1. Introduction
Crohn’s disease (CD) isimmune-mediated, chronic, recurrent disease from the group of inflammatory bowel diseases (IBD), its etiology is not understood. Urbanization increase, environmental degradation, nutrition quality decrease, high mental and psychological loads, all together lead to annual increase in morbidity of CD, and up to 25% of new cases are children and adolescents[
1,
2,
3,
4,
5,
6,
7]. CD course in children is more severe with development of forms that are resistant to medications or lead to surgical complications [
4,
5,
6,
7]. Deep ulcers, stenoses and fistulas are formed due to transmural lesions of the bowel wall [
5].
Specific feature of CD course is segmental damage in different parts of the gastrointestinal tract, thus, complications requiring surgery may occur in both small and large bowel. However, the most frequent CD localization (up to 70%) is the ileocecal region [
5,
6,
7].
Despite numerous publications in world literature about issues of surgical treatment of children with CD, many questions remain relevant in modern pediatric surgery [
8,
9,
10,
11]. The surgery timing is crucial, especially when medications (modern biological drugs included) do not cause persistent remission and in case of disease progression [
12,
13,
14]. Extent of surgery is defined by resection length and possibility of simultaneous forming of intestinal anastomosis or necessity of intestinal ostomy. The timing of gastrointestinal tract (GIT) continuity restoration is stable remission and opportunity for the next stage of surgical treatment [
4,
7,
15].
2. Materials and Methods
Cross-sectional, retrospective-prospective study of 64 children (39 boys (61%) and 25 girls (39%)) aged from 2 years 4 months to 17 years 5 months (median – 15) with complicated course of CD (strictures, infiltrates, and/or peritoneal abscess), or with refractory course of the disease, was carried out. All surgeries were performed in the Federal State Budgetary Institution "National Medical Research Center of Children’s Health" of the Ministry of Health of Russian Federation (Moscow, Russian Federation) from 2018 to 2021.
Clinical and laboratory diagnostics
We evaluated height-to-age and BMI-to-age ratio in all children prior to surgery via WHO AnthroPlus software. CD activity was evaluated via pediatric Crohn's disease activity index (PCDAI). Anemia degree, albumin levels, and C-reactive protein (as a marker of bacterial inflammation) were considered among laboratory tests.
