Submitted:
11 October 2023
Posted:
13 October 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
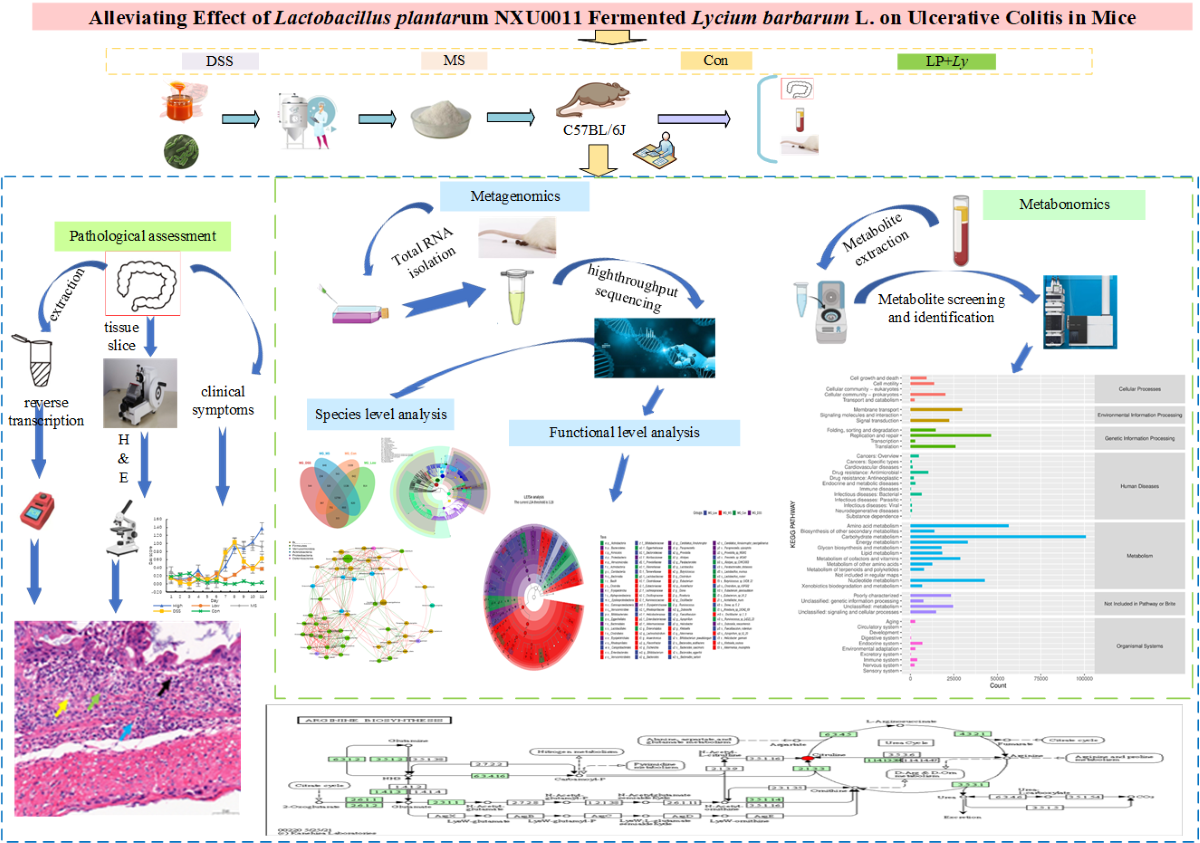
2. Materials and Methods
2.1. Preparation of LP+Ly
2.2. Animal Experimental Design
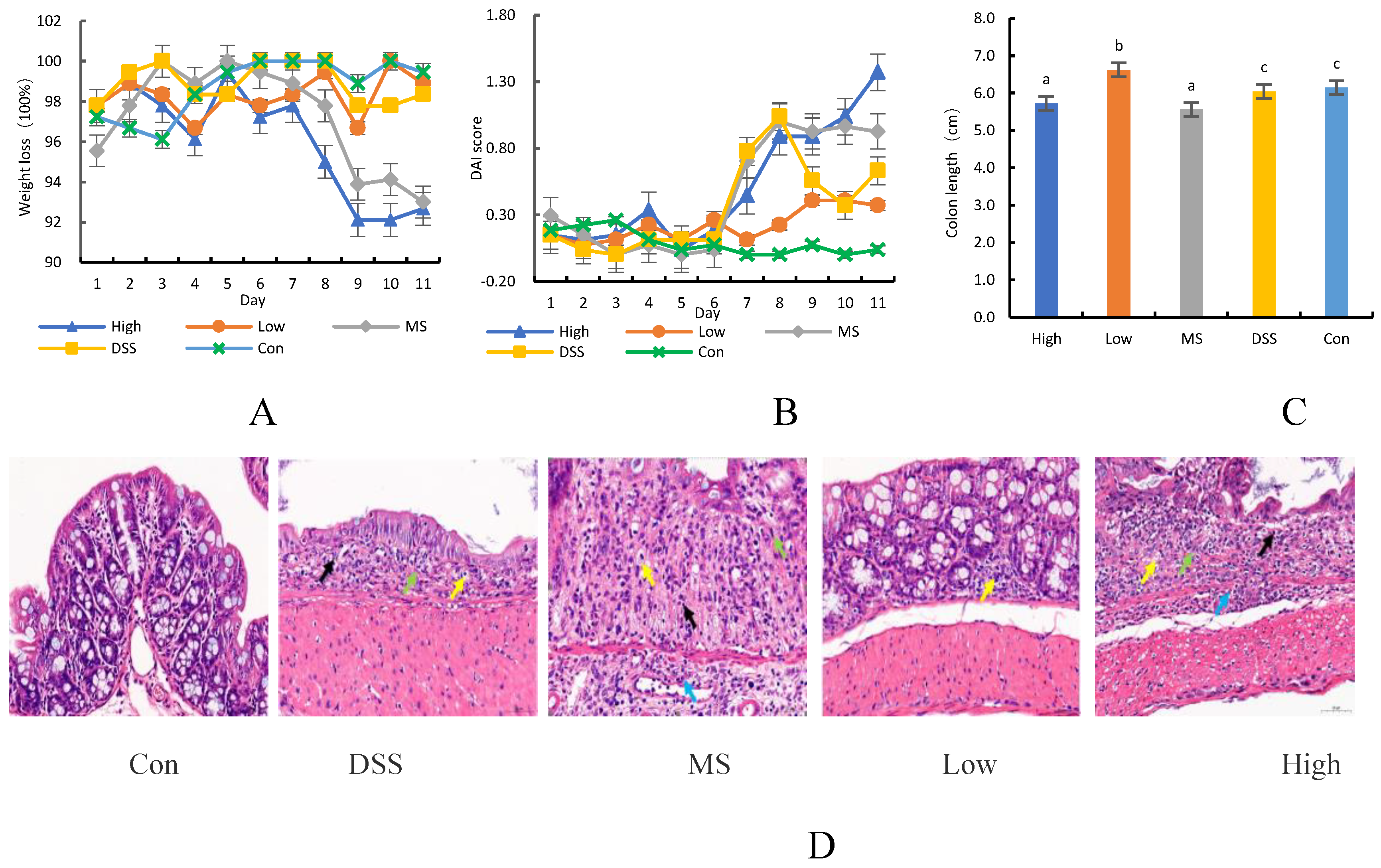
2.3. Disease Activity Index (DAI)
2.4. Histological Assessment
2.5. RNA Isolation and qRT-PCR
| Gene | Forward (5′-3′) | Reverse (5′-3′) |
|---|---|---|
| miR-214 | CGCTTTACAGCAGGCACAGA | TAAGGTTCATCACGACAGGTICAC |
| GAPDH | AAGGTCGGAGTCACCGGATT | CTGGAAGATGGTGATGGGATT |
2.6. Immunohistochemistry Staining
2.7. DNA Sequencing and Gut Microbiota Analysis
2.8. Plasma Metabolites Analysis via Untargeted Metabolomics
2.9. Statistical and Bioinformatics Analysis
3. Results
3.1. Protective Effect of LP+Ly on DSS-induced Colitis in Mice
3.2. Effect of LP+Ly on Cytokine Concentrations in the Colon
| Group | Number of samples (cases) | miR-214 | IL-6 | P-STAT3 |
|---|---|---|---|---|
| Con | 6 | 1.147±0.768 | 0.8007±0.3948 | 0.9345±0.9819 |
| DSS | 6 | 3.623±1.128 ## | 6.2169±1.8290 ## | 17.3432±5.2125 ## |
| MS | 6 | 1.197±0.686 * | 4.9281±2.3704 | 12.4073±3.3159 |
| High | 6 | 1.450±1.329 * | 2.8525±0.2716 ** | 5.8161±2.3814 ** |
| Low | 6 | 2.580±0.548 | 4.6217±1.2715 | 5.0924±1.8529 ** |
3.3. LP+Ly and the Structure of Gut Microbiota
3.3.1. Analysis of Intestinal Flora Diversity in Mice Following LP+Ly Intervention
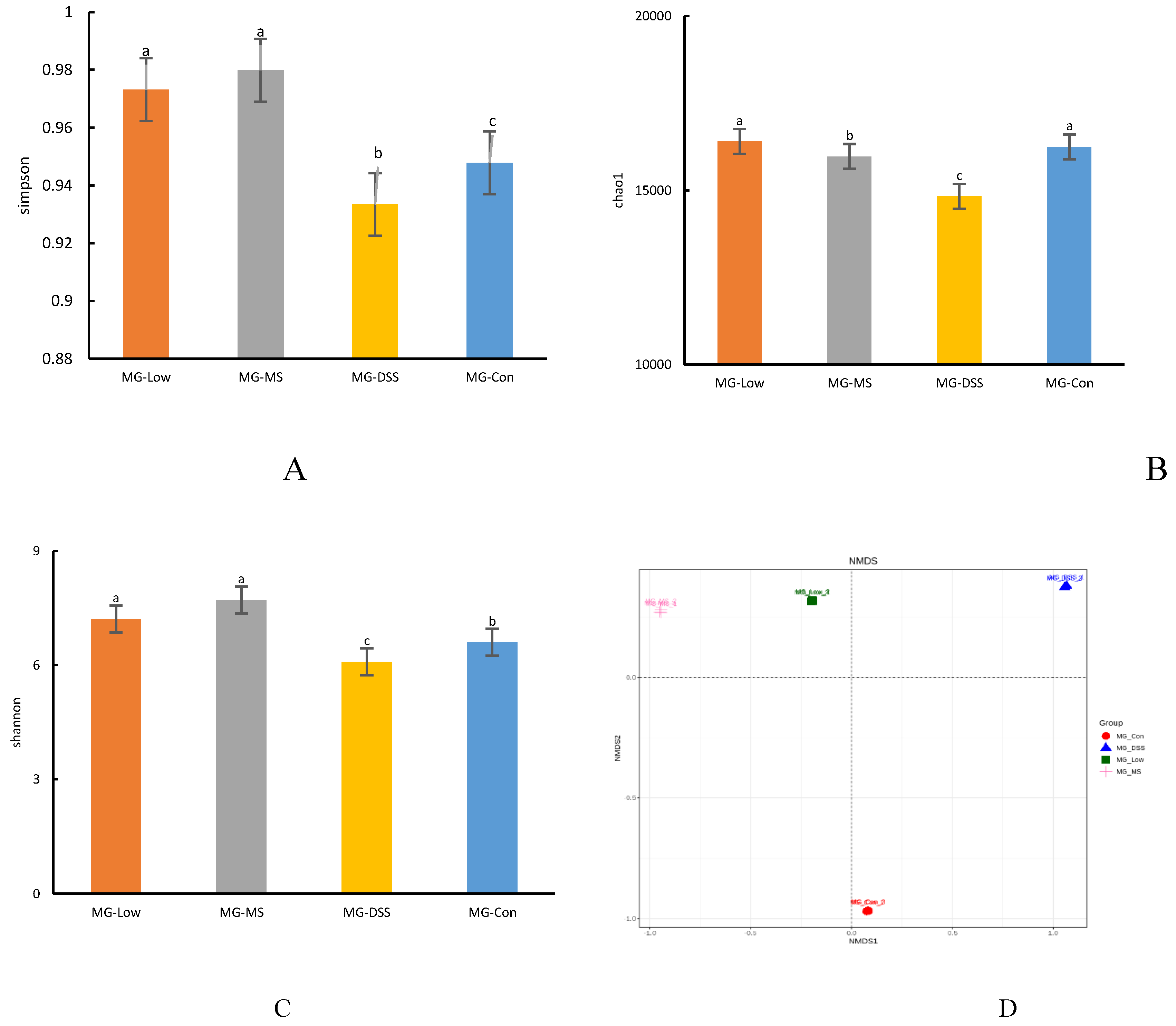
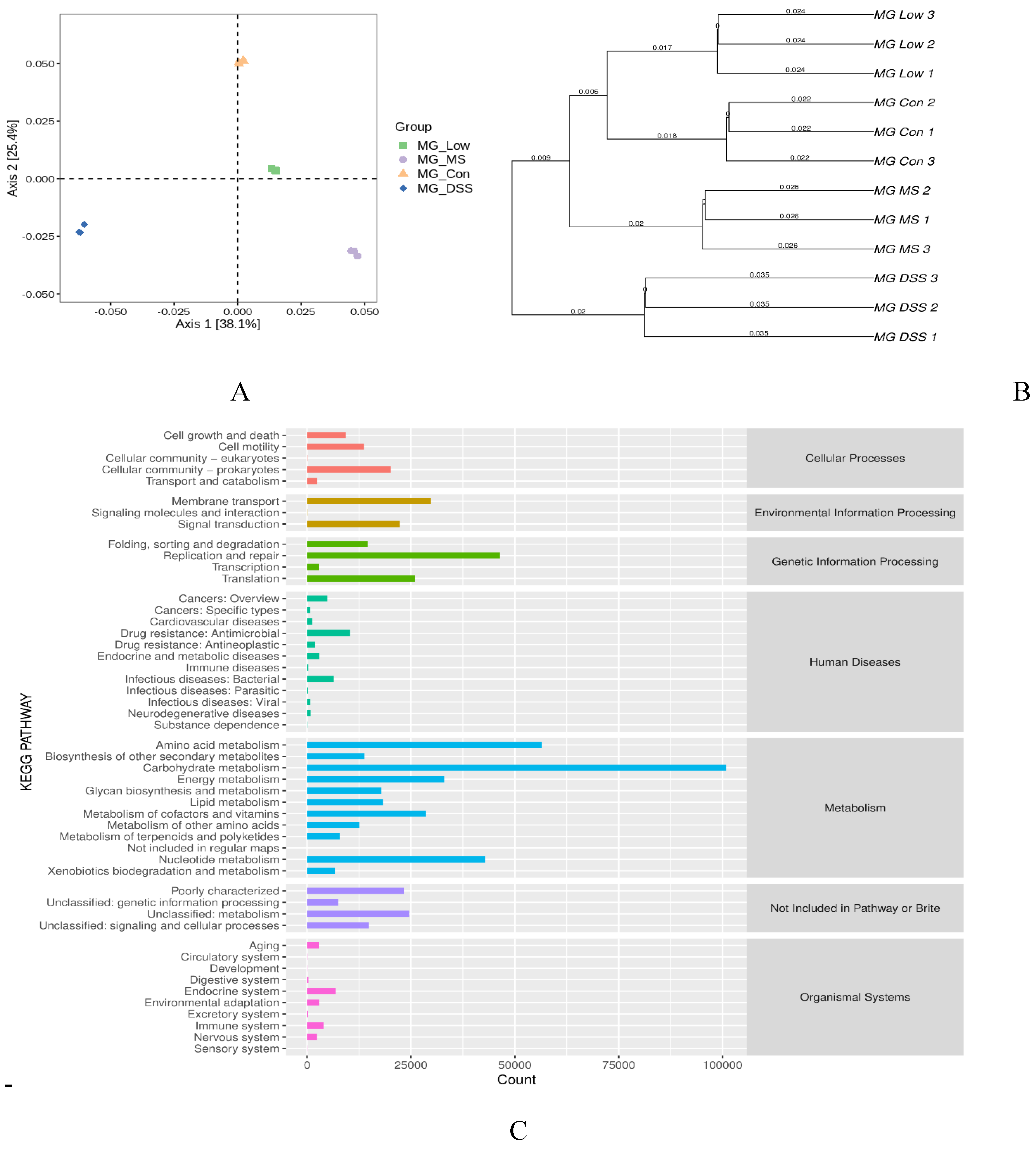
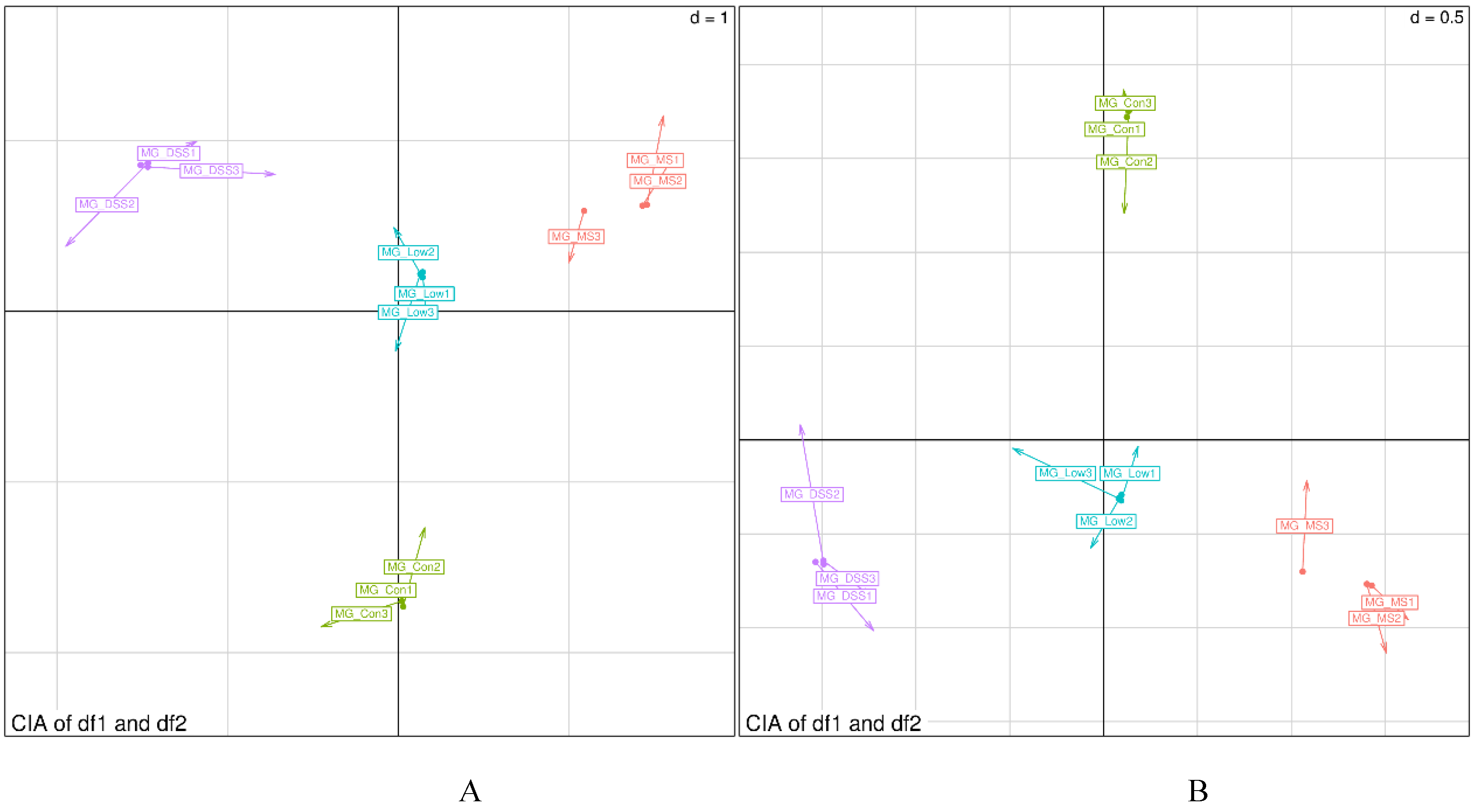
3.3.2. Impact of LP+Ly on the Structure of Gut Microbiota
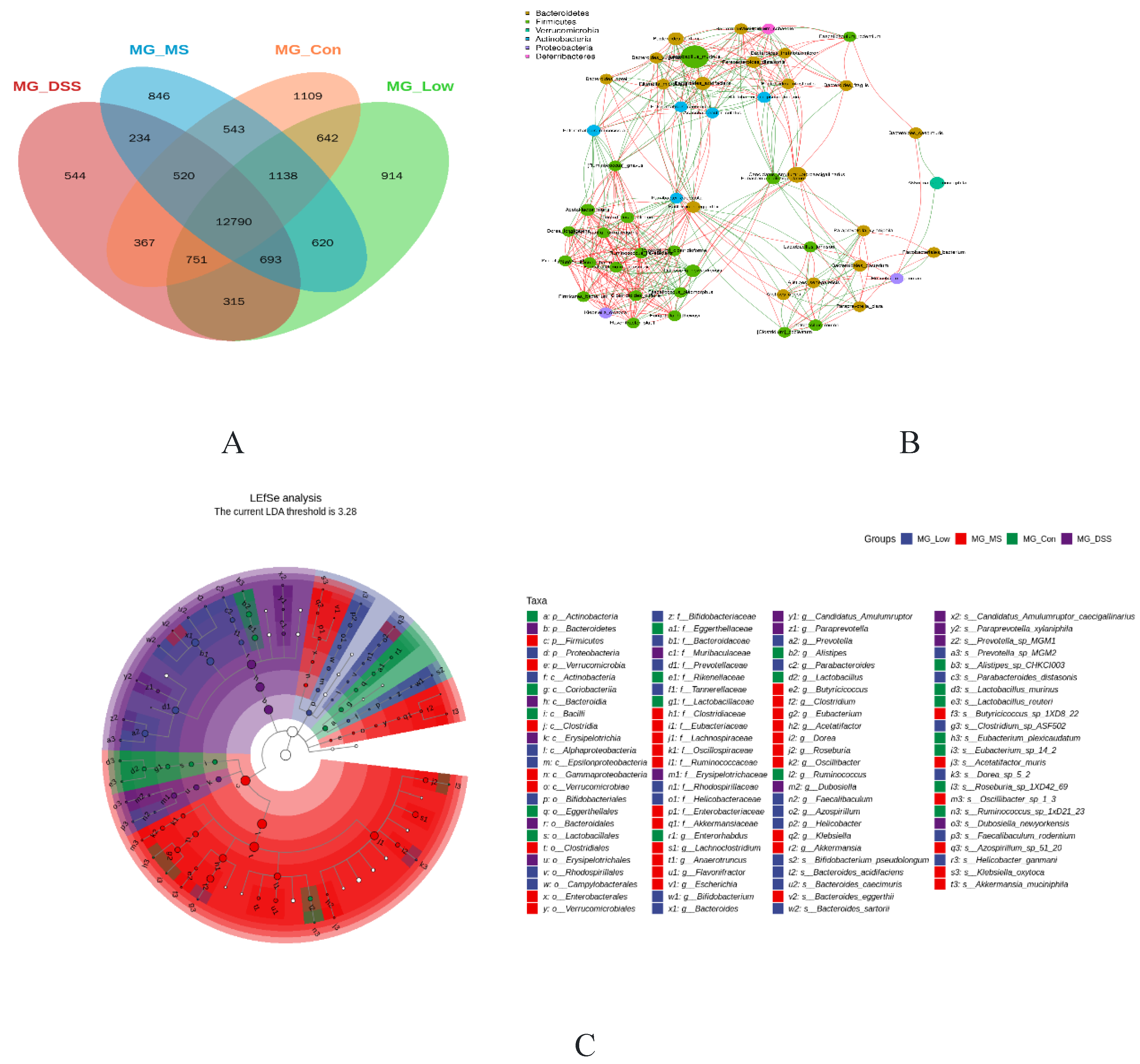
3.3.3. Analysis of the Effect of LP+Ly on the Functional Level of Intestinal Flora in Mice
3.4. Impact of LP+Ly on the Metabolome of Serum Samples
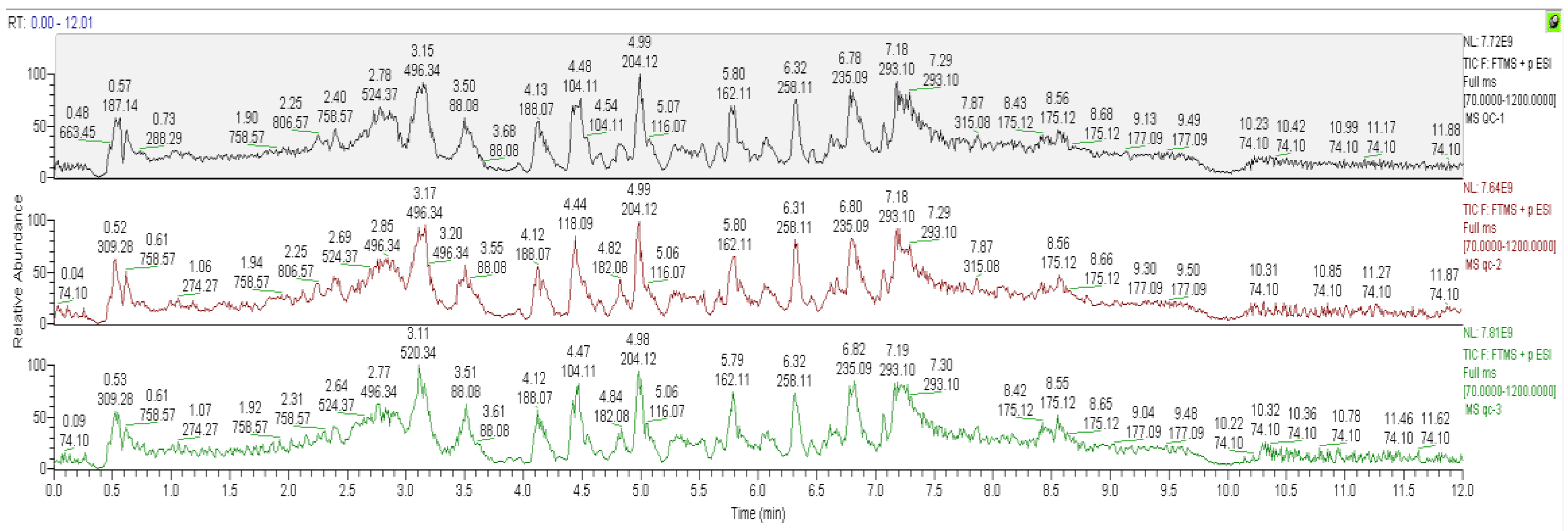
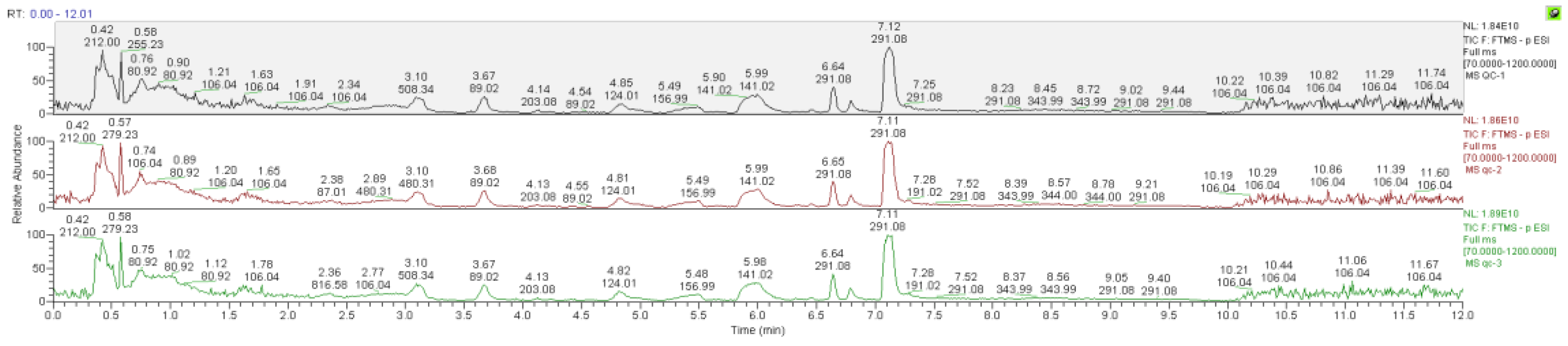
3.4.1. Data Quality Control (QC) Analysis
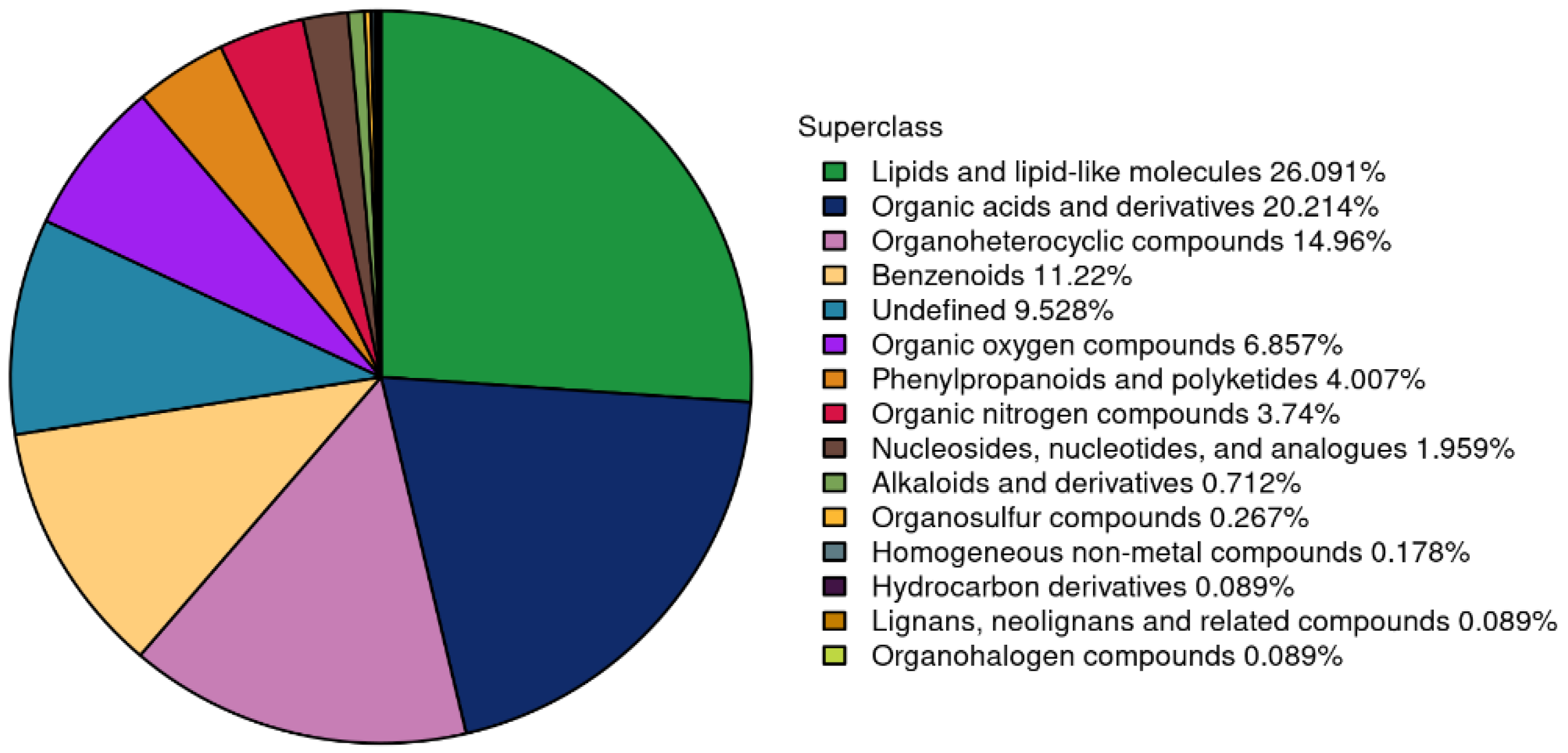
3.4.2. Summary of Plasma Metabolite Identification Results
