1. Introduction
Acute bowel ischemia (ABI) is a life-threatening abdominal emergency, which can result in death, multiorgan failure, or severe nutritional problems [
1]. It primarily affects elderly patients, and usually develops as a consequence of chronic atherosclerotic plaques of the visceral arteries [
2]. Typically, there is a pre-existing atheroscletotic stenosis, with abdominal symptoms such as post-prandial pain, weight loss and abstaining from food. Usually, atherosclerotic plaques are found in proximal parts of the visceral arteries. Thrombosis resulting in complete closure of such an artery can be triggered by several clinical situations, comprising severe heart decompensation, surgical procedure, dehydratation or hemorrhage.
Although traditional treatment of ABI comprise emergency open surgical repair, in order to reduce periprocedural morbidity and mortality that are very high, endovascular and hybrid approaches have been suggested [
3,
8]. Indeed, data from the Swedish Vascular Registry, revealed much better results in terms of 30-day mortality in patients who underwent endovascular revascularization. Endovascular procedure as an alternative approach to the open surgical repair primarily concerns thrombotic occlusions of the superior mesenteric artery (SMA). However, in many patients there are important technical problems associated with endovascular repair in this vascular territory. Therefore, endovascular procedures should be performed only in adequately equipped hospitals (hybrid operation room, access to the specialized endovascular armamentarium, etc.) and by interventionalists with high expertise in such procedures. Inability to navigate across occluding plaques of the SMA in an antegrade direction represents one of the important technical challenges, therefore we decided to present this report, describing details of the repair of a difficult-to-recanalize SMA.
