Submitted:
05 February 2024
Posted:
05 February 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
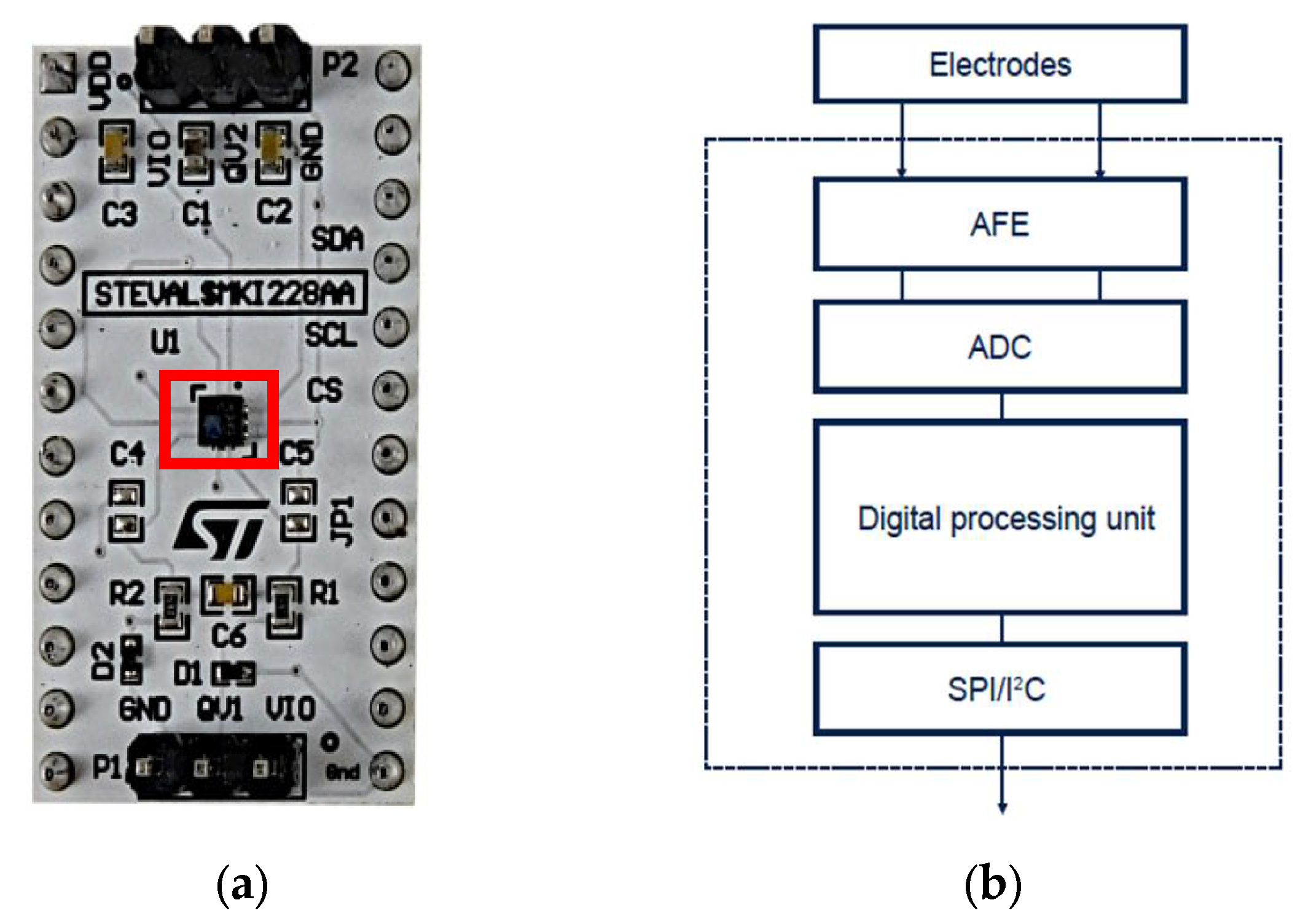
2. Materials: The QVAR Sensor
2.1. Operation Principles
- Electrodes: the electrodes are always necessary to read the signals. Usually they are made of copper, silver, tin, gold and can change in dimensions. It is important to reduce at minimum the series resistance introduced by electrodes, but the high input impedance of the QVAR helps in the choice.
- AFE: it is an Analog Front-End which realizes the conditioning and the amplification. External amplification is not always necessary.
- ADC: it is a 12-bits analogic to digital converter
