Submitted:
09 August 2023
Posted:
10 August 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
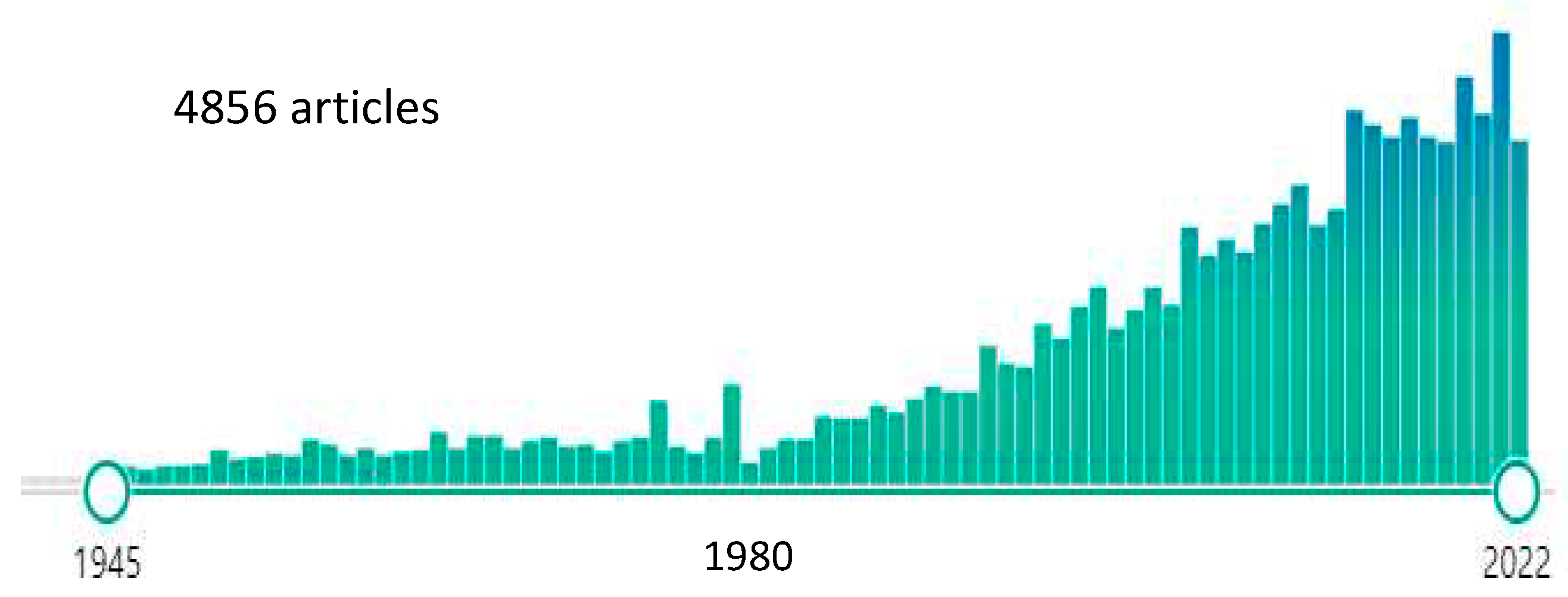
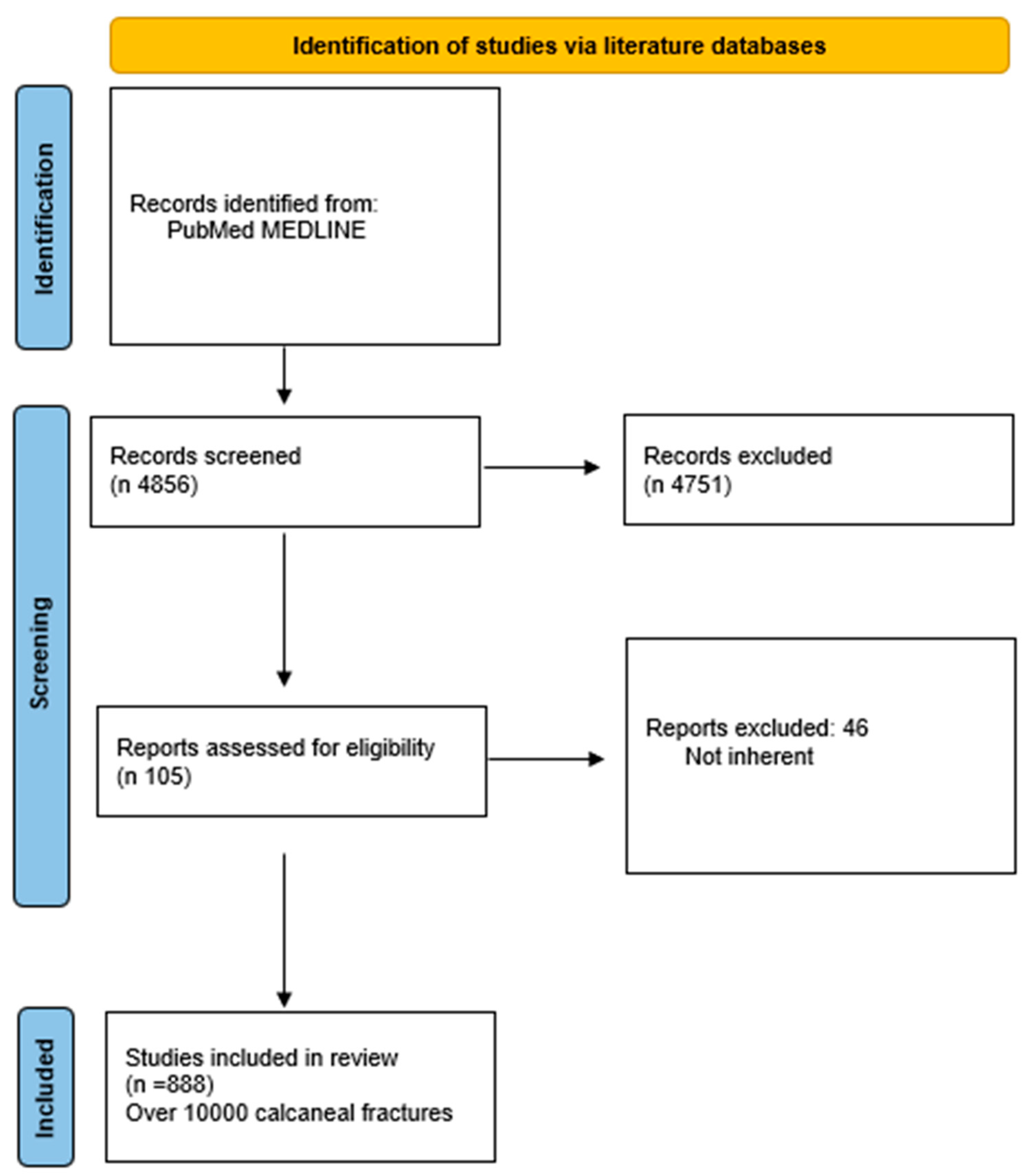
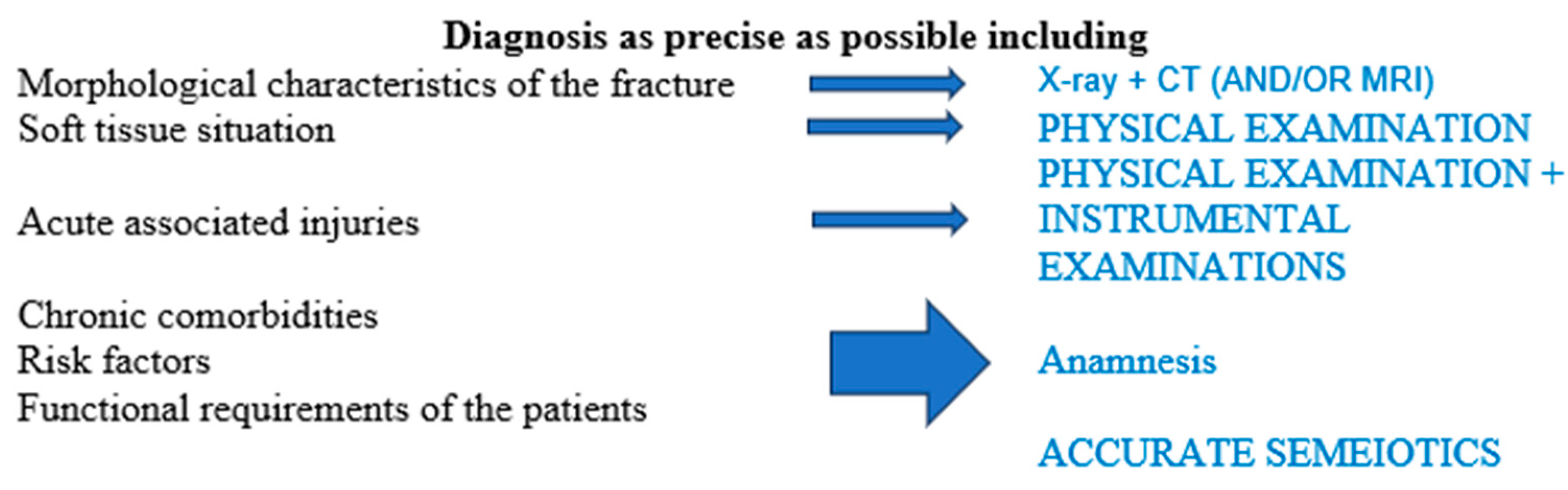
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Zhang F, Tian H, Li S, Liu B, Dong T, Zhu Y, Zhang Y: Meta-analysis of two surgical approaches for calcaneal fractures: sinus tarsi versus extensile lateral approach. ANZ journal of surgery 2017, 87, 126–131. [CrossRef]
- Schepers T: The sinus tarsi approach in displaced intra-articular calcaneal fractures: a systematic review. International orthopaedics 2011, 35, 697–703. [CrossRef] [PubMed]
- Peng C, Yuan B, Guo W, Li N, Tian H: Extensile lateral versus sinus tarsi approach for calcaneal fractures: A meta-analysis. Medicine 2021, 100, e26717. [CrossRef]
- Ma D, Huang L, Liu B, Liu Z, Xu X, Liu J, Chu T, Pan L: Efficacy of Sinus Tarsal Approach Compared With Conventional L-Shaped Lateral Approach in the Treatment of Calcaneal Fractures: A Meta-Analysis. Frontiers in surgery 2020, 7, 602053.