2. Detailed Case Description
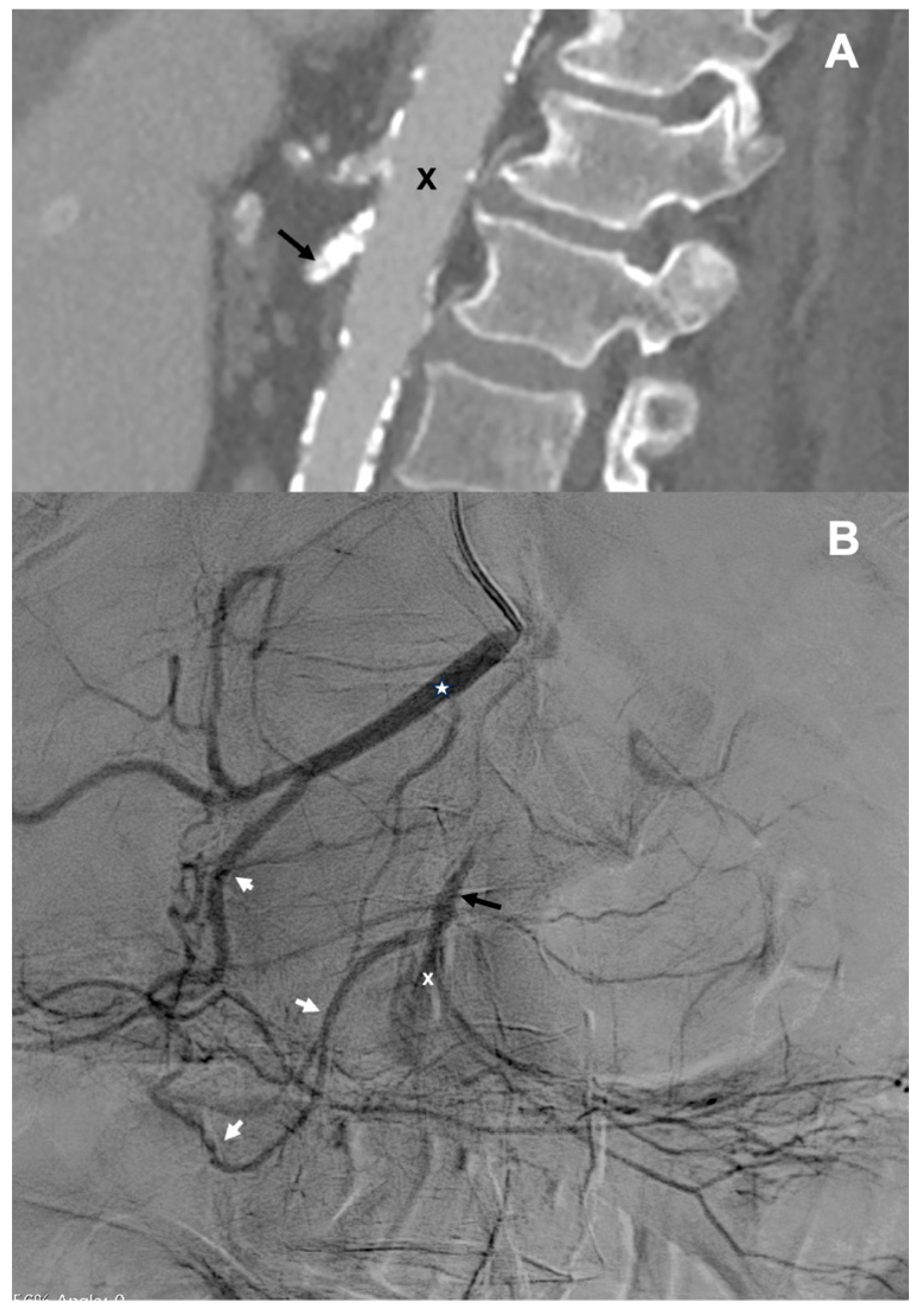
Here, we present the case of percutaneous retrograde recanalization of an occluded SMA in the patient presenting with ABI. An 82-year-old female patient developed progressing abdominal symptoms during hospital stay after thrombarterectomy of the femoral artery, which was performed for the treatment of critical lower limb ischemia. CT angiography revealed calcified plaques in the SMA, located 3 mm distally from the aorta (
Figure 1A). This lesion completely occluded proximal part the SMA. This examination also demonstrated patent celiac trunk, wide common hepatic artery (CHA), and patent, although narrow, gastroduodenal artery (GDA). Distal branches of the SMA were not visible. The overall clinical picture suggested thrombosis of the SMA resulting in bowel ischemia.
Since the patient, in addition to abdominal symptoms, presented with heart failure and was hemodynamically very unstable, surgical exploratory laparotomy was not possible. Therefore, the decision upon a life-saving endovascular intervention has been made. Catheter angiography of the abdominal visceral arteries, which was performed from the left brachial access, did not show the SMA. When the catheter was advanced to the CHA, proximal part of the SMA was revealed. This artery received inflow though the GDA. Also, several proximal jejunal branches were shown, while other branches of the SMA were not visible (
Figure 1B). Considering the fact that the origin of SMA was not visible, we decided to recanalyze this artery in a retrograde manner, via the branches of the celiac trunk.