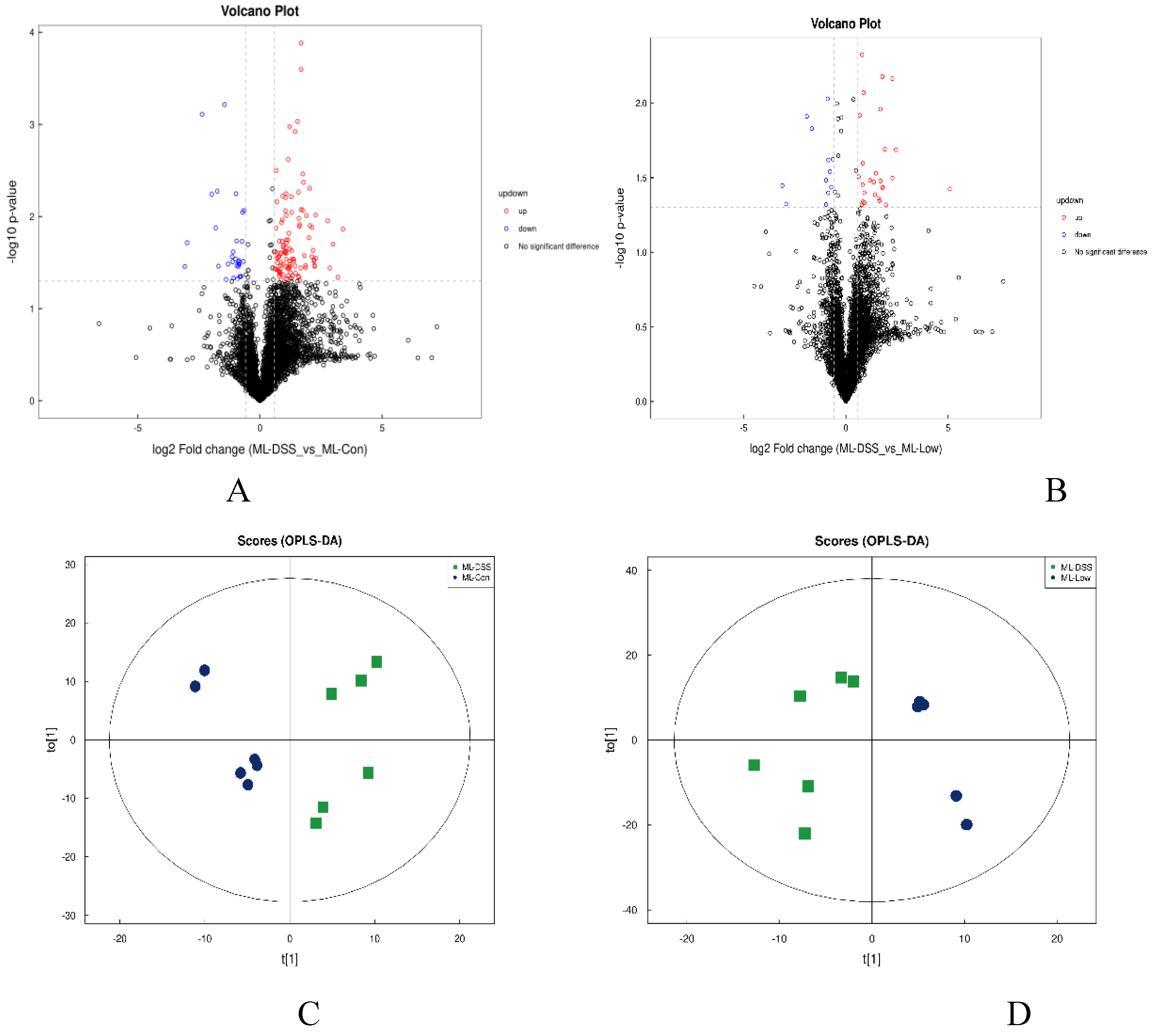
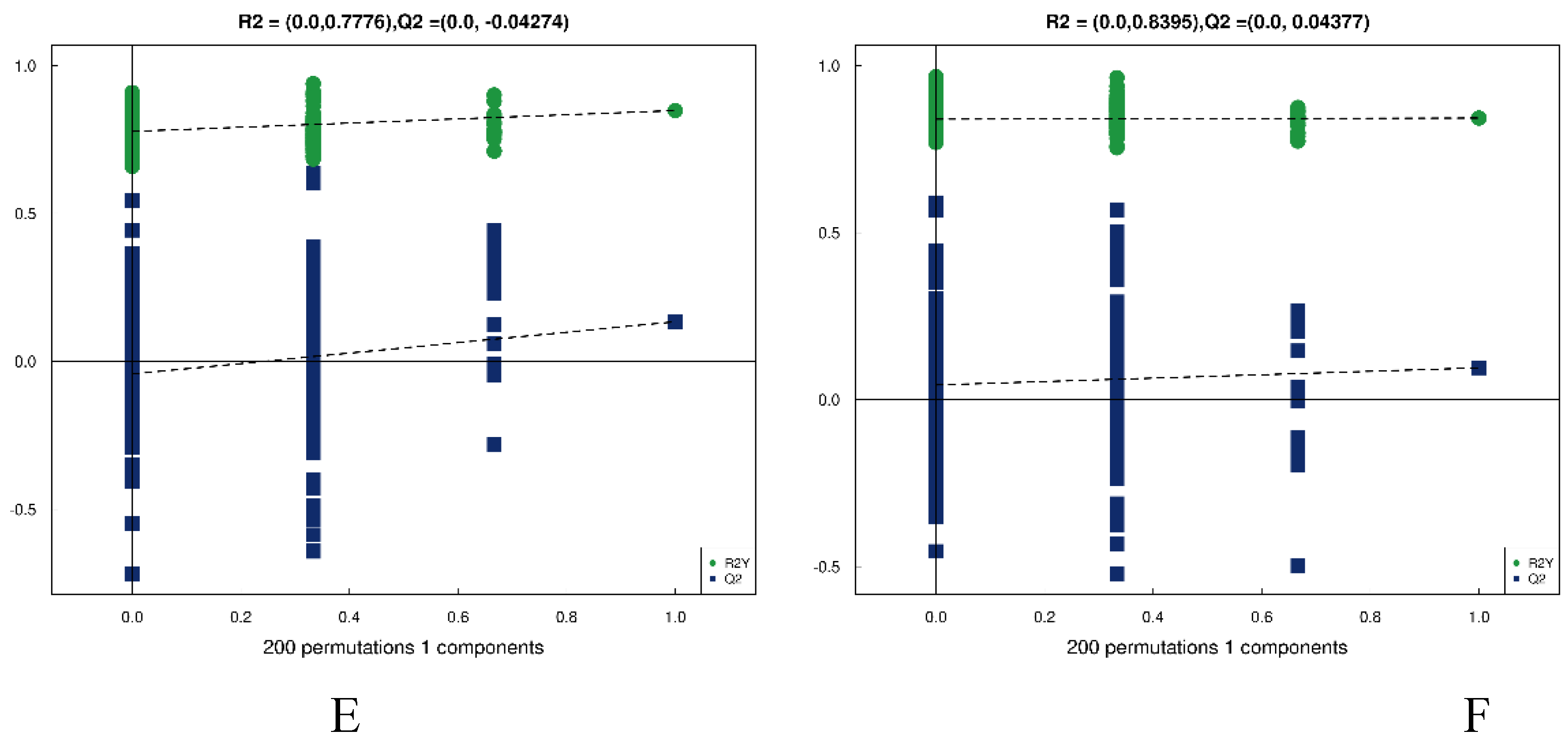
3.4.3. Analysis of Differences Between Groups of Plasma Metabolites and Permutation Test
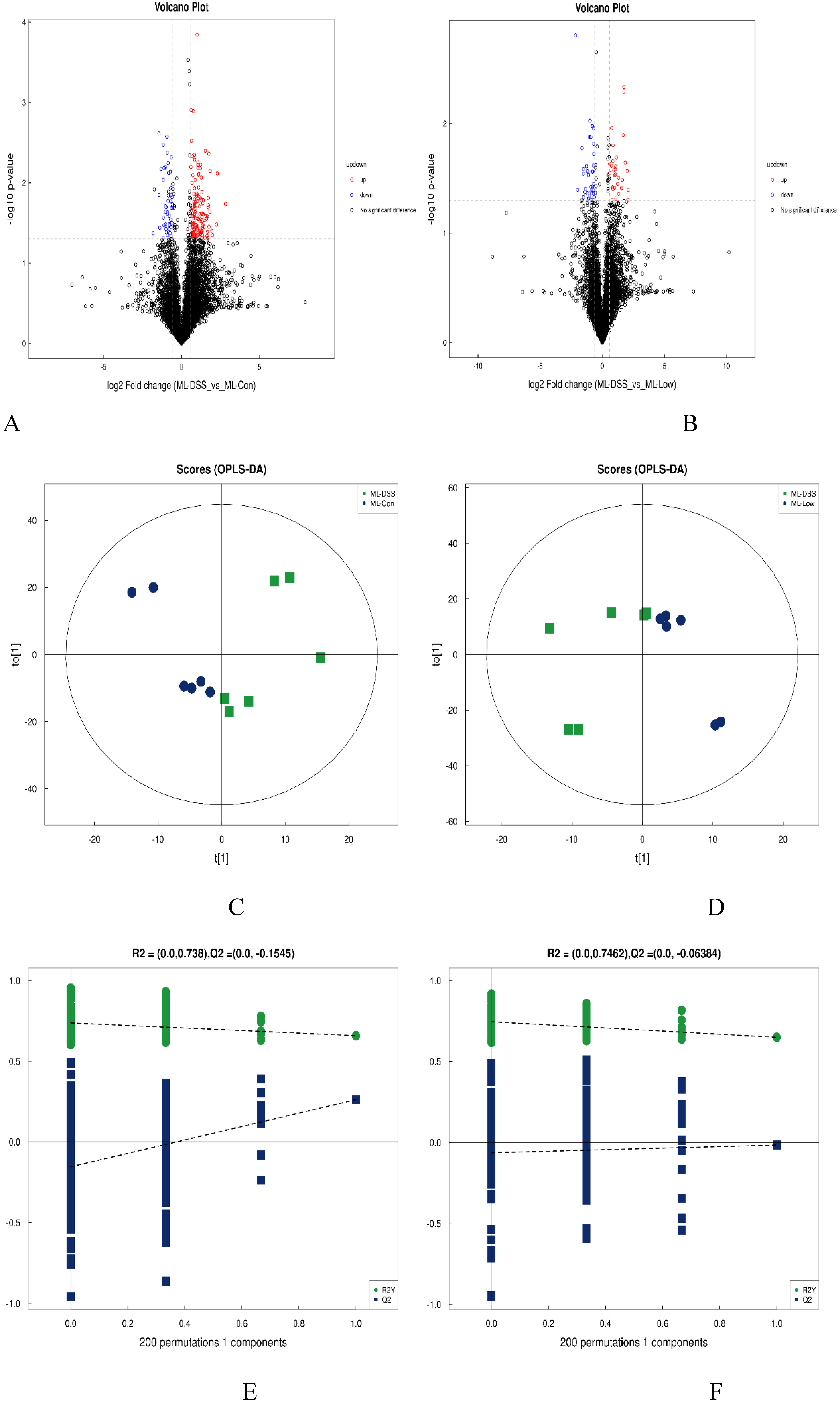
3.4.4. Screening of Differential Metabolites
| rt(s) | Name | VIP | FC | p-value | m/z | adduct |
|---|---|---|---|---|---|---|
| 476.16 | Fenarimol | 5.74 | 0.44 | 0.009 | 331.05 | [M+H]+ |
| 407.39 | L-citrulline | 2.34 | 1.46 | 0.033 | 198.08 | [M+Na]+ |
| 447.33 | Asp-Thr | 19.54 | 0.74 | 0.033 | 235.09 | [M+H]+ |
| 86.17 | Nudifloramide | 1.07 | 0.72 | 0.035 | 153.07 | [M+H]+ |
| 23.96 | Bergaptol | 6.86 | 2.44 | 0.006 | 201.02 | [M-H]- |
| 24.08 | 2-phosphonoethylphosphonic acid | 6.14 | 3.06 | 0.013 | 188.99 | [M-H]- |
| 331.83 | D-proline | 1.52 | 1.95 | 0.022 | 114.06 | [M-H]- |
| 23.94 | Pyrocatechol | 1.43 | 2.60 | 0.029 | 109.03 | [M-H]- |
| 25.02 | Daidzein 4’-sulfate | 1.03 | 4.61 | 0.030 | 333.01 | [M-H]- |
| 37.76 | 14-hydroxy-4z,7z,10z,12e,16z,19z-docosahexaenoic acid | 1.13 | 0.47 | 0.046 | 343.23 | [M-H]- |
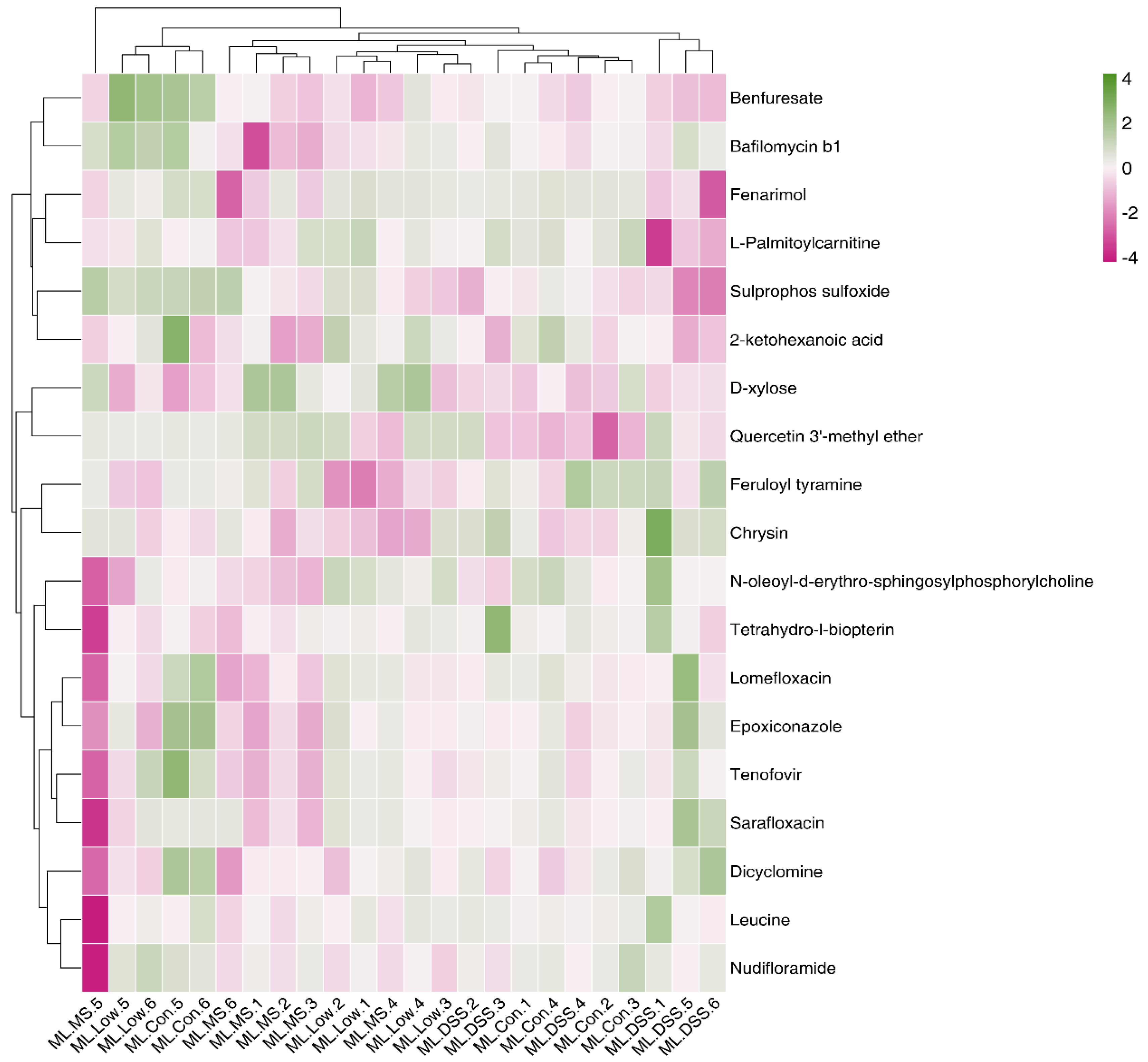
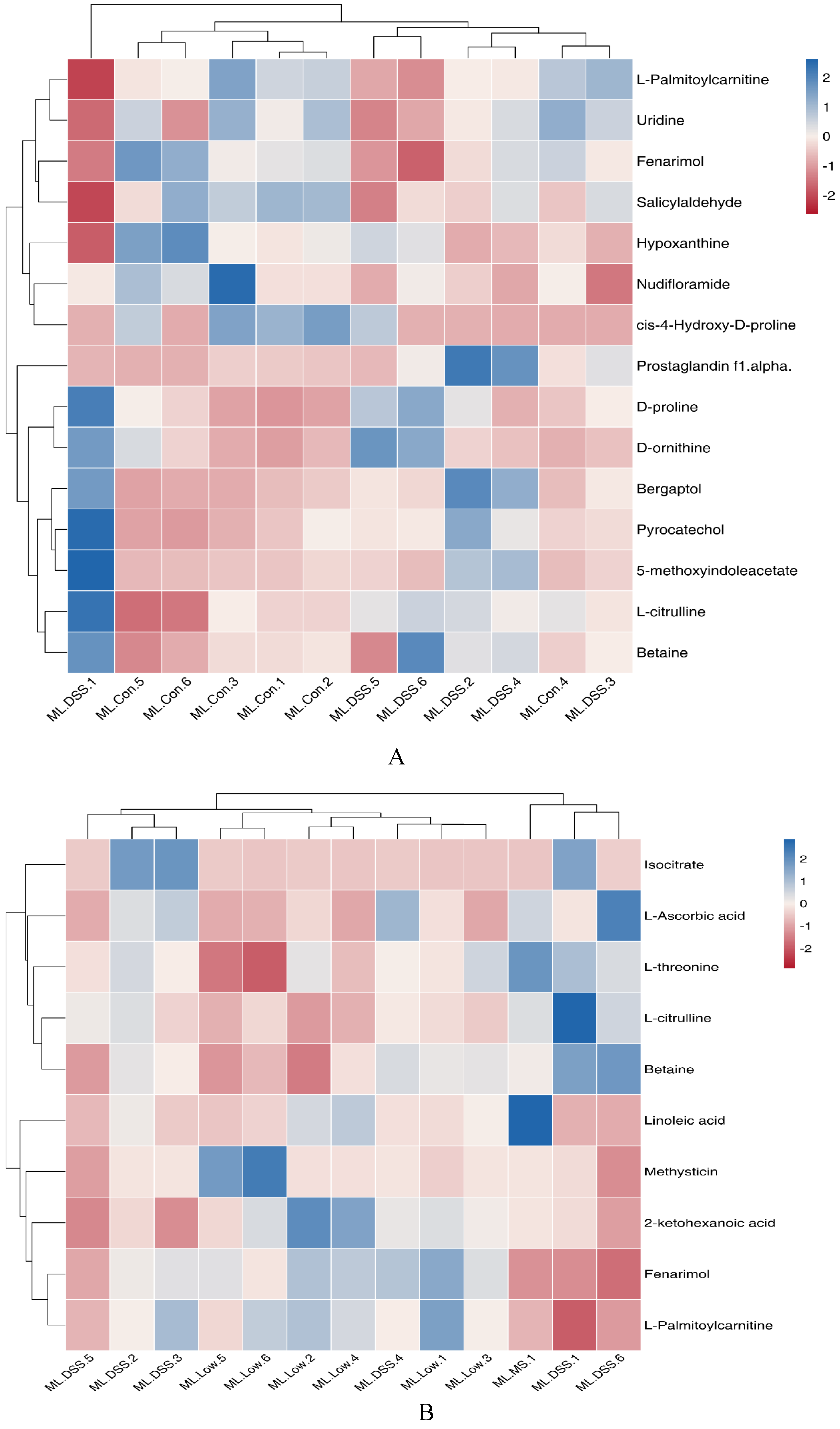
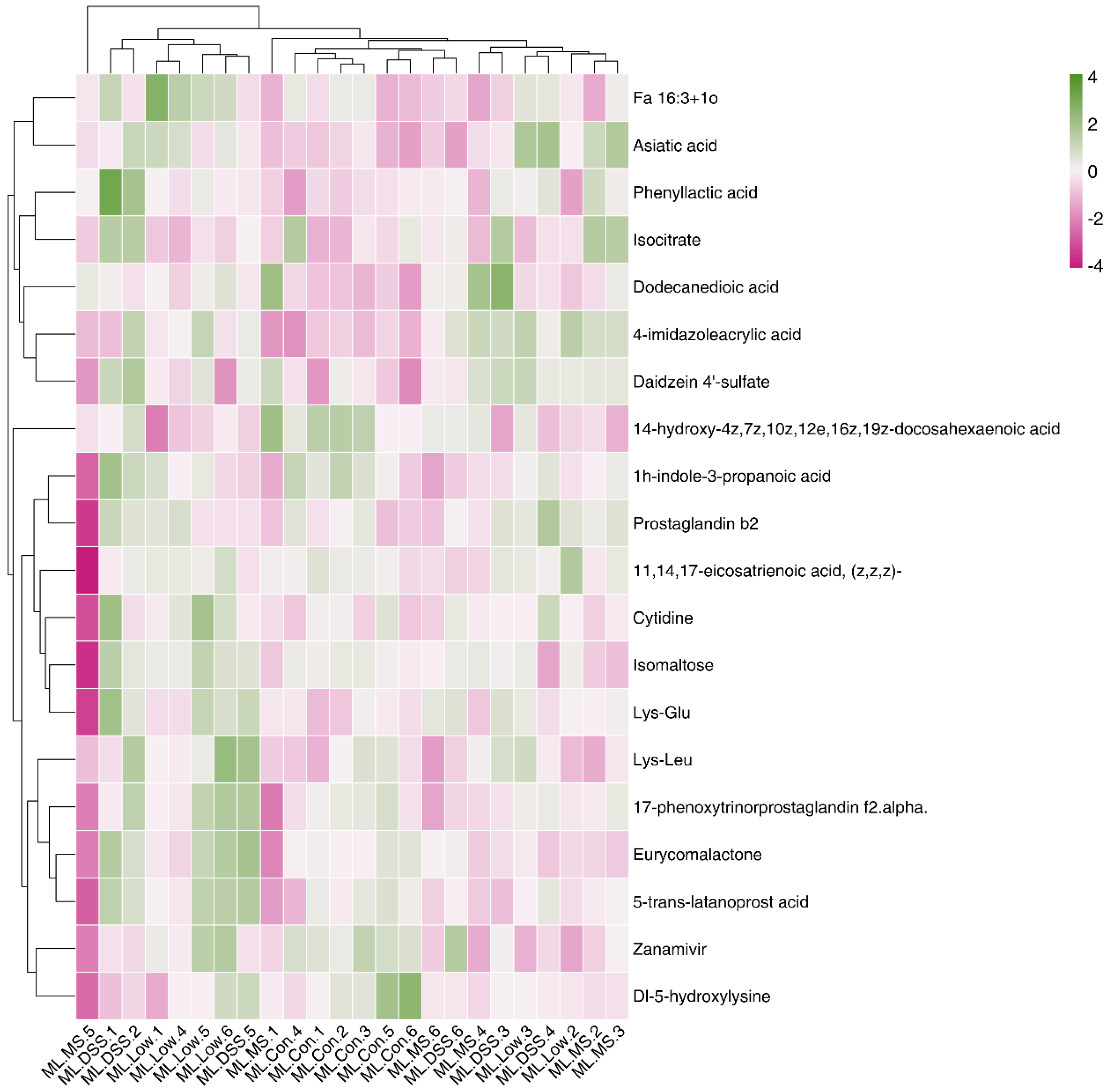
3.4.5. Cluster Analysis of Differential Metabolites
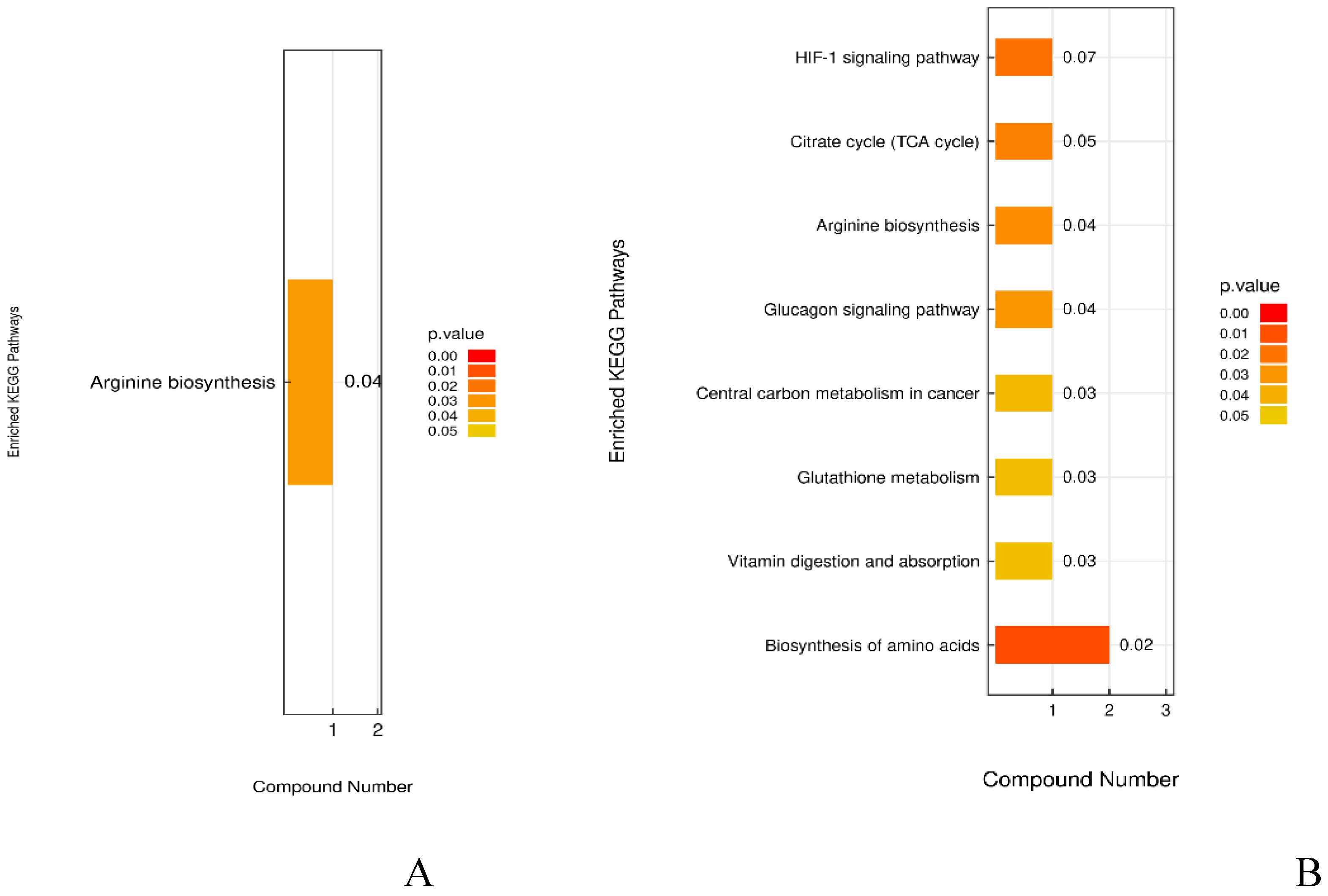
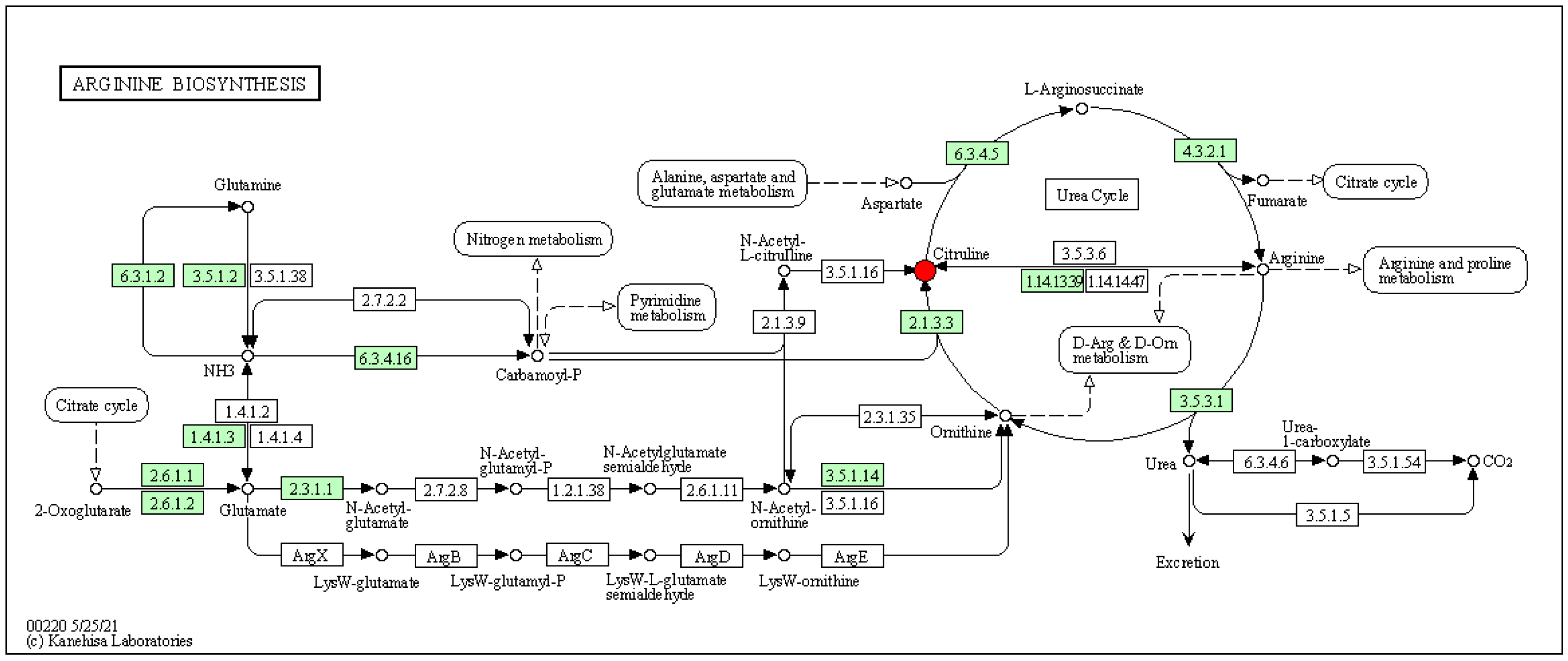
3.4.6. Analysis of the KEGG Metabolic Pathway with Differential Metabolites
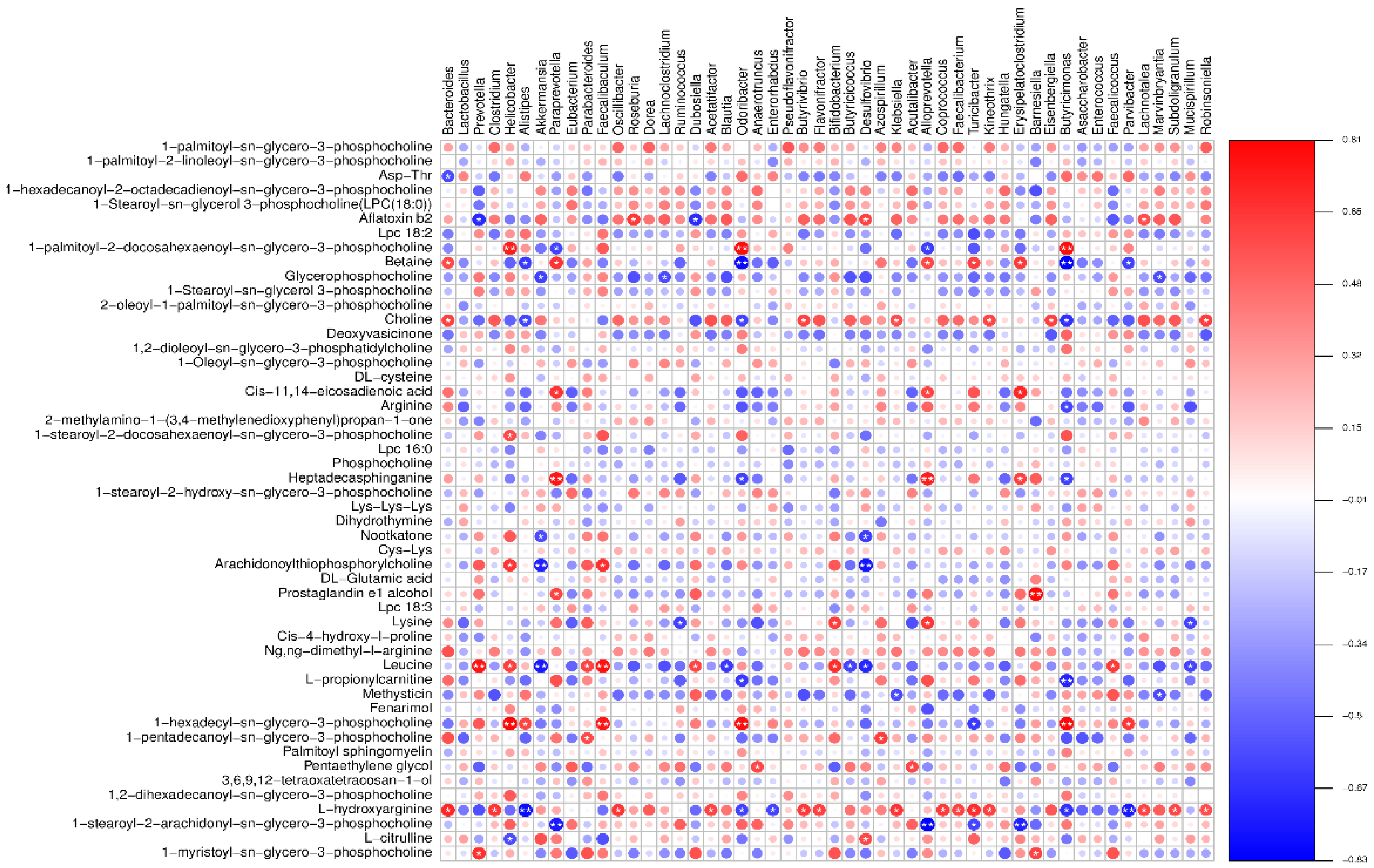
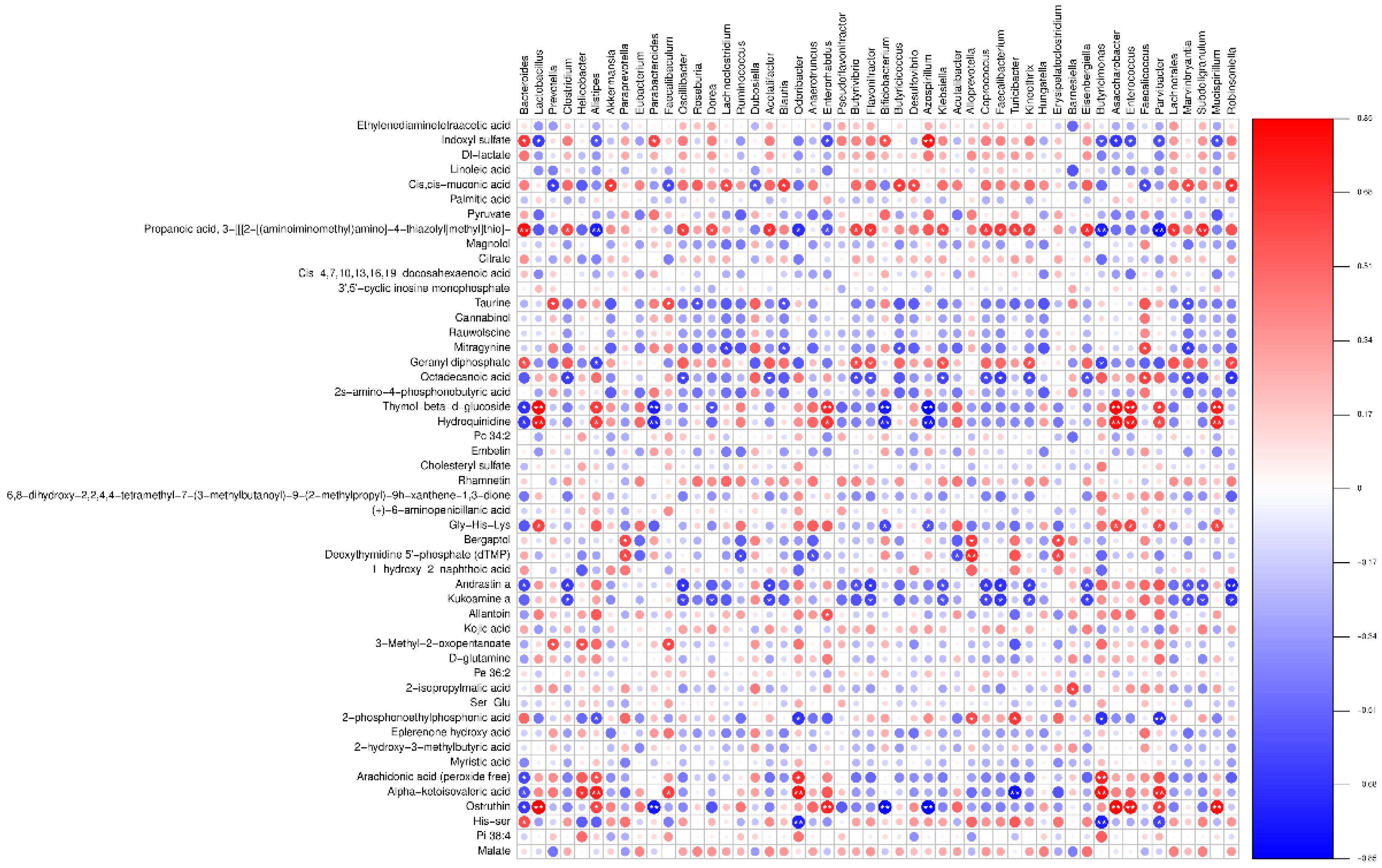
3.5. Combined Resonance Analysis of Intestinal Flora and Metabolites
4. Analysis and Discussion
5. Conclusion
Author Contributions
Funding
Conflicts of Interest
Appendix A
| Scoring/Points | Weight loss /% | Stool characteristics | Rectal bleeding (occult blood / gross blood in stool) |
|---|---|---|---|
| 0 | 0 | Normal | Occult blood |
| 1 | 1-5 | Stool consistency: Soft but formed | Occult blood |
| 2 | 6-10 | Stool consistency: Soft | Visible blood traces |
| 3 | 11-18 | Stool consistency: Very soft and loose | Visible significant blood |
