Submitted:
26 July 2023
Posted:
28 July 2023
You are already at the latest version
Abstract
Keywords:
- COVID-19 - Coronavirus infection disease 2019
- SARS-CoV-2 - Severe acute respiratory syndrome coronavirus 2
- MERS - Middle East Respiratory Syndrome
- S-protein - Spike protein
- ACE2 - Angiotensin-Converting Enzyme 2
- RBD - Receptor-Binding Domain
- ARDS - Acute respiratory distress syndrome
- PAMPs - Pathogen-Associated Molecular Patterns
- PRRs - Pattern Recognition Receptors
- DAMPs - Damage Associated Molecular Patterns
- TLR - Toll-like receptor
- NLR - Nucleotide-binding oligomerization domain-like receptors
- RLR - Retinoic Acid-Inducible Gene I Like Receptor
- ISG - IFN-Stimulated Gene
- TRAF - TNF-Receptor Associated Factor
- IKK - IĸB kinase
- TBK - TANK-binding kinase
- RAGE - Receptor for advanced glycation end-products
- RAAS - Renin-Angiotensin-Aldosterone System
- AT1 - Type 1 Angiotensin II Receptor
Author's contribution
Funding Statement
Conflicts of Interests
Ethics approval
Availability of data and materials
References
- Osuchowski MF, Aletti F, Cavaillon JM, et al. SARS-CoV-2/COVID-19: Evolving Reality, Global Response, Knowledge Gaps, and Opportunities. Shock. 2020;54(4):416-437. https://doi.org/10.1097/SHK.0000000000001565. [CrossRef]
- Salian VS, Wright JA, Vedell PT, et al. COVID-19 Transmission, Current Treatment, and Future Therapeutic Strategies. Mol Pharm. 2021;18(3):754-771. https://doi.org/10.1021/acs.molpharmaceut.0c00608. [CrossRef]
- Rochwerg B, Parke R, Murthy S, et al. Misinformation During the Coronavirus Disease 2019 Outbreak: How Knowledge Emerges From Noise. Crit Care Explor. 2020;2(4):e0098. https://doi.org/10.1097/cce.0000000000000098. [CrossRef]
- Zhou P, Yang X Lou, Wang XG, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579(7798):270-273. https://doi.org/10.1038/s41586-020-2012-7. [CrossRef]
- Wrapp D, Wang N, Corbett KS, et al. Cryo-EM structure of the 2019-nCoV spike in the prefusion conformation. Science (80- ). 2020;367(6483):1260-1263. https://doi.org/10.1126/science.aax0902. [CrossRef]
- Sungnak W, Huang N, Bécavin C, et al. SARS-CoV-2 entry factors are highly expressed in nasal epithelial cells together with innate immune genes. Nat Med. 2020;26(5):681-687. https://doi.org/10.1038/s41591-020-0868-6. [CrossRef]
- Rezaei N. COVID-19 affects healthy pediatricians more than pediatric patients. Infect Control Hosp Epidemiol. 2020;41(9):1106-1107. https://doi.org/10.1017/ice.2020.139. [CrossRef]
- Jia HP, Look DC, Shi L, et al. ACE2 Receptor Expression and Severe Acute Respiratory Syndrome Coronavirus Infection Depend on Differentiation of Human Airway Epithelia. J Virol. 2005;79(23):14614-14621. https://doi.org/10.1128/jvi.79.23.14614-14621.2005. [CrossRef]
- Hoffmann M, Kleine-Weber H, Schroeder S, et al. SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor. Cell. 2020;181(2):271-280.e8. https://doi.org/10.1016/j.cell.2020.02.052. [CrossRef]
- Coutard B, Valle C, de Lamballerie X, Canard B, Seidah NG, Decroly E. The spike glycoprotein of the new coronavirus 2019-nCoV contains a furin-like cleavage site absent in CoV of the same clade. Antiviral Res. 2020;176(February):104742. https://doi.org/10.1016/j.antiviral.2020.104742. [CrossRef]
- Cheng YW, Chao TL, Li CL, et al. Furin Inhibitors Block SARS-CoV-2 Spike Protein Cleavage to Suppress Virus Production and Cytopathic Effects. Cell Rep. 2020;33(2):108254. https://doi.org/10.1016/j.celrep.2020.108254. [CrossRef]
- Abassi ZA, Skorecki K, Heyman SN, Kinaneh S, Armaly Z. Covid-19 infection and mortality: A physiologist's perspective enlightening clinical features and plausible interventional strategies. Am J Physiol - Lung Cell Mol Physiol. 2020;318(5):L1020-L1022. https://doi.org/10.1152/AJPLUNG.00097.2020. [CrossRef]
- Gupta A, Madhavan M V., Sehgal K, et al. Extrapulmonary manifestations of COVID-19. Nat Med. 2020;26(7):1017-1032. https://doi.org/10.1038/s41591-020-0968-3. [CrossRef]
- Lonsdale J, Thomas J, Salvatore M, et al. The Genotype-Tissue Expression (GTEx) project. Nat Genet. 2013;45(6):580-585. https://doi.org/10.1038/ng.2653. [CrossRef]
- Zou X, Chen K, Zou J, Han P, Hao J, Han Z. Single-cell RNA-seq data analysis on the receptor ACE2 expression reveals the potential risk of different human organs vulnerable to 2019-nCoV infection. Front Med. 2020;14(2):185-192. https://doi.org/10.1007/s11684-020-0754-0 RESEARCH. [CrossRef]
- Xu H, Zhong L, Deng J, et al. High expression of ACE2 receptor of 2019-nCoV on the epithelial cells of oral mucosa. Int J Oral Sci. 2020;12(1):1-5. https://doi.org/10.1038/s41368-020-0074-x. [CrossRef]
- Conde Cardona G, Quintana Pájaro LD, Quintero Marzola ID, Ramos Villegas Y, Moscote Salazar LR. Neurotropism of SARS-CoV 2: Mechanisms and manifestations. J Neurol Sci. 2020;412:116824. https://doi.org/10.1016/j.jns.2020.116824. [CrossRef]
- Frontera JA, Sabadia S, Lalchan R, et al. A Prospective Study of Neurologic Disorders in Hospitalized Patients With COVID-19 in New York City. Neurology. 2021;96(4):e575-e586. https://doi.org/10.1212/WNL.0000000000010979. [CrossRef]
- Gänger S, Schindowski K. Tailoring formulations for intranasal nose-to-brain delivery: A review on architecture, physico-chemical characteristics and mucociliary clearance of the nasal olfactory mucosa. Pharmaceutics. 2018;10(3). https://doi.org/10.3390/pharmaceutics10030116. [CrossRef]
- Stevenson PG, Hawke S, Sloan DJ, Bangham CR. The immunogenicity of intracerebral virus infection depends on anatomical site. J Virol. 1997;71(1):145-151. https://doi.org/10.1128/jvi.71.1.145-151.1997. [CrossRef]
- Ye M, Ren Y, Lv T. Encephalitis as a clinical manifestation of COVID-19. Brain Behav Immun. 2020;88(April):945-946. https://doi.org/10.1016/j.bbi.2020.04.017. [CrossRef]
