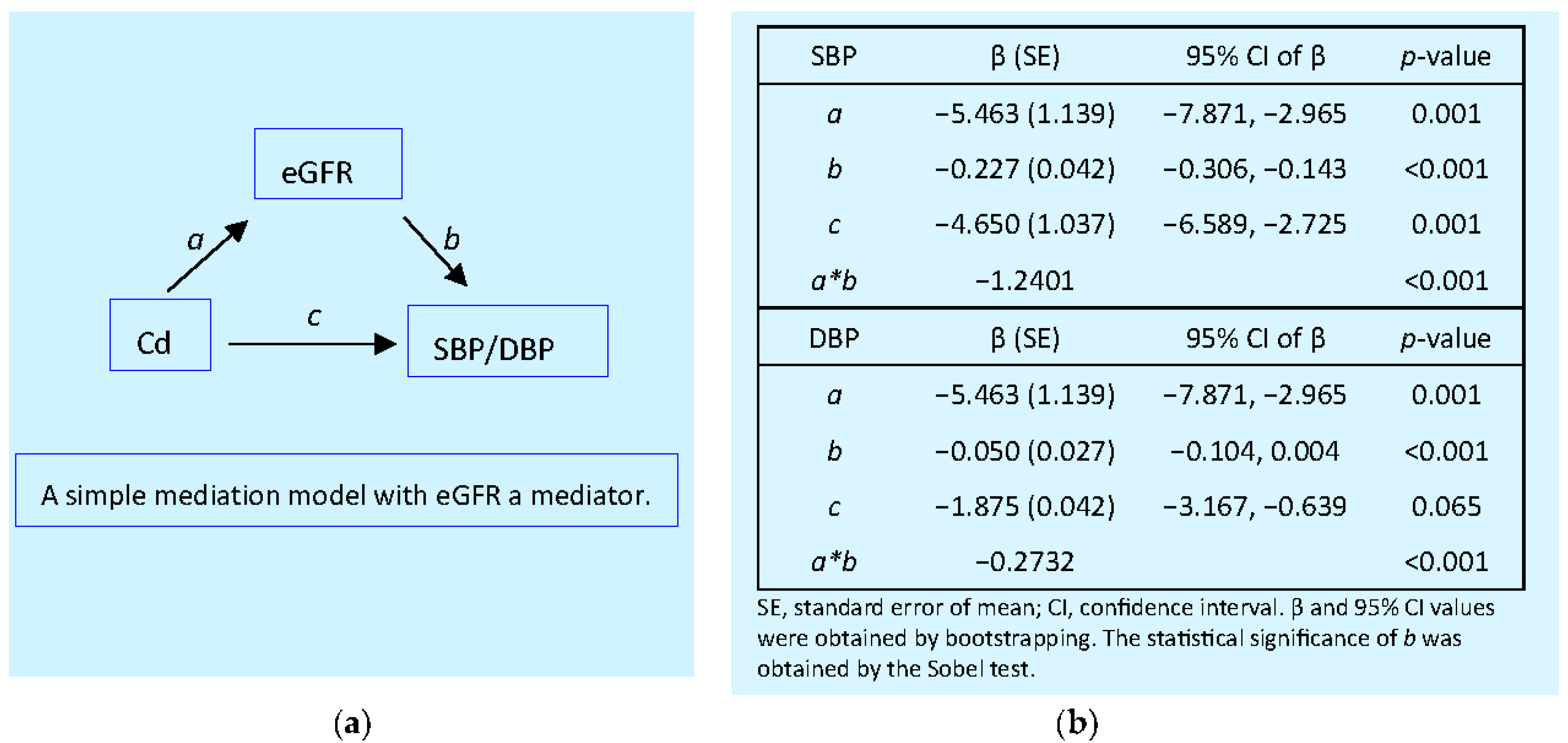
2.6. Mediation Analysis
3. Discussion
4. Materials and Methods
4.1. Participants
4.2. Blood Pressure and Cadmium Exposure Ascertainment
4.3. Normalization of Cadmium Excretion Rate
4.4. Estimated Glomerular Filtration Rate (eGFR)
4.5. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bloch, M.J.; Basile, J.N. Review of recent literature in hypertension: Updated clinical practice guidelines for chronic kidney disease now include albuminuria in the classification system. J. Clin. Hypertens. 2013, 15, 865–867. [Google Scholar] [CrossRef] [PubMed]
- Crowley, S.D.; Coffman, T.M. The inextricable role of the kidney in hypertension. J. Clin. Investig. 2014, 124, 2341–2347. [Google Scholar]
- Verzelloni, P.; Urbano, T.; Wise, L.A.; Vinceti, M.; Filippini, T. Cadmium exposure and cardiovascular disease risk: A systematic review and dose-response meta-analysis. Environ. Pollut. 2024, 345, 123462. [Google Scholar] [CrossRef] [PubMed]
- Doccioli, C.; Sera, F.; Francavilla, A.; Cupisti, A.; Biggeri, A. Association of cadmium environmental exposure with chronic kidney disease: A systematic review and meta-analysis. Sci. Total Environ. 2024, 906, 167165. [Google Scholar] [CrossRef]
- Chen, S.; Shen, R.; Shen, J.; Lyu, L.; Wei, T. Association of blood cadmium with all-cause and cause-specific mortality in patients with hypertension. Front. Public Health 2023, 11, 1106732. [Google Scholar] [CrossRef]
- Liu, Y.; Yang, D.; Shi, F.; Wang, F.; Liu, X.; Wen, H.; Mubarik, S.; Yu, C. Association of serum 25(OH)D, cadmium, CRP with all-cause, cause-specific mortality: A prospective cohort study. Front. Nutr. 2022, 9, 803985. [Google Scholar] [CrossRef]
- Zhang, J.; Wang, X.; Ma, Z.; Dang, Y.; Yang, Y.; Cao, S.; Ouyang, C.; Shi, X.; Pan, J.; Hu, X. Associations of urinary and blood cadmium concentrations with all-cause mortality in US adults with chronic kidney disease: A prospective cohort study. Environ. Sci. Pollut. Res. Int. 2023, 30, 61659–61671. [Google Scholar] [CrossRef] [PubMed]
- Tellez-Plaza, M.; Navas-Acien, A.; Crainiceanu, C.M.; Guallar, E. Cadmium exposure and hypertension in the 1999-2004 National Health and Nutrition Examination Survey (NHANES). Environ. Health Perspect. 2008, 116, 51–56. [Google Scholar] [CrossRef]
- Scinicariello, F.; Abadin, H.G.; Murray, H.E. Association of low-level blood lead and blood pressure in NHANES 1999-2006. Environ. Res. 2011, 111, 1249–1257. [Google Scholar] [CrossRef]
- Oliver-Williams, C.; Howard, A.G.; Navas-Acien, A.; Howard, B.V.; Tellez-Plaza, M.; Franceschini, N. Cadmium body burden, hypertension, and changes in blood pressure over time: Results from a prospective cohort study in American Indians. J. Am. Soc. Hypertens. 2018, 12, 426–437.e9. [Google Scholar] [CrossRef]
