1. Introduction
Numerous studies have assessed factors that may influence outcome of conservative treatment of apical periodontitis (1). Many of the preoperative, perioperative and postoperative host- and tooth-specific factors that are readily recorded have not been found to significantly impact results in patient-based, cohort studies or in randomised clinical tests Felt (2). However, preoperative periapical diagnosis strongly influences outcome (3), and tooth type, periodontal status, and age are factors with an uncertain relationship to treatment result (2) .
The number of visits is not normally included as a variable in cohort studies of treatment outcome. Randomized studies have established the principle of single-visit treatment as an adequate procedure (4, 5), and systematic reviews (6-8) have clearly documented that the procedure is viable and performs similarly to the more conventional concept of applying an interim dressing between appointments. Moreover, a meta-analysis of relevant clinical data found no benefit from a calcium hydroxide dressing (9). However, controlled trials do not address the effect of number of visits in actual clinical practice. Here, case complexity (10) with time constraints may determine whether a tooth is treated in one or more sessions, and many teeth that could be completed in a single visit are likely to be treated in two or more sessions, possibly improving their chance of success. On the other hand, time constraints may cause the tooth to be poorly cleaned, and the temporary filling is a risk factor for bacterial contamination. Thus, while the dressing may reduce the bacterial load in many cases, an increase in the level of infection may also take place (11, 12).
Only a few studies have addressed the impact of the number of sessions in a practice setting, with conflicting results (13, 14). Thus the outcome of single-visit treatments outside of randomized studies in a research setting is largely unknown. The single-visit approach has been accepted but not explicitly promoted in the postgraduate endodontic clinic at the University clinic for more than 15 years. The present study aims to assess the radiographic outcome of root canal treatment in teeth with periapical lesions, with specific attention to the impact of number of visits in comparison with, and adjusted for, other salient prognostic factors.
2. Materials and Method
2.1. Source of Data
The patient databases at the Department of Endodontics provided treatment details and radiographs for all endodontic treatments. The study is part of a project that has been reviewed and accepted by the Regional Ethics Board (REC southeast) in Norway (64 996 Resultatanalyse av endodontisk behandling).
2.2. Case Selection and Treatment
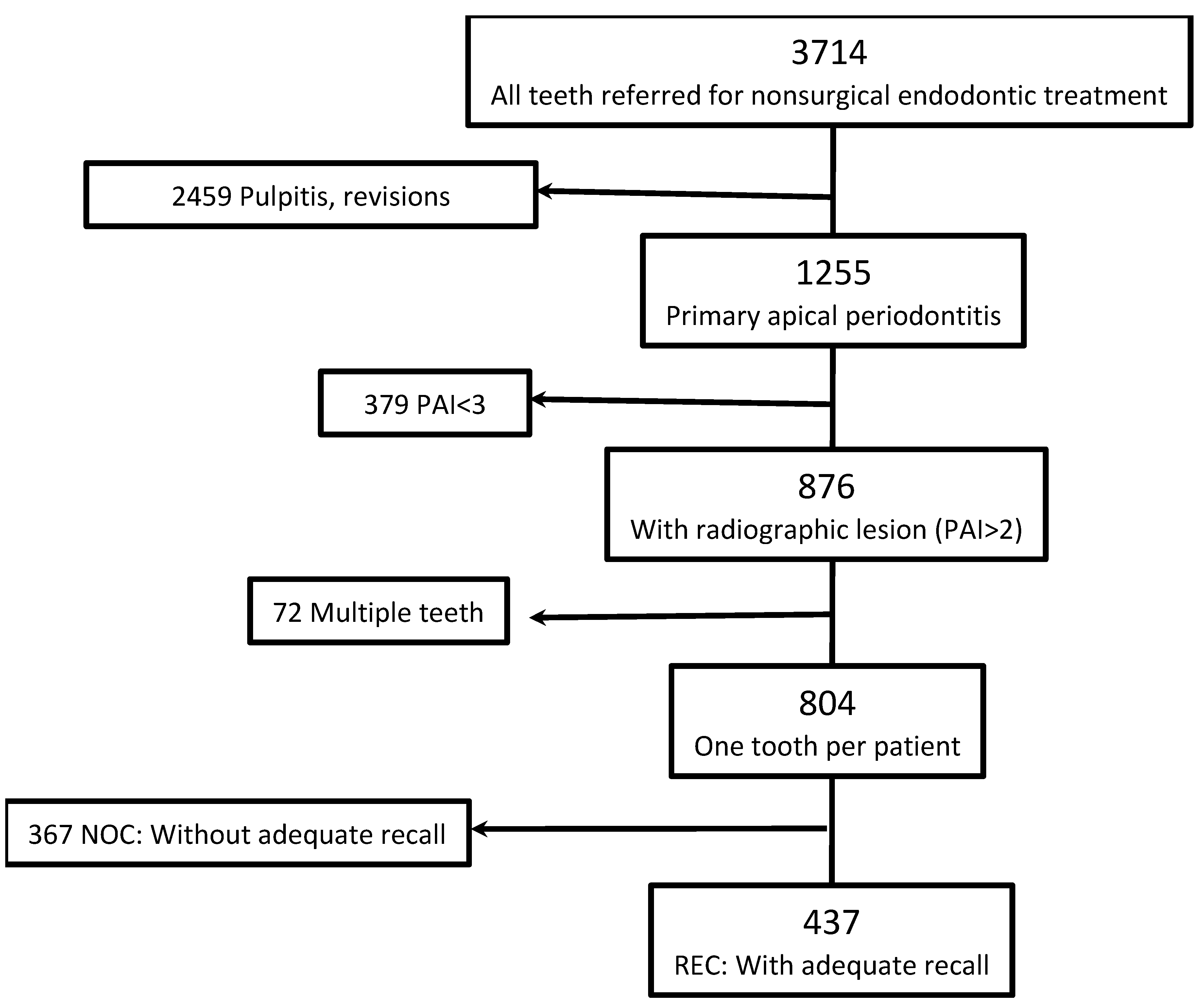
