Submitted:
16 January 2024
Posted:
17 January 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Results and Discussion
2.1. Selection of the candidate plants
2.2. Screening of extracts against Trypanosoma brucei rhodesiense
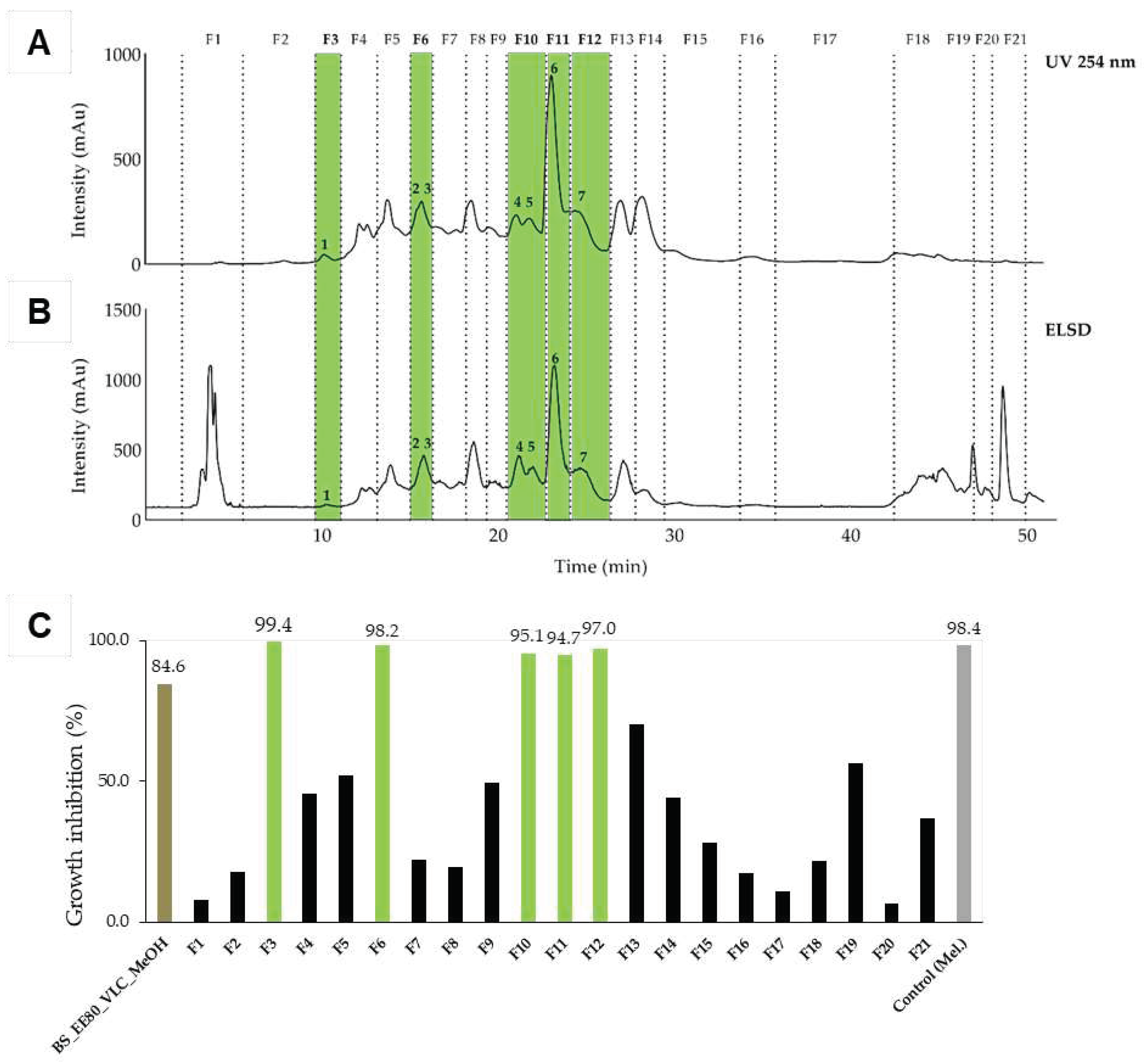
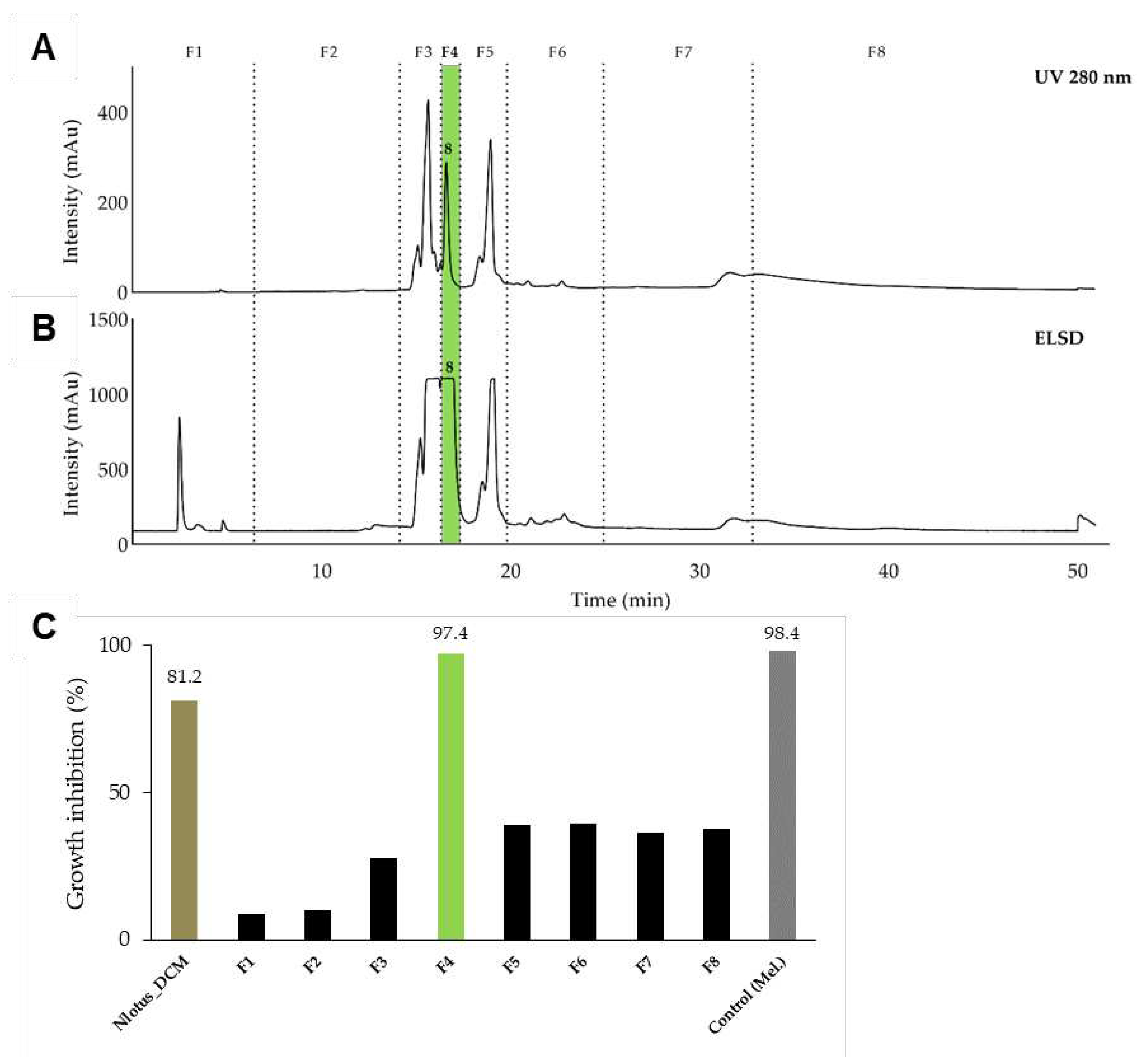
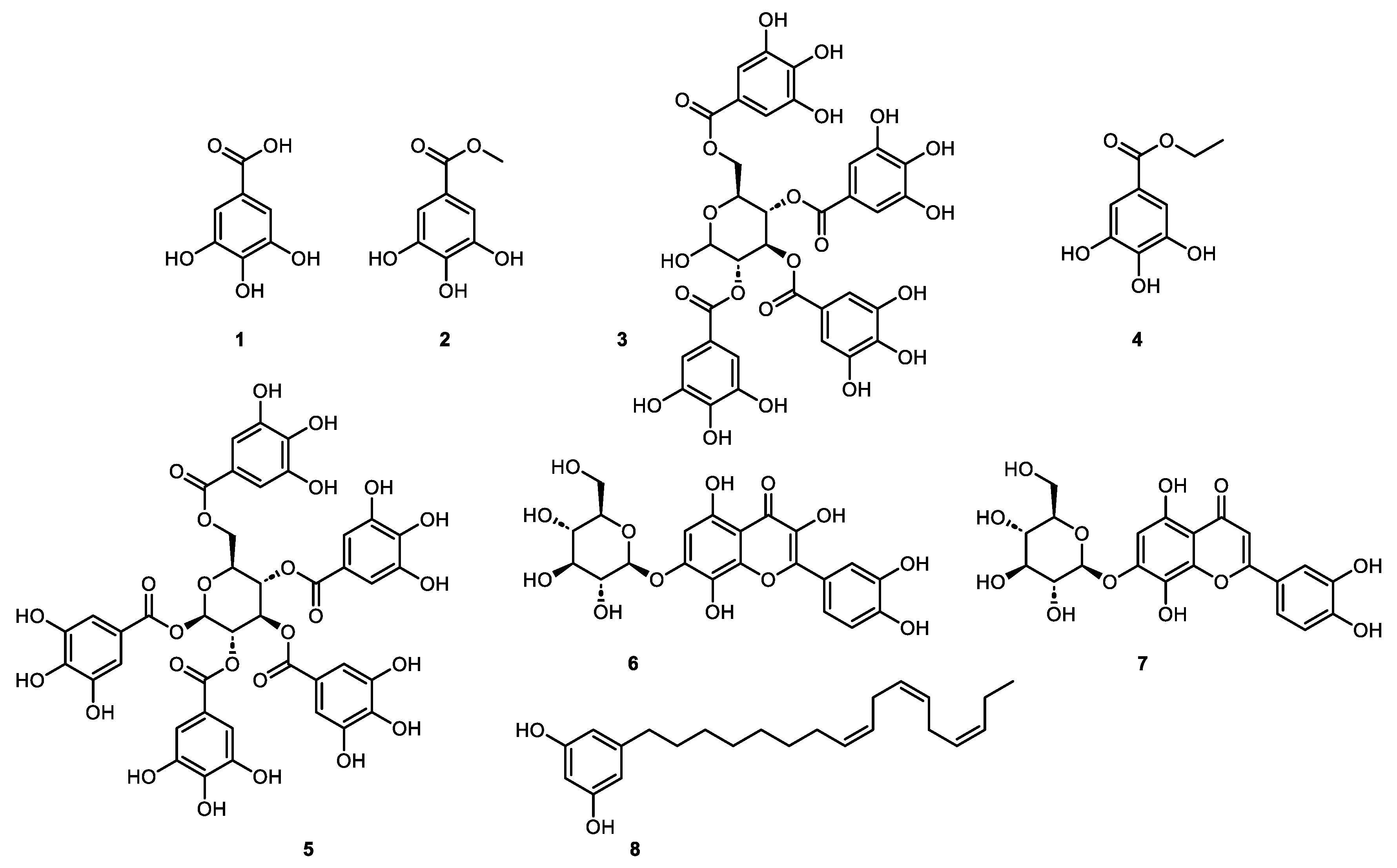
2.3. Isolation of active constituents from Brasenia schreberi and Nymphaea lotus
2.4. Antiprotozoal activity of the identified components
2.5. Active constituents in local herbal preparation
3. Materials and Methods
3.1. Chemicals
3.2. Plant collection and identification
3.3. Extract preparation
3.4. General chromatographic procedures
3.5. Fractionation and isolation of active constituents
3.6. UHPLC_HRMS / MS analysis
3.7. HPLC-DAD-ELSD analysis
3.8. NMR spectroscopic data
3.9. Quantification of active pure compounds
3.10. Antiprotozoal activity and cytotoxicity testing
4. Conclusion
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
| 1 | Percentage given by the hosting country’s speaker at the 1st National Conference of Traditional Medicine and Complementary Practices held in Luanda in August 2012. |
| 2 | It has to be clarified that in case of B. schreberi the leaves without petiole were extracted and tested, whereas for N. lotus, leaves and petiole were tested. In both cases, the plant part is referred as “leaves”. |
References
- WHO. Stratégie de l'OMS pour la médecine traditionnelle pour 2002-2005. World Health Organization.; Genève: Organisation mondiale de la Santé: 2002.