- Garner, R.E.; Levallois, P. Associations between cadmium levels in blood and urine, blood pressure and hypertension among Canadian adults. Environ. Res. 2017, 155, 64–72. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Wang, Z.; Zhu, G.; Liang, Y.; Jin, T. Benchmark dose estimation of cadmium reference level for hypertension in a Chinese population. Environ. Toxicol. Pharmacol. 2015, 39, 208–212. [Google Scholar] [CrossRef] [PubMed]
- Wu, W.; Liu, D.; Jiang, S.; Zhang, K.; Zhou, H.; Lu, Q. Polymorphisms in gene MMP-2 modify the association of cadmium exposure with hypertension risk. Environ. Int. 2019, 124, 441–447. [Google Scholar] [CrossRef] [PubMed]
- Zhong, Q.; Wu, H.B.; Niu, Q.S.; Jia, P.P.; Qin, Q.R.; Wang, X.D.; He, J.L.; Yang, W.J.; Huang, F. Exposure to multiple metals and the risk of hypertension in adults: A prospective cohort study in a local area on the Yangtze River, China. Environ. Int. 2021, 153, 106538. [Google Scholar] [CrossRef] [PubMed]
- Lee, B.K.; Kim, Y. Association of blood cadmium with hypertension in the Korean general population: Analysis of the 2008–2010 Korean National Health and Nutrition Examination Survey data. Am. J. Ind. Med. 2012, 55, 1060–1067. [Google Scholar] [CrossRef] [PubMed]
- Kwon, J.A.; Park, E.; Kim, S.; Kim, B. Influence of serum ferritin combined with blood cadmium concentrations on blood pressure and hypertension: From the Korean National Health and Nutrition Examination Survey. Chemosphere 2022, 288, 132469. [Google Scholar] [CrossRef] [PubMed]
- Kaneda, M.; Wai, K.M.; Kanda, A.; Ando, M.; Murashita, K.; Nakaji, S.; Ihara, K. Low level of serum cadmium in relation to blood pressures among Japanese general population. Biol. Trace Element Res. 2021, 200, 67–75. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, T.; Kataoka, Y.; Hayashi, K.; Matsuda, R.; Uneyama, C. Dietary exposure of the Japanese general population to elements: Total diet study 2013–2018. Food Saf. 2022, 10, 83–101. [Google Scholar] [CrossRef]
- Almerud, P.; Zamaratskaia, G.; Lindroos, A.K.; Bjermo, H.; Andersson, E.M.; Lundh, T.; Ankarberg, E.H.; Lignell, S. Cadmium, total mercury, and lead in blood and associations with diet, sociodemographic factors, and smoking in Swedish adolescents. Environ. Res. 2021, 197, 110991. [Google Scholar] [CrossRef]
- Kim, J.; Song, H.; Lee, J.; Kim, Y.J.; Chung, H.S.; Yu, J.M.; Jang, G.; Park, R.; Chung, W.; Oh, C.M.; Moon, S. Smoking and passive smoking increases mortality through mediation effect of cadmium exposure in the United States. Sci. Rep. 2023, 13, 3878. [Google Scholar] [CrossRef]