- Lv Y, Zhou YF, Li L, Yu Z, Wang Q, Sun YY, Zhou DS: Sinus tarsi approach versus the extended lateral approach for displaced intra-articular calcaneal fractures: a systematic review and meta-analysis. Archives of orthopaedic and trauma surgery 2021, 141, 1659–1667. [CrossRef] [PubMed]
- Seat A, Seat C: Lateral Extensile Approach Versus Minimal Incision Approach for Open Reduction and Internal Fixation of Displaced Intra-articular Calcaneal Fractures: A Meta-analysis. The Journal of foot and ankle surgery : official publication of the American College of Foot and Ankle Surgeons 2020, 59, 356–366. [CrossRef]
- Ieropoli G, Villafane JH, Zompi SC, Morozzo U, D'Ambrosi R, Usuelli FG, Berjano P: Successful treatment of infected wound dehiscence after minimally invasive locking-plate osteosynthesis of tibial pilon and calcaneal fractures by plate preservation, surgical debridement and antibiotics. Foot 2017, 33, 44–47.
- Indino C, Villafane JH, D'Ambrosi R, Manzi L, Maccario C, Berjano P, Usuelli FG: Effectiveness of subtalar arthroereisis with endorthesis for pediatric flexible flat foot: a retrospective cross-sectional study with final follow up at skeletal maturity. Foot and ankle surgery : official journal of the European Society of Foot and Ankle Surgeons 2020, 26, 98–104. [CrossRef]
- Fan B, Zhou X, Wei Z, Ren Y, Lin W, Hao Y, Shi G, Feng S: Cannulated screw fixation and plate fixation for displaced intra-articular calcaneus fracture: A meta-analysis of randomized controlled trials. International journal of surgery 2016, 34, 64–72. [CrossRef]
- Zeng Z, Yuan L, Zheng S, Sun Y, Huang F: Minimally invasive versus extensile lateral approach for sanders type II and III calcaneal fractures: A meta-analysis of randomized controlled trials. International journal of surgery 2018, 50, 146–153. [CrossRef]
- Selim A, Ponugoti N, Chandrashekar S: Systematic Review of Operative vs Nonoperative Treatment of Displaced Intraarticular Calcaneal Fractures. Foot & ankle orthopaedics 2022, 7, 24730114221101609.
- Meena S, Hooda A, Sharma P, Mittal S, Sharma J, Chowdhury B: Operative versus Non operative treatment of displaced intraarticular fracture of calcaneum: a meta-analysis of randomized controlled trials. Acta orthopaedica Belgica 2017, 83, 161–169.
