1. Introduction
Cannabis is the most commonly used illicit drug worldwide [
1]. An increase in the prevalence of cannabis use could be explained by its legalization in several countries and a reduced societal perception of the associated risks [1-3].
Yet, cannabis use was found to be associated with cognitive deficits, psychiatric diseases (i.e., psychosis), and reduced functioning [4, 5]. In people with psychotic disorders, CUD is about 5 times more prevalent compared to the general population, resulting in a prevalence of up to 25% [6, 7]
. This may exacerbate symptoms, leading to more hospital readmissions and lower adherence to treatment [8-14]. The societal costs of cannabis use exceed a billion dollars annually [15, 16].
No pharmacological treatment has yet been approved to treat CUD [17, 18], and the first line of treatment remains psychotherapy. Current behavioral therapies (relapse prevention, CBT, contingency management [CM], motivational enhancement therapy [MET], and their combination) were shown to have a moderate effect on the general population. However, the impact on individuals with a dual diagnosis of psychosis and CUD showed that both cognitive behavioral therapy (CBT) and CBT plus motivational interviewing (MI) have been found to be ineffective [19-21]. Mixed results were reported for MI alone [22, 23]. Indeed, this complex population might be more challenging to treat [24-26], possibly because of their strong tendency to seek short-term rewards or to self-medicate using this drug [2, 27]. Therefore, effective treatments for CUD in individuals with a concomitant psychotic disorder are critically needed.
Virtual reality (VR) has recently been effectively integrated into treating multiple mental health disorders. With the immersive nature of VR allowing the recreation of a multitude of day-to-day situations, VR-based interventions stand out as an effective therapeutic modality for several psychiatric diagnoses, including anxiety disorders, a psychotic disorder with auditory hallucinations, or even paranoid ideation [28-30]. Notably, VR can be used in cue-exposed therapy (VET) in substance use disorders. This exposition-based intervention aims at decreasing cravings through extinction by the principle of Pavlovian conditioning [
31]. Adding VR may produce a more complex and ecologically valid cue and environment compared to presenting photographs/videos. Moreover, virtual environments are more controlled, safer, and more feasible than real-life recreation of craving-inducing situations [32, 33]. VET was shown to reduce cravings for alcohol and nicotine addiction, but it has not yet been investigated for cannabis [33-35], and whether VET resulted in a decrease in consumption was generally not reported. For nicotine use disorder, a therapy combining CBT elements with VET showed significant reductions in the number of cigarettes used and a higher abstinence rate; however, exposure alone was ineffective [32, 36-38].
These results show that individuals may need to practice their skills while being in a state of craving, which is achievable using VR [
39].
As it was already shown to be beneficial in many other psychiatric disorders, VR could also increase the efficacy of CUD treatments. Therefore, our team created a new intervention: Avatar intervention for cannabis use disorder. This intervention, which is the first integrating VR to treat CUD, includes an important relational component and allows personalization of the immersive experience for each patient. First, patients are invited to create an avatar representing a person intrinsically linked to their cannabis consumption. During immersive sessions, this avatar is then animated by the therapist, allowing the patient to learn and practice coping strategies in situations as close as possible to their reality. By inducing cravings and other strong emotions associated with substance use and by learning to regulate them in a safe and supervised environment, the goal is to reduce cannabis use.
In the present paper, we report the case of the very first patient to undergo Avatar intervention and complete a 12-month follow-up evaluation, which is part of a pre-post pilot study that has been previously published [
40]. Firstly, this paper will provide an overview of the intervention’s course and the participant’s progress. Secondly, it will provide feedback from the participant as well as from his family and treating psychiatrist.
2. Case description
2.1. History of the Patient
At the time of the present study, Mr. C was a college student in his mid-twenties living with his parents. At the age of 15, he began to use cannabis for the first time. The use of cannabis, which was initially occasional and mostly on weekends, gradually increased to daily and even several times a day. His most severe period of polysubstance use occurred when he was 18-19 years old, during which he consumed 3 grams of cannabis, up to 29 standard drinks of alcohol, and 1 gram of cocaine per day. At that time, he had multiple legal concerns (driver’s license loss and fine) due to regularly driving under the influence of substances.
At 20 years of age, he decided to quit all consumption (tobacco, alcohol, drugs) for financial reasons. This period was marked by new objectives, such as keeping the household impeccably clean, changing his diet drastically, getting healthier, and not spending as much money. Later, it was identified that this period coincided with the onset of an obsessive-compulsive disorder (OCD). Moreover, it was at this moment that he started experiencing his first psychotic symptoms. The ideas of grandiosity, telepathy, and mandatory auditory hallucinations progressed to invade him 24 hours a day. He became uninhibited and disorganized, eventually leading to a police intervention and a forced hospitalization in a psychiatric ward. At this time, he received a diagnosis of unspecified psychosis. From then, he was followed by a team for his first psychotic episodes. The diagnosis was then specified as being a schizoaffective disorder, in addition to many comorbidities, including OCD, pathological gambling, and substance use disorder.
