1. Introduction
A variety of flap techniques have been developed to reconstruct defects caused by trauma or tumor resection in various body areas. After facial tumor surgery, it is important to choose an appropriate flap suited for the patients’ specific needs, whereby both the recipient site requirements and the donor site aspects must be considered. The lateral arm free flap is very widely used free flaps due to its various advantages and applicability. Although it has relatively short pedicle length, it has several advantages, such as having a constant vascular anatomy, and its dissection is not difficult [
1,
2,
3]. It is an especially good option for reconstruction in hand, forearm, elbow, foot and lower leg, head and neck region with of small- to medium-sized defects[
4,
5,
6,
7,
8]. Easy dissection, minimal donor-site morbidity, and a constant vascular anatomy with long pedicle are advantages of the flap [
9,
10]. However, There was no report of facial specific subunit reconstruction after malignant tumor ablation. In the present study, we evaluated patients that successfully underwent reconstruction using the free lateral arm flap after temple skin cancer surgery.
2. Materials and Methods
We included 12 patients who underwent reconstruction with fasciocutaneous type of free lateral arm flaps from 2020 to 2023 at a single institution. Our study comprised 7 women and 5 men, with a mean age of 60.6 (range: 47–81) years. Among the patients with cancer, six had squamous cell carcinoma, five had basal cell carcinoma and one had myxofibrosarcoma. We performed an institutional review board- approved retrospective review of our database to identify patient pools. The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Institutional Review Board of Seoul National University (B-2402-880-103). Demographics and operative data with specific information pertaining to all patients are presented in
Table 1.
3. Surgical Technique
The patient is placed in the supine position and the flap can be harvested with the upper limb on an arm table with elbow mild flexion position. Any pneumatic tourniquet or Esmark rubber tourniquet is not applied. The flap is outlined on the distal third of the lateral aspect of the arm. The axis of the skin island of the flap is centered with a line drawn from the deltoid insertion to the lateral epicondyle, which corresponds to the lateral intermuscular septum. Flap width commonly should not exceed 6 cm to allow for primary skin closure of the donor defect. Both from posterior or anterior directed flap elevation is possible. The flap is elevated deep to the muscular fascia over the triceps or brachialis, which is peeled until the septum is encountered.
This fascia is included in the flap to preserve vascularity. As the flap is elevated toward the septum, small muscular perforators are encountered and have to be coagulated or ligated. The fascia here is slightly more attached to the muscles. The flap can be elevated from distal to proximal. Staying deep to these vessels, the intermuscular septum is released to the level of humeral periosteum and the septum is now raised, with periosteum, from the humerus proximally to the level of deltoid insertion. As the dissection proceeds more proximally, the distance between the vessels and the humerus increases, and the dissection is easier. If the neurosensory flap is to be harvested, only the septal branch was included in the flap, with the preservation of posterior antebrahial cutaneous nerve(PABCN) under loupe magnification. At this stage, the radial nerve comes into view proximally. Once adequate pedicle length is gained, the posterior radial collateral artery(PRCA) and venae comitantes are divided. After flap transfer, microanastomosis is done between PRCA and superficial temporal artery, venae comitantes and superficial temporal vein.
4. Results
There was no tumor recurrence. All the flaps survived, provided stable coverage for the various defects, and produced satisfactory outcomes with good contours. Flap debulking surgery was not conducted in all cases. The dimensions of the lateral arm flap ranged from 3×4 to 5×7 cm (Average size of flap 22.7cm2). The average pedicle length was 6.1cm. All patients whose donor sites underwent primary closure attained full range of motion of their donor arm during the follow-up period, without radial nerve injury. The small sensory deficit on the dorsolateral aspect of the forearm occurred in 3 patients. The posterior cutaneous nerve of the forearm apparently was preserved in the other cases. The donor site scar was tolerated well by all patients. (
Table 1).
