1. Introduction
The contemporary lifestyle, characterized by its frenetic pace and myriad stressors, has given rise to an unprecedented focus on holistic well-being [
1]. The consequences of neglecting the intricate balance between physical and mental health are becoming increasingly evident, with a surge in chronic conditions and a decline in overall quality of life [
2]. As society grapples with the repercussions of this reality, researchers have delved into the complex connections between the mind and the body, seeking insights that can inform strategies for promoting lasting health. The advent of psychoneuroimmunology has proven instrumental in unraveling the intricate dance between psychological states, immune function, and overall health [
3]. Among the myriad avenues explored within this interdisciplinary field, the gut-brain axis has emerged as a pivotal player in shaping our understanding of how mental well-being and physical health intertwine [
4].
The Gut-Brain Axis (GBA), a multifaceted communication network, establishes a profound connection between the central nervous system and the enteric nervous system embedded in the gastrointestinal tract. This dynamic interplay enables bidirectional communication, allowing the gut to influence cognitive and emotional processes, while the brain exerts regulatory control over gastrointestinal function [
5]. The implications of this symbiotic relationship extend beyond traditional realms, permeating into domains of nutrition, psychology, and overall health. Against this backdrop, the synergy between mindfulness and the GBA stands out as a compelling area of investigation with far-reaching implications for health-related quality of life [
6].
Mindfulness, a practice rooted in ancient contemplative traditions, has garnered increasing attention in contemporary scientific discourse for its potential to foster mental well-being and mitigate the effects of stress [
7]. The convergence of mindfulness with the GBA opens a fascinating avenue for understanding how the intentional cultivation of present-moment awareness may impact not only psychological states but also the intricate balance of the gut microbiome and gut function. Furthermore, the role of nutrition in this paradigm cannot be overstated, as the symbiotic relationship between the gut microbiota and dietary patterns influences both physical and mental health [
8].
An example of a prudent dietary pattern that has been extensively researched and found to be beneficial for both gut microbiota as well as overall physical and mental health, is the Mediterranean diet. The Mediterranean diet is a nutritional pattern inspired by the traditional eating habits of countries bordering the Mediterranean Sea, emphasizing fruits, vegetables, whole grains, fish, and olive oil while minimizing red meat and processed foods. It is associated with various health benefits, including reduced risk of heart disease and improved overall well-being [
9]. The Mediterranean diet and lifestyle share a common philosophical basis with mindfulness, as they both encompass values such as eudaemonia, sustainability and sociability [
10].
As researchers delve into the interconnections among mindfulness, nutrition, and the GBA, a compelling narrative emerges, suggesting that interventions targeting these intertwined elements may hold the key to enhancing the health-related quality of life [
11]. Health-Related Quality of Life (HRQoL) serves as a comprehensive metric encompassing the multidimensional aspects of an individual's well-being, reflecting not only the absence of disease but also the intricate interplay between physical health, mental states, and social functioning [
12]. In the context of the paradigm explored in this study, HRQoL emerges as a pivotal focal point, particularly concerning individuals grappling with inflammatory bowel diseases.
Inflammatory Bowel Disease (IBD) is a chronic disorder characterized by inflammation of the digestive tract, including conditions such as Crohn's disease and ulcerative colitis. For those affected by IBD, the challenges extend beyond the physical manifestations of the condition, encompassing the psychological toll of managing chronic symptoms, the impact on daily activities, and the potential disruption of social interactions [
13]. Understanding and enhancing HRQoL in the realm of IBD necessitates a nuanced exploration of factors such as mindfulness and the GBA, acknowledging the interconnected web of influences that contribute to the overall well-being of individuals facing these complex health challenges.
This research aims to unravel the intricate dynamics shaping HRQoL within the context of healthy individuals as well as IBD patients, offering insights that may inform holistic approaches to improve their quality of life. By investigating the convergence of mindfulness, nutrition, and the GBA on HRQoL, this cross-sectional study aims to contribute to the growing body of knowledge that underscores the importance of addressing mental well-being, nutrition, and the GBA in tandem. The ultimate goal of this study is to shed light on novel therapeutic avenues that transcend conventional approaches, addressing the holistic needs of individuals grappling with these complex conditions.
2. Materials and Methods
2.1. Design and Procedure
This research employed a cross-sectional research design, utilizing an online survey administered in both the Greek and English languages via the Sogolytics online survey tool [
14]. The initial two survey questions served as inclusion and exclusion criteria, ensuring participants' acknowledgment of the study's terms and conditions and verifying their age within the specified range of 18 to 65 years. The survey was distributed through direct messaging on various social media platforms, accompanied by follow-up reminders to foster participant engagement and establish a platform for addressing any inquiries or concerns related to the study. This hybrid approach capitalizes on the advantages of both web-based and mailed questionnaires [
15,
16,
17].