After 2 years of cessation, a friend made him smoke cannabis without his knowledge, using a homemade cigarette, which he enjoyed. From then, he again resumed his consumption of alcohol, cannabis, and cocaine. The medical team observed an exacerbation of his psychotic and manic symptoms. His injectable antipsychotic medication (paliperidone) was increased and given within a shorter interval. Closer monitoring was installed, and the possibility of a new hospitalization was considered. In addition, the medical team and his mother observed that his personal hygiene was neglected, and he showed signs of deficits in making visual and verbal contact with others. He had a hostile attitude (i.e., irritable, offensive, threatening), causing his relationships with others to become conflictual, leading to his dismissal from work. His motivation for his ongoing projects dropped drastically (e.g., school, work in his field of study), and he failed all his classes as he was unable to concentrate. Furthermore, a weakness in his personal esteem, in the long run, was also reported in the medical file. According to his treating team, the main problem that impacted the different spheres of his life (i.e., symptomatology, interpersonal relationship, studies) was his excessive cannabis consumption, for which they tried different approaches (motivational interviewing, harm reduction). As reported by his psychiatrist, interactions with his friends were central to his use, which made her believe that the Avatar intervention model (i.e., a relational-based intervention) would benefit him. After several refusals to enter an addiction rehabilitation center, Mr. C finally agreed to participate in this project to receive Avatar intervention in January 2020 since the aspect of VR aroused his interest.
2.2. The course of the Intervention
The intervention sessions were provided by a psychiatrist (AD) once a week for 10 weeks, from February to April 2020. It should be noted that this period corresponded to the occurrence of the COVID-19 pandemic and that half of the intervention sessions took place during this period. Avatar intervention includes techniques already used by other interventions (i.e., refusal skills, motivation to change, alternative activities to consumption, and emotion regulation). Still, the addition of an avatar also allows for the integration of a relational component. The emotions and cravings induced in the VR environment aim to be similar to those that would arise in real life, and the patient is invited to learn how to manage them in real time under the supervision of an experienced therapist.
Sessions 1-3
During the first session, the therapist drew up a general portrait of the patient, including his consumption history, motivations, objectives, and expectations. In this case, Mr. C’s main goal was to stop consuming alcohol and drugs. The second and third sessions focused on psychoeducation concerning the effects of cannabis and allowed for the creation of avatars, which represented significant people having a key role in his consumption (e.g., the consumer friend who encouraged him to consume and a family member).
Sessions 4-10
During immersion sessions using VR, the patient was able to meet the avatars (animated by the therapist) in environments conducive to consumption: a park, an apartment with a joint of cannabis in an ashtray on the table (
Figure 1), and a pub. During each session, Mr. C chose the avatar with whom he wanted to practice a situation from his daily life. With the therapist, they discussed the scenario as well as the roles assigned to each.
1st Immersion (Session 4)
During this session, the patient discussed with an avatar who strongly encouraged him to smoke cannabis. Mr. C was assertive in his choice not to use, practiced saying no, and listed the reasons why this was the right decision (i.e., succeeding in school, stabilizing his mental health).
2nd Immersion (Session 5)
This session consisted of a scenario aiming to provoke craving by having the patient insist and trying to convince an avatar to make him consume, as it sometimes happened in real life. However, the avatar always refused. To learn how to manage his cravings, in the middle of the immersion, the psychiatrist proposed switching roles, and Mr. C had to go back on his choice not to consume. This exercise allowed the patient to practice managing his ambivalence and reconsider his decision (flexibility of thought) in periods of craving when he ends up deciding to consume.
3rd Immersion (Session 6)
This session had the highest emotional charge (anxiety, anger, fear) and induced a strong feeling of craving (9 out of 10). Mr. C was determined to take part in a weekend trip with his friends between sessions 6 and 7. However, using drugs was part of their plans. During this immersion, the avatar encouraged him to maintain his abstinence. The main goal was to raise the patient’s awareness that using on even one occasion can lead to relapse, increase mental flexibility, and control cravings. By negotiating with an avatar, he was able to find alternatives to substance use and think about new activities that could also provide pleasure. He resisted his urge and chose not to go to the weekend he had planned with his friends. He reported that he had the most challenging time saying “no”.
4th Immersion (Session 7)
The session’s goal was to strengthen his assertiveness. For example, Mr. C had difficulty asserting himself regarding things that could help his recovery (e.g., asking his friend not to consume in his car or do other activities). Therefore, he practiced his assertion with his avatar. The feeling of control was the predominant emotion during this session.
Afterward, there was an interruption of 3 weeks between sessions 7 and 8 due to the beginning of the COVID-19 pandemic in March 2020. However, since the intervention was beneficial to him, the research center granted a special authorization to continue the sessions during the pandemic following the request of Mr. C’s treating psychiatrist. During that delay, Mr. C was able to manage his cravings, increase his assertiveness, and transpose his learning into the situations of his daily life.
5th Immersion (Session 8)
This session aimed at dealing with negative emotions that led Mr. C to consume. Specifically, the patient had a very negative view of himself and, when his negative thoughts became too predominant, the urge to consume became stronger. Self-esteem was therefore worked on through his discussion with an avatar whose speech reproduces the negative self-talk that Mr. C had about himself. (i.e., feeling worthless). The patient defended himself by stating his qualities and achievements, as well as by enumerating the efforts he was making (i.e., stopping consuming, going to the gym, better attendance to his appointments, and looking for a student job).
6th Immersion (Session 9)
During this session, Mr. C wanted to practice asking people around him not to encourage him to consume since that was bothering him (i.e., stop buying him cannabis, offering him glasses of wine). During this session, he told the avatar that it pained him instead of pleasing him. On several occasions, Mr. C raised a duality between acting like a teenager (with no responsibility, who liked to consume with his friends, was not autonomous, and did nothing all day), and becoming an adult who desired to succeed in his studies as well as undertaking future projects without consumption.
7th Immersion (Session 10)
The scenario of the last session put forward the consolidation of his objectives without consumption (finish school, work in his field of study. Also, the discussion revolved around compromises to find a balance between having fun and doing things he likes without consuming or being excessive.
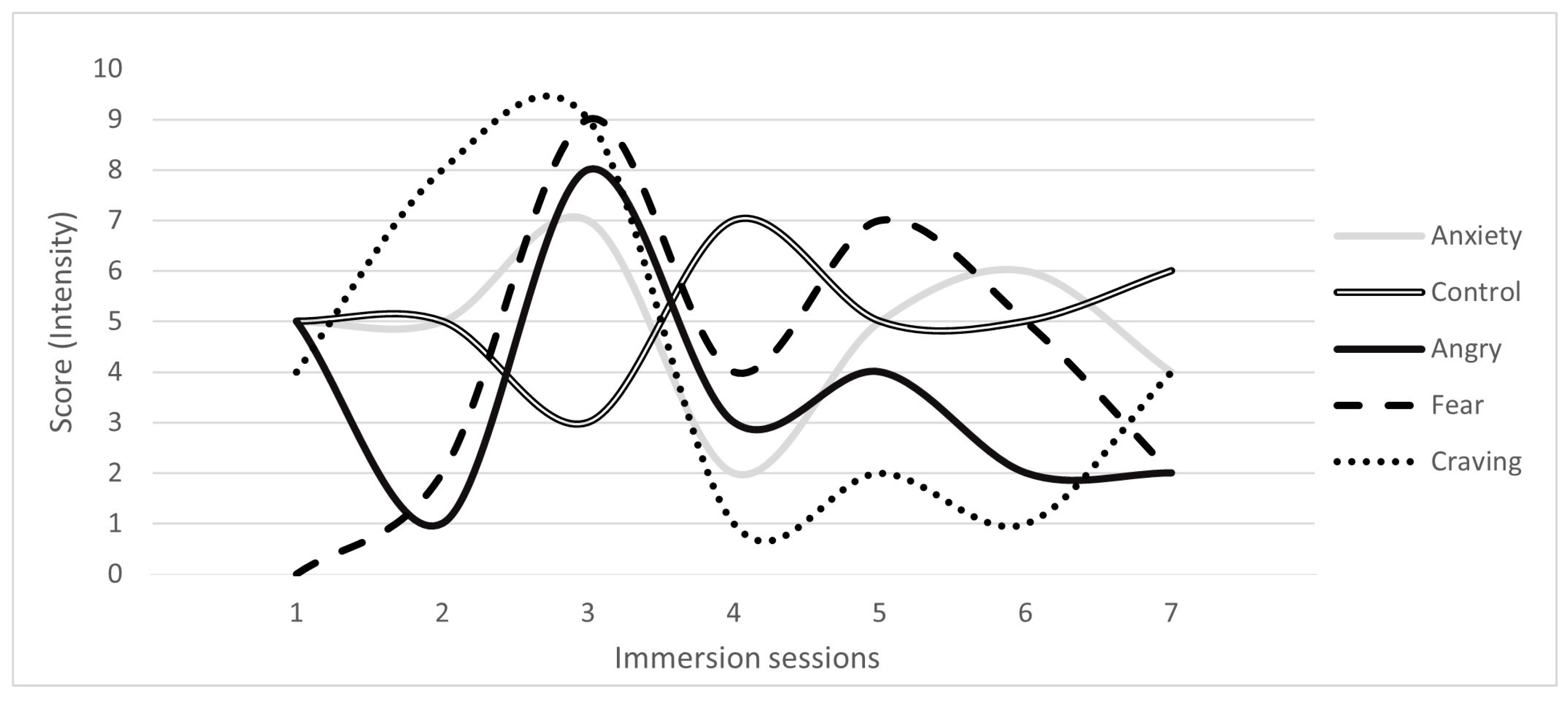
After each immersion, the therapist and the patient discussed the content of the immersion and the emotions that arose. On a scale of 0 (not at all) to 10 (very strongly), Mr. C was asked about the intensity of several emotions (e.g., sense of control, anger) as well as the cravings that arose during the VR immersion (
Figure 2). From the evaluation, it was possible to observe that the sessions during which negative emotions were stronger were also sessions after which he reported a stronger intensity of craving (i.e., session 2). Conversely, in the sessions when the feeling of control was more predominant, the level of craving was lower (e.g., session 4). Finally, the craving seemed to decrease as the intervention progressed.
3. Results
Periodical evaluations have been conducted by a research nurse pre- and post-intervention, and at the 3-, 6- and 12-month follow-up visits (See
Table S1 for a detailed list of questionnaires and their psychometric properties). Moreover, a semi-guided interview with Mr. C. was done pre- and post-intervention, as well as 16 months after Avatar intervention, to inquire about additional information for the present case report. During these evaluations, the interview guide ensured that the following topics were discussed: consumption, consequences/effects associated with consumption, quality of life, psychotic and manic symptoms, and interpersonal relationships.
3.1. Consumption and Addiction
At baseline, Mr. C had a severe CUD, a severe alcohol use disorder, and a light cocaine use disorder, all assessed using the
Structured clinical interview for DSM-5 [41, 42]. During the week preceding the pre-intervention evaluation, Mr. C consumed 23 grams of cannabis, 94 standard alcoholic drinks (i.e., beer: 5%=341mL, wine: 12%=142mL; [
43]), 2 pills of amphetamine and 1 gram of cocaine. However, between the pre-intervention evaluation and the first intervention session, Mr. C quit using alcohol and drugs to be more productive and better performance in his studies. Subsequently, he was able to maintain total abstinence throughout the course of the intervention, all the way until the post-intervention evaluation. However, he later experienced a relapse for cannabis that was detected at the 3- and 6-month post-intervention follow-up visits. Nevertheless, a return to abstinence was observed at the one-year follow-up visit and was maintained until the additional semi-guided interview which occurred 16 months post-intervention, although he mentioned having used cocaine during this period. Nevertheless, he still had not consumed any alcohol since the beginning of the intervention. The
cannabis use problematic identification test (CUPIT),
used for the detection of current and potentially problematic cannabis use [
44]
, showed a decrease of almost half (41%) of the total score between baseline and the end of intervention. Because of his relapse, the follow-up evaluations did not show the maintenance of this result. Nevertheless, interviews with Mr. C showed a decrease in problematic cannabis use. For example, he showed a clear improvement in his academic performance (i.e., passing all his courses) and mentioned having a better focus. Also, Mr. C was no longer driving while intoxicated and frequently acted as the designated driver.
The motivation to change cannabis use was assessed using
Marijuana Ladder, which showed that Mr. C went from preparation (almost ready to make plans for a change) to maintenance (the change was made and never went back to the consumption it was before) between pre- and post-intervention [
45]. Mr. C reported that he particularly appreciated the suggestion to engage in new activities that do not involve substance consumption. He implemented this strategy and could now do activities he liked without a consumption component (i.e., attending hockey and soccer games, and going to outdoor shows). In addition, Mr. C reported that the strategies learned during the immersion sessions had increased his self-confidence, notably in his ability to stay abstinent by having better control. Indeed, he was now able to refuse when offered to consume and became assertive and confident in his choices. His insight also improved as he recognized that cannabis was deteriorating his mental health.
3.2. Affective and Psychotic Symptoms
The patient’s anxiety (Scale of anxiety evaluation in schizophrenia: SAES) decreased by 36% by the end of the intervention and by 71% by the 3-month follow-up, which was maintained until the 12-year follow-up (71%). Depressive symptoms (Calgary depression scale of schizophrenia: CDSS) were reduced by 75% after intervention, and these improvements were maintained during the whole follow-up period (3-months: 100%, 6-and 12-months: 75%)
Qualitative assessments conducted with the patient, his psychiatrist, and his mother revealed improvements in manic and psychotic symptoms. Mr. C mentioned no longer having telepathy or grandiosity delusions, feeling freer in his thoughts, and no longer hearing voices. In addition, hospitalization is no longer considered by his treatment team, and, to date, he has not been re-hospitalized.
3.3. Quality of Life
Quality of life assessments with the Quality of life enjoyment and satisfaction questionnaire short form (QLES-Q-SF) showed a slight improvement (9%) at the end of the intervention and a greater increase (13%) at the 3-month follow-up, and then a decrease at the 6- and 12-months follow-ups (6% and 7%, respectively), which remained above the baseline score. Nevertheless, the final 16-month interview with Mr. C allowed us to observe a qualitative improvement in the relationship quality with his mother (i.e., increased trust, better communication, telling her ‘’I love you’’ more often). He also started to make plans for his future, gained confidence, and became more autonomous (e.g., taking medication alone, planning on moving into an apartment in a few months). At the end of the Avatar intervention, Mr. C applied for an internship and started working in his field while continuing his studies. Since then, he has been promoted with more responsibilities at work.
3.4. Feasibility and Acceptability
The patient reported no adverse effects, which was also the case in a similar population with psychotic disorders having followed a VR therapy for auditory hallucinations [
46].
3.5. Impressions of the Patient, His Mother, and His Psychiatrist
During the post-intervention assessment, Mr. C told us about the benefits that Avatar intervention had given him.
“It was very revealing. These were good discussions, I started to ask myself questions and to doubt my choices and my desires. I doubted these were the right choices I was making, and that created ways for me to avoid relapses. It changed me a lot. Before my appointments, I was excited and looking forward to them”. – Mr. C
More than 16 months after Avatar intervention, Mr. C, his mother, and his psychiatrist were still observing its benefits.
“It allowed me to question myself, reduce temptations and confront people. It’s a bit related to the confidence I had, I could say no, and I could say why I didn’t like it. Today I see good things, other than those related to cannabis. I’m more confident in myself; I’m less afraid of confronting my friends. I tell them what I think that I like or dislike”. – Mr. C
His psychiatrist explained that the relapse observed at the 3- and 6-month follow-ups was shorter, and Mr. C did not lose control over his consumption as he had in the past. She hypothesized that her patient achieved more results with Avatar intervention since it increased his self-confidence and allowed him to gain control, notably by being more invested in the intervention. In particular, the psychiatrist associated the in vivo aspect of VR with the success of the intervention.
“I think it’s testing strategies in vivo with VR that has helped him the most to put himself in contexts and to develop tools from there”. – Mr. C’s psychiatrist’
Mr. C’s mother had also noticed significant changes in her relationship with her son and reported that she was able to bond with him again after he stopped using cannabis. According to her, Avatar intervention allowed her son to be more open to discussion and to express himself to her. She mentioned that her son had started planning for his future (i.e., having his apartment, and getting a girlfriend).
“He has also said it many times that if he had not been there [Avatar intervention], he wonders where he would be today”. – Mr. C’s mother’
4. Discussion
This case study illustrates the application of Avatar intervention for CUD in a person with a psychotic disorder and its potential short- and long-term benefits. Before the intervention, the patient’s consumption was an important factor affecting an extensive range of his life (i.e., manic and psychotic symptoms, concentration and motivation at school, withdrawal of driver’s license, interpersonal conflicts). His psychiatrist referred this patient to receive Avatar intervention as she saw it as a way to elicit Mr. C’s interest in a substance use intervention with its relational and immersive approach. Indeed, for the first time since he was followed in psychiatry, he developed an interest in undergoing intervention to address his substance use and decided to undergo an intervention. Once started, he was assiduous, involved, and enthusiastic at each session. When several services were stopped due to COVID-19, her psychiatrist requested a waiver to continue the intervention since she observed significant benefits, in addition to Mr. C’s desire to continue the intervention. Indeed, the benefits surpassed that of abstinence from cannabis use and a diminution of the severity of CUD, as the intervention also had an impact on his affective symptomatology (anxiety and depression). The qualitative analyses allowed the observation of the various benefits, notably on his quality of life (i.e., interpersonal relationships, self-esteem, motivation) and his psychotic symptoms. The patient reported these changes but also observed by his mother and his psychiatrist.
The specificity of this intervention, in addition to using VR, is the relational aspect (discussion with an avatar representing a significant person in the patient’s consumption). The relational component could allow the patient to modify his relationship with others and with himself, all of which used to lead to substance use. This principle is similar to that of VR therapies for auditory hallucinations, in which there is a modification in the relationship between the voice hearer and their persecuting voice [46, 47]. Also, the relational and immersive component of Avatar intervention can generate craving and strong (but tolerable) emotions at an intensity similar to that of real life [31, 48]. By integrating the combination of several interventional methods, learning how to manage cravings, and stress, and regulate emotions as they occur could be transposed to real life [
48]
.
Although Avatar intervention seems to have resulted in substantial gains for Mr. C, some limitations must be acknowledged. The pandemic had a significant impact on the consumption of several individuals, and therefore it could also have affected Mr. C. On the one hand, the results could be overestimated since the number of opportunities to consume with friends was reduced. On the other hand, a recent systematic review has shown increased cannabis use among users during the pandemic [
49]. For Mr. C., who completely stopped consuming at the start of the intervention, it is difficult to assess whether the pandemic, which was declared in the middle of the intervention, has significantly impacted his consumption. This case report is a first step towards gaining a more detailed insight into the intervention process and the evolution of a participant over the course of the therapeutic sessions. However, a future qualitative study on the therapeutic processes of the therapy will be necessary to understand each component of the intervention better. In addition, the open interview with a family member, the participant’s psychiatrist, and the participant himself revealed benefits that quantitative questionnaires would not have detected [50, 51]. However, generalizing these results is not currently possible, and an analysis of a larger sample is required. The recently published pilot trial evaluated the efficacy, acceptability, and feasibility of the Avatar intervention, which will be replicated in a single-blind control trial, comparing the intervention with a conventional substance abuse intervention in a large sample.
5. Conclusions
In conclusion, this case suggests that Avatar intervention may be helpful for CUD in patients with a psychotic disorder. This patient successfully maintained abstinence from alcohol as well as from cannabis, with only one short relapse over a 16-month period after intervention. Avatar intervention seems very promising for the moment. Results are being replicated in a single-blind randomized controlled trial comparing the intervention to a classical therapy in a larger sample.
Supplementary Materials
The following supporting information can be downloaded at:
www.mdpi.com/xxx/s1, Table S1: characteristics of the questionnaires.
Author Contributions
SG and MAL collected data on the patient. SG, LD, MB, and AD wrote the paper. All authors provided critical comments. All authors approved the final version of the manuscript.
Funding
This research was funded by by the Services et recherches psychiatriques AD, Fondation Lévesque and IRSC Catalyseur.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Ethics Committee of Research center of the University Institute in Mental Health of Montreal (MP-12-2019-1564; 2018-10-09).
Informed Consent Statement
Written informed consent has been obtained from the patient to publish this paper.
Data Availability Statement
The data presented in this study are available upon reasonable request to the corresponding author.
Acknowledgments
AD is holder of a Junior 2 salary award from the FRQS. LD and MB’s doctoral studies are funded by the FRQS as well, and MB is also funded by the Canadian Institutes of Health Research (CIHR). SP is the holder of the Eli Lilly Chair on schizophrenia research.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Hall, W., et al., Public health implications of legalising the production and sale of cannabis for medicinal and recreational use. Lancet, 2019. 394(10208): p. 1580-1590. [CrossRef]
- Lowe, D.J.E., et al., Cannabis and mental illness: a review. Eur Arch Psychiatry Clin Neurosci, 2019. 269(1): p. 107-120. [CrossRef]
- Smart, R. and R.L. Pacula, Early evidence of the impact of cannabis legalization on cannabis use, cannabis use disorder, and the use of other substances: Findings from state policy evaluations. Am J Drug Alcohol Abuse, 2019. 45(6): p. 644-663.
- Dellazizzo, L., et al., Evidence on the acute and residual neurocognitive effects of cannabis use in adolescents and adults: a systematic meta-review of meta-analyses. Addiction, 2022. 117(7): p. 1857-1870. [CrossRef]
- Sorkhou, M., R.H. Bedder, and T.P. George, The Behavioral Sequelae of Cannabis Use in Healthy People: A Systematic Review. Front Psychiatry, 2021. 12: p. 630247. [CrossRef]
- Hunt, G.E., et al., Prevalence of comorbid substance use in schizophrenia spectrum disorders in community and clinical settings, 1990-2017: Systematic review and meta-analysis. Drug Alcohol Depend, 2018. 191: p. 234-258. [CrossRef]
- Koskinen, J., et al., Rate of cannabis use disorders in clinical samples of patients with schizophrenia: a meta-analysis. Schizophr Bull, 2010. 36(6): p. 1115-30. [CrossRef]
- Athanassiou, M., et al., A systematic review of longitudinal studies investigating the impact of cannabis use in patients with psychotic disorders. Expert Rev Neurother, 2021. 21(7): p. 779-791.
- Clausen, L., et al., Change in cannabis use, clinical symptoms and social functioning among patients with first-episode psychosis: a 5-year follow-up study of patients in the OPUS trial. Psychological Medicine, 2014. 44(1): p. 117-126. [CrossRef]
- Foti, D.J., et al., Cannabis use and the course of schizophrenia: 10-year follow-up after first hospitalization. American Journal of Psychiatry, 2010. 167(8): p. 987-993. [CrossRef]
- Colizzi, M., et al., Longitudinal assessment of the effect of cannabis use on hospital readmission rates in early psychosis: A 6-year follow-up in an inpatient cohort. Psychiatry Research, 2018. 268: p. 381-387. [CrossRef]
- Schoeler, T., et al., Continued versus discontinued cannabis use in patients with psychosis: a systematic review and meta-analysis. Lancet Psychiatry, 2016. 3(3): p. 215-25. [CrossRef]
- Schoeler, T., et al., Poor medication adherence and risk of relapse associated with continued cannabis use in patients with first-episode psychosis: a prospective analysis. Lancet Psychiatry, 2017. 4(8): p. 627-633. [CrossRef]
- Patel, R., et al., Association of cannabis use with hospital admission and antipsychotic treatment failure in first episode psychosis: an observational study. BMJ Open, 2016. 6(3): p. e009888. [CrossRef]
- Canadian Substance Use Costs and Harms Scientific Working Group, Canadian substance use costs and harms 2015–2017. , in Canadian substance use cost and harms. 2020, Canadian Centre on Substance Use and Addiction. : Ottawa, Ontario.
- Gryczynski, J., et al., Understanding Patterns Of High-Cost Health Care Use Across Different Substance User Groups. Health Aff (Millwood), 2016. 35(1): p. 12-9. [CrossRef]
- Marshall, K., et al., Pharmacotherapies for cannabis dependence. Cochrane Database Syst Rev, 2014. 12(12): p. Cd008940. [CrossRef]
- Nielsen, S., et al., Pharmacotherapies for cannabis dependence. Cochrane Database Syst Rev, 2019. 1(1): p. Cd008940.
- Edwards, J., et al., Randomized controlled trial of a cannabis-focused intervention for young people with first-episode psychosis. Acta Psychiatr Scand, 2006. 114(2): p. 109-17. [CrossRef]
- Madigan, K., et al., A multi-center, randomized controlled trial of a group psychological intervention for psychosis with comorbid cannabis dependence over the early course of illness. Schizophr Res, 2013. 143(1): p. 138-42. [CrossRef]
- Baker, A., et al., Cognitive-behavioural therapy for substance use disorders in people with psychotic disorders: Randomised controlled trial. Br J Psychiatry, 2006. 188: p. 439-48.
- Bonsack, C., et al., Motivational intervention to reduce cannabis use in young people with psychosis: a randomized controlled trial. Psychother Psychosom, 2011. 80(5): p. 287-97. [CrossRef]
- Martino, S., et al., A randomized controlled pilot study of motivational interviewing for patients with psychotic and drug use disorders. Addiction, 2006. 101(10): p. 1479-92. [CrossRef]
- Lees, R., et al., Psychosocial and pharmacological treatments for cannabis use disorder and mental health comorbidities: a narrative review. Psychol Med, 2021. 51(3): p. 353-364. [CrossRef]
- Hjorthøj, C., A. Fohlmann, and M. Nordentoft, Treatment of cannabis use disorders in people with schizophrenia spectrum disorders - a systematic review. Addict Behav, 2009. 34(6-7): p. 520-5. [CrossRef]
- Hunt, G.E., et al., Psychosocial interventions for people with both severe mental illness and substance misuse. Cochrane Database Syst Rev, 2019. 12(12): p. Cd001088. [CrossRef]
- Bonn-Miller, M.O., et al., Self-reported cannabis use characteristics, patterns and helpfulness among medical cannabis users. Am J Drug Alcohol Abuse, 2014. 40(1): p. 23-30. [CrossRef]
- Dellazizzo, L., et al., Evidence on Virtual Reality-Based Therapies for Psychiatric Disorders: Meta-Review of Meta-Analyses. J Med Internet Res, 2020. 22(8): p. e20889. [CrossRef]
- Freeman, D., et al., Virtual reality in the assessment, understanding, and treatment of mental health disorders. Psychol Med, 2017. 47(14): p. 2393-2400. [CrossRef]
- Emmelkamp, P.M.G. and K. Meyerbröker, Virtual Reality Therapy in Mental Health. Annu Rev Clin Psychol, 2021. 17: p. 495-519. [CrossRef]
- Hone-Blanchet, A., T. Wensing, and S. Fecteau, The use of virtual reality in craving assessment and cue-exposure therapy in substance use disorders. Front Hum Neurosci, 2014. 8: p. 844. [CrossRef]
- Bordnick, P.S., et al., A Feasibility Study of Virtual Reality-Based Coping Skills Training for Nicotine Dependence. Res Soc Work Pract, 2012. 22(3): p. 293-300. [CrossRef]
- Choi, Y.J., Lee, Jang-Han, The effect of virtual covert sensitization on reducing alcohol craving in heavy social drinkers. Virtual Reality, 2015. 19: p. 111–117. [CrossRef]
- Lee, S.H., et al., Quantitative electroencephalographic (qEEG) correlates of craving during virtual reality therapy in alcohol-dependent patients. Pharmacol Biochem Behav, 2009. 91(3): p. 393-7. [CrossRef]
- Pericot-Valverde, I., et al., Individual variables related to craving reduction in cue exposure treatment. Addict Behav, 2015. 49: p. 59-63. [CrossRef]
- Girard, B., et al., Crushing virtual cigarettes reduces tobacco addiction and treatment discontinuation. Cyberpsychol Behav, 2009. 12(5): p. 477-83.