5. Patient Reports
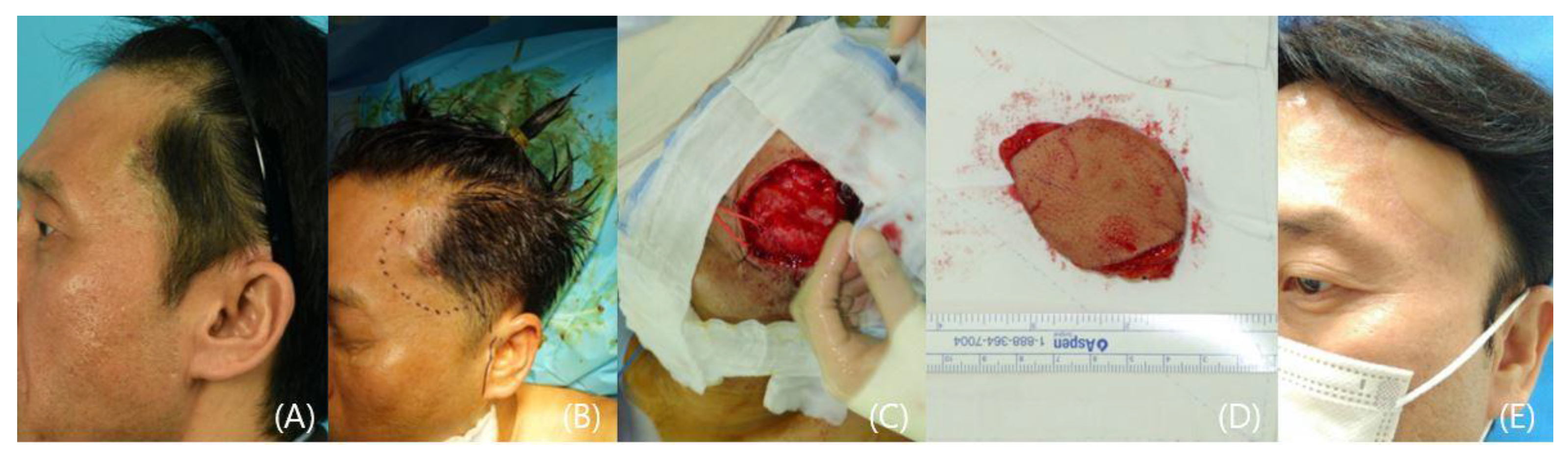
5.1. Patient I
A 81-year-old female patient was diagnosed with a 2.2 x 1.3 cm squamous cell carcinoma on her left temple area. The wide excision aimed to ensure complete tumor removal, and the temporal branch of the facial nerve was successfully preserved. The 4 x 6 cm sized lateral arm free flap was harvested and transferred to the defect area and it provided ample tissue coverage. The flap was healed uneventfully with no tumor recurrence (
Figure 1).
5.2. Patient 2
A 78-year-old woman was referred to our clinic with squamous cell cancer on the right temporal. She already underwent an excisional biopsy of a 2 × 1cm protruding lesion at other hospital and there was a linear scar remained on her temple. We planned reconstruction using a free lateral arm flap in the right upper arm with wide excision of the lesion (1cm free margin). After extensive excision of the tumor, the recipient superficial temporal artery and vein were prepared. After flap transfer, the superficial temporal vessels were anastomosed to the posterior radial collateral artery and its vena comitans, and the operation was completed after flap inset. After 7 months, the patient showed relative satisfaction with the surgical site scars at both the donor and recipient sites (
Figure 2).
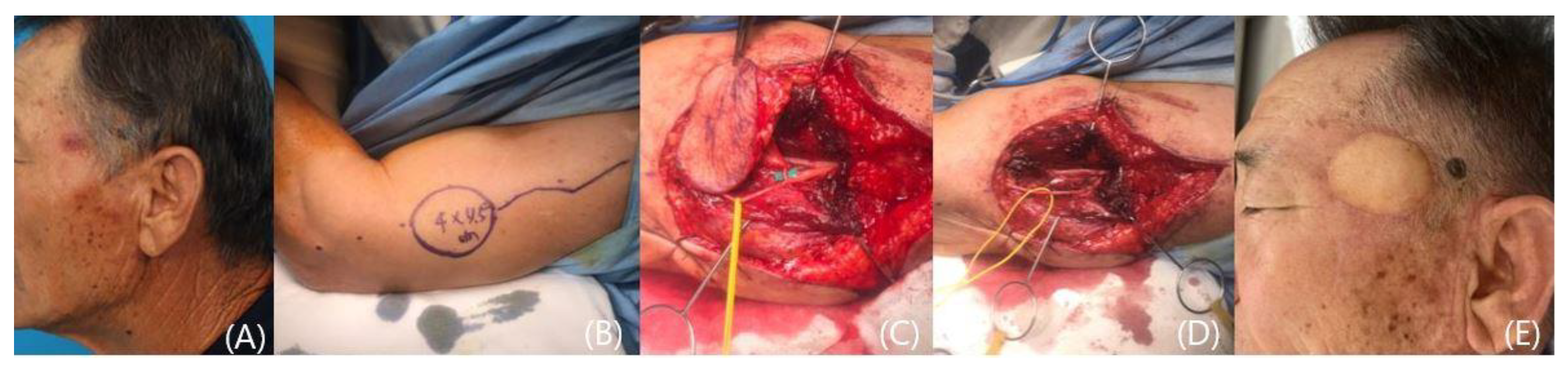
5.3. Patient 3
A 52-year-old male with a palpable mass on his left temporal area was referred to outpatients clinic. A punch biopsy was shown to be myxofibrosarcoma. We widely resected the tumor with 1~1.5cm surgical safety margin. Fresh frozen sections were found to be negative with free margins. The lateral arm fasciocutaneous flap was elevated and transferred to the defect. Microanastomosis was done using superficial temporal vessels as a recipient. The flap was healed uneventfully with no tumor recurrence (
Figure 3).
5.4. Patient 4
A 71-year-old man with left temple squamous cell carcinoma visited our clinic. The cancer measures 1.5 x 2.5 cm and the preoperative MRI showed invasion into subcutaneous tissue and closed to superficial temporal fascia. A radical resection was performed, including superficial temporal fascia with 1cm surgical safety margin. Fresh frozen sections showed free margins. We reconstructed the defect using a left fasciocutaneous lateral arm free flap. In the flap harvest, only the septal branch was included in the flap, with the preservation of posterior antebrahial cutaneous nerve(PABCN). The flap and the donor site healed uneventfully. Eleven months later, there is no tumor recurrence and flap showed excellent result with good contour. But, left forehead hemi-palsy was noticed owing to frontal branch of facial nerve resection (
Figure 4).
5.5. Patient 5
A 53-year-old man was visited our clinic with basal cell cancer on the right temple. We widely resected the tumor with 1cm surgical safety margin with successful preservation of the facial nerve temporal branches. We harvested 3 x 4 cm sized lateral arm flap and prepared superficial temporal artery and vein underneath the tumor. The flap was healed uneventfully with no tumor recurrence (
Figure 5).
6. Discussion
The facial defects arising from tumor surgery can lead to esthetic and functional deficits. In facial temple subunit region reconstruction, it requires a pliable flap with a good color match and flap integration into the recipient site for optimal contour [
11]. Free flap surgery has been widely performed in the reconstruction of various defects due to several definite reasons. High success rates, fast healing, and good functional and esthetic results have popularized the application of free flaps after tumor ablative procedures. Several types of free flaps are available in the body and surgeons can choose from a wide variety of flaps.
For many years, the radial forearm flap had been the fasciocutaneous flap of choice for reconstruction in the head and neck region. This flap provides a very thin skin paddle, ideal for intraoral reconstruction and for all areas needing a very pliable flap [
12]. However, recently, donor site morbidity has been considered as important as recipient site morbidity [
13]. When a radial forearm flap is harvested, a major supplying artery to the hand has to be sacrificed, and the use of the radial artery might compromise the vascular supply to the hand. Moreover, the scar of the radial forearm flap is a difficult area to cover, and an additional skin graft may increase the scar width, causing abnormal pigmentation and depression [
12]. The ALT or TDAP flap is a medium or large sized flap with particularly long pedicles; however, in the temple subunit, it needs not large sized flap nor long flap pedicle. Also these flap have an anatomical variation and is not stable, which subsequently increases the risk of complications, including partial necrosis of the flap [
14,
15]. For this reason, the lateral arm flap is considered a more suitable alternative. It has a constant vascular anatomy and there is no damage to the vascular supply of the hand because the flap contains a non-essential terminal branch of the profunda brachii artery [
16,
17,
18]. The lateral arm area is among the donor sites with a better color match than the radial, fibula, thigh and latissimus region. The flap may be harvested in a bloodless field under a tourniquet. Especially in oncologic and multi-morbid patients, it is important to reduce operating time. This is possible with a two-team approach, with one team raising the flap and the other team resecting the tumor and preparing the recipient site [
19,
20].
There are only a few limitations restricting the use of the lateral arm flap. The amount of tissue available restricts its use to the reconstruction of small- to moderate-sized defects. But, for temple subunit reconstruction, lateral arm flap is a perfect choice because there doesn’t need large skin paddle. For large sized skin defect reconstruction, other fasciocutaneous flap like ALT or TDAP flap will be needed. The relatively small diameter and short pedicle length of the vessels are another disadvantage of the flap. But, for temple reconstruction, it was long enough to reach the recipient superficial temporal vessels and shows adequate size to do microanastomosis [
21].
Postoperative sensory disturbances in the dorsolateral forearm area might be disturbing to the patient but will eventually improve with time [
22]. For the better sensory preserving, surgeons can isolate the septal branch of the posterior antebrachial cutaneous nerve in the flap and maintain the main trunk within a few centimeters of the proximal lateral epicondyle to prevent permanent sensory loss after surgery [
23]. In contrast, sometimes it requires temporal branch of facial nerve reconstruction after resection with the cancer, especially in squamous cell cancer or melanoma cases. If the cancer was adjacent to this facial motor nerve, there is no choice but to do en-bloc excision including nerve to prevent perineural invasion. In that case, the posterior cutaneous nerve of the lateral arm may be used as a vascularized nerve graft with the lateral arm free flap. But this case is not reported yet. Further precise anatomical and clinical research is required.
7. Conclusion
A variety of flaps are available and ultimate success depends on the optimal choice of the flap. Easy and quick dissection, design variability, and potential sensory innervation make the lateral forearm flap superior to some other fasciocutaneous flaps. We find that the lateral arm flap is very reliable and versatile in the reconstruction of facial temple subunit defects reconstruction.
Author Contributions
Conceptualization, S.E.; Formal analysis, S.L., and S.E.; Investigation, S.L. and S.E.; Data curation, S.E.; Writing-original drat, S.E.; Writiing-review & editing, S.E. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Institutional Review Board of Seoul National University (B-2403-886-102).
Informed Consent Statement
Patient consent was waived due to retrospective design of the study.
Data Availability Statement
The Data presented in this study are available on request from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Civantos, F.J., Jr.; Burkey, B.; Lu, F.L.; Armstrong, W. Lateral arm microvascular flap in head and neck reconstruction. Arch Otolaryngol Head Neck Surg 1997, 123, 830–836. [Google Scholar] [CrossRef] [PubMed]
- Nahabedian, M.Y.; Deune, E.G.; Manson, P.N. Utility of the lateral arm flap in head and neck reconstruction. Ann Plast Surg 2001, 46, 501–505. [Google Scholar] [CrossRef] [PubMed]
- Marques Faria, J.C.; Rodrigues, M.L.; Scopel, G.P.; Kowalski, L.P.; Ferreira, M.C. The versatility of the free lateral arm flap in head and neck soft tissue reconstruction: Clinical experience of 210 cases. J Plast Reconstr Aesthet Surg 2008, 61, 172–179. [Google Scholar] [CrossRef] [PubMed]
- Akinci, M.A.S.; Kamiloglu, S.; Erçetin, O. Lateral arm free flaps in the defects of the upper extremity-a review of 72 cases. Hand Surg 2005, 10, 177–185. [Google Scholar] [CrossRef] [PubMed]
- Atzei, A.; Pignatti, M.; Udali, G.; Cugola, L.; Maranzano, M. The distal lateral arm flap for resurfacing of extensive defects of the digits. Microsurgery 2007, 27, 8–16. [Google Scholar] [CrossRef] [PubMed]
- Smit, J.M.; Darcy, C.M.; Audolfsson, T.; Hartman, E.H.; Acosta, R. Multilayer reconstructions for defects overlying the Achilles tendon with the lateral-arm flap: Long-term follow-up of 16 cases. Microsurgery 2012, 32, 438–444. [Google Scholar] [CrossRef] [PubMed]
- Ulusal, B.G.; Lin, Y.T.; Ulusal, A.E.; Lin, C.H. Free lateral arm flap for 1-stage reconstruction of soft tissue and composite defects of the hand: A retrospective analysis of 118 cases. Ann Plast Surg 2007, 58, 173–178. [Google Scholar] [CrossRef] [PubMed]
- Jordan, S.W.; Wayne, J.D.; Dumanian, G.A. The pedicled lateral arm flap for oncologic reconstruction near the shoulder. Ann Plast Surg 2015, 74, 30–33. [Google Scholar] [CrossRef]
- Windhofer, C.; Michlits, W.; Karlbauer, A.; Papp, C. Treatment of segmental bone and soft-tissue defects of the forearm with the free osteocutaneous lateral arm flap. J Trauma 2011, 70, 1286–1290. [Google Scholar] [CrossRef]
- Haas, F.; Rappl, T.; Koch, H.; Pittler, P.; Scharnagl, E. Free osteocutaneous lateral arm flap: Anatomy and clinical applications. Microsurgery 2003, 23, 87–95. [Google Scholar] [CrossRef]
- Olshinka, A.; Maricevich, R.; Shay, T.; Cohen, A.A.; Ad-El, D.; Ali, K. Algorithm for Temple Reconstruction With Consideration of Anatomic and Defect Characteristics. J Craniofac Surg. 2020, 31, 1261–1265. [Google Scholar] [CrossRef]
- Cho, K.; Park, J.; Eun, S. The Central Facial Defect Reconstruction Using a Radial Forearm Free Flap after Malignant Cutaneous Tumor Ablation. J Clin Med. 2023, 12, 7148. [Google Scholar] [CrossRef] [PubMed]
- Hamdi, M.; Coessens, B.C. Evaluation of the donor site morbidity after lateral arm flap with skin paddle extending over the elbow joint. Br J Plast Surg 2000, 53, 215–219. [Google Scholar] [CrossRef]
- Klinkenberg, M.; Fischer, S.; Kremer, T.; Hernekamp, F.; Lehnhardt, M.; Daigeler, A. Comparison of anterolateral thigh, lateral arm, and parascapular free flaps with regard to donor-site morbidity and aesthetic and functional outcomes. Plast Reconstr Surg 2013, 131, 293–302. [Google Scholar] [CrossRef]
- Busnardo, F.F.; Coltro, P.S.; Olivan, M.V.; Faes, J.C.; Lavor, E.; Ferreira, M.C.; et al. Anatomical comparison among the anterolateral thigh, the parascapular, and the lateral arm flaps. Microsurgery 2015, 35, 387–392. [Google Scholar] [CrossRef] [PubMed]
- Sauerbier, M.; Germann, G.; Giessler, G.A.; Sedigh Salakdeh, M.; Döll, M. The free lateral arm flap-a reliable option for reconstruction of the forearm and hand. Hand (N Y) 2012, 7, 163–171. [Google Scholar] [CrossRef] [PubMed]
- Sullivan, M.J.C.W.; Kuriloff, D.B. Lateral Arm Free Flap in Head and Neck Reconstruction. Arch Otolaryngol Head Neck Surg 1992, 118, 1095–1101. [Google Scholar] [CrossRef]
- Schipper, J.R.G.; Boedeker, C.C.; Fradis, M.; Golz, A.; Gellrich, N.C. Lateral upper arm free flap for primary reconstruction of pharyngeal defects in ablative oncological surgery; Report of six consecutive cases. Ann Otol Rhinol Laryngol 2003, 112, 611–616. [Google Scholar] [CrossRef]
- Kang, S.Y.; Old, M.O.; Teknos, T.N. Lateral arm free tissue transfer for parotid reconstruction: A pictorial essay. Head Neck 2017, 39, 1015–1019. [Google Scholar] [CrossRef]
- Kang, S.H.; Jeon, S.; Jung, Y.H.; Eun, S.C. Verifying the Versatility and Reliability of Free Lateral Arm Flap for Head and Neck Reconstruction. J Craniofac Surg. 2020, 31, 688–693. [Google Scholar] [CrossRef]
- Chang, E.I.; Ibrahim, A.; Papazian, N.; Jurgus, A.; Nguyen, A.T.; Suami, H.; et al. Perforator Mapping and Optimizing Design of the Lateral Arm Flap: Anatomy Revisited and Clinical Experience. Plast Reconstr Surg 2016, 138, 300e–306e. [Google Scholar] [CrossRef] [PubMed]
- Kalbermatten, D.F.; Wettstein, R.; vonKanel, O.; Erba, P.; Pierer, G.; Wiberg, M.; Haug, M. Sensate lateral arm flap for defects of the lower leg. Ann Plast Surg 2008, 61, 40–46. [Google Scholar] [CrossRef] [PubMed]
- Ki, S.H. Lateral Arm Free Flap With Preservation of the Posterior Antebrachial Cutaneous Nerve. Ann Plast Surg 2016, 76, 517–520. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).