1. Introduction
Sexually Transmitted Infections (STIs) remains a major public health concern. More than 30 pathogens can be transmitted through sexual intercourse, and near one million people are infected with a curable sexually transmitted pathogen every day [1,2]. The World Health Organization estimated an incidence of more than 377 million cases of chlamydia, gonorrhoea, trichomoniasis and syphilis in women and men during 2020 [3]. Although the incident cases of trichomoniasis are near 156 million [4], these epidemiological data may be underestimated due to the high number of asymptomatic patients [5], the low sensitivity of the preferred diagnostic methods used in many regions [6] and the fact that Trichomonas vaginalis infection is not a notifiable disease [7]. For all these, trichomoniasis has been included in the list of neglected parasitic infections (NPI) by the Center for Disease Control and Prevention (CDC) [8].
Trichomoniasis is characterized by a wide range of signs and symptoms associated with the inflammatory response triggered by the settlement of the parasite [9]. In women, about 75% of patients develop clinical manifestations. The most common are pruritus, local edema, erythema, dysuria and/or a typical green, frothy and malodorous vaginal discharge, among others [5,10,11]. In men, near 80% are asymptomatic, however, nongonococcal urethritis, epididymitis, or prostatitis may occur [5,10]. Although trichomoniasis has been considered as a “nuisance” infection [12,13], the complications and risks associated with this STI have led to its inclusion in the WHO Global Health Strategy on STIs for the period 2022-2030 [2]. T. vaginalis increases 1.5 times the risk of acquiring HIV [14] but also favors its transmission due to the imbalance in the vaginal microbiome, the proinflammatory immune response and the elevated vaginal pH [15]. In this scenario, co-infections with different urogenital pathogens are common among women with trichomoniasis i.e. Chlamydia trachomatis, Neisseria gonorrhoeae, Treponema pallidum, human papillomavirus or herpes simplex virus types 1 and 2 [16,17]. Other serious sequelae include pelvic inflammatory disease (PID) [2], adverse pregnancy outcomes [9,18] and infertility [9]. Moreover, several studies have associated trichomoniasis with an increased risk of cervical carcinogenesis [19,20,21]; notwithstanding, the association between T. vaginalis and prostate cancer remains under discussion [22,23,24].
This STI has been treated with metronidazole since 1959 [25]. Four decades later the use of tinidazole was accepted [26,27,28] and recently the Food and Drug Administration has approved the use of secnidazole in the United States [29]. Despite the existence of drugs against T. vaginalis, almost 10% of clinical cases are resistant [30] and cross-resistance between 5-nitroimidazole drugs has been reported [31]. The absence of pharmacological alternatives to cope with treatment failure, hypersensitivity to 5-nitroimidazoles or side effects [32,33] increase the risk of transmission and the development of chronic infection. Additionally, as trichomoniasis is highly asymptomatic and there are no diagnostic procedures to identify resistant and asymptomatic cases, the diagnosis based on syndromic management or microscopic identification of the parasite [34] hinders the correct management of the infected population. Therefore, the implementation of techniques with high sensitivity and specificity for use in routine and universal screening would reduce the incidence of this STI and therefore, the risk associated with the acquisition of other pathologies, contributing significantly to this serious health problem.
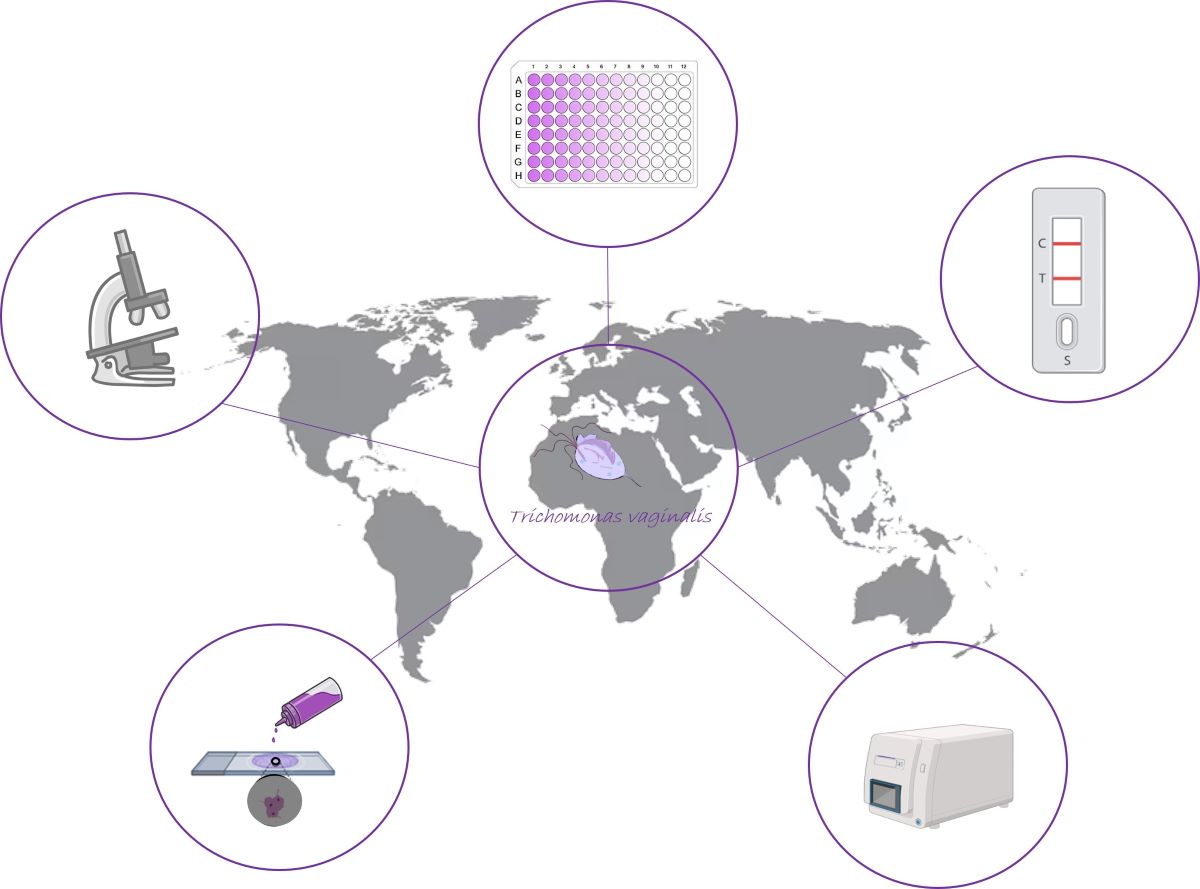
In this review, we describe the different diagnostic techniques that has been used for the identification of T. vaginalis in female and male population. In particular, we focus on the classical methods, based on microscopic identification such as wet mount and culture, as they have been the gold-standard. Then, we revise the immunological and molecular techniques that have been recently developed. We bravely discuss the information exposed with the aim of giving a general overview of what is happening in the diagnosis of this neglected STI.
2. Diagnosis based on clinical signs and symptoms
Because specific treatment for trichomoniasis is available, the identification of infected people, including asymptomatic, is mandatory to prevent the sexual transmission of the organism [35]. Clinicians manage symptomatic women who present different and unspecific symptoms [10,11] including combination of vaginal discharge, vulvar irritation, and odor. This irritation is more prominent in trichomoniasis than in bacterial vaginosis [36].
Physical examination of patients usually shows an erythematous vulva in less than one-third of infected women. On speculum examination, excessive discharge is noted in 50% to 75% of patients [36]. A yellowish-green frothy discharge suggests trichomoniasis [37,38], however, this characteristic frothy discharge is only seen in a minority of patients. Moreover, bubbles are present in only 8% to 50% of infected women, and their presence is non-specific [38]. The clinical presentation, observed in 20% to 75% of cases, includes pruritus, dysuria, dyspareunia [37,39] and vaginal wall erythema, occasionally with edema. Punctate hemorrhages lesions are detected on the vaginal walls or the exocervix (strawberry cervix) in about 2% of women during routine physical examination [37], but these characteristic hemorrhages can be visualized in 45% of patients by colposcopy [36].
After completing the physical examination, it is useful to determine the pH of vaginal secretions. This is conveniently accomplished by inserting a strip of indicator paper into the vaginal discharge pooled in the lower lip of the speculum. Normal vaginal pH of 4.7 or less, is maintained in most patients with vulvovaginal candidiasis. Vaginal pH is elevated above 4.7 in most women with trichomoniasis [40], but elevated pH is also found in women with bacterial vaginosis, becoming a nonspecific sign. Moreover, the vaginal pH may be artifactually elevated if the sample is contaminated with cervical discharge or semen. After the pH has been determined, the Whiff test may be performed. Briefly, several drops of 10% to 20% potassium hydroxide should be added to the discharge in the speculum. The clinician then seeks the production of a pungent, fishy, amine-like odor. The positive result of the whiff test is manifested by 75% of women with trichomoniasis, but also by most women with bacterial vaginosis [40]; while it is not positive in vulvovaginal candidiasis [36]. Because clinical manifestations are not reliable parameters, and asymptomatic infection is common, demonstration of the organism with appropriate laboratory methods is required to confirm T. vaginalis infection [5,36,41,42,43].
2.1. Specimens required for T. vaginalis detection in secretions.
In women, the sample is usually collected from the posterior fornix by cotton wool-tipped applicator sticks or polyester sponges [44,45]. Cervicovaginal material for Papanicolaou staining is best obtained using an Ayre’s spatula, with the slide immediately immersed in a suitable cytologic fixative [35].
In men, T. vaginalis infection is difficult to detect. Because organisms are more likely to be found in semen than in urine or urethral exudates, a fresh sample obtained by masturbation into a clean sterile container should be examined [35]. Likewise, urethral material taken with a polyester sponge [46], or a urine sample, taken preferably after the patient has retained urine overnight, can be also examined.
3. Classical diagnostic procedures: Microscopy
Diagnosis of trichomoniasis has traditionally consisted of taking a specimen from the patient and examine it immediately under the microscope [48], to identify the characteristic morphology and motility of the trophozoite from vaginal or cervical samples in females and urethral or prostatic secretions in males [49]. Currently, wet mount microscopy is the most rapid and widely used method for diagnosing trichomoniasis in resource-constrained settings [50]. This method can have a specificity of 100%, nevertheless, it must be carried out quickly enough and at a temperature that does not impair the viability of the trophozoite. It is important to note that sensitivity values may decrease depending on the time elapsed from sample collection to microscopic examination [41]. Furthermore, it is a subjective test that requires experience and even in the hands of trained observers, presents a range of sensitivity between 35 - 80% compared to culture [51,52,53]. This lack of sensitivity contributes to the under diagnosis of the disease. Also, since viable organisms are required, a delay in the transport of sample reduces motility of the organism and, consequently, diagnostic sensitivity [54]. Although this method is certainly the most cost-effective diagnostic test, it is far from optimal, in terms of reliability and sensitivity [52,53].
Ideally, the saline wet mount preparations should be examined from the swab collected by the clinician, as well as inoculation of the samples immediately after collection in an appropriate culture medium [35,54]. Many physicians, however, work at considerable distances from the diagnostic laboratory and, since the protozoan is susceptible to dehydration and changes in redox potential, specimens should be sent in a suitable transport medium. Stuart’s transport medium [55,56] or Amies’ modification [57] present remarkable utility. During the first 24 hours, trichomonads survive well in Stuart’s medium, but there is a significant decline in the recovery rate of the organisms beyond this time [58]. The use of transport media leads to dilution of the number of organisms in the original sample and this should be considered if negative results are obtained by culture or microscopy. Delays as short as 10-30 min between specimen collection and microscopic examination can dramatically reduce the sensitivity of the test [59]. In addition, suboptimal specimen storage or transportation conditions, especially temperatures below 22 °C, further reduce parasite motility and thus wet mount sensitivity [41]. This can be overcome by using staining techniques in adjunct to wet mount microscopy [48].