Instrumental diagnostics
All patients underwent magnetic resonance enterography (MR-enterography) with intravenous contrast and oral mannitol administration thus we were able to diagnose inflammation in the intestinal wall and the presence of strictures in small intestine and ileocecal area. Additionally, we used GIT X-ray study with barium sulfate contrast to estimate the stenosis length and the presence of dilations near stenosis.
Endoscopic examination was performed to evaluate the prevalence of inflammation and to determine the stricture level. All children underwent ileocolonoscopy and esophagogastroduodenoscopy (EGD) with biopsy for histological examination. We evaluated the endoscopic activity of CD according to the ileocolonoscopy results via Simple Endoscopic Score for Crohn Disease (SES-CD).
We determined the extent of the proposed surgery according to the obtained data from laboratory and instrumental studies. The final decision on the possibility of performing simultaneous or staged surgical treatment was made intraoperatively and collectively together with gastroenterologists and pediatric surgeons according to the data from diagnostic laparoscopy, clinical data and results of laboratory and instrumental diagnostics on preoperative stage.
Surgical treatment
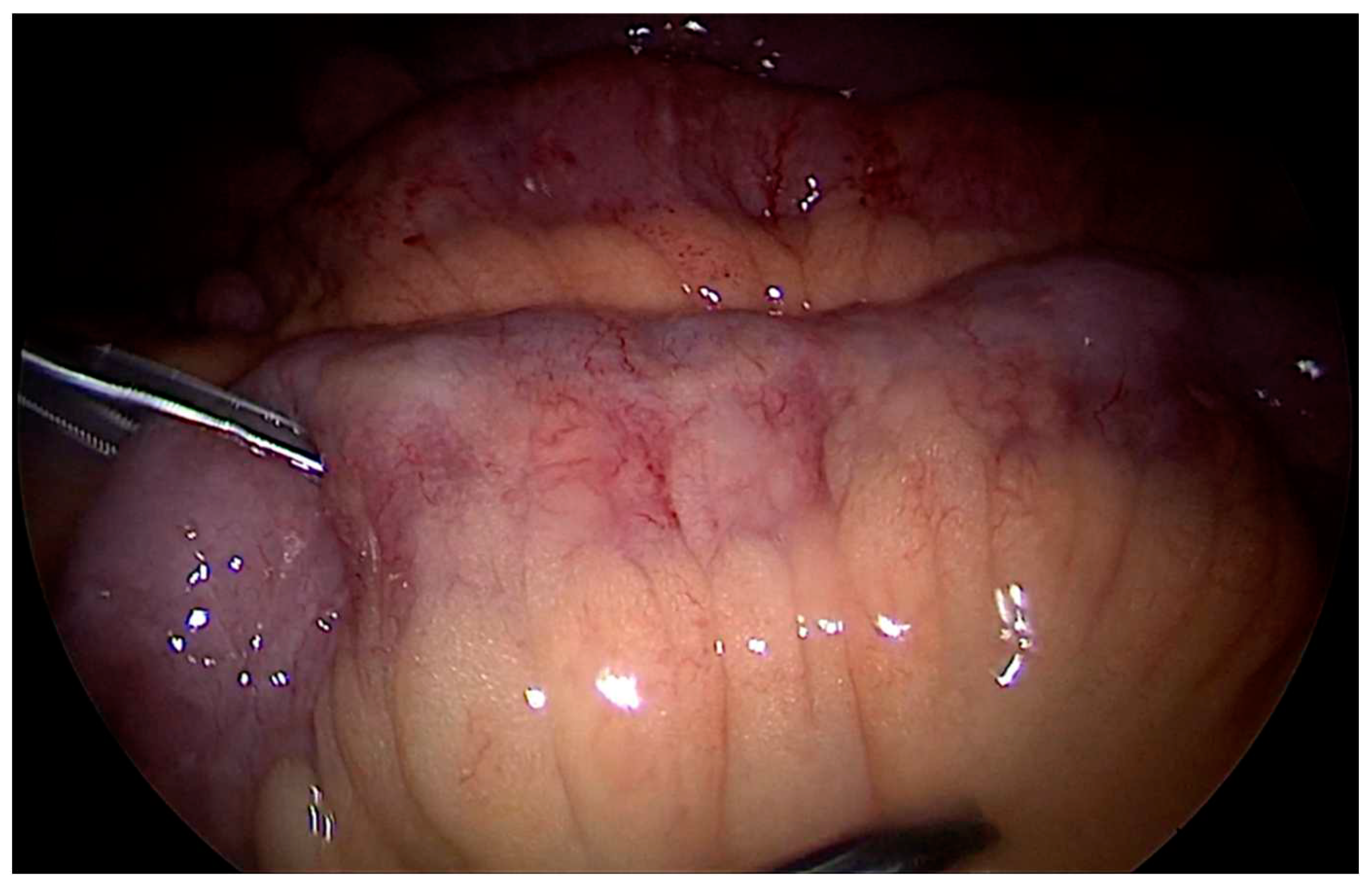
One-stage surgical treatment was performed in case of visualisation of localized affected area of the bowel with no infiltrates and or, no hormonal therapy at the time of surgery, endoscopic remission in other parts of the colon, normal albumin and hemoglobin levels, low or moderate degree of CD activity according to PCDAI. We performed laparoscopic mobilization of the affected bowel segment represented by the area with higher density (chondroid), petechial hemorrhages on edematous mesentery, and hypertrophic fat tissue (creeping fat) (
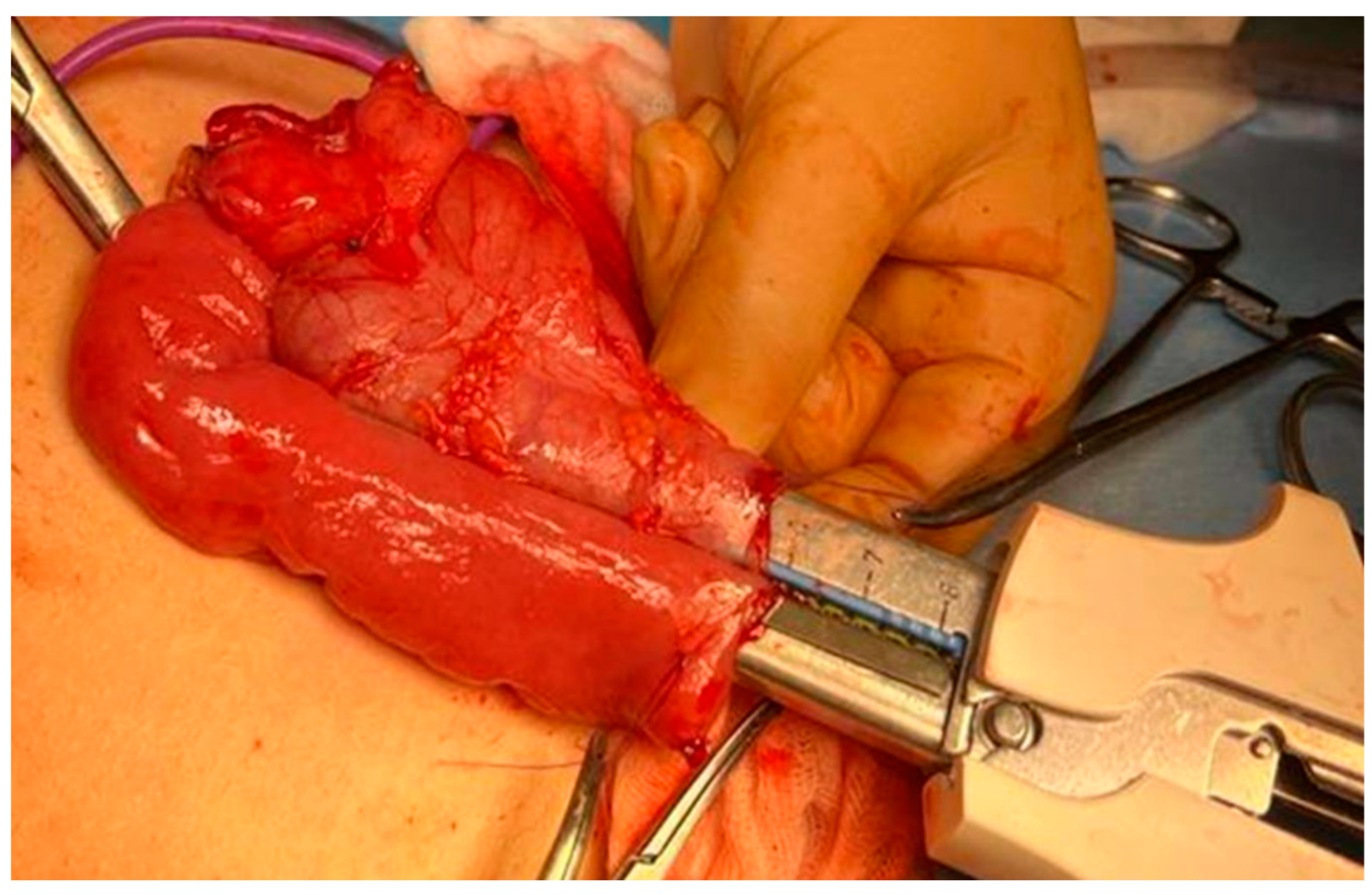
Figure 1). It was later delivered from the abdomen through minilaparotomy access. Resection within visually healthy tissues was performed with staplers. Intraoperative biopsy via the cryotomy at the edges of resected bowel was performed to confirm that radical resection of the affected area was successful, and the anastomosis would be made on healthy tissues. The side-to-side ileocolic anastomosis (