| 4 | >18 | Watery diarrhea | Profuse bleeding |
| Reagent | 20ul System | Final concentration |
|---|---|---|
| 2X SYBR Green Mix | 10μL | 1X |
| RT Product | 2μL | |
| Bulge-LoopTM miRNA Forward Primer (5M) | 0.8μL | 200 nM |
| Bulge-LoopTM Reverse Primer (5M) | 0.8μL | 200 nM |
| RNase-free H2O | To 20μL |
| rt(s) | Name | VIP | FC | p-value | m/z | adduct |
|---|---|---|---|---|---|---|
| 510.32 | 2-ketohexanoic acid | 1.61 | 0.53 | 0.0133 | 131.08 | [M+H]+ |
| 407.39 | L-citrulline | 1.98 | 1.33 | 0.0332 | 198.08 | [M+Na]+ |
| 476.16 | Fenarimol | 4.00 | 0.55 | 0.0498 | 331.05 | [M+H]+ |
| 169.08 | L-Ascorbic acid | 2.10 | 5.44 | 0.021 | 197.01 | (M+Na-2H)- |
| 584.04 | Isocitrate | 3.28 | 33.75 | 0.038 | 173.01 | (M-H2O-H)- |
Appendix B
References
- Y. Rahbar Saadat, A. Yari Khosroushahi, B. Pourghassem Gargari, A comprehensive review of anticancer, immunomodulatory and health beneficial effects of the lactic acid bacteria exopolysaccharides, Carbohydr. Polym. 217 (2019) 79–89. https://doi.org/10.1016/j.carbpol.2019.04.025. [CrossRef]
- C. Cremon, M.R. Barbaro, M. Ventura, G. Barbara, Pre- and probiotic overview, Curr. Opin. Pharmacol. 43 (2018) 87–92. https://doi.org/10.1016/j.coph.2018.08.010. [CrossRef]
- S. Najafi, F. Sotoodehnejadnematalahi, M.M. Amiri, M.R. Pourshafie, M. Rohani, Prophylactic vs. Therapeutic Effect of Probiotics on the Inflammation Mediated by the NF-κB Pathway in Inflammatory Bowel Conditions, Biomedicines. 11 (2023) 1675. https://doi.org/10.3390/biomedicines11061675. [CrossRef]
- C.-M. Yang, M.-Y. Chien, L.-Y. Wang, C.-H. Chuang, C.-H. Chen, Goji Ferment Ameliorated Acetaminophen-Induced Liver Injury in vitro and in vivo, Probiotics Antimicrob. Proteins. (2022). https://doi.org/10.1007/s12602-022-09956-y. [CrossRef]
- K.M. Hooper, P.G. Barlow, C. Stevens, P. Henderson, Inflammatory Bowel Disease Drugs: A Focus on Autophagy, J. Crohns Colitis. 11 (2017) 118–127. https://doi.org/10.1093/ecco-jcc/jjw127. [CrossRef]