Prior to commencing the data collection process, the research's objectives and hypotheses were explicitly outlined, offering a comprehensive framework for the subsequent analysis and interpretation of the research findings. The final sample that satisfied the inclusion-exclusion criteria comprised a total of 315 adults.
2.2. Scales
2.2.1. Mindfulness Awareness Attention Scale (MAAS-15)
The Mindful Attention Awareness Scale (MAAS-15) stands as a robust and widely accepted tool for quantifying mindfulness [
18]. Developed by Kirk Warren Brown and Richard M. Ryan, this self-report measure targets an individual's receptive awareness of and attention to present-moment experiences [
19]. Spanning 15 items, the MAAS captures the essential facets of mindfulness, emphasizing attention and awareness in everyday situations. Its design diverges from conventional mindfulness scales by probing into the innate capacity for sustained attention across various activities rather than focusing solely on meditation or specific mindfulness practices. This inclusive approach renders the MAAS versatile, offering a comprehensive assessment applicable to diverse contexts and populations. Its psychometric properties contribute to its credibility as a reliable measure; the scale demonstrates high internal consistency, test-retest reliability, and construct validity, aligning well with the theoretical underpinnings of mindfulness. Moreover, the MAAS avoids jargon and convoluted language, making it accessible and user-friendly for respondents, irrespective of their familiarity with mindfulness concepts. Its widespread use across cultural and demographic boundaries attests to its transcultural applicability, a crucial aspect in measuring such subjective experiences [
20]. The MAAS-15 scale is validated in Greek [
21]. In our study MAAS-15 had a reliable internal consistency index (Cronbach’s α), α=0.896
2.2.2. Mediterranean Diet Adherence Scale (14-MEDAS)
The 14-MEDAS scale, a creation of Schroeder et al. [
22] within the PREDIMED study framework, is a 14-item tool designed to assess adherence to the Mediterranean diet. A sample question from the 14-MEDAS is: "Is olive oil your primary culinary fat?" Each query is rated on a scale from 0 to 1, with a final 14-MEDAS score ranging from 0 to 14 points. Scores between 0 and 5 reflect low adherence, 6 to 9 indicate moderate adherence, and 10 to 14 demonstrate high adherence [
22]. Validated in various countries and languages, including Greek, the Greek version of 14-MEDAS displayed a significant concordance (81.2 ± 10.7%) with the Food Frequency Questionnaire (FFQ) in a study by García-Conesa et al. [
23], affirming its validity and reliability as a research instrument for evaluating adherence to the Mediterranean diet within the Greek population.
2.2.3. The EuroQol 5-Dimension 5-Level Questionnaire (EQ-5D-5L)
The EQ-5D-5L scale serves as a pivotal instrument in assessing health-related quality of life (HRQoL), offering a comprehensive and multidimensional evaluation. Developed by the EuroQol Group, this standardized measure evaluates health status across five domains: mobility, self-care, usual activities, pain/discomfort, and anxiety/depression. What sets the EQ-5D-5L apart is its simplicity and ease of administration; respondents rate their health state on each dimension using a five-level scale, capturing a more nuanced and refined assessment compared to its predecessor, the EQ-5D-3L. Its improved granularity allows for a more precise quantification of health states, enhancing sensitivity to subtle changes in health conditions and treatment outcomes [
24]. Furthermore, the EQ-5D-5L is validated in Greek [
25]. Its versatility and brevity make it suitable for various applications, including clinical trials, population health surveys, and economic evaluations in healthcare. This standardized measure facilitates cross-comparisons across different health conditions and interventions, enabling healthcare professionals, researchers, and policymakers to make informed decisions based on a robust assessment of HRQoL [
26]. Despite its widespread use and applicability, the EQ-5D-5L does have limitations, such as its generic nature, which might not capture condition-specific nuances. Nonetheless, its ability to succinctly capture multidimensional aspects of HRQoL, its simplicity in administration, and its adaptability across diverse populations cement its position as an indispensable tool in assessing health outcomes and guiding healthcare interventions [
27]. The score of the EQ-5D-5L scale (EQIndex) is calculated by converting responses on five dimensions of health (mobility, self-care, usual activities, pain/discomfort, and anxiety/depression) into a single index using country-specific value sets, with a range typically between -0.594 and 1, where 1 represents full health and values less than 0 indicating health states worse than death [
28].
2.3. Demographic and Anthropometric Information
To minimize survey dropout rates [
29], questions pertaining to demographic and somatometric data were positioned at the survey's conclusion. Demographic inquiries encompassed aspects such as education, employment status, marital status, and gender. Participants were requested to provide their height and weight for the computation of their Body Mass Index (BMI). While relying on self-reported height and weight may not yield the most accurate data regarding respondents' body composition, it remains a valid approach for calculating BMI in adult populations across diverse socio-demographic groups [
30]. Based on established guidelines [
31], individuals' BMIs were classified into subcategories, including underweight, normal weight, overweight, and obesity.