Figure 2) was formed only after morphological confirmation that there was no active inflammation. We preferred anastomoses with stapler.
We performed two-stage surgical treatment in case of inter-intestinal fistulas visualization (that were not diagnosed before surgery) or infiltrates and/or abscesses formation, and in case of generalized active inflammation on laparoscopy and endoscopy. The first stage involved resection of the affected bowel with intraoperative histological confirmation of radically performed resection and Brooke end ileostomy. The main step of colon mobilization and resection was performed via laparoscopic techniques. 4 children (9%) had infiltrate with abscess formation in the ileocecal angle. We had to perform conversion due to the generalized infiltrative and adhesion process in abdomen.
The second stage after achieving persistent clinical and endoscopic remission involved GIT continuity restoration with ileostomy reversal. Furthermore, two-stage surgical treatment was used in children with inflammation in the colon or in cases of recurrent purulent-septic lesions of the perianal region, that were amenable to medications. The first stage of surgical treatment was colon bypass. The second stage was performed to restore the gastrointestinal tract continuity after achieving remission or recovery of perianal inflammation.
Particular attention was paid to patients with isolated stenotic lesions of the colon, who had unstable clinical and laboratory remission. The results of magnetic resonance imaging (MRI) did not give clear answer about the inflammation in the intestine walls, that is, isolated fibrous stricture. The major difficulty in choosing the extent of surgery, in our opinion, was the lack of reliable data about mucous membrane state, depth and prevalence of the lesion in prestenotic area of the colon and ileocecal region, as we could not carry out appropriate endoscopic examination at the preoperative stage. Diagnostic laparoscopy allowed us to visually evaluate the limited part of the colon (anterior wall). Even though part of the colon is located retroperitoneally, we revealed indirect signs of active inflammation in intestine walls by small petechial hemorrhages, mesenteric edema, and omentum fixation in the affected area.