- Park, C.B., et al., Comparison of the effectiveness of virtual cue exposure therapy and cognitive behavioral therapy for nicotine dependence. Cyberpsychol Behav Soc Netw, 2014. 17(4): p. 262-7. [CrossRef]
- Pericot-Valverde, I., R. Secades-Villa, and J. Gutiérrez-Maldonado, A randomized clinical trial of cue exposure treatment through virtual reality for smoking cessation. J Subst Abuse Treat, 2019. 96: p. 26-32. [CrossRef]
- Conklin, C.A. and S.T. Tiffany, Applying extinction research and theory to cue-exposure addiction treatments. Addiction, 2002. 97(2): p. 155-67. [CrossRef]
- Giguère, S., et al., Avatar Intervention for Cannabis Use Disorder in Individuals with Severe Mental Disorders: A Pilot Study. J Pers Med, 2023. 13(5). [CrossRef]
- American Psychiatric Association, Diagnostic and statistical manual of mental disorders : dsm-5-tr (Fifth edition, text revision). 2022: American Psychiatric Association Publishing.
- First, M.B., et al., User’s guide for the SCID-5-CV Structured Clinical Interview for DSM-5® disorders: Clinical version. User’s guide for the SCID-5-CV Structured Clinical Interview for DSM-5® disorders: Clinical version. 2016, Arlington, VA, US: American Psychiatric Publishing, Inc. xii, 158-xii, 158.
- Éduc Alcool, Alcool et santé, les niveaux de consommation d’alcool à faible risque. 2007.
- Bashford, J., R. Flett, and J. Copeland, The Cannabis Use Problems Identification Test (CUPIT): development, reliability, concurrent and predictive validity among adolescents and adults. Addiction, 2010. 105(4): p. 615-25. [CrossRef]
- Slavet, J.D., et al., The Marijuana Ladder: measuring motivation to change marijuana use in incarcerated adolescents. Drug Alcohol Depend, 2006. 83(1): p. 42-8. [CrossRef]
- Dellazizzo, L., et al., One-year randomized trial comparing virtual reality-assisted therapy to cognitive-behavioral therapy for patients with treatment-resistant schizophrenia. NPJ Schizophr, 2021. 7(1): p. 9. [CrossRef]
- Craig, T.K., et al., AVATAR therapy for auditory verbal hallucinations in people with psychosis: a single-blind, randomised controlled trial. Lancet Psychiatry, 2018. 5(1): p. 31-40. [CrossRef]
- Colombo, D., et al., Virtual reality for the enhancement of emotion regulation. Clin Psychol Psychother, 2021. 28(3): p. 519-537. [CrossRef]
- Roberts, A., et al., Alcohol and other substance use during the COVID-19 pandemic: A systematic review. Drug Alcohol Depend, 2021. 229(Pt A): p. 109150. [CrossRef]
- Beaudoin, M., et al., The therapeutic processes of avatar therapy: A content analysis of the dialogue between treatment-resistant patients with schizophrenia and their avatar. Clin Psychol Psychother, 2021. 28(3): p. 500-518. [CrossRef]
- Dellazizzo, L., et al., Exploration of the dialogue components in Avatar Therapy for schizophrenia patients with refractory auditory hallucinations: A content analysis. Clin Psychol Psychother, 2018. 25(6): p. 878-885.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).