2.4. Statistical Analysis
A thorough review of the data was conducted to identify any potential omissions. Instances where participants abruptly discontinued the questionnaire (Missing Completely at Random) resulted in the exclusion of the respective data from the analysis [
32]. In the event of accidental oversights (Missing at Random), the missing data points were substituted with the mean value derived from all respondents' answers.
The data was exported in a format compatible with import and processing in SPSS v28. Analysis and visualization of the data were carried out using the statistical analysis software SPSS v28. Prior to subjecting the data to statistical tests, a regularity check was performed to ensure their distribution met established criteria. The literature recommends conducting the regularity test before engaging in statistical analyses. To ensure the most accurate and reliable assessment of regularity, a combination of visual examination and the Shapiro-Wilk test was employed [
33]. Statistical analysis was performed by Pearson’s correlation, Independent samples t-test and one-way ANOVA for continuous variables found to follow the normal distribution by the use of Kolmogorov-Smirnov test. Multinomial logistic regression analysis was performed to assess the influence of mindfulness in HRQoL in individuals with IBD, after adjustment for possible confounders. The predetermined statistical significance level was established at p<0.05.
3. Results
3.1. Subjects
The survey drew 376 participants. After eliminating 35 respondents who did not fulfill the survey's inclusion requirements, as well as three incomplete (less than 50% of total questions answered) or random responses (items answered in less than 3 minutes), the final sample size was 338 individuals (75.4% female, 24.3% male, 0.3% non-binary).
There was a significant difference (p<0.05) in the means of MAAS-15, MEDAS, and BMI across age groups, with younger participants having lower scores. Higher education level was associated with significantly higher MAAS-15 and MEDAS-14 scores (p<0.05). Married participants had significantly higher (p<0.05) MAAS-15 scores.
3.2. Correlations between Mindfulness, the Mediterranean Diet, HRQoL and BMI among Healthy Individuals
In order to investigate the potential associations between MAAS-15, 14-MEDAS, EQIndex, and BMI in healthy individuals, Pearson’s correlation coefficients were calculated. The statistical analysis unveiled a significant correlation between MAAS-15 and 14-MEDAS with EQIndex. Additionally, a negative correlation was observed between EQIndex and BMI (Table 1).
Table 1.
Pearson’s correlations (r) between MAAS-15 (mindfulness), 14-MEDAS (Mediterranean diet), EQIndex (HRQoL) and BMI.
Table 1.
Pearson’s correlations (r) between MAAS-15 (mindfulness), 14-MEDAS (Mediterranean diet), EQIndex (HRQoL) and BMI.
| |
MAAS-15 |
14-MEDAS |
EQIndex |
BMI |
| MAAS-15 |
1 |
0.080 |
0.389**
|
0.007 |
| 14-MEDAS |
0.080 |
1 |
0.131*
|
-0.003 |
| EQIndex |
0.389**
|
0.131*
|
1 |
-0.208**
|
| BMI |
0.007 |
-0.003 |
-0.208**
|
1 |
3.2. Correlations between Mindfulness, the Mediterranean Diet, HRQoL and BMI in Individuals with IBD
To explore potential relationships among MAAS-15, 14-MEDAS, EQIndex, and BMI in patients with IBD, Pearson’s correlation coefficients were computed. The statistical analysis revealed a significant correlation solely between MAAS-15 and EQIndex (Table 2). There was no statistically significant correlation between EQIndex, 14-MEDAS and BMI.
Table 2.
Pearson’s correlations (r) between MAAS-15 (mindfulness), 14-MEDAS (Mediterranean diet), EQIndex (HRQoL) and BMI in IBD patients.
Table 2.
Pearson’s correlations (r) between MAAS-15 (mindfulness), 14-MEDAS (Mediterranean diet), EQIndex (HRQoL) and BMI in IBD patients.