- Hill, D.T.; Jandev, V.; Petroni, M.; Atallah-Yunes, N.; Bendinskas, K.; Brann, L.S.; Heffernan, K.; Larsen, D.A.; MacKenzie, J.A.; Palmer, C.D.; et al. Airborne levels of cadmium are correlated with urinary cadmium concentrations among young children living in the New York state city of Syracuse, USA. Environ. Res. 2023, 223, 115450. [Google Scholar] [CrossRef]
- Kikuchi, Y.; Nomiyama, T.; Kumagai, N.; Dekio, F.; Uemura, T.; Takebayashi, T.; Nishiwaki, Y.; Matsumoto, Y.; Sano, Y.; Hosoda, K.; et al. Uptake of cadmium in meals from the digestive tract of young non-smoking Japanese female volunteers. J. Occup. Health 2003, 45, 43–52. [Google Scholar] [CrossRef] [PubMed]
- Horiguchi, H.; Oguma, E.; Sasaki, S.; Miyamoto, K.; Ikeda, Y.; Machida, M.; Kayama, F. Comprehensive study of the effects of age, iron deficiency, diabetes mellitus, and cadmium burden on dietary cadmium absorption in cadmium-exposed female Japanese farmers. Toxicol. Appl. Pharmacol. 2004, 196, 114–123. [Google Scholar] [CrossRef] [PubMed]
- Satarug, S.; Phelps, K.R. Chapter 14: Cadmium Exposure and Toxicity. In Metal Toxicology Handbook; Bagchi, D., Bagchi, M., Eds.; CRC Press: Boca Raton, FL, USA, 2021; pp. 219–274. [Google Scholar]
- Satarug, S.; Vesey, D.A.; Gobe, G.C.; Phelps, K.R. Estimation of health risks associated with dietary cadmium exposure. Arch. Toxicol. 2023, 97, 329–358. [Google Scholar] [CrossRef]
- Fujita, Y.; el Belbasi, H.I.; Min, K.S.; Onosaka, S.; Okada, Y.; Matsumoto, Y.; Mutoh, N.; Tanaka, K. Fate of cadmium bound to phytochelatin in rats. Res. Commun. Chem. Pathol. Pharmacol. 1993, 82, 357–365. [Google Scholar] [PubMed]
- Langelueddecke, C.; Roussa, E.; Fenton, R.A.; Thévenod, F. Expression and function of the lipocalin-2 (24p3/NGAL) receptor in rodent and human intestinal epithelia. PLoS ONE 2013, 8, e71586. [Google Scholar] [CrossRef] [PubMed]
- Langelueddecke, C.; Lee, W.K.; Thévenod, F. Differential transcytosis and toxicity of the hNGAL receptor ligands cadmium-metallothionein and cadmium-phytochelatin in colon-like Caco-2 cells: Implications for in vivo cadmium toxicity. Toxicol. Lett. 2014, 226, 228–235. [Google Scholar] [CrossRef] [PubMed]
- Satarug, S.; Baker, J.R.; Reilly, P.E.; Moore, M.R.; Williams, D.J. Cadmium levels in the lung, liver, kidney cortex, and urine samples from Australians without occupational exposure to metals. Arch. Environ. Health 2002, 57, 69–77. [Google Scholar] [CrossRef] [PubMed]
- Barregard, L.; Sallsten, G.; Lundh, T.; Mölne, J. Low-level exposure to lead, cadmium and mercury, and histopathological findings in kidney biopsies. Environ. Res. 2022, 211, 113119. [Google Scholar] [CrossRef]