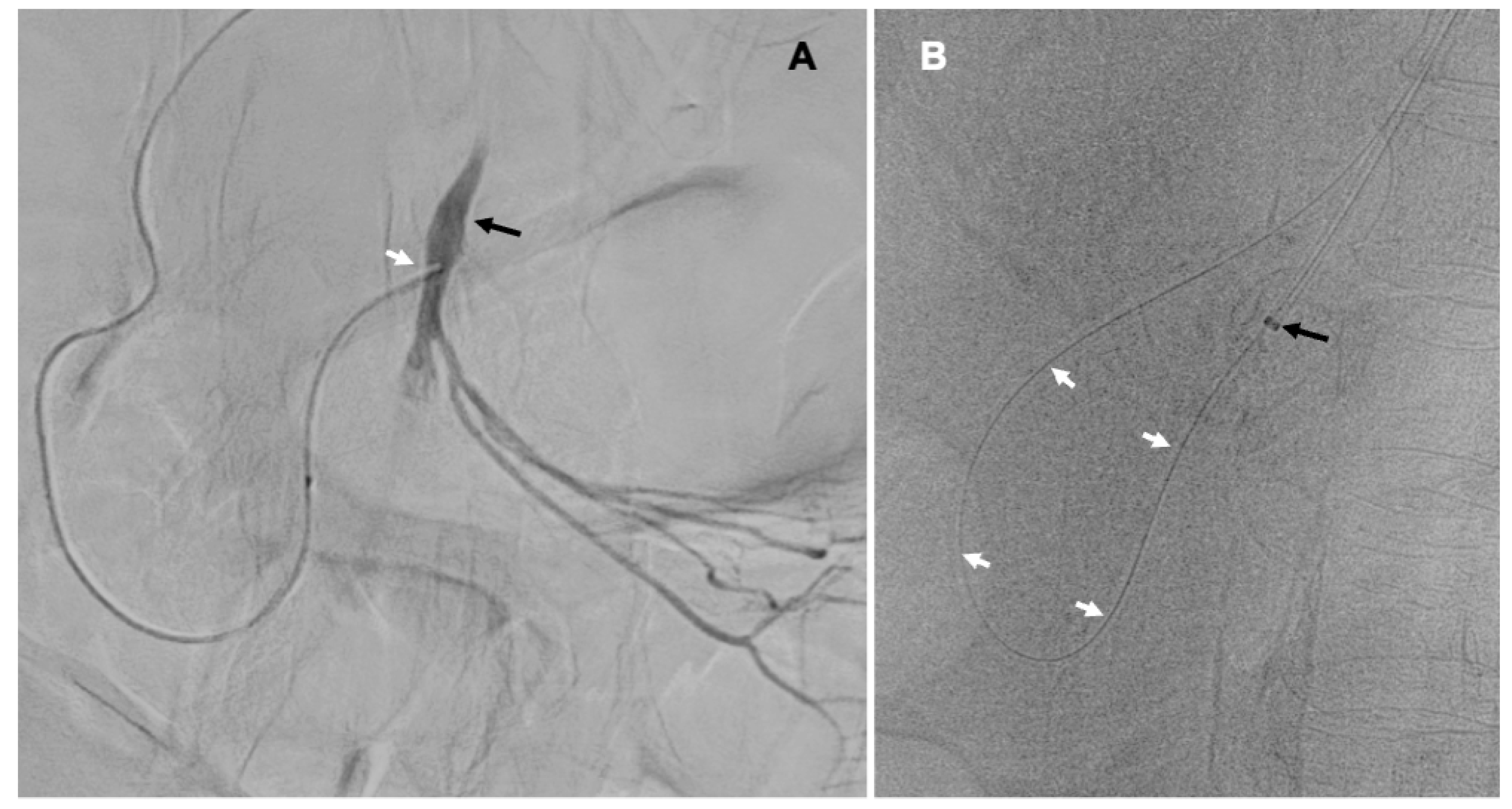
First, we introduced 5F vertebral diagnostic catheter to the distal part of the CHA, then the coaxial Progreat microcatheter (Terumo, Tokyo, Japan), which was navigated through the GDA and the pancreaticoduodenal arteries (PDA) to the SMA distally from the occluding plaque (
Figure 2A). Thereafter, the occlusion that was highly calcified, was crossed with 0.014” and then 0.018” guidewires. From the right brachial access we introduced another 6F introducer sheath, which was placed at the level of the SMA. Guidewire, which has been previously navigated to the abdominal aorta across the lesion, through the celiac trunk, the CHA, the GDA, the PDA and proximal SMA, was caught with a loop (
Figure 2B). Then, through the 6F introducer sheath, in an antegrade direction, we introduced 2.5/20 mm and 4.0/20 mm Trek coronary dilatation catheters (Abbott Vascular, Abbott Park, IL, USA) and with these balloons we predilated the plaque under the pressure of 6-18 atm.