| |
MAAS-15 |
14-MEDAS |
EQIndex |
BMI |
| MAAS-15 |
1 |
0.041 |
0.414*
|
0.066 |
| 14-MEDAS |
0.041 |
1 |
0.016 |
-0.011 |
| EQIndex |
0.414*
|
0.016 |
1 |
-0.137 |
| BMI |
0.066 |
-0.011 |
-0.137 |
1 |
3.3. HRQoL Assessments in Healthy Individuals and Individuals with IBD
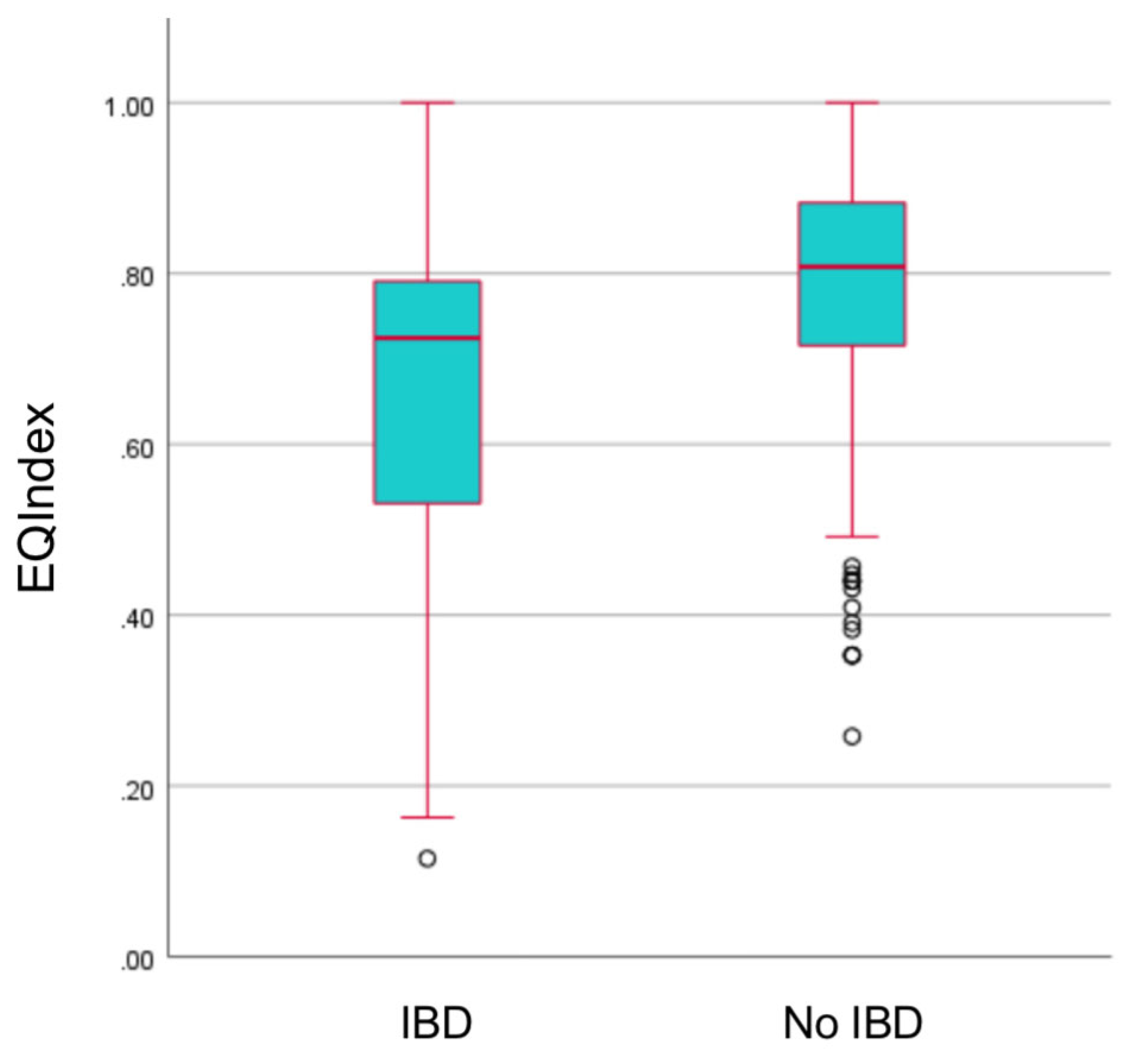
The analysis of HRQoL assessments revealed notable distinctions between healthy individuals and those diagnosed with IBD. Individuals with IBD exhibited significantly lower HRQoL scores, as indicated by their EQIndex scores, compared to healthy counterparts (Figure 1). Furthermore, a comprehensive examination of the EQ-5D-5L scale dimensions revealed statistically significant differences between individuals with IBD and healthy individuals across all aspects, including mobility, self-care, usual activities, pain/discomfort, and anxiety/depression.
Figure 1.
Boxplots depicting the statistically significant difference in HRQoL scores between IBD patients and healthy individuals.
Figure 1.
Boxplots depicting the statistically significant difference in HRQoL scores between IBD patients and healthy individuals.