- Zhang H, Kang Z, Gong H, et al. Digestive system is a potential route of COVID-19: An analysis of single-cell coexpression pattern of key proteins in viral entry process. Gut. 2020;69(6):1010-1018. https://doi.org/10.1136/gutjnl-2020-320953. [CrossRef]
- Zhao X-Y, Xu X-X, Yin H-S, et al. Clinical Characteristics of Patients with 2019 Coronavirus disease in a non-Wuhan area of Hubei Province, China: a retrospective study. BMC Infect Dis. 2020;20(311). https://doi.org/10.21203/rs.3.rs-15734/v1. [CrossRef]
- Effenberger M, Grabherr F, Mayr L, et al. Faecal calprotectin indicates intestinal inflammation in COVID-19. Gut. 2020;69(8). [CrossRef]
- Lin L, Jiang X, Zhang Z, et al. Gastrointestinal symptoms of 95 cases with SARS-CoV-2 infection. Gut. 2020;69(6):997-1001. https://doi.org/10.1136/gutjnl-2020-321013. [CrossRef]
- Madissoon E, Wilbrey-Clark A, Miragaia RJ, et al. ScRNA-seq assessment of the human lung, spleen, and esophagus tissue stability after cold preservation. Genome Biol. 2019;21(1):1-16. https://doi.org/10.1186/s13059-019-1906-x. [CrossRef]
- Xu J, Xu X, Jiang L, Dua K, Hansbro PM, Liu G. SARS-CoV-2 induces transcriptional signatures in human lung epithelial cells that promote lung fibrosis. Respir Res. 2020;21(1):1-12. https://doi.org/10.1186/s12931-020-01445-6. [CrossRef]
- Mao L, Jin H, Wang M, et al. Neurologic Manifestations of Hospitalized Patients with Coronavirus Disease 2019 in Wuhan, China. JAMA Neurol. 2020;77(6):683-690. https://doi.org/10.1001/jamaneurol.2020.1127. [CrossRef]
- Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497-506. https://doi.org/10.1016/S0140-6736(20)30183-5. [CrossRef]
- Shi H, Han X, Jiang N, et al. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. Lancet Infect Dis. 2020;20(4):425-434. https://doi.org/10.1016/S1473-3099(20)30086-4. [CrossRef]
- Duffin J. Measuring the ventilatory response to hypoxia. J Physiol. 2007;584(1):285-293. https://doi.org/10.1113/jphysiol.2007.138883. [CrossRef]
- Brochard L, Slutsky A, Pesenti A. Mechanical ventilation to minimize progression of lung injury in acute respiratory failure. Am J Respir Crit Care Med. 2017;195(4):438-442. https://doi.org/10.1164/rccm.201605-1081CP. [CrossRef]
- Lang M, Som A, Mendoza DP, et al. Hypoxaemia related to COVID-19: vascular and perfusion abnormalities on dual-energy CT. Lancet Infect Dis. 2020;20(12):1365-1366. https://doi.org/10.1016/S1473-3099(20)30367-4. [CrossRef]
- Mo X, Jian W, Su Z, et al. Abnormal pulmonary function in COVID-19 patients at time of hospital discharge. Eur Respir J. 2020;55(6):2-5. https://doi.org/10.1183/13993003.01217-2020. [CrossRef]
- Tobin MJ, Laghi F, Jubran A. Why COVID-19 silent hypoxemia is baffling to physicians. Am J Respir Crit Care Med. 2020;202(3):356-360. https://doi.org/10.1164/rccm.202006-2157CP. [CrossRef]
- Dhont S, Derom E, Van Braeckel E, Depuydt P, Lambrecht BN. The pathophysiology of happy hypoxemia in COVID-19. Respir Res. 2020;21:198. https://doi.org/10.1186/s12931-020-01462-5. [CrossRef]
- Siswanto, Gani M, Fauzi AR, et al. Possible silent hypoxemia in a COVID-19 patient: A case report. Ann Med Surg. 2020;60:583-586. https://doi.org/10.1016/j.amsu.2020.11.053. [CrossRef]
- Williams AE, Chambers RC. The mercurial nature of neutrophils: Still an enigma in ARDS? Am J Physiol - Lung Cell Mol Physiol. 2014;306(3). https://doi.org/10.1152/ajplung.00311.2013. [CrossRef]
- Cameron MJ, Bermejo-Martin JF, Danesh A, Muller MP, Kelvin DJ. Human immunopathogenesis of severe acute respiratory syndrome (SARS). Virus Res. 2008;133(1):13-19. https://doi.org/10.1016/j.virusres.2007.02.014. [CrossRef]
- Channappanavar R, Perlman S. Pathogenic human coronavirus infections: causes and consequences of cytokine storm and immunopathology. Semin Immunopathol. 2017;39(5):529-539. https://doi.org/10.1007/s00281-017-0629-x. [CrossRef]
- Wilson MS, Wynn TA. Pulmonary fibrosis: Pathogenesis, etiology and regulation. Mucosal Immunol. 2009;2(2):103-121. https://doi.org/10.1038/mi.2008.85. [CrossRef]
- Eapen MS, Lu W, Gaikwad AV, et al. Endothelial to mesenchymal transition: a precursor to post-COVID-19 interstitial pulmonary fibrosis and vascular obliteration? Eur Respir J. 2020;56(4):2-4. https://doi.org/10.1183/13993003.03167-2020. [CrossRef]
- Chen W. A potential treatment of COVID-19 with TGF-β blockade. Int J Biol Sci. 2020;16(11):1954-1955. https://doi.org/10.7150/ijbs.46891. [CrossRef]
- Gu J, Korteweg C. Pathology and pathogenesis of severe acute respiratory syndrome. Am J Pathol. 2007;170(4):1136-1147. https://doi.org/10.2353/ajpath.2007.061088. [CrossRef]
- Hui DS, Joynt GM, Wong KT, et al. Impact of severe acute respiratory syndrome (SARS) on pulmonary function, functional capacity and quality of life in a cohort of survivors. Thorax. 2005;60(5):401-409. https://doi.org/10.1136/thx.2004.030205. [CrossRef]
- Menezes RG, Rizwan T, Saad Ali S, et al. Postmortem findings in COVID-19 fatalities: A systematic review of current evidence. Leg Med. 2021;54(October 2020):102001. https://doi.org/10.1016/j.legalmed.2021.102001. [CrossRef]
- Edler C, Schröder AS, Aepfelbacher M, et al. Dying with SARS-CoV-2 infection-an autopsy study of the first consecutive 80 cases in Hamburg, Germany (International journal of legal medicine (2020) 134 4 (1275-1284)). Int J Legal Med. 2020;134(5):1977. https://doi.org/10.1007/s00414-020-02336-7. [CrossRef]
- Yu M, Liu Y, Xu D, Zhang R, Lan L, Xu H. Prediction of the development of pulmonary fibrosis using serial thin-section ct and clinical features in patients discharged after treatment for COVID-19 pneumonia. Korean J Radiol. 2020;21(6):746-755. https://doi.org/10.3348/kjr.2020.0215. [CrossRef]
