Submitted:
26 June 2023
Posted:
27 June 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
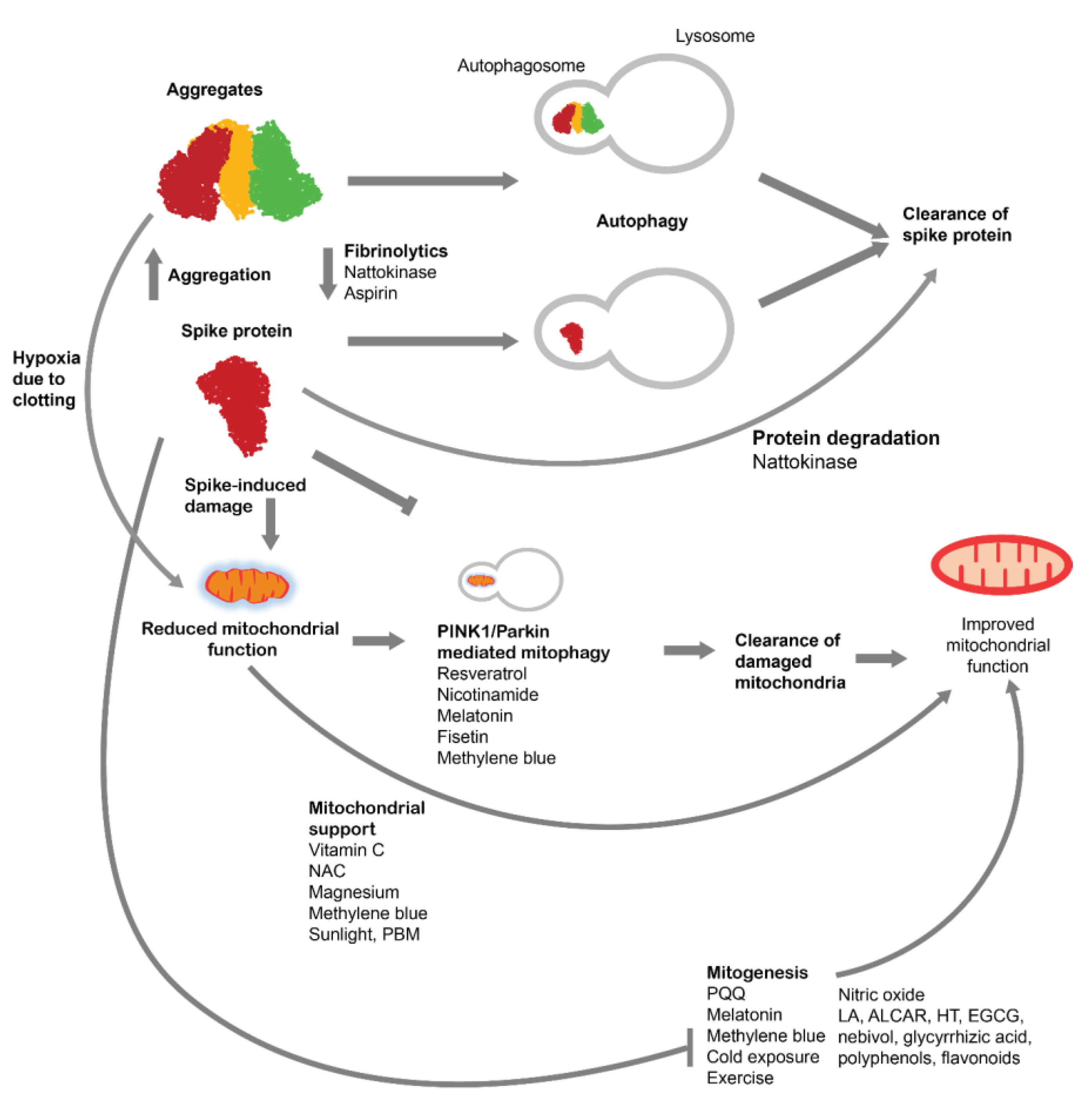
2. Pathophysiology related to spike protein
3. Autophagy mechanism
3.2. Regulation of Autophagy
4. Autophagy of spike protein and aggregates
4. Autophagy for treatment of spike protein-induced pathologies
4.1. Fasting and autophagy
4.2. Compounds for increasing autophagy
4.2.1. Spermidine
4.2.2. Caffeine
4.2.3. Resveratrol
4.2.4. Curcumin
4.2.5. Other compounds
4.2.6. Other non-pharmacological modalities
5. Improving mitochondrial function
5.1. Mitophagy
5.2. Mitochondrial biogenesis
5.2.1. PQQ
5.2.2. Cold exposure
5.2.3. Endurance exercise
5.2.4. Nitric Oxide
5.2.5. Melatonin
5.2.6. Others
5.3. Improving Mitochondrial Function
5.3.1. Vitamin C
5.3.2. N-acetyl cysteine
5.3.3. Magnesium
5.3.4. Methylene Blue
5.3.5. Light therapy
5.3.6. Others
6. Conclusion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Venegas-Borsellino, C.; Sonikpreet; Martindale, R.G. From Religion to Secularism: The Benefits of Fasting. Curr Nutr Rep 2018, 7, 131–138. [CrossRef]
- Fazel, M. Medical Implications of Controlled Fasting. J R Soc Med 1998, 91, 260–263. [Google Scholar] [CrossRef] [PubMed]
- Sanchetee, P.; Sanchetee, P.; Garg, M.K. Effect of Jain Fasting on Anthropometric, Clinical and Biochemical Parameters. Indian J Endocrinol Metab 2020, 24, 187–190. [Google Scholar] [CrossRef] [PubMed]
- Cohen, K. Native American Medicine. Altern Ther Health Med 1998, 4, 45–57. [Google Scholar]
- Sanz-Biset, J.; Cañigueral, S. Plant Use in the Medicinal Practices Known as “Strict Diets” in Chazuta Valley (Peruvian Amazon). Journal of Ethnopharmacology 2011, 137, 271–288. [Google Scholar] [CrossRef]
- Krakoff, L.R. Fasting and Ambulatory Blood Pressure Monitoring. Blood Pressure Monitoring 2017, 22, 258. [Google Scholar] [CrossRef]
- Hoffman, V.J. Eating and Fasting for God in Sufi Tradition. Journal of the American Academy of Religion 1995, 63, 465–484. [Google Scholar] [CrossRef]
- Patterson, R.E.; Laughlin, G.A.; Sears, D.D.; LaCroix, A.Z.; Marinac, C.; Gallo, L.C.; Hartman, S.J.; Natarajan, L.; Senger, C.M.; Martínez, M.E.; et al. INTERMITTENT FASTING AND HUMAN METABOLIC HEALTH. J Acad Nutr Diet 2015, 115, 1203–1212. [Google Scholar] [CrossRef]
- Visioli, F.; Mucignat-Caretta, C.; Anile, F.; Panaite, S.-A. Traditional and Medical Applications of Fasting. Nutrients 2022, 14, 433. [Google Scholar] [CrossRef]