- Büscher, P.; Cecchi, G.; Jamonneau, V.; Priotto, G. Human African trypanosomiasis. The Lancet 2017, 390, 2397-2409. [CrossRef]
- Simarro, P.P.; Cecchi, G.; Franco, J.R.; Paone, M.; Diarra, A.; Ruiz-Postigo, J.A.; Fevre, E.M.; Mattioli, R.C.; Jannin, J.G. Estimating and mapping the population at risk of sleeping sickness. PLoS Negl Trop Dis 2012, 6, e1859. [CrossRef]
- Truc, P.; Grebaut, P.; Lando, A.; Makiadi Donzoau, F.; Penchenier, L.; Herder, S.; Geiger, A.; Vatunga, G.; Josenando, T. Epidemiological aspects of the transmission of the parasites causing human African trypanosomiasis in Angola. Ann Trop Med Parasitol 2011, 105, 261-265. [CrossRef]
- Kennedy, P.G. Clinical features, diagnosis, and treatment of human African trypanosomiasis (sleeping sickness). The Lancet Neurology 2013, 12, 186-194. [CrossRef]
- Valverde Mordt, O.; Tarral, A.; Strub-Wourgaft, N. Development and Introduction of Fexinidazole into the Global Human African Trypanosomiasis Program. Am J Trop Med Hyg 2022, 106, 61-66. [CrossRef]
- Bernhard, S.; Kaiser, M.; Burri, C.; Maser, P. Fexinidazole for Human African Trypanosomiasis, the Fruit of a Successful Public-Private Partnership. Diseases 2022, 10. [CrossRef]
- Vahekeni, N.; Neto, P.M.; Kayimbo, M.K.; Maser, P.; Josenando, T.; da Costa, E.; Falquet, J.; van Eeuwijk, P. Use of herbal remedies in the management of sleeping sickness in four northern provinces of Angola. J Ethnopharmacol 2020, 256, 112382. [CrossRef]
- Gurib-Fakim, A.; Mahomoodally, M. African Flora as potential sources of medicinal plants: towards the chemotherapy of major parasitic and other infectious diseases- a review. Jordan Journal of Biological Sciences 2013. [CrossRef]
- Ibrahim, M.A.; Mohammed, A.; Isah, M.B.; Aliyu, A.B. Anti-trypanosomal activity of African medicinal plants: a review update. J Ethnopharmacol 2014, 154, 26-54. [CrossRef]
- Schmidt, T.; Khalid, S.; Romanha, A.; Alves, T.; Biavatti, M.; Brun, R.; Da Costa, F.; De Castro, S.; Ferreira, V.; de Lacerda, M. The potential of secondary metabolites from plants as drugs or leads against protozoan neglected diseases-part I. Curr Med Chem 2012, 19, 2128-2175. [CrossRef]
- Ogungbe, I.; Setzer, W. The potential of secondary metabolites from plants as drugs or leads against protozoan neglected diseases—Part III: In-silico molecular docking investigations. Molecules 2016, 21, 1389. [CrossRef]
- Mahomoodally, M.F. Traditional Medicines in Africa: An Appraisal of Ten Potent African Medicinal Plants. Evidence-Based Complementary and Alternative Medicine 2013, 2013. [CrossRef] [PubMed]
- Simoben, C.V.; Ntie-Kang, F.; Akone, S.H.; Sippl, W. Compounds from African Medicinal Plants with Activities Against Selected Parasitic Diseases: Schistosomiasis, Trypanosomiasis and Leishmaniasis. Nat Prod Bioprospect 2018, 10.1007/s13659-018-0165-y. [CrossRef]
- Nwodo, N.J.; Ibezim, A.; Ntie-Kang, F.; Adikwu, M.U.; Mbah, C.J. Anti-Trypanosomal Activity of Nigerian Plants and Their Constituents. Molecules 2015, 20, 7750-7771. [CrossRef]
- Gehrig, S.; Efferth, T. Development of drug resistance in Trypanosoma brucei rhodesiense and Trypanosoma brucei gambiense. Treatment of human African trypanosomiasis with natural products (Review). International journal of molecular medicine 2008, 22, 411-419. [CrossRef]
- Mwangi, V.I.; Mumo, R.M.; Nyachieo, A.; Onkoba, N. Herbal medicine in the treatment of poverty associated parasitic diseases: A case of sub-Saharan Africa. Journal of herbal medicine 2017, 10, 1-7. [CrossRef]
- Tullius Scotti, M.; Scotti, L.; Ishiki, H.; Fávaro Ribeiro, F.; Marques Duarte da Cruz, R.; Pedrosa de Oliveira, M.; Jaime Bezerra Mendonça, F. Natural products as a source for antileishmanial and antitrypanosomal agents. Combinatorial chemistry & high throughput screening 2016, 19, 537-553. [CrossRef]
- Plaatjie, M.; Onyiche, T.; Legoabe, L.; Ramatla, T.; Nyembe, N.; Suganuma, K.; Thekisoe, O. Medicinal plants as potential therapeutic agents for trypanosomosis: a systematic review. Adv Trad Med 2022. [CrossRef]