- Leisman DE, Ronner L, Pinotti R, et al. Cytokine elevation in severe and critical COVID-19: a rapid systematic review, meta-analysis, and comparison with other inflammatory syndromes. Lancet Respir Med. 2020;8(12):1233-1244. https://doi.org/10.1016/S2213-2600(20)30404-5. [CrossRef]
- Schaller T, Hirschbühl K, Burkhardt K, et al. Postmortem Examination of Patients with COVID-19. JAMA - J Am Med Assoc. 2020;323(24):2518-2520. https://doi.org/10.1001/jama.2020.8907. [CrossRef]
- Ackermann M, Verleden SE, Kuehnel M, et al. Pulmonary Vascular Endothelialitis, Thrombosis, and Angiogenesis in Covid-19. N Engl J Med. 2020;383(2):120-128. https://doi.org/10.1056/nejmoa2015432. [CrossRef]
- Buja LM, Wolf D, Zhao B, et al. The emerging spectrum of cardiopulmonary pathology of the coronavirus disease 2019 (COVID-19): Report of 3 autopsies from Houston, Texas, and review of autopsy findings from other United States cities. Cardiovasc Pathol. 2020;48:107233. https://doi.org/10.1016/j.carpath.2020.107233. [CrossRef]
- Sadegh Beigee F, Pourabdollah Toutkaboni M, Khalili N, et al. Diffuse alveolar damage and thrombotic microangiopathy are the main histopathological findings in lung tissue biopsy samples of COVID-19 patients. Pathol Res Pract. 2020;216(10):153228. https://doi.org/10.1016/j.prp.2020.153228. [CrossRef]
- Varga Z, Flammer AJ, Steiger P, et al. Endothelial cell infection and endotheliitis in COVID-19. Lancet. 2020;395(10234):1417-1418. https://doi.org/10.1016/S0140-6736(20)30937-5. [CrossRef]
- Osuchowski MF, Winkler MS, Skirecki T, et al. The COVID-19 puzzle: deciphering pathophysiology and phenotypes of a new disease entity. Lancet Respir Med. 2021;9(6):622-642. https://doi.org/10.1016/S2213-2600(21)00218-6. [CrossRef]
- Su H, Yang M, Wan C, et al. Renal histopathological analysis of 26 postmortem findings of patients with COVID-19 in China. Kidney Int. 2020;98(1):219-227. https://doi.org/10.1016/j.kint.2020.04.003. [CrossRef]
- Kral AH, Lambdin BH, Wenger LD, Davidson PJ. Multiorgan and Renal Tropism of SARS-CoV-2. N Engl J Med. 2020;383(6):589-590. https://doi.org/10.1056/nejmc2015435. [CrossRef]
- Srinivasan S, Cui H, Gao Z, et al. Structural genomics of SARS-COV-2 indicates evolutionary conserved functional regions of viral proteins. Viruses. 2020;12(4). https://doi.org/10.3390/v12040360. [CrossRef]
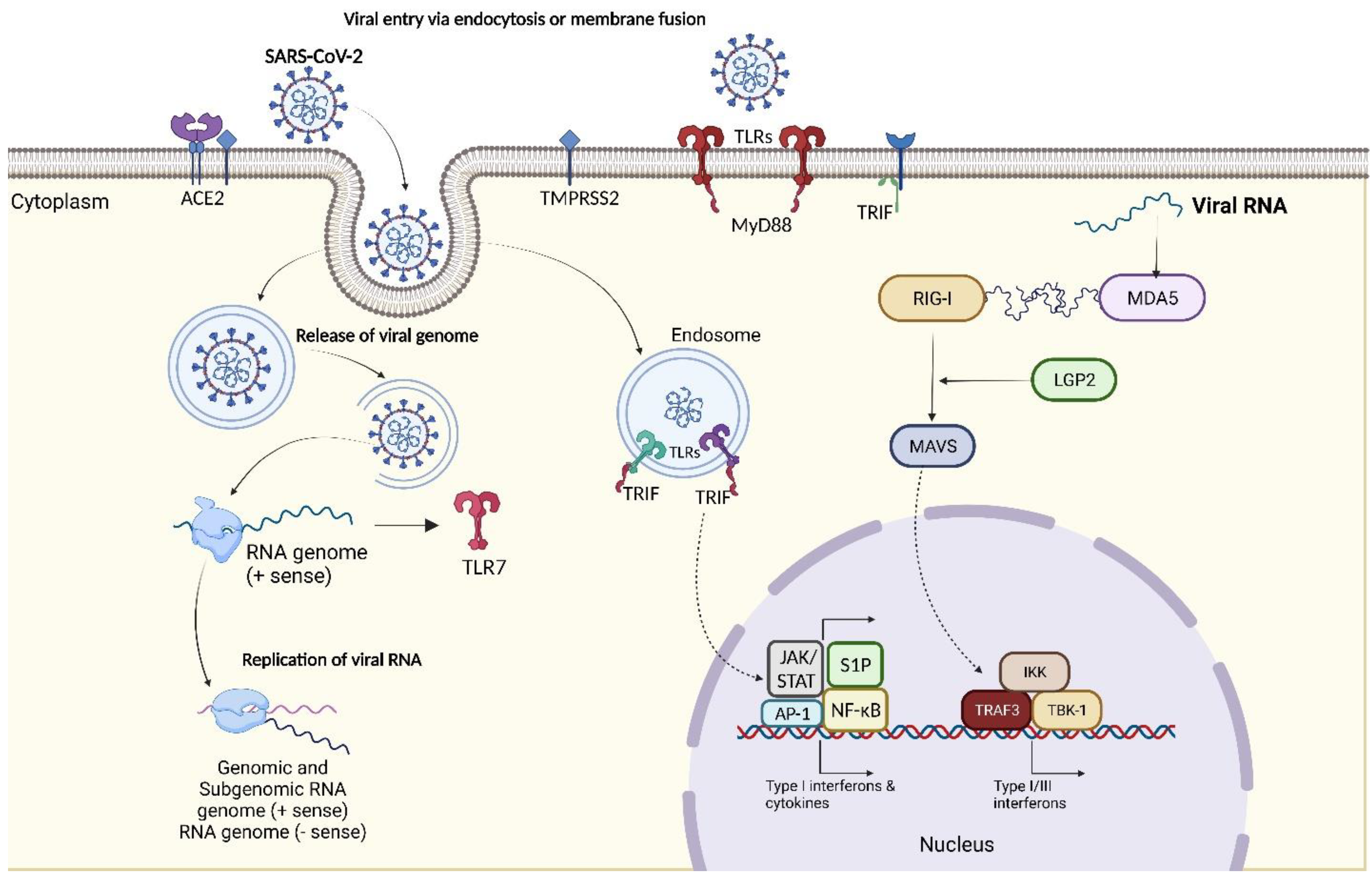
- Li X, Geng M, Peng Y, Meng L, Lu S. Molecular immune pathogenesis and diagnosis of COVID-19. J Pharm Anal. 2020;10(2):102-108. https://doi.org/10.1016/j.jpha.2020.03.001. [CrossRef]
- Kanneganti TD. Intracellular innate immune receptors: Life inside the cell. Immunol Rev. 2020;297(1):5-12. https://doi.org/10.1111/imr.12912. [CrossRef]
- Kawasaki T, Kawai T. Toll-like receptor signaling pathways. Front Immunol. 2014;5(SEP):1-8. https://doi.org/10.3389/fimmu.2014.00461. [CrossRef]
- Zheng M, Karki R, Williams EP, et al. TLR2 senses the SARS-CoV-2 envelope protein to produce inflammatory cytokines. Nat Immunol. 2021;22(7):829-838. https://doi.org/10.1038/s41590-021-00937-x. [CrossRef]
- Potapov I, Kanneganti TD, del Sol A. Fostering experimental and computational synergy to modulate hyperinflammation. Trends Immunol. 2022;43(1):4-7. https://doi.org/10.1016/j.it.2021.11.004. [CrossRef]
- Jung S, Potapov I, Chillara S, del Sol A. Leveraging systems biology for predicting modulators of inflammation in patients with COVID-19. Sci Adv. 2021;7(6):1-11. https://doi.org/10.1126/sciadv.abe5735. [CrossRef]
- Choudhury A, Mukherjee S. In silico studies on the comparative characterization of the interactions of SARS-CoV-2 spike glycoprotein with ACE-2 receptor homologs and human TLRs. J Med Virol. 2020;92(10):2105-2113. https://doi.org/10.1002/jmv.25987. [CrossRef]
- Asano T, Boisson B, Onodi F, et al. X-linked recessive TLR7 deficiency in ~1% of men under 60 years old with life-threatening COVID-19. Sci Immunol. 2021;6(62). https://doi.org/10.1126/sciimmunol.abl4348. [CrossRef]
- Van Der Made CI, Simons A, Schuurs-Hoeijmakers J, et al. Presence of Genetic Variants among Young Men with Severe COVID-19. JAMA - J Am Med Assoc. 2020;324(7):663-673. https://doi.org/10.1001/jama.2020.13719. [CrossRef]
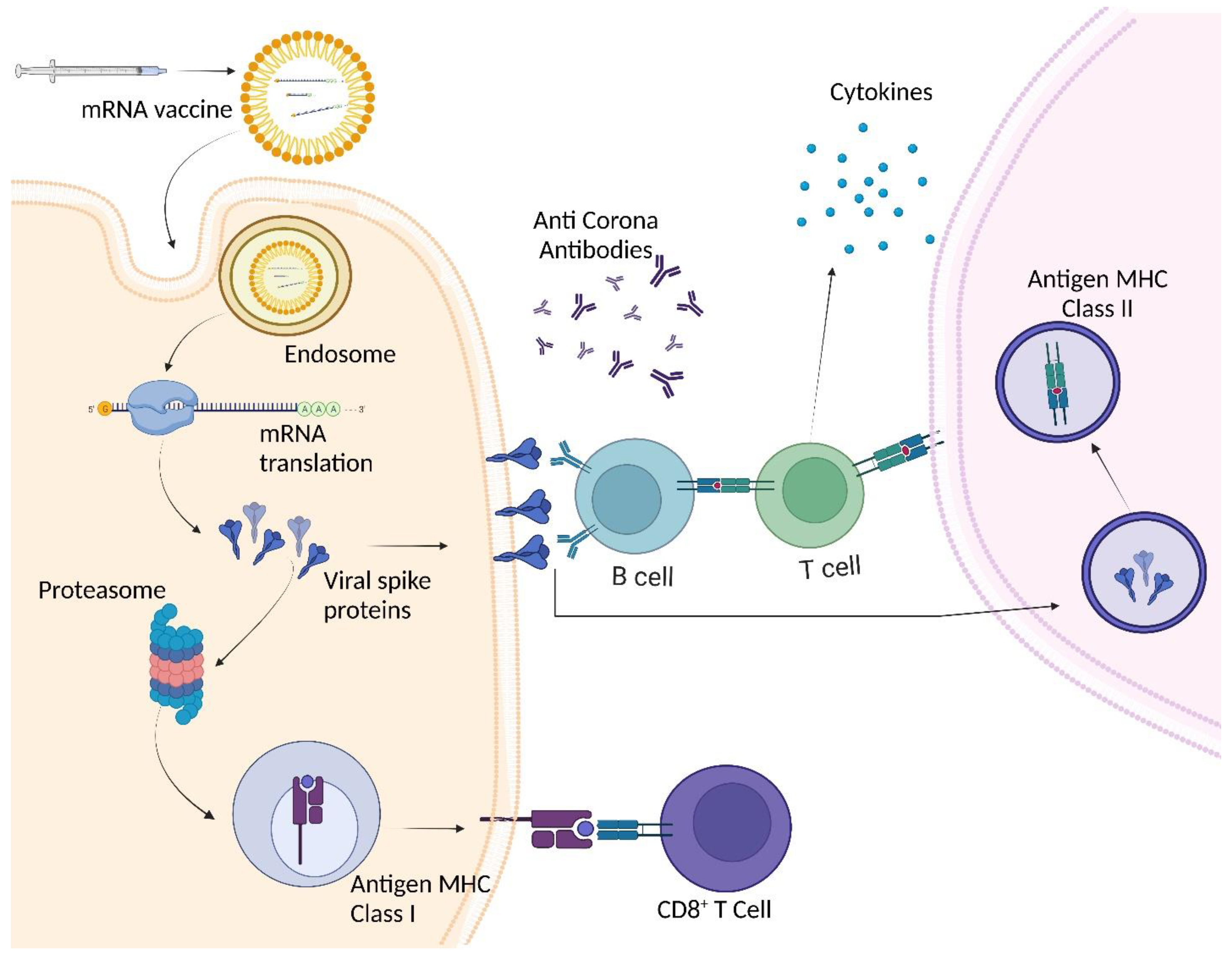
- Prompetchara E, Ketloy C, Palaga T. Immune responses in COVID-19 and potential vaccines: Lessons learned from SARS and MERS epidemic. Asian Pacific J Allergy Immunol. 2020;38(1):1-9. https://doi.org/10.12932/AP-200220-0772. [CrossRef]
- Marcken M de, Dhaliwal K, Danielsen AC, Gautron AS, Dominguez-Villar M. TLR7 and TLR8 activate distinct pathways in monocytes during RNA virus infection. Sci Signal. 2019;12(605):1-19. https://doi.org/10.1126/scisignal.aaw1347. [CrossRef]
- Spiegel S, Milstien S. The outs and the ins of sphingosine-1-phosphate in immunity. Nat Rev Immunol. 2011;11(6):403-415. https://doi.org/10.1038/nri2974. [CrossRef]
- De Wit E, Van Doremalen N, Falzarano D, Munster VJ. SARS and MERS: Recent insights into emerging coronaviruses. Nat Rev Microbiol. 2016;14(8):523-534. https://doi.org/10.1038/nrmicro.2016.81. [CrossRef]
- Barnes BJ, Adrover JM, Baxter-Stoltzfus A, et al. Targeting potential drivers of COVID-19: Neutrophil extracellular traps. J Exp Med. 2020;217(6):1-7. https://doi.org/10.1084/jem.20200652. [CrossRef]
- Wack A, Terczyńska-Dyla E, Hartmann R. Guarding the frontiers: The biology of type III interferons. Nat Immunol. 2015;16(8):802-809. https://doi.org/10.1038/ni.3212. [CrossRef]
- Loo YM, Gale M. Immune Signaling by RIG-I-like Receptors. Immunity. 2011;34(5):680-692. https://doi.org/10.1016/j.immuni.2011.05.003. [CrossRef]
- Horner SM, Liu HM, Park HS, Briley J, Gale M. Mitochondrial-associated endoplasmic reticulum membranes (MAM) form innate immune synapses and are targeted by hepatitis C virus. Proc Natl Acad Sci U S A. 2011;108(35):14590-14595. https://doi.org/10.1073/pnas.1110133108. [CrossRef]
- Stark GR, Darnell JE. The JAK-STAT Pathway at Twenty. Immunity. 2012;36(4):503-514. https://doi.org/10.1016/j.immuni.2012.03.013. [CrossRef]
- Yin X, Riva L, Pu Y, et al. MDA5 Governs the Innate Immune Response to SARS-CoV-2 in Lung Epithelial Cells. Cell Rep. 2021;34(2). https://doi.org/10.1016/j.celrep.2020.108628. [CrossRef]
- Rebendenne A, Chaves Valadão AL, Tauziet M, et al. SARS-CoV-2 Triggers an MDA-5-Dependent Interferon Response Which Is Unable To Control Replication in Lung Epithelial Cells. J Virol. 2021;95(8). https://doi.org/10.1128/jvi.02415-20. [CrossRef]
- Thorne LG, Reuschl A, Zuliani-Alvarez L, et al. SARS-CoV-2 sensing by RIG-I and MDA5 links epithelial infection to macrophage inflammation. EMBO J. 2021;40(15):1-17. https://doi.org/10.15252/embj.2021107826. [CrossRef]
- Christgen S, Kanneganti TD. Inflammasomes and the fine line between defense and disease. Curr Opin Immunol. 2020;62:39-44. https://doi.org/10.1016/j.coi.2019.11.007. [CrossRef]
- Kayagaki N, Kornfeld OS, Lee BL, et al. NINJ1 mediates plasma membrane rupture during lytic cell death. Nature. 2021;591(7848):131-136. https://doi.org/10.1038/s41586-021-03218-7. [CrossRef]
- Diamond MS, Kanneganti T-D. Innate immunity: the first line of defense against SARS-CoV-2. Nat Immunol. 2022;23(2):165-176. https://doi.org/10.1038/s41590-021-01091-0. [CrossRef]
- Anand U, Jakhmola S, Indari O, et al. Potential Therapeutic Targets and Vaccine Development for SARS-CoV-2/COVID-19 Pandemic Management: A Review on the Recent Update. Front Immunol. 2021;12(December 2019):1-27. https://doi.org/10.3389/fimmu.2021.658519. [CrossRef]
- Ye X, Xiao X, Li B, et al. Low Humoral Immune Response and Ineffective Clearance of SARS-Cov-2 in a COVID-19 Patient With CLL During a 69-Day Follow-Up. Front Oncol. 2020;10(July):1-7. https://doi.org/10.3389/fonc.2020.01272. [CrossRef]
- Wen W, Su W, Tang H, et al. Immune cell profiling of COVID-19 patients in the recovery stage by single-cell sequencing. Cell Discov. 2020;6(1). https://doi.org/10.1038/s41421-020-0168-9. [CrossRef]
- You X, Zhang R, Shao M, et al. Double Negative B Cell Is Associated With Renal Impairment in Systemic Lupus Erythematosus and Acts as a Marker for Nephritis Remission. Front Med. 2020;7(April):1-9. https://doi.org/10.3389/fmed.2020.00085. [CrossRef]
- Zhu L, Yin Z, Ju B, et al. Altered frequencies of memory B cells in new-onset systemic lupus erythematosus patients. Clin Rheumatol. 2018;37(1):205-212. https://doi.org/10.1007/s10067-017-3877-1. [CrossRef]
- Li CK, Wu H, Yan H, et al. T Cell Responses to Whole SARS Coronavirus in Humans. J Immunol. 2008;181(8):5490-5500. https://doi.org/10.4049/jimmunol.181.8.5490. [CrossRef]
- Casillo GM, Mansour AA, Raucci F, et al. Could IL-17 represent a new therapeutic target for the treatment and/or management of COVID-19-related respiratory syndrome? Pharmacol Res. 2020;156(April):104791. https://doi.org/10.1016/j.phrs.2020.104791. [CrossRef]
- Yazdanpanah F, Hamblin MR, Rezaei N. The immune system and COVID-19: Friend or foe? Life Sci. 2020;256(May):117900. https://doi.org/10.1016/j.lfs.2020.117900. [CrossRef]
- Bhattacharjee A, Saha M, Halder A, Debnath A, Mukherjee O. Therapeutics and Vaccines: Strengthening Our Fight Against the Global Pandemic COVID-19. Curr Microbiol. 2021;78(2):435-448. https://doi.org/10.1007/s00284-020-02310-x. [CrossRef]
- Klasse PJ. Neutralization of Virus Infectivity by Antibodies: Old Problems in New Perspectives. Adv Biol. 2014;2014:1-24. https://doi.org/10.1155/2014/157895. [CrossRef]
- Ju B, Zhang Q, Ge J, et al. Human neutralizing antibodies elicited by SARS-CoV-2 infection. Nature. 2020;584(7819):115-119. https://doi.org/10.1038/s41586-020-2380-z. [CrossRef]
- To KKW, Tsang OTY, Leung WS, et al. Temporal profiles of viral load in posterior oropharyngeal saliva samples and serum antibody responses during infection by SARS-CoV-2: an observational cohort study. Lancet Infect Dis. 2020;20(5):565-574. https://doi.org/10.1016/S1473-3099(20)30196-1. [CrossRef]
- Amanat F, Stadlbauer D, Strohmeier S, et al. A serological assay to detect SARS-CoV-2 seroconversion in humans. Nat Med. 2020;26(7):1033-1036. https://doi.org/10.1038/s41591-020-0913-5. [CrossRef]
- Mo H, Zeng G, Ren X, et al. Longitudinal profile of antibodies against SARS-coronavirus in SARS patients and their clinical significance. Respirology. 2006;11(1):49-53. https://doi.org/10.1111/j.1440-1843.2006.00783.x. [CrossRef]
- Wu LP, Wang NC, Chang YH, et al. Duration of antibody responses after severe acute respiratory syndrome. Emerg Infect Dis. 2007;13(10):1562-1564. https://doi.org/10.3201/eid1310.070576. [CrossRef]
- Dan JM, Mateus J, Kato Y, et al. Immunological memory to SARS-CoV-2 assessed for up to 8 months after infection. Science (80- ). 2021;371(6529). https://doi.org/10.1126/science.abf4063. [CrossRef]
- Mahal BA, Alshalalfa M, Kensler KH, et al. Rapid Decay of Anti–SARS-CoV-2 Antibodies in Persons with Mild Covid-19. N Engl J Med. 2020;383(11):1083-1085. https://doi.org/10.1056/nejmc2000069. [CrossRef]
- Seow J, Graham C, Merrick B, et al. Longitudinal observation and decline of neutralizing antibody responses in the three months following SARS-CoV-2 infection in humans. Nat Microbiol. 2020;5(12):1598-1607. https://doi.org/10.1038/s41564-020-00813-8. [CrossRef]
- Long QX, Tang XJ, Shi QL, et al. Clinical and immunological assessment of asymptomatic SARS-CoV-2 infections. Nat Med. 2020;26(8):1200-1204. https://doi.org/10.1038/s41591-020-0965-6. [CrossRef]
- Infantino M, Damiani A, Li Gobbi F, et al. Serological assays for sars-cov-2 infectious disease: Benefits, limitations and perspectives. Isr Med Assoc J. 2020;22(4):203-210.
- Lessler J, Reich NG, Brookmeyer R, Perl TM, Nelson KE, Cummings DA. Incubation periods of acute respiratory viral infections: a systematic review. Lancet Infect Dis. 2009;9(5):291-300. https://doi.org/10.1016/S1473-3099(09)70069-6. [CrossRef]
- Zhang Y, Zhang J, Chen Y, et al. The ORF8 protein of SARS-CoV-2 mediates immune evasion through potently downregulating MHC-I. bioRxiv. Published online 2020. https://doi.org/10.1101/2020.05.24.111823. [CrossRef]
- Wilk AJ, Rustagi A, Zhao NQ, et al. A single-cell atlas of the peripheral immune response in patients with severe COVID-19. Nat Med. 2020;26(7):1070-1076. https://doi.org/10.1038/s41591-020-0944-y. [CrossRef]
- Giamarellos-Bourboulis EJ, Netea MG, Rovina N, et al. Complex Immune Dysregulation in COVID-19 Patients with Severe Respiratory Failure. Cell Host Microbe. 2020;27(6):992-1000.e3. https://doi.org/10.1016/j.chom.2020.04.009. [CrossRef]
- Arabi YM, Murthy S, Webb S. COVID-19: a novel coronavirus and a novel challenge for critical care. Intensive Care Med. 2020;46(5):833-836. https://doi.org/10.1007/s00134-020-05955-1. [CrossRef]
- Qin C, Zhou L, Hu Z, et al. Dysregulation of immune response in patients with coronavirus 2019 (COVID-19) in Wuhan, China. Clin Infect Dis. 2020;71(15):762-768. https://doi.org/10.1093/cid/ciaa248. [CrossRef]
- Dong P, Ju X, Yan Y, et al. γδ T Cells Provide Protective Function in Highly Pathogenic Avian H5N1 Influenza A Virus Infection. Front Immunol. 2018;9(December):1-11. https://doi.org/10.3389/fimmu.2018.02812. [CrossRef]
- Bahl K, Kim S-K, Calcagno C, et al. IFN-Induced Attrition of CD8 T Cells in the Presence or Absence of Cognate Antigen during the Early Stages of Viral Infections. J Immunol. 2006;176(7):4284-4295. https://doi.org/10.4049/jimmunol.176.7.4284. [CrossRef]
- Shiow LR, Rosen DB, Brdičková N, et al. CD69 acts downstream of interferon-α/β to inhibit S1P 1 and lymphocyte egress from lymphoid organs. Nature. 2006;440(7083):540-544. https://doi.org/10.1038/nature04606. [CrossRef]
- Gordon DE, Jang GM, Bouhaddou M, et al. A SARS-CoV-2 protein interaction map reveals targets for drug repurposing. Nature. 2020;583(7816):459-468. https://doi.org/10.1038/s41586-020-2286-9. [CrossRef]
- Diao B, Wang C, Tan Y, et al. Reduction and Functional Exhaustion of T Cells in Patients With Coronavirus Disease 2019 (COVID-19). Front Immunol. 2020;11(May):1-7. https://doi.org/10.3389/fimmu.2020.00827. [CrossRef]
- Zheng M, Gao Y, Wang G, et al. Functional exhaustion of antiviral lymphocytes in COVID-19 patients. Cell Mol Immunol. 2020;17(5):533-535. https://doi.org/10.1038/s41423-020-0402-2. [CrossRef]
- Oja AE, Saris A, Ghandour CA, et al. Divergent SARS-CoV-2-specific T- and B-cell responses in severe but not mild COVID-19 patients. Eur J Immunol. 2020;50(12):1998-2012. https://doi.org/10.1002/eji.202048908. [CrossRef]
- Chen G, Wu D, Guo W, et al. Clinical and immunological features of severe and moderate coronavirus disease 2019. J Clin Invest. 2020;130(5):2620-2629. https://doi.org/10.1172/JCI137244. [CrossRef]
- Wong CK, Lam CWK, Wu AKL, et al. Plasma inflammatory cytokines and chemokines in severe acute respiratory syndrome. Clin Exp Immunol. 2004;136(1):95-103. https://doi.org/10.1111/j.1365-2249.2004.02415.x. [CrossRef]
- Rokni M, Ghasemi V, Tavakoli Z. Immune responses and pathogenesis of SARS-CoV-2 during an outbreak in Iran: Comparison with SARS and MERS. Rev Med Virol. 2020;30(3). https://doi.org/10.1002/rmv.2107. [CrossRef]
- Wu D, Yang XO. TH17 responses in cytokine storm of COVID-19: An emerging target of JAK2 inhibitor Fedratinib. J Microbiol Immunol Infect. 2020;53(3):368-370. https://doi.org/10.1016/j.jmii.2020.03.005. [CrossRef]
- Davis BK, Wen H, Ting JPY. The Inflammasome NLRs in immunity, inflammation, and associated diseases. Annu Rev Immunol. 2011;29:707-735. https://doi.org/10.1146/annurev-immunol-031210-101405. [CrossRef]
- Hou W, Jin Y-H, Kang HS, Kim BS. Interleukin-6 (IL-6) and IL-17 Synergistically Promote Viral Persistence by Inhibiting Cellular Apoptosis and Cytotoxic T Cell Function. J Virol. 2014;88(15):8479-8489. https://doi.org/10.1128/jvi.00724-14. [CrossRef]
- Lin L, Lu L, Cao W, Li T. Hypothesis for potential pathogenesis of SARS-CoV-2 infection–a review of immune changes in patients with viral pneumonia. Emerg Microbes Infect. 2020;9(1):727-732. https://doi.org/10.1080/22221751.2020.1746199. [CrossRef]
- Li X, Xu S, Yu M, et al. Risk factors for severity and mortality in adult COVID-19 inpatients in Wuhan. J Allergy Clin Immunol. 2020;146(1):110-118. https://doi.org/10.1016/j.jaci.2020.04.006. [CrossRef]
- Vita G, Syambani Z. Crucial laboratory parameters in COVID-19 diagnosis and prognosis: An updated meta-analysis. Med Clin. 2020;155(4):143-151. [CrossRef]
- Rokni M, Hamblin MR, Rezaei N. Cytokines and COVID-19: friends or foes? Hum Vaccines Immunother. 2020;16(10):2363-2365. https://doi.org/10.1080/21645515.2020.1799669. [CrossRef]
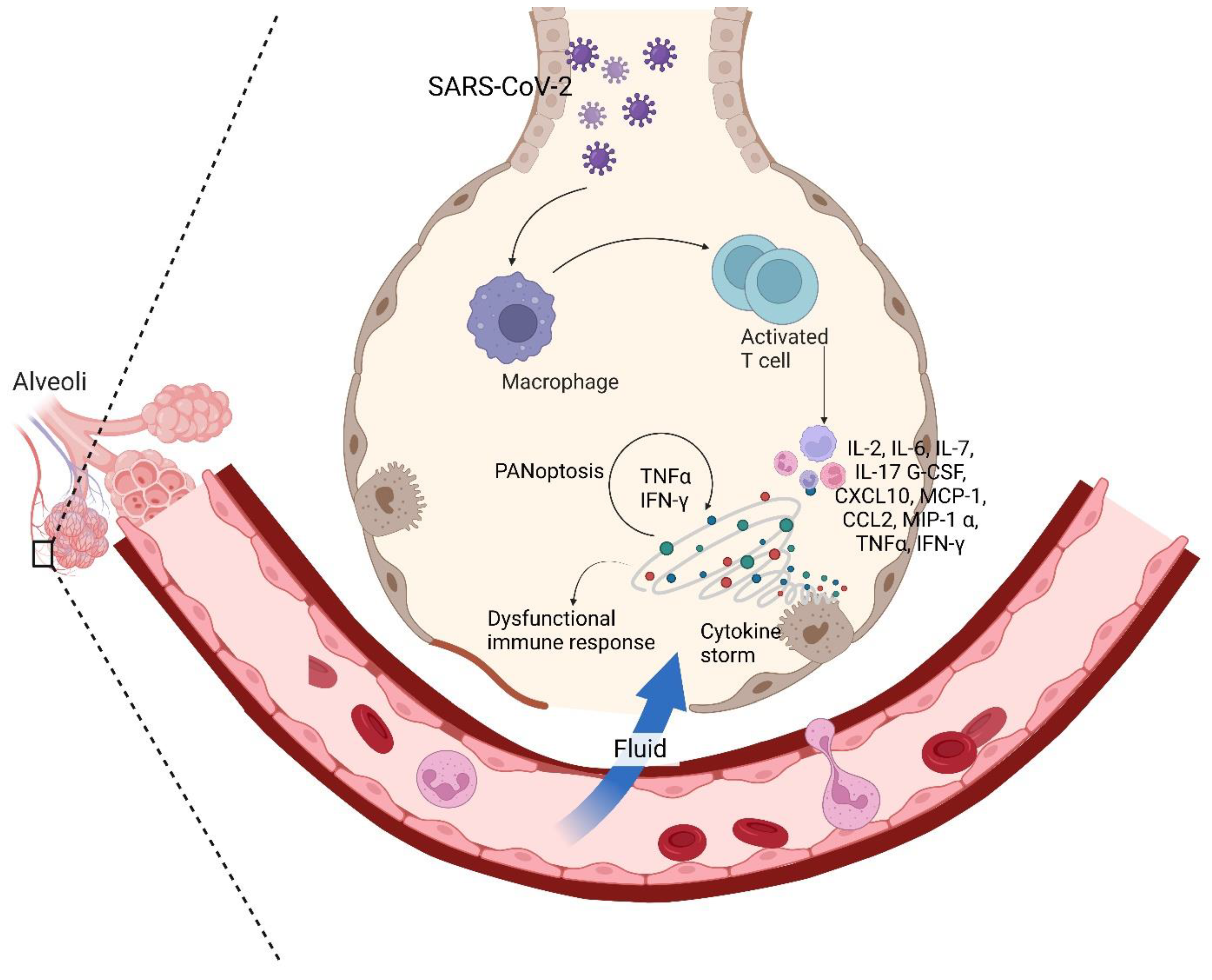
- Karki R, Kanneganti TD. The 'cytokine storm': molecular mechanisms and therapeutic prospects. Trends Immunol. 2021;42(8):681-705. https://doi.org/10.1016/j.it.2021.06.001. [CrossRef]
- Karki R, Sharma BR, Tuladhar S, et al. Synergism of TNF-α and IFN-γ Triggers Inflammatory Cell Death, Tissue Damage, and Mortality in SARS-CoV-2 Infection and Cytokine Shock Syndromes. Cell. 2021;184(1):149-168.e17. https://doi.org/10.1016/j.cell.2020.11.025. [CrossRef]
- Kuriakose T, Man SM, Subbarao Malireddi RK, et al. ZBP1/DAI is an innate sensor of influenza virus triggering the NLRP3 inflammasome and programmed cell death pathways. Sci Immunol. 2016;1(2). https://doi.org/10.1126/sciimmunol.aag2045. [CrossRef]
- Malireddi RKS, Gurung P, Kesavardhana S, et al. Innate immune priming in the absence of TAK1 drives RIPK1 kinase activity–independent pyroptosis, apoptosis, necroptosis, and inflammatory disease. J Exp Med. 2020;217(3):1-13. https://doi.org/10.1084/jem_20191644. [CrossRef]
- Malireddi RKS, Gurung P, Mavuluri J, et al. TAK1 restricts spontaneous NLRP3 activation and cell death to control myeloid proliferation. J Exp Med. 2018;215(4):1023-1034. https://doi.org/10.1084/jem.20171922. [CrossRef]
- Gurung P, Anand PK, Malireddi RKS, et al. FADD and Caspase-8 Mediate Priming and Activation of the Canonical and Noncanonical Nlrp3 Inflammasomes. J Immunol. 2014;192(4):1835-1846. https://doi.org/10.4049/jimmunol.1302839. [CrossRef]
- Schwarzer R, Laurien L, Pasparakis M. New insights into the regulation of apoptosis, necroptosis, and pyroptosis by receptor interacting protein kinase 1 and caspase-8. Curr Opin Cell Biol. 2020;63:186-193. https://doi.org/10.1016/j.ceb.2020.02.004. [CrossRef]
- Fritsch M, Günther SD, Schwarzer R, et al. Caspase-8 is the molecular switch for apoptosis, necroptosis and pyroptosis. Nature. 2019;575(7784):683-687. https://doi.org/10.1038/s41586-019-1770-6. [CrossRef]
- Newton K, Wickliffe KE, Maltzman A, et al. Activity of caspase-8 determines plasticity between cell death pathways. Nature. 2019;575(7784):679-682. https://doi.org/10.1038/s41586-019-1752-8. [CrossRef]
- Malireddi RKS, Kesavardhana S, Karki R, Kancharana B, Burton AR, Kanneganti T-D. RIPK1 Distinctly Regulates Yersinia -Induced Inflammatory Cell Death, PANoptosis . ImmunoHorizons. 2020;4(12):789-796. https://doi.org/10.4049/immunohorizons.2000097. [CrossRef]
- Totura AL, Whitmore A, Agnihothram S, et al. Toll-like receptor 3 signaling via TRIF contributes to a protective innate immune response to severe acute respiratory syndrome coronavirus infection. MBio. 2015;6(3):1-14. https://doi.org/10.1128/mBio.00638-15. [CrossRef]
- Onofrio L, Caraglia M, Facchini G, Margherita V, Placido S De, Buonerba C. Toll-like receptors and COVID-19: A two-faced story with an exciting ending. Futur Sci OA. 2020;6(8):10-13. https://doi.org/10.2144/fsoa-2020-0091. [CrossRef]
- Merad M, Martin JC. Pathological inflammation in patients with COVID-19: a key role for monocytes and macrophages. Nat Rev Immunol. 2020;20(6):355-362. https://doi.org/10.1038/s41577-020-0331-4. [CrossRef]
- Sinha P, Matthay MA, Calfee CS. Is a "cytokine Storm" Relevant to COVID-19? JAMA Intern Med. 2020;180(9):1152-1154. https://doi.org/10.1001/jamainternmed.2020.3313. [CrossRef]
- Chen X, Zhao B, Qu Y, et al. Detectable Serum Severe Acute Respiratory Syndrome Coronavirus 2 Viral Load (RNAemia) Is Closely Correlated with Drastically Elevated Interleukin 6 Level in Critically Ill Patients with Coronavirus Disease 2019. Clin Infect Dis. 2020;71(8):1937-1942. https://doi.org/10.1093/cid/ciaa449. [CrossRef]
- Gao Y, Li T, Han M, et al. Diagnostic utility of clinical laboratory data determinations for patients with the severe COVID-19. J Med Virol. 2020;92(7):791-796. https://doi.org/10.1002/jmv.25770. [CrossRef]
- Ruan Q, Yang K, Wang W, Jiang L, Song J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med. 2020;46(5):846-848. https://doi.org/10.1007/s00134-020-05991-x. [CrossRef]
- Bösmüller H, Traxler S, Bitzer M, et al. The evolution of pulmonary pathology in fatal COVID-19 disease: an autopsy study with clinical correlation. Virchows Arch. 2020;477(3):349-357. https://doi.org/10.1007/s00428-020-02881-x. [CrossRef]
- Yang L, Han Y, Nilsson-Payant BE, et al. A Human Pluripotent Stem Cell-based Platform to Study SARS-CoV-2 Tropism and Model Virus Infection in Human Cells and Organoids. Cell Stem Cell. 2020;27(1):125-136.e7. https://doi.org/10.1016/j.stem.2020.06.015. [CrossRef]
- Xu Z, Shi L, Wang Y, et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med. 2020;8(4):420-422. https://doi.org/10.1016/S2213-2600(20)30076-X. [CrossRef]
- Pensato U, Muccioli L, Cani I, et al. Brain dysfunction in COVID-19 and CAR-T therapy: cytokine storm-associated encephalopathy. Ann Clin Transl Neurol. 2021;8(4):968-979. https://doi.org/10.1002/acn3.51348. [CrossRef]
- Kempuraj D, Selvakumar GP, Ahmed ME, et al. COVID-19, Mast Cells, Cytokine Storm, Psychological Stress, and Neuroinflammation. Neuroscientist. 2020;26(5-6):402-414. https://doi.org/10.1177/1073858420941476. [CrossRef]
- Ahmadian E, Hosseiniyan Khatibi SM, Razi Soofiyani S, et al. Covid-19 and kidney injury: Pathophysiology and molecular mechanisms. Rev Med Virol. 2021;31(3):1-13. https://doi.org/10.1002/rmv.2176. [CrossRef]
- Premkumar M, Kedarisetty CK. Cytokine storm of covid-19 and its impact on patients with and without chronic liver disease. J Clin Transl Hepatol. 2021;9(2):256-264. https://doi.org/10.14218/JCTH.2021.00055. [CrossRef]