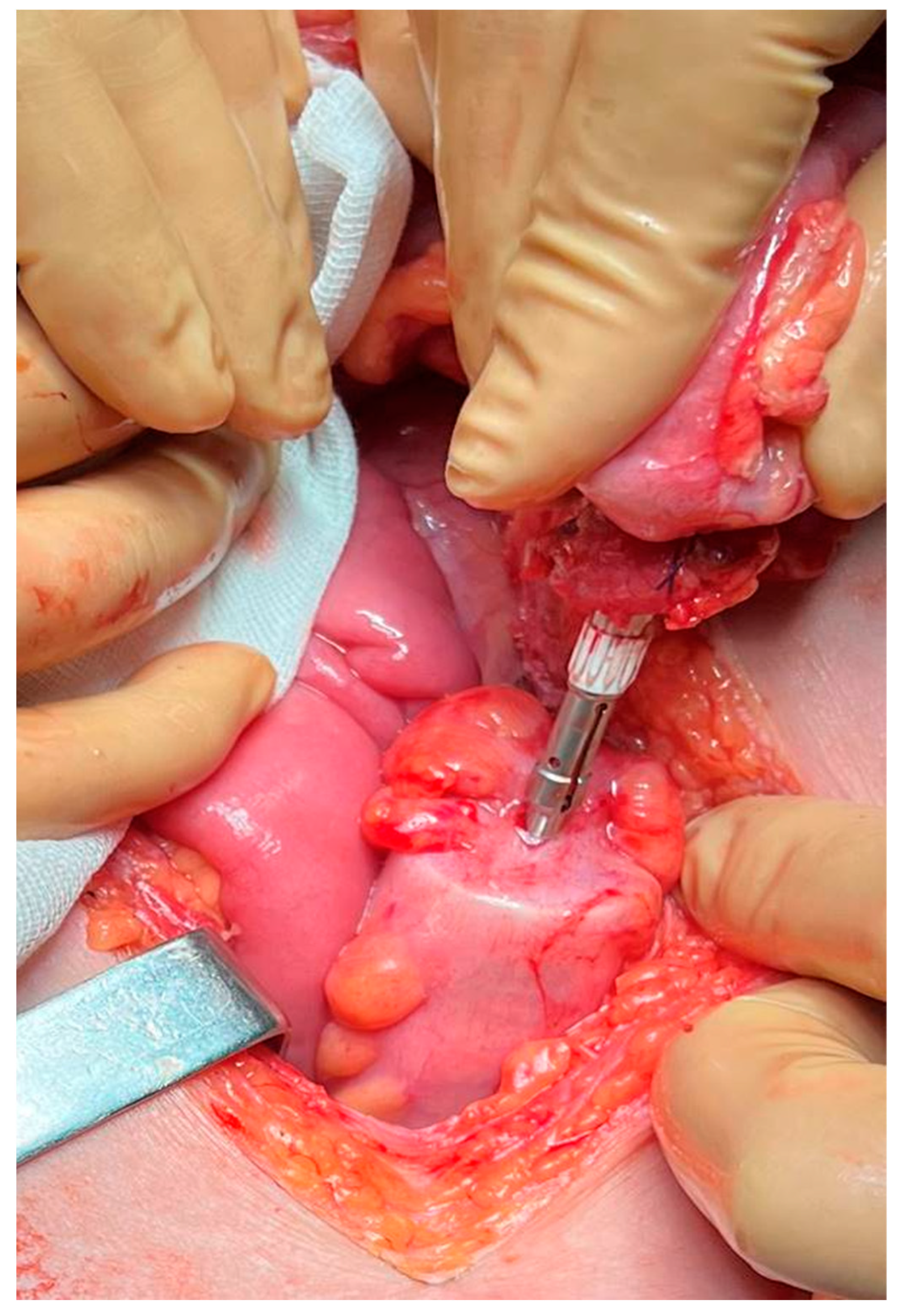
The first stage of surgical treatment was intestine disconnection at the ileum level. Ileocolonoscopy was performed intraoperatively through the efferent end to visualise active, generalized inflammatory process with deep fissured ulcers and pseudopolyps spreading up to the stenosis. Resection within healthy tissues in this situation was impossible due to the size of affected region, and there was high risk of anastomotic dehiscence. Therefore, we decided to perform three-stage surgical treatment. The next stage after intraoperative ileocolonoscopy, was colon bypass and end ileostomy. We saw localized fibrous stricture after achieving persistent remission according to abdominal organs MRI, its length significantly reduced if compared to the size at the first stage of surgical treatment. We saw localized fibrous stricture after achieving persistent remission according to abdominal organs MRI, its length significantly reduced if compared to the size at the first stage of surgical treatment. The second stage consisted of resection of the stenosis zone with intraoperative histological confirmation of absence of any active inflammation, and formation of manual or stapler colo-colic anastomosis (
Figure 3). The healing process was sustained with help of ileostomy. Then, on the third stage, we performed gastrointestinal tract restoration after endoscopic confirmation of the absence of inflammation in the anastomosis area, colon, and ileocecal region.
Thus, all patients were divided into 3 groups according to the surgical treatment staging.
Group 1 included 17 (26.6%) children with one-stage surgical treatment. Group 2 included 44 (68.7%) children who underwent two-stage surgical treatment. Group 3 (with isolated involvement of the colon) included 3 (4.7%) children with three-stage surgical treatment.