3.1. Wet smears
Although direct microscopy of prostatic fluid or the deposit from centrifuged urine is useful, the density of polymorphonuclear leukocytes and epithelial cells in vaginal exudate tends to hinder the trichomonads identification and particularly the movement of the flagella. Microscopy of exudate diluted with isotonic saline is preferable. This remains the only widely accepted routine procedure for making an on-the-spot diagnosis of vaginal trichomoniasis. As noted above, the sensitivity of wet smear using transmitted light, phase contrast, and dark-field microscopy can vary widely, from as low as 35% to almost 85% compared to culture [51,52,53,60,61]. This variation may be due to the use of different culture media and the number of organisms in the samples tested. Because of the marked variability that can exist in the number of organisms per unit of volume in a vaginal exudate from patient to patient, prolonged time under the microscope may be necessary when few trichomonads are present. Feinberg and Whittington found that the results obtained by microscopy of urethral material from men were superior to those obtained by culture [60]. Others, however, have identified more infected men when culture methods have been used [62].
3.2. Staining techniques
To improve the sensitivity of direct microscopy different stains have been developed. Stained smears have the advantage that there can be a considerable delay between staining and examination of the sample, without loss of reliability in diagnosis, provided by de adequately fixation [48]. Various stains commonly used are Papanicolaou, Giemsa and other Romanowsky dyes [63,64,65]. Besides these, several staining techniques using acridine orange, Leishman, periodic acid-Schiff, and Fontana-Masson staining methods have been used to improve the sensitivity of direct microscopy [66,67,68,69]. Undoubtedly, the Giemsa stain is the most readily available in a laboratory and the results, even in poorly prepared smear, justify its application. Certain features, such as spindle shaped nucleus, the contours of the organism, and the cytoplasmic inclusions, allow easy identification of the organism. Although trichomonads are not stained by safranin, malachite green, methylene blue, and brilliant cresyl blue, other cellular material takes up the dye and the organisms stand out against this colored background [70,71,72]. However, these staining methods has not been shown convincingly to improve the detection rate of trichomonads in secretions and is not recommended for the routine clinical laboratory. Vital staining of T. vaginalis can be accomplished by addition of fluorescein to the saline mount preparation, in dark field illumination these organisms appear emerald green [73].
Fixed smears of vaginal exudate stained with Giemsa’s stain have been used for more than 100 years in the diagnosis of trichomoniasis [74]. In carefully prepared smears, the trichomonads nucleus is stained purplish red and the cytoplasm is light red, pink or bright blue, depending on pH; with a darker-staining small eccentric nucleus that may be elongated, fusiform, or oval. The axostyle and flagella may be seen [75]. Overall, more infections are identified by microscopic examination of Giemsa-stained smears than by wet smear microscopy [76,77,78], and in some studies, the sensitivity of this diagnostic method has approached that of culture [67,76,79].
In carefully taken and well-fixed Papanicolaou-stained smears (Pap smears) of cervicovaginal material,
T. vaginalis appears as an ovoid structure varying in size from 10 to 30 μm. The cytoplasm is gray-green which contains minute eosinophilic granules and the eccentric nucleus stains blue. There are conflicting data on the efficacy of Pap smear microscopy in the diagnosis of vaginal trichomoniasis, as the sensitivity and specificity of this technique vary depending on the experience of the microscopist [71,80]. Commonly used in cytological studies, the staining of the specimens with liquid Papanicolaou stains can present a sensitivity between 60-96% and a specificity of 98-100%, as shows
Table 1 [41].
Other authors have suggested the acridine orange staining method. This method is a nonspecific nucleic acid staining procedure which can be applied for fluorescence-based detection of T. vaginalis [81]. Acridine orange staining was found to be the best microscopic method when compared with wet mount examination and Giemsa staining. Hence, it should be used in routine diagnosis of T. vaginalis infection in places where fluorescent microscopic facility is available [48].
Although wet mount examination is the most used test in routine diagnosis of T. vaginalis infection, staining techniques should be used as an additional diagnostic test to identify cases missed either due to unavailability of immediate microscopic facility or delay in the transport of samples to the laboratory for culture [48]. The traditional diagnostic methodology is easy realization; however, these techniques have the disadvantage of not being very sensitive.
3.3. Culture
The liquid or broth culture method has been considered the gold standard for the direct diagnosis of trichomoniasis because it is simple and requires as few as 300 to 500 trichomonads/mL of inoculum to initiate its growth in culture [82]. There are various media for cultivation of T. vaginalis, such as Kupferberg, Kupferberg STS, Hirsch, Trichosel, Modified Diamond, Lash serum, or the most recent, called InPouch® TV [83,84,85]. However, the most common are Diamond (TYM), modified Diamond or Roiron® [41]. Diamond’s medium must be stored at 4 °C prior to use, warmed to room temperature before inoculation. Specimens from women (vaginal swabs) or men (urethral swabs or urine sediment) should be immediately inoculated in the culture medium at least 1 h after collection. Then, cultures should be incubated at 37 °C under preferably anaerobic conditions and examined microscopically each day for up to 5 days until motile trichomonads are observed [41]. Cultures from women with trichomoniasis are usually positive within the first 3 days after inoculation. However, cultures from men should be examined daily for 5 days or longer before being considered negative. Extended incubation times are often required in male samples to permit the growth of a detectable numbers of organisms [6].
Thus, this methodology is simple and inexpensive, but requires the direct microscopic examination during a period between 2 to 7 days [46]; during this time infected patients may continue to transmit the infection [86]. Moreover, there are inherent limitations to culture diagnosis e.g. culture contamination with vaginal microbiota (bacteria or yeasts) can be very frequent [87,88]. Nevertheless, sensitivity rates can rise to 81-94% depending on the sample and the medium used (
Table 1).
To improve the acceptability of the diagnosis by culture, a good procedure is the so-called delayed inoculation, a method that combines both techniques: first, the fresh sample for direct examination and, if negative, its incubation in the culture medium, observing it for 2-5 days [89]. InPouch® TV is a self-contained system, which permits both immediate examination and culture in a single device of vaginal, urethral and urine samples. The results are comparable to wet smears and culture techniques [90,91]. The transparent oxygen-resistant plastic can be examined directly under the microscope, eliminating the need to remove material from the culture for daily examination. InPouch® TV can be stored at room temperature before use, and inoculated pouches can remain at room temperature up to 48 h before incubation at 37 °C [41]. This device can be used with. Levi and collaborators showed that the InPouch® TV system was at least as sensitive as Diamond’s modified medium for the detection of T. vaginalis [92]. Borchardt and collaborators showed that this system was significantly more sensitive than either Diamond’s modified medium or Trichosel medium [93]. However, the InPouch® TV continues being a procedure that requires observing the sample during for quite a few days, not being a rapid diagnostic method [41,46].
Therefore, it has been necessary to develop and implement more rapid, sensitive, and specific tests, that allow early diagnosis in risk population and even the identification of asymptomatic cases. These new methods, some of them point-of-care (POC) techniques, are currently being implemented in many diagnostic services [91].
Table 1.
Relevant characteristics of the techniques used in the direct diagnosis of T. vaginalis.
Table 1.
Relevant characteristics of the techniques used in the direct diagnosis of T. vaginalis.
| Type of diagnosis |
Test |
Sensitivity (Se)
Specificity (Sp) |
Advantages |
Disadvantages |
Ref. |
| Microscopy |
Wet smears |
Se: 35-85%
Sp: 100%
|
Fast, simple, and
inexpensive
|
Sensitivity depends on the skills of the microscopist
Not applicable to male specimens |
[51,52,53,60,61] |
| Staining |
Giemsa
Acridine orange
Papanicolaou
|
Se: 80%
Sp: 99.4%
Se: 100%
Sp: 100%
Se: 60-95%
Sp: 98-100% |
Fast, simple, and
Inexpensive. Improved sensitivity vs. wet smears
Stain used in Pap smears. Fast, simple, and
Inexpensive |
Staining specialists required to improve sensitivity
|
[67,76,79]
[48]
[41] |
| Culture |
Diamond medium
InPouch®
|
Se: 56-95,8%
Sp: 100%
Se: 92%
Sp: 98%
|
Improved sensitivity vs. wet smears
Less handling, simple, easy to transport |
Requires equipment and laboratory specialist. Long incubation period. Risk of pathogen contamination and false negatives |
[41,90,91]
[92,93] |
4. Immunodiagnosis
4.1. Latex agglutination techniques
One of the techniques used for the serodiagnosis of trichomoniasis is latex agglutination. Among the different commercial tests available for the detection of T. vaginalis, Kalon TV latex® agglutination test stands out. The kit includes a suspension containing latex particles sensitized with rabbit anti-T. vaginalis [94], which must be brought into contact with a drop of diluted sample of vaginal exudate from the patient [95]. If the sample is positive and contains T. vaginalis antigens, an agglutination reaction will occur between the commercial antibody and the antigen present in the patient (immunocomplex), directly detectable and visualized in form of aggregates [95]. Besides, some laboratories have developed agglutination kits that identify simultaneously other microorganisms that cause infections vaginal infections, such as Candida spp. [96,97]. These tests use two different sera, one sensitized with anti-T. vaginalis antibodies, and another with anti-Candida spp. [97]. Latex agglutination methods offer a better sensitivity than fresh examination and comparable to culture, this being 98.8% [98], reaching up to 100% in more recent studies, becoming a technique with a quite acceptable cost-effectiveness ratio (
Table 2) [95]. Therefore, agglutination tests present quite a few advantages, it takes less than three minutes to offer results, is very simple to carry out and does not require a microscope or any special equipment, nor personnel specialized. Its specificity is comparable to that of cultivation, with the difference that agglutination test gives a result in the same day [98]. However, in those symptomatic patients with a negative agglutination result, a different diagnostic method must be performed, with the aim of (i) avoiding overlooking possible infections due to T. vaginalis in case of a false negative result and (ii) confirm true positives [95,98]. This is due to its low positive predictive value, being only 60% [95]. Fits mention that these tests cannot be used for diagnosis in men, because they can only be performed with vaginal exudate samples [95,98].
4.2. ELISA
The indirect ELISA (enzyme-linked immuno-sorbent technique assay) is a serodiagnostic test that detects specific antibodies revealing the exposure of the patient to the parasite. This test uses immobilized T. vaginalis antigens in a multi-well microplate of polystyrene, which are specifically recognized by host antibodies [99]. The formation of the immune complex is revealed with a second antibody labeled with an enzyme, called conjugate. This conjugate is usually goat anti-human IgG [100] and is usually found labeled with peroxidase or alkaline phosphatase. Then, when the chromogenic substrate is added, an enzymatic reaction takes place and produces color. The recorded absorbance is directly proportional to the amount of antibody present in the sample [99], thus allowing serum titer determination. To avoid cross-reactions and false positives, the epitopes recognized by the patient’s antibodies must be specific to T. vaginalis and not present homology with those of other microorganisms, nor with the host’s own cells [101,102]. In relation to the antigens of T. vaginalis, the following stand out for their immunogenicity: α-actinin, α-enolase, aldolase, and glyceraldehyde-3-phosphate dehydrogenase [102].
With the aim of designing an ELISA test with the best sensitivity and specificity, some researchers have explored the possibility of obtaining synthetic recombinant peptides, which contain a more than one epitope, so that they are recognized by a greater number of specific antibodies different from the host [102]. Over time, these recombinant chimeric proteins have been improved, with the aim of including additional epitopes and eliminating those that share certain homology with proteins from other organisms, thus increasing the sensitivity of this technique for screening patient sera [102,103,104]. The synthesis of recombinant chimeric proteins using bacterial plasmids is much more advantageous and efficient than using whole cells or cell lysates to avoid cross-reactions of common epitopes [102]. However, when recombinant antigen technology is not available, it is common to use a lysate of different strains of the parasite to perform the indirect ELISA and quantify the seropositivity of patients. Some studies carried out on male samples, have shown sensitivity and specificity values of 71.2% and 96.3%, respectively [100]. Serum is the most suitable sample for the detection of anti- T. vaginalis antibodies, since IgG are found in a higher percentage in serum than in vaginal exudate, while IgM are not even detected in some studies [105]. Moreover, the use of serum makes this methodology suitable for the diagnosis of trichomoniasis in both sexes [103]. However, if the aim is to detect IgA antibodies, the predominant isotype in seromucous secretions, vaginal and endocervical exudate are more appropriate samples [106].