- Cococcia S, Lenti MV, Santacroce G, Achilli G, de Andreis FB, Sabatino A Di. Liver-spleen axis dysfunction in COVID-19. World J Gastroenterol. 2021;27(35):5919-5931. https://doi.org/10.3748/wjg.v27.i35.5919. [CrossRef]
- Peng X, Wang Y, Xi X, et al. Promising Therapy for Heart Failure in Patients with Severe COVID-19: Calming the Cytokine Storm. Cardiovasc Drugs Ther. 2021;35(2):231-247. https://doi.org/10.1007/s10557-020-07120-8. [CrossRef]
- Yang X, Yu Y, Xu J, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020;8(5):475-481. https://doi.org/10.1016/S2213-2600(20)30079-5. [CrossRef]
- Zhu L, She ZG, Cheng X, et al. Association of Blood Glucose Control and Outcomes in Patients with COVID-19 and Pre-existing Type 2 Diabetes. Cell Metab. 2020;31(6):1068-1077.e3. https://doi.org/10.1016/j.cmet.2020.04.021. [CrossRef]
- Marshall RJ, Armart P, Hulme KD, et al. Glycemic variability in Diabetes increases the severity of influenza. MBio. 2020;11(2). https://doi.org/10.1128/mBio.02841-19. [CrossRef]
- Nielsen TB, Pantapalangkoor P, Yan J, et al. Diabetes exacerbates infection via hyperinflammation by signaling through TLR4 and RAGE. MBio. 2017;8(4). https://doi.org/10.1128/mBio.00818-17. [CrossRef]
- Pal R, Bhansali A. COVID-19, diabetes mellitus and ACE2: The conundrum. Diabetes Res Clin Pract. 2020;162(January). [CrossRef]
- Gebhard C, Regitz-Zagrosek V, Neuhauser HK, Morgan R, Klein SL. Impact of sex and gender on COVID-19 outcomes in Europe. Biol Sex Differ. 2020;11(1):1-13. https://doi.org/10.1186/s13293-020-00304-9. [CrossRef]
- Busse LW, Chow JH, McCurdy MT, Khanna AK. COVID-19 and the RAAS - A potential role for angiotensin II? Crit Care. 2020;24(1):1-4. https://doi.org/10.1186/s13054-020-02862-1. [CrossRef]
- Han Y, Runge MS, Brasier AR. Angiotensin II induces interleukin-6 transcription in vascular smooth muscle cells through pleiotropic activation of nuclear factor-κb transcription factors. Circ Res. 1999;84(6):695-703. https://doi.org/10.1161/01.RES.84.6.695. [CrossRef]
- Carissimo G, Xu W, Kwok I, et al. Whole blood immunophenotyping uncovers immature neutrophil-to-VD2 T-cell ratio as an early marker for severe COVID-19. Nat Commun. 2020;11(1):1-12. https://doi.org/10.1038/s41467-020-19080-6. [CrossRef]
- Bordoni V, Sacchi A, Cimini E, et al. An inflammatory profile correlates with decreased frequency of cytotoxic cells in coronavirus disease 2019. Clin Infect Dis. 2020;71(16):2272-2275. https://doi.org/10.1093/cid/ciaa577. [CrossRef]
- Silvin A, Chapuis N, Dunsmore G, et al. Elevated Calprotectin and Abnormal Myeloid Cell Subsets Discriminate Severe from Mild COVID-19. Cell. 2020;182(6):1401-1418.e18. https://doi.org/10.1016/j.cell.2020.08.002. [CrossRef]
- Schulte-Schrepping J, Reusch N, Paclik D, et al. Severe COVID-19 Is Marked by a Dysregulated Myeloid Cell Compartment. Cell. 2020;182(6):1419-1440.e23. https://doi.org/10.1016/j.cell.2020.08.001. [CrossRef]
- Schaefer IM, Padera RF, Solomon IH, et al. In situ detection of SARS-CoV-2 in lungs and airways of patients with COVID-19. Mod Pathol. 2020;33(11):2104-2114. https://doi.org/10.1038/s41379-020-0595-z. [CrossRef]
- Grant RA, Morales-Nebreda L, Markov NS, et al. Circuits between infected macrophages and T cells in SARS-CoV-2 pneumonia. Nature. 2021;590(7847):635-641. https://doi.org/10.1038/s41586-020-03148-w. [CrossRef]
- Karmakar S. SENDING THE WRONG MESSAGE. The Daily Guardian. 2022.
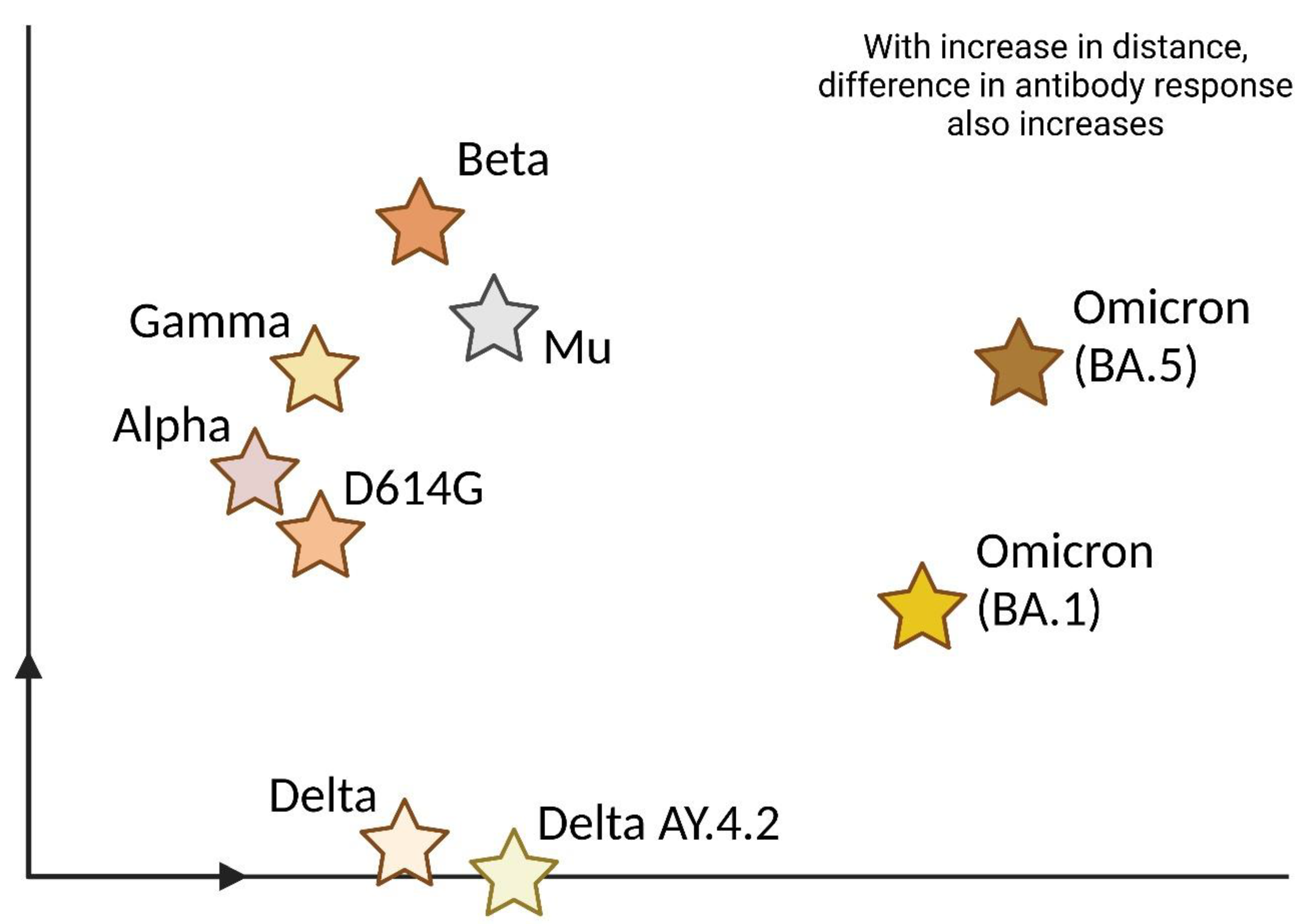
- Li Q, Nie J, Wu J, et al. SARS-CoV-2 501Y.V2 variants lack higher infectivity but do have immune escape. Cell. 2021;184(9):2362-2371.e9. https://doi.org/10.1016/j.cell.2021.02.042. [CrossRef]
- Garcia-Beltran WF, Lam EC, St. Denis K, et al. Erratum: Multiple SARS-CoV-2 variants escape neutralization by vaccine-induced humoral immunity (Cell (2021) 184(9) (2372–2383.e9), (S0092867421002981), (10.1016/j.cell.2021.03.013)). Cell. 2021;184(9):2523. https://doi.org/10.1016/j.cell.2021.04.006. [CrossRef]
- Zhang L, Li Q, Liang Z, et al. The significant immune escape of pseudotyped SARS-CoV-2 variant Omicron. Emerg Microbes Infect. 2022;11(1):1-5. https://doi.org/10.1080/22221751.2021.2017757. [CrossRef]
- Ingraham NE, Ingbar DH. The omicron variant of SARS-CoV-2: Understanding the known and living with unknowns. Clin Transl Med. 2021;11(12):1-6. https://doi.org/10.1002/ctm2.685. [CrossRef]
- Dejnirattisai W, Huo J, Zhou D, Schreiber G, Stuart DI, Screaton GR. SARS-CoV-2 Omicron-B.1.1.529 leads to widespread escape from neutralizing antibody responses. Cell. 2022;185:1-18. https://doi.org/10.1016/j.cell.2021.12.046. [CrossRef]
- Sharma V, Rai H, Gautam DNS, Prajapati PK, Sharma R. Emerging evidence on Omicron (B.1.1.529) SARS-CoV-2 variant. J Med Virol. 2022;(January). https://doi.org/10.1002/jmv.27626. [CrossRef]
- Arora S, Grover V, Saluja P, et al. Literature Review of Omicron: A Grim Reality Amidst COVID-19. Microorganisms. 2022;10(2):1-7. https://doi.org/10.3390/microorganisms10020451. [CrossRef]
- Mohandas S, Yadav PD, Sapkal G, et al. Pathogenicity of SARS-CoV-2 Omicron in Syrian hamsters and its neutralization with different Variants of Concern. bioRxiv. Published online 2022:2022.01.19.477013. http://biorxiv.org/content/early/2022/01/20/2022.01.19.477013.abstract.