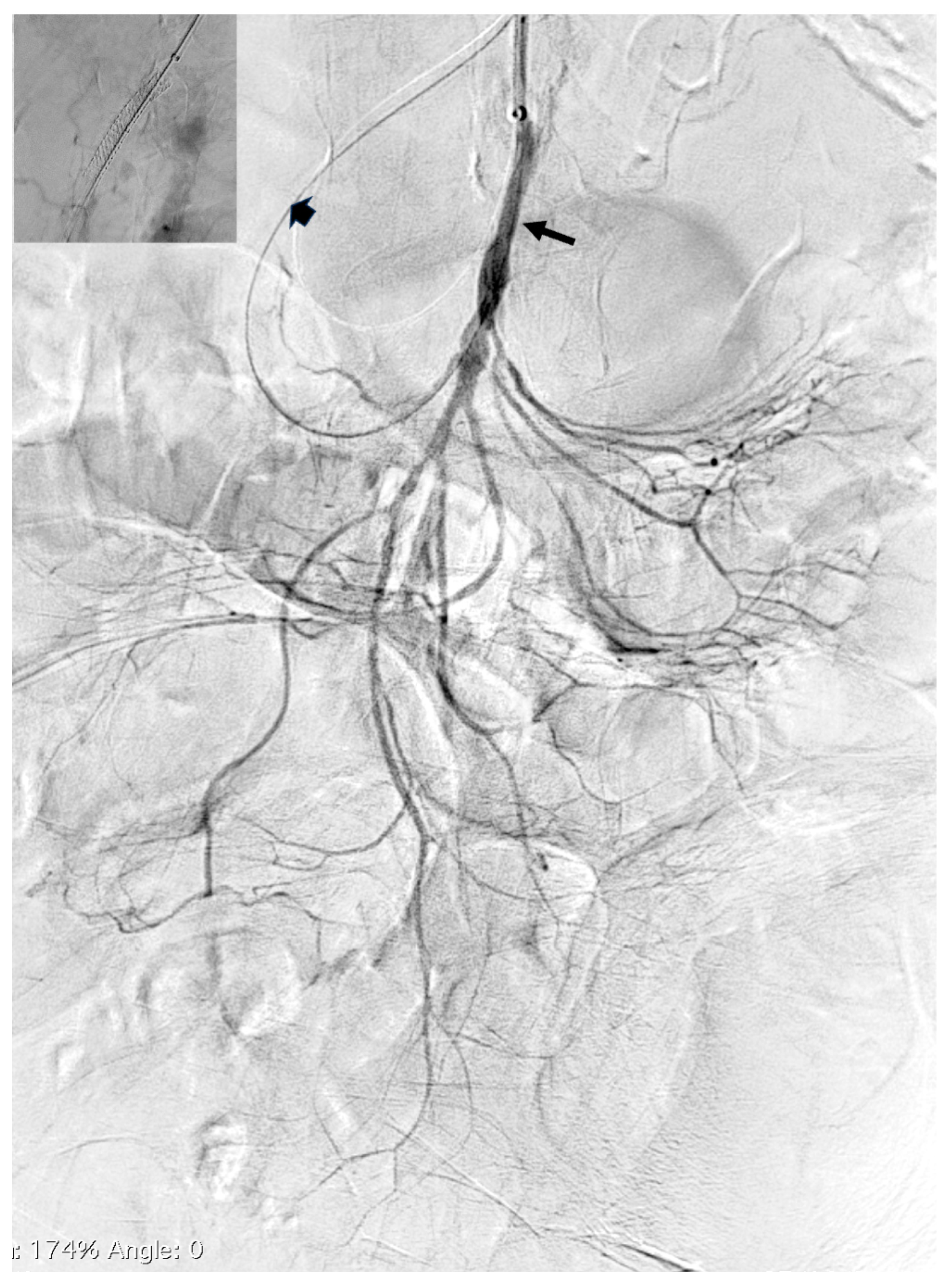
After predilation there was good inflow to the SMA and its branches (
Figure 3). Finally, the 6.0/38 mm Omnilink Elite balloon-expandable stent (Abbott Vascular, Abbott Park, IL, USA) was implanted to the proximal part of the SMA. After stent implantation there was good inflow to the target artery and its branches.