- Gaikwad, S.; Gaikwad, P.; Saxena, V. Principles of Fasting in Ayurveda. International Journal of Science, Environment and Technology 2017, 6, 787–792. [Google Scholar]
- Wang, C.; Ming, L.; Jia, L.; Wang, Q.; Cao, T.; Wang, L.; Zhou, Z.; Tong, D.; Li, W.; Wu, Y.; et al. Long-Term Extreme Fasting Following a Traditional Chinese “Bigu” Regimen: A Preliminary Retrospective and Prospective Cohort Study 2019.
- Ganesh Iyyer, S.; Mooventhan, A.; Nandakumar, B. Effectiveness of Liquid Fasting with Yoga and Naturopathy Treatments in Reducing Metabolic and Cardiovascular Risks in Obesity. Adv Mind Body Med 2021, 35, 24–28. [Google Scholar] [PubMed]
- Chockalingam, A.; Kumar, S.; Ferrer, M.S.; Gajagowni, S.; Isaac, M.; Karuparthi, P.; Aggarwal, K.; Shunmugam, S.; Amuthan, A.; Aggarwal, A.; et al. Siddha Fasting in Obese Acute Decompensated Heart Failure May Improve Hospital Outcomes through Empowerment and Natural Ketosis. EXPLORE 2022, 18, 714–718. [Google Scholar] [CrossRef] [PubMed]
- Ljungqvist, O.; Søreide, E. Preoperative Fasting. British Journal of Surgery 2003, 90, 400–406. [Google Scholar] [CrossRef]
- Temkin, O. The Falling Sickness: A History of Epilepsy from the Greeks to the Beginnings of Modern Neurology; JHU Press: Baltimore, MD, USA, 1994; Volume 4, ISBN ISBN 0-8018-4849-0. [Google Scholar]
- Hubert, V.; Weiss, S.; Rees, A.J.; Kain, R. Modulating Chaperone-Mediated Autophagy and Its Clinical Applications in Cancer. Cells 2022, 11, 2562. [Google Scholar] [CrossRef]
- Galan-Acosta, L.; Xia, H.; Yuan, J.; Vakifahmetoglu-Norberg, H. Activation of Chaperone-Mediated Autophagy as a Potential Anticancer Therapy. Autophagy 2015, 11, 2370–2371. [Google Scholar] [CrossRef]
- Kaushik, S.; Cuervo, A.M. The Coming of Age of Chaperone-Mediated Autophagy. Nat Rev Mol Cell Biol 2018, 19, 365–381. [Google Scholar] [CrossRef]
- Swank, Z.; Senussi, Y.; Manickas-Hill, Z.; Yu, X.G.; Li, J.Z.; Alter, G.; Walt, D.R. Persistent Circulating Severe Acute Respiratory Syndrome Coronavirus 2 Spike Is Associated With Post-Acute Coronavirus Disease 2019 Sequelae. Clinical Infectious Diseases 2023, 76, e487–e490. [Google Scholar] [CrossRef]
- Theoharides, T.C. Could SARS-CoV-2 Spike Protein Be Responsible for Long-COVID Syndrome? Mol Neurobiol 2022, 59, 1850–1861. [Google Scholar] [CrossRef]
- Attinà, A.; Leggeri, C.; Paroni, R.; Pivari, F.; Dei Cas, M.; Mingione, A.; Dri, M.; Marchetti, M.; Di Renzo, L. Fasting: How to Guide. Nutrients 2021, 13, 1570. [Google Scholar] [CrossRef]