- Yusuf, A.B.; Iliyasu, B.; Abubakar, A.; Onyekwelu, N.A.; Igweh, A.C.; Ojiegbu, F.N.; Bot, D.Y. Preliminary evaluation for anti-trypanosomal activity of aqueous stem bark extract of Crossopteryx febrifuga in Trypanosoma congolense-infected rats. Journal of Pharmacy & Bioresources 2005, 2, 111-115. [CrossRef]
- Mesia, G.K.; Tona, G.L.; Nanga, T.H.; Cimanga, R.K.; Apers, S.; Cos, P.; Maes, L.; Pieters, L.; Vlietinck, A.J. Antiprotozoal and cytotoxic screening of 45 plant extracts from Democratic Republic of Congo. J Ethnopharmacol 2008, 115, 409-415. [CrossRef]
- Freiburghaus, F.; Ogwal, E.N.; Nkunya, M.H.; Kaminsky, R.; Brun, R. In vitro antitrypanosomal activity of African plants used in traditional medicine in Uganda to treat sleeping sickness. Tropical Medicine & International Health 1996, 1, 765-771. [CrossRef]
- Freiburghaus, F.; Steck, A.; Pfander, H.; Brun, R. Bioassay-guided isolation of a diastereoisomer of kolavenol from Entada abyssinica active on Trypanosoma brucei rhodesiense. Journal of ethnopharmacology 1998, 61, 179-183. [CrossRef]
- Atindehou, K.K.; Schmid, C.; Brun, R.; Koné, M.; Traore, D. Antitrypanosomal and antiplasmodial activity of medicinal plants from Côte d’Ivoire. Journal of Ethnopharmacology 2004, 90, 221-227. [CrossRef]
- Nibret, E.; Ashour, M.L.; Rubanza, C.D.; Wink, M. Screening of some Tanzanian medicinal plants for their trypanocidal and cytotoxic activities. Phytother Res 2010, 24, 945-947. [CrossRef]
- Gupta, S.; Raychaudhuri, B.; Banerjee, S.; Das, B.; Mukhopadhaya, S.; Datta, S.C. Momordicatin purified from fruits of Momordica charantia is effective to act as a potent antileishmania agent. Parasitology international 2010, 59, 192-197. [CrossRef]
- Santos, K.K.; Matias, E.F.; Sobral-Souza, C.E.; Tintino, S.R.; Morais-Braga, M.F.; Guedes, G.M.; Santos, F.A.; Sousa, A.C.; Rolon, M.; Vega, C., et al. Trypanocide, cytotoxic, and antifungal activities of Momordica charantia. Pharm Biol 2012, 50, 162-166. [CrossRef]
- García, M.; Monzote, L.; Scull, R.; Herrera, P. Activity of Cuban plants extracts against Leishmania amazonensis. ISRN pharmacology 2012, 2012. [CrossRef]
- Phillips, E.A.; Sexton, D.W.; Steverding, D. Bitter melon extract inhibits proliferation of Trypanosoma brucei bloodstream forms in vitro. Exp Parasitol 2013, 133, 353-356. [CrossRef]
- Garba, M.H.; Kabiru, A.Y.; Yusuf, A.M.; Muhammad, A.H.; Lekene, B.J.; Kabir, M.; Joseph, A. In vivo trypanocidal activity of Nymphaea lotus Linn. methanol extract against Trypanosoma brucei brucei. Asian Pacific Journal of Tropical Disease 2015, 5, 808-812. [CrossRef]
- Camacho, M.d.R.; Phillipson, J.D.; Croft, S.L.; Solis, P.N.; Marshall, S.J.; Ghazanfar, S.A. Screening of plant extracts for antiprotozoal and cytotoxic activities. Journal of Ethnopharmacology 2003, 89, 185-191. [CrossRef]
- Bizimana, N.; Tietjen, U.; Zessin, K.H.; Diallo, D.; Djibril, C.; Melzig, M.F.; Clausen, P.H. Evaluation of medicinal plants from Mali for their in vitro and in vivo trypanocidal activity. J Ethnopharmacol 2006, 103, 350-356. [CrossRef]
- Igoli, J.O.; Gray, A.I.; Clements, C.J.; Mouad, H.A. Anti-Trypanosomal Activity and cytotoxicity of some compounds and extracts from Nigerian Medicinal Plants. In Phytochemicals-Bioactivities and impact on Health, IntechOpen: 2011.
- Longdet, I.; Achemu, H.; Okanlawon, C. Potentials of Methanolic Extract of N. Latifolia Stem Bark Against T. Congolense Infection in Experimental Rats. Journal of Agricultural Sciences and Policy Research 2014.
- Olanrewaju, C.A.; Idris, H.S.; Okwute, S.K. Investigation on the trypanocidal effects of aqueous extracts of Vernonia amygdalina and Nauclea latifolia in albino rats. Researcher 2014, 6, 61-69. [CrossRef]
- Nwodo, N.; Okoye, F.; Lai, D.; Debbab, A.; Kaiser, M.; Brun, R.; Proksch, P. Evaluation of the in vitro trypanocidal activity of methylated flavonoid constituents of Vitex simplicifolia leaves. BMC Complement Altern Med 2015, 15, 82. [CrossRef]
- Nwodo, N.; Agbo, M.; Brun, R. In vitro and in vivo Antitrypanosomal studies of the leaf extract of Vitex simplicifolia. Afr. J. Pharm. Res. Dev 2012, 4, 35-40.
- Ayawa, N.G.; Ramon-Yusuf, S.B.; Wada, Y.A.; Oniye, S.J.; Shehu, D.M. Toxicity study and anti-trypanosomal activities of aqueous and methanol whole plant extracts of Brillantaisia owariensis on Trypanosoma brucei-induced infection in BALB/c mice. Clin Phytoscience 2021, 7, 39-49. [CrossRef]
- Etim, I.S.; Ugwu, T.N.; Ukachukwu, C.O.; Aroh, K.U. Preliminary Evaluation of Anti-trypanosome Impact of Methanol, Alkaloid and Flavonoid Extracts of Sarcocephalus latifolius in T. brucei Infected Mice. Int J Biochem Res Rev 2022, 10.9734/IJBCRR/2022/v31i630332. [CrossRef]
- Sempombe, J.; Mugoyela, V.; Mihale, M.J.; Zacharia, A.; Ipagala, P.; Kilulya, K.F. Preliminary in vivo antitrypanosomal activity and cytotoxicity of Entada abyssinica, Securinega virosa and Ehretia amoena. East and Central African Journal of Pharmaceutical Sciences 2014, 17, 37-43.
- Akinjogunla, O.; Adegoke, A.; Udokang, I.; Adebayo-Tayo, B. Antimicrobial potential of Nymphaea lotus (Nymphaeaceae) against wound pathogens. Journal of medicinal plants Research 2009, 3, 138-141.
- Akinjogunla, O.; Yah, C.; Eghafona, N.; Ogbemudia, F. Antibacterial activity of leave extracts of Nymphaea lotus (Nymphaeaceae) on Methicillin resistant Staphylococcus aureus (MRSA) and Vancomycin resistant Staphylococcus aureus (VRSA) isolated from clinical samples. Ann Biol Res 2010, 1, 174-184.
- Elakovich, S.D.; Wooten, J.W. An examination of the phytotoxicity of the water shield, Brasenia schreberi. Journal of chemical ecology 1987, 13, 1935-1940. [CrossRef]
- Challal, S.; Queiroz, E.F.; Debrus, B.; Kloeti, W.; Guillarme, D.; Gupta, M.P.; Wolfender, J.-L. Rational and efficient preparative isolation of natural products by MPLC-UV-ELSD based on HPLC to MPLC gradient transfer. Planta medica 2015, 81, 1636-1643. [CrossRef]
- Kamatham, S.; Kumar, N.; Gudipalli, P. Isolation and characterization of gallic acid and methyl gallate from the seed coats of Givotia rottleriformis Griff. and their anti-proliferative effect on human epidermoid carcinoma A431 cells. Toxicology Reports 2015, 2, 520-529. [CrossRef]
- Cammann, J.; Denzel, K.; Schilling, G.; Gross, G.G. Biosynthesis of gallotannins: β-glucogallin-dependent formation of 1, 2, 3, 4, 6-pentagalloylglucose by enzymatic galloylation of 1, 2, 3, 6-tetragalloylglucose. Archives of biochemistry and biophysics 1989, 273, 58-63. [CrossRef]
- Leela, V.; Saraswathy, A. Isolation and characterization of phytoconstituents from Acacia leucophloea flowers (Roxb) wild. Int Res J Pharm 2013, 4, 107-109. [CrossRef]
- Zhao, W.-H.; Gao, C.-C.; Ma, X.-F.; Bai, X.-Y.; Zhang, Y.-X.J.J.o.C.B. The isolation of 1, 2, 3, 4, 6-penta-O-galloyl-beta-D-glucose from Acer truncatum Bunge by high-speed counter-current chromatography. 2007, 850, 523-527. [CrossRef]
- Yang, C.; Shi, J.-G.; Mo, S.-Y.; Yang, Y.-C.J.J.o.A.n.p.r. Chemical constituents of Pyrrosia petiolosa. Journal of Asian Natural Products Research 2003, 5, 143-150. [CrossRef]
- Zapesochnaya, G.; Pangarova, T. Hypolaetin 7-glucoside from Caryopteris monolica. Chemistry of Natural Compounds 1973, 9, 521-521. [CrossRef]
- Choubey, S.; Varughese, L.R.; Kumar, V.; Beniwal, V. Medicinal importance of gallic acid and its ester derivatives: a patent review. Pharmaceutical patent analyst 2015, 4, 305-315. [CrossRef]
- Daglia, M.; Di Lorenzo, A.; F Nabavi, S.; S Talas, Z.; M Nabavi, S. Polyphenols: well beyond the antioxidant capacity: gallic acid and related compounds as neuroprotective agents: you are what you eat! Current Pharmaceutical Biotechnology 2014, 15, 362-372. [CrossRef]
- Kroes, B.v.; Van den Berg, A.; Van Ufford, H.Q.; Van Dijk, H.; Labadie, R. Anti-inflammatory activity of gallic acid. Planta medica 1992, 58, 499-504. [CrossRef]
- Hu, H.; Lee, H.-J.; Jiang, C.; Zhang, J.; Wang, L.; Zhao, Y.; Xiang, Q.; Lee, E.-O.; Kim, S.-H.; Lü, J. Penta-1, 2, 3, 4, 6-O-galloyl-β-d-glucose induces p53 and inhibits STAT3 in prostate cancer cells in vitro and suppresses prostate xenograft tumor growth in vivo. Molecular cancer therapeutics 2008, 7, 2681-2691. [CrossRef]
- Kant, R.; Yen, C.-H.; Hung, J.-H.; Lu, C.-K.; Tung, C.-Y.; Chang, P.-C.; Chen, Y.-H.; Tyan, Y.-C.; Chen, Y.-M.A. Induction of GNMT by 1, 2, 3, 4, 6-penta-O-galloyl-beta-D-glucopyranoside through proteasome-independent MYC downregulation in hepatocellular carcinoma. Scientific reports 2019, 9, 1968. [CrossRef]
- Locatelli, C.; Filippin-Monteiro, F.B.; Creczynski-Pasa, T.B. Alkyl esters of gallic acid as anticancer agents: A review. European journal of medicinal chemistry 2013, 60, 233-239. [CrossRef]
- Lee, H.; Lee, H.; Kwon, Y.; Lee, J.-H.; Kim, J.; Shin, M.-K.; Kim, S.-H.; Bae, H. Methyl gallate exhibits potent antitumor activities by inhibiting tumor infiltration of CD4+ CD25+ regulatory T cells. The Journal of Immunology 2010, 185, 6698-6705. [CrossRef]
- Borges, A.; Ferreira, C.; Saavedra, M.J.; Simões, M. Antibacterial activity and mode of action of ferulic and gallic acids against pathogenic bacteria. Microbial Drug Resistance 2013, 19, 256-265. [CrossRef]
- Buzzini, P.; Arapitsas, P.; Goretti, M.; Branda, E.; Turchetti, B.; Pinelli, P.; Ieri, F.; Romani, A. Antimicrobial and antiviral activity of hydrolysable tannins. Mini reviews in medicinal chemistry 2008, 8, 1179-1187. [CrossRef]
- Choi, J.G.; Mun, S.H.; Chahar, H.S.; Bharaj, P.; Kang, O.H.; Kim, S.G.; Shin, D.W.; Kwon, D.Y. Methyl gallate from Galla rhois successfully controls clinical isolates of Salmonella infection in both in vitro and in vivo systems. PLoS One 2014, 9, e102697. [CrossRef]
- Legault, J.; Perron, T.; Mshvildadze, V.; Girard-Lalancette, K.; Perron, S.; Laprise, C.; Sirois, P.; Pichette, A. Antioxidant and anti-inflammatory activities of quercetin 7-O-β-D-glucopyranoside from the leaves of Brasenia schreberi. Journal of medicinal food 2011, 14, 1127-1134. [CrossRef]
- Shimoda, H.; Nakamura, S.; Hitoe, S.; Terazawa, S.; Tanaka, J.; Matsumoto, T.; Matsuda, H. Anti-adipogenic polyphenols of water shield suppress TNF-alpha-induced cell damage and enhance expression of HAS2 and HABP2 in adiponectin. Nat. Prod. Chem. Res 2014, 2, 146.
- Braunberger, C.; Zehl, M.; Conrad, J.; Fischer, S.; Adhami, H.-R.; Beifuss, U.; Krenn, L.J.J.o.C.B. LC–NMR, NMR, and LC–MS identification and LC–DAD quantification of flavonoids and ellagic acid derivatives in Drosera peltata. 2013, 932, 111-116. [CrossRef]
- Veit, M.; Beckert, C.; Höhne, C.; Bauer, K.; Geiger, H.J.P. Interspecific and intraspecific variation of phenolics in the genus Equisetum subgenus Equisetum. 1995, 38, 881-891. [CrossRef]
- Barrow, R.; Capon, R. Alkyl and alkenyl resorcinols from an Australian marine sponge, Haliclona Sp (Haplosclerida: Haliclonidae). Australian Journal of Chemistry 1991, 44, 1393-1405. [CrossRef]
- Kozubek, A.; Tyman, J.H. Resorcinolic lipids, the natural non-isoprenoid phenolic amphiphiles and their biological activity. Chemical reviews 1999, 99, 1-26. [CrossRef]
- Kozubek, A.; Zarnowski, R.; Stasiuk, M.; Gubernator, J. Natural amphiphilic phenols as bioactive compounds. Cellular and Molecular Biology Letters 2001, 6, 351-355.
- Oguntoye, S.O.; Bello, O.M.; Fasinu, P.S.; Khan, I.A.; Ali, Z.; Khan, S.I.; Usman, L.A. Evaluation of Selected Nigerian Medicinal Plants for in vitro Antiprotozoal Activity. The Natural Products Journal 2018, 8, 175-184. [CrossRef]
- Tasdemir, D.; Kaiser, M.; Brun, R.; Yardley, V.; Schmidt, T.J.; Tosun, F.; Rüedi, P.J.A.a.; chemotherapy. Antitrypanosomal and antileishmanial activities of flavonoids and their analogues: in vitro, in vivo, structure-activity relationship, and quantitative structure-activity relationship studies. Antimibrobial Agents and Chemotherapy 2006, 50, 1352-1364. [CrossRef]
- Koide, T.; Nose, M.; Inoue, M.; Ogihara, Y.; Yabu, Y.; Ohta, N. Trypanocidal effects of gallic acid and related compounds. Planta medica 1998, 64, 27-30. [CrossRef]
- Nose, M.; Koide, T.; Morikawa, K.; Inoue, M.; Ogihara, Y.; Yabu, Y.; Ohta, N. Formation of reactive oxygen intermediates might be involved in the trypanocidal activity of gallic acid. Biological and Pharmaceutical Bulletin 1998, 21, 583-587. [CrossRef]
- Grady, R.W.; Bienen, E.J.; Clarkson Jr, A.B.J.M.; parasitology, b. Esters of 3, 4-dihydroxybenzoic acid, highly effective inhibitors of the sn-glycerol-3-phosphate oxidase of Trypanosoma brucei brucei. Molecular and Biochemical Parasitology 1986, 21, 55-63. [CrossRef]
- Amisigo, C.M.; Antwi, C.A.; Adjimani, J.P.; Gwira, T.M.J.P.o. In vitro anti-trypanosomal effects of selected phenolic acids on Trypanosoma brucei. PLoS One 2019, 14, e0216078. [CrossRef]
- Andjelković, M.; Van Camp, J.; De Meulenaer, B.; Depaemelaere, G.; Socaciu, C.; Verloo, M.; Verhe, R.J.F.C. Iron-chelation properties of phenolic acids bearing catechol and galloyl groups. Food Chemistry 2006, 98, 23-31. [CrossRef]
- Wink, M. Medicinal plants: a source of anti-parasitic secondary metabolites. Molecules 2012, 17, 12771-12791. [CrossRef]
- Jeacock, L.; Baker, N.; Wiedemar, N.; Maser, P.; Horn, D. Aquaglyceroporin-null trypanosomes display glycerol transport defects and respiratory-inhibitor sensitivity. PLoS Pathog 2017, 13, e1006307. [CrossRef]
- Andréo, R.; Regasini, L.O.; Petrônio, M.S.; Chiari-Andréo, B.G.; Tansini, A.; Silva, D.H.S.; Cicarelli, R.M.B. Toxicity and loss of mitochondrial membrane potential induced by alkyl gallates in trypanosoma cruzi. International scholarly research notices 2015, 2015: 924670. [CrossRef]
- Calderon, A.I.; Romero, L.I.; Ortega-Barria, E.; Brun, R.; Correa A, M.D.; Gupta, M.P. Evaluation of Larvicidal and in Vitro. Antiparasitic Activities of Plants in a Biodiversity Plot in the Altos de Campana National Park, Panama. Pharmaceutical Biology 2006, 44, 487-498. [CrossRef]