Unfortunately, although the revascularization was successful, abdominal symptoms improved and there were no longer biochemical signs of bowel ischemia, including normal values of serum lactate, patient died 2days after the procedure due to cardiogenic shock.
3. Discussion
We demonstrated that retrograde percutaneous recanalization of the occluded SMA is technically feasible, even in hemodynamically unstable patients. Currently, a recommended procedure in these patients is a hybrid one, comprising open exploratory laparotomy and retrograde endovascular recanalization of the SMA from direct puncture of this artery [
8,
9]. This is, however, not feasible in critically-ill elderly patients, in whom an endovascular repair that is performed before irreversible bowel ischemia occurs, remains the only life-saving option.
Of note, endovascular procedures are associated with fewer bowel resections and lower periprocedural mortality; on the other hand an assessment of bowel viability is easier to perform during open surgical laparotomy. Nowadays the following endovascular techniques aimed at revasculatization of occluded SMA are available:
antegrade (i.e. from the aorta) recanalization; this procedure should optimally be performed from the radial/brachial access, since in case of unfavorable aorta/SMA angle the procedure is difficult to perform, also this approach can be complicated by artery dissection,
retrograde recanalization; this type of revascularization is typically performed as a hybrid procedure during the open laparotomy, which requires general anesthesia and is associated with surgical complications; currently it is the recommended procedure for SMA revascularization,
aspiration embolectomy: this procedure is relatively easy to perform and clinical outcomes after embolectomy are usually good, still, it can be done almost exclusively for the closures of embolic etiology,
local thrombolysis of SMA; is it rarely performed for the closures of SMA, since it is associated with frequent life-threatening hemorrhagic complications.
In patients presenting with SMA occlusion, who are unsuitable for hybrid retrograde recanalization of this artery, an antegrade transcutaneous endovascular revasculatization is the preferred method. Still, the origin of the SMA should be visible on angiography. Optimally, patent proximal segment of this artery should be at least 5-10 mm long. This problem cannot be overcome using the combination of CT angiography and catheter angiography (the so-called FUSION mode). A sharp angle between the aorta and SMA is another limitation of this approach, since it is difficult to re-open stenotic plaques from the standard femoral access.
Therefore, an antegrade navigation through the proximal part of SMA is not always possible. In such a case, if open surgical exploration and retrograde recanalization during laparotomy cannot be done, the percutaneous endovascular retrograde procedure remains the only reasonable option to save patient’s life. Navigation to the patent segment of SMA can be performed either through the branches of the celiac trunk [
4,
5,
6,
7], or through the inferior mesenteric artery [
10]. Preprocedural diagnostic should reveal which of these two potential routes is better. A relatively non-tortuous option should be preferred, since a straight segment in the proximity to the target lesion facilitates retrograde navigation of the guidewire to the aorta; otherwise the SMA would be at risk of dissection and intraparietal guidewire placement. The decision upon stent or stentgraft implantation after successful revascularization should depend on hemodynamic success of the repair. In this particular patient the predilation resulted in good inflow to the SMA, therefore an uncovered stent was implanted.