- Digital Processing Unit: it is composed by Finite State Machine and Machine Learning Core.
2.2. Electrical Features
2.3. Potentiality and Limits of the QVAR Sensor
3. Methods: Biopotential Acquisition by QVAR
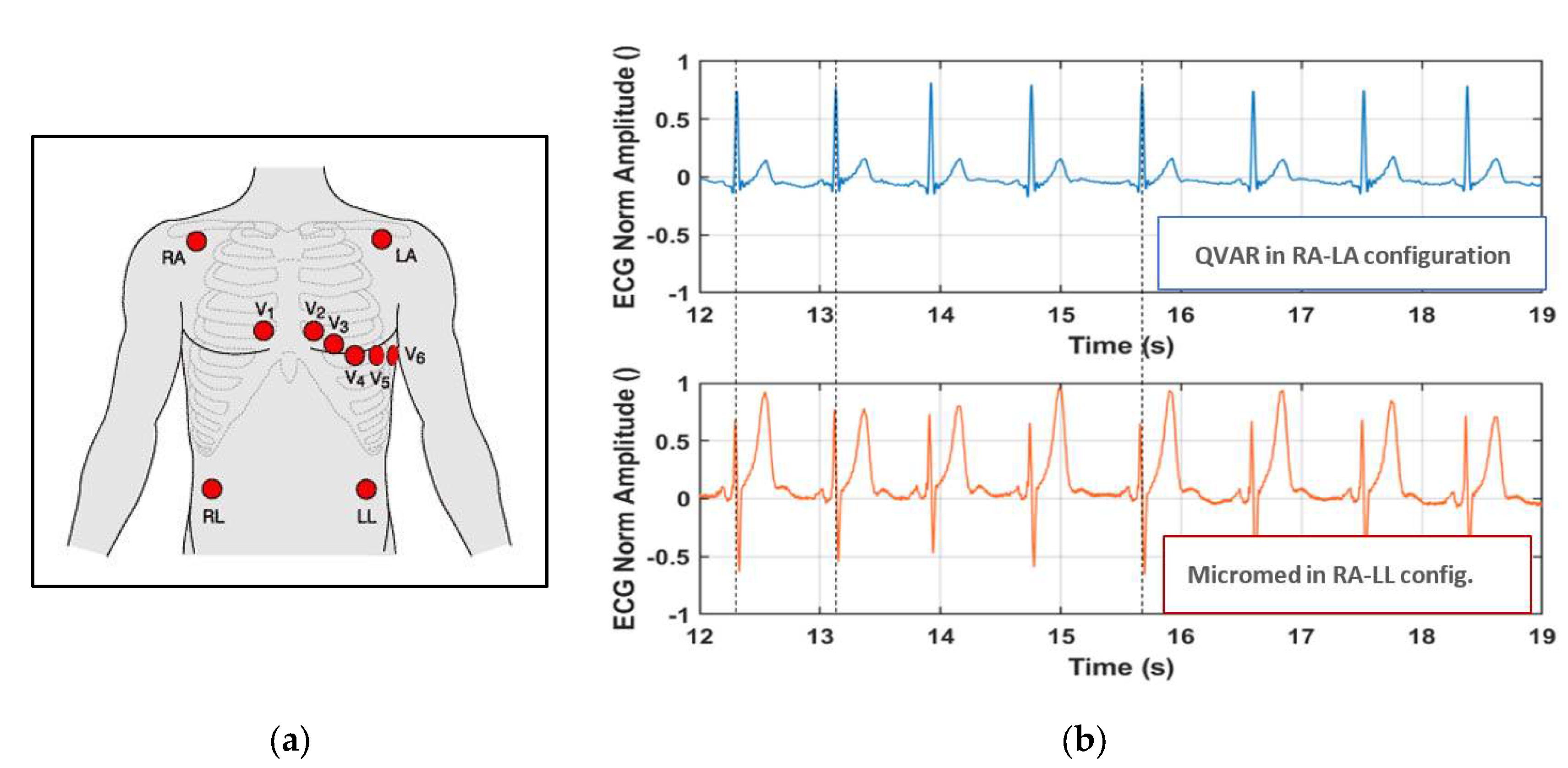
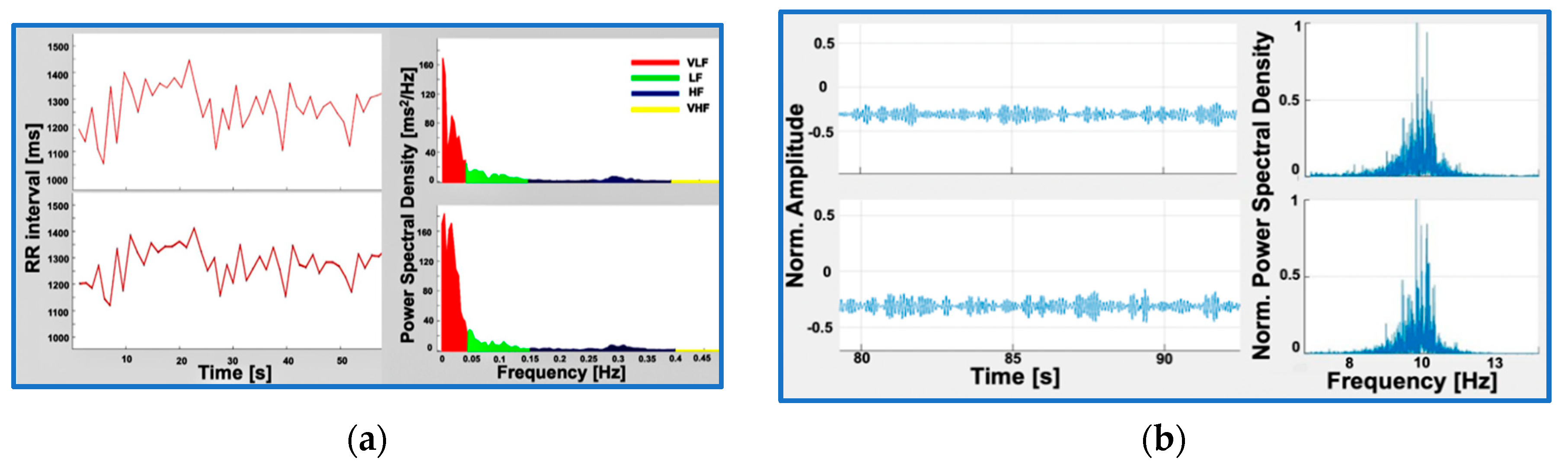
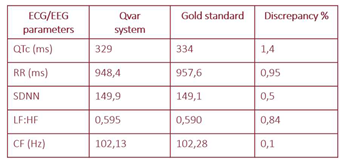
3.1. Acquisition of ECG
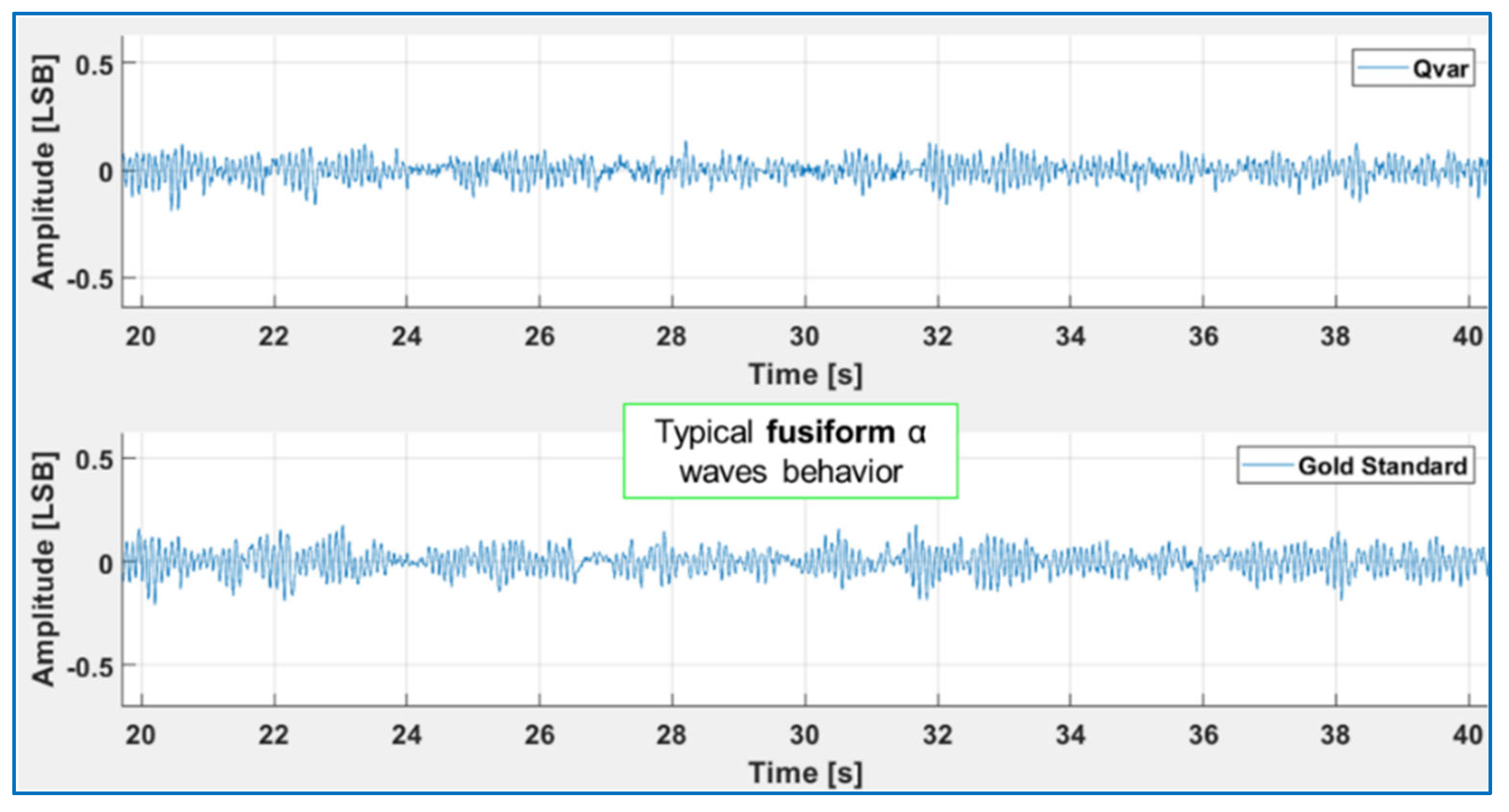
3.2. Acquisition of EEG and EOG
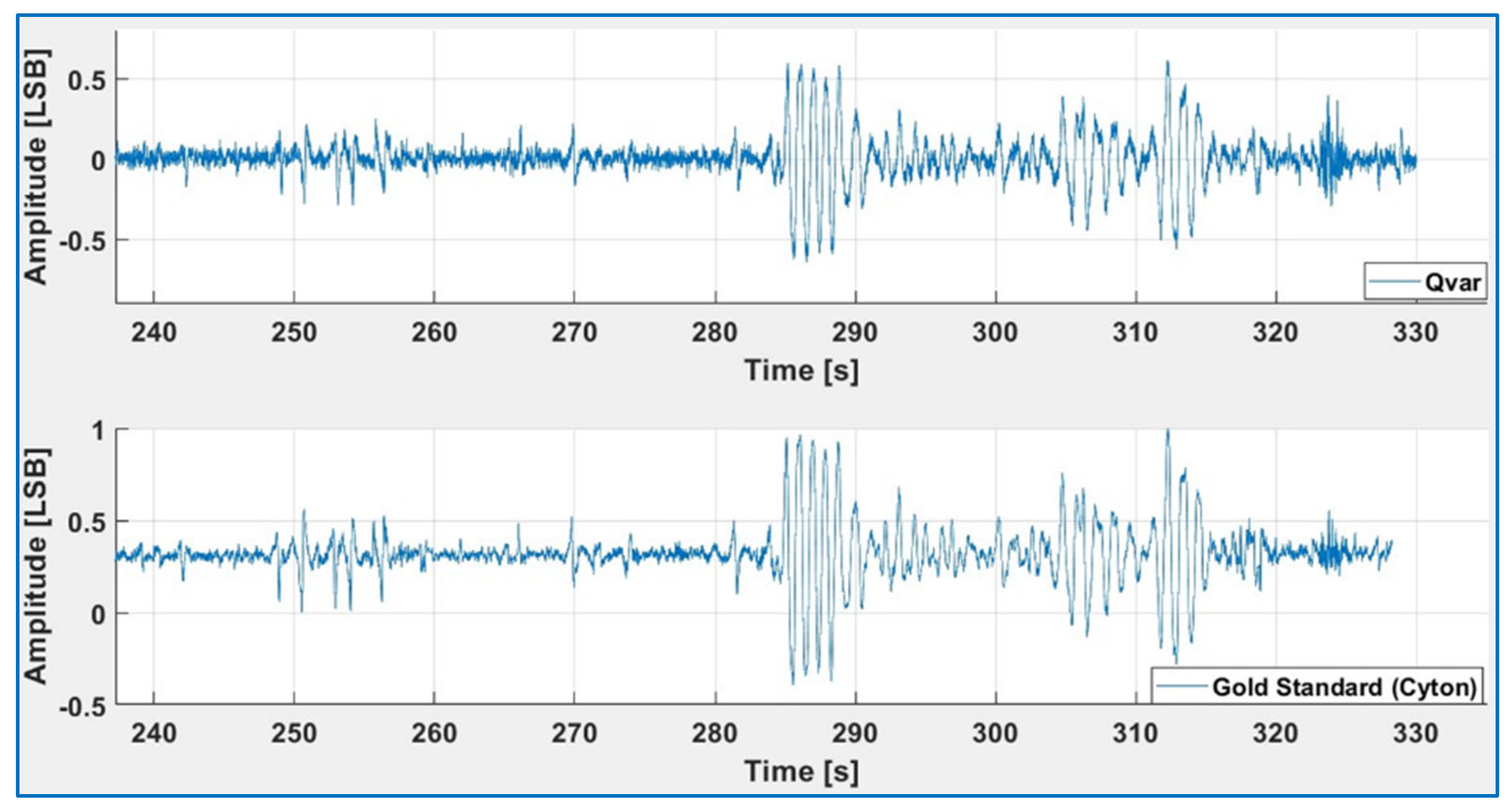
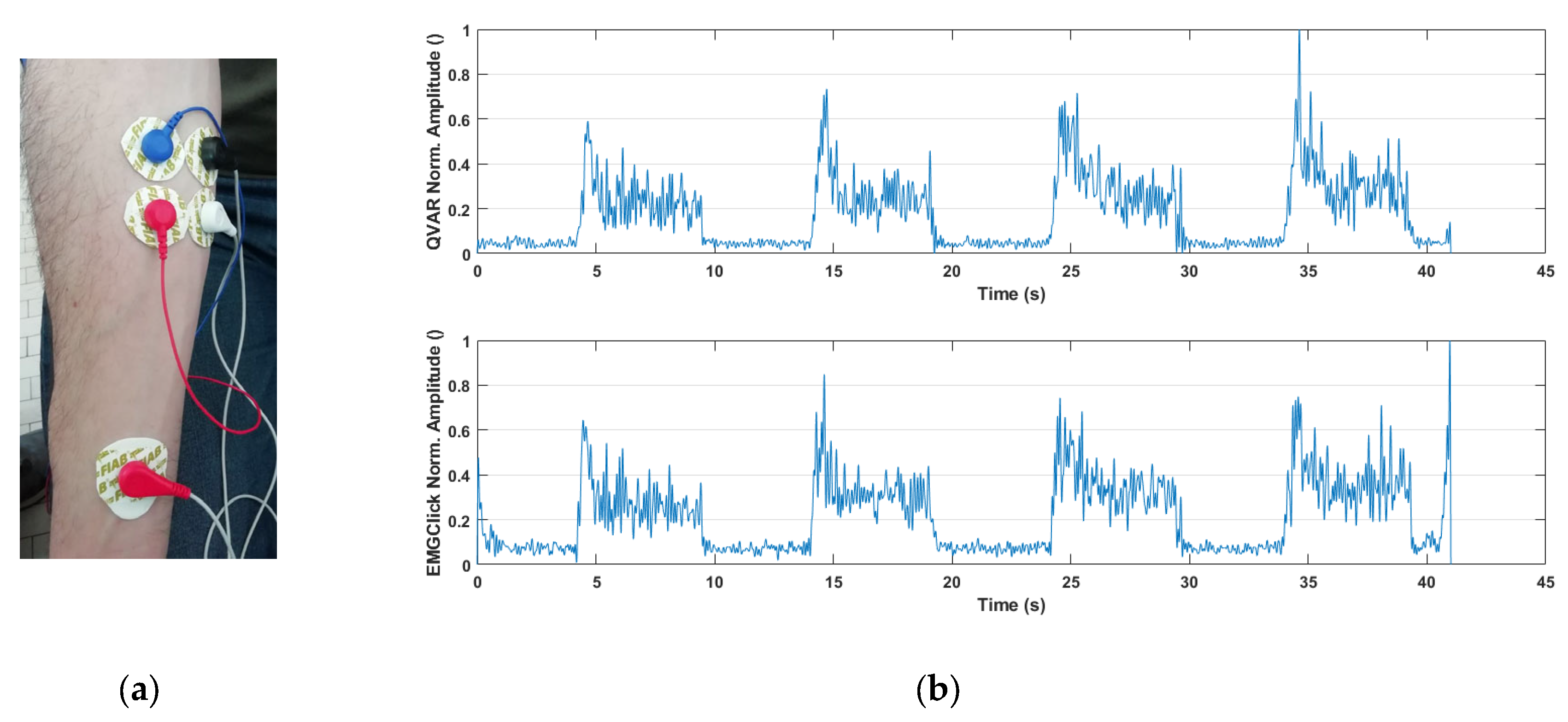
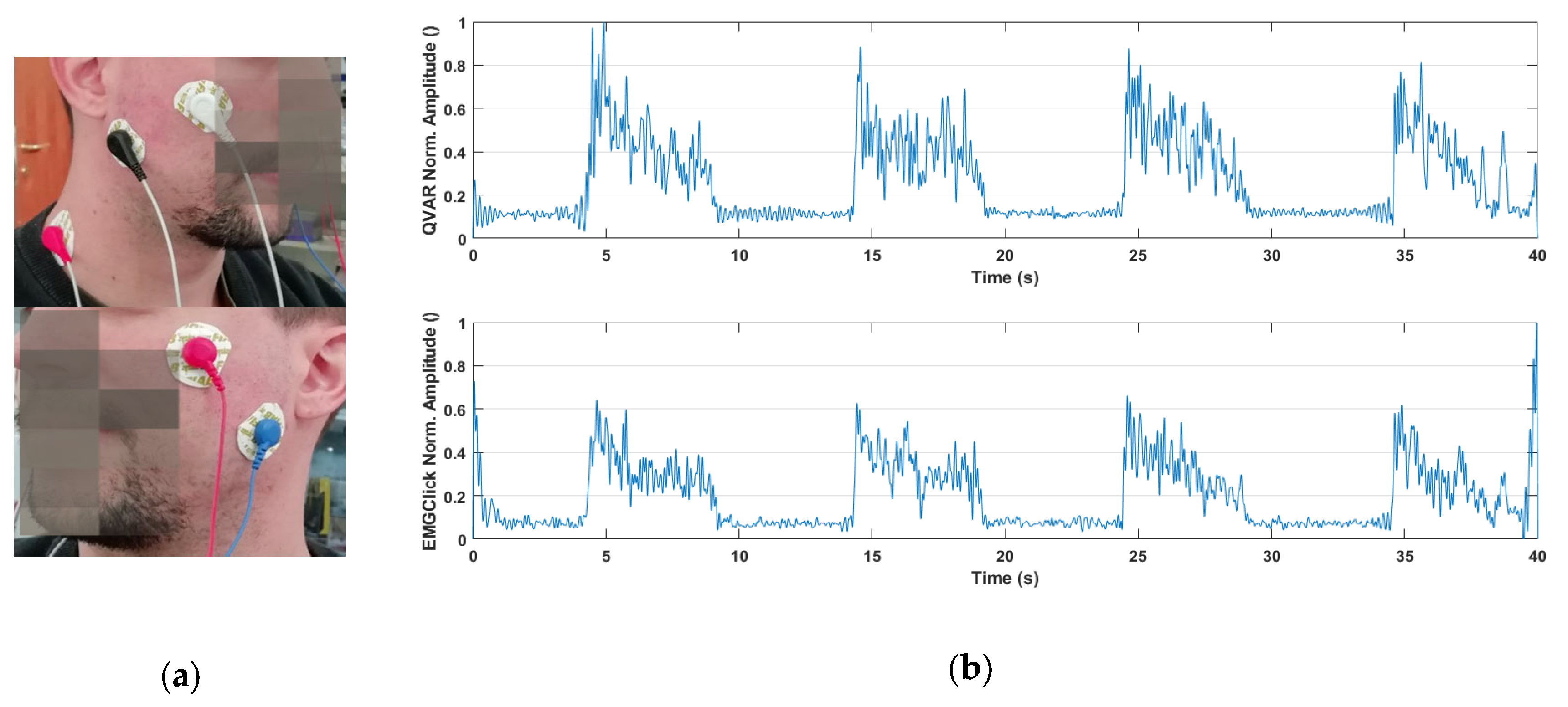
3.3. Acquisition of sEMG
4. Discussion: Two Case Studies
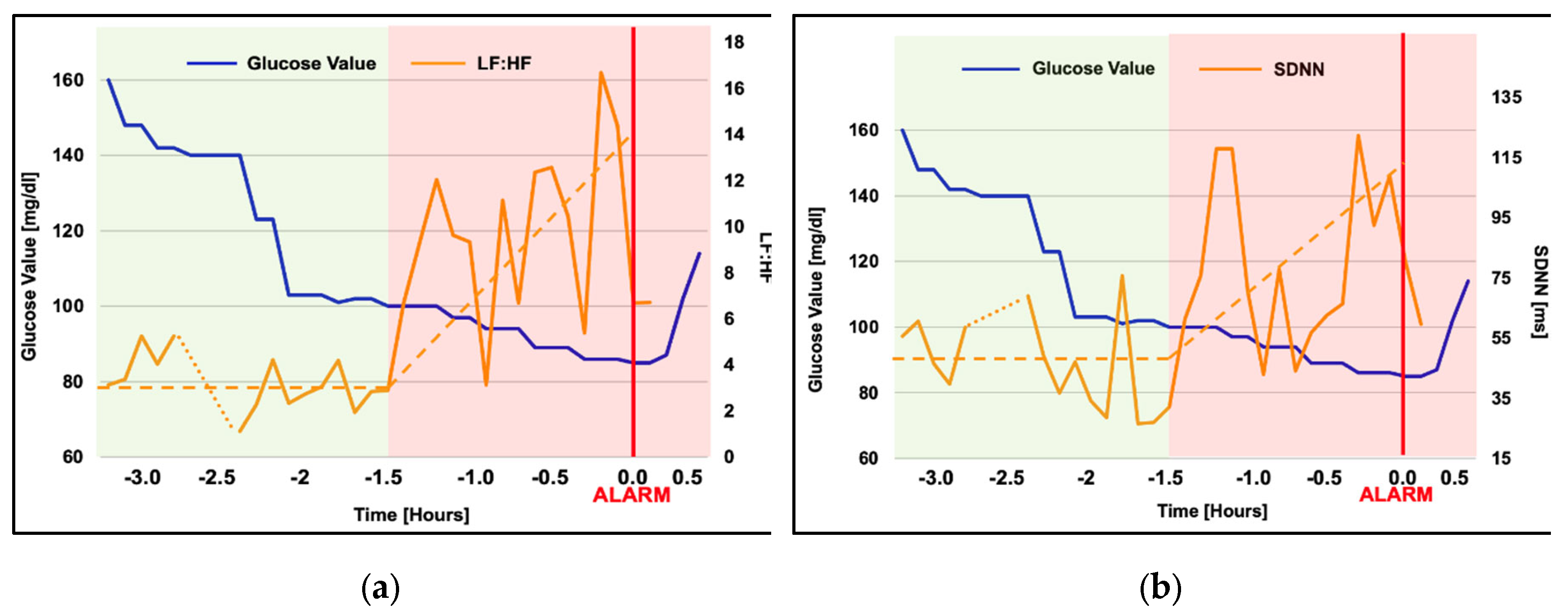
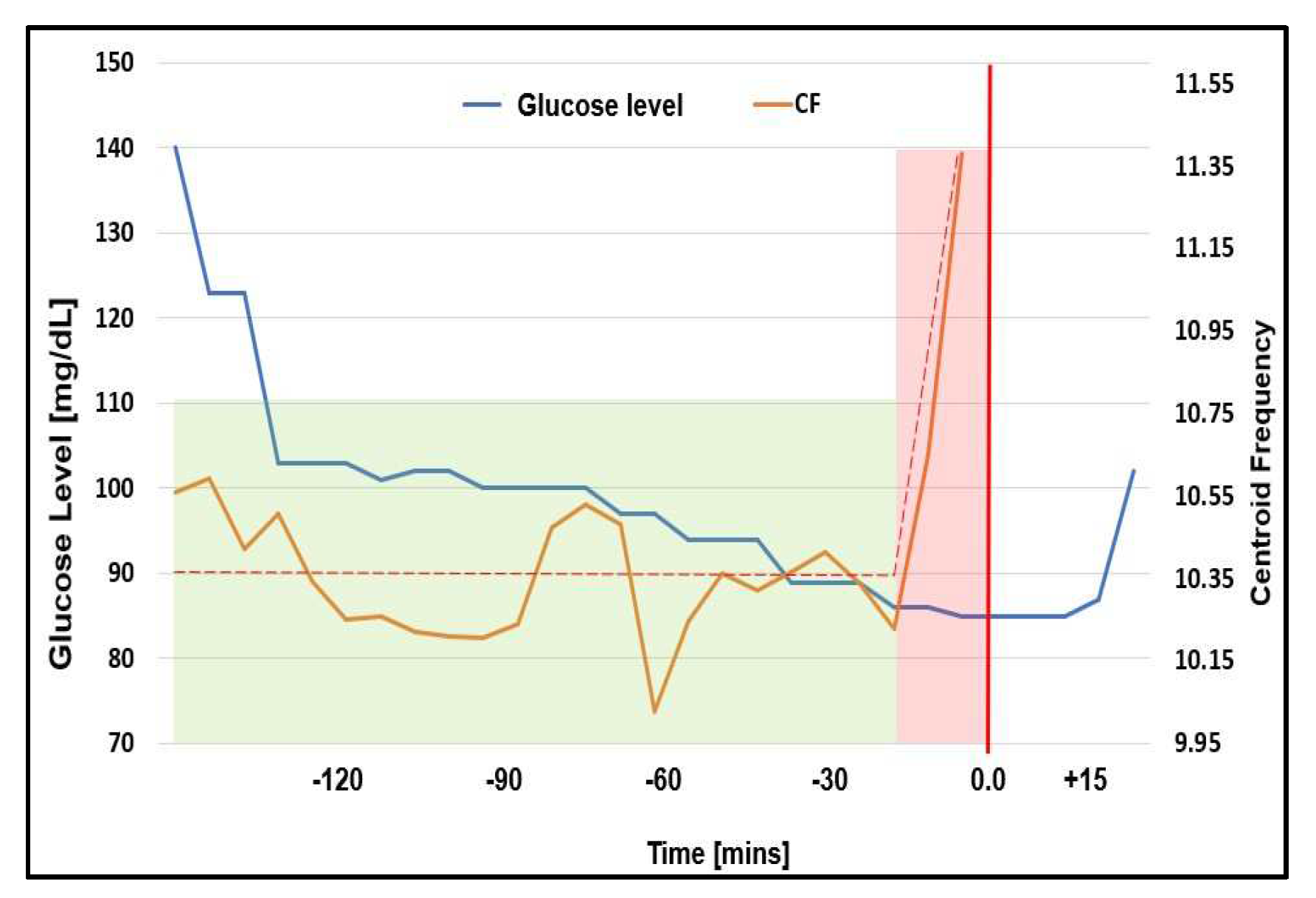
4.1. Domestic Monitoring of Vital Signs in Hypoglycemia