- Zhang C, Ye ZM, Lin P, Miao XD: Lateral Fracture-Dislocation of the Calcaneus: Case Reports and a Systematic Review. Orthopaedic surgery 2021, 13, 682–691. [CrossRef] [PubMed]
- Barini M, Zagaria D, Licandro D, Pansini S, Airoldi C, Leigheb M, Carriero A: Magnetic Resonance Accuracy in the Diagnosis of Anterior Talo-Fibular Ligament Acute Injury: A Systematic Review and Meta-Analysis. Diagnostics 2021, 11.
- Yang Y, Zhao H, Zhou J, Yu G: Treatment of displaced intraarticular calcaneal fractures with or without bone grafts: A systematic review of the literature. Indian journal of orthopaedics 2012, 46, 130–137. [CrossRef] [PubMed]
- Yao H, Liang T, Xu Y, Hou G, Lv L, Zhang J: Sinus tarsi approach versus extensile lateral approach for displaced intra-articular calcaneal fracture: a meta-analysis of current evidence base. Journal of orthopaedic surgery and research 2017, 12, 43. [CrossRef]
- Yu T, Xiong Y, Kang A, Zhou H, He W, Zhu H, Yang Y: Comparison of sinus tarsi approach and extensile lateral approach for calcaneal fractures: A systematic review of overlapping meta-analyses. Journal of orthopaedic surgery 2020, 28, 2309499020915282.
- Nosewicz TL, Dingemans SA, Backes M, Luitse JSK, Goslings JC, Schepers T: A systematic review and meta-analysis of the sinus tarsi and extended lateral approach in the operative treatment of displaced intra-articular calcaneal fractures. Foot and ankle surgery : official journal of the European Society of Foot and Ankle Surgeons 2019, 25, 580–588. [CrossRef]
- Wu MH, Sun WC, Yan FF, Hou ZQ, Feng F, Cai L: [Minimally invasive sinus tarsal approach versus conventional L-shaped lateral approach in treating calcaneal fractures: a Meta-analysis]. Zhongguo gu shang = China journal of orthopaedics and traumatology 2017, 30, 1118–1126.
- Bai L, Hou YL, Lin GH, Zhang X, Liu GQ, Yu B: Sinus tarsi approach (STA) versus extensile lateral approach (ELA) for treatment of closed displaced intra-articular calcaneal fractures (DIACF): A meta-analysis. Orthopaedics & traumatology, surgery & research : OTSR 2018, 104, 239–244.
- Meena S, Gangary SK, Sharma P: Review Article: Operative versus nonoperative treatment for displaced intraarticular calcaneal fracture: a meta-analysis of randomised controlled trials. Journal of orthopaedic surgery 2016, 24, 411–416. [CrossRef] [PubMed]
- Jiang N, Lin QR, Diao XC, Wu L, Yu B: Surgical versus nonsurgical treatment of displaced intra-articular calcaneal fracture: a meta-analysis of current evidence base. International orthopaedics 2012, 36, 1615–1622. [CrossRef] [PubMed]
- Griffin D, Parsons N, Shaw E, Kulikov Y, Hutchinson C, Thorogood M, Lamb SE, Investigators UKHFT: Operative versus non-operative treatment for closed, displaced, intra-articular fractures of the calcaneus: randomised controlled trial. Bmj 2014, 349, g4483. [CrossRef] [PubMed]
- Luo X, Li Q, He S, He S: Operative Versus Nonoperative Treatment for Displaced Intra-Articular Calcaneal Fractures: A Meta-Analysis of Randomized Controlled Trials. The Journal of foot and ankle surgery : official publication of the American College of Foot and Ankle Surgeons 2016, 55, 821–828. [CrossRef] [PubMed]
- Zhang W, Lin F, Chen E, Xue D, Pan Z: Operative Versus Nonoperative Treatment of Displaced Intra-Articular Calcaneal Fractures: A Meta-Analysis of Randomized Controlled Trials. Journal of orthopaedic trauma 2016, 30, e75–81. [CrossRef] [PubMed]
- Bruce J, Sutherland A: Surgical versus conservative interventions for displaced intra-articular calcaneal fractures. The Cochrane database of systematic reviews 2013, CD008628.
- Randle JA, Kreder HJ, Stephen D, Williams J, Jaglal S, Hu R: Should calcaneal fractures be treated surgically? A meta-analysis. Clinical orthopaedics and related research 2000, 217–227.