Current endovascular armementatium allows for relatively easy and safe navigation through the branches of the celiac trunk, on condition that the interventionalist is experienced in the use of these tiny and flexible catheters and guidewires [
11,
12,
13,
14]. It should also be noted that the progress in endovascular techniques for revascularization of abdominbal visceral arteries particulary regards embolic occlusions. For example, mechanical thrombectomy devices, such as the Rotarex rotational athrectomy system (Becton Dickinson, Franklin Lakes, NJ, USA), allow for successful removal of embolic material [
15]. Still, mechanical thrombectomy cannot be safely used for the revascularization of distally located occlusions. Is such cases there is a considerably high risk of artery injury by the thrombectomy device. Therefore, distally located lesions should rather be recanalized in the similar manner that cerebral arteries. In our 3 patients (yet unpublished) we used for the thrombus removal from the distally located arteries, such as the ileocecal artery or ileal arteries), cerebral reperfusion catheters: the Sofia microcatheter (MicroVention, Aliso Viejo, CA, USA) and React aspiration catheter (Medtronic, Minneapolis, MN, USA). These devices can be safely navigated to the target location with the use of the Progreat microcatheter
(Terumo, Tokyo, Japan
) and a 0.014” flexifle guidewire. It should be emphasized that the aforementioned reperfusion microcatheters are very flexible, therefore can be quite easily navigated into the distally located thin arteries, including very tortuous ones. In addition, these catheters are equiped with the inner lumen, which allows for aspiration thrombectomy of the occluding material. These catheters are available in the sizes from 5F to 7F that facilitates a tailored approach to such procedures. Moreover, local catheter angiography can be performed through these devices, which allows for the detailed imaging of the target blood vessels and - if needed - for a modification of the procedure. It is also possible to deploy over these 0.014” guidewires the coronary artery-dedicated balloon angioplasty catheters or stents. Threse catheters and stents, which are typically used in the coronary arteries, can also be applied in the arteries suppluing the intestines. On the other hand, rheolytic thrombectomy devices, such as the AngioJet (Boston Scientific, Natick, MA, USA)
are less frequently used. These endovascular devices are rather dedicated to the revascularization of a secondary embolism associated with the opening of proximally located critical stenosis in the superior mesenteric artery.
It can be summarized that there are several studies demonstating better clinical outcomes after endovascular revasculatization in comparison with open surgical treatment [
16,
17,
18] and further progress should be expected in this field. Yet, the meta-analisis from 2021 did not reveal significal differences between endovascular and surgical methods in terms of early and late clinical outcomes [
19], therefore more studies in this field are needed. Still, several technical issues should be solved before these procedures become standard ones. In this paper we present how one of these challenges can be overcome.
4. Conclusions
It can be concluded that percutaneous endovascular retrograde revascularization of thrombosed SMA in the settings of bowel ischemia is technically feasible, even in critically ill and hemodynamically unstable patients.
Author Contributions
Conceptualization, Pawel Latacz and Marian Simka; methodology, Pawel Latacz and Marian Simka; formal analysis, Marian Simka; investigation, Pawel Latacz, Piotr Piekorz; writing—original draft preparation, Pawel Latacz, Piotr Piekorz; writing—review and editing, Marian Simka; visualization, Pawel Latacz, Piotr Piekorz; All authors have read and agreed to the published version of the manuscript.