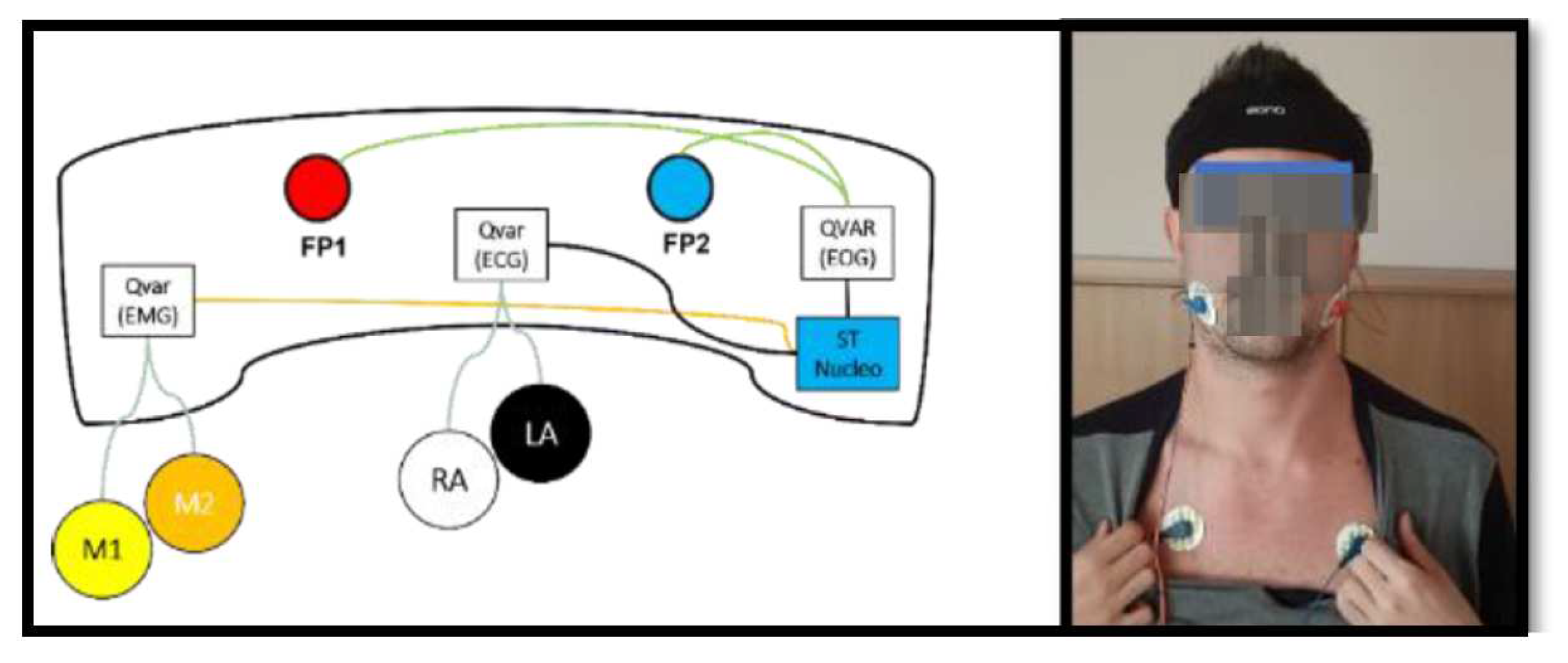
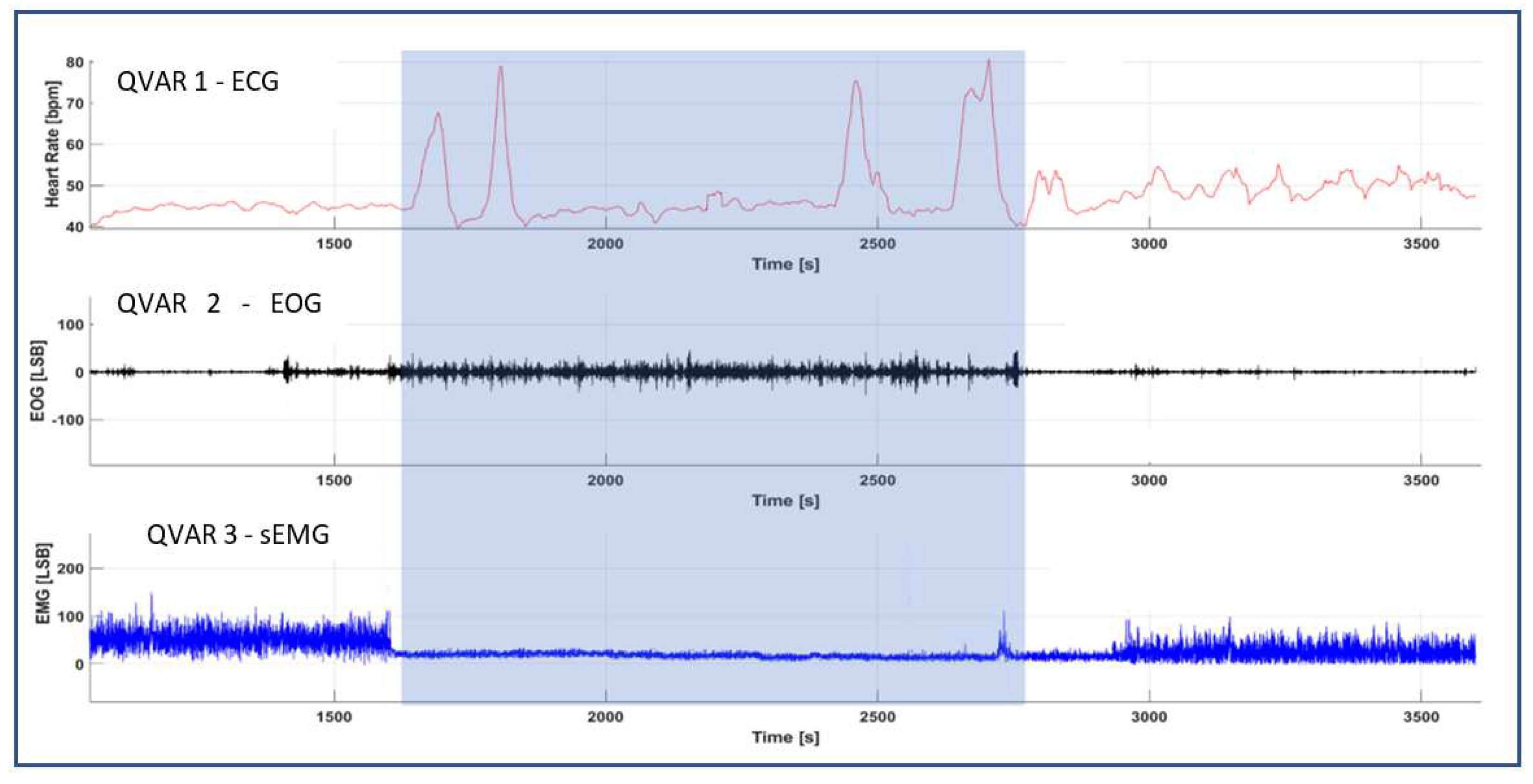
4.2. Domestic Monitoring of Non-EEG Biopotentials for REM/NREM Sleep Screening
5. Conclusions
Authors Contribution
Acknowledgments
References
- Zampogna, A.; Mileti, I.; Palermo, E.; Celletti, C.; Paoloni, M.; Manoni, A.; Mazzetta, I.; Dalla Costa, G.; Pérez-López, C.; Camerota, F.; et al. Fifteen Years of Wireless Sensors for Balance Assessment in Neurological Disorders. Sensors 2020, 20, 3247. [Google Scholar] [CrossRef] [PubMed]
- Jani, A.B.; Bagree, R.; Roy, A.K. Design of a Low-Power, Low-Cost ECG Amp; EMG Sensor for Wearable Biometric and Medical Application. In Proceedings of the 2017 IEEE SENSORS; October 2017; pp. 1–3. [Google Scholar]