Although the indirect ELISA is one of the most specific and can detect active infection, as well as past exposure to it, this methodology is only capable of detecting relative recent past infection, as antibody levels have become undetectable around 6-12 months after infection [102]. Nevertheless, it is a sophisticated technique that requires specialized personnel, as well as special laboratory equipment that may not be available in some areas.
On the other hand, the sandwich ELISA technique uses specific capture antibodies immobilized on the microtiter plate for the detection of
T. vaginalis antigens [99,107]. Recent studies have confirmed that this type of ELISA has a sensitivity of 88.9% and a specificity of 97.1% in the detection of
T. vaginalis antigen when compared with culture as the reference method [108]. These values have already been defined in previous studies, using monoclonal antibodies for the detection of parasitic surface antigens present in vaginal exudate samples [109]. However, beyond these excellent data, this method has a false positive rate of 2.9% as shows
Table 2. This could be due to the detection of non-viable trophozoites, something that occurs less frequently in culture, which is based on the identification of organisms viable with motility [108].
4.3. Inmunofluorescence
Immunofluorescence techniques are not routinely used for diagnosis. In recent years, direct immunofluorescence (DIF) has been used for research purposes using fluorophore-labeled monoclonal antibodies as a conjugated to detect T. vaginalis antigens [110]. DIF is commonly used for the study of morphological and metabolic characteristics of the parasite [110,111]. Likewise, the application of this technique has allowed to evaluate the presence of T. vaginalis virus (TVV) harbored by the trophozoite, using the monoclonal antibody C20A3 directed towards the P270 protein [56]. This molecule undergoes a phenotypic change, being expressed on the surface of the parasite when TVV is present [112].
Nevertheless, researcher have used acridine orange for the identification of T. vaginalis in female samples, reaching sensitivity values of 73.5% to 96% [113]. It should be noted that this sensitivity is achieved when the vaginal exudates come from women infected only with this parasite, while if patients with other STI co-infections, this value decreases to 67% [114].
The use of immunofluorescence techniques for the diagnosis of
T. vaginalis can offer certain advantages, being a very specific and accurate test, providing easy interpretation of the results. However, it is quite sophisticated and requires a fluorescence microscope, as well as trained personnel for its management (
Table 2). Some authors consider that it could be a useful technique for confirmation of negative results after direct microscopic examination of the sample or culture, for example [115].
4.4. Immunochromatography
As mentioned above, POC tests are being implemented to improve syndromic management and classical techniques to facilitate prompt diagnosis and treatment. These tests offer results in minutes and are easier to perform [116]. They do not need sophisticated equipment and since they are simple procedures, it can be performed with minimal training [117]. The most used POC tests are immunochromatography type, rapid molecular assays or based on agglutination reactions [116]. This is the case of the OSOM®
Trichomonas test, a lateral flow immunoassay capable of detecting an adhesin of
T. vaginalis by using monoclonal antibodies immobilized on the nitrocellulose membrane [118]. This test also uses another antibody conjugated with colored particles blue, so when the immune complex is formed, a line of this color shows a positive result. As in many immunochromatographic test, the control line, which should always appear, is colored red in this test [119]. OSOM®
Trichomonas test exhibits a sensitivity between 83-90%, comparable to NAAT (nucleic acid amplification test), and a specificity in vaginal exudate samples > 98.8% (
Table 2). Furthermore, this test can be also performed by the patient at home [34].
Alderete and Chan (2023) have recently developed a POC using the MedMira Rapid Vertical Flow (RVF ) Technology. The antigen used is a 72.4-kDa truncated version of -actinin called ACT::SOE3 that can be detected by specific antibodies present in human sera. This immunochromatographic device stands out because it can be used in both men and women with trichomoniasis [120].
5. Molecular diagnosis
Different commercial and “in house” PCR-based assays to detect T. vaginalis nucleic acids have been implemented in the last years. PCR techniques provide a remarkable higher sensitivity than microscopic methods, however, trained staff, equipment and cost reagents are the main drawbacks associated with main of these techniques [91]. Prior to the development of nucleic acid amplification test (NAAT), wet mount and culture methods were the gold standard for trichomoniasis diagnosis, however, in the last decades, molecular techniques have become the most appropriate techniques for the diagnosis of this infection when is possible [121].
There are a dozen FDA-approved assays for the detection of
T. vaginalis by NAAT. Some of them also comply with European Standards as reflects
Table 3 [121,122]. These tests can detect DNA or RNA of the parasite in symptomatic and asymptomatic patients, with a high range of sensitivity and specificity, depending on the assay.
All the mentioned tests identify specimens in clinician-collected vaginal swabs. However, the differences between the following techniques are mainly based on the method used for the identification of nucleic acids, the possibility of detecting more than one urogenital pathogen and the type of sample that can be analyzed (
Table 4). For example, the Xpert® TV assay (Cepheid, Sunnyvale, CA) stands out because it can be used in self-collected vaginal swabs, as well as female and male urine [123]. This system includes a kit designed to collect, preserved and transport
C. trachomatis, N. gonorrhoeae and
T. vaginalis specimens that can be analyzed posteriorly in two different assays using the same real time PCR (RT-PCR) platform: Xpert® CT/NG and TV Assays. The studies of microbial interference using a panel of 124 microorganisms revealed no cross-reaction apart from
Trichomonas tenax when concentration was higher than 200 cell/mL [122]. The Aptima®
T. vaginalis Assay (Hologic, Bedford, MA) identifies a specific region of the small ribosomal subunit in female endocervical and vaginal samples, which are collected in tubes with transport media (PreservCyt®) that releases and protects RNA during storage. Then, the rRNA is capture by specific oligomers associated to magnetic particles and posteriorly the amplification is performed by transcription mediated amplification (TMA). The Aptima® system is already used to discriminates between
T. vaginalis, C. glabrata and
Candida spp. (i.e.
C. albicans, C. dubliniensis, C. parapsilosis, C. tropicalis) as well as
Chlamydia trachomatis and
Neisseria gonorrhoeae using the same Panther® platform [122]. All the devices developed by Hologic are based on the identification of specific rRNA targets of the different pathogens mentioned. Curiously, BD Affirm
TM VPIII (Becton Dickinson &Co.) also detects rRNA from three urogenital pathogens: the protozoan
T. vaginalis, the bacteria
Gardnerella vaginalis and the yeast
Candida spp. (including
C. albicans,
C. glabrata,
C. kefyr,
C. krusei,
C. parapsilosis, and
C. tropicalis). Female samples should be collected and transported at room temperature or refrigerated (2-8 °C) using a specific collection swab and a transport system provided by the company which conserves the samples up to 72 h [135]. The comparing studies between Xpert® Tv assay and Aptima® system with endocervical swabs, patient-collected vaginal swabs and urine samples have demonstrated similar sensitivity and specificity values, slightly higher than those detected with the InPouch system [123]. While the comparison performed by Andrea and Chapin (2011) of the two rRNA assays (Aptima® and Affirm VPIII) for the detection of
T. vaginalis in 41 positive and 740 negative samples indicated that the Aptima® system was significantly more sensitive (41/41) than the Affirm
TM VPIII device (26/41) [127]. Roche has also developed a NAAT device to identify
T. vaginalis and
M. genitalium by targeting multicopy regions of rRNA from the parasite by RT-PCR. The Cobas
® TV/MG highlights for the large number of samples that can be used for the diagnosis of these two urogenital pathogens, including self-collected vaginal swabs, endocervical samples, liquid-based cytology specimens in PreservCyt solution and urine from both male and female patients. As occurs with other NAAT systems, for the correct transport and DNA processing, the swab and urine samples must be taken using a Sample Kit provided by the laboratory [131]. Other two cleared tests that can detect
T. vaginalis in the same type of samples as indicated for Cobas
® are BD CTGCTV2 (Becton Dickinson & Co.) and Alinity m STI Assay (Abbott). Both systems detect simultaneously
C. trachomatis, N. gonorrhoeae and
T. vaginalis [122,136]. Moreover, both includes and automated DNA extraction prior to the quantitative real-time PCR all in the same benchtop instrument [128]. The only difference is that Alinity also identifies rRNA from
Mycoplasma genitalium [120]. BD Diagnostics has developed another NAAT system for the detection of
T. vaginalis in self and clinician-collected vaginal swabs, endocervical swabs and female urine samples. The BD ProbeTec Q
x Assay needs a prewarming step prior to process the sample onto the Viper System which automatically performs the extraction and amplification steps based on the strand displacement amplification (SDA) technique. The DNA target used for the diagnosis of
T. vaginalis on female patients is the gene that encodes the parasitic adhesion protein AP65 [121,125]. This platform can be used for the detection of other STI pathogens such as
N. gonorrhoeae or
C. trachomatis [125].
Although Solana® Trichomonas assay identifies only T. vaginalis in samples, it should be highlighted that has been developed as a Point-of-Care (POC) test for qualitative detection of T. vaginalis using isothermal Helicase-Dependent Amplification (HDA) for the detection of a multi-copy DNA fragment of the parasite in the sample [132]. In this sense, another POC using HDA technology has been developed by Quidel Corporation: the AmpliVueTM Trichomonas Assay. The main difference between both systems are the samples that can be used and the automatization of the detection technique. For the former, clinician-collected vaginal swabs and female urine samples can be employed. The method consists in two steps: first, the sample is included in a lysis tube and heat-treated at 95 ºC. Then, an aliquot is added to the reaction tube which contains the HDA reagents for the automated detection of the T. vaginalis DNA target in the Solana instrument [132]. No cross-reaction with 47 different microorganisms including bacteria, virus, and protozoa, neither interference has been detected [122]. While for the latter, only clinician-collected vaginal swabs can be used. The management of the sample by heat treatment and the isothermal DNA amplification is performed as mentioned above, however, the identification of the parasitic DNA target is effectuated in a cassette after the HDA reaction. In other words, the AmpliVueTM test needs a third step with includes a vertical-flow strip for the colorimetric detection of the parasitic DNA. Both POC methods have presented similar sensitivity and specificity as other NAAT assays such as Aptima® [34,133]. The last POC system based on NAAT, is the Visby Medical Sexual Health Test, a compact device that can detect C. trachomatis, N. gonorrhoeae and T. vaginalis ins self-collected female vaginal swabs using a specific collection kit in 30-50 minutes [122,134].
The development of detection systems that includes (i) the automatization of DNA extraction, (ii) the identification of more than one pathogen in the same sample or (iii) the ability to process self-collected samples, endocervical swabs or/and male urine samples can significantly improve the sensitivity and specificity of classical diagnostic methods becoming much more useful techniques for the diagnosis of STIs [2]. However, the increased cost of these techniques for the diagnosis of
T. vaginalis, which continues receiving the less attention [13], could explain why their implementation is reduced. Fortunately, the development of diagnostic assays that can be implemented in the systems used for the detection of other STIs have become an interesting tool for laboratories like Abbott, Roche, Hologic/Gen-Probe, BD or Cepheid to invest in the development of NAAT tests to identify
T. vaginalis (
Table 3 and
Table 4).
In addition to the cleared systems mentioned above, different RT-PCR assays for the simultaneously detection of more the one STI pathogen (including T. vaginalis) have also been published. Recently, different research groups have designed an in-house multiplex RT-PCR for the diagnosis of up to nine pathogens (C. trachomatis, N. gonorrhoeae, T. vaginalis, C. albicans, Mycoplasma hominis, M. genitalium, Ureaplasma urealyticum, U. parvum, Gardnerella vaginalis and human herpes viruses) with sensitivity and specificity values > 91% and an estimated cost per test of near $3 [139,140]. Also, different groups have developed loop-mediated isothermal amplification (LAMP) assays for detection of T. vaginalis. This methodology presents a high sensitivity and specificity, it can be used with urine and genital samples, and can amplify DNA with only a heat block or water bath in less than 130 min. However, it is not free from contamination and can give false positives [141,142].