Informed Consent Statement
Informed consent was obtained from the subject involved in this study.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Newton 3rd WB, Sagransky MJ, Andrews JS, et al. Outcomes of revascularized acute mesenteric ischemia in the American College of Surgeons National Surgical Quality Improvement Program database. Am Surg, 2011, 77, 832e8. [CrossRef]
- Ryer EJ, Oderich GS, Bower TC, et al. Differences in anatomy and outcomes in patients treated with open mesenteric revascularization before and after the endovascular era. J Vasc Surg 2011, 53, 1611e8. [CrossRef]
- Bjorck M, Koelemay M, Acosta S, et al. Editor’s Choice - Management of the Diseases of Mesenteric Arteries and Veins: Clinical Practice Guidelines of the European Society of Vascular Surgery (ESVS). Eur J Vasc Endovasc Surg 2017, 53, 460-e510. [CrossRef]
- Wang G, Zhou X, Shu X, et al. Transcollateral recanalization of an occluded superior mesenteric artery. Ann Vasc Surg 2021, 74, 525.e7-e12. [CrossRef]
- Kersjes, W.H., Hesse, A. Percutaneous retrograde revascularization of chronic occlusions of the superior mesenteric artery via collaterals of the celiac artery. CVIR Endovasc 2020, 143, 81. 2020; 143, 81. [CrossRef]
- Robken J, Shammas NW. Treatment of a totally occluded superior mesenteric artery facilitated by retrograde crossing via collaterals from the celiac artery. J Endovasc Ther 2007, 14, 745-747. [CrossRef]
- Milner R, Woo EY, Carpenter JP. Superior mesenteric artery angioplasty and stenting via a retrograde approach in a patient with bowel ischemia—a case report. Vasc Endovascular Surg 2004, 38, 89-91. [CrossRef]
- Rebelo A, Partsakhashvili J, John E, et al. Current concepts and evidence on open, endovascular and hybrid treatment of mesenteric ischemia: The retrograde open mesenteric stenting. Surgery in Practice and Science 5 2021, 100022. [CrossRef]
- Oderich GS, Macedo R, Stone DH, et al. Multicenter study of retrograde open mesenteric artery stenting through laparotomy for treatment of acute and chronic mesenteric ischemia. J Vasc Surg 2018, 68: 470-480.e1. [CrossRef]
- Saadi EK, Oderich G, Medronha E, et al. Endovascular recanalization of occluded superior mesenteric artery using retrograde access through the inferior mesenteric artery. J Vasc Surg Cases Innov Tech 2017, 3, 155–158. [CrossRef]
- Naazar AA, Omair A, Chu SH, et al. A shifting trend towards endovascular intervention in the treatment of acute mesenteric ischemia. Cureus 2021, 13: e18544. [CrossRef]
- Acosta-Mérida MA, Marchena-Gómez J, Saavedra-Santana P, et al. Surgical outcomes in acute mesenteric ischemia: has anything changed over the years? World J Surg 2020, 44, 100–7. [CrossRef]
- Smith SF, Gollop ND, Klimach SG, Murray PJ. Is open surgery or endovascular therapy best to treat acute mesenteric occlusive disease? Int J Surg 2013, 11, 1043–7. [CrossRef]
- Zhang Z, Wang D, Li G, et al. Endovascular treatment for acute thromboembolic occlusion of the superior mesenteric artery and the outcome comparison between endovascular and open surgical treatments: a retrospective study. Biomed Res Int 2017, 2017, 1964765. [CrossRef]
- Latacz P, Simka M, Mrowiecki T. Endovascular embolectomy of the superior mesenteric artery using the Rotarex® system for the treatment of acute mesenteric ischemia. Pol Arch Med Wewn 2016, 126, 196-7. [CrossRef]
- Arnaoutakis KD, Abularrage CJ, Efron DT, at el. Comparison of open and endovascular treatment of acute mesenteric ischemia. J Vasc Surg 2014, 59, 159–64. [CrossRef]
- El Farargy M, Abdel Hadi A, Abou Eisha M, at al. Systematic review and meta-analysis of endovascular treatment for acute mesenteric ischaemia. Vascular 2017, 25, 430–8. [CrossRef]
- Björck M, Koelemay M, Acosta S, et al. Editor’s Choice - Management of the diseases of mesenteric arteries and veins clinical practice guidelines of the European Society of Vascular Surgery (ESVS). Eur J Vasc Endovasc Surg 2017, 53, 460–510. [CrossRef]
- Hou L, Wang T, Wang J, et al. Outcomes of different acute mesenteric ischemia therapies in the last 20 years: a meta-analysis and systematic review. Vascular 2021, 21,17085381211024504. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).