Submitted:
05 December 2023
Posted:
06 December 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Results
2.1. Demographic and Clinical Data of Patients
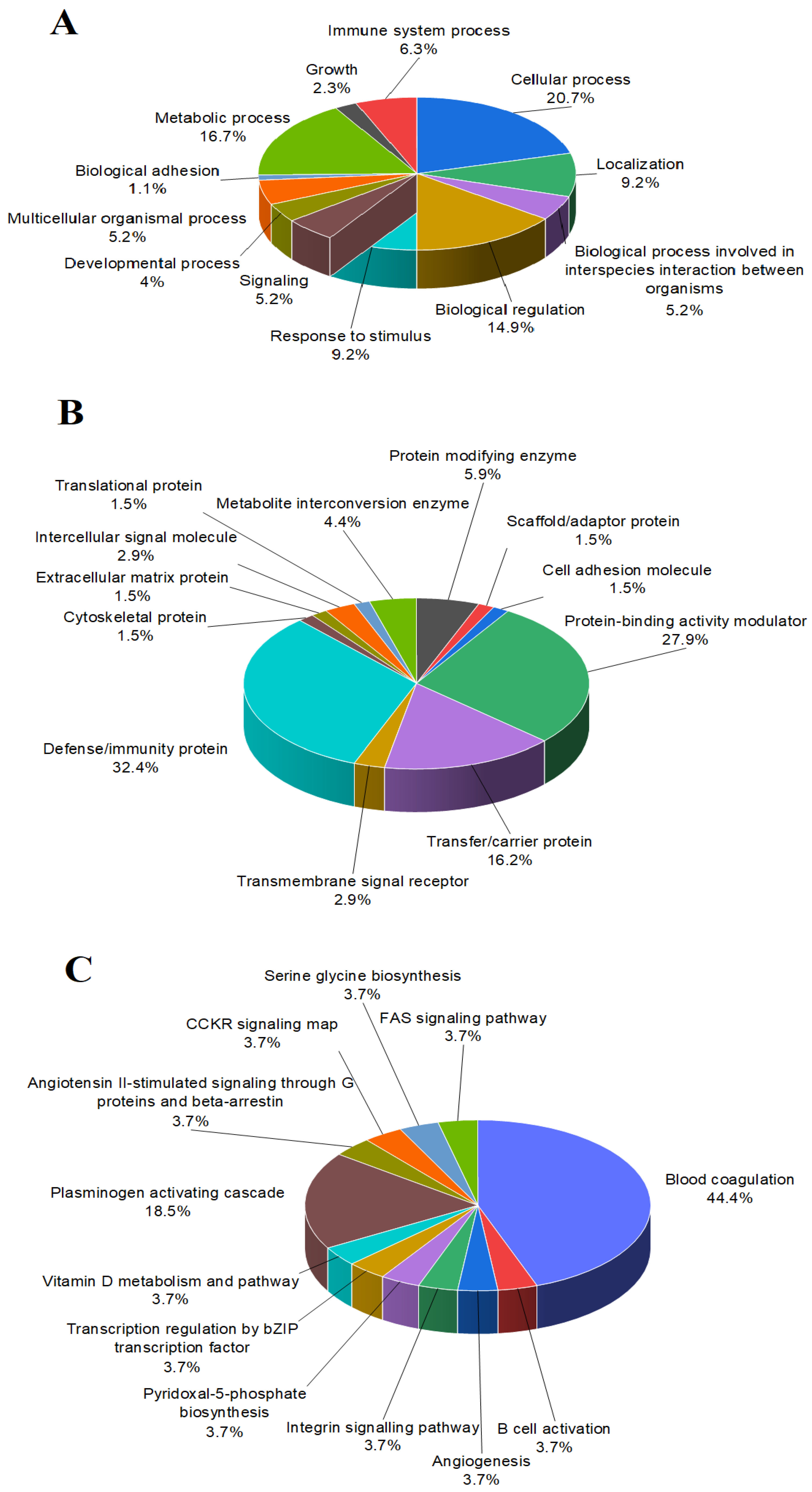
2.2. Classification of the Proteins in the Follicular Fluids
2.3. Relative Quantification of the Identified Proteins
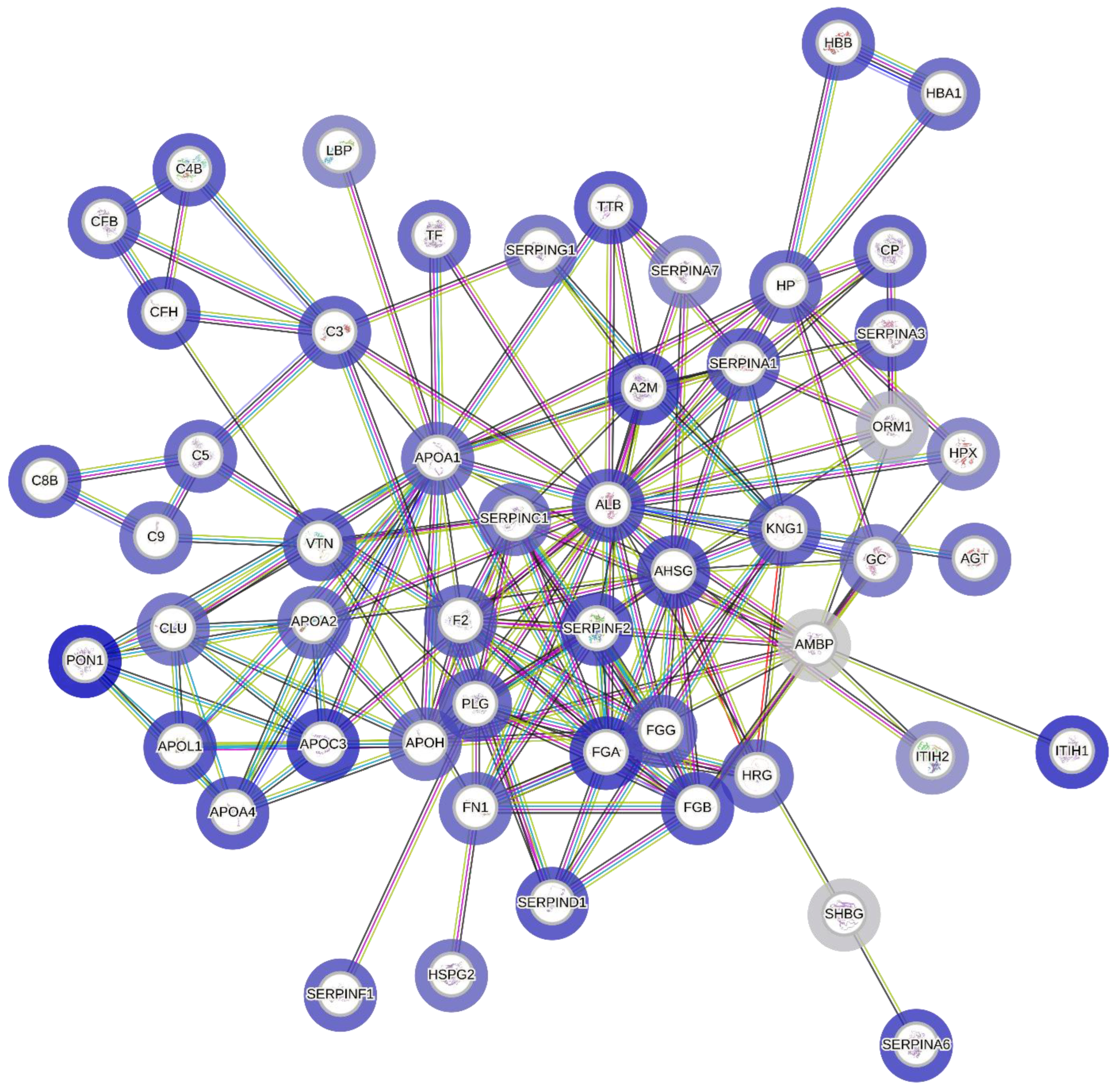
2.4. Protein-Protein Interactions (PPIs)
2.5. Functional Enrichment Analysis
3.6. Quantitative and Statistical Analysis of the Selected Proteins
2.6.1. Comparison of the Protein Concentrations Based on the Outcome
2.6.2. Comparison of Protein Concentrations Based on the Age of the Patients
2.6.3. Comparison of the Protein Concentrations Based on the BMI
3. Discussion
4. Materials and Methods
4.1. Patient Enrollment
4.2. Follicular Fluid Sample Collection
4.3. Chemicals
4.3.1. Sample Preparation for HPLC/MS Measurement
4.3.2. Parameters of the HPLC/MS Method
4.4. Measurement of ApoA1, Haptoglobin and HDL Cholesterol
4.5. Data Analysis
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgements
Conflicts of Interest
References
- F. Zegers-Hochschild et al., “The International Glossary on Infertility and Fertility Care, 2017,” Fertil Steril, vol. 108, no. 3, pp. 393–406, Sep. 2017. [CrossRef]
- M. Vander Borght and C. Wyns, “Fertility and infertility: Definition and epidemiology,” Clinical Biochemistry, vol. 62. Elsevier Inc., pp. 2–10, Dec. 01, 2018. [CrossRef]
- G. Collodel et al., “Follicular Fluid Components in Reduced Ovarian Reserve, Endometriosis, and Idiopathic Infertility,” Int J Mol Sci, vol. 24, no. 3, Feb. 2023. [CrossRef]
- I. Kosteria, A. K. Anagnostopoulos, C. Kanaka-Gantenbein, G. P. Chrousos, and G. T. Tsangaris, “The use of proteomics in assisted reproduction,” In Vivo, vol. 31, no. 3. International Institute of Anticancer Research, pp. 267–283, May 01, 2017. [CrossRef]
- S. Al-Amrani, Z. Al-Jabri, A. Al-Zaabi, J. Alshekaili, and M. Al-Khabori, “Proteomics: Concepts and applications in human medicine,” World J Biol Chem, vol. 12, no. 5, pp. 57–69, Sep. 2021. [CrossRef]
- M. L. Hennet and C. M. H. Combelles, “The antral follicle: A microenvironment for oocyte differentiation,” International Journal of Developmental Biology, vol. 56, no. 10–12, pp. 819–831, 2012. [CrossRef]
- A. T. Brinca et al., “Follicular Fluid: A Powerful Tool for the Understanding and Diagnosis of Polycystic Ovary Syndrome,” Biomedicines, vol. 10, no. 6. MDPI, Jun. 01, 2022. [CrossRef]
- A. E. Lewandowska, K. Macur, P. Czaplewska, J. Liss, K. Łukaszuk, and S. Ołdziej, “Qualitative and Quantitative Analysis of Proteome and Peptidome of Human Follicular Fluid Using Multiple Samples from Single Donor with LC-MS and SWATH Methodology,” J Proteome Res, vol. 16, no. 8, pp. 3053–3067, Aug. 2017. [CrossRef]
- L. Bianchi et al., “Protein pathways working in human follicular fluid: The future for tailored IVF?,” Expert Reviews in Molecular Medicine, vol. 18. Cambridge University Press, Jan. 18, 2016. [CrossRef]
- G. Mariani and J. Bellver, “Proteomics and metabolomics studies and clinical outcomes,” in Reproductomics: The -Omics Revolution and Its Impact on Human Reproductive Medicine, Elsevier, 2018, pp. 147–170. [CrossRef]
- X. Zhang, T. Wang, J. Song, J. Deng, and Z. Sun, “Study on follicular fluid metabolomics components at different ages based on lipid metabolism,” Reproductive Biology and Endocrinology, vol. 18, no. 1, May 2020. [CrossRef]
- M. G. Da Broi, V. S. I. Giorgi, F. Wang, D. L. Keefe, D. Albertini, and P. A. Navarro, “Influence of follicular fluid and cumulus cells on oocyte quality: Clinical implications,” J Assist Reprod Genet, vol. 35, no. 5, pp. 735–751, Mar. 2018. [CrossRef]
- M. Hashemitabar, M. Bahmanzadeh, A. Mostafaie, M. Orazizadeh, M. Farimani, and R. Nikbakht, “A proteomic analysis of human follicular fluid: Comparison between younger and older women with normal FSH levels,” Int J Mol Sci, vol. 15, no. 10, pp. 17518–17540, Sep. 2014. [CrossRef]
- E. C. A. Porta, M. Balestrieri, M. Bianco, R. Picone, C. De Stefano, and P. Abrescia, “Haptoglobin transport into human ovarian follicles and its binding to apolipoprotein A-1,” Zygote, vol. 7, pp. 67–77, 1999.
- M. Balestrieri, L. Cigliano, M. L. De Simone, B. Dale, and P. Abrescia, “Haptoglobin inhibits lecithin-cholesterol acyltransferase in human ovarian follicular fluid,” Mol Reprod Dev, vol. 59, no. 2, pp. 186–191, 2001. [CrossRef]
- T. E. Willnow, A. Hammes, and S. Eaton, “Lipoproteins and their receptors in embryonic development: More than cholesterol clearance,” Development, vol. 134, no. 18. pp. 3239–3249, Sep. 2007. [CrossRef]
- L. M. Mains, L. Christenson, B. Yang, A. E. T. Sparks, S. Mathur, and B. J. Van Voorhis, “Identification of apolipoprotein A1 in the human embryonic secretome,” Fertil Steril, vol. 96, no. 2, 2011. [CrossRef]
- R. L. Stouffer, F. Xu, and D. M. Duffy, “Molecular control of ovulation and luteinization in the primate follicle,” 2007.
- M. Cherian-Shaw, M. Puttabyatappa, E. Greason, A. Rodriguez, C. A. Vandevoort, and C. L. Chaffin, “Expression of scavenger receptor-BI and low-density lipoprotein receptor and differential use of lipoproteins to support early steroidogenesis in luteinizing macaque granulosa cells,” Endocrinology, vol. 150, no. 2, pp. 957–965, Feb. 2009. [CrossRef]
- N. Argov, U. Moallem, and D. Sklan, “Lipid transport in the developing bovine follicle: Messenger RNA expression increases for selective uptake receptors and decreases for endocytosis receptors,” Biol Reprod, vol. 71, no. 2, pp. 479–485, Aug. 2004. [CrossRef]
- A. S. Bhale and K. Venkataraman, “Leveraging knowledge of HDLs major protein ApoA1: Structure, function, mutations, and potential therapeutics,” Biomedicine and Pharmacotherapy, vol. 154. Elsevier Masson s.r.l., Oct. 01, 2022. [CrossRef]
- F. Amjadi, R. Aflatoonian, S. H. Javanmard, B. Saifi, M. Ashrafi, and M. Mehdizadeh, “Apolipoprotein A1 as a novel anti-implantation biomarker in polycystic ovary syndrome: A case-control study,” Journal of Research in Medical Sciences, vol. 20, no. 11, pp. 1039–1045, Nov. 2015. [CrossRef]
- X. Chen, T. O. Scholl, T. P. Stein, R. A. Steer, and K. P. Williams, “Maternal circulating lipid profile during early pregnancy: Racial/ethnic differences and association with spontaneous preterm delivery,” Nutrients, vol. 9, no. 1, Jan. 2017. [CrossRef]
- P. Verma et al., “High Level of APOA1 in Blood and Maternal Fetal Interface Is Associated With Early Miscarriage,” Reproductive Sciences, vol. 26, no. 5, pp. 649–656, May 2019. [CrossRef]
- T. Rødgaard, P. M. H. Heegaard, and H. Callesen, “Non-invasive assessment of in-vitro embryo quality to improve transfer success,” Reproductive BioMedicine Online, vol. 31, no. 5. Elsevier Ltd, pp. 585–592, Nov. 01, 2015. [CrossRef]
- J. Nyalwidhe et al., “The search for biomarkers of human embryo developmental potential in IVF: A comprehensive proteomic approach,” Mol Hum Reprod, vol. 19, no. 4, pp. 250–263, Apr. 2013. [CrossRef]
- D. R. Deutsch et al., “Stage-specific proteome signatures in early bovine embryo development,” J Proteome Res, vol. 13, no. 10, pp. 4363–4376, Oct. 2014. [CrossRef]
- J. J. Brosens et al., “Proteomic analysis of endometrium from fertile and infertile patients suggests a role for apolipoprotein A-I in embryo implantation failure and endometriosis,” Mol Hum Reprod, vol. 16, no. 4, pp. 273–285, Dec. 2009. [CrossRef]
- J. Zheng, Q. Yin, J. Cao, and B. Zhang, “Obesity contributes more to increasing ApoB/ApoA1 ratio than hyperandrogenism in PCOS women aged 20-38 years in China,” Exp Ther Med, vol. 13, no. 4, pp. 1337–1342, Apr. 2017. [CrossRef]
- K. Kim, M. S. Bloom, R. W. Browne, E. M. Bell, R. M. Yucel, and V. Y. Fujimoto, “Associations between follicular fluid high density lipoprotein particle components and embryo quality among in vitro fertilization patients,” J Assist Reprod Genet, vol. 34, no. 1, pp. 1–10, Jan. 2017. [CrossRef]
- B. Jaspard, X. Collet, R. Barbaras, J. Manent, C. Vieu, and J. Parinaud, “Biochemical Characterization of Pre-1 High-Density Lipoprotein from Human Ovarian Follicular Fluid: Evidence for the Presence of a Lipid Core †, ‡,” 1996. [Online]. Available: https://pubs.acs.org/sharingguidelines.
- Jaspard B et al., “Structural and functional comparison of HDL from homologous human plasma and follicular fluid. A model for extravascular fluid,” Arterioscler Thromb Vasc Biol., pp. 1605–13, 1997. [CrossRef]
- A. Yesilaltay et al., “Effects of hepatic expression of the high-density lipoprotein receptor SR-BI on lipoprotein metabolism and female fertility,” Endocrinology, vol. 147, no. 4, pp. 1577–1588, Apr. 2006. [CrossRef]
- A. Arias, A. Quiroz, N. Santander, E. Morselli, and D. Busso, “Implications of High-Density Cholesterol Metabolism for Oocyte Biology and Female Fertility,” Frontiers in Cell and Developmental Biology, vol. 10. Frontiers Media S.A., Sep. 14, 2022. [CrossRef]
- B. J. Ansell et al., “Inflammatory/Antiinflammatory Properties of High-Density Lipoprotein Distinguish Patients from Control Subjects Better Than High-Density Lipoprotein Cholesterol Levels and Are Favorably Affected by Simvastatin Treatment,” Circulation, vol. 108, no. 22, pp. 2751–2756, Dec. 2003. [CrossRef]
- V. Y. Fujimoto, J. P. Kane, B. Y. Ishida, M. S. Bloom, and R. W. Browne, “High-density lipoprotein metabolism and the human embryo,” Human Reproduction Update, vol. 16, no. 1. pp. 20–38, Aug. 28, 2009. [CrossRef]
- R. W. Browne, M. S. Bloom, W. B. Shelly, A. J. Ocque, H. G. Huddleston, and V. Y. Fujimoto, “Follicular fluid high density lipoprotein-associated micronutrient levels are associated with embryo fragmentation during IVF,” J Assist Reprod Genet, vol. 26, no. 11–12, pp. 557–560, 2009. [CrossRef]
- T. Y. Tan, M. S. K. Lau, S. F. Loh, and H. H. Tan, “Female ageing and reproductive outcome in assisted reproduction cycles,” Singapore Med J, vol. 55, no. 6, pp. 305–309, 2014. [CrossRef]
- W. Wei, X. Zhang, B. Zhou, B. Ge, J. Tian, and J. Chen, “Effects of female obesity on conception, pregnancy and the health of offspring,” Frontiers in Endocrinology, vol. 13. Frontiers Media S.A., Aug. 11, 2022. [CrossRef]
- A. Pirnat, L. A. Deroo, R. Skjærven, and N. H. Morken, “Women’s prepregnancy lipid levels and number of children: A Norwegian prospective population-based cohort study,” BMJ Open, vol. 8, no. 6, Jun. 2018. [CrossRef]
- J. Song, S. Xiang, C. Pang, J. Guo, and Z. Sun, “Metabolomic alternations of follicular fluid of obese women undergoing in-vitro fertilization treatment,” Sci Rep, vol. 10, no. 1, Dec. 2020. [CrossRef]
- S. D. M. Valckx et al., “BMI-related metabolic composition of the follicular fluid of women undergoing assisted reproductive treatment and the consequences for oocyte and embryo quality,” Human Reproduction, vol. 27, no. 12, pp. 3531–3539, 2012. [CrossRef]
| Pregnant [Mean± SD] (n=15) |
Non-pregnant [Mean± SD] (n=15) |
|
|---|---|---|
| Age | 36.31±5.51 | 32.93±4.94 |
| BMI | 26.31±5.84 | 25.92±5.65 |
| Number of oocytes retrieved | 12.27±7.54 | 11.85±8.4 |
| Number of fertilized oocytes | 4.86±3.68 | 3.15±2.69 |
| Number of IVF cycles | 1.89±0.9 | 2.07±0.75 |
| Name of node (protein) | Node degree |
|---|---|
| ALB | 27 |
| ApoA1 | 18 |
| AHSG | 17 |
| FGA | 14 |
| APOH | 13 |
| PLG | 13 |
| AMBP | 12 |
| F2 | 12 |
| FGB | 11 |
| FGG | 11 |
| HP | 10 |
| A2M | 10 |
| SERPINC1 | 10 |
| Term description (Function) |
Count in network | Strength | False discovery rate |
|---|---|---|---|
| High-density lipoprotein particle receptor binding | 3 of 3 | 2.5 | 0.00018 |
| Phosphatidylcholine-sterol O-acyltransferase activator activity | 3 of 6 | 2.2 | 0.00067 |
| Apolipoprotein receptor binding | 2 of 6 | 2.02 | 0.0426 |
| Lipoprotein particle receptor binding | 5 of 30 | 1.72 | 2.56E-05 |
| Serine-type endopeptidase inhibitor activity | 16 of 98 | 1.71 | 9.09E-20 |
| Cholesterol transfer activity | 3 of 23 | 1.62 | 0.0156 |
| Endopeptidase inhibitor activity | 21 of 177 | 1.58 | 2.24E-23 |
| Complement binding | 3 of 26 | 1.56 | 0.0185 |
| Phosphatidylcholine binding | 3 of 29 | 1.52 | 0.0233 |
| Peptidase regulator activity | 22 of 227 | 1.49 | 2.28E-23 |
| Proteoglycan binding | 3 of 37 | 1.41 | 0.0426 |
| Cholesterol binding | 4 of 52 | 1.39 | 0.0067 |
| Steroid binding | 7 of 101 | 1.34 | 1.62E-05 |
| Enzyme inhibitor activity | 23 of 396 | 1.27 | 4.86E-20 |
| Chaperone binding | 6 of 108 | 1.25 | 0.00044 |
| Molecular carrier activity | 4 of 72 | 1.25 | 0.0181 |
| Glycosaminoglycan binding | 13 of 245 | 1.23 | 6.10E-10 |
| Heparin binding | 9 of 173 | 1.22 | 2.34E-06 |
| Antioxidant activity | 4 of 76 | 1.22 | 0.0205 |
| Extracellular matrix structural constituent | 6 of 131 | 1.16 | 0.0012 |
| Sulfur compound binding | 10 of 272 | 1.07 | 6.86E-06 |
| Protease binding | 5 of 135 | 1.07 | 0.016 |
| Enzyme regulator activity | 28 of 1239 | 0.86 | 8.74E-15 |
| Lipid binding | 15 of 796 | 0.78 | 8.08E-06 |
| Molecular function regulator activity | 30 of 1960 | 0.69 | 1.11E-11 |
| Signaling receptor binding | 23 of 1499 | 0.69 | 3.28E-08 |
| Protein binding | 40 of 7242 | 0.24 | 0.0022 |
| Pregnant [Mean± SD] (n=15) |
Non-pregnant [Mean± SD] (n=15) |
|
|---|---|---|
| Total protein (g/l) | 45.37±6.21 | 47.61±11.14 |
| Albumin (g/l) | 32.72±4.25 | 34.43±8.05 |
| ApoA1 (mg/dl) | 123.54±16.51 | 139.96±22.27 |
| HP (g/l) | 0.55±0.373 | 0.43±0.24 |
| HP/ApoA1 ratio | 0.46±0.29 | 0.32±0.26 |
| HDL-C (mmol/l) | 0.55±0.24 | 0.78±0.23 |
| HDL/ApoA1 ratio | 0.17±0.07 | 0.21±0.04 |
| Protein name | Parameter | p value |
|---|---|---|
| TP | Outcome | 0.595 |
| ALB | Outcome | 0.567 |
| HP | Outcome | 0.367 |
| ApoA1 | Outcome | 0.007 |
| HDL-C | Outcome | 0.010 |
| HDL-C/ApoA1 ratio | Outcome | 0.045 |
| HP/ApoA1 ratio | Outcome | 0.148 |
| TP | Age | 0.232 |
| ALB | Age | 0.267 |
| HP | Age | 0.439 |
| ApoA1 | Age | 0.325 |
| HDL | Age | 0.325 |
| TP | BMI | 0.846 |
| ALB | BMI | 0.559 |
| HP | BMI | 0.449 |
| ApoA1 | BMI | 0.268 |
| HDL | BMI | 0.503 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