- Z.F. Dai, X.Y. Ma, R. Yang, H. Wang, D. Xu, J. Yang, X. Guo, S. Meng, R. Xu, Y. Li, Y. Xu, K. Li, X. Lin, Intestinal flora alterations in patients with ulcerative colitis and their association with inflammation, Exp. Ther. Med. 22 (2021) 1322. https://doi.org/10.3892/etm.2021.10757. [CrossRef]
- D. Bergemalm, E. Andersson, J. Hultdin, C. Eriksson, S.T. Rush, R. Kalla, A.T. Adams, Å.V. Keita, M. D’Amato, F. Gomollon, J. Jahnsen, P. Ricanek, J. Satsangi, D. Repsilber, P. Karling, J. Halfvarson, I.D. Arnott, M. Bayes, F. Bonfiglio, R.K. Boyapati, A. Carstens, C. Casén, E. Ciemniejewska, F.A. Dahl, T.E. Detlie, H.E. Drummond, G.S. Ekeland, D. Ekman, A.B. Frengen, M. Gullberg, I.G. Gut, M. Gut, S.C. Heath, F. Hjelm, H. Hjortswang, G.-T. Ho, D. Jonkers, J. Söderholm, N.A. Kennedy, C.W. Lees, T. Lindahl, M. Lindqvist, A. Merkel, E. Modig, A.E.F. Moen, H. Nilsen, E.R. Nimmo, C.L. Noble, N. Nordberg, K.R. O’Leary, A. Ocklind, C. Olbjørn, E. Pettersson, M. Pierik, Dominique, Systemic Inflammation in Preclinical Ulcerative Colitis, Gastroenterology. 161 (2021) 1526-1539.e9. https://doi.org/10.1053/j.gastro.2021.07.026. [CrossRef]
- D. Liu, F. Galvanin, Y. Yu, Formulation Screening and Freeze-Drying Process Optimization of Ginkgolide B Lyophilized Powder for Injection, AAPS PharmSciTech. 19 (2018) 541–550. https://doi.org/10.1208/s12249-017-0858-2. [CrossRef]
- Y. Chen, Y. Jin, C. Stanton, R.P. Ross, Z. Wang, J. Zhao, H. Zhang, B. Yang, W. Chen, Dose-response efficacy and mechanisms of orally administered CLA-producing Bifidobacterium breve CCFM683 on DSS-induced colitis in mice, J. Funct. Foods. 75 (2020) 104245. https://doi.org/10.1016/j.jff.2020.104245. [CrossRef]
- Z. Wu, S. Huang, T. Li, N. Li, D. Han, B. Zhang, Z.Z. Xu, S. Zhang, J. Pang, S. Wang, G. Zhang, J. Zhao, J. Wang, Gut microbiota from green tea polyphenol-dosed mice improves intestinal epithelial homeostasis and ameliorates experimental colitis, Microbiome. 9 (2021) 184. https://doi.org/10.1186/s40168-021-01115-9. [CrossRef]