- Wei N, Yuwen P, Liu W, Zhu Y, Chang W, Feng C, Chen W: Operative versus nonoperative treatment of displaced intra-articular calcaneal fractures: A meta-analysis of current evidence base. Medicine 2017, 96, e9027. [CrossRef]
- Liu Y, Li Z, Li H, Zhang Y, Wang P: Protective Effect of Surgery Against Early Subtalar Arthrodesis in Displaced Intra-articular Calcaneal Fractures: A Meta-Analysis. Medicine 2015, 94, e1984–e1980. [CrossRef]
- Backes M, Spierings KE, Dingemans SA, Goslings JC, Buckley RE, Schepers T: Evaluation and quantification of geographical differences in wound complication rates following the extended lateral approach in displaced intra-articular calcaneal fractures - A systematic review of the literature. Injury 2017, 48, 2329–2335.
- Zhang W, Chen E, Xue D, Yin H, Pan Z: Risk factors for wound complications of closed calcaneal fractures after surgery: a systematic review and meta-analysis. Scandinavian journal of trauma, resuscitation and emergency medicine 2015, 23, 18. [CrossRef]
- Zhang L, Su P, Li J: Complications in the Management of Displaced Intra-articular Calcaneal Fractures: A Systematic Review and Network Meta-Analysis of 2538 Patients. The Journal of foot and ankle surgery : official publication of the American College of Foot and Ankle Surgeons 2022.
- Halvachizadeh S, Klingebiel FKL, Pfeifer R, Gosteli M, Schuerle S, Cinelli P, Zelle BA, Pape HC: The local soft tissue status and the prediction of local complications following fractures of the ankle region. Injury 2022, 53, 1789–1795. [CrossRef] [PubMed]
- Williams CE, Joo P, Oh I, Miller C, Kwon JY: Arthroscopically Assisted Internal Fixation of Foot and Ankle Fractures: A Systematic Review. Foot & ankle orthopaedics 2021, 6, 2473011420950214.
- Marouby S, Cellier N, Mares O, Kouyoumdjian P, Coulomb R: Percutaneous arthroscopic calcaneal osteosynthesis for displaced intra-articular calcaneal fractures: Systematic review and surgical technique. Foot and ankle surgery : official journal of the European Society of Foot and Ankle Surgeons 2020, 26, 503–508. [CrossRef] [PubMed]
- Almeida JF, Vale C, Gonzalez T, Gomes TM, Oliva XM: Osteosynthesis or primary arthrodesis for displaced intra-articular calcaneus fractures Sanders type IV - A systematic review. Foot and ankle surgery : official journal of the European Society of Foot and Ankle Surgeons 2022, 28, 281–287. [CrossRef] [PubMed]
- Shi G, Liu W, Shen Y, Cai X: 3D printing-assisted extended lateral approach for displaced intra-articular calcaneal fractures: a systematic review and meta-analysis. Journal of orthopaedic surgery and research 2021, 16, 682. [CrossRef]
- Wang Q, Zhang N, Guo W, Wang W, Zhang Q: Cannulated screw fixation versus plate fixation in treating displaced intra-articular calcaneus fractures: a systematic review and meta-analysis. International orthopaedics 2021, 45, 2411–2421. [CrossRef]
- Gougoulias N, Khanna A, McBride DJ, Maffulli N: Management of calcaneal fractures: systematic review of randomized trials. British medical bulletin 2009, 92, 153–167. [CrossRef]
- Bridgman S, Dunn K, McBride D, Richards P: WITHDRAWN: Interventions for treating calcaneal fractures. The Cochrane database of systematic reviews 2008, CD001161.
