1. Introduction
Today, especially tooth-colored dental restorations are predominantly bonded to tooth hard tissues
1. Successful enamel bonding guarantees for overall retention, and dentin adhesion stabilizes the remaining tooth and mainly helps to effectively seal the pulpo-dentin complex in order to avoid postoperative hypersensitivities [
1,
2,
3,
4]. In this course, conventional cement liners such as phosphate or glass ionomer cements are normally not applied, because they significantly reduce the dentin bonding area [
1,
2,
5]. Furthermore, non-adhesive cements are time-consuming without additional value for pulp vitality [
1,
5,
6]. In contrast, decades ago conventional liners played a greater role i.e. they were routinely applied beneath every cast gold or amalgam restoration[
7]. Moreover, in cavities having been estimated to be very deep, special measures have been taken to preserve tooth vitality [
8,
9,
10].
Today, IPC has been largely sidelined due to a fundamentally different understanding of caries excavation [
11,
12,
13]. It has been scientifically proven that selective excavation is preferable to the old-fashioned, “complete” and usually aggressive excavation method used in caries excavation [
11,
14]. As with most paradigm shifts, the introduction of this approach to caries excavation into dental practice is usually a slow and gradual process which takes at least one generation of dentists to implement [
13]. In the specific case of the excavation strategy, this is probably also due to the fact that many colleagues are afraid of being discredited as not working cleanly in the event of a dentist change. Therefore, seemingly complete excavation is still widespread, especially among older colleagues. And the more aggressively you excavate, the more often you are confronted with situations that are classified as “caries profunda”, i.e. measures should then be taken to maintain pulp vitality in view of the thin residual dentin layer [
8,
15,
16]. And this still happens millions of times a day in dental practices.
The next mystery is the theory behind IPC. It is assumed that at residual dentin thicknesses of <300 microns, the barrier function of the dentin is reduced and it is advisable to apply agents that provoke dentin formation[
14,
17,
18]. For decades, this was calcium hydroxide, which was said to stimulate new dentin formation due to its high pH[
8]. But does it really work? In this context, it is interesting that glass ionomer cement is also mentioned in the current ESE guideline on the topic of IPC[
8]. However, glass ionomer cement and calcium hydroxide have nothing in common[
8,
19]. Is it ultimately just a matter of covering deeper areas to prevent the penetration of resin tags when dentin is bonded?
The purpose of this retrospective study was to evaluate the effect of IPC on the long-term clinical performance of restorations for 40 years, where the capping material was zinc oxide-eugenol and the restorative material was amalgam in posterior teeth and resin composite in anterior teeth.
2. Materials and Methods
The study group was selected retrospectively from dental records of patients who underwent vital pulp therapy in a private dental practice and the research goes back as far as to the year 1969. The investigation of 1412 dental records yielded 159 patients and 366 treated teeth. The 159 patients comprised 366 cases between 1969 and 1980. This means that an average of 2.3 (± 1.58) teeth were treated per patient. The average year of birth was 1941. The average patient age at the beginning of the observation period was 26.5 (± 9.24) years. A total of 159 people were examined in the study. Of these, 82 were female (51.57%) and 77 were male (48.43%). The most frequently treated tooth in both the lower jaw (n=61) and the upper jaw (n=46) was the second permanent molar. Overall, the most frequently treated teeth were the first and second molars of the 4th quadrant with a frequency of 34 (9.29%) each.
Selected patients were treated by one experienced practitioner in the years between 1969 and 1980 and received indirect pulp capping. Inclusion criteria were vital permanent teeth with deep caries within the inner third of dentin, non-existent clinical signs of irreversible pulpitis and no pulp exposure. Subsequent to standardized ice-cold pulp-test teeth were anaesthetized if required and cavities were prepared using a sterile high-speed bur with water coolant. Caries was excavated thoroughly with a round bur until the dentin showed increased resistance when streaking by a testing probe. Teeth with accidental exposed pulp tissue were excluded. The remaining dentin layer was capped with zinc-oxide-eugenol cement according to manufacturer’s instructions. Posterior teeth were restored with amalgam fillings, anterior teeth received resin composite fillings after covering the zinc oxide eugenol capping with Harvard zinc phosphate cement.
Gathered parameters with possible influences on survival rates consist of age, gender, tooth location/position, date of vital therapy, numbers of filled surfaces, type of primary restoration material, successional treatments on each tooth and the last date of surveillance. Data collection and statistical analysis was performed by using excel sheets (Microsoft Excel, Microsoft corporation, USA) and DataTab (DataTab, Seiersberg, Austria). Significant differences among groups were checked by cox regression analysis and significance level was set at p=0.05. Kaplan Meier curves were utilised to illustrate survival rates. Treatment success was reached by keeping vitality beyond 365 days. Loss of vitality within 365 days was determined as treatment failure. Treatment outcome was assessed after different time periods (1 and 6 months; 1, 2, 5, 10, 20 and 40 years).