3.4. Mindfulness, the Mediterranean Diet and HRQoL
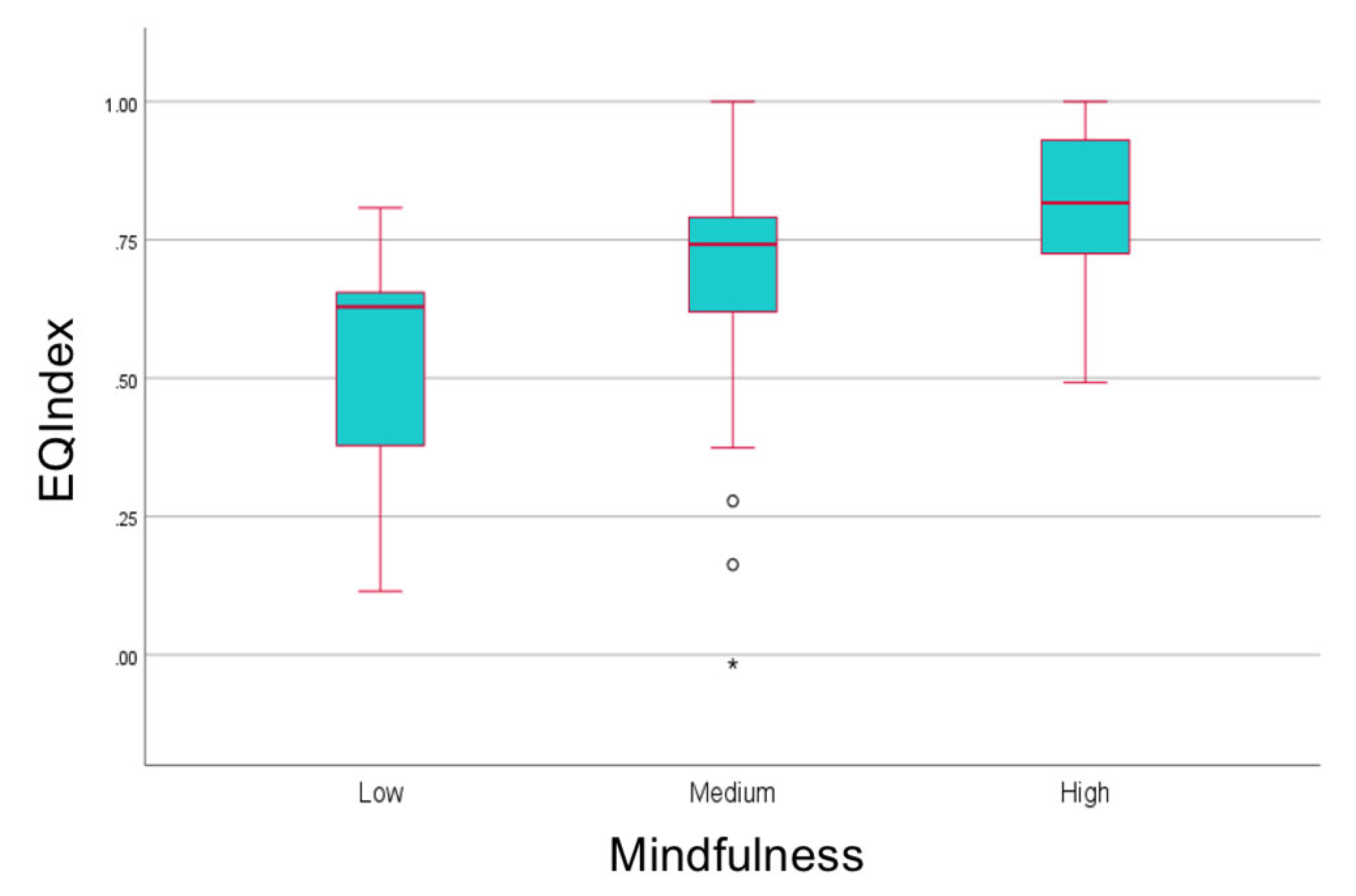
In our investigation, Mindfulness demonstrated a moderate correlation (r = 0.365, p < 0.001) with HRQoL for healthy individuals, while mindfulness had robust correlation (r = 0.414, p < 0.001) with HRQoL among individuals diagnosed with IBD (Figure 2). This finding highlights a stronger association between mindfulness and the perceived quality of health among IBD patients.
Figure 2.
Boxplots of HRQoL scores in different mindfulness levels among individuals with IBD.
Figure 2.
Boxplots of HRQoL scores in different mindfulness levels among individuals with IBD.
Moreover, multinomial logistic regression analysis revealed that heightened levels of mindfulness served as predictive factors for improved HRQoL in individuals living with IBD (OR: 1.101, 95% CI: 1.008, 1.202, p < 0.05) when compared to those with lower levels of mindfulness (Table 3).
Table 3.
Multinomial logistic analysis results.
Table 3.
Multinomial logistic analysis results.
| |
OR |
95% CI |
p-value |
| Mindfulness (Low vs High) |
1.101 |
1.008-1.202 |
<0.05 |
4. Discussion
The present study represents the first known investigation into the interconnections among mindfulness, the GBA, and HRQoL in Greece, specifically in individuals diagnosed with IBD. By focusing on this intersection, our research expands upon existing literature concerning the psychological functioning of individuals with IBD [
34]. While previous studies have examined various aspects of psychological well-being and coping strategies in this population [
35], to our knowledge, none have explored the combined influence of mindfulness and factors affecting the gut-brain axis such as the Mediterranean diet on HRQoL in individuals with IBD.