- Mazzetta, I.; Zampogna, A.; Suppa, A.; Gumiero, A.; Pessione, M.; Irrera, F. Wearable Sensors System for an Improved Analysis of Freezing of Gait in Parkinson’s Disease Using Electromyography and Inertial Signals. Sensors 2019, 19, 948. [Google Scholar] [CrossRef] [PubMed]
- Mai, N.-D.; Hoang Long, N.M.; Chung, W.-Y. 1D-CNN-Based BCI System for Detecting Emotional States Using a Wireless and Wearable 8-Channel Custom-Designed EEG Headset. In Proceedings of the 2021 IEEE International Conference on Flexible and Printable Sensors and Systems (FLEPS); June 2021; pp. 1–4. [Google Scholar]
- Ogino, M.; Kanoga, S.; Muto, M.; Mitsukura, Y. Analysis of Prefrontal Single-Channel EEG Data for Portable Auditory ERP-Based Brain–Computer Interfaces. Frontiers in Human Neuroscience 2019, 13. [Google Scholar] [CrossRef] [PubMed]
- Hughes, J.R.; Zialcita, M.L. EEG in the Elderly: Seizures vs. Syncope. Clinical Electroencephalography 2000, 31, 131–137. [Google Scholar] [CrossRef] [PubMed]
- Livia Fantini, M.; Gagnon, J.-F.; Petit, D.; Rompré, S.; Décary, A.; Carrier, J.; Montplaisir, J. Slowing of Electroencephalogram in Rapid Eye Movement Sleep Behavior Disorder: Electroencephalogram in RBD. Ann Neurol. 2003, 53, 774–780. [Google Scholar] [CrossRef]
- Diadem Available online:. Available online: https://www.bitbrain.com/neurotechnology-products/dry-eeg/diadem (accessed on 13 December 2021).