3. Results
All Children Underwent Follow-Up Examination at 6, 12, 18 and 24 Months after Surgery. Dynamics of Mass-Growth Indicators, Disease Activity According to PCDAI, Anemia and Albumin Levels, and Endoscopic Activity Were Evaluated. The Presence of Any Post-Surgery Complications Was Also Mentioned
Patients in Group 1 (n=17) were in remission at the time of surgery. All children received GEBD with monoclonal antibodies to tumor necrosis factor-alpha (anti-TNF-α), adalimumab. The PCDAI score did not exceed 10. Standard deviation score (SDS) was in the ±1 range when we were evaluating z-score height-to-age and BMI-to-age ratio. There were no cases of anemia or protein metabolism disorders. 10 (53%) children had terminal ileal stenosis, 7 (35%) children – ileocecal valve stricture with cecum deformity, and 2 (12%) children – stenosis at the descending colon according to ileocolonoscopy data. All patients had signs of active inflammation in the stricture area according to MRI.
Clinical, laboratory, and endoscopic remission persisted in all cases at evaluating surgical treatment efficacy. There was no violation of mass-growth indicators. No inflammatory changes or lumen strictures were revealed in the anastomosis area.
Children from Group 2 (n=44) had different degrees of CD activity according to PCDAI at the first stage of surgical treatment. 26 (59%) children had high activity (30-75.2 points), 18 (41%) children had moderate activity (at least 25 points). Remission was observed in 8 (18.2%) children and mild course in 36 (81.8%) children after all the stages of surgical treatment (p < 0.05).
All children from Group 2 showed high endoscopic activity according to the SES-CD index at the pre-operative stage. We have revealed statistically significant positive changes (p = 0.011) with no active inflammation in the colon at evaluating the endoscopic activity of postoperative recurrence of CD according to Rutgeerts index.
Statistical analysis of anthropometric parameters, z-scores for height-for-age ratio (HAZ) and BMI-for-age ratio (BAZ) revealed statistically significant differences in Group 2, HAZ p < 0.05, BAZ p < 0.001. This represented improvement in mass-growth parameters after surgical treatment.
Statistical analysis of hemoglobin, albumin, and C-reactive protein levels dynamics showed positive changes (p<0.001). There was no anemia, hypoalbuminemia, bacterial inflammation, that also indicated the surgical treatment efficacy.
16 (36.3%) patients received anti-TNFα therapy at the time of surgery. The biologic therapy duration before surgery ranged from 1 to 35 months (median – 15.5 months). GEBD therapy was continued in all children after surgery. Induction therapy with anti-TNFα inhibitors was administrated between 1 and 120 weeks (median – 2 weeks) in remaining 27 (62.8%) children to initiate remission.
Stoma duration ranged from 5 to 20 months (median – 8 months).
Patients in Group 3 (n=3) had moderate clinical activity according to pediatric index (PCDAI from 20 to 25) at the time of surgery indication. All children in this Group had mild clinical activity after surgical treatment (PCDAI 15 points).
Evaluation of endoscopic activity (SES-CD) showed that all children of Group 3 had high activity at the pre-operative stage. Endoscopic activity according to the Rutgeerts index showed positive changes with the absence of active inflammation in the colon after surgical treatment.
Statistical analysis of HAZ showed statistically significant differences, HAZ p<0.05 with postoperative scores improvement in children with CD. However, there were no statistically significant changes at evaluating BAZ in this group of children (p=0.066).
Statistically significant differences of pre- and post-operative hemoglobin, albumin, and C-reactive protein levels also indicated the efficacy of surgical treatment.
Stoma duration between surgical treatment stages in Group 3 ranged from 12 to 24 months (median – 16 months).
Statistical analysis of laboratory and anthromometric parameters of all children with complicated CD who undergone surgery was performed in our retro-prospective study. The follow-up data was obtained 6, 12, 18 and 24 months after surgery for children with one-stage surgical treatment and after the first surgical stage for children with two- and three-stage surgical treatment.
Evaluation of anthropometric parameters, z-scores for height-for-age ratio (HAZ) (
Table 1) and BMI-for-Age ratio (BAZ) showed statistically significant differences, HAZ p<0.05, BAZ p<0.001 (
Table 2). Evaluation of dynamics in laboratory parameters of hemoglobin (
Table 3), albumin (
Table 4), and C-reactive protein (
Table 5) showed statistically significant positive changes (p<0.001). There was no anemia or hypoalbuminemia, bacterial inflammation relief was noted. Altogether, it indicates the efficacy of surgical treatment.