The results of the study examining the association between mindfulness, the GBA, and HRQoL provide valuable insights into the interplay of psychological and physiological factors in influencing well-being, particularly in the context of IBD. The findings reveal several key observations. Firstly, among healthy participants, there is a moderate correlation between HRQoL and mindfulness, indicating that individuals with higher levels of mindfulness tend to report better overall well-being. This aligns with previous research demonstrating the positive impact of mindfulness on various aspects of health and quality of life [
36,
37,
38]. Similarly, the low correlation between HRQoL and adherence to the Mediterranean Diet suggests that while diet may influence certain dimensions of well-being, its association with overall quality of life may be less pronounced. These findings corroborate existing literature highlighting the complex relationship between dietary habits and HRQoL, with dietary patterns such as the Mediterranean Diet often linked to improved health outcomes but with varying effects on overall well-being [
39].
In contrast, individuals with IBD exhibit significantly lower mean HRQoL scores compared to healthy counterparts, underscoring the substantial impact of this chronic inflammatory condition on overall well-being. However, within the IBD population, higher levels of mindfulness are strongly correlated with better HRQoL. This novel finding suggests that mindfulness interventions may hold promise for mitigating the negative effects of IBD on quality of life. This aligns with previous research indicating the beneficial effects of mindfulness-based interventions on symptom management and coping strategies in individuals with chronic illnesses [
40].
Furthermore, the study identifies elevated mindfulness levels as predictive factors for higher HRQoL in IBD patients, highlighting the potential therapeutic value of mindfulness-based interventions in clinical practice. This supports the hypothesis that enhancing mindfulness may lead to improvements in quality of life among individuals with chronic inflammatory conditions.
However, it's essential to interpret these findings within the broader context of the study's limitations. The cross-sectional design limits the ability to establish causality or determine the direction of the observed associations. Additionally, the reliance on self-reported measures introduces the possibility of response bias and does not capture objective physiological markers of mindfulness or dietary adherence. Moreover, the study's sample size may restrict the generalizability of the findings, warranting caution in extrapolating the results to broader populations.
Future research directions may include longitudinal studies to assess the long-term effects of mindfulness interventions on HRQoL in individuals with IBD, as well as randomized controlled trials to evaluate the efficacy of mindfulness-based interventions as adjunctive treatments for IBD. Additionally, investigations into the underlying mechanisms through which mindfulness influences the GBA and physiological pathways implicated in IBD could provide further insights into the potential therapeutic targets for intervention. Overall, while the study's findings offer promising avenues for enhancing quality of life in individuals with IBD, further research is needed to validate and expand upon these preliminary observations.
Author Contributions
Conceptualization, Efstratios Christodoulou ; Data curation, Efstratios Christodoulou ; Formal analysis, Efstratios Christodoulou ; Investigation, Tsambika Mpali and Maroula-Eleni Dimitriadou; Methodology, Efstratios Christodoulou , Tsambika Mpali and Maroula-Eleni Dimitriadou; Project administration, Antonios Koutelidakis; Resources, Tsambika Mpali and Maroula-Eleni Dimitriadou; Software, Efstratios Christodoulou , Tsambika Mpali and Maroula-Eleni Dimitriadou; Supervision, Antonios Koutelidakis; Validation, Antonios Koutelidakis; Visualization, Antonios Koutelidakis; Writing – original draft, Efstratios Christodoulou ; Writing – review & editing, Antonios Koutelidakis. All authors have read and agreed to the published version of the manuscript.
Funding
External funding was not secured for this research
Institutional Review Board Statement
This study adhered to the principles outlined in the Declaration of Helsinki and received approval from the University of the Aegean’s ethics and deontology committee (approval no. 17715/09.09.2021).
Informed Consent Statement
All participants provided informed consent prior to their involvement in this study. Consent has also been obtained from the patient(s) for publication of this paper.
Data Availability Statement
The data presented in this study are available upon request from the corresponding author.