- K. Wang, X. Jin, Q. Li, A.C.H.F. Sawaya, R.K. Le Leu, M.A. Conlon, L. Wu, F. Hu, Propolis from Different Geographic Origins Decreases Intestinal Inflammation and Bacteroides spp. Populations in a Model of DSS-Induced Colitis, Mol. Nutr. Food Res. 62 (2018) 1800080. https://doi.org/10.1002/mnfr.201800080. [CrossRef]
- B. Barberio, S. Facchin, I. Patuzzi, A.C. Ford, D. Massimi, G. Valle, E. Sattin, B. Simionati, E. Bertazzo, F. Zingone, E.V. Savarino, A specific microbiota signature is associated to various degrees of ulcerative colitis as assessed by a machine learning approach, Gut Microbes. 14 (2022) 2028366. https://doi.org/10.1080/19490976.2022.2028366. [CrossRef]
- L. Shang, H. Liu, H. Yu, M. Chen, T. Yang, X. Zeng, S. Qiao, Core Altered Microorganisms in Colitis Mouse Model: A Comprehensive Time-Point and Fecal Microbiota Transplantation Analysis, Antibiotics. 10 (2021) 643. https://doi.org/10.3390/antibiotics10060643. [CrossRef]
- M.L. Santoru, C. Piras, A. Murgia, V. Palmas, T. Camboni, S. Liggi, I. Ibba, M.A. Lai, S. Orrù, S. Blois, A.L. Loizedda, J.L. Griffin, P. Usai, P. Caboni, L. Atzori, A. Manzin, Cross sectional evaluation of the gut-microbiome metabolome axis in an Italian cohort of IBD patients, Sci. Rep. 7 (2017) 9523. https://doi.org/10.1038/s41598-017-10034-5. [CrossRef]
- Z. Wang, K. Guo, P. Gao, Q. Pu, P. Lin, S. Qin, N. Xie, J. Hur, C. Li, C. Huang, M. Wu, Microbial and genetic-based framework identifies drug targets in inflammatory bowel disease, Theranostics. 11 (2021) 7491–7506. https://doi.org/10.7150/thno.59196. [CrossRef]
- K.T. Wilson, Dietary Arginine Regulates Severity of Experimental Colitis and Affects the Colonic Microbiome, Front. Cell. Infect. Microbiol. 9 (2019). [CrossRef]
- H. Kahleova, S. Levin, N. Barnard, Cardio-Metabolic Benefits of Plant-Based Diets, Nutrients. 9 (2017) 848. https://doi.org/10.3390/nu9080848. [CrossRef]