- BrainBit Available online:. Available online: http://brainbit.com/ (accessed on 13 December 2021).
- Dry EEG Headsets | Products | CGX Available online:. Available online: https://www.cgxsystems.com/products (accessed on 13 December 2021).
- Li, D.; Puglia, M.P.; Lapointe, A.P.; Ip, K.I.; Zierau, M.; McKinney, A.; Vlisides, P.E. Age-Related Changes in Cortical Connectivity During Surgical Anesthesia. Frontiers in Aging Neuroscience 2020, 11, 371. [Google Scholar] [CrossRef] [PubMed]
- Miller, S.; Chelian, S.; Mcburnett, W.; Tsou, W.; Kruse, A. An Investigation of Computer-Based Brain Training on the Cognitive and EEG Performance of Employees.; 2019; Vol. 2019. 24 July.
- Kim, H.; Yoshimura, N.; Koike, Y. Classification of Movement Intention Using Independent Components of Premovement EEG. Frontiers in Human Neuroscience 2019, 13, 63. [Google Scholar] [CrossRef]
- DSI 7 Flex Available online:. Available online: https://wearablesensing.com/products/dsi-7-flex/ (accessed on 13 December 2021).
- Product Available online:. Available online: https://mentalab.com/product (accessed on 2 February 2022).
- Apicella, A.; Arpaia, P.; Mastrati, G.; Moccaldi, N. High-Wearable EEG-Based Detection of Emotional Valence for Scientific Measurement of Emotions. 2021. [Google Scholar]
- Nakamura, T.; Alqurashi, Y.D.; Morrell, M.J.; Mandic, D.P. Hearables: Automatic Overnight Sleep Monitoring With Standardized In-Ear EEG Sensor. IEEE Transactions on Biomedical Engineering 2020, 67, 203–212. [Google Scholar] [CrossRef] [PubMed]
- Hölle, D.; Meekes, J.; Bleichner, M.G. Mobile Ear-EEG to Study Auditory Attention in Everyday Life. Behav Res 2021, 53, 2025–2036. [Google Scholar] [CrossRef]
- Steinberg, C.; Bennett, M.T.; Krahn, A.D. Extended ECG Monitoring. In Cardiac Arrhythmias, Pacing and Sudden Death; Kowey, P., Piccini, J.P., Naccarelli, G., Reiffel, J.A., Eds.; Cardiovascular Medicine; Springer International Publishing: Cham, 2017; pp. 49–60. ISBN 978-3-319-58000-5. [Google Scholar]
- Bulková, V. Long-Term ECG Monitoring. Vnitr Lek 2021, 67, 16–21. [Google Scholar] [CrossRef]
- Bender, E. Prolonged Holter-ECG Monitoring Found to Improve Detection of Atrial Fibrillation After Acute Stroke. Neurology Today 2017, 17, 8. [Google Scholar] [CrossRef]
- Bayoumy, K.; Gaber, M.; Elshafeey, A.; Mhaimeed, O.; Dineen, E.H.; Marvel, F.A.; Martin, S.S.; Muse, E.D.; Turakhia, M.P.; Tarakji, K.G.; et al. Smart Wearable Devices in Cardiovascular Care: Where We Are and How to Move Forward. Nat Rev Cardiol 2021, 18, 581–599. [Google Scholar] [CrossRef] [PubMed]
- D. Brunelli, A. M. Tadesse, B. Vodermayer. Low-cost wearable multichannel surface EMG acquisition for prosthetic hand control. 6th International Workshop on Advances in Sensors and Interfaces (IWASI), Gallipoli, Italy; 2015; pp. 94–99. [Google Scholar] [CrossRef]
- F. Yinfeng, L. Honghai, L. Gongfa, Z. Xiangyang, A Multichannel Surface EMG System for Hand Motion Recognition. International Journal of Humanoid Robotics 2015, 12, 1–13. [CrossRef]
- MYO Armband: https://www.myo.
- Liu, Y.; Huang, H. Towards a high-stability EMG recognition system for prosthesis control: A one-class classification based non-target EMG pattern filtering scheme. In Proceedings of the 2009 IEEE International Conference on Systems, Man and Cybernetics, San Antonio, TX, USA, 11–14 October 2009; pp. 4752–4757. [Google Scholar]
- Huang, P.; Wang, H.; Wang, Y.; Liu, Z.; Samuel, O.W.; Yu, M.; Li, X.; Chen, S.; Li, G. Identification of Upper-Limb Movements Based on Muscle Shape Change Signals for Human-Robot Interaction. Comput. Math. Methods Med. 2020, 2020, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Su, Y.; Fisher, M.H.; Wolczowski, A.; Bell, G.D.; Burn, D.; Gao, R. Towards an EMG Controlled Prosthetic Hand Using a 3D Electromagnetic Positioning System. In Proceedings of the 2005 IEEE Instrumentationand Measurement Technology Conference Proceedings, Ottawa, ON, Canada, 16–19 May 2005; pp. 261–266. [Google Scholar]
- Trignotm Wireless Biofeedback System User’s Guide Delsys Incorporated. 2021. Available online: https://www.delsys.com/downloads/USERSGUIDE/trigno/wireless-biofeedback-system.pdf.
- Mini Wave Infinity. 2004. Available online: http://www.h-elmar-ms.pl/helmar-ms/plik/cometa-systems_wavetrack-inertial-system_nn4776.pdf.
- Ultium EMG Brochure. 2019. Available online: https://www.noraxo-n.com/noraxon-download/ultium-emg-datasheet/.
- Shimmer User Manual Revision 3p. 2017. Available online: http://www.shimmersensing.com/images/uploads/docs/Shimmer_User_Manual_rev3p.pdf.