Data for 1255 teeth referred to the postgraduate clinic at the Department of Endodontics for first-time, non-surgical treatment of teeth with periapical lesions between March 2008 and December 2021 were retrieved from the electronic records. Cases with less than 11 months of follow-up data were excluded, as were cases with no or unclear radiographic signs of apical periodontitis (pre-operative periapical index [PAI]) score 1 or 2 (15)). If more than one tooth was treated in a patient, only the most distal tooth was included (
Figure 1).
Table 1 lists the registrations done for each case. In all, 437 cases fulfilled the inclusion criteria with adequate recall. See
Figure 1.
Protocols for non-surgical treatment were stable with minimal alterations from 2008 through 2021, and followed the Guidelines of the European Society of Endodontology (ESE) (16).
2.3. Radiographic Evaluation
The periapical conditions were scored with the PAI scoring system. All scoring was done by two observers (EG, TD) calibrated against a standard set of 100 periapical radiographs scored twice. Weighted Cohen’s kappa values were 0.8 and 0.71, respectively. All radiographs were digital, acquired by the Digora phosphor storage plate system (PSP; DIGORA Accessory intraoral imaging plates, Soredex Tuusula, Finland) and evaluated on screen in a dimly lit room. PAI scores at control were adjusted to record outcome by 2 different criteria (
Table 2).
2.4. Statistical Analysis
Chi-square test was used to determine differences in treatment outcome among groups of teeth. Actual p values were recorded. Logistic regression analyses of outcome were performed for a comprehensive evaluation of all recorded factors influencing outcome, with a gradual elimination of factors with p values below 0.2. All analyses were with Stata version 18.0 software (17).
3. Results
3.1. Characterization of Cases
Recall cases vs cases excluded. The recorded parameters were generally similar for the NOC and REC groups; however, there were more teeth with PAI score 4 and more teeth with soft tissue affections at completion of treatment in the NOC group. See Supplementary
Table 1.
3.2. Factors Influencing Treatment Outcome
Binary analyses. The success rate of treatment for all recalled teeth was 69% by strict and 84% by lenient criteria. The results of all binary analyses are given in Supplementary
Table 2. PAI score at start, patients’ age, periodontal status, and the number of visits showed strong associations with outcome, and there was a tendency for premolars and molars to do better than anterior teeth (
Table 3).
While pain/discomfort had a marginal association with better outcome for teeth with pain at the time of filling (p=0.18) and root fillings with questionable density tended to have better outcome than densely filled teeth (p=0.09); these subgroups had very low numbers, showed no effect in preliminary regression analyses and were therefore excluded from the final model. (Supplementary
Table 2A & B.)