Moreover, other research groups are focusing on the development of novel systems based on the use of aptamers for the diagnosis of T. vaginalis in vaginal samples. This novel method targets the detection of the parasitic immunogenic protein AP65 and could become an interesting tool based on its potential used in microtiter plate and lateral flow assays [143].
4. Discussion
Sexually transmitted infection is a global public health challenge with an increasing trend in the last years (58.15% since 1990) [144]. Of the different pathogens that can be transmitted by sexual intercourse, T. vaginalis causes the most prevalent non-viral sexually transmitted infection worldwide, affecting mainly the most disadvantaged population in both developed and low-income countries [4,145,146]. Its prevalence is underestimated because it is not a notifiable disease. This is compounded by the lack of tests to diagnose asymptomatic patients, the limited sensitivity of some methods and the absence of pharmacovigilance systems to detect resistance phenomena. In this context, many researchers, and organisms as the CDC have classified trichomoniasis as a neglected disease [8,145,146,147].
The priority population groups for preventing STI infections have been changing in the last decades [121], due to the evolution observed in social/sexual behavior. This may explain why the age of first sexual intercourse has been reduced, as well as the perception of certain sexual behaviors as non-risky (i.e.: the use of condom), increasing exposure to STIs [147,148,149]. Thus, sexual education and the inclusion of the main STI pathogens in the gynecological revisions could be interesting tools for the reduction of these infections.
This review notes the recent development of novel diagnostic techniques with higher sensitivity and specificity than those based on microscopic identification (i.e. wet mount, Papanicolaou or Giemsa stain and culture). However, the highest prevalence rates of trichomoniasis are associated with low- and middle-income countries and regions [4], where the diagnostic protocols are frequently chosen based on their low cost and ease of use, in which no specialized equipment or personnel are required. Although wet amount diagnosis is easy and inexpensive, their main limitations are: (i) the microscopic visualization of the samples must be taken within 20 min of its collection, (ii) it presents a reduced sensitivity, (iii) it is only possible for vaginal swab samples and urine [93,124].
The association between trichomoniasis and the risk of acquiring other pathogens through sexual intercourse has been demonstrated [14,16,17,150]. In this context, T. vaginalis could be used as a marker of high-risk sexual behavior. Considering that more than 746 new cases of HIV could be imputable to T. vaginalis [151], the diagnosis and treatment of patients with trichomoniasis becomes an interesting public health strategy for the control of STIs. This proposal becomes even more important if we take into consideration that in relation to the economic burden, the total costs of non-viral STIs in the United States are being estimated in $0.4 billion, with an average lifetime medical costs per T. vaginalis infection in $5 for men and $36 for women [152,153].
In general, both guidelines from East European countries [154] and CDC [155] recommend the following procedures for T. vaginalis diagnosis: (i) diagnostic testing in all women with vaginal discharge, specially in high prevalence settings (STI clinics) and for asymptomatic population at high risk for infection (e.g. persons with multiple sex partners, prostitution, drug abuse or a history of STI) and (ii) employ NAATs if trichomonads are not detected on microscopic examination. According to the updated CDC STDs Treatment Guidelines, culture would no longer be considered as the gold standard for diagnosis of T. vaginalis infection if effective molecular detection methods are available [155].
It is mandatory to reinforce new diagnostic strategies that could diagnose simultaneously multiple STI pathogens with technologies that could be implemented in low-income regions. In this sense, the POC diagnosis seems the best way to cope with this necessity. Currently, four POC devices have been developed for T. vaginalis diagnosis: one based on the detection of a parasitic antigen protein and the other four in DNA detection. OSOM® Trichomonas test is a low complex dipstick that can be performed in less than 15 minutes without specific equipment. Solana® and AmpliVueTM are FDA approved as moderately complex POC assays which requires small platforms to develop the assay in less than 1 hour. Both require small heat blocks for the lytic and the isothermal amplification steps at 95 °C and 65 °C, respectively [122,132,133]. Although the GeneXpert assay is also cataloged as a moderately complex POC, stands out from the others because of the diversity of genitourinary samples that can be analyzed, including men urine specimens [34,132]. While the recent FDA-cleared Visby Medical Sexual Health Test is a simple compact device that can detect simultaneously N. gonorrhoeae, C. trachomatis and T. vaginalis in self-collected vaginal samples [122,134].
In addition, another disadvantage that must be overcome in many of the diagnostic techniques described is that many of them are not suitable for male samples. As men are mainly asymptomatic carriers, the recommendations, rutinary test and methods developed for these patients are scarce [138,156]. Wet mount of urine or urethral samples are inexpensive and easy to perform, however, the main limitation is its reduced sensitivity due to the limited time between sample collection and the observation in the microscope. The identification must be performed within 20 min before collection as not motile
T. vaginalis can be difficult to recognize by microscopy [124,157]. Fortunately, in the last years, some NAAT devices can identify
T. vaginalis in both male urine samples and meatal swabs, i.e.: GeneXpert assay, Cobas
® TV/MG, BD CTGCTV2 or Alinity m STI Assay. It is important to highlight that all these devices can identify other STI as shown in
Table 4. Thus, these detection systems together with POC are becoming the most powerful and useful tools to correctly identify this parasitosis in the population.
5. Conclusions
In conclusion, this article reviews the different diagnostic approaches to trichomoniasis in different circumstances. While in developed countries, nucleic acid amplification testing (NAAT) should displace direct examination of wet smears and culture, in middle and low-income regions, this is not possible due to the equipment required in some molecular techniques. In addition, skilled laboratory technicians are also required in many cases. These requirements constitute a serious challenge in low-income countries, due to the high economic cost of providing adequate facilities and training specialists. In these regions, the diagnosis of trichomoniasis relies on anamnesis, clinical diagnosis supported by physiological test (i.e. vaginal pH or Whiff’s test) and direct examination. Considering the importance of this STI as a marker of high-risk sexual activity, the implementation of affordable and easy-to-use POC techniques (i.e. OSOM® Trichomonas test, GeneXpert, Visby Medical Sexual Health Test or LAMP techniques among others) opens the door for the future management of this neglected STI.
Author Contributions
Conceptualization, A.I-E.; investigation, A.I-E. and J.J.N-R.; data curation, A.I-E. and J.J.N-R.; writing-original draft preparation, A.I-E. and J.J.N-R.; supervision: A.I-E. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- World Health Organization. Sexually transmitted infections (STIs). Available online: https://www.who.int/news-room/fact-sheets/detail/sexually-transmitted-infections-(stis) (accessed on 19 June 2023).
- World Health Organization. Global health sector strategies on, respectively, HIV, viral hepatitis and sexually transmitted infections for the period 2022-2030. Available online: https://www.who.int/publications/i/item/9789240053779 (accessed on 27 September 2023).
- Van Gerwen, O.T.; Muzny, C.A.; Marrazzo, J.M. Sexually transmitted infections and female reproductive health. Nat. Microbiol. 2022, 7, 1116–1126. [Google Scholar] [CrossRef] [PubMed]
- Rowley, J.; Vander Hoorn, S.; Korenromp, E.; Low, N.; Unemo, M.; Abu-Raddad, L.J.; Chico, R.M.; Smolak, A.; Newman, L.; Gottlieb, S.; Thwin, S.S.; Broutet, N.; Taylor, M.M. Chlamydia, gonorrhoea, trichomoniasis and syphilis: global prevalence and incidence estimates, 2016. Bull. World Health Organ. 2019, 97, 548–562P. [Google Scholar] [CrossRef] [PubMed]
- Seña, A.C.; Miller, W.C.; Hobbs, M.M.; Schwebke, J.R.; Leone, P.A.; Swygard, H.; Atashili, J.; Cohen, M.S. Trichomonas vaginalis infection in male sexual partners: implications for diagnosis, treatment, and prevention. Clin. Infect. Dis. 2007, 44, 13–22. [Google Scholar] [CrossRef] [PubMed]
- Meites, E. Trichomoniasis: The “Neglected” Sexually Transmitted Disease. Infect. Dis. Clin. North. Am. 2013, 27, 755–764. [Google Scholar] [CrossRef] [PubMed]
- Hoots, B.E.; Peterman, T.A.; Torrone, E.A.; Weinstock, H.; Meites, E.; Bolan, G.A. A Trich-y question: should Trichomonas vaginalis infection be reportable? Sex. Transm. Dis. 2013, 40, 113–116. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. Parasites – parasitic infections in the United States. Available online: https://www.cdc.gov/parasites/npi/index.html (accessed on 20 July 2023).