4. Discussion
Laparoscopic assisted ileostomy was performed in 8 children (18,2%) from the Group 2 (44 patients in total). The reason for ileostomy in 5 patients was generalized purulent-septic lesion of the perianal region, and in 2 patients – severe colitis resistant to conservative treatment with GEBD. One child with very early onset of CD, relapsing colitis, and generalized pararectal lesions required proctocolectomy with ileostomy on the second stage.
The period from diagnosis verification to the first surgery ranged from 1 to 39 months (median – 9 months). The period between the first and second stages of surgical treatment ranged from 6 to 9 months (median – 15 months).
Seamann N.M., King S.K., Elkadri A., et al. covered 57 children in their study and reported 14 (24.6%) ileostomy cases in patients with severe pararectal lesions16. 2 (3.5%) patients underwent proctocolectomies. The period from diagnosis verification to the first surgery was 19 months (range from 7 to 100) and from diagnosis to radical surgery was 52 months (range from 7 to 114).
It was noted at post-surgery complications estimation that 5 children (11.4%) from Group 2 (n=44) had local inflammatory lesions in surgical wound area at long-term post-operative period. In three children who underwent conversions, wound healing was with secondary union. Suture sinuses were revealed in 2 patients after ileostomas reversal. We removed ligatures under regional anaesthesia, then local inflammatory changes were recovered. 3 children (6.8%) from Group 2 were re-operated on 5 and 7 days after surgery due to acute adhesive intestinal obstruction.
Pini-Prato A., Faticato M.G., Barabino A., et al.12 showed in the publication of literature review and their clinical observations on comparison of laparoscopic and open surgeries in children with IBD that there was no significant difference in postoperative complications when using these techniques, and that postoperative complications requiring re-surgery occurred in average in 29% of cases (158 out of 541 pediatric patients).
Fehmel E., Teague W.J., Simpson D., et al.13 reported that 16 (13.2%) patients with CD developed postoperative complications in their study on postoperative complications in children with IBD. 10 patients had small bowel obstruction, 5 of them required emergency laparotomy, while remaining 5 patients were treated conservatively. Anastomosis strictures were revealed in 4 children, and 2 of them required surgical treatment. Anastomotic dehiscence occurred in 1 patient. There were following stoma complications: stoma dehiscence (n=1) and stoma prolapse (n=2). One patient had stoma retraction and required required stoma revision.
Our study covered 64 children with complicated CD requiring surgical treatment. It showed that the rarest phenotype was isolated colon lesion (L2) occurs, and the group of these children was 4.9%. Kim H.J., Oh S.H., Kim D.Y., et al. reported in their study that the most common CD lesion (79.3%) develop in the ileocolic area (L3), while isolated colon lesion (L2) was less common – 8.2%1 . Also, Biko D.M., Mamula P., Chauvin N.A., et al. reported in their study on the results of MR-enterography of colon strictures in children and young adults with CD, and showed small amount of such pediatric patients, thus, colon strictures were not typical for children17. Prevalence of colon strictures is only 10% in 1/3 of patients with Crohn's disease, while prevalence of colon strictures in children is still unknown.
Three children (out of 64) with colon involvement underwent three-stage surgical treatment in our study. Scientists from the IBD Porto Group indicated in their guidelines on surgical treatment of CD that children requiring colectomy should not be subjects of urgent reconstruction, they had to undergo two- or three-stage surgical treatment18. Children with refractory colon lesions usually require total colectomy with ileorectal anastomosis (as operation of choice). Elective resection with primary anastomosis can be considered only in stable patient with good nutritional status. However, staged procedure would be the best variant in case of severe disease course. Patients with ileorectal anastomosis have good chances of avoiding protectomy and the formation of permanent stoma. Furthermore, these specialists recommend performing colon segmental resections in children with left colitis. Colon stricture-plasty is associated with higher risk of complications and is, therefore, rarely used. These guidelines also include personal message from Ian Sugarman who covered recent data on 81 patients most of whom ultimately required colectomy. In our study none of these 3 patients had colectomies possibly due to the small size of the sample for this category of patients. Additionally, this publication refers to the study by Harper P.H., Truelove S.C., Lee E.C., et al., who stated that temporary ileostomy was safe conservative procedure that could improve the condition of seriously ill and debilitated patients with Crohn's colitis.
We used intraoperative colonoscopy after separation of the intestinal tube at the ileal level to determine the volume of colon mucosa involvement. Then we used intraoperative morphological examination via the cryotomy at the edges of resected fragment at the second stage of surgical treatment (stricture resection). We have not seen any publications related to such intraoperative strategy in foreign or Russian literature.
Children of the Group 3 of our study had moderate clinical activity estimated according to PCDAI values. Berger TD, Lee HM, Padmanaban LR, et al. and scientists from IBD Porto Group of ESPGHAN determined PCDAI mean value at 27.5 points (20.0 to 40.0 points) in their publication on clinical features and outcomes in children with isolated CD of the colon19. Most patients in this group had inflammation in the left colon with lower rates in the transverse and right colon. In our study, stricture was revealed only in the left colon. 2.3% of patients developed colon strictures within 36 months after diagnosis, whereas, in our study, strictures formation ranged from 2 to 8 years 8 months (median – 3 years 7 months).
5. Conclusions
CD manifestation in children is characterized by more aggressive course and more often requires surgical interventions as compared with adult patients.
Isolated forms of fibrous strictures that can be formed on therapy are natural course of Crohn's disease in children. The surgical management of children nowadays is well studied. The treatment strategy for such patients is well covered in the world literature, and do not deserve any extensive discussion.
However, there is no uniform understanding on surgical management of children with CD and generalized lesions neither in foreign, nor in Russian literature, including clinical guidelines. Comprehensive laboratory and instrumental examination in our study revealed complicated course of CD with luminal narrowing of the intestine in the ileocecal angle and generalized colon inflammation in 44 children and generalized colitis with severe purulent-septic lesion of the perianal region in 8 children. The progressive course of CD caused the development of chronic anemia, protein metabolism disorders, maintained chronic bacterial inflammation, and negatively affected the children physical development. We believe that the choice of two-stage surgical treatment using laparoscopic technologies, intraoperative biopsy of the edges of resected bowel has allowed us to avoid re-surgery due to postoperative complications associated with anastomotic dehiscence. The surgical treatment followed by the administration of genetically engineered biologic drugs made it possible not only to significantly improve physical development, stop perianal inflammation, and achieve sustained remission, but also to improve the quality of life. Thus, socio-environmental adaptation of children with CD became possible.
Isolated colon involvement is the rarest phenotype in children with CD. Colon strictures require surgical treatment, but it is difficult to prognose the extent of surgery at the pre-operative stage. Endoscopic examination is limited by the stricture itself. Radiologic imaging can determine only the extent of stenosis but cannot reliably evaluate the state of the mucous membrane of the colon and ileocecal area. Intraoperative ileocolonoscopy can diagnose generalized colon lesions behind the stricture. The chosen strategy of three-stage surgical treatment alongside with drug therapy correction after colon bypass allow us not only to avoid postoperative anastomosis complications, but also to achieve remission. Whereafter, the second stage of surgical treatment included resection of significantly smaller area of stricture with safe forming of colo-colic anastomosis on the defunctioned bowel.
Statistical analysis of obtained results on surgical treatment of children with Crohn's disease (n=64) showed significant positive dynamics. We evaluated all the data from clinical, endoscopic and laboratory studies before surgery and at 6, 12, 18 months follow-up.
6. Patents
Patent No. 2791404 C1 Russian Federation, IPC A61B 17/00, A61B 17/11, A61B 1/313. The method of choosing the tactics of surgical treatment of Crohn's disease in children : No. 2022113122 : Appl. 05/17/2022 : publ. 03/07/2023 / E. Yu. Dyakonova, A. S. Bekin, A. A. Gusev [and others]; applicant Federal State Autonomous Institution "National Medical Research Center for Children's Health" of the Ministry of Health of the Russian Federation. – EDN OMKKFG.
Author Contributions
(CRediT author statement) .Alexandr Bekin.: Conceptualization, Resources, Provision of patients, participation in surgery and data collection, writing - Original Draft; Elena Dyakonova.: Resources, Provision of patients, instrumentation; Aleksey Gusev.: Data curation, Writing- Original draft preparation. ; Dmitry Sladkov.: Participation in data collection, draft preparation; Maksim Lochmatov.: Resources, Provision of study materials, patients, instrumentation, computing resources ; Alexandr Potapov.: Resources, Provision of patients, Methodology; Sergey Yatsyk.: Supervision, Provision of patients, participation in surgery and data collection; Andrey Fisenko.: Resources, Supervision; Darya Pereladova.: Participation in data collection, draft preparation.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Local Independent Ethics Committee of the National Research Center for Children's Health of the Ministry of Health of the Russian Federation (protocol code № 1 17.01.2020).
Informed Consent Statement
Informed consent for the operation and scientific products was obtained from all subjects participating in the study.
Data Availability Statement
additional information can be requested by e-mail.
Acknowledgments
With great gratitude to the community of our National Scientific Center, for the opportunity to conduct and combine our practical work and scientific research for the benefit of the children's population.
Conflicts of Interest
The authors declare no conflict of interest.
Abbreviations
| CD |
Crohn's disease |
| IBD |
inflammatory bowel disease |
| GEBD |
genetically engineered biologic drugs |
| PCDAI |
Pediatric Crohn's Disease Activity Index |
| MR-enterography |
magnetic resonance enterography |
| MRI |
magnetic resonance imaging |
| GIT |
gastrointestinal tract |
| anti-TNFα |
monoclonal antibodies to tumor necrosis factor-alpha |
| SDS |
Standart Deviation Score |
| BMI |
Body Mass Index |
| BAZ |
BMI-for-age ratio |
| HAZ |
height-for-age ratio |
| SES-CD |
Simple Endoscopic Score for Crohn Disease |
References
- Kim HJ, Oh SH, Kim DY, et al. Clinical Characteristics and Long-Term Outcomes of Paediatric Crohn's Disease: A Single-Centre Experience. J Crohns Colitis. 2017, 11, 157–164. [Google Scholar] [CrossRef] [PubMed]
- Tarnok A, Kiss Z, Kadenczki O, et al. Characteristics of biological therapy in pediatric patients with Crohn's disease. Expert OpinBiolTher. 2019, 19, 181–196. [Google Scholar] [CrossRef]
- Dotlačil V, Škába R, Rousková B, et al. Surgical treatment of Crohns disease in children in the era of biological treatment. RozhlChir. 2022, 101, 56–60. [Google Scholar] [CrossRef]
- Stewart, D. Surgical care of the pediatric Crohn's disease patient. Seminars in Pediatric Surgery. 2017, 26, 373–378. [Google Scholar] [CrossRef] [PubMed]
- Cantoro L, Lenti MV, Monterubbianesi R, et al. Early-onset versus late-onset Crohn's disease: An Italian cohort study. United European Gastroenterol J. 2020, 8, 52–58. [Google Scholar] [CrossRef] [PubMed]
- Maccioni F, Bencardino D, Buonocore V, et al. MRI reveals different Crohn's disease phenotypes in children and adults. EurRadiol. 2019, 29, 5082–5092. [Google Scholar] [CrossRef]
- Bekin, A.S, D'yakonova E.Yu, Surkov A.N, et al. Crohn's disease in children: the current state of the problem. Pediatriya im. G.N. Speranskogo. 2021, 100, 78–85. [CrossRef]
- Quiroz, H.J, Perez E.A, El Tawil R.A, et al. Open Versus Laparoscopic Right Hemicolectomies in Pediatric Patients with Crohn's Disease. J LaparoendoscAdvSurg Tech A. 2020, 30, 820–825. [CrossRef]
- Hansen LF, Jakobsen C, Paerregaard A, et al. Surgery and postoperative recurrence in children with Crohn disease. J PediatrGastroenterolNutr. 2015, 60, 347–351. [Google Scholar] [CrossRef]
- Bekin, A.S, D'yakonova E.Yu, Surkov A.N., et al. Complicated forms of Crohn's disease in children requiring surgical treatment. Detskaya Khirurgiya. Zhurnal im. Yu.F. Isakova. (in Russian). 2022, 26, 21.
- Newton, L., Delbecque, L., Coşkun, U. et al. A qualitative study to explore symptoms and impacts of pediatric and adolescent Crohn’s disease from patient and caregiver perspective. J Patient Rep Outcomes 2021, 5, 49. [CrossRef] [PubMed]
- Pini-Prato A, Faticato MG, Barabino A, et al. Minimally invasive surgery for paediatric inflammatory bowel disease: Personal experience and literature review. World J Gastroenterol. 2015, 21, 11312–11320. [Google Scholar] [CrossRef] [PubMed]
- Fehmel E, Teague WJ, Simpson D, et al. The burden of surgery and postoperative complications in children with inflammatory bowel disease. J Pediatr Surg. 2018, 53, 2440–2443. [Google Scholar] [CrossRef] [PubMed]
- Adegbola, S.O., Pisani A, Sahnan K, et al. Medical and surgical management of perianal Crohn's disease. Ann Gastroenterol. 2018, 31, 129–139. [CrossRef]
- Shcherbakova, O.V, Razumovskij A. Ju. Indications for surgical treatment of children and adolescents with complicated Crohn's disease. Detskaja hirurgija. 2018, 22, 35–41. [CrossRef]
- Seemann, N.M, King S.K, Elkadri A, et al. The operative management of children with complex perianal Crohn's disease. J Pediatr Surg. 2016, 51, 1993–1997. [CrossRef] [PubMed]
- Biko, D.M, Mamula P, Chauvin N.A, et al. Colonic strictures in children and young adults with Crohn's disease: Recognition on MR enterography. Clin Imaging. 2018, 48, 122–126. [CrossRef]
- Amil-Dias J, Kolacek S, Turner D, et al. Surgical Management of Crohn Disease in Children: Guidelines From the Paediatric IBD Porto Group of ESPGHAN. J PediatrGastroenterolNutr. 2017, 64, 818–835. [Google Scholar] [CrossRef]
- Zimmerman, L.A, Saites C.G, Bairdain S, et al. Postoperative Complications in Children with Crohn Disease Treated With Infliximab. J PediatrGastroenterolNutr. 2016, 63, 352–356. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).