- Wallin KJ, Cozzetto D, Russell L, Hallare DA, Lee DK: Evidence-based rationale for percutaneous fixation technique of displaced intra-articular calcaneal fractures: a systematic review of clinical outcomes. The Journal of foot and ankle surgery : official publication of the American College of Foot and Ankle Surgeons 2014, 53, 740–743. [CrossRef] [PubMed]
- Veltman ES, Doornberg JN, Stufkens SA, Luitse JS, van den Bekerom MP: Long-term outcomes of 1,730 calcaneal fractures: systematic review of the literature. The Journal of foot and ankle surgery : official publication of the American College of Foot and Ankle Surgeons 2013, 52, 486–490. [CrossRef] [PubMed]
- Pelliccioni AA, Bittar CK, Zabeu JL: Surgical treatment of intraarticular calcaneous fractures of sanders' types II and III. Systematic review. Acta ortopedica brasileira 2012, 20, 39–42. [Google Scholar]
- Shi F, Wu S, Cai W, Zhao Y: Comparison of 5 Treatment Approaches for Displaced Intra-articular Calcaneal Fractures: A Systematic Review and Bayesian Network Meta-Analysis. The Journal of foot and ankle surgery : official publication of the American College of Foot and Ankle Surgeons 2020, 59, 1254–1264. [CrossRef]
- Sanders FRK, Peters JJ, Schallig W, Mittlmeier T, Schepers T: What is the added value of pedobarography for assessing functional outcome of displaced intra-articular calcaneal fractures? A systematic review of existing literature. Clinical biomechanics 2020, 72, 8–15. [CrossRef] [PubMed]
- Muir RL, Forrester R, Sharma H: Fine Wire Circular Fixation for Displaced Intra-Articular Calcaneal Fractures: A Systematic Review. The Journal of foot and ankle surgery : official publication of the American College of Foot and Ankle Surgeons 2019, 58, 755–761. [CrossRef]
- Spierings KE, Min M, Nooijen LE, Swords MP, Schepers T: Managing the open calcaneal fracture: A systematic review. Foot and ankle surgery : official journal of the European Society of Foot and Ankle Surgeons 2019, 25, 707–713. [CrossRef]
- Zheng W, Xie L, Xie H, Chen C, Chen H, Cai L: With versus without bone grafts for operative treatment of displaced intra-articular calcaneal fractures: A meta-analysis. International journal of surgery 2018, 59, 36–47. [CrossRef]
- Wang XJ, Su YX, Li L, Zhang ZH, Wei XC, Wei L: Percutaneous poking reduction and fixation versus open reduction and fixation in the treatment of displaced calcaneal fractures for Chinese patients: A systematic review and meta-analysis. Chinese journal of traumatology = Zhonghua chuang shang za zhi 2016, 19, 362–367.
- Wu J, Zhou F, Yang L, Tan J: Percutaneous Reduction and Fixation with Kirschner Wires versus Open Reduction Internal Fixation for the Management of Calcaneal Fractures: A Meta-Analysis. Scientific reports 2016, 6, 30480. [CrossRef]
- Majeed H, Barrie J, Munro W, McBride D: Minimally invasive reduction and percutaneous fixation versus open reduction and internal fixation for displaced intra-articular calcaneal fractures: A systematic review of the literature. EFORT open reviews 2018, 3, 418–425. [CrossRef] [PubMed]
- Mahmoud K, Mekhaimar MM, Alhammoud A: Prevalence of Peroneal Tendon Instability in Calcaneus Fractures: A Systematic Review and Meta-Analysis. The Journal of foot and ankle surgery : official publication of the American College of Foot and Ankle Surgeons 2018, 57, 572–578. [CrossRef] [PubMed]
- De Boer AS, Van Lieshout EMM, Van Moolenbroek G, Den Hartog D, Verhofstad MHJ: The effect of time to post-operative weightbearing on functional and clinical outcomes in adults with a displaced intra-articular calcaneal fracture; A systematic review and pooled analysis. Injury 2018, 49, 743–752.
- Dingemans SA, Sintenie FW, de Jong VM, Luitse JSK, Schepers T: Fixation Methods for Calcaneus Fractures: A Systematic Review of Biomechanical Studies Using Cadaver Specimens. The Journal of foot and ankle surgery : official publication of the American College of Foot and Ankle Surgeons 2018, 57, 116–122. [CrossRef] [PubMed]
- van Hoeve S, Poeze M: Outcome of Minimally Invasive Open and Percutaneous Techniques for Repair of Calcaneal Fractures: A Systematic Review. The Journal of foot and ankle surgery : official publication of the American College of Foot and Ankle Surgeons 2016, 55, 1256–1263. [CrossRef]
- Bajammal SS, Zlowodzki M, Lelwica A, Tornetta P, 3rd, Einhorn TA, Buckley R, Leighton R, Russell TA, Larsson S, Bhandari M: The use of calcium phosphate bone cement in fracture treatment. A meta-analysis of randomized trials. The Journal of bone and joint surgery American volume 2008, 90, 1186–1196. [Google Scholar] [CrossRef]
- Schepers T: The primary arthrodesis for severely comminuted intra-articular fractures of the calcaneus: a systematic review. Foot and ankle surgery : official journal of the European Society of Foot and Ankle Surgeons 2012, 18, 84–88. [CrossRef]
- Schepers T: The subtalar distraction bone block arthrodesis following the late complications of calcaneal fractures: a systematic review. Foot 2013, 23, 39–44. [CrossRef]
- Leigheb M: Wrist traumatology in the 2020s. Minerva Orthop 2021, 72, 93–94.