- Mielczarek, E.; Blaszkowska, J. Trichomonas vaginalis: pathogenicity and potential role in human reproductive failure. Infect. 2016, 44, 447–458. [Google Scholar] [CrossRef]
- Lewis, D. Trichomoniasis. Medicine. 2014, 43, 369–371. [Google Scholar] [CrossRef]
- Muzny, C.A.; Schwebke, J.R. The clinical spectrum of Trichomonas vaginalis infection and challenges to management. Sex. Transm. Infect. 2013, 89, 423–425. [Google Scholar] [CrossRef]
- Poole, D.N.; McClelland, R.S. Global epidemiology of Trichomonas vaginalis. Sex. Transm. Infect. 2013, 89, 418–422. [Google Scholar] [CrossRef]
- Van Der Pol, B. Trichomonas vaginalis infection: the most prevalent nonviral sexually transmitted infection receives the least public health attention. Clin. Infect. Dis. 2007, 44, 23–25. [Google Scholar] [CrossRef]
- Masha, S.C.; Cools, P.; Sanders, E.J.; Vaneechoutte, M.; Crucitti, T. Trichomonas vaginalis and HIV infection acquisition: a systematic review and meta-analysis. Sex. Transm. Infect. 2019, 95, 36–42. [Google Scholar] [CrossRef]
- Kissinger, P.; Adamski, A. Trichomoniasis and HIV interactions: a review. Sex. Transm. Infect. 2013, 89, 426–433. [Google Scholar] [CrossRef] [PubMed]
- Allsworth, J.E.; Ratner, J.A.; Peipert, J.F. Trichomoniasis and other sexually transmitted infections: results from the 2001-2004 national health and nutrition examination surveys. Sex. Transm. Dis. 2009, 36, 738–744. [Google Scholar] [CrossRef] [PubMed]
- Noël, J.C.; Fayt, I.; Romero Munoz, M.R.; Simon, P. ; Engohan-Aloghe, High prevalence of high-risk human papillomavirus infection among women with Trichomonas vaginalis infection on monolayer cytology. Arch. Gynecol. Obstet. 2010, 282, 503–505. [Google Scholar] [CrossRef]
- Cotch, M.F.; Pastorek, J.G.; Nugent, R.P.; Hillier, S.L.; Gibbs, R.S.; Martin, D.H.; Eschenbach, D.A.; Edelman, R.; Carey, C.; Regan, J.A.; Krohn, M.A.; Klebanoff, M.A.; Rao, A.V.; Rhoads, G.G. Trichomonas vaginalis associated with low birth weight and preterm delivery. The vaginal infections and prematurity study group. Sex. Transm. Dis. 1997, 24, 353–360. [Google Scholar] [CrossRef]
- Viikki, M.; Pukkala, E.; Nieminen, P.; Hakama, M. Gynecological infections as risk determinants of subsequent cervical neoplasia. Acta Oncol 2000, 39, 71–75. [Google Scholar] [CrossRef]
- Hammar, B.; Teutsch, B.; Hoffmann, E.; Hegyi, P.; Váradi, A.; Nyirády, P.; Hunka, Z.; Ács, N.; Lintner, B.; Harmánné, R.J.; Melczer, Z. Trichomonas vaginalis infection is associated with increased risk of cervical carcinogenesis: A systematic review and meta-analysis of 470 000 patients. Int. J. Gynecol. Obstet. 2023, 0, 1–13. [Google Scholar] [CrossRef]
- Fazlollahpour-Naghibi, A.; Bagheri, K.; Almukhtar, M.; Taha, S.R.; Zadeh, M.S.; Moghadam, K.B.; Tadi, M.J.; Rouholamin, S.; Razavi, M.; Sepidarkish, M.; Rostami, A. Trichomonas vaginalis infection and risk of cervical neoplasia: A systematic review and meta-analysis. Plos one, 2023, 18, e0288443. [Google Scholar] [CrossRef] [PubMed]
- Hann, I.-H.; Kim, J.-H.; Ryu, J.-S. Inflammatory response to Trichomonas vaginalis in the pathogenesis of prostatitis and benign prostatic hyperplasia. Parasit. Host. Dis. 2023, 61, 2–14. [Google Scholar] [CrossRef] [PubMed]
- Marous, M.; Huang, W.Y.; Rabkin, C.S.; Hayes, R.B.; Alderete, J.F.; Rosner, B.; Grubb, R.L.; Winter, A.C.; Sutcliffe, S. Trichomonas vaginalis infection and risk of prostate cancer: associations by disease aggressiveness and race/ethnicity in the PLCO Trial. Cancer Causes Control, 2017, 28, 889–898. [Google Scholar] [CrossRef] [PubMed]
- Nagata, M.; Tome, A.; White, K.; Wilkens, L.R.; Park, S.-Y.; Marchand, L.L.; Haiman, C.; Hernandez, B.Y. No association of Trichomonas vaginalis seropositivity with advanced prostate cancer risk in the multiethnic cohort: a nested case-control study. Cancers 2023, 15, 5194. [Google Scholar] [CrossRef]
- Rodin, P.; King, A.J.; Nicol, C.S.; Barrow, J. Flagyl in the treatment of trichomoniasis. Brit. J. Vener. Dis. 1960, 36, 147–151. [Google Scholar] [CrossRef]
- Fung, H.B.; Doan, T.-L. Tinidazole: A nitroimidazole antiprotozoal agent. Clin. Therapeut. 2005; 27, 1859–1884. [Google Scholar] [CrossRef]
- Sherrard, J.; Wilson, J.; Donders, G.; Mendling, W.; Jensen, J.S. 2018 European (IUSTI/WHO) International Union against sexually transmitted infections (IUSTI) World Health Organization (WHO) guideline on the management of vaginal discharge. Int. J. STD AIDS. 2018, 29, 1258–1272. [Google Scholar] [CrossRef] [PubMed]
- Kissinger, P.J.; Gaydos, C.A.; Seña, A.C.; McClelland, R.C.; Soper, D.; Secor, W.E.; Legendre, D.; Workowski, K.A.; Muzny, C.A. Diagnosis and management of Trichomonas vaginalis: Summary of evidence reviewed for the 2021 Centers for Disease Control and Prevention Sexually Transmitted Infections treatment guidelines. Clin. Infect. Dis. 2022, 74, S152–S161. [Google Scholar] [CrossRef] [PubMed]
- Muzny, C.A.; Van Gerwen, O.T. Secnidazole for Trichomoniasis in women and men. Sex. Med. Rev. 2022, 10, 255–262. [Google Scholar] [CrossRef]
- Kissinger, P. Trichomonas vaginalis: a review of epidemiologic, clinical and treatment issues. BMC Infect. Dis. 2015, 15, 307–315. [Google Scholar] [CrossRef]
- Dunne, R.L.; Dunn, L.A.; Upcroft, P.; O´Donoghue, P.J.; Upcroft, J.A. Drug resistance in the sexually transmitted protozoan Trichomonas vaginalis. Cell Res. 2003, 13, 239–249. [Google Scholar] [CrossRef]
- Helms, D.J.; Mosure, D.J.; Secor, E.; Workowski, K.A. Management of Trichomonas vaginalis in women with suspected metronidazole sensitivity. Am. J. Obstet. Gynecol. 2008, 198, 370.e1–370.e7. [Google Scholar] [CrossRef] [PubMed]
- Forna, F.; Gülmezoglu, A.M. Interventions for treating trichomoniasis in women. Cochrane Database Syst. Rev. 2003, 2, CD000218. [Google Scholar] [CrossRef]
- Gaydos, C.A.; Klausner, J.D.; Pai, N.P.; Kelly, H.; Coltart, C.; Peeling, R.W. Rapid and point-of-care tests for the diagnosis of Trichomonas vaginalis in women and men. Sex. Transm. Infect. 2017, 93, S31–S35. [Google Scholar] [CrossRef] [PubMed]
- McMillan, A. Laboratory diagnostic methods and cryopreservation of trichomonads. In Trichomonads Parasitic in Humans. Honigberg, B.M. ed.; Springer-Verlag, New York, NY, USA, 1990; pp. 297–310.
- Rein, M.F. Trichomoniasis. In Hunter’s Tropical Medicine and Emerging Infectious Diseases (Tenth Edition). Ryan, E.T.; Hill, D.R.; Solomon, T.; Aronson, N.; Endy, T.P. ed.; Elsevier Health Sciences, New York, NY, USA, 2020; pp. 731–733. ISBN: 9780323555128.
- Petrin, D.; Delgaty, K.; Bhatt, R.; Garber, G. Clinical and microbiological aspects of Trichomonas vaginalis. Clin. Microbiol. Rev., 1998, 11, 300–317. [Google Scholar] [CrossRef]
- Schwebke, J.R. Trichomonas vaginalis. In Mandell, Douglas, and Bennett’s Principles and Practice of Infectious Diseases (Eighth Edition). Bennett, J.E.; Dolin, R.; Blaser, M.J. ed.; Elsevier Saunders, Philadelphia, PA, USA, 2015; 2, pp. 3161–3164. ISBN: 9781455748013.
- Donné, M.A. Animacules observes dans les matières purulentes et le produit des sécretions des organes genitaux de l’homme et de la femme. C. R. Acad. Sci., 1836, 3, 385–386. [Google Scholar]
- Sivaranjini, R.; Jaisankar, T.J.; Thappa, D.M.; Kumari, R.; Chandrasekhar, L.; Malathi, M.; Parija, S.C.; Habeebullah, S. Trichomoniasis: How do we diagnose in a resource poor setting? Indian J. Sex. Transm. Dis. AIDS, 2013, 34, 25–31. [Google Scholar] [PubMed]
- Hobbs, M.M.; Seña, A.C. Modern diagnosis of Trichomonas vaginalis infection. Sex. Transm. Infect., 2013, 89, 434–438. [Google Scholar] [CrossRef]
- Piperaki, E.T.; Theodora, M.; Mendris, M. , Barbitsa, L.; Pitiriga, V.; Antsaklis, A.; Tsakris, A. Prevalence of Trichomonas vaginalis infection in women attending a major gynaecological hospital in Greece: a cross-sectional study. J. Clin. Pathol., 2010, 63, 249–253. [Google Scholar] [CrossRef] [PubMed]
- Schwebke, J.R.; Hook, E.W. III. High rates of Trichomonas vaginalis among men attending a sexually transmitted diseases clinic: implications for screening and urethritis management. J. Infect. Dis., 2003, 188, 465–468. [Google Scholar] [CrossRef] [PubMed]
- Robertson, D.H.H.; Lumsden, W.H.R.; Fraser, K.F.; Hosie, D.D.; Moore, D.M. Simultaneous isolation of Trichomonas vaginalis and collection of vaginal exudates. Br. J. Vener. Dis., 1969, 45, 42–43. [Google Scholar] [CrossRef] [PubMed]
- Oates, J.K.; Selwyn, S.; Breach, M.R. Polyester sponge swabs to facilitate examination for genital infection in women. B. J. Vener. Dis., 1971, 47, 289–292. [Google Scholar] [CrossRef] [PubMed]
- Galán-Montemayor, J.C.; Lepe-Jiménez, J.A.; Otero-Guerra, L.; Serra-Pladevall, J.; Vázquez-Valdés, F. Diagnóstico microbiológico de las infecciones de transmisión sexual y otras infecciones genitales. In Procedimientos en Microbiología Clínica (24 edición). Cercenado-Mansilla, E.; Cantón-Moreno, R. ed.; Sociedad Española de Enfermedades Infecciosas y Microbiología Clínica (SEIMC), Madrid, España, 2018; pp. 1–94. ISBN: 978-84-09-07783-0.
- Krieger, J.N. Trichomoniasis in men: old issues and new data. Sex. Transm. Dis., 1995, 22, 83–96. [Google Scholar] [CrossRef]
- Khatoon, R.; Jahan, N.; Khan, H.M.; Rabbani, T.; Ahmad, S. Evaluation of different staining techniques in the diagnosis of Trichomonas vaginalis infection in females of reproductive age group. J. Clin. Diagnostic Res., 2014, 8, 5–8. [Google Scholar] [CrossRef]
- Alcamo, I.E. Fundamentals of Microbiology. 6th illustrated edition. Jones and Bartlett Publishers, Boston. MA, USA; 2001, pp. 486–487. ISBN: 978-0-7637-0067-6.
- Madhivanan, P.; Li, T.; Trammell, S.; Desai, C.; Srinivas, V.; Arun, A.; Klausner, J.D.; Krupp, K. Performance of the OSOM Trichomonas Rapid Test for diagnosis of Trichomonas vaginalis infection among women in Mysore, India. Sex. Health, 2013, 10, 320–324. [Google Scholar] [CrossRef] [PubMed]
- Beverly, A.L.; Vengtarik, L.M.; Cotton, B.; Schwebke, J.R. Viability of Trichomonas vaginalis in transport medium. J. Clin. Microbiol., 1999, 37, 3749–3750. [Google Scholar] [CrossRef] [PubMed]
- Martin, R.D.; Kaufman, R.H.; Burns, M. Trichomonas vaginalis: a statistical evaluation of diagnostic methods. Am. J. Obstet. Gynecol., 1963, 87, 1024–1027. [Google Scholar] [CrossRef] [PubMed]
- McCann, J.S. Comparison of direct microscopy and culture in the diagnosis of trichomoniasis. Br. J. Vener. Dis., 1974, 50, 450–452. [Google Scholar] [CrossRef]
- Clark, D.H., Solomons. An evaluation of routine culture examination for Trichomonas vaginalis and Candida. Am. J. Obstet. Gynecol., 1959, 78, 1314–1319. [Google Scholar] [CrossRef] [PubMed]
- Stuart, R.D. Transport problems in public health bacteriology. Can. J. Public Health, 1956, 47, 114–122. [Google Scholar]
- Bolumburu, C.; Zamora, C.; Muñoz-Algarra, M.; Portero-Azorín, F.; Escario, J.A.; Ibáñez-Escribano, A. Trichomoniasis in a tertiary hospital of Madrid, Spain (2013–2017): prevalence and pregnancy rate, coinfections, metronidazole resistance, and endosymbiosis. Parasitol. Res., 2020, 119, 1915–1923. [Google Scholar] [CrossRef] [PubMed]
- Amies, C.R. A modified formula for the preparation of Stuart’s transport medium. Can. J. Public Health, 1967, 58, 296–300. [Google Scholar]
- Nielsen, R. Trichomonas vaginalis. Survival in solid Stuart’s medium. Br. J. Vener. Dis., 1969; 45, 328–331. [Google Scholar] [CrossRef]
- Kingston, M.A.; Carlin, D.; Bansal, E.M. Shelf life of Trichomonas vaginalis. Int. J. STD AIDS, 2003, 14, 28–29. [Google Scholar] [CrossRef]
- Feinberg, J.G.; Whittington, M.J. A culture medium for Trichomonas vaginalis Donné and species of Candida. J. Clin. Pathol., 1957, 10, 327–329. [Google Scholar] [CrossRef] [PubMed]
- Eriksson, G.; Wanger, L. Frequency of N. gonorrhoeae, T. vaginalis and C. albicans in female venereological patients. Br. J. Vener. Dis. 1975, 51, 192–197. [Google Scholar] [CrossRef] [PubMed]
- Hoffman, B.; Kilczewski, W.; Malyszko, E. Studies in trichomoniasis in males. Br. J. Vener. Dis., 1961, 37, 172–175. [Google Scholar] [CrossRef] [PubMed]
- Hughes, H.E.; Gordon, A.M.; Barr, G.T.D. A clinical laboratory study of trichomoniasis of the female genital tract. Br. J. Obstet. Ginecol., 1966, 73, 821–827. [Google Scholar] [CrossRef]
- Freeman, F. A modified staining technique for Trichomonas vaginalis. S. Afr. Med. J. 1958; 32, 1235. [Google Scholar] [PubMed]
- Lowe, G.H. The laboratory diagnosis of trichomoniasis. In Laboratory Diagnosis of Venereal Disease. Public Health Laboratory Service Monograph Series No. 1, London, UK, 1972; pp. 40–42. Record Number: 19732702663.
- Fripp, P.J.; Mason, P.R.; Super, H. A method for the diagnosis of Trichomonas vaginalis using acridine orange. J. Parasitol., 1975, 61, 966–967. [Google Scholar] [CrossRef] [PubMed]
- Levett, P.N. A comparison of five methods for the detection of Trichomonas vaginalis in clinical specimens. Med. Lab. Sci., 1980, 37, 85–88. [Google Scholar] [PubMed]
- Rodriguez-Martinez, H.A.; De la Luz Rosales, M.; Gallaso de Bello, L.; Ruiz-Moreno, J.A. Adequate staining of Trichomonas vaginalis by McManus’ periodic acid-Schiff stain. Am. J. Clin. Pathol., 1973, 59, 741–746. [Google Scholar] [CrossRef] [PubMed]
- Nagesha, C.N.; Ananthkrishna, N.C.; Sulochana, P. Clinical and laboratory studies on vaginal trichomoniasis. Am. J. Obstet. Gynecol., 1970, 106, 933–935. [Google Scholar] [CrossRef] [PubMed]
- Miller, J.R. Contrast stain for the rapid identification of Trichomonas vaginalis. Am. J. Clin. Pathol, 1937, 7, 40. [Google Scholar] [CrossRef]
- Eddie, D.A.S. The laboratory diagnosis of vaginal infections caused by Trichomonas and Candida (Monilia) species. J Med Microbiol., 1968, 1, 153–159. [Google Scholar] [CrossRef] [PubMed]
- Perju, A.; Strîmbeanu, I. Valeur de la spermoculture dans ie diagnostic de la trichomonase urogenitale chez I’homme. Wiad. Parazytol., 1966, 12, 475–480. [Google Scholar]
- Coutts, W.E.; Silva-Inzunza, E. Vital staining of Trichomonas vaginalis with fluorescein. Br. J. Vener. Dis., 1954, 30, 43–46. [Google Scholar] [CrossRef] [PubMed]
- Tanabe, M. Morphological Studies on Trichomonas. J. Parasitol., 1926, 12, 120–130. [Google Scholar] [CrossRef]
- Sorel, C. Trois techniques de recherche du Trichomonas vaginalis: leurs valeurs comparées. Presse Med., 1954, 62, 602–604. [Google Scholar] [PubMed]
- Lowe, G.H. A comparison of current laboratory methods with a new semisolid culture medium for the detection of Trichomonas vaginalis. J. Clin. Pathol., 1965, 18, 432–434. [Google Scholar] [CrossRef]
- Rogers, S.; Goldsmid, J.M. A study of the possible value of acridine orange-O stain in the diagnosis of Trichomonas vaginalis infection. Cent. Afr. J. Med., 1977, 23, 56–58. [Google Scholar] [PubMed]
- Buharowski, K.; Wolanska, M. Usefulness of staining specimens with acridine orange in the diagnosis of Trichomonas vaginalis. Wiad. Parazytol., 1984, 30, 499–501. [Google Scholar]
- Mason, P.R. , Super, H., Fripp, P.J. Comparison of four techniques for the routine diagnosis of Trichomonas vaginalis infection. J. Clin. Pathol., 1976, 29, 154–157. [Google Scholar] [CrossRef]
- Thin, R.N.T.; Atia, W.; Parker, J.D.J.; Nicol, C.S.; Canti, G. Value of Papanicolaou-stained smears in the diagnosis of trichomoniasis, candidiasis and cervical herpes simplex virus infection in women. Br. J. Vener. Dis., 1975, 51, 116–118. [Google Scholar] [CrossRef] [PubMed]
- Bickley, L.S.; Krisher, K.K.; Punsalang, A.; Trupei, M.A.; Reichman, R.C.; Menegus, M.A. Comparison of direct fluorescent antibody, acridine orange, wet mount, and culture for detection of Trichomonas vaginalis in women attending a public sexually transmitted diseases clinic. Sex Transm Dis. 1989; 16, 127–131. [Google Scholar] [CrossRef]
- Garber, G.E.; Sibau, L.; Ma, R.; Proctor, E.M.; Shaw, C.E.; Bowie, W.R. Cell culture compared with broth for detection of Trichomonas vaginalis. J. Clin. Microbiol., 1987, 25, 1275–1279. [Google Scholar] [CrossRef] [PubMed]
- Thomason, J.L.; Gelbart, S.M.; Sobun, J.F.; Schulien, M.B.; Hamilton, P.R. Comparison of four methods to detect Trichomonas vaginalis. J. Clin. Microbiol. 1988; 26, 1869–1870. [Google Scholar] [CrossRef]
- Schmid, G.P. , Matheny, L.C., Zaidi, A.A., Kraus, S.J. Evaluation of six media for the growth of Trichomonas vaginalis from vaginal secretions. Journal of Clinical Microbiology, 1986; 27, 1230–1233. [Google Scholar] [CrossRef]
- Patil, M.J.; Nagamoti, J.M.; Metgud, S.C. Diagnosis of Trichomonas vaginalis from vaginal specimens by wet mount microscopy, InPouch TV culture system, and PCR. J. Glob. Infect. Dis., 2012, 4, 22–25. [Google Scholar] [CrossRef] [PubMed]
- Moldwin, R.M. Sexually transmitted protozoal infections. Trichomonas vaginalis, Entamoeba histolytica, and Giardia lamblia. Urol. Clin. North Am. 1992, 19, 93–101. [Google Scholar] [CrossRef] [PubMed]
- Fouts, A.C.; Kraus, S.J. Trichomonas vaginalis: reevaluation of its clinical presentation and laboratory diagnosis. J. Infect. Dis., 1980, 141, 137–143. [Google Scholar] [CrossRef] [PubMed]
- Van Gerwen, O.T.; Muzny, C.A. Recent advances in the epidemiology, diagnosis, and management of Trichomonas vaginalis infection. F1000Res, 2019, 8, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Schwebke, J.R.; Burgess, D. Trichomoniasis. Clin. Microbiol. Rev., 2004, 17, 794–803. [Google Scholar] [CrossRef] [PubMed]
- Sood, S.; Mohanty, S.; Kapil, A.; Tolosa, J.; Mittal, S. InPouch TV culture for detection of Trichomonas vaginalis. Indian J. Med. Res. 2007, 125, 567–571. [Google Scholar]
- Méndez-Izquierdo, J.E.; Fonseca-Berzal, C.R.; Ibáñez-Escribano, A. Trichomonas vaginalis: Diagnosis of a forgotten sexually transmitted infection. An. Real Acad. Farm., 2023, 89, 135–148. [Google Scholar] [CrossRef]
- Levi, M.H.; Torres, J.; Pina, C.; Klein, R.S. Comparison of the InPouch system and Diamond´s modified medium for detection of Trichomonas vaginalis J. Clin. Microbiol. 1996, 35, 3308–3310. [Google Scholar] [CrossRef]
- Borchardt, K.A.; Zhang, M.; Shing, H.; Flink, K. A comparison of the sensitivity of the InPouch TV, Diamond’s and Trichosel media for the detection of Trichomonas vaginalis. Genitourin. Med., 1997, 73, 297–298. [Google Scholar] [CrossRef] [PubMed]
- Ibáñez-Escribano, A.; Gómez-Barrio, A. Trichomonas vaginalis: la versatilidad de un parásito tenaz. An. Real Acad. Farm., 2017, 83, 10–47. [Google Scholar]
- Mahmoud, A.; Sherif, N.A.; Abdella, R.; El-Genedy, A.R.; El Kateb, A.Y.; Askalani, A.N. Prevalence of Trichomonas vaginalis infection among Egyptian women using culture and latex agglutination: cross sectional study. BMC Women’s Health 2015, 15, 1–6. [Google Scholar] [CrossRef]
- Darani, H.Y.; Ahmadi, F.; Zabardast, N.; Yousefi, H.A.; Shirzad, H. Development of a latex agglutination test as a simple and rapid method for diagnosis of Trichomonas vaginalis infection. Avicenna J. Med. Biotechnol. 2010, 2, 63–66. [Google Scholar] [PubMed]
- Yousofi-Darani, H.; Sharafi, S.; Heidari, M.; Poor, S.; Jafari, R.; Hosseini, S. Diagnosis of vaginal candidiasis and Trichomonas vaginalis infection by antibody coated latex particles. J. Adv. Med. Med. Res. 2017, 24, 1–5. [Google Scholar] [CrossRef]
- Adu-Sarkodie, Y.; Opoku, B.K.; Danso, K.A.; Weiss, H.A.; Mabey, D. Comparison of latex agglutination, wet preparation, and culture for the detection of Trichomonas vaginalis. Sex. Transm. Infect., 2004, 80, 201–203. [Google Scholar] [CrossRef]
- Gan, S.D.; Patel, K.R. Enzyme immunoassay and enzyme-linked immunosorbent assay. J. Invest. Dermatol., 2013, 133, 1–3. [Google Scholar] [CrossRef]
- Kim, J.H.; Moon, H.S.; Kim, K.S.; Hwang, H.S.; Ryu, J.S.; Park, S.Y. Comparison of seropositivity to Trichomonas vaginalis between men with prostatic tumor and normal men. Korean J Parasitol., 2019, 57, 21–25. [Google Scholar] [CrossRef]
- Alderete, J.F.; Neace, C.J. Identification, characterization, and synthesis of peptide epitopes and a recombinant six-epitope protein for Trichomonas vaginalis serodiagnosis. Immunotargets Ther., 2013, 2, 91–103. [Google Scholar] [CrossRef]
- Alderete, J.F. Advancing prevention of STIs by developing specific serodiagnostic targets: Trichomonas vaginalis as a model. Int. J. Environ. Res. Public Health 2020, 17, 5783–5799. [Google Scholar] [CrossRef]
- Alderete, J.F. Epitopes within recombinant α-actinin protein is serodiagnostic target for Trichomonas vaginalis sexually transmitted infections. Heliyon 2017, 3, e00237. [Google Scholar] [CrossRef] [PubMed]
- Alderete, J.F. Recombinant protein of immunogenic metabolic enzyme epitopes of Trichomonas vaginalis are common to humans and microorganisms. Am. J. Biomed. Res., 2021, 13, 630–638. [Google Scholar] [CrossRef]
- Bedair, N.H.; Ali, H.Z. Comparison of trichomoniasis diagnosis by microscopic methods and indirect ELISA technique in a sample of Iraqi women. Iraqi J. Sci., 2020, 61, 742–748. [Google Scholar] [CrossRef]
- Street, D.A.; Taylor-Robinson, D.; Ackers, J.P.; Hanna, N.F.; McMillan, A. Evaluation of an enzyme-linked immunosorbent assay for the detection of antibody to Trichomonas vaginalis in sera and vaginal secretions. Br. J. Vener. Dis., 1982, 58, 330–333. [Google Scholar] [CrossRef]
- Watt, R.M.; Philip, A.; Wos, S.M.; Sam, G.J. Rapid assay for immunological detection of Trichomonas vaginalis. J. Clin. Microbiol., 1986, 24, 551–555. [Google Scholar] [CrossRef] [PubMed]
- Adjei, C.; Boateng, R.; Dompreh, A.; Okyere, B.; Owiredu, E.W. Prevalence and the evaluation of culture, wet mount, and ELISA methods for the diagnosis of Trichomonas vaginalis infection among Ghanaian women using urine and vaginal specimens. Trop. Med. Health., 2019, 47, 33–41. [Google Scholar] [CrossRef] [PubMed]
- Lisi, P.J.; Dondero, R.S.; Kwiatkoski, D.; Spence, M.R.; Rein, M.F.; Alderete, J.F. Monoclonal-antibody-based enzyme-linked immunosorbent assay for Trichomonas vaginalis. J. Clin. Microbiol., 1988, 26, 1684–1686. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.; Li, Y.; Wang, S.; Hao, L.; Zhu, Y.; Li, H.; Song, X.; Duan, Y.; Sang, Y.; Wu, P.; Li, X. The molecular characterization and immunity identification of Trichomonas vaginalis adhesion protein 33 (AP33). Front. Microbiol., 2020, 11, 1433. [Google Scholar] [CrossRef] [PubMed]
- Juliano, C.; Rubino, S.; Zicconi, D.; Cappuccinelli, P. An immunofluorescent study of the microtubule organization in Trichomonas vaginalis using antitubulin antibodies. J. Protozool., 1986, 33, 56–59. [Google Scholar] [CrossRef]
- Khoshnan, A.; Alderete, J.F. Trichomonas vaginalis with a double stranded RNA virus has upregulated levels of phenotypically variable immunogen mRNA. J. Virol., 1994, 68, 4035–4038. [Google Scholar] [CrossRef]
- Khatoon, R.; Jahan, N.; Ahmad, S.; Khan, H.M.; Rabbani, T. Comparison of four diagnostic techniques for detection of Trichomonas vaginalis infection in females attending tertiary care hospital of North India. Indian J. Pathol. Microbiol., 2015, 58, 36–39. [Google Scholar] [CrossRef]
- Bickley, L.S.; Krisher, K.K.; Punsalang, A. , Trupei, M.A.; Reichman, R.C.; Menegus, M.A. Comparison of direct fluorescent antibody, acridine orange, wet mount, and culture for detection of Trichomonas vaginalis in women attending a public sexually transmitted diseases clinic. Sex. Transm. Dis., 1989, 16, 127–131. [Google Scholar] [CrossRef] [PubMed]
- Smith, R.F. Detection of Trichomonas vaginalis in vaginal specimens by direct immunofluorescence assay. J. Clin. Microbiol., 1986, 24, 1107–1108. [Google Scholar] [CrossRef] [PubMed]
- Muralidhar, S. Molecular methods in the laboratory diagnosis of sexually transmitted infections. Indian J. Sex. Transm. Dis. AIDS, 2015, 36, 9–17. [Google Scholar] [CrossRef] [PubMed]
- Adamson, P.C.; Loeffelholz, M.J.; Klausner, J.D. Point-of-Care testing for sexually transmitted infections: a review of recent developments. Arch. Pathol. Lab. Med., 2020, 144, 1344–1351. [Google Scholar] [CrossRef]
- Alderete, J.F. Trichomonas vaginalis, reproductive health, and a minority scientist’s experiences. Biol Reprod., 2011, 85 (Suppl_1), 96. [Google Scholar] [CrossRef]
- Sekisui Diagnostics. Training lesson of OSOM® Trichomonas IFU. Sekisui Diagnostics. 2023. Available online: https://sekisuidiagnostics.com/product/osom-trichomonas-test/ (accessed on 12 September 2023).
- Alderete, J.F.; Chan, H. Poinf-of-Care diagnostic for Trichomonas vaginalis, the most prevalent, non-viral sexually transmitted infection. Pathogens, 2023, 12, 77. [Google Scholar] [CrossRef] [PubMed]
- Boeras, D.; Cohan, J.S.; Vojnov, L.; Wi, T.; Toskin, I.; Barrett, K.; Ghadreshenas, A.; Maatouk, I.; McCartney, D. The diagnostic landscape for sexually transmitted infections; Geneva: World Health Organization, 2013; pp. 5–38. [Google Scholar]
- U.S. Food & Drug Administration. Nucleic Acid Based Test. Available online: https://www.fda.gov/medical-devices/in-vitro-diagnostics/nucleic-acid-based-tests#microbial (accessed on 27 September 2023).
- Schwbke, J.R.; Gaydos, C.A.; Davis, T.; Marrazzo, J.; Furgerson, D.; Taylor, S.N.; Smith, B.; Bachmann, L.H.; Ackerman, R.; Spurrell, T.; Ferris, D.; Burnham, C.-A.D.; Reno, H.; Lebed, J.; Eisenberg, D.; Kerndt, P.; Philip, S.; Jordan, J.; Quigley, N. Clinical evaluation of the Cepheid Xpert TV Assay for detection of Trichomonas vaginalis with prospectively collected specimens from men and women. J. Clin. Microbiol. 2018, 56, e01091-17. [Google Scholar] [CrossRef] [PubMed]
- Chapin, K.; Andrea, S. APTIMA® Trichomonas vaginalis, a transcription-mediated amplification assay for detection of Trichomonas vaginalis in urogenital specimens. Expert Rev. Mol. Diagn. 2011, 11(7), 679–688. [Google Scholar] [CrossRef] [PubMed]
- Van Der Pol, B.; Williams, JA.; Taylor, S.N.; Cammarata, C.L.; Rivers, C.A.; Body, B.A.; Nye, M.; Fuller, D.; Schwebke, J.R.; Barnes, M.; Gaydos, C.A. Detection of Trichomonas vaginalis DNA by use of self-obtained vaginal swabs with the BD ProbeTec Qx assay on the BD viper system. J. Clin. Micribiol., 2014, 52, 885–889. [Google Scholar] [CrossRef] [PubMed]
- Shipitsyna, E.; Unemo, M. A profile of the FDA-approved and CE/IVD-marked Aptima Mycoplasma genitalium assay (Hologic) and key priorities in the management of M. genitalium infections. Exp. Rev. Mol. Diagnostics 2020, 20, 1063–1074. [Google Scholar] [CrossRef]
- Andrea, S.B.; Chapin, K.C. Comparison of Aptima Trichomonas vaginalis transcription-mediated amplification assay and BD affirm VPIII for detection of T. vaginalis in symptomatic women: performance parameters and epidemiological implications. J. Clin. Microbiol., 2011, 49, 866–869. [Google Scholar] [CrossRef]
- Van Der Pol, B.; Torres-Chavolla, E.; Kodsi, S.; Cooper, C.K.; Davis, T.E.; Fife, K.H.; Taylor, S.N.; Augenbraun, M.H.; Gaydos, C.A. Clinical performance of the BD CTGCTV2 assay for the BD MAX System for detection of Chlamydia trachomatis, Neisseria gonorrhoeae, and Trichomonas vaginalis infections. Sex Transm Dis., 2021, 48, 134–140. [Google Scholar] [CrossRef]
- Goldstein, E.; Martinez-García, L.; Obermeier, M.; Glass, A.; Krügel, M.; Maree, L.; Gunson, R.; Onelia, F.; Pacenti, M.; Nelson, K.; Joseph, A.; Palm, M.; Lucic, D.; Marlowe, N.; Dhein, J.; Reinhardt, B.; Pfeifer, K.; Galan, J.; Azzato, F. Simultaneous identification of Chlamydia trachomatis, Neisseria gonorrhoeae, Mycoplasma genitalium, and Trichomonas vaginalis ‒ multicenter evaluation of the Alinity m STI assay. J. Lab. Med., 2021, 45, 213–223. [Google Scholar] [CrossRef]
- Matysiak, C.; Cheng, A.; Kirby, J.E. Evaluation of the Abbott Alinity m STI assay for diagnosis of the primary cases of sexually transmitted infections in the United States. Pract. Lab. Med., 2023, 36, e00332. [Google Scholar] [CrossRef] [PubMed]
- Marlowe, E.M.; Gohl, P.; Steidle, M.; Arcenas, R.; Bier, C. Trichomonas vaginalis detection in female specimens with cobas® TV/MG for use on the cobas® 6800/8800 Systems. Eur. J. Microbiol. Immunol., 2019, 9, 42–45. [Google Scholar] [CrossRef] [PubMed]
- Gaydos, C.A.; Schwebke, J.; Dombrowski, J.; Marrazzo, J.; Coleman, J.; Silver, B.; Barnes, M.; Crane, L.; Fine, P. Clinical performance of the Solana® Point-of-Care Trichomonas assay from clinician-collected vaginal swabs and urine specimens from symptomatic and asymptomatic women. Exp. Rev. Mol. Diagn., 2017, 17, 303–306. [Google Scholar] [CrossRef] [PubMed]
- Gaydos, C.A.; Hobbs, M.; Marrazzo, J.; Schwebke, J.; Coleman, J.S.; Masek, B.; Dize, L.; Jang, D.; Li, J.; Chernesky, M. Rapid diagnosis of Trichomonas vaginalis by testing vaginal swabs in an isothermal helicase-dependent AmpliVue™ Assay. Sex. Transm. Dis., 2016, 43, 369–373. [Google Scholar] [CrossRef] [PubMed]
- Morris, S.R.; Bristow, C.C.; Wierzbicki, M.R.; Sarno, M.; Asbel, L.; French, A.; Gaydos, C.A.; Hazan, L.; Mena, L.; Madhivanan, P.; Philip, S.; Schwartz, S.; Brown, C.; Styers, D.; Waymer, T.; Klausner, J.D. Performance of a single-use, rapid, point-of-care PCR device for the detection of Neisseria gonorrhoeae, Chlamydia trachomatis, and Trichomonas vaginalis: a cross-sectional study. Lancet Infect. Dis., 2021, 21, 668–676. [Google Scholar] [CrossRef] [PubMed]
- Brown, H.L.; Fuller, D.D.; Davis, T.E.; Schwebke, J.R.; Hillier, S.L. Evaluation of the Affirm ambient temperature transport system for the detection and identification of Trichomonas vaginalis, Garderella vaginalis, and Candida species from vaginal fluid specimens. J. Clin. Mirobiol., 2001, 39, 3197–3199. [Google Scholar] [CrossRef] [PubMed]
- Taylor, S.; Rucky, A.; Lockamy, E.; Wolfe, D.; Streck, N.; Uribe, G.; Cammarata, C.; Diodene, D.; Cooper, C.K.; Vaughan, L.; Greene, W. Validation of a new high-throughput BD COR System using the BD CTGCTV2 assay. J. Mol. Diagnost., 2022, 24, 485–493. [Google Scholar] [CrossRef]
- Tipple, C.; Rayment, M.; Mandalia, S.; Walton, L.; O’Neill, S.; Murray, J.; O´Riordan, A.; Rebec, M.; Harrington, L.; Jones, R.; Wilkinson, D. An evaluation study of the Becton-Dickinson ProbeTec Qx (BDQx) Trichomonas vaginalis trichomoniasis molecular diagnostic test in two large, urban STD services. Sex. Transm. Infect., 2018, 94, 334–336. [Google Scholar] [CrossRef] [PubMed]
- Van Der Pol, B.; Rao, A.; Nye, M.B.; Chavoustie, S.; Ermel, A.; Kaplan, C.; Eisenber, D.; Chan, P.A.; Mena, L.; Pacheco, S.; Waites, K.B.; Xiao, L.; Krishnamurthy, S.; Mohan, R.; Bertuzis, R.; McGowin, C.L.; Arcenas, R.; Marlowe, E.M.; Taylor, S.N. Trichomonas vaginalis detection in urogenital specimens from symptomatic and asymptomatic men and women by use of the cobas TV/MG Test. J. Clin. Microbiol 2021, 59, 10–1128. [Google Scholar] [CrossRef]
- Bui, H.T.V.; Bui, H.T.; Chu, S.V.; Nguyen, H.T.; Nguyen, A.T.V.; Truong, P.T.; Dang, T.T.H.; Nguyen, A.T.V. Simultaneous real-time PCR detection of nine prevalent sexually transmitted infections using a predesigned double-quenched TaqMan probe panel. PLoS ONE, 2023, 18, E0282439. [Google Scholar] [CrossRef] [PubMed]
- Hu, X.-M.; Xu., J.-X.; Jiang, L.-X.; Deng, L.-R.; Gu, Z.-M.; Xie, X.-Y.; Ji, H.-C.; Wang, W.-H.; Li, L.-M.; Tian, C.-N.; Song, F.-L.; Huang, S.; Zheng, L.; Zhong, T-Y. Design and evaluation of a novel multiplex Real-Time PCR melting curve assay for the simultaneous detection of nine Sexually Transmitted Disease pathogens in genitourinary secretions. Front. Cell. Infect. Microbiol 2019, 9, 382. [Google Scholar] [CrossRef] [PubMed]
- Reyes, J.C.B.; Solon, J.A.A.; Rivera, W.L. Development of a loop-mediated isothermal amplification assay for detection of Trichomonas vaginalis. Diagn. Microbiol. Infect. Dis. 2014, 79, 337–341. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Wang, S.; Li, H.; Song, X.; Zhang, H.; Duan, Y.; Luo, C.; Wang, B.; Ji, S.; Xie, Q.; Zhang, Z. Development of a convenient detection method for Trichomonas vaginalis based on loop-mediated isothermal amplification targeting adhesion protein 65. BMC Infect. Dis. 2020, 20, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Espiritu, C.A.L.; Justo, C.A.C.; Jauset Rubio, M.; Svobodova, M.; Bashammakh, A.S.; Alyoubi, A.O.; Rivera, W.L.; Rollon, A.P.; O´Sullivan, C.K. Aptamer selection against a Trichomonas vaginalis adhesion protein for diagnostic applications. ACS Infect. Dis., 2018, 4, 1306–1315. [Google Scholar] [CrossRef]
- Fu, L.; Sun, Y.; Han, M.; Wang, B.; Xiao, F.; Zhou, Y.; Gao, Y.; Fitzpatrick, T.; Yuan, T.; Li, P.; Zhan, Y.; Lu, Y.; Luo, G.; Duan, J.; Hong, Z.; Fairley, C.K.; Zhang, T.; Zhao, J.; Zou, H. Incidence trends of five common sexually transmitted infections excluding HIV from 1990 to 2019 at the global, regional, and national levels: results from the global burden of disease study 2019. Front. Med. 2022, 9, 851635. [Google Scholar] [CrossRef] [PubMed]
- Hotez, P.J.; Gurwith, M. Europe’s neglected infections of poverty. Int. J. Infect. Dis. 2011, 15, e611–e619. [Google Scholar] [CrossRef] [PubMed]
- Secor, W.E.; Meites, E.; Starr, M.C.; Workowski, K.A. Neglected parasitic infections in the United States: trichomoniasis. Am. J. Trop. Med. Hyg. 2014, 90, 800. [Google Scholar] [CrossRef] [PubMed]
- CDC. Sexual Risk Behaviours. 2023. Available online: https://www.cdc.gov/healthyyouth/sexualbehaviors/index.htm.
- Clifton, S.; Mercer, C.H.; Sonnenberg, P.; Tanton, C.; Field, N.; Gravningen, K.; Hughes, G.; Mapp, F.; Johnson, A.M. STI risk perception in the British population and how it relates to sexual behaviour and STI healthcare use: findings from a cross-sectional survey (Natsal-3). J. Clin. Med 2018, 2, 29–36. [Google Scholar] [CrossRef]
- Lara, L.A.S.; Abdo, C.H.N. Age at time of initial sexual intercourse and health of adolescent girls. J. Pediatr. Adolesc. Gynecol. 2016, 29, 417–423. [Google Scholar] [CrossRef] [PubMed]
- Menezes, C.B.; Frasson, A.P.; Tasca, T. Trichomoniasis - are we giving the deserved attention to the most common non-viral sexually transmitted disease worldwide? Microb. Cell 2016, 3, 404–419. [Google Scholar] [CrossRef]
- Cheeson, H.W.; Blandford, J.M.; Pinkerton, S.D. Estimates of the annual number and cost of new HIV infections among women attributable to trichomoniasis in the United States. Sex. Transm. Dis. 2004, 31, 547–551. [Google Scholar] [CrossRef]
- Chesson, H.W.; Blandford, J.M.; Gift, T.L.; Tao, G.; Irwin, K.L. The estimated direct medical cost of Sexually Transmitted Diseases among American youth, 2000. Persp. Sex. Reprod. Health. 2007, 35, 11–19. [Google Scholar] [CrossRef]
- Kumar, S.; Chesson, H.W.; Spicknall, I.H.; Kreisel, K.M.; Grift, T. The estimated lifetime medical cost of Chlamydia, Gonorrhea, and Trichomoniasis in the United States, 2018. Sex. Transm. Dis. 2021, 48, 238–246. [Google Scholar] [CrossRef]
- Workowski, K.A.; Bolan, G.A. Sexually transmitted diseases treatment guidelines, 2015. Morb. Mortal. Wkly. Rep., 2015, 64, 1–137. [Google Scholar]
- Domeika, M.; Zhurauskaya, L.; Savicheva, A.; Frigo, N.; Sokolovskiy, E.; Hallen, A.; Unemo, M.; Ballard, R.C. Guidelines for the laboratory diagnosis of trichomoniasis in East European countries. J. Eur. Acad. Dermatol. Venereol. 2010, 24, 1125–1134. [Google Scholar] [CrossRef] [PubMed]
- Hobbs, M.M.; Lapple, D.M.; Lawing, L.F.; Schwebke, J.R.; Cohen, M.S.; Swygard, H.; Atashili, J.; Leone, P.A.; Miller, W.C.; Seña, A.C. Methods for detection of Trichomonas vaginalis in male partners or infected women: implications for control of trichomoniasis. J. Clin. Microbiol, 2006, 44, 3994–3999. [Google Scholar] [CrossRef]
- Garber, G.E. The laboratory diagnosis of Trichomonas vaginalis. Can. J. Infect. Dis. Med. Microbiol., 2005, 16, 35–38. [Google Scholar] [CrossRef] [PubMed]
Table 2.
Relevant characteristics of the techniques most used in the immunodiagnostic of T. vaginalis.
Table 2.
Relevant characteristics of the techniques most used in the immunodiagnostic of T. vaginalis.
| Test |
Trade name
(manufacturer) |
Sensitivity (Se)
Specificity (Sp) |
Advantages |
Disadvantages |
Ref. |
| Agglutination |
Kalon® TV latex agglutination test
(Kalon Biological)
Darari and others |
Se: 98.9%
Sp: 92.1%
Se: 70%
Sp: 96% |
Fast, simple, and
inexpensive
|
In case of negative results, other method must be carried out
Not designed for male specimens |
[98,99] |
| Indirect ELISA |
|
Se: 71-73%
Sp: 96.3% |
Detects past infections
Admits male specimens. |
Requires complex and expensive equipment
Low sensitivity |
[100] |
| Direct ELISA |
|
Se: 88.9%
Sp: 97.1% |
Good sensitivity and specificity |
Detects only active infections
High rate of false positive rate |
[108] |
DIF*
|
|
Se: 96%
Sp: ND |
Good sensitivity |
Requires complex and expensive equipment |
[114] |
| IC* |
OSOM® TV test
(Sekisui Diagnostics)
|
Se: 83-90%
Sp: 98.9%
|
Fast, and simple
Good sensitivity and specificity |
Not suitable for asymptomatic patients |
[34] |
Table 3.
Sensitivity and specificity ranges of the Nucleic acid amplification test (NAAT) approved by the U.S. Food and Drug Administration. Sens: sensitivity; Spec: specificity: CE-IVD: Devices with the Conformité Européene marking for in vitro diagnostic medical devices.
Table 3.
Sensitivity and specificity ranges of the Nucleic acid amplification test (NAAT) approved by the U.S. Food and Drug Administration. Sens: sensitivity; Spec: specificity: CE-IVD: Devices with the Conformité Européene marking for in vitro diagnostic medical devices.
| Assay |
Manufacturer |
Average Sens. % (range)* |
Average Spec. % (range)* |
Approval status |
Ref. |
| Xpert® Trichomonas vaginalis
|
Cepheid |
Female: 99.5-100
Male: 97.2 |
Female: 99.4-99.9
Male: 99.3 |
FDA
CE-IVD |
[121,123] |
| APTIMA® Trichomonas vaginalis
|
Hologic/Gen-Probe |
98.1 (96.6-100) |
98.3 (96.4-100) |
FDA
CE-IVD |
[124,125,126] |
| BD AffirmTM VPIII |
Becton Dickinson |
63.4 (55.0-65.4) |
99.9 (99.4-100) |
FDA |
[124,127] |
| BD CTGCTV2 |
Becton Dickinson |
Female (86.6-100)
Male (97.9) |
> 98.7 |
FDA |
[122,128] |
| BD ProbeTec Qx Assay |
Becton Dickinson |
98.3 (93.93-99.53) |
99.0 (98.01-99.53) |
FDA
CE-IVD |
[121,125] |
| Alinity m STI |
Abbott |
Female: 95.6-99.7
Male: 98.7 |
Female: 96.9-99.4
Male: 99.2 |
FDA |
[129,130] |
| Cobas® TV/MG |
Roche |
Female: 100 |
Female: ≥99.2 |
FDA
CE-IVD |
[131] |
| Solana® Trichomonas Assay |
Quidel |
98.0-100 |
97.9-98.9 |
FDA |
[132] |
| AmpliVueTM Trichomonas Assay |
Quidel |
96.9-100 |
97.0-98.9 |
FDA |
[132,133] |
| Visby Medical Sexual Health Test |
Visby Medical |
95.5-99.9 |
95.8-97.7 |
FDA |
[123,134] |
Table 4.
Type of samples and other sexually transmitted pathogens that can be detected in the same NAAT platform. PC-VS: patient-collected vaginal swab; CC-VS: clinician-collected vaginal swab; ES: endocervical swab; US: urine sample; PC-E: endocervical specimens collected in PrservCyt® solution; MS: maetal swab.
Table 4.
Type of samples and other sexually transmitted pathogens that can be detected in the same NAAT platform. PC-VS: patient-collected vaginal swab; CC-VS: clinician-collected vaginal swab; ES: endocervical swab; US: urine sample; PC-E: endocervical specimens collected in PrservCyt® solution; MS: maetal swab.
| Assay |
Test |
Samples |
STI |
Ref. |
| Xpert® Trichomonas vaginalis
|
RT PCR |
Female SC-VS, CC-VS, ES and US
Male US |
C. trachomatis, N. gonorrhoeae |
[123,132] |
| APTIMA® Trichomonas vaginalis
|
TMA |
Female SC-VS, CC-VS, ES, PC-E and US |
C. trachomatis, N. gonorrhoeae, Candida spp. |
[124] |
| BD AffirmTM VPIII |
rRNA hybridization |
Female CC-VS, US |
G. vaginalis, C. albicans |
[127] |
| BD CTGCTV2 |
RT PCR |
Female SC-VS, CC-VS, ES, PC-E and US
Male US |
C. trachomatis, N. gonorrhoeae |
[128] |
| BD ProbeTec Qx Assay |
SDA |
Female SC-VS, CC-VS, ES and US |
C. trachomatis, N. gonorrhoeae |
[137] |
| Alinity m STI |
RT PCR |
Female SC-VS, CC-VS, ES and US
Male US |
C. trachomatis, N. gonorrhoeae, M. genitalium |
[122,130] |
| Cobas® TV/MG |
RT PCR |
Female SC-VS, CC-VS, ES, PC-E and US
Male US and MS |
M. genitalium |
[131,138] |
| Solana® Trichomonas Assay |
HDA |
Female CC-VS and US |
|
[132] |
| AmpliVueTM Trichomonas Assay |
HDA |
Female CC-VS |
|
[132] |
| Visby Medical Sexual Health Test |
RT-PCR |
Female SC-VS |
C. trachomatis, N. gonorrhoeae |
[134]
|
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).