- C. Polytarchou, D.W. Hommes, T. Palumbo, M. Hatziapostolou, M. Koutsioumpa, G. Koukos, A.E. Van Der Meulen-de Jong, A. Oikonomopoulos, W.K. Van Deen, C. Vorvis, O.B. Serebrennikova, E. Birli, J. Choi, L. Chang, P.A. Anton, P.N. Tsichlis, C. Pothoulakis, H.W. Verspaget, D. Iliopoulos, MicroRNA214 Is Associated With Progression of Ulcerative Colitis, and Inhibition Reduces Development of Colitis and Colitis-Associated Cancer in Mice, Gastroenterology. 149 (2015) 981-992.e11. https://doi.org/10.1053/j.gastro.2015.05.057. [CrossRef]
- F. Imhann, A. Vich Vila, M.J. Bonder, J. Fu, D. Gevers, M.C. Visschedijk, L.M. Spekhorst, R. Alberts, L. Franke, H.M. Van Dullemen, R.W.F. Ter Steege, C. Huttenhower, G. Dijkstra, R.J. Xavier, E.A.M. Festen, C. Wijmenga, A. Zhernakova, R.K. Weersma, Interplay of host genetics and gut microbiota underlying the onset and clinical presentation of inflammatory bowel disease, Gut. 67 (2018) 108–119. https://doi.org/10.1136/gutjnl-2016-312135. [CrossRef]
- F.A. Farraye, R.D. Odze, J. Eaden, S.H. Itzkowitz, AGA Technical Review on the Diagnosis and Management of Colorectal Neoplasia in Inflammatory Bowel Disease, Gastroenterology. 138 (2010) 746-774.e4. https://doi.org/10.1053/j.gastro.2009.12.035. [CrossRef]
- Y. Yang, G. Chen, Q. Yang, J. Ye, X. Cai, P. Tsering, X. Cheng, C. Hu, S. Zhang, P. Cao, Gut microbiota drives the attenuation of dextran sulphate sodium-induced colitis by Huangqin decoction, Oncotarget. 8 (2017) 48863–48874. https://doi.org/10.18632/oncotarget.16458. [CrossRef]
- Y. Kang, Y. Xue, M. Du, M.-J. Zhu, Preventive effects of Goji berry on dextran-sulfate-sodium-induced colitis in mice, J. Nutr. Biochem. 40 (2017) 70–76. https://doi.org/10.1016/j.jnutbio.2016.10.009. [CrossRef]
- M.E.V. Johansson, J.K. Gustafsson, J. Holmén-Larsson, K.S. Jabbar, L. Xia, H. Xu, F.K. Ghishan, F.A. Carvalho, A.T. Gewirtz, H. Sjövall, G.C. Hansson, Bacteria penetrate the normally impenetrable inner colon mucus layer in both murine colitis models and patients with ulcerative colitis, Gut. 63 (2014) 281–291. https://doi.org/10.1136/gutjnl-2012-303207. [CrossRef]