- Leigheb M, Janicka P, Andorno S, Marcuzzi A, Magnani C, Grassi F: Italian translation, cultural adaptation and validation of the "American Orthopaedic Foot and Ankle Society's (AOFAS) ankle-hindfoot scale". Acta bio-medica : Atenei Parmensis 2016, 87, 38–45.
- Leigheb M, Massa M, Bosetti M, Nico P, Tarallo L, Pogliacomi F, Grassi FA: Autologous Platelet Rich Plasma (PRP) in the treatment of elbow epicondylitis and plantar fasciitis: medium to long term clinical outcome. Acta bio-medica : Atenei Parmensis 2020, 91, e2020029.
- Leigheb M, Rusconi M, De Consoli A, Fredo M, Rimondini L, Cochis A, Pogliacomi F, Grassi FA: Arthroscopically-assisted Reduction and Internal Fixation (ARIF) of tibial plateau fractures: clinical and radiographic medium-term follow-up. Acta bio-medica : Atenei Parmensis 2020, 91, 152–159.
- Villafane JH, Valdes K, Pedersini P, Berjano P: Osteoarthritis: a call for research on central pain mechanism and personalized prevention strategies. Clinical rheumatology 2019, 38, 583–584. [CrossRef] [PubMed]
- Caruso I, Leonardini A, Caizzi G, Vicenti G, Caporusso M, Guarini F, Bernardis M, Moretti B, Giorgino F: Diabetic foot: clinical ap-proach. Minerva Orthop 2022, 73, 63–75.
- Buda R, Bruni D, Pantalone A: Current concepts in the treatment of ankle osteoarthritis. Minerva Orthop 2021, 72, 539–540.
- Cochis A, Bonetti L, Sorrentino R, Contessi Negrini N, Grassi F, Leigheb M, Rimondini L, Fare S: 3D Printing of Thermo-Responsive Methylcellulose Hydrogels for Cell-Sheet Engineering. Materials 2018, 11.
- Parchi P: 3D printing in orthopedic surgery. Minerva Orthop 2021, 72, 347–348.
- Aprato A, Giudice C: 3D printing in pediatrics orthopedics. Minerva Orthop 2022, 73, 551–553.
- Bonatti AF, Chiesa I, Micalizzi S, Vozzi G, De Maria C: Bioprinting for bone tissue engineering. Minerva Orthop 2021, 72, 376–394.
- Leigheb M, Veneziano M, Tortia R, Bosetti M, Cochis A, Rimondini L, Grassi FA: Osteosynthesis devices in absorbable Magnesium alloy in comparison to standard ones: a Systematic Review on effectiveness and safety. Acta bio-medica : Atenei Parmensis 2021, 92, e2021025.
- Bosetti M, Borrone A, Leigheb M, Shastri VP, Cannas M: Injectable Graft Substitute Active on Bone Tissue Regeneration. Tissue engineering Part A 2017, 23, 1413–1422. [CrossRef] [PubMed]
- Vicenti G, Ottaviani G, Bizzoca D, Carrozzo M, Simone F, Grosso A, Zavattini G, Elia R, MAuruccia M, SOlarino G et al: The manage-ment of post-traumatic bone defects: a systematic review. Minerva Orthop 2022, 73, 10–19.
- Waldorff EI, Markov MS: Magnetic and electromagnetic field in therapeutic application for bone stimulation. Minerva Orthop 2022, 73, 73–74.
- Mazzotti A, Langone L, Artioli E, Zielli SO, Arceri A, Setti S, Leigheb M, Samaila EM, Faldini C: Applications and Future Perspective of Pulsed Electromagnetic Fields in Foot and Ankle Sport-Related Injuries. Applied Sciences 2023, 13, 5807. [CrossRef]
| TOPIC | N Metanalysis or/and systematic reviews |
N Articles compared |
Results |
|---|---|---|---|
| STA VS ELA [1,2,3,4,5,6,10,15,16,17,18,19,20] |
13 | 8 8 7 8 X 12 15 5 27 9 8 7 8 |
STA > ELA 9 STA = ELA 4 |
| Conservative treatment VS Surgical treatment [11,12,21,22,23,24,25,26,27,28,29] |
11 | 8 10 18 8 7 4 7 7 13 8 18 4 |
Conservative treatment < Surgical treatment 11 Conservative treatment = Surgical treatment 1 |
| Complications and soft tissues [30,31,32,33] |
4 | 123 10 26 34 |
ELA experienced the most frequent complications PA better results The state of the overlying tissues is the + important predictor No difference between POWI and POWC over the countries |
| ARIF VS AREF [34,35] |
2 | 32 8 |
ARIF = others treatments ARIF > into diagnosyis |
| ORIF VS Arthrodesys [35,36] |
2 | 14 9 |
ORIF > arthrodesis in Sanders type II/III ORIF = arthrodesis in Sanders type IV |
| 3D printed-assisted [37] |
1 | 9 | “Excellent and good outcome, shorter operation time, less intraoperative blood loss, fewer intraoperative fluoroscopies, fewer complications.” |
| Cannulated screws VS ORIF [9,38] |
2 | 5 7 |
Same functional results Screw > ORIF for complications, quality of reduction, surgical timing |
| Dislocated fractures [13] |
1 | 4 | “Timely surgical intervention is essential for satisfactory clinic outcomes.” |
| Comparison between treatments [13,39,40,41,42,43,44] |
6 | 4 7 25 3 2 17 |
“PRF (87.0%), MILA (52.9%), STA (46.6%), ELA (40.4%), nonoperative (23.1%). In terms of excellent and good satisfaction ratings, the treatments were ranked as follows: STA (96.2%), ELA (66.8%), PRF (34.9%), and nonoperative (2%). In terms of incision complications, the treatments were ranked as follows: PRF (84.1%), MILA (80.0%), STA (35.8%), and ELA (0.1%).” “Results showed no difference in residual pain, but favoured surgical management on ability to return to the same work and to wear the same shoes as before the fracture.” “Displaced calcaneal fractures are treated surgically from 1 level I evidence study, 1 level II, and multiple studies with less than level II evidence, with open reduction and internal fixation as the method of choice. If the fracture is less complex, percutaneous treatment can be a good alternative according to current level 3 and 4 retrospective data.” “The results from the current data appear to be promising; however, the lack of statistical power and inconsistent documentation have made it difficult to determine any superiority. The complication rates were much lower than those with open procedures, regardless of the technique. The percutaneous fixation technique appears to be a favorable option for displaced intra-articular calcaneal fractures. Percutaneous fixation using Kirschner wires presented the best results, however, evidence is insufficient to assert superiority of this treatment in comparison with other surgical techniques. Sanders II/III” |
| Pedobarography for outcomes [45] |
1 | 9 | “As a prediction tool, it should be more standardised. may be useful in developing customized aids such as insoles, aiming for a more individualized improvement.” |
| Circular external fixator [46] |
1 | 11 | “Pin site infections were common (22.6%), serious complications, including deep infection (0.8%), wound infection (1.6%), and complex regional pain syndrome (0.8%), were exceedingly rare.” |
| Open fractures [47] |
1 | 18 | The degree of exposure affects the result, especially on the wound healing time |
| Bone plug [15,48] |
2 | 32 9 |
“Bone grafts achieved better AOFAS scores than the non-bone graft group. The two groups had similar results in Böhler angle, Gissane angle, calcaneal width, and calcaneal height. No increased risk of postoperative complications was identified.” |
| Percutaneous osteosyntesis VS ORIF [49,50,51] |
3 | 15 18 9 |
No differences in functional scores ORIF < in wound complications |
| Peroneal tendons instability [52] |
1 | 9 | “Prevalence of peroneal tendon instability is associated with intraarticular calcaneal fractures and increases with the severity of the fracture.” |
| Timing of load bearing [53] |
1 | 72 | “The adverse sequelae which are assumed to be associated with starting partial weightbearing already within six weeks after internal fixation of calcaneal fractures, is not supported by literature data.” |
| Osteosintesys on cadaver [54] |
1 | 14 | “None of the studies found a significant difference in favor of any of the fixation methods.” |
| Percutaneal osteosyntheses [55] |
1 | 46 | “Best outcomes for the minimal invasive open surgical treatment of calcaneal fractures” |
| Cementation with Calcium Phosphate [56] |
1 | 14 | “Lower prevalence of pain at the fracture site”; loss of fracture reduction |
| Arthrodesys in Sanders type IV [57,58] |
2 | 7 22 |
“Good results considering the severe nature of the injury.” |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