- Satarug, S.; Vesey, D.A.; Ruangyuttikarn, W.; Nishijo, M.; Gobe, G.C.; Phelps, K.R. The source and pathophysiologic significance of excreted cadmium. Toxics 2019, 7, 55. [Google Scholar] [CrossRef]
- Akerstrom, M.; Barregard, L.; Lundh, T.; Sallsten, G. The relationship between cadmium in kidney and cadmium in urine and blood in an environmentally exposed population. Toxicol. Appl. Pharmacol. 2013, 268, 286–293. [Google Scholar] [CrossRef] [PubMed]
- Satarug, S.; Gobe, G.C.; Vesey, D.A.; Phelps, K.R. Cadmium and lead exposure, nephrotoxicity, and mortality. Toxics 2020, 8, 86. [Google Scholar] [CrossRef]
- Lang, S.M.; Schiffl, H. Smoking status, cadmium, and chronic kidney disease. Renal Replacement Therapy 2024, 10, 17. [Google Scholar] [CrossRef]
- Levey, A.S.; Stevens, L.A.; Scmid, C.H.; Zhang, Y.; Castro, A.F., III; Feldman, H.I.; Kusek, J.W.; Eggers, P.; Van Lente, F.; Greene, T.; et al. A new equation to estimate glomerular filtration rate. Ann. Intern. Med. 2009, 150, 604–612. [Google Scholar] [CrossRef] [PubMed]
- Phelps, K.R.; Gosmanova, E.O. A generic method for analysis of plasma concentrations. Clin. Nephrol. 2020, 94, 43–49. [Google Scholar] [CrossRef] [PubMed]
- Tsai, H.J.; Hung, C.H.; Wang, C.W.; Tu, H.P.; Li, C.H.; Tsai, C.C.; Lin, W.Y.; Chen, S.C.; Kuo, C.H. Associations among heavy metals and proteinuria and chronic kidney disease. Diagnostics (Basel) 2021, 11, 282. [Google Scholar] [CrossRef] [PubMed]
- Shi, P.; Yan, H.; Fan, X.; Xi, S. A benchmark dose analysis for urinary cadmium and type 2 diabetes mellitus. Environ. Pollut. 2021, 273, 116519. [Google Scholar] [CrossRef]
- Lee, J.; Oh, S.; Kang, H.; Kim, S.; Lee, G.; Li, L.; Kim, C.T.; An, J.N.; Oh, Y.K.; Lim, C.S.; et al. Environment-Wide Association Study of CKD. Clin. J. Am. Soc. Nephrol. 2020, 15, 766–775. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Fagerberg, B.; Sallsten, G.; Borné, Y.; Hedblad, B.; Engström, G.; Barregard, L.; Andersson, E.M. Smoking-induced risk of future cardiovascular disease is partly mediated by cadmium in tobacco: Malmö Diet and Cancer Cohort Study. Environ. Health 2019, 18, 56. [Google Scholar] [CrossRef]
- Hecht, E.M.; Landy, D.C.; Ahn, S.; Hlaing, W.M.; Hennekens, C.H. Hypothesis: cadmium explains, in part, why smoking increases the risk of cardiovascular disease. J. Cardiovasc. Pharmacol. Ther. 2013, 18, 550–554. [Google Scholar] [CrossRef]
- Liao, K.W.; Chien, L.C.; Chen, Y.C.; Kao, H.C. Sex-specific differences in early renal impairment associated with arsenic, lead, and cadmium exposure among young adults in Taiwan. Environ. Sci. Pollut. Res. Int. 2022, 29, 52655–52664. [Google Scholar] [CrossRef] [PubMed]
- Perry, H.M.; Erlanger, M.; Perry, E.F. Increase in the systolic pressure of rats chronically fed cadmium. Environ. Health Perspect. 1979, 28, 251–260. [Google Scholar] [CrossRef] [PubMed]
- Perry, H.M., Jr.; Erlanger, M.W. Sodium retention in rats with cadmium-induced hypertension. Sci. Total Environ. 1981, 22, 31–38. [Google Scholar] [CrossRef] [PubMed]
- Peña, A.; Iturri, S.J. Cadmium as hypertensive agent. Effect on ion excretion in rats. Comp. Biochem. Physiol. C Comp. Pharmacol. Toxicol. 1993, 106, 315–319. [Google Scholar] [CrossRef] [PubMed]
- Yimthiang, S.; Pouyfung, P.; Khamphaya, T.; Kuraeiad, S.; Wongrith, P.; Vesey, D.A.; Gobe, G.C.; Satarug, S. Effects of environmental exposure to cadmium and lead on the risks of diabetes and kidney dysfunction. Int. J. Environ. Res. Public Health 2022, 19, 2259. [Google Scholar] [CrossRef] [PubMed]
- Satarug, S.; Swaddiwudhipong, W.; Ruangyuttikarn, W.; Nishijo, M.; Ruiz, P. Modeling cadmium exposures in low- and high-exposure areas in Thailand. Environ. Health Perspect. 2013, 121, 531–536. [Google Scholar] [CrossRef] [PubMed]
- Zarcinas, B.A.; Pongsakul, P.; McLaughlin, M.J.; Cozens, G. Heavy metals in soils and crops in Southeast Asia. 2. Thailand. Environ. Geochem. Health 2004, 26, 359–371. [Google Scholar] [CrossRef] [PubMed]
- Sripaoraya, K.; Siriwong, W.; Pavittranon, S.; Chapman, R.S. Environmental arsenic exposure and risk of diabetes type 2 in Ron Phibun subdistrict, Nakhon Si Thammarat Province, Thailand: unmatched and matched case-control studies. Risk Manag Healthc Policy 2017, 10, 41–48. [Google Scholar] [CrossRef] [PubMed]
- Suwatvitayakorn, P.; Ko, M.S.; Kim, K.W.; Chanpiwat, P. Human health risk assessment of cadmium exposure through rice consumption in cadmium-contaminated areas of the Mae Tao sub-district, Tak, Thailand. Environ. Geochem. Health 2020, 42, 2331–2344. [Google Scholar] [CrossRef]
- Swaddiwudhipong, W.; Mahasakpan, P.; Limpatanachote, P.; Krintratun, S. Correlations of urinary cadmium with hypertension and diabetes in persons living in cadmium-contaminated villages in northwestern Thailand: A population study. Environ. Res. 2010, 110, 612–616. [Google Scholar] [CrossRef]
- Hornung, R.W.; Reed, L.D. Estimation of average concentration in the presence of nondetectable values. Appl. Occup. Environ. Hyg. 1990, 5, 46–51. [Google Scholar] [CrossRef]
- Satarug, S.; Vesey, D.A.; Nishijo, M.; Ruangyuttikarn, W.; Gobe, G.C.; Phelps, K.R. The effect of cadmium on GFR is clarified by normalization of excretion rates to creatinine clearance. Int. J. Mol. Sci. 2021, 22, 1762. [Google Scholar] [CrossRef] [PubMed]
- White, C.A.; Allen, C.M.; Akbari, A.; Collier, C.P.; Holland, D.C.; Day, A.G.; Knoll, G.A. Comparison of the new and traditional CKD-EPI GFR estimation equations with urinary inulin clearance: A study of equation performance. Clin. Chim. Acta 2019, 488, 189–195. [Google Scholar] [CrossRef] [PubMed]
- MacKinnon, D.P.; Warsi, G.; Dwyer, J.H. A simulation study of mediated effect measures. Multiv. Behav. Res. 1995, 30, 41–62. [Google Scholar] [CrossRef]
- Preacher, K.J.; Hayes, A.F. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behav. Res. Meth. Instrum. Comput. 2004, 36, 717–731. [Google Scholar] [CrossRef]
| Parameters | All, n = 447 | Cd Burden Tertiles | p | ||
|---|---|---|---|---|---|
| Low, n =148 | Middle, n =149 | High, n = 150 | |||
| Age, years | 51.1 ± 8.6 | 56.6 ± 9.7 | 48.1 ± 6.9 | 48.7 ± 6.1 | <0.001 |
| BMI, kg/m2 | 24.8 ± 4.0 | 25.5 ± 4.5 | 24.8 ± 3.8 | 24.0 ± 3.4 | 0.006 |
| eGFR a, mL/min/1.73m2 | 90 ± 18 | 84 ± 18 | 96 ± 17 | 91 ± 18 | <0.001 |
| % eGFR ≤ 60 mL/min/1.73m2 | 6.9 | 10.3 | 1.3 | 8.7 | 0.005 |
| % Hypertension | 48.8 | 51.4 | 46.3 | 48.7 | 0.685 |
| % Smoking | 31.1 | 16.2 | 34.9 | 42.7 | <0.001 |
| % Diabetes | 15.4 | 39.2 | 3.4 | 4.0 | <0.001 |
| Systolic blood pressure, mmHg | 128 ± 17 | 134 ± 17 | 126 ± 16 | 126 ± 16 | <0.001 |
| Diastolic blood pressure, mmHg | 81 ± 10 | 83 ± 10 | 80 ± 10 | 80 ± 11 | 0.019 |
| [cr]p, mg/dL | 0.82 ± 0.22 | 0.86 ± 0.25 | 0.77 ± 0.17 | 0.83 ± 0.23 | 0.001 |
| [cr]u, mg/dL | 114 ± 74 | 113 ± 72 | 131 ± 72 | 99 ± 75 | <0.001 |
| [Cd]b, µg/L | 2.75 ± 3.19 | 0.72 ± 0.83 | 2.37 ± 2.06 | 5.14 ± 3.95 | <0.001 |
| [Cd]u, µg/L | 4.23 ± 5.68 | 0.71 ± 1.20 | 3.91 ± 2.50 | 8.03 ± 7.86 | <0.001 |
| Normalized to Ecr (ECd/Ecr) b | |||||
| ECd/Ecr, µg/g creatinine | 4.03 ± 4.42 | 0.48 ± 0.62 | 3.07 ± 0.93 | 8.48 ± 4.87 | <0.001 |
| Normalized to Ccr, (ECd/Ccr) c | |||||
| (ECd/Ccr) ×100, µg/L filtrate | 3.20 ± 3.73 | 0.38 ± 0.46 | 2.28 ± 0.56 | 6.89 ± 4.31 | <0.001 |
| Independent Variables/Factors |
Hypertension | ||||
|---|---|---|---|---|---|
| β Coefficients | POR | 95% CI | p | ||
| (SE) | Lower | Upper | |||
| Age, years | 0.023 (0.014) | 1.024 | 0.997 | 1.051 | 0.085 |
| BMI, kg/m2 | 0.079 (0.027) | 1.082 | 1.027 | 1.140 | 0.003 |
| Gender | −0.070 (0.260) | 0.932 | 0.560 | 1.551 | 0.788 |
| Smoking | −0.444 (0.250) | 0.642 | 0.393 | 1.048 | 0.076 |
| Diabetes | 0.575 (0.329) | 1.777 | 0.932 | 3.388 | 0.081 |
| Cd burden a | |||||
| Mild | Referent | ||||
| Moderate | 0.748 | 2.114 | 1.049 | 4.260 | 0.036 |
| Heavy | 0.504 | 1.655 | 0.921 | 2.973 | 0.092 |
| Independent Variables/Factors |
Hypertension | ||||
|---|---|---|---|---|---|
| β Coefficients | POR | 95% CI | p | ||
| (SE) | Lower | Upper | |||
| Age, years | 0.018 (0.012) | 1.018 | 0.994 | 1.042 | 0.148 |
| BMI, kg/m2 | 0.080 (0.026) | 1.083 | 1.029 | 1.140 | 0.002 |
| Gender | −0.050 (0.254) | 0.951 | 0.578 | 1.565 | 0.844 |
| Smoking | −0.433 (0.255) | 0.649 | 0.394 | 1.069 | 0.089 |
| Diabetes | 0.422 (0.294) | 1.526 | 0.858 | 2.713 | 0.150 |
| Quartile of [Cd]b, µg/L | |||||
| Q1: < 0.60 | Referent | ||||
| Q2: 0.61−1.69 | 0.748 (0.293) | 2.113 | 1.191 | 3.749 | 0.011 |
| Q3: 1.70−3.38 | 0.606 (0.309) | 1.833 | 1.000 | 3.360 | 0.050 |
| Q4: >3.38 | 0.587 (0.337) | 1.798 | 0.928 | 3.482 | 0.082 |
| Independent variables/ Factors |
eGFR, mL/min/1.73m2 | |||||||
|---|---|---|---|---|---|---|---|---|
| Women, n = 333 |
Men, n = 114 |
Normotension, n = 229 |
Hypertension, n = 218 |
|||||
| β | p | β | p | β | p | β | p | |
| Age, years | −0.528 | <0.001 | −0.505 | <0.001 | −0.559 | <0.001 | −0.517 | <0.001 |
| BMI, kg/m2 | −0.050 | 0.308 | −0.136 | 0.122 | −0.037 | 0.532 | −0.077 | 0.216 |
| Log2[(ECd/Ccr)×105], µg/L filtrate | −0.121 | 0.051 | −0.077 | 0.463 | −0.056 | 0.440 | −0.177 | 0.023 |
| Gender | − | − | − | − | −0.017 | 0.787 | −0.012 | 0.870 |
| Hypertension | −0.045 | 0.344 | −0.203 | 0.018 | − | − | − | − |
| Smoking | 0.031 | 0.533 | 0.043 | 0.624 | 0.152 | 0.020 | −0.098 | 0.178 |
| Diabetes | −0.133 | 0.016 | −0.018 | 0.854 | −0.049 | 0.445 | −0.175 | 0.012 |
| Adjusted R2 | 0.279 | <0.001 | 0.248 | <0.001 | 0.318 | <0.001 | 0.242 | <0.001 |
| Independent Variables/Factors |
SBP or DBP | |||||
|---|---|---|---|---|---|---|
| All, n = 447 | Mild Cd Burden a n = 123 |
Medium + Heavy n = 324 |
||||
| β | p | β | p | β | p | |
| Model 1: SBP | ||||||
| Age, years | 0.243 | <0.001 | 0.395 | <0.001 | 0.091 | 0.143 |
| BMI, kg/m2 | 0.113 | 0.013 | 0.081 | 0.361 | 0.097 | 0.084 |
| Log2[(ECd/Ccr)× 105], µg/L filtrate | 0.027 | 0.624 | 0.080 | 0.372 | −0.051 | 0.352 |
| eGFR, mL/min/1.73m2 | −0.106 | 0.036 | 0.011 | 0.907 | −0.176 | 0.004 |
| Gender | −0.044 | 0.378 | −0.096 | 0.360 | −0.024 | 0.688 |
| Smoking | −0.075 | 0.145 | −0.176 | 0.093 | −0.031 | 0.600 |
| Diabetes | 0.216 | <0.001 | 0.202 | 0.020 | 0.265 | <0.001 |
| Adjusted R2 | 0.199 | <0.001 | 0.157 | <0.001 | 0.150 | <0.001 |
| Model 2: DBP | ||||||
| Age, years | −0.028 | 0.650 | 0.036 | 0.739 | −0.081 | 0.213 |
| BMI, kg/m2 | 0.123 | 0.013 | 0.069 | 0.475 | 0.123 | 0.037 |
| Log2[(ECd/Ccr)× 105], µg/L filtrate | −0.069 | 0.255 | −0.059 | 0.546 | −0.025 | 0.660 |
| eGFR, mL/min/1.73m2 | −0.085 | 0.123 | 0.057 | 0.582 | −0.130 | 0.041 |
| Gender | −0.055 | 0.314 | −0.207 | 0.074 | −0.003 | 0.968 |
| Smoking | −0.050 | 0.373 | −0.209 | 0.068 | 0.008 | 0.897 |
| Diabetes | 0.102 | 0.064 | 0.027 | 0.775 | 0.193 | 0.001 |
| Adjusted R2 | 0.046 | <0.001 | −0.005 | 0.498 | 0.058 | 0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