3. Results
3.1. Clinical Outcome Within the First Year
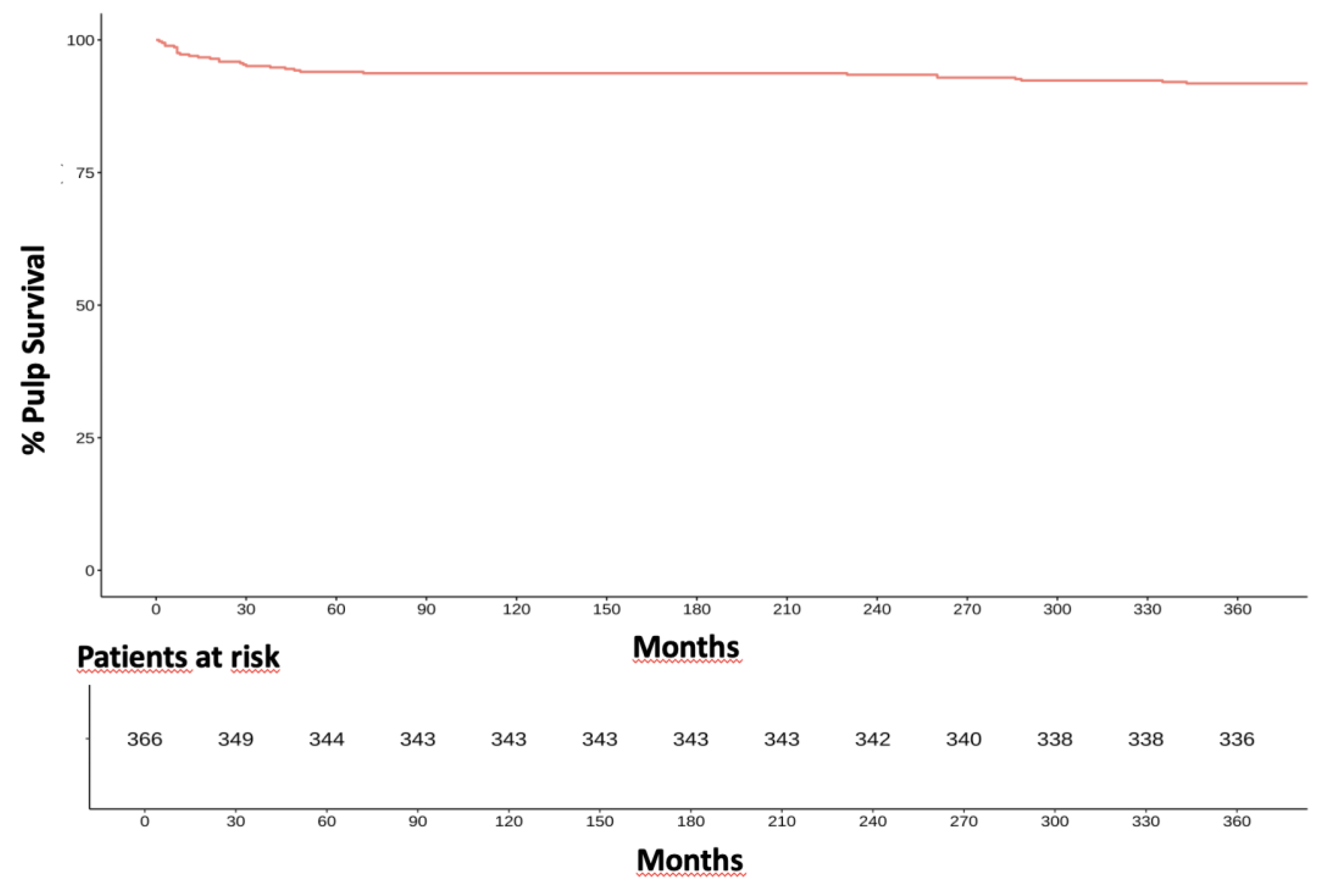
336 of 366 indirectly capped pulps survived the first year after IPC. A detailed analysis of the survival rates within the first year after IPC showed an initial drop in the survival rates within the first 30 days. Here, the survival rate dropped to 95% after 30 days. 343 of the 366 treated pulps (94%) survived the first three months. The survival rate dropped more pronounced during the first 10 days – from 100% to 97%. In the following 80 days, the survival rate dropped by a further 3%. In the further course, the survival rate dropped significantly slower (p<0.05). After one year, the survival rate was 92%. (
Figure 1). This means that the success rate of IPC in the present study was 92% because only failures until 12 months were previously defined as related to the IPC treatment.