Logistic regression analyses. Logistic regression with independent variables selected from binary comparisons confirmed pre-operative PAI score, number of visits, marginal bone level, age, and tooth group as primary influencers on outcome (
Table 4 A). Results with lenient criteria lost the effect of PAI score, age and bone height, but the effect of tooth type and the number of visits remained (
Table 4 B).
3.3. Binary Analyses of Subgroups of Categories with Impact in the Regression
Age distribution: When cases were grouped by age as younger than 35, from 35 to 65, and above 65, the older age group (>65) contributed most to the effect of age.
Table 5 A.
Periodontal status: Cases were grouped by bone height into 4 categories: > 2/3 of root length; from ½ to 2/3 of root length; from 1/3 to ½ of root length; and <1/3 of root length. Seven teeth could not be scored reliably. The negative effect on prognosis was clearly greater for the latter two categories.
Table 5 B.
Tooth group: Teeth were grouped as anterior teeth (A), premolars (P), and molars (M). Premolars tended to do better than molars and, especially, anterior teeth.
Table 5 C.
Number of visits: When cases were grouped as single-visit (SV) and multiple-visit (MV) cases, the SV cases had a higher success rate (80 vs 66%) in chi square analyses (
p =0.045). When comparing SV with two visits only (TV) the association weakened but was still strong (p=0.076).
Table 5 D & E.
4. Discussion
This study focused exclusively on teeth with a radiographically confirmed diagnosis of apical periodontitis, representing a definitive sign of infection. Most of the commonly recognized tooth-related factors were registered in our study; however, patients’ health status and smoking habits were not registered. While these factors may influence outcome to a degree (2), there is little reason to assume that they would be distributed systematically different among the groups compared.
About 46 per cent of the cohort studied did not have adequate details or did not appear for a follow-up. These cases were largely similar to the cases with control but differed in distribution of PAI scores in that more had PAI 3 at start. While it may be assumed that as a group, these teeth would therefore have had a better prognosis, this difference would not likely affect the generalizability of the main findings.
The true outcome estimate will be influenced also by factors not recorded here, such as smoking, general health issues and others. However, there is no reason to believe that such factors would be distributed unevenly across the groups we have analyzed, which makes it likely that the results in binary and in regression analyses are valid for comparisons among and between groups of teeth.
Up to 4 years may be required to record a stable outcome that reflects the true prognosis of the endodontic treatment (18), but the general trend of healing is evident after one year (19). Our patients were followed for up to four years, which is consistent with recommendations (20), but we chose control data closest to one year for groups to be comparable in this respect even when later information was available. One year is also the standard recall period recommended (21).
Preoperative PAI score was another robust predictor of healing in the present study. Teeth with higher baselines scores had lower healing rates, which is consistent with the literature (3) and with our understanding that more advanced lesions require longer healing processes.
The outcome was significantly influenced also by age. Technical challenges during root canal treatment may increase with age, particularly due to the increased occurrence of root canal calcifications (22, 23). A systematic review examining longitudinal outcomes of endodontic treatment suggested that increased patient age is not generally a prognostic factor (24), but a more recent report found that younger patients tended to have more favorable outcomes (25). Periodontal status similarly showed a strong association with outcome in our study, which is consistent with most reports on marginal bone level and endodontic treatment outcome (2). Given that age and marginal bone level were highly correlated, this could help explain the strong effect of age in in our material. Despite this correlation, however, both factors retained a strong impact when combined in regression analyses. Therefore, it may be possible that they may differ in the way they influence prognosis.
Tooth type also influenced prognosis. Anterior teeth, despite generally simpler root canal anatomy, demonstrated lower success rates compared to premolar and molars in our cohort. This may be related to unmeasured clinical factors, like calcified root canals in traumatized teeth.
The results of this study demonstrated that the radiographic outcome was negatively affected by the number of visits, even when corrected for confounders in regression analyses.
The time and visits needed to treat chronic apical periodontitis in a practice setting depends on numerous factors. Available time and case complexity are important factors, and simple cases that may be treated quickly are obviously more often treated in a single visit. The present study was moreover conducted in a teaching environment where didactic considerations may have played a role, thus making the assignment of cases to one or more visits even more complex. However, single- vs multiple-visit approaches may differ in a way that could be reflected in outcome irrespective of the mode of case selection for the two approaches: on the one hand, instrumentation and disinfection in one appointment may not be sufficient for adequate disinfection thereby necessitating and benefitting from more appointments; on the other, inadequacies in instrumentation, irrigation, medication and the temporary filling may impair rather than improve infection control in two or more appointments.