- Khasanah, U.; WidyaWaruyanti, A.; Hafid, A.F.; Tanjung, M.J.P.r. Antiplasmodial activity of isolated polyphenols from Alectryon serratus leaves against 3D7 Plasmodium falciparum. Pharmacognosy Research 2017, 9, S57. [CrossRef]
- Arsianti, A.; Astuti, H.; Simadibrata, D.M.; Adyasa, Z.M.; Amartya, D.; Bahtiar, A.; Tanimoto, H.; Kakiuchi, K.J.O.J.o.C. Synthesis and in Vitro Antimalarial Activity of Alkyl Esters Gallate as a Growth Inhibitors of Plasmodium Falciparum. Oriental Journal of Chemistry 2018, 34, 655. [CrossRef]
- Torres-Leon, C.; Ventura-Sobrevilla, J.; Serna-Cock, L.; Ascacio-Valdes, J.A.; Contreras-Esquivel, J.; Aguilar, C.N. Pentagalloylglucose (PGG): a valuable phenolic compound with functional properties. Journal of functional foods 2017, 37, 176-189. [CrossRef]
- Kolodziej, H.; Kayser, O.; Kiderlen, A.; Ito, H.; Hatano, T.; Yoshida, T.; Foo, L. Antileishmanial activity of hydrolyzable tannins and their modulatory effects on nitric oxide and tumour necrosis factor-α release in macrophages in vitro. Planta medica 2001, 67, 825-832. [CrossRef]
- Jin, W.; Zjawiony, J.K.J.J.o.N.p. 5-Alkylresorcinols from Merulius i ncarnatus. Journal of Natural Products 2006, 69, 704-706. [CrossRef]
- Jiménez-Romero, C.; Torres-Mendoza, D.; González, L.D.U.; Ortega-Barría, E.; McPhail, K.L.; Gerwick, W.H.; Cubilla-Rios, L.J.J.o.n.p. Hydroxyalkenylresorcinols from Stylogyne turbacensis. Journal of Natural Products 2007, 70, 1249-1252. [CrossRef]
- Belmonte-Reche, E.; Martínez-García, M.; Peñalver, P.; Gomez-Perez, V.; Lucas, R.; Gamarro, F.; Pérez-Victoria, J.M.; Morales, J.C.J.E.j.o.m.c. Tyrosol and hydroxytyrosol derivatives as antitrypanosomal and antileishmanial agents. European Journal of Medicinal Chemistry 2016, 119, 132-140. [CrossRef]
- Matutino Bastos, T.; Mannochio Russo, H.; Silvio Moretti, N.; Schenkman, S.; Marcourt, L.; Gupta, M.P.; Wolfender, J.L.; Ferreira Queiroz, E.; Botelho Pereira Soares, M. Chemical Constituents of Anacardium occidentale as Inhibitors of Trypanosoma cruzi Sirtuins. Molecules 2019, 24. [CrossRef]
- Mahmoud, A.B.; Maser, P.; Kaiser, M.; Hamburger, M.; Khalid, S. Mining Sudanese Medicinal Plants for Antiprotozoal Agents. Front Pharmacol 2020, 11, 865. [CrossRef]
- Oyeyemi, I.T.; Akanni, O.O.; Adaramoye, O.A.; Bakare, A.A. Methanol extract of Nymphaea lotus ameliorates carbon tetrachloride-induced chronic liver injury in rats via inhibition of oxidative stress. Journal of basic and clinical physiology and pharmacology 2017, 28, 43-50. [CrossRef]
- Xiao, H.; Cai, X.; Fan, Y.; Luo, A. Antioxidant activity of water-soluble polysaccharides from Brasenia schreberi. Pharmacognosy magazine 2016, 12, 193. [CrossRef]
- Adelakun, K.M.; Mustapha, M.K.; Muazu, M.M.; Omotayo, O.L.; Olaoye, O. Phytochemical screening and antibacterial activities of crude extract of Nymphaea lotus (water lily) against fish pathogens. Journal of Biomedical Sciences 2015, 2, 38-42. [CrossRef]
- Kim, H.; Wang, Q.; Shoemaker, C.F.; Zhong, F.; Bartley, G.E.; Yokoyama, W.H. Polysaccharide gel coating of the leaves of Brasenia schreberi lowers plasma cholesterol in hamsters. Journal of traditional and complementary medicine 2015, 5, 56-61. [CrossRef]
- Hisayoshi, T.; Shinomura, M.; Konishi, A.; Tanaka, J.; Shimoda, H.; Hata, K.; Takahashi, S.; Yasukawa, K.J.J.o.B.M. Inhibition of HIV-1 reverse transcriptase activity by Brasenia schreberi (Junsai) components. Journal of Biological Macromolecules 2014, 14, 59-65. [CrossRef]
- Hisayoshi, T.; Shinomura, M.; Yokokawa, K.; Kuze, I.; Konishi, A.; Kawaji, K.; Kodama, E.N.; Hata, K.; Takahashi, S.; Nirasawa, S., et al. Inhibition of the DNA polymerase and RNase H activities of HIV-1 reverse transcriptase and HIV-1 replication by Brasenia schreberi (Junsai) and Petasites japonicus (Fuki) components. J Nat Med 2015, 69, 432-440. [CrossRef]