- Keeton R, Tincho MB, Ngomti A, et al. T cell responses to SARS-CoV-2 spike cross-recognize Omicron. Nature. Published online 2022:1-5. https://doi.org/10.1038/s41586-022-04460-3. [CrossRef]
- GeurtsvanKessel CH, Geers D, Schmitz KS, et al. Divergent SARS CoV-2 Omicron-specific T- and B-cell responses in COVID-19 vaccine recipients. Sci Immunol. Published online 2022:2021.12.27.21268416. https://doi.org/10.1126/sciimmunol.abo2202. [CrossRef]
- Jergovic M, Coplen CP, Uhrlaub JL, et al. Resilient T cell responses to B.1.1.529 (Omicron) SARS-CoV-2 variant. medRxiv. 2022;529:2022.01.16.22269361. https://www.medrxiv.org/content/10.1101/2022.01.16.22269361v1%0Ahttps://www.medrxiv.org/content/10.1101/2022.01.16.22269361v1.abstract.
- Singhal T. The Emergence of Omicron: Challenging Times Are Here Again! Indian J Pediatr. 2022;(0123456789). https://doi.org/10.1007/s12098-022-04077-4. [CrossRef]
- Lewnard J, Hong V, Patel M, Kahn R, Lipsitch M, Tartof SY. Clinical outcomes among patients infected with Omicron (B.1.1.529) SARS-CoV-2 variant in southern California. medRxiv. Published online 2022. https://doi.org/10.1101/2022.01.11.22269045. [CrossRef]
- Fonager J, Bennedbak M, Bager P, et al. Molecular epidemiology of the SARS-CoV-2 variant Omicron BA.2 sub-lineage in Denmark, 29 November 2021 to 2 January 2022. Eurosurveillance. 2022;27(10):1-7. https://doi.org/10.2807/1560-7917.ES.2022.27.10.2200181. [CrossRef]
- Huang J, Zeng G. Letter to the editor : Epidemiology of the SARS-CoV-2 variant Omicron BA . 2 – vigilance needed. Eurosurveillance. 2022;27(13):22-00254. https://doi.org/10.2807/1560-7917.ES.2022.27.13.2200254. [CrossRef]
- Fan Y, Li X, Zhang L, Wan S, Zhang L, Zhou F. SARS-CoV-2 Omicron variant: recent progress and future perspectives. Signal Transduct Target Ther. 2022;7(1):141. https://doi.org/10.1038/s41392-022-00997-x. [CrossRef]
- Shrestha LB, Foster C, Rawlinson W, Bull RA. Evolution of the SARS-CoV-2 omicron variants BA.1 to BA.5: Implications for immune escape and transmission. Rev Med Virol. 2022;e2381. https://doi.org/10.1002/rmv.2381. [CrossRef]
- Tuekprakhon A, Huo J, Nutalai R, et al. Antibody escape of SARS-CoV-2 Omicron BA.4 and BA.5 from vaccine and BA.1 serum. Cell. Published online 2022:2422-2433. https://doi.org/10.1016/j.cell.2022.06.005. [CrossRef]
- Hachmann NP, Miller J, Collier AY, et al. Neutralization Escape by SARS-CoV-2 Omicron Subvariants BA.2.12.1, BA.4, and BA.5. N Engl J Med. 2022;387:86-88. https://doi.org/10.1056/nejmc2206576. [CrossRef]
- Xia S, Wang L, Zhu Y, Lu L. Origin , virological features , immune evasion and intervention of SARS-CoV-2 Omicron sublineages. Signal Transduct Target Ther. 2022;7:241. https://doi.org/10.1038/s41392-022-01105-9. [CrossRef]
- Houhamdi L, Gautret P, Hoang VT, Fournier PE, Colson P, Raoult D. Characteristics of the first 1119 SARS-CoV-2 Omicron variant cases, in Marseille, France, November−December 2021. J Med Virol. 2022;94(5):2290-2295. https://doi.org/10.1002/jmv.27613. [CrossRef]
- Ulloa AC, Buchan SA, Daneman N, Brown KA. Estimates of SARS-CoV-2 Omicron Variant Severity in Ontario, Canada. JAMA - J Am Med Assoc. 2022;327(13):1286-1288. https://doi.org/10.1001/jama.2022.2274. [CrossRef]
- Wolter N, Jassat W, Walaza S, et al. Early assessment of the clinical severity of the SARS-CoV-2 omicron variant in South Africa: a data linkage study. Lancet. 2022;399(10323):437-446. https://doi.org/10.1016/S0140-6736(22)00017-4. [CrossRef]
- Rajah MM, Hubert M, Bishop E, et al. SARS-CoV-2 Alpha, Beta, and Delta variants display enhanced Spike-mediated syncytia formation. EMBO J. 2021;40(24):1-17. https://doi.org/10.15252/embj.2021108944. [CrossRef]
- Suzuki R, Yamasoba D, Kimura I, et al. Attenuated fusogenicity and pathogenicity of SARS-CoV-2 Omicron variant. Nature. 2022;603(March). https://doi.org/10.1038/s41586-022-04462-1. [CrossRef]
- Meng B, Abdullahi A, Ferreira IATM, et al. Altered TMPRSS2 usage by SARS-CoV-2 Omicron impacts infectivity and fusogenicity. Nature. 2022;603(7902):706-714. https://doi.org/10.1038/s41586-022-04474-x. [CrossRef]
- Bojkova D, Widera M, Ciesek S, Wass MN, Michaelis M, Cinatl J. Reduced interferon antagonism but similar drug sensitivity in Omicron variant compared to Delta variant of SARS-CoV-2 isolates. Cell Res. 2022;32(3):319-321. https://doi.org/10.1038/s41422-022-00619-9. [CrossRef]
- Du X, Tang H, Gao L, et al. Omicron adopts a different strategy from Delta and other variants to adapt to host. Signal Transduct Target Ther. 2022;7(1):5-7. https://doi.org/10.1038/s41392-022-00903-5. [CrossRef]
- Shuai H, Chan JFW, Hu B, et al. Attenuated replication and pathogenicity of SARS-CoV-2 B.1.1.529 Omicron. Nature. 2022;603(7902):693-699. https://doi.org/10.1038/s41586-022-04442-5. [CrossRef]
- Weekly epidemiological update on COVID-19 - 21 December 2022. Published 2022. Accessed December 21, 2022. https://www.who.int/publications/m/item/covid-19-weekly-epidemiological-update---21-december-2022.
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