Acknowledgments
The authors extend their gratitude to all individuals who participated in this study.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Christodoulou, E.; Markopoulou, V.; Koutelidakis, A.E. Exploring the Link between Mindful Eating, Instagram Engagement, and Eating Disorders: A Focus on Orthorexia Nervosa. Psychiatry International. 2024, 5, 27–38. [Google Scholar] [CrossRef]
- Christodoulou E, Pavlidou E, Mantzorou M, et al. Depression is associated with worse health-related quality of life, lower physical activity levels, and inadequate sleep quality in a Greek elderly population. Psychol Health Med. 2023, 28, 2486–2500. [Google Scholar] [CrossRef] [PubMed]
- Oroian, B.A.; Costandache, G.I.; Salaru, A.; Ionescu, P.F.; Nechita, P. The wrinkles of the soul- a psychoneuroimmunological approach to aging. Eur Psychiatry. 2023, 66 (Suppl 1). [Google Scholar] [CrossRef]
- Zheng, Y.; Bonfili, L.; Wei, T.; Eleuteri, A.M. Understanding the Gut–Brain Axis and Its Therapeutic Implications for Neurodegenerative Disorders. Nutrients. 2023, 15, 4631. [Google Scholar] [CrossRef] [PubMed]
- Saxami, G.; Kerezoudi, E.N.; Eliopoulos, C.; Arapoglou, D.; Kyriacou, A. The Gut–Organ Axis within the Human Body: Gut Dysbiosis and the Role of Prebiotics. Life. 2023, 13, 2023. [Google Scholar] [CrossRef] [PubMed]
- Peppas, S.; Pansieri, C.; Piovani, D.; Danese, S.; Peyrin-Biroulet, L.; Tsantes, A.G.; Brunetta, E.; Tsantes, A.E.; Bonovas, S. The Brain-Gut Axis: Psychological Functioning and Inflammatory Bowel Diseases. Journal of Clinical Medicine. 2021, 10, 10–377. [Google Scholar] [CrossRef] [PubMed]
- Foale, S.; Botma, Y.; Heyns, T. Mindfulness-based interventions to support wellbeing of adults in low socio-economic settings: a realist review. BMC Complement Med Ther. 2024, 24, 52. [Google Scholar] [CrossRef] [PubMed]
- Guiducci, L.; Nicolini, G.; Forini, F. Dietary Patterns, Gut Microbiota Remodeling, and Cardiometabolic Disease. Metabolites. 2023, 13, 760. [Google Scholar] [CrossRef] [PubMed]
- Georgoulis M, Damigou E, Chrysohoou C, et al. Mediterranean diet trajectories and 20-year incidence of cardiovascular disease: The ATTICA cohort study (2002-2022). Nutr Metab Cardiovasc Dis. 2024, 34, 153–166. [Google Scholar] [CrossRef]
- Christodoulou, E.; Deligiannidou, G.-E.; Kontogiorgis, C.; Giaginis, C.; Koutelidakis, A.E. Fostering Resilience and Wellness: The Synergy of Mindful Eating and the Mediterranean Lifestyle. Applied Biosciences. 2024, 3, 59–70. [Google Scholar] [CrossRef]
- Lee CC, Yang HW, Liu CJ, et al. Unraveling the connections between gut microbiota, stress, and quality of life for holistic care in newly diagnosed breast cancer patients. Sci Rep. 2023, 13, 17916. [Google Scholar] [CrossRef]
- Yin, S.; Njai, R.; Barker, L.; Siegel, P.Z.; Liao, Y. Summarizing health-related quality of life (HRQOL): development and testing of a one-factor model. Popul Health Metr. 2016, 14, 22. [Google Scholar] [CrossRef]
- Greywoode, R.; Ullman, T.; Keefer, L. National Prevalence of Psychological Distress and Use of Mental Health Care in Inflammatory Bowel Disease. Inflamm Bowel Dis. 2023, 29, 70–75. [Google Scholar] [CrossRef]
- Christodoulou, E.; Meca, A.; Koutelidakis, A.E. Herbal Infusions as a Part of the Mediterranean Diet and Their Association with Psychological Resilience: The Paradigm of Greek Mountain Tea. Nutraceuticals. 2023, 3, 438–450. [Google Scholar] [CrossRef]
- Menon, V.; Muraleedharan, A. Internet-based surveys: relevance, methodological considerations and troubleshooting strategies. Gen Psychiatr. 2020, 33, e100264. [Google Scholar] [CrossRef]
- Saeedbakhsh, M.; Omid, A.; Khodadoostan, M.; Shavakhi, A.; Adibi, P. Using instant messaging applications to promote clinical teaching of medical students. J Educ Health Promot. 2022, 11, 254. [Google Scholar] [CrossRef]
- Christodoulou, E.; Deligiannidou, G.-E.; Kontogiorgis, C.; Giaginis, C.; Koutelidakis, A.E. Natural Functional Foods as a Part of the Mediterranean Lifestyle and Their Association with Psychological Resilience and Other Health-Related Parameters. Applied Sciences. 2023, 13, 4076. [Google Scholar] [CrossRef]
- Osman, A.; Lamis, D.A.; Bagge, C.L.; Freedenthal, S.; Barnes, S.M. The Mindful Attention Awareness Scale: Further Examination of Dimensionality, Reliability, and Concurrent Validity. J Pers Assess. 2016, 98, 189–199. [Google Scholar] [CrossRef]