3.2. Failures Within the First Year
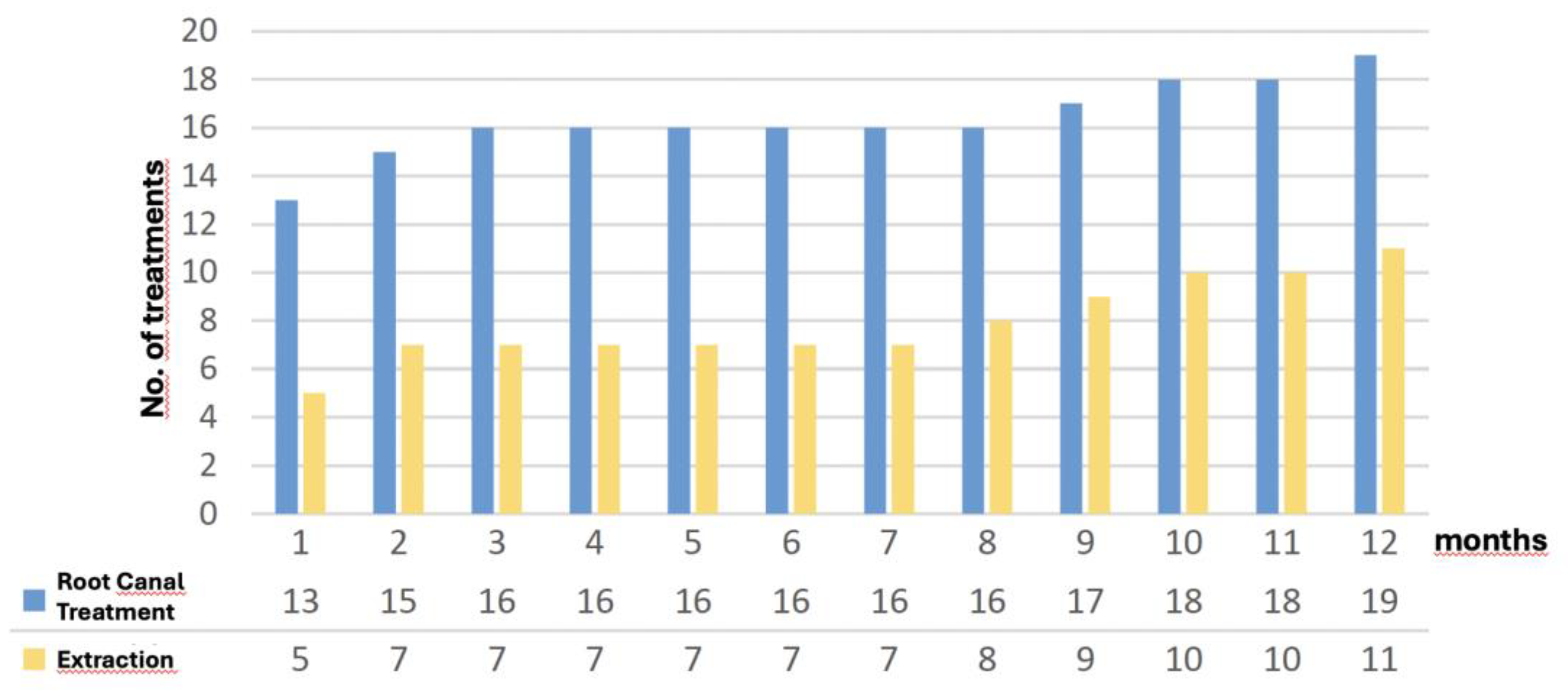
The consequent treatments of failures within the first year i.e. failures per definitionem, are displayed in
Figure 2. Within the first month of observation, a total of 18 IPC treated teeth failed. Of these, 5 teeth were extracted and 13 teeth of the total of 366 treated teeth received root canal treatment within the first month. Thus, 94.1% of the 366 treated teeth survived the first month. After three months, a total of 23 teeth (6.3%) had failed. During this period, two more teeth (out of the original five) were removed and four more teeth (out of the original 12) received root canal treatment. Over the following four months, the failure rate remained static. During this period, no further teeth failed. From the 9th to the 12th month of observation, the failure rate increased to a total of 30 teeth (8.2%). The number of extractions and root canal treatments continued to rise steadily.
3.3. Overall Clinical Outcome
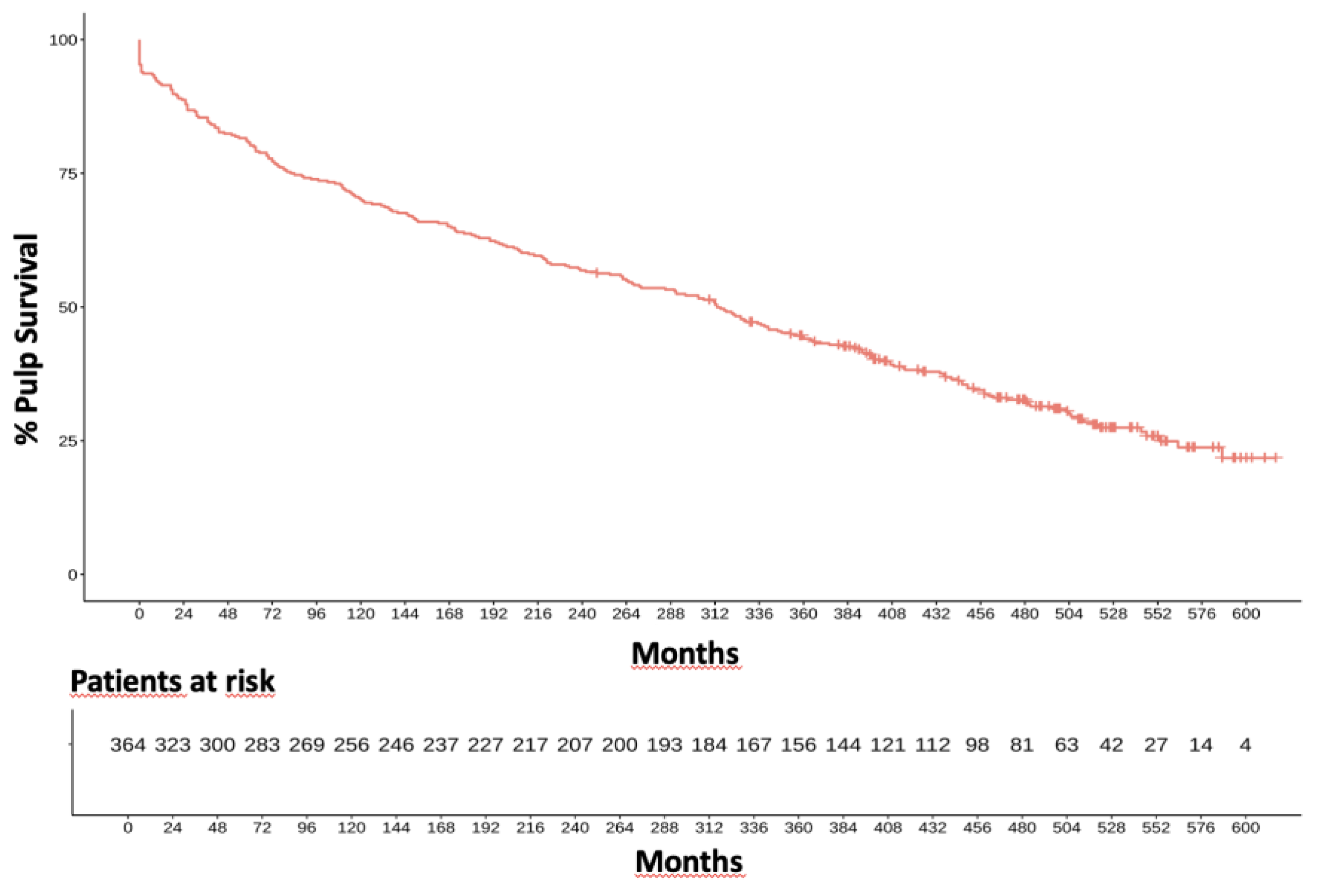
During the remaining 39 years of investigation, a linear occurrence of pulp vitality loss has been observed (