| Plant | Family | Collection number |
|---|---|---|
| Brillantaisia owariensis | Acanthaceae | 7925 |
| Brasenia schreberi | Cabombaceae | n.d. |
| Palisota schweinfurthii | Commelinaceae | 894 |
| Momordica charantia | Cucurbitaceae | 8591 |
| Entada abyssinica | Fabaceae | 3468 |
| Vitex madiensis | Lamiaceae | 7186 |
| Nymphaea lotus | Nymphaeaceae | 2513 |
| Crossopteryx febrifuga | Rubiaceae | 8212 |
| Sarcocephalus latifolius | Rubiaceae | 8231 |
| Extract ID | Plant name | Plant part | Solvent | GI (%) 1 |
|---|---|---|---|---|
| 46 | E. abyssinica | Ri | Aqueous | 103 |
| 47 | E. abyssinica | Ri | EtOH 80% | 101 |
| 91 | N. lotus | AeP | Hexane | 98 |
| 54 | E. abyssinica | Rb | EtOH 80% | 98 |
| 109 | B. schreberi | L | Aqueous | 99 |
| 110 | B. schreberi | L | EtOH 80% | 96 |
| 111 | B. schreberi | L | MeOH 70% | 96 |
| 92 | N. lotus | AeP | DCM | 74 |
| 115 | N. lotus | AeP | Hexane | 96 |
| 116 | N. lotus | AeP | DCM | 81 |
| 69 | V. madiensis | R | Hexane | 79 |
| 20 | C. febrifuga | L | Hexane | 85 |
| 28 | V. madiensis | L | Hexane | 96 |
| 64 | M. charantia | AeP | DCM | 72 |
| 35 | B. owariensis | L | Hexane | 96 |
| Extract ID | Plantplant part | T. brucei | T. cruzi | L. donovani | P. falciparum | L6 | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| IC50 | SI 1 | IC50 | SI | IC50 | SI | IC50 | SI | IC50 | ||
| 46 | E. abyssinicaRi | 1.8 | 4.5 | 14.0 | 0.6 | 29.9 | 0.3 | 6.5 | 1.2 | 6.3 |
| 47 | E. abyssinicaRi | 4.1 | 4.0 | 16.1 | 1.0 | 43.4 | 0.4 | 12.7 | 1.3 | 16.3 |
| 91 | N. lotusLi | 4.8 | 5.8 | 36.8 | 0.8 | 44.2 | 0.6 | 10.3 | 2.7 | 32.9 |
| 54 | E. abyssinicaRb | 5.1 | 3.6 | 26.4 | 0.7 | 45.8 | 0.4 | 10.4 | 1.8 | 16.0 |
| 109 | B. schreberiL | 5.9 | 2.9 | 26.7 | 0.6 | 53.0 | 0.3 | 3.5 | 4.9 | 33.8 |
| 110 | B. schreberiL | 7.1 | 4.3 | 61.5 | 0.5 | 48.1 | 0.6 | 8.1 | 3.8 | 33.8 |
| 111 | B. schreberiL | 7.9 | 4.0 | 65.9 | 0.5 | 42.4 | 0.7 | 7.5 | 4.2 | 36.0 |
| 92 | N. lotusL | 9.8 | 3.8 | 56.7 | 0.7 | 14.5 | 2.5 | 6.3 | 5.9 | 42.4 |
| 115 | N. lotusL | 11.9 | 2.5 | 45.5 | 0.6 | 20.1 | 1.5 | 14.7 | 2.0 | 34.5 |
| 116 | N. lotusL | 12.2 | 3.6 | 56.3 | 0.8 | 17.7 | 2.5 | 7.9 | 5.5 | 49.7 |
| 69 | V. madiensisR | 12.8 | 2.2 | 53.0 | 0.5 | 11.7 | 2.4 | 20.7 | 1.4 | 41.9 |
| 20 | C. febrifugaL | 13.1 | 3.5 | 64.1 | 0.7 | 46.9 | 1.0 | 21.2 | 2.2 | 47.0 |
| 28 | V. madiensisL | 13.6 | 1.7 | 42.2 | 0.6 | 23.2 | 1.0 | 23.9 | 1.0 | 22.8 |
| 64 | M. charantiaWp | 30.5 | 1.1 | 48.1 | 0.7 | 25.5 | 1.3 | 8.7 | 3.9 | 26.0 |
| 35 | B. owariensisL | 40.2 | 1.2 | 55.9 | 0.9 | 62.1 | 0.8 | >50 | n.d | 48.2 |
| T. brucei | T. cruzi | L. donovani | P. falciparum | L6 | |||||
|---|---|---|---|---|---|---|---|---|---|
| IC50 | SI | IC50 | SI | IC50 | SI | IC50 | SI | IC50 | |
| Gallic acid (1) | 0.5 | 34 | 66 | 0.2 | 56 | 0.3 | >10 | n.d. | 16 |
| Methyl gallate (2) | 1.1 | 15 | 16 | 1.0 | 8.5 | 1.9 | 2.1 | 7.8 | 16 |
| Ethyl gallate (4) | 0.6 | 25 | 16 | 0.9 | 6.8 | 2.2 | 3.0 | 4.9 | 15 |
| Pentagalloyl-β-glucopyranoside (5) | 20.0 | 1.0 | 44 | 0.5 | 15 | 1.4 | 6.7 | 3.1 | 21 |
| Gossypetin-7-O-β-glucopyranoside (6) | 5.5 | 1.6 | 12 | 0.8 | 53 | 0.2 | n.d. | n.d. | 8.9 |
| Hypolaetin-7-O-glucoside (7) | 5.7 | 3.2 | 49 | 0.4 | 52 | 0.4 | n.d. | n.d. | 19 |
| Resorcinol-alkyl (8) | 5.3 | 2.5 | 9.1 | 1.4 | 2.5 | 5.2 | n.d. | n.d. | 13 |
| Active component | B. schreberi decoction | N. lotus decoction | ||
|---|---|---|---|---|
| Raw material | Extract | Raw material | Extract | |
| Gallic acid (1) | 8.8 | 50 | 5.6 | 22 |
| Methyl gallate (2) | 0.007 | 0.04 | 0.005 | 0.022 |
| Ethyl gallate (4) | n.d. | <19 ppm | n.d. | <19 ppm |
| Pentagalloyl-β-glucopyranoside (5) | 0.39 | 2.3 | 0.09 | 0.36 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