- Brown, K.W.; Ryan, R.M. The benefits of being present: mindfulness and its role in psychological well-being. J Pers Soc Psychol. 2003, 84, 822–848. [Google Scholar] [CrossRef]
- Poorebrahim A, Lin CY, Imani V, et al. Using Mindful Attention Awareness Scale on male prisoners: Confirmatory factor analysis and Rasch models. PLoS One. 2021, 16, e0254333. [Google Scholar] [CrossRef]
- Mantzios, M.; Wilson, J.C.; Giannou, K. Psychometric Properties of the Greek Versions of the Self-Compassion and Mindful Attention and Awareness Scales. Mindfulness, 2015; 6, 123–132. [Google Scholar] [CrossRef]
- Schröder H, Fitó M, Estruch R, et al. A short screener is valid for assessing Mediterranean diet adherence among older Spanish men and women. J Nutr. 2011, 141, 1140–1145. [Google Scholar] [CrossRef]
- García-Conesa MT, Philippou E, Pafilas C, et al. Exploring the Validity of the 14-Item Mediterranean Diet Adherence Screener (MEDAS): A Cross-National Study in Seven European Countries around the Mediterranean Region. Nutrients. 2020, 12, 2960. [Google Scholar] [CrossRef]
- Herdman M, Gudex C, Lloyd A, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res. 2011, 20, 1727–1736. [Google Scholar] [CrossRef]
- Yfantopoulos, J.N.; Chantzaras, A.E. Validation and comparison of the psychometric properties of the EQ-5D-3L and EQ-5D-5L instruments in Greece. Eur J Health Econ. 2017, 18, 519–531. [Google Scholar] [CrossRef]
- Wadasadawala T, Mohanty SK, Sen S, et al. Health-Related Quality of Life (HRQoL) Using EQ-5D-5L: Value Set Derived for Indian Breast Cancer Cohort. Asian Pac J Cancer Prev. 2023, 24, 1199–1207. [Google Scholar] [CrossRef]
- Feng, Y.S.; Kohlmann, T.; Janssen, M.F.; Buchholz, I. Psychometric properties of the EQ-5D-5L: a systematic review of the literature. Qual Life Res. 2021, 30, 647–673. [Google Scholar] [CrossRef]
- McClure, N.S.; Sayah, F.A.; Xie, F.; Luo, N.; Johnson, J.A. Instrument-Defined Estimates of the Minimally Important Difference for EQ-5D-5L Index Scores. Value Health. 2017, 20, 644–650. [Google Scholar] [CrossRef]
- Jones, T.L.; Baxter, M.A.; Khanduja, V. A quick guide to survey research. Ann R Coll Surg Engl. 2013, 95, 5–7. [Google Scholar] [CrossRef]
- Hodge, J.M.; Shah, R.; McCullough, M.L.; Gapstur, S.M.; Patel, A.V. Validation of self-reported height and weight in a large, nationwide cohort of U.S. adults. PLoS One. 2020, 15, e0231229. [Google Scholar] [CrossRef]
- Nuttall, F.Q. Body Mass Index: Obesity, BMI, and Health: A Critical Review. Nutr Today. 2015, 50, 117–128. [Google Scholar] [CrossRef]
- Kwak, S.K.; Kim, J.H. Statistical data preparation: management of missing values and outliers. Korean J Anesthesiol. 2017, 70, 407–411. [Google Scholar] [CrossRef] [PubMed]
- Ghasemi, A.; Zahediasl, S. Normality tests for statistical analysis: a guide for non-statisticians. Int J Endocrinol Metab. 2012, 10, 10–486. [Google Scholar] [CrossRef] [PubMed]
- Peppas S, Pansieri C, Piovani D, et al. The Brain-Gut Axis: Psychological Functioning and Inflammatory Bowel Diseases. J Clin Med. 2021, 10, 377. [Google Scholar] [CrossRef] [PubMed]
- Mitropoulou MA, Fradelos EC, Lee KY, et al. Quality of Life in Patients With Inflammatory Bowel Disease: Importance of Psychological Symptoms. Cureus. 2022, 14, e28502. [Google Scholar] [CrossRef] [PubMed]
- Greeson, J.M.; Chin, G.R. Mindfulness and physical disease: a concise review. Curr Opin Psychol. 2019, 28, 204–210. [Google Scholar] [CrossRef] [PubMed]
- Simpson R, Posa S, Langer L, et al. A systematic review and meta-analysis exploring the efficacy of mindfulness-based interventions on quality of life in people with multiple sclerosis. J Neurol. 2023, 270, 726–745. [Google Scholar] [CrossRef] [PubMed]
- Chang, Y.Y.; Wang, L.Y.; Liu, C.Y.; Chien, T.J.; Chen, I.J.; Hsu, C.H. The Effects of a Mindfulness Meditation Program on Quality of Life in Cancer Outpatients: An Exploratory Study. Integr Cancer Ther. 2018, 17, 363–370. [Google Scholar] [CrossRef]
- 39. Ventriglio A, Sancassiani F, Contu MP, et al. Mediterranean Diet and its Benefits on Health and Mental Health: A Literature Review. Clin Pract Epidemiol Ment Health. 2020; 16(Suppl-1), 156–164. [CrossRef]
- Merkes, M. Mindfulness-based stress reduction for people with chronic diseases. Aust J Prim Health. 2010, 16, 200–210. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).