Figure 2). The portions of vital pulps were tested to be 88% after two years, 80% after five years, 70% after 10 years, 57% after 20 years, and 32% after 40 years of clinical investigation resulting in an annual failure rate of 1.7% (
Figure 3).
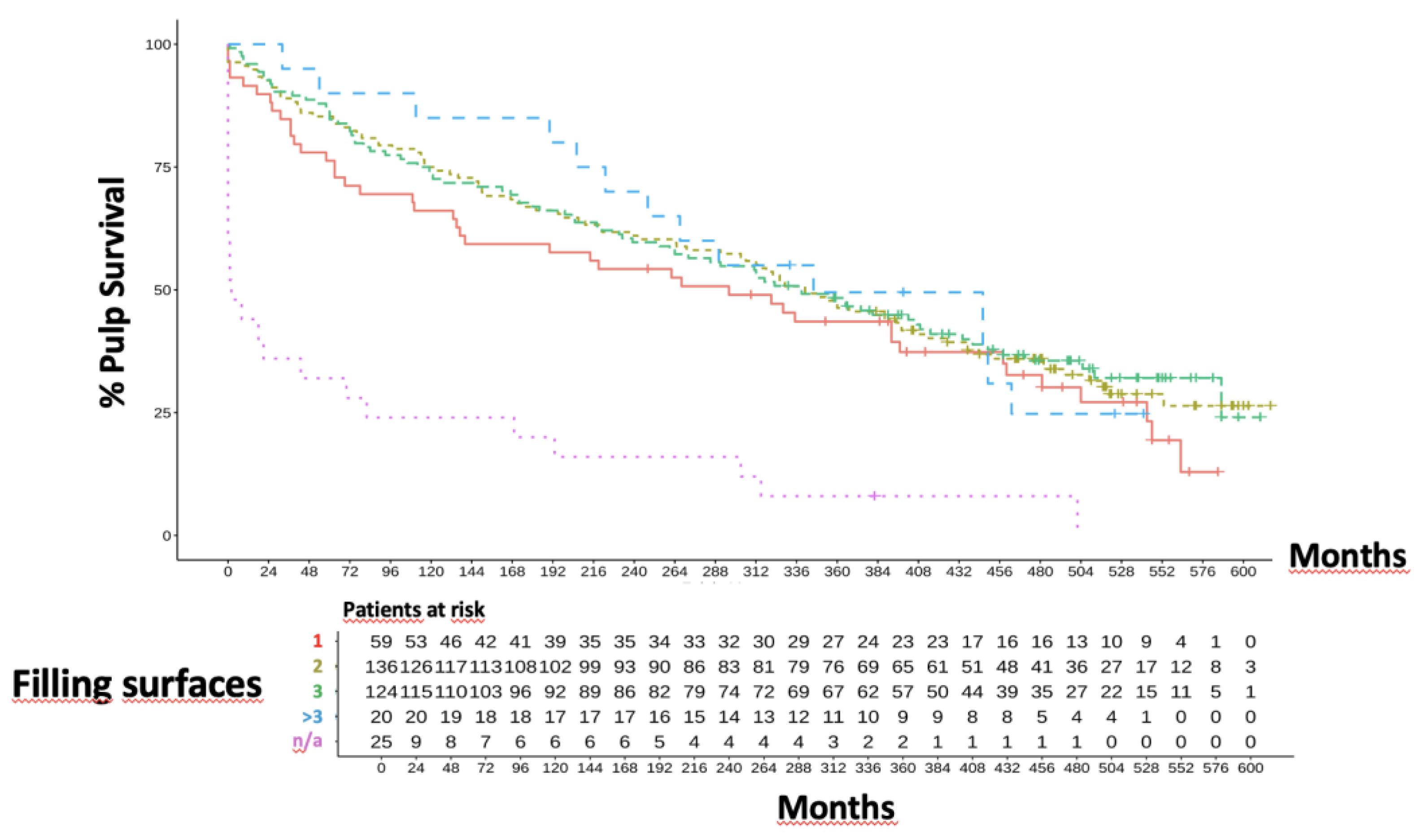
3.3.1. Overall Clinical Outcome Related to Cavity Size
The probability of a tooth with a IPC treatment and a subsequent two-surface filling surviving for 40 years was 36% (
Figure 4). The survival probability of these teeth was thus significantly higher than that of teeth without information on the size of the filling (p<0.05). In 25 of 336 cases, no information was provided regarding the size of the filling or cavity. The cavities of these teeth were treated in their entirety with zinc eugenol cement in order to test survival. These teeth showed highly significantly more failures (>50% after 2 years; p<0.001). This confirmed a statistically significant difference in the survival curves based on cavity size. The cohort comparison of the filling sizes primarily showed that the 336 teeth examined most frequently received a 2- (n=136) or 3- (n=124) surface filling. Smaller, 1-surface fillings were placed about half as often over IPC (n=59). Over the whole observation period of 40 years, cavity size had no negative influence anymore (p=0.063).
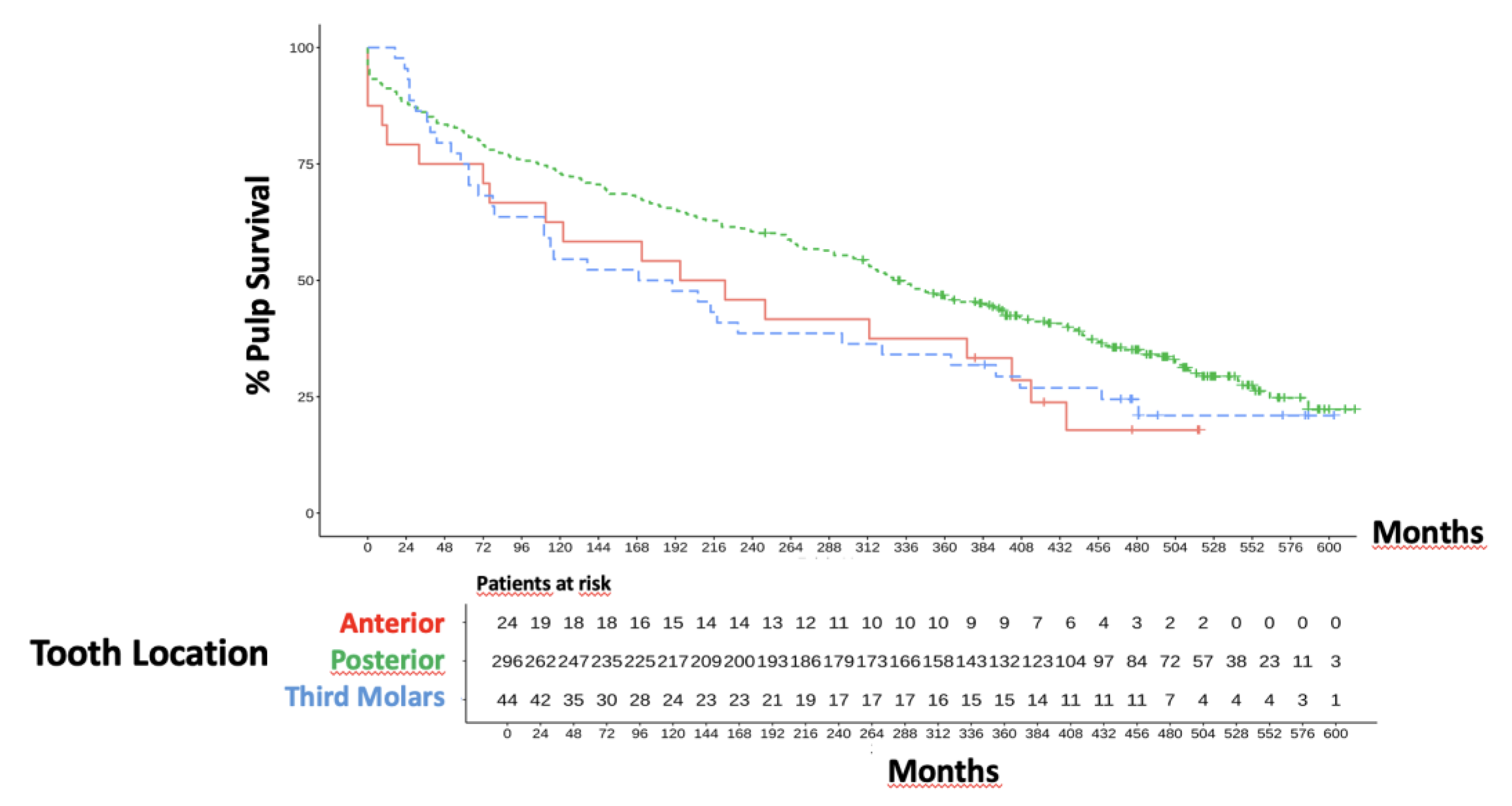
3.3.2. Overall Clinical Outcome Related to Tooth Position
Wisdom teeth initially appeared to have a higher survival rate (93% after 2 years). This value was relativized when considering the survival rates after 5 years to 66% (
Figure 5). In the course of time, the survival rates of wisdom teeth were inferior to those of posterior or anterior teeth. In the long-term analysis (40 years), the curve for the wisdom teeth fell between the survival rates of the front and side teeth. Posterior teeth have been the largest cohort. Here, the number of surviving teeth fell from 296 to 262 within the first 2 years (p=0.774). Thus, no statistically significant differences could be derived with regard to the compared survival rates.
4. Discussion
The present retrospective practice-based study examined the long-term success of indirect capping prior to direct restorative therapy. Given the time period covered by the study, it is logical that materials were used that are now considered outdated[
2]. Nevertheless, the study serves the purpose of evaluating the pulp long-term survival with reduced tooth hard tissues, and this has not been done often in the past[
20,
21,
22,
23]. Of course, the 40-year study period is an advantage of the study, but the main disadvantage is its cross-sectional nature. Today, any kind of restorative therapy is characterized by a fundamentally different way of caries excavation. When the presented treatments have been carried out, of course the chosen excavation strategy was quite aggressive, i.e. extending in to the hypermineralized dentin layer providing a maximum hardness[
16]. Decades later, it has been clearly shown that selective excavation is preferable over the old-fashioned, “complete” and usually aggressive excavation method[
11,
13,
14]. However, also due to the age structure in dentist communities, seemingly complete excavation is still often practiced. Furthermore, the more a complete excavation is conducted, the more often “caries profunda” is present and consequently pulp vitality has to be preserved using IPC[
21,
24,
25].
There are still different views and paradigms when it comes to the phenomenon of deep caries. However, there is always the risk that the vital pulp has already changed due to the effect of bacterial toxins from the carious biomass to such an extent that no indirect capping can stop this process towards pulpitis[
17]. In such cases, it is generally irrelevant whether or not the decimated dentin near the pulp is covered. In theory, these cases should be excluded before the study, but due to the rather stone age pulp diagnostics using cold, this is not possible. Today, it is considered relatively certain that the best way to ensure the vitality of the pulp is to seal the pulp-dentin complex as tightly as possible[
3,
4,
8,
26]. It is also certain that the best quality of the dentin sealing is achieved by an effective adhesive seal of the cavity floor in dentin[
1,
5,
14]. However, this raises the problem that in very deep cavities – we are talking about 300 micrometers and less residual dentin thickness – not only the hybrid layer creates adhesion, but resin tags also always arise independently of the bonding protocol[
1]. However, the latter penetrate up to 300 micrometers into dentin, which means that these resin tags would then be located at the entrance to the pulp in direct contact to the odontoblast layer, which is definitely not beneficial for a healthy pulp[
27]. Regardless of the filling protocol, this leads to the necessity of covering these deep dentin areas[
19]. Would it therefore be sufficient to cover the deep part of the cavity with a non-adhesive cement just to prevent the tags? This theory is at least discussed in an ESE guideline[
8].
The second very widespread paradigm is to cover these deep cavity areas with a bioactive material to actively stimulate tertiary dentin formation, not least to reduce the influence on the pulp through dentin apposition[
19,
22,
25,
28,
29]. For decades, calcium hydroxide was such a material[
30]. In retrospect, the range of applications of calcium hydroxide can almost be considered a fairytale. However, it is not only the effectiveness of calcium hydroxide that is doubted today, but also the clinical handling of the soft pastes and, last but not least, the resorption rate[
8]. Therefore, hydraulic cements are considered the material of choice today, but here too, it must be honestly noted that their effect on pulp exposure has been definitively proven, while the findings for indirect capping vary widely and in some cases light-curing calcium salicylate materials are also considered to be positive[
20,
24]. These facts lead to the assumption that in the end it really doesn't matter what we use to cover this area, since “the seal is the deal” remains the primary success factor[
3]. And this is precisely where the current study comes full circle. Regardless of whether deep dentin is covered with old-fashioned or “modern” materials, long-term clinical observations remain the key to gaining insights. And that is why the present study is of general interest to the field of restorative dentistry.
The present retrospective, practice-based investigation demonstrates that even old-fashioned IPC using conventional zinc eugenol cement as base material works out nicely over 40 years. It was a characteristic finding that apparently the first weeks after treatment decide whether the IPC treatment is successful or not. Of course, several of these cases may have suffered the fact that irreversible pulp damage was already present without having been exactly diagnosable prior to the treatment. This is clearly visible when early losses of pulp vitality occurred. Another interesting finding is that the teeth that received n/a, i.e. where expectative measures were taken into account, extremely often failed. Although the size of the carious lesion and consequently the size of the cavity did not appear to influence the long-term results, this was different at least during the vulnerable first phase of the observation period.
So what is finally the decisive factor for successful treatment of deep caries? From today’s knowledge, it seems to be advisable to selectively remove caries in order not even get close to the question whether IPC is necessary at all[
11,
12,
13,
16,
31,
32]. For the case of old-school, seemingly complete caries excavation (which fakes sterile conditions and actually never happens[
13]) also conventional cements like in the present study may be successful. For the case of fully adhesive restorations such as direct resin composites, it is finally also important that IPC materials are compatible with consequent bonding procedures instead of corroborating them via substantial contamination of the bonded surface[
26].
5. Conclusions
IPC showed an excellent long-term success after 40 years of clinical service. The predominant number of failures after IPC occurred during the first three months. In this vulnerable period, larger defects as well as expectative measures lead to significantly more frequent pulp damage.
Supplementary Materials
on file.
Author Contributions
Conceptualization, S.B. methodology, R.F.; software, A.K., B.B.-B., validation, R.F. and A.K.; formal analysis, R.F.; investigation, L.P.; resources, S.B.; data curation, R.F.; writing—original draft preparation, R.F. and A.K.; writing—review and editing, R.F.; visualization, A.K.; supervision, S.B. and R.F.; project administration, R.F.; All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Data Availability Statement
Data are available on reasonable request.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Van Meerbeek B, Yoshihara K, Van Landuyt K et al. From Buonocore’s Pioneering Acid-Etch Technique to Self-Adhering Restoratives. A Status Perspective of Rapidly Advancing Dental Adhesive Technology. J. Adhes. Dent 2020, 2020 22, 7–34.
- Pilcher L, Pahlke S, Urquhart O et al. Direct materials for restoring caries lesions: Systematic review and meta-analysis-a report of the American Dental Association Council on Scientific Affairs. J Am Dent Assoc 2023; 154 (2): e1-e98.
- Bergenholtz, G. Evidence for Bacterial Causation of Adverse Pulpal Responses in Resin-Based Dental Restorations. Crit. Rev. Oral Biol. Med. 2000, 11, 467–480. [Google Scholar] [CrossRef] [PubMed]
- Frankenberger, R.; Reinelt, C.; Glatthöfer, C.; Krämer, N. Clinical performance and SEM marginal quality of extended posterior resin composite restorations after 12 years. Dent. Mater. 2020, 36, E217–E228. [Google Scholar] [CrossRef] [PubMed]
- van de Sande, F.H.; Rodolpho, P.A.D.R.; Basso, G.R.; Patias, R.; da Rosa, Q.F.; Demarco, F.F.; Opdam, N.J.; Cenci, M.S. 18-year survival of posterior composite resin restorations with and without glass ionomer cement as base. Dent. Mater. 2015, 31, 669–675. [Google Scholar] [CrossRef]
- Gorodovsky, S.; Zidan, O. Retentive strength, disintegration, and marginal quality of luting cements. J. Prosthet. Dent. 1992, 68, 269–274. [Google Scholar] [CrossRef]
- Opdam NJ, Bronkhorst EM, Loomans BA, Huysmans MC. 12-year survival of composite vs. amalgam restorations. J Dent Res 2010; 89 (10): 1063-1067.
- By, E.S.O.E. (.D.; Duncan, H.F.; Galler, K.M.; Tomson, P.L.; Simon, S.; El-Karim, I.; Kundzina, R.; Krastl, G.; Dammaschke, T.; Fransson, H.; et al. European Society of Endodontology position statement: Management of deep caries and the exposed pulp. Int. Endod. J. 2019, 52, 923–934. [Google Scholar] [CrossRef]
- Akin, D.; Ozkaya, C.A.; Armagan, G.; Birim, D.; Ates, M.; Tezel, H. Biological and physical properties of calcium hydroxide-based pulp-capping materials and their modifications. J. Oral Sci. 2024, 66, 91–95. [Google Scholar] [CrossRef]
- Taghvaei, N.; Ghavami-Lahiji, M.; Evazalipour, M.; Davalloo, R.T.; Zamani, E. Ion release, biocompatibility, and bioactivity of resin-modified calcium hydroxide cavity liners. BMC Oral Heal. 2023, 23, 1–11. [Google Scholar] [CrossRef]
- Maltz, M.; Alves, L.S.; Jardim, J.J.; Moura, M.D.S.; De Oliveira, E.F. Incomplete caries removal in deep lesions: a 10-year prospective study. . 2011, 24, 211–4. [Google Scholar]
- Recchi, A.F.; de Azambuja, R.S.; Alves, L.S.; Maltz, M.; Jardim, J.J. Restorations performance after selective caries removal to soft dentine: 18-month follow-up of a controlled clinical trial. J. Dent. 2024, 147, 105099. [Google Scholar] [CrossRef]
- Schwendicke F, Dorfer CE, Paris S. Incomplete caries removal: a systematic review and meta-analysis. J Dent Res 2013; 92 (4): 306-314.
- Widbiller, M.; Weiler, R.; Knüttel, H.; Galler, K.M.; Buchalla, W.; Scholz, K.J. Biology of selective caries removal: a systematic scoping review protocol. BMJ Open 2022, 12, e061119. [Google Scholar] [CrossRef] [PubMed]
- Arandi, N.Z.; Rabi, T. Cavity Bases Revisited. Clin Cosmet Investig Dent 2020, 12, 305–312. [Google Scholar] [CrossRef] [PubMed]
- Fraser, J.; MacInnes, A. Which caries removal method to select? Evid Based Dent 2024. [Google Scholar]
- Schweikl, H.; Buchalla, W.; Krifka, S. Cell responses to cariogenic microorganisms and dental resin materials-Crosstalk at the dentin-pulp interface? Dent Mater 2017, 33, 514–524. [Google Scholar]
- Galler, K.; Schweikl, H.; Hiller, K.-A.; Cavender, A.; Bolay, C.; Ouza, D.; Schmalz, G. ; D’souza TEGDMA Reduces Mineralization in Dental Pulp Cells. J. Dent. Res. 2010, 90, 257–262. [Google Scholar] [CrossRef]
- Vural, U.; Kiremitçi, A.S.; Gökalp, S. Which is the most effective biomaterial in indirect pulp capping? 4- year comparative randomized clinical trial. Eur. Oral Res. 2022, 56, 35–41. [Google Scholar] [CrossRef]
- Yavuz, Y.; Kotanli, S.; Dogan, M.S.; Almak, Z. Examination of 6 and 12 month follow-up of calcium hydroxide and calcium silicate materials used in direct and indirect pulp capping. Adv. Clin. Exp. Med. 2025, 34. [Google Scholar] [CrossRef]
- García-Mota, L.F.; Hardan, L.; Bourgi, R.; Zamarripa-Calderón, J.E.; Rivera-Gonzaga, J.A.; Hernández-Cabanillas, J.C.; Cuevas-Suárez, C.E. Light-Cured Calcium Silicate Based-Cements as Pulp Therapeutic Agents: A Meta-Analysis of Clinical Studies. J. Évid. Based Dent. Pr. 2022, 22, 101776. [Google Scholar] [CrossRef]
- Vural, U.K.; Kiremitci, A.; Gokalp, S. Randomized Clinical Trial to Evaluate MTA Indirect Pulp Capping in Deep Caries Lesions After 24-Months. Oper. Dent. 2017, 42, 470–477. [Google Scholar] [CrossRef]
- Miotti, L.L.; Vissotto, C.; De Nardin, L.; Manjabosco, B.d.A.; Tuchtenhagen, S.; Münchow, E.A.; Emmanuelli, B. Does the liner material influence pulpal vitality in deep carious cavities submitted to selective caries removal? A network meta-analysis review. Clin. Oral Investig. 2023, 27, 1–14. [Google Scholar] [CrossRef]
- Semprum-Clavier, A.; Rodriguez, A.; Salazar, D.; Afshari, F.; Manzotti, A.; Saleh-Hassan, L.; Viana, M.; Bedran-Russo, A. Clinical Comparison of Three Indirect Pulp Capping Restorative Protocols: A Randomized Controlled Prospective Study. Oper. Dent. 2024, 49, 11–19. [Google Scholar] [CrossRef] [PubMed]
- Kunert, M.; Lukomska-Szymanska, M. Bio-Inductive Materials in Direct and Indirect Pulp Capping—A Review Article. Materials 2020, 13, 1204. [Google Scholar] [CrossRef]
- Frankenberger, R.; Nassiri, S.; Lücker, S.; Lygidakis, N.N.; Krämer, N. The effect of different liners on the bond strength of a compomer to primary teeth dentine: in vitro study. Eur. Arch. Paediatr. Dent. 2021, 22, 643–649. [Google Scholar] [CrossRef] [PubMed]
- Shang, W.; Zhang, Z.; Zhao, X.; Dong, Q.; Schmalz, G.; Hu, S. [Retracted] The Understanding of Vital Pulp Therapy in Permanent Teeth: A New Perspective. BioMed Res. Int. 2022, 2022, 8788358. [Google Scholar] [CrossRef]
- Lin, Y.-Y.; Zhang, P.; Cheon, K.; Jackson, J.G.; Lawson, N.C. Chemical and Physical Properties of Contemporary Pulp Capping Materials. Pediatr Dent 2022, 44, 207–212. [Google Scholar] [PubMed]
- Mahapatra, J.; Nikhade, P.; Patel, A.; Taori, P.; Relan, K. Comparative Evaluation of the Efficacy of Light-Cured Calcium Hydroxide and a Fourth-Generation Calcium Silicate Cement (TheraCal LC) as Indirect Pulp Capping Materials in Patients With Deep Carious Lesions: A Randomized Parallel-Group Clinical Trial. Cureus 2022, 14. [Google Scholar] [CrossRef]
- Selvendran, K.; Ahamed, A.S.; Krishnamurthy, M.; Kumar, V.N.; Raju, V.G. Comparison of three different materials used for indirect pulp capping in permanent molars: An in vivo study. J. Conserv. Dent. 2022, 25, 68–71. [Google Scholar] [CrossRef]
- Jardim, J.J.; Alves, L.S.; Decourt, R.F.; de Paula, L.M.; Mestrinho, H.D.; Maltz, M. Cost-effectiveness of selective caries removal versus stepwise excavation for deep caries lesions. Braz. Oral Res. 2023, 37, e083. [Google Scholar] [CrossRef]
- Jardim, J.J.; Mestrinho, H.D.; Koppe, B.; de Paula, L.M.; Alves, L.S.; Yamaguti, P.M.; Almeida, J.C.F.; Maltz, M. Restorations after selective caries removal: 5-Year randomized trial. J. Dent. 2020, 99, 103416. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).