- M.P. Francino, The Gut Microbiome and Metabolic Health, Curr. Nutr. Rep. 6 (2017) 16–23. https://doi.org/10.1007/s13668-017-0190-1. [CrossRef]
- N. Castaño-Rodríguez, N.O. Kaakoush, W.S. Lee, H.M. Mitchell, Dual role of Helicobacter and Campylobacter species in IBD: a systematic review and meta-analysis, Gut. 66 (2017) 235–249. https://doi.org/10.1136/gutjnl-2015-310545. [CrossRef]
- T.W.-C. Yap, H.-M. Gan, Y.-P. Lee, A.H.-R. Leow, A.N. Azmi, F. Francois, G.I. Perez-Perez, M.-F. Loke, K.-L. Goh, J. Vadivelu, Helicobacter pylori Eradication Causes Perturbation of the Human Gut Microbiome in Young Adults, PLOS ONE. 11 (2016) e0151893. https://doi.org/10.1371/journal.pone.0151893. [CrossRef]
- D. Parada Venegas, M.K. De La Fuente, G. Landskron, M.J. González, R. Quera, G. Dijkstra, H.J.M. Harmsen, K.N. Faber, M.A. Hermoso, Short Chain Fatty Acids (SCFAs)-Mediated Gut Epithelial and Immune Regulation and Its Relevance for Inflammatory Bowel Diseases, Front. Immunol. 10 (2019) 277. https://doi.org/10.3389/fimmu.2019.00277. [CrossRef]
- R. Kumari, Fluctuations in butyrate-producing bacteria in ulcerative colitis patients of North India, World J. Gastroenterol. 19 (2013) 3404. https://doi.org/10.3748/wjg.v19.i22.3404. [CrossRef]
- K. Takahashi, A. Nishida, T. Fujimoto, M. Fujii, M. Shioya, H. Imaeda, O. Inatomi, S. Bamba, A. Andoh, M. Sugimoto, Reduced Abundance of Butyrate-Producing Bacteria Species in the Fecal Microbial Community in Crohn’s Disease, Digestion. 93 (2016) 59–65. https://doi.org/10.1159/000441768. [CrossRef]
- M. Ganji-Arjenaki, M. Rafieian-Kopaei, Probiotics are a good choice in remission of inflammatory bowel diseases: A meta analysis and systematic review, J. Cell. Physiol. 233 (2018) 2091–2103. https://doi.org/10.1002/jcp.25911. [CrossRef]
- Y. Derwa, D.J. Gracie, P.J. Hamlin, A.C. Ford, Systematic review with meta-analysis: the efficacy of probiotics in inflammatory bowel disease, Aliment. Pharmacol. Ther. 46 (2017) 389–400. https://doi.org/10.1111/apt.14203. [CrossRef]
- F. He, C. Wu, P. Li, N. Li, D. Zhang, Q. Zhu, W. Ren, Y. Peng, Functions and Signaling Pathways of Amino Acids in Intestinal Inflammation, BioMed Res. Int. 2018 (2018) 1–13. https://doi.org/10.1155/2018/9171905. [CrossRef]
- Z.H. Song, G. Tong, K. Xiao, L.F. Jiao, Y.L. Ke, C.H. Hu, L -Cysteine protects intestinal integrity, attenuates intestinal inflammation and oxidant stress, and modulates NF-κB and Nrf2 pathways in weaned piglets after LPS challenge, Innate Immun. 22 (2016) 152–161. https://doi.org/10.1177/1753425916632303. [CrossRef]
- S. Vidal-Lletjós, M. Beaumont, D. Tomé, R. Benamouzig, F. Blachier, A. Lan, Dietary Protein and Amino Acid Supplementation in Inflammatory Bowel Disease Course: What Impact on the Colonic Mucosa?, Nutrients. 9 (2017) 310. https://doi.org/10.3390/nu9030310. [CrossRef]
- S. Shin, H.M. Jeong, S.E. Chung, T.H. Kim, S.K. Thapa, D.Y. Lee, C.H. Song, J.Y. Lim, S.-M. Cho, K.-Y. Nam, W.-H. Kang, Y.-W. Choi, B.S. Shin, Simultaneous analysis of acetylcarnitine, proline, hydroxyproline, citrulline, and arginine as potential plasma biomarkers to evaluate NSAIDs-induced gastric injury by liquid chromatography–tandem mass spectrometry, J. Pharm. Biomed. Anal. 165 (2019) 101–111. https://doi.org/10.1016/j.jpba.2018.11.051. [CrossRef]
- F. Hugenholtz, W.M. De Vos, Mouse models for human intestinal microbiota research: a critical evaluation, Cell. Mol. Life Sci. 75 (2018) 149–160. https://doi.org/10.1007/s00018-017-2693-8. [CrossRef]
- V. Singh, B.S. Yeoh, B. Chassaing, X. Xiao, P. Saha, R. Aguilera Olvera, J.D. Lapek, L. Zhang, W.-B. Wang, S. Hao, M.D. Flythe, D.J. Gonzalez, P.D. Cani, J.R. Conejo-Garcia, N. Xiong, M.J. Kennett, B. Joe, A.D. Patterson, A.T. Gewirtz, M. Vijay-Kumar, Dysregulated Microbial Fermentation of Soluble Fiber Induces Cholestatic Liver Cancer, Cell. 175 (2018) 679-694.e22. https://doi.org/10.1016/j.cell.2018.09.004. [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