- Kepp, O.; Chen, G.; Carmona-Gutierrez, D.; Madeo, F.; Kroemer, G. A Discovery Platform for the Identification of Caloric Restriction Mimetics with Broad Health-Improving Effects. Autophagy 2020, 16, 188–189. [Google Scholar] [CrossRef] [PubMed]
- Patikorn, C.; Roubal, K.; Veettil, S.K.; Chandran, V.; Pham, T.; Lee, Y.Y.; Giovannucci, E.L.; Varady, K.A.; Chaiyakunapruk, N. Intermittent Fasting and Obesity-Related Health Outcomes: An Umbrella Review of Meta-Analyses of Randomized Clinical Trials. JAMA Network Open 2021, 4, e2139558. [Google Scholar] [CrossRef]
- Liang, S.; Bao, C.; Yang, Z.; Liu, S.; Sun, Y.; Cao, W.; Wang, T.; Schwantes-An, T.-H.; Choy, J.S.; Naidu, S.; et al. SARS-CoV-2 Spike Protein Induces IL-18-Mediated Cardiopulmonary Inflammation via Reduced Mitophagy. Sig Transduct Target Ther 2023, 8, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Clough, E.; Inigo, J.; Chandra, D.; Chaves, L.; Reynolds, J.L.; Aalinkeel, R.; Schwartz, S.A.; Khmaladze, A.; Mahajan, S.D. Mitochondrial Dynamics in SARS-COV2 Spike Protein Treated Human Microglia: Implications for Neuro-COVID. J Neuroimmune Pharmacol 2021, 16, 770–784. [Google Scholar] [CrossRef]
- Sun, X.; Yu, J.; Wong, S.H.; Chan, M.T.V.; Zhang, L.; Wu, W.K.K. SARS-CoV-2 Targets the Lysosome to Mediate Airway Inflammatory Cell Death. Autophagy 2022, 18, 2246–2248. [Google Scholar] [CrossRef]
- Nguyen, V.; Zhang, Y.; Gao, C.; Cao, X.; Tian, Y.; Carver, W.; Kiaris, H.; Cui, T.; Tan, W. The Spike Protein of SARS-CoV-2 Impairs Lipid Metabolism and Increases Susceptibility to Lipotoxicity: Implication for a Role of Nrf2. Cells 2022, 11, 1916. [Google Scholar] [CrossRef]
- Li, F.; Li, J.; Wang, P.-H.; Yang, N.; Huang, J.; Ou, J.; Xu, T.; Zhao, X.; Liu, T.; Huang, X.; et al. SARS-CoV-2 Spike Promotes Inflammation and Apoptosis through Autophagy by ROS-Suppressed PI3K/AKT/MTOR Signaling. Biochimica et Biophysica Acta (BBA) - Molecular Basis of Disease 2021, 1867, 166260. [Google Scholar] [CrossRef] [PubMed]
- Davidovich, P.; Kearney, C.J.; Martin, S.J. Inflammatory Outcomes of Apoptosis, Necrosis and Necroptosis. Biol Chem 2014, 395, 1163–1171. [Google Scholar] [CrossRef]
- Kim, E.S.; Jeon, M.-T.; Kim, K.-S.; Lee, S.; Kim, S.; Kim, D.-G. Spike Proteins of SARS-CoV-2 Induce Pathological Changes in Molecular Delivery and Metabolic Function in the Brain Endothelial Cells. Viruses 2021, 13, 2021. [Google Scholar] [CrossRef]