The results were conspicuously poorer for teeth that were treated in more than three sessions: these teeth could be complex with a poor prognosis from the outset regardless of the number of visits. We therefore did a separate analysis comparing single visit cases with cases completed in two sessions, which would exclude many such cases that would otherwise reduce the success rate of multi-visit cases. While the difference in favor of single-visit treatment was reduced when cases with more than two visits were excluded, the association was still strong. These findings strengthen the clinical practice guidelines from The European Society of Endodontology, which recommend using a single-visit approach without the use of interappointment dressing with Ca(OH)2 in cases where appropriate clinical procedures can be performed within an adequate time frame (21).
5. Conclusions
The overall outcome of first-time treatment of teeth with periapical lesions by postgraduate students was negatively influenced by higher pre-operative PAI scores, higher number of visits, poorer periodontal status, older age, and anterior tooth type. Single-visit treatment showed better outcome compared to multiple- or two-visit treatment in binary and regression analyse, suggesting that a single-visit approach may have some advantage in addition to saving time and cost.
Acceptance for using the patient data was obtained from The Regional Committee for Medical and Health Research Ethics in Norway (REK 2018/64996).
Supplementary Materials
The following supporting information can be downloaded at the website of this paper posted on Preprints.org.
Author Contributions
Design of study: PTS, EG, TD, TH, DØ; collection and retrieval of data from records: EG, TD, DØ; scoring of data: EG, TD; analyses and statistics: DØ, TD, EG, PTS; manuscript preparation and finalization: PTS, EG, TD, TH, DØ.
Funding
The study has no external funding.
Institutional Review Board Statement
The study has ethics approval. The relevant documents are uploaded separately.
Informed Consent Statement
Patient consent was deemed not necessary by the ethics committee.
Data Availability Statement
The data underlying this study may be available on appropriate request.
Conflicts of Interest
None of the authors has any conflict of interest.
References
- Piñas-Alonzo, R.; Bello, R.; Hernández, A.; Lacerda, M.; Vinuesa-Maqueda, C.; Pérez-Ron, O.; et al. Clinical outcomes and prognostic factors in endodontic treatment: a systematic review from 2002-2022. British dental journal 2025. [CrossRef] [PubMed]
- Kirkevang, L.L.; Vaeth, M. Epidemiology, Treatment Outcome, and Risk Factors for Apical Periodontitis. In: Orstavik D, editor. Essential Endodontology: Prevention and Treatment of Apical Periodontitis. Oxford: Wiley; 2020. p. 143-178.
- Kirkevang, L.L.; Orstavik, D.; Wenzel, A.; Vaeth, M. Prognostic value of the full-scale Periapical Index. Int Endod J 2014. [CrossRef] [PubMed]
- Paredes-Vieyra, J.; Enriquez, F.J. Success rate of single- versus two-visit root canal treatment of teeth with apical periodontitis: a randomized controlled trial. J Endod 2012, 38, 1164–1169. [Google Scholar] [CrossRef] [PubMed]
- Karaoğlan, F.; Miçooğulları Kurt, S.; Çalışkan, M.K. Outcome of single- versus two-visit root canal retreatment in teeth with periapical lesions: A randomized clinical trial. Int Endod J 2022, 55, 833–843. [Google Scholar] [CrossRef] [PubMed]
- Moreira, M.S.; Anuar, A.S.N.-S.; Tedesco, T.K.; Dos Santos, M.; Morimoto, S. Endodontic treatment in single and multiple visits: an overview of systematic reviews. Journal of endodontics 2017, 43, 864–870. [Google Scholar] [CrossRef] [PubMed]
- Schwendicke, F.; Gostemeyer, G. Single-visit or multiple-visit root canal treatment: systematic review, meta-analysis and trial sequential analysis. BMJ open 2017, 7, e013115. [Google Scholar] [CrossRef] [PubMed]
- Mergoni, G.; Ganim, M.; Lodi, G.; Figini, L.; Gagliani, M.; Manfredi, M. Single versus multiple visits for endodontic treatment of permanent teeth. Cochrane Database of Systematic Reviews 2022(12).
- Rossi-Fedele, G.; Roedig, T. Effectiveness of root canal irrigation and dressing for the treatment of apical periodontitis: A systematic review and meta-analysis of clinical trials. International endodontic journal 2023, 56:422-435.
- Chung, S.H.; Chang, J. Impact of endodontic case difficulty on operating time of single visit nonsurgical endodontic treatment under general anesthesia. BMC Oral Health 2021, 21, 231. [Google Scholar] [CrossRef] [PubMed]
- Peters, L.B.; van Winkelhoff, A.J.; Buijs, J.F.; Wesselink, P.R. Effects of instrumentation, irrigation and dressing with calcium hydroxide on infection in pulpless teeth with periapical bone lesions. Int Endod J 2002, 35, 13–21. [Google Scholar] [CrossRef] [PubMed]
- Zandi, H.; Kristoffersen, A.K.; Orstavik, D.; Rocas, I.N.; Siqueira, J.F.; Jr Enersen, M. Microbial Analysis of Endodontic Infections in Root-filled Teeth with Apical Periodontitis before and after Irrigation Using Pyrosequencing. J Endod 2018, 44, 372–378. [Google Scholar] [CrossRef] [PubMed]
- Jurič, R.; Vidmar, G.; Blagus, R.; Jan, J. Factors associated with the outcome of root canal treatment—A cohort study conducted in a private practice. Int Endod J 2024, 57, 377–393. [Google Scholar] [CrossRef] [PubMed]
- Field, J.W.; Gutmann, J.L.; Solomon, E.S.; Rakusin, H. A clinical radiographic retrospective assessment of the success rate of single-visit root canal treatment. Int Endod J 2004, 37, 70–82. [Google Scholar] [CrossRef] [PubMed]
- Orstavik, D.; Kerekes, K.; Eriksen, H.M. The periapical index: a scoring system for radiographic assessment of apical periodontitis. Endodontics & dental traumatology 1986, 2, 20–34. [Google Scholar]
- Loest, C. Quality guidelines for endodontic treatment: consensus report of the European Society of Endodontology. International endodontic journal 2006, 39:921-930.
- Stata. Stata Statistical Software: Release 18. In. College Station, TX: Stata Corp.; 2023.
- Kerekes, K.; Tronstad, L. Long-term results of endodontic treatment performed with a standardized technique. Journal of endodontics 1979, 5, 83–90. [Google Scholar] [CrossRef] [PubMed]
- Orstavik, D. Time-course and risk analyses of the development and healing of chronic apical periodontitis in man. International endodontic journal 1996, 29, 150–155. [Google Scholar] [CrossRef] [PubMed]
- Endodontology ESo. Quality guidelines for endodontic treatment: consensus report of the European Society of Endodontology. Int Endod J 2006, 39, 921–930.
- Duncan, H.F.; Kirkevang, L.L.; Peters, O.A.; El-Karim, I.; Krastl, G.; Del Fabbro, M.; et al. Treatment of pulpal and apical disease: The European Society of Endodontology (ESE) S3-level clinical practice guideline. International endodontic journal 2023. [CrossRef] [PubMed]
- Morse, D.R.; Esposito, J.V.; Schoor, R.S.; Williams, F.L.; Furst, M.L. A review of aging of dental components and a retrospective radiographic study of aging of the dental pulp and dentin in normal teeth. Quintessence International 1991, 22. [Google Scholar]
- Kiefner, P.; Connert, T.; ElAyouti, A.; Weiger, R. Treatment of calcified root canals in elderly people: a clinical study about the accessibility, the time needed and the outcome with a three-year follow-up. Gerodontology 2017, 34, 164–170. [Google Scholar] [CrossRef] [PubMed]
- Shakiba, B.; Hamedy, R.; Pak, J.G.; Barbizam, J.V.; Ogawa, R.; White, S.N. Influence of increased patient age on longitudinal outcomes of root canal treatment: a systematic review. Gerodontology 2017, 34, 101–109. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.-Q.; Chen, X.; Wang, X.-X.; Liu, W.; Zhou, X.; Wang, X. Outcomes and prognostic factors of apical periodontitis by root canal treatment and endodontic microsurgery-a retrospective cohort study. Annals of Palliative Medicine 2021, 10, 5027–5045. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).