- Yi-Da Wu, Shanq-Jang Ruan, Yu-Hao Lee B. An Ultra-Low Power Surface EMG Sensor for Wearable Biometric and Medical Applications. iosensors 2021, 11, 411. [Google Scholar] [CrossRef] [PubMed]
- Casson, A.J. Wearable EEG and Beyond. Biomed Eng Lett 2019, 9, 53–71. [Google Scholar] [CrossRef] [PubMed]
- Roy, S.K.; Shah, S.U.; Villa-Lopez, E.; Murillo, M.; Arenas, N.; Oshima, K.; Chang, R.-K.; Lauzon, M.; Guo, X.; Pillutla, P. Comparison of Electrocardiogram Quality and Clinical Interpretations Using Prepositioned ECG Electrodes and Conventional Individual Electrodes. Journal of Electrocardiology 2020, 59, 126–133. [Google Scholar] [CrossRef] [PubMed]
- Manoni, A.; Gumiero, A.; Zampogna, A.; Ciarlo, C.; Panetta, L.; Suppa, A.; Della Torre, L.; Irrera, F. ; Long-Term Polygraphic Monitoring through MEMS and Charge Transfer for Low-Power Wearable Applications. Sensors (Basel). 2022, 22, 2566. [Google Scholar] [CrossRef] [PubMed]
- Hossain, M.B.; Bashar, S.K.; Walkey, A.J.; McManus, D.D.; Chon, K.H. An Accurate QRS Complex and P Wave Detection in ECG Signals Using Complete Ensemble Empirical Mode Decomposition with Adaptive Noise Approach. IEEE Access 2019, 7, 128869–128880. [Google Scholar] [CrossRef]
- Cai, Z.; Li, J.; Zhang, X.; Shen, Q.; Murray, A.; Liu, C. How Accurate Are ECG Parameters from Wearable Single-Lead ECG System for 24-Hours Monitoring. In Proceedings of the 2019 Computing in Cardiology (CinC); September 2019; p. Page 1-Page 4. [Google Scholar]
- Witvliet, M.P.; Karregat, E.P.M.; Himmelreich, J.C.L.; de Jong, J.S.S.G.; Lucassen, W.A.M.; Harskamp, R.E. Usefulness, Pitfalls and Interpretation of Handheld Single-lead Electrocardiograms. Journal of Electrocardiology 2021, 66, 33–37. [Google Scholar] [CrossRef]
- Jurcak, V.; Tsuzuki, D.; Dan, I. 10/20, 10/10, and 10/5 Systems Revisited: Their Validity as Relative Head-Surface-Based Positioning Systems. Neuroimage 2007, 34, 1600–1611. [Google Scholar] [CrossRef] [PubMed]
- Zeng, H.; Song, A.; Yan, R.; Qin, H. EOG Artifact Correction from EEG Recording Using Stationary Subspace Analysis and Empirical Mode Decomposition. Sensors (Basel) 2013, 13, 14839–14859. [Google Scholar] [CrossRef] [PubMed]
- Belkhiria, C.; Peysakhovich, V. Electro-Encephalography and Electro-Oculography in Aeronautics: A Review Over the Last Decade (2010–2020). Frontiers in Neuroergonomics 2020, 1, 3. [Google Scholar] [CrossRef] [PubMed]
- Creel, D.J. The Electrooculogram. Handb Clin Neurol 2019, 160, 495–499. [Google Scholar] [CrossRef]
- Peever, J.; Fuller, P.M. The Biology of REM Sleep. Current Biology 2017, 27, R1237–R1248. [Google Scholar] [CrossRef]
- D. Artanto, M. P. Pramesta, Drowsiness detection system based on eye-closure using a low-cost EMG and ESP8266. 2nd International conferences on Information Technology, Information Systems and Electrical Engineering (ICITISEE), Yogyakarta, Indonesia; 2017; pp. 235–238. [Google Scholar] [CrossRef]
- S. Shin, Y. Baek, J. Lee. Korean sign language recognition using EMG and IMU sensors based on group-dependent NN models. IEEE Symposium Series on Computational Intelligence (SSCI), Honolulu, HI, USA, 2017; 1–7. [Google Scholar] [CrossRef]
- Yamaguchi, T., Mikami. Newly developed ultraminiature wearable electromyogram system useful for analyses of masseteric activity during the whole day. Journal of Prosthodontic Research; 2018; 62, pp. 110–115. [Google Scholar] [CrossRef]
- Gruebler and, K. Suzuki, Design of a Wearable Device for Reading Positive Expressions from Facial EMG Signals. in IEEE Transactions on Affective Computing 2014, 5, 227–237. [Google Scholar] [CrossRef]
- Available online: https://www.mikroe.com/emg-click.
- T., Yosef. Hypoglycemia Among Type 1 Diabetes Patients After Insulin Use in Southwest Ethiopia. Front. Endocrinol. 2021, 12, 684570. [Google Scholar] [CrossRef]
- R. J. McCrimmon and R. S., Sherwin. Hypoglycemia in Type 1 Diabetes. Diabetes 2010, 59, 2333–2339. [Google Scholar] [CrossRef]
- P. Loumpardia and M. S.B., Huda. Symptoms of Hypoglycaemia. In Blood Glucose Levels; L. Szablewski, Ed.; IntechOpen, 2020. [Google Scholar] [CrossRef]
- et al. Altered ventricular repolarization during hypoglycaemia in patients with diabetes. Diabet. Med. 1997, 14, 648–654. [Google Scholar] [CrossRef]
- E. M. Kallergis, C. A. Goudis, E. N. Simantirakis. Mechanisms, Risk Factors, and Management of Acquired Long QT Syndrome: A Comprehensive Review. The Scientific World Journal 2012, 2012, 1–8. [Google Scholar] [CrossRef]
- et al. Autonomic cardiac regulation during spontaneous nocturnal hypoglycemia in children with type 1 diabetes. Pediatric Diabetes 2021, 22, 1023–1030. [Google Scholar] [CrossRef]
- M. Mylona, S. Liatis, G. Anastasiadis. Severe iatrogenic hypoglycaemia requiring medical assistance is associated with concurrent prolongation of the QTc interval. Diabetes Research and Clinical Practice 2020, 161, 108038. [Google Scholar] [CrossRef]
- et al. Hypoglycaemia detection and prediction techniques: A systematic review on the latest developments. Diabetes Metabolism Res, 2021; 37. [Google Scholar] [CrossRef]
- Elvebakk et al.; et al. A multiparameter model for non-invasive detection of hypoglycemia. Physiol. Meas. 2019, 40, 085004. [Google Scholar] [CrossRef]
- M. Porumb, S. Stranges, A. Pescapè. Precision Medicine and Artificial Intelligence: A Pilot Study on Deep Learning for Hypoglycemic Events Detection based on ECG. Sci Rep 2020, 10, 170. [Google Scholar] [CrossRef]
- M. Olde Bekkink, M. Koeneman, B. E. de Galan. Early Detection of Hypoglycemia in Type 1 Diabetes Using Heart Rate Variability Measured by a Wearable Device. Diabetes Care 2019, 42, 689–692. [Google Scholar] [CrossRef]
- C. J. Hsu and S. T., Chen. IDF21-0409 Hypoglycemia and heart rate variability: synchronous detection by Holter and continuous glucose monitors. Diabetes Research and Clinical Practice 2022, 186, 109534. [Google Scholar] [CrossRef]
- C. Q. Ngo, R. Chai, T. V. Nguyen. «Nocturnal Hypoglycemia Detection using EEG Spectral Moments under Natural Occurrence Conditions». 2019 41st Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Berlin, Germany, lug. 2019; pp. 7177–7180. [Google Scholar] [CrossRef]
- C. Q. Ngo, R. Chai, T. V. Nguyen. «Electroencephalogram Spectral Moments for the Detection of Nocturnal Hypoglycemia». IEEE J. Biomed. Health Inform. 2020, 24, 1237–1245. [Google Scholar] [CrossRef]
- C. Q. Ngo, R. Chai, T. W. Jones. «The Effect of Hypoglycemia on Spectral Moments in EEG Epochs of Different Durations in Type 1 Diabetes Patients». IEEE J. Biomed. Health Inform. 2021, 25, 2857–2865. [Google Scholar] [CrossRef]
- Sateia, M.J. International Classification of Sleep Disorders-Third Edition. Chest 2014, 146, 1387–1394. [Google Scholar] [CrossRef]
- Gorantla, S.; Rodriguez, C.L. The Diagnostic Challenge of Dream-Enactment Behaviors. Journal of Clinical Sleep Medicine 2020, 16, 1837–1838. [Google Scholar] [CrossRef]
- 67. Masi,G; Ampriamo,G; Priano, L.; Ferraris, C. Electronics, 2023; 12, 1098. [CrossRef]
- Korotun, M.; Quintero, L.; Hahn, S.S. Rapid Eye Movement Behavior Disorder and Other Parasomnias. Clinics in Geriatric Medicine 2021, 37, 483–490. [Google Scholar] [CrossRef]
- Mieno, Y.; Hayashi, M.; Hirochi, M.; Ikeda, A.; Kako, H.; Ina, T.; Maeda, Y.; Maeda, S.; Inoue, T.; Souma, T.; et al. Availability of Home Sleep Apnea Test Equipment LS-140 on a Comparison with Polysomnography. Fujita Med J 2022, 8, 17–24. [Google Scholar] [CrossRef]
- White, C.; Hill, E.A.; Morrison, I.; Riha, R.L. Diagnostic Delay in REM Sleep Behavior Disorder (RBD). J Clin Sleep Med 2012, 8, 133–136. [Google Scholar] [CrossRef]
- Postuma, R.B.; Gagnon, J.-F.; Montplaisir, J.Y. REM Sleep Behavior Disorder: From Dreams to Neurodegeneration. Neurobiology of Disease 2012, 46, 553–558. [Google Scholar] [CrossRef]
- Manoni, A.; Loreti, F.; Radicioni, V.; Pellegrino, D.; Torre, L.D.; Gumiero, A.; Halicki, D.; Palange, P.; Irrera, F. A New Wearable System for Home Sleep Apnea Testing, Screening, and Classification. Sensors 2020, 20, 7014. [Google Scholar] [CrossRef]
- Arulvallal, S.; U., S.; T., R. Design and Development of Wearable Device for Continuous Monitoring of Sleep APNEA Disorder. In Proceedings of the 2019 International Conference on Communication and Signal Processing (ICCSP), April 2019; pp. 0050–0053. [Google Scholar]
- Sarmiento, K.F.; Folmer, R.L.; Stepnowsky, C.J.; Whooley, M.A.; Boudreau, E.A.; Kuna, S.T.; Atwood, C.W.; Smith, C.J.; Yarbrough, W.C. National Expansion of Sleep Telemedicine for Veterans: The TeleSleep Program. J Clin Sleep Med 2019, 15, 1355–1364. [Google Scholar] [CrossRef]
- Hwang, D.; Chang, J.W.; Benjafield, A.V.; Crocker, M.E.; Kelly, C.; Becker, K.A.; Kim, J.B.; Woodrum, R.R.; Liang, J.; Derose, S.F. Effect of Telemedicine Education and Telemonitoring on Continuous Positive Airway Pressure Adherence. The Tele-OSA Randomized Trial. Am J Respir Crit Care Med 2018, 197, 117–126. [Google Scholar] [CrossRef]
- Rb, B.; R., Brooks; C.E., Gamaldo; S.M., *!!! REPLACE !!!*. Harding AASM Scoring Manual Version 2.2. 2015, 7. [Google Scholar]
- Kanady, J.C.; Drummond, S.P.A.; Mednick, S.C. Actigraphic Assessment of a Polysomnographic-Recorded Nap: A Validation Study. Journal of Sleep Research 2011, 20, 214–222. [Google Scholar] [CrossRef]
- Kosmadopoulos, A.; Sargent, C.; Darwent, D.; Zhou, X.; Roach, G.D. Alternatives to Polysomnography (PSG): A Validation of Wrist Actigraphy and a Partial-PSG System. Behav Res 2014, 46, 1032–1041. [Google Scholar] [CrossRef]
- Long, X.; Fonseca, P.; Foussier, J.; Haakma, R.; Aarts, R.M. Sleep and Wake Classification With Actigraphy and Respiratory Effort Using Dynamic Warping. IEEE Journal of Biomedical and Health Informatics 2014, 18, 1272–1284. [Google Scholar] [CrossRef]
- Assessing Sleep Using Hip and Wrist Actigraphy - Slater - 2015 - Sleep and Biological Rhythms - Wiley Online Library. Available online: https://onlinelibrary.wiley.com/doi/abs/10.1111/sbr.12103 (accessed on 28 September 2022).
- Kagawa, M.; Suzumura, K.; Matsui, T. Sleep Stage Classification by Non-Contact Vital Signs Indices Using Doppler Radar Sensors. In Proceedings of the 2016 38th Annual International Conference of the IEEE Engin. in Medicine and Biology Society (EMBC); 2016; pp. 4913–16. [Google Scholar]
- Ye, Y.; Yang, K.; Jiang, J.; Ge, B. Automatic Sleep and Wake Classifier with Heart Rate and Pulse Oximetry: Derived Dynamic Time Warping Features and Logistic Model. In Proceedings of the 2016 Annual IEEE Systems Conference (SysCon); April 2016; pp. 1–6. [Google Scholar]
- Osterbauer, B.; A. Koempel, J.; L. Davidson Ward, S.; M. Fisher, L.; M. Don, D. A Comparison Study Of The Fitbit Activity Monitor And PSG For Assessing Sleep Patterns And Movement In Children. JOA 2016, 1, 24–35. [Google Scholar] [CrossRef]
- Chinoy, E.D.; Cuellar, J.A.; Jameson, J.T.; Markwald, R.R. <p>Performance of Four Commercial Wearable Sleep-Tracking Devices Tested Under Unrestricted Conditions at Home in Healthy Young Adults</P>. NSS 2022, 14, 493–516. [Google Scholar] [CrossRef]
- Stone, J.D.; Rentz, L.E.; Forsey, J.; Ramadan, J.; Markwald, R.R.; Finomore, V.S.; Galster, S.M.; Rezai, A.; Hagen, J.A. Evaluations of Commercial Sleep Technologies for Objective Monitoring During Routine Sleeping Conditions. Nat Sci Sleep 2020, 12, 821–842. [Google Scholar] [CrossRef]
- de Zambotti, M.; Cellini, N.; Goldstone, A.; Colrain, I.M.; Baker, F.C. Wearable Sleep Technology in Clinical and Research Settings. Med Sci Sports Exerc 2019, 51, 1538–1557. [Google Scholar] [CrossRef]
- Gavriloff, D.; Sheaves, B.; Juss, A.; Espie, C.A.; Miller, C.B.; Kyle, S.D. Sham Sleep Feedback Delivered via Actigraphy Biases Daytime Symptom Reports in People with Insomnia: Implications for Insomnia Disorder and Wearable Devices. J Sleep Res 2018, 27, e12726. [Google Scholar] [CrossRef]
- Imtiaz, S.A. A Systematic Review of Sensing Technologies for Wearable Sleep Staging. Sensors 2021, 21, 1562. [Google Scholar] [CrossRef]
- Wulterkens, B.M.; Fonseca, P.; Hermans, L.W.; Ross, M.; Cerny, A.; Anderer, P.; Long, X.; Dijk, J.P. van; Vandenbussche, N.; Pillen, S.; et al. It Is All in the Wrist: Wearable Sleep Staging in a Clinical Population versus Reference Polysomnography</P>. NSS 2021, 13, 885–897. [Google Scholar] [CrossRef]
- Fonseca, P.; van Gilst, M.M.; Radha, M.; Ross, M.; Moreau, A.; Cerny, A.; Anderer, P.; Long, X.; van Dijk, J.P.; Overeem, S. Automatic Sleep Staging Using Heart Rate Variability, Body Movements, and Recurrent Neural Networks in a Sleep Disordered Population. Sleep 2020, 43, zsaa048. [Google Scholar] [CrossRef]
- Korkalainen, H.; Aakko, J.; Duce, B.; Kainulainen, S.; Leino, A.; Nikkonen, S.; Afara, I.O.; Myllymaa, S.; Töyräs, J.; Leppänen, T. Deep Learning Enables Sleep Staging from Photoplethysmogram for Patients with Suspected Sleep Apnea. Sleep 2020, 43, zsaa098. [Google Scholar] [CrossRef]
- Yuda, E.; Yoshida, Y.; Sasanabe, R.; Tanaka, H.; Shiomi, T.; Hayano, J. Sleep Stage Classification by a Combination of Actigraphic and Heart Rate Signals. Journal of Low Power Electronics and Applications 2017, 7, 28. [Google Scholar] [CrossRef]
| Electrical Parameters @ VDD = 1.8 V, T = 25 °C | Typ. |
|---|---|
| Supply voltage | 1.62 V to 3.6 V |
| I/O pins supply voltage | 1.62 V to 3.6 V |
| Current consumption | 50 A |
| Current consumption in power-down | 2.1 A |
| Digital high-level input voltage | 0.7*VDDIO |
| Digital low-level input voltage | 0.3*VDDIO |
| Digital high-level output voltage | VDDIO - 0.2 V |
| Digital low-level output voltage | 0.2 V |
| Electrical Characteristics @ VDD = 1.8 V, T = 25 °C | Typ. |
|---|---|
| ODR (Configurable output data rate) | 800 to 3200 Hz |
| Input range (DC coupled) | ±25 to ±200 mV |
| Offset (Input referred) | ±1 mV |
| Noise Shorted input, gain 16, BW 20 ÷ 400 Hz, input referred |
10 uVRMS |
| ADC gain (Gain = 16, input referred) | 1311 LSB/mV |
| Channel gain (Configurable) | 2 to 16 V/V |
| Input common mode | 0.61 V |
| CMRR 50 Ω input source, sinus. input 100 mVp@50 Hz, gain 2 |
80 dB |
| Input impedance (Configurable) | 100 to 1000 MΩ |
| Bandwidth (Configurable) | 50 to 1600 Hz |
| ADC resolution | 12 bit |
 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