- Huynh, T.V.; Rethi, L.; Lee, T.-W.; Higa, S.; Kao, Y.-H.; Chen, Y.-J. Spike Protein Impairs Mitochondrial Function in Human Cardiomyocytes: Mechanisms Underlying Cardiac Injury in COVID-19. Cells 2023, 12, 877. [Google Scholar] [CrossRef]
- Pickrell, A.M.; Youle, R.J. The Roles of PINK1, Parkin, and Mitochondrial Fidelity in Parkinson’s Disease. Neuron 2015, 85, 257–273. [Google Scholar] [CrossRef]
- Tanaka, K. The PINK1–Parkin Axis: An Overview. Neuroscience Research 2020, 159, 9–15. [Google Scholar] [CrossRef]
- Jin, S.M.; Lazarou, M.; Wang, C.; Kane, L.A.; Narendra, D.P.; Youle, R.J. Mitochondrial Membrane Potential Regulates PINK1 Import and Proteolytic Destabilization by PARL. Journal of Cell Biology 2010, 191, 933–942. [Google Scholar] [CrossRef]
- Li, X.; Hou, P.; Ma, W.; Wang, X.; Wang, H.; Yu, Z.; Chang, H.; Wang, T.; Jin, S.; Wang, X.; et al. SARS-CoV-2 ORF10 Suppresses the Antiviral Innate Immune Response by Degrading MAVS through Mitophagy. Cell Mol Immunol 2022, 19, 67–78. [Google Scholar] [CrossRef]
- Couzin-Frankel, J. The Mystery of the Pandemic’s ‘Happy Hypoxia'. Science 2020, 368, 455–456. [Google Scholar] [CrossRef] [PubMed]
- Pujhari, S.; Paul, S.; Ahluwalia, J.; Rasgon, J.L. Clotting Disorder in Severe Acute Respiratory Syndrome Coronavirus 2. Reviews in Medical Virology 2021, 31, e2177. [Google Scholar] [CrossRef] [PubMed]
- Adzigbli, L.; Sokolov, E.P.; Wimmers, K.; Sokolova, I.M.; Ponsuksili, S. Effects of Hypoxia and Reoxygenation on Mitochondrial Functions and Transcriptional Profiles of Isolated Brain and Muscle Porcine Cells. Sci Rep 2022, 12, 19881. [Google Scholar] [CrossRef] [PubMed]
- Solaini, G.; Baracca, A.; Lenaz, G.; Sgarbi, G. Hypoxia and Mitochondrial Oxidative Metabolism. Biochimica et Biophysica Acta (BBA) - Bioenergetics 2010, 1797, 1171–1177. [Google Scholar] [CrossRef]
- Halma, M.T.J.; Rose, J.; Lawrie, T. The Novelty of MRNA Viral Vaccines and Potential Harms: A Scoping Review. J 2023, 6, 220–235. [Google Scholar] [CrossRef]
- Khan, S.; Shafiei, M.S.; Longoria, C.; Schoggins, J.W.; Savani, R.C.; Zaki, H. SARS-CoV-2 Spike Protein Induces Inflammation via TLR2-Dependent Activation of the NF-ΚB Pathway. Elife 2021, 10, e68563. [Google Scholar] [CrossRef]
- Hsu, A.C.-Y.; Wang, G.; Reid, A.T.; Veerati, P.C.; Pathinayake, P.S.; Daly, K.; Mayall, J.R.; Hansbro, P.M.; Horvat, J.C.; Wang, F.; et al. SARS-CoV-2 Spike Protein Promotes Hyper-Inflammatory Response That Can Be Ameliorated by Spike-Antagonistic Peptide and FDA-Approved ER Stress and MAP Kinase Inhibitors in Vitro 2020, 2020.09.30.317818.
- Forsyth, C.B.; Zhang, L.; Bhushan, A.; Swanson, B.; Zhang, L.; Mamede, J.I.; Voigt, R.M.; Shaikh, M.; Engen, P.A.; Keshavarzian, A. The SARS-CoV-2 S1 Spike Protein Promotes MAPK and NF-KB Activation in Human Lung Cells and Inflammatory Cytokine Production in Human Lung and Intestinal Epithelial Cells. Microorganisms 2022, 10, 1996. [Google Scholar] [CrossRef] [PubMed]
- Lei, Y.; Zhang, J.; Schiavon, C.R.; He, M.; Chen, L.; Shen, H.; Zhang, Y.; Yin, Q.; Cho, Y.; Andrade, L.; et al. SARS-CoV-2 Spike Protein Impairs Endothelial Function via Downregulation of ACE 2. Circulation Research 2021, 128, 1323–1326. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.-Y.; Park, J.H.; Jo, C.; Kim, K.-C.; Koh, Y.H. SARS-CoV-2 Spike S1 Subunit Protein-Mediated Increase of Beta-Secretase 1 (BACE1) Impairs Human Brain Vessel Cells. Biochem Biophys Res Commun 2022, 626, 66–71. [Google Scholar] [CrossRef] [PubMed]
- Bhargavan, B.; Kanmogne, G.D. SARS-CoV-2 Spike Proteins and Cell-Cell Communication Inhibits TFPI and Induces Thrombogenic Factors in Human Lung Microvascular Endothelial Cells and Neutrophils: Implications for COVID-19 Coagulopathy Pathogenesis. Int J Mol Sci 2022, 23, 10436. [Google Scholar] [CrossRef]
- Buzhdygan, T.P.; DeOre, B.J.; Baldwin-Leclair, A.; Bullock, T.A.; McGary, H.M.; Khan, J.A.; Razmpour, R.; Hale, J.F.; Galie, P.A.; Potula, R.; et al. The SARS-CoV-2 Spike Protein Alters Barrier Function in 2D Static and 3D Microfluidic in-Vitro Models of the Human Blood-Brain Barrier. Neurobiol Dis 2020, 146, 105131. [Google Scholar] [CrossRef]
- Nyström, S.; Hammarström, P. Amyloidogenesis of SARS-CoV-2 Spike Protein. J Am Chem Soc 2022, 144, 8945–8950. [Google Scholar] [CrossRef]
- Petrlova, J.; Samsudin, F.; Bond, P.J.; Schmidtchen, A. SARS-CoV-2 Spike Protein Aggregation Is Triggered by Bacterial Lipopolysaccharide. FEBS Letters 2022, 596, 2566–2575. [Google Scholar] [CrossRef]
- Gill, J.R.; Tashjian, R.; Duncanson, E. Autopsy Histopathologic Cardiac Findings in 2 Adolescents Following the Second COVID-19 Vaccine Dose. Archives of Pathology & Laboratory Medicine 2022, 146, 925–929. [Google Scholar] [CrossRef]
- Schwab, C.; Domke, L.M.; Hartmann, L.; Stenzinger, A.; Longerich, T.; Schirmacher, P. Autopsy-Based Histopathological Characterization of Myocarditis after Anti-SARS-CoV-2-Vaccination. Clin Res Cardiol 2023, 112, 431–440. [Google Scholar] [CrossRef]
- Choi, S.; Lee, S.; Seo, J.-W.; Kim, M.-J.; Jeon, Y.H.; Park, J.H.; Lee, J.K.; Yeo, N.S. Myocarditis-Induced Sudden Death after BNT162b2 MRNA COVID-19 Vaccination in Korea: Case Report Focusing on Histopathological Findings. J Korean Med Sci 2021, 36, e286. [Google Scholar] [CrossRef] [PubMed]
- Mörz, M. A Case Report: Multifocal Necrotizing Encephalitis and Myocarditis after BNT162b2 MRNA Vaccination against COVID-19. Vaccines 2022, 10, 1651. [Google Scholar] [CrossRef]
- Tsukada, M.; Ohsumi, Y. Isolation and Characterization of Autophagy-Defective Mutants of Saccharomyces Cerevisiae. FEBS Letters 1993, 333, 169–174. [Google Scholar] [CrossRef]
- Suzuki, S.W.; Onodera, J.; Ohsumi, Y. Starvation Induced Cell Death in Autophagy-Defective Yeast Mutants Is Caused by Mitochondria Dysfunction. PLoS ONE 2011, 6, e17412. [Google Scholar] [CrossRef] [PubMed]
- Shang, C.; Liu, Z.; Zhu, Y.; Lu, J.; Ge, C.; Zhang, C.; Li, N.; Jin, N.; Li, Y.; Tian, M.; et al. SARS-CoV-2 Causes Mitochondrial Dysfunction and Mitophagy Impairment. Front Microbiol 2021, 12, 780768. [Google Scholar] [CrossRef]
- Yang, X.; Zhang, R.; Nakahira, K.; Gu, Z. Mitochondrial DNA Mutation, Diseases, and Nutrient-Regulated Mitophagy. Annu Rev Nutr 2019, 39, 201–226. [Google Scholar] [CrossRef]
- Chourasia, A.H.; Boland, M.L.; Macleod, K.F. Mitophagy and Cancer. Cancer & Metabolism 2015, 3, 4. [Google Scholar] [CrossRef]
- Park, H.; Kang, J.-H.; Lee, S. Autophagy in Neurodegenerative Diseases: A Hunter for Aggregates. International Journal of Molecular Sciences 2020, 21, 3369. [Google Scholar] [CrossRef]
- Su, L.; Zhang, J.; Gomez, H.; Kellum, J.A.; Peng, Z. Mitochondria ROS and Mitophagy in Acute Kidney Injury. Autophagy 2023, 19, 401–414. [Google Scholar] [CrossRef] [PubMed]
- Cheng, Y.; Luo, R.; Wang, K.; Zhang, M.; Wang, Z.; Dong, L.; Li, J.; Yao, Y.; Ge, S.; Xu, G. Kidney Disease Is Associated with In-Hospital Death of Patients with COVID-19. Kidney International 2020, 97, 829–838. [Google Scholar] [CrossRef]
- Bruchfeld, A. The COVID-19 Pandemic: Consequences for Nephrology. Nat Rev Nephrol 2021, 17, 81–82. [Google Scholar] [CrossRef] [PubMed]
- Vargas, J.N.S.; Hamasaki, M.; Kawabata, T.; Youle, R.J.; Yoshimori, T. The Mechanisms and Roles of Selective Autophagy in Mammals. Nat Rev Mol Cell Biol 2023, 24, 167–185. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, H.; Zhang, S.; Mizushima, N. Autophagy Genes in Biology and Disease. Nat Rev Genet 2023, 24, 382–400. [Google Scholar] [CrossRef] [PubMed]
- Lei, Y.; Klionsky, D.J. Transcriptional Regulation of Autophagy and Its Implications in Human Disease. Cell Death Differ 2023, 1–14. [Google Scholar] [CrossRef]
- Kriegenburg, F.; Ellgaard, L.; Hartmann-Petersen, R. Molecular Chaperones in Targeting Misfolded Proteins for Ubiquitin-Dependent Degradation. The FEBS Journal 2012, 279, 532–542. [Google Scholar] [CrossRef]
- Hartl, F.U.; Bracher, A.; Hayer-Hartl, M. Molecular Chaperones in Protein Folding and Proteostasis. Nature 2011, 475, 324–332. [Google Scholar] [CrossRef]
- Arndt, V.; Rogon, C.; Höhfeld, J. To Be, or Not to Be — Molecular Chaperones in Protein Degradation. Cell. Mol. Life Sci. 2007, 64, 2525. [Google Scholar] [CrossRef]
- Dice, J.F. Chaperone-Mediated Autophagy. Autophagy 2007, 3, 295–299. [Google Scholar] [CrossRef]
- Lescat, L.; Véron, V.; Mourot, B.; Péron, S.; Chenais, N.; Dias, K.; Riera-Heredia, N.; Beaumatin, F.; Pinel, K.; Priault, M.; et al. Chaperone-Mediated Autophagy in the Light of Evolution: Insight from Fish. Molecular Biology and Evolution 2020, 37, 2887–2899. [Google Scholar] [CrossRef]
- Liao, Z.; Wang, B.; Liu, W.; Xu, Q.; Hou, L.; Song, J.; Guo, Q.; Li, N. Dysfunction of Chaperone-Mediated Autophagy in Human Diseases. Mol Cell Biochem 2021, 476, 1439–1454. [Google Scholar] [CrossRef]
- Finn, P.F.; Dice, J.F. Ketone Bodies Stimulate Chaperone-MediatedAutophagy *. Journal of Biological Chemistry 2005, 280, 25864–25870. [Google Scholar] [CrossRef] [PubMed]
- Cuervo, A.M.; Knecht, E.; Terlecky, S.R.; Dice, J.F. Activation of a Selective Pathway of Lysosomal Proteolysis in Rat Liver by Prolonged Starvation. American Journal of Physiology-Cell Physiology 1995, 269, C1200–C1208. [Google Scholar] [CrossRef] [PubMed]
- Schneider, J.L.; Suh, Y.; Cuervo, A.M. Deficient Chaperone-Mediated Autophagy in Liver Leads to Metabolic Dysregulation. Cell Metabolism 2014, 20, 417–432. [Google Scholar] [CrossRef]
- Hurley, J.H.; Young, L.N. Mechanisms of Autophagy Initiation. Annual Review of Biochemistry 2017, 86, 225–244. [Google Scholar] [CrossRef] [PubMed]
- Montella-Manuel, S.; Pujol-Carrion, N.; Mechoud, M.A.; de la Torre-Ruiz, M.A. Bulk Autophagy Induction and Life Extension Is Achieved When Iron Is the Only Limited Nutrient in Saccharomyces Cerevisiae. Biochem J 2021, 478, 811–837. [Google Scholar] [CrossRef]
- Bento, C.F.; Renna, M.; Ghislat, G.; Puri, C.; Ashkenazi, A.; Vicinanza, M.; Menzies, F.M.; Rubinsztein, D.C. Mammalian Autophagy: How Does It Work? Annu. Rev. Biochem. 2016, 85, 685–713. [Google Scholar] [CrossRef]
- Cheng, X.; Chen, Q.; Sun, P. Natural Phytochemicals That Affect Autophagy in the Treatment of Oral Diseases and Infections: A Review. Frontiers in Pharmacology 2022, 13. [Google Scholar] [CrossRef] [PubMed]
- Halma, M.T.J.; Plothe, C.; Marik, P.; Lawrie, T.A. Strategies for the Management of Spike Protein-Related Pathology. Microorganisms 2023, 11, 1308. [Google Scholar] [CrossRef]
- Tanikawa, T.; Kiba, Y.; Yu, J.; Hsu, K.; Chen, S.; Ishii, A.; Yokogawa, T.; Suzuki, R.; Inoue, Y.; Kitamura, M. Degradative Effect of Nattokinase on Spike Protein of SARS-CoV-2. Molecules 2022, 27, 5405. [Google Scholar] [CrossRef]
- Oba, M.; Rongduo, W.; Saito, A.; Okabayashi, T.; Yokota, T.; Yasuoka, J.; Sato, Y.; Nishifuji, K.; Wake, H.; Nibu, Y.; et al. Natto Extract, a Japanese Fermented Soybean Food, Directly Inhibits Viral Infections Including SARS-CoV-2 in Vitro. Biochemical and Biophysical Research Communications 2021, 570, 21–25. [Google Scholar] [CrossRef]
- Grune, T.; Jung, T.; Merker, K.; Davies, K.J.A. Decreased Proteolysis Caused by Protein Aggregates, Inclusion Bodies, Plaques, Lipofuscin, Ceroid, and ‘Aggresomes’ during Oxidative Stress, Aging, and Disease. The International Journal of Biochemistry & Cell Biology 2004, 36, 2519–2530. [Google Scholar] [CrossRef]
- Fujita, M.; Nomura, K.; Hong, K.; Ito, Y.; Asada, A.; Nishimuro, S. Purification and Characterization of a Strong Fibrinolytic Enzyme (Nattokinase) in the Vegetable Cheese Natto, a Popular Soybean Fermented Food in Japan. Biochemical and Biophysical Research Communications 1993, 197, 1340–1347. [Google Scholar] [CrossRef]
- Sumi, H.; Hamada, H.; Tsushima, H.; Mihara, H.; Muraki, H. A Novel Fibrinolytic Enzyme (Nattokinase) in the Vegetable Cheese Natto; a Typical and Popular Soybean Food in the Japanese Diet. Experientia 1987, 43, 1110–1111. [Google Scholar] [CrossRef]
- Chen, H.; McGowan, E.M.; Ren, N.; Lal, S.; Nassif, N.; Shad-Kaneez, F.; Qu, X.; Lin, Y. Nattokinase: A Promising Alternative in Prevention and Treatment of Cardiovascular Diseases. Biomark�Insights 2018, 13, 1177271918785130. [Google Scholar] [CrossRef] [PubMed]
- Jang, J.-Y.; Kim, T.-S.; Cai, J.; Kim, J.; Kim, Y.; Shin, K.; Kim, K.S.; Park, S.K.; Lee, S.-P.; Choi, E.-K.; et al. Nattokinase Improves Blood Flow by Inhibiting Platelet Aggregation and Thrombus Formation. Lab Anim Res 2013, 29, 221–225. [Google Scholar] [CrossRef] [PubMed]
- Pais, E.; Alexy, T.; Holsworth, J.; Meiselman, H.J. Effects of Nattokinase, a pro-Fibrinolytic Enzyme, on Red Blood Cell Aggregation and Whole Blood Viscosity. Clinical Hemorheology and Microcirculation 2006, 35, 139–142. [Google Scholar] [PubMed]
- Kurosawa, Y.; Nirengi, S.; Homma, T.; Esaki, K.; Ohta, M.; Clark, J.F.; Hamaoka, T. A Single-Dose of Oral Nattokinase Potentiates Thrombolysis and Anti-Coagulation Profiles. Sci Rep 2015, 5, 11601. [Google Scholar] [CrossRef]
- Hsu, R.-L.; Lee, K.-T.; Wang, J.-H.; Lee, L.Y.-L.; Chen, R.P.-Y. Amyloid-Degrading Ability of Nattokinase from Bacillus Subtilis Natto. J. Agric. Food Chem. 2009, 57, 503–508. [Google Scholar] [CrossRef]
- Yanagisawa, Y.; Chatake, T.; Chiba-Kamoshida, K.; Naito, S.; Ohsugi, T.; Sumi, H.; Yasuda, I.; Morimoto, Y. Purification, Crystallization and Preliminary X-Ray Diffraction Experiment of Nattokinase from Bacillus Subtilis Natto. Acta Crystallogr Sect F Struct Biol Cryst Commun 2010, 66, 1670–1673. [Google Scholar] [CrossRef]
- Frallicciardi, J.; Gabba, M.; Poolman, B. Determining Small-Molecule Permeation through Lipid Membranes. Nat Protoc 2022, 17, 2620–2646. [Google Scholar] [CrossRef]
- Jamshed, H.; Beyl, R.A.; Della Manna, D.L.; Yang, E.S.; Ravussin, E.; Peterson, C.M. Early Time-Restricted Feeding Improves 24-Hour Glucose Levels and Affects Markers of the Circadian Clock, Aging, and Autophagy in Humans. Nutrients 2019, 11, 1234. [Google Scholar] [CrossRef]
- Alirezaei, M.; Kemball, C.C.; Flynn, C.T.; Wood, M.R.; Whitton, J.L.; Kiosses, W.B. Short-Term Fasting Induces Profound Neuronal Autophagy. Autophagy 2010, 6, 702–710. [Google Scholar] [CrossRef] [PubMed]
- Godar, R.J.; Ma, X.; Liu, H.; Murphy, J.T.; Weinheimer, C.J.; Kovacs, A.; Crosby, S.D.; Saftig, P.; Diwan, A. Repetitive Stimulation of Autophagy-Lysosome Machinery by Intermittent Fasting Preconditions the Myocardium to Ischemia-Reperfusion Injury. Autophagy 2015, 11, 1537–1560. [Google Scholar] [CrossRef] [PubMed]
- Martinez-Lopez, N.; Tarabra, E.; Toledo, M.; Garcia-Macia, M.; Sahu, S.; Coletto, L.; Batista-Gonzalez, A.; Barzilai, N.; Pessin, J.E.; Schwartz, G.J.; et al. System-Wide Benefits of Intermeal Fasting by Autophagy. Cell Metabolism 2017, 26, 856–871.e5. [Google Scholar] [CrossRef] [PubMed]
- Fernandes, S.A.; Demetriades, C. The Multifaceted Role of Nutrient Sensing and MTORC1 Signaling in Physiology and Aging. Frontiers in Aging 2021, 2. [Google Scholar] [CrossRef]
- Kim, J.; Guan, K.-L. MTOR as a Central Hub of Nutrient Signalling and Cell Growth. Nat Cell Biol 2019, 21, 63–71. [Google Scholar] [CrossRef]
- Yu, L.; McPhee, C.K.; Zheng, L.; Mardones, G.A.; Rong, Y.; Peng, J.; Mi, N.; Zhao, Y.; Liu, Z.; Wan, F.; et al. Termination of Autophagy and Reformation of Lysosomes Regulated by MTOR. Nature 2010, 465, 942–946. [Google Scholar] [CrossRef]
- Regmi, P.; Heilbronn, L.K. Time-Restricted Eating: Benefits, Mechanisms, and Challenges in Translation. iScience 2020, 23, 101161. [Google Scholar] [CrossRef]
- Longo, V.D.; Mattson, M.P. Fasting: Molecular Mechanisms and Clinical Applications. Cell Metab 2014, 19, 181–192. [Google Scholar] [CrossRef]
- Mattson, M.P.; Longo, V.D.; Harvie, M. Impact of Intermittent Fasting on Health and Disease Processes. Ageing Research Reviews 2017, 39, 46–58. [Google Scholar] [CrossRef]
- Anton, S.D.; Moehl, K.; Donahoo, W.T.; Marosi, K.; Lee, S.A.; Mainous, A.G.; Leeuwenburgh, C.; Mattson, M.P. Flipping the Metabolic Switch: Understanding and Applying the Health Benefits of Fasting. Obesity (Silver Spring) 2018, 26, 254–268. [Google Scholar] [CrossRef]
- Patterson, R.E.; Sears, D.D. Metabolic Effects of Intermittent Fasting. Annual Review of Nutrition 2017, 37, 371–393. [Google Scholar] [CrossRef]
- Chowdhury, E.A.; Richardson, J.D.; Tsintzas, K.; Thompson, D.; Betts, J.A. Effect of Extended Morning Fasting upon Ad Libitum Lunch Intake and Associated Metabolic and Hormonal Responses in Obese Adults. Int J Obes 2016, 40, 305–311. [Google Scholar] [CrossRef]
- Fuhrman, J.; Sarter, B.; Glaser, D.; Acocella, S. Changing Perceptions of Hunger on a High Nutrient Density Diet. Nutr J 2010, 9, 51. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, C.L.P.; Boulé, N.G.; Berg, A.; Sharma, A.M.; Elliott, S.A.; Siervo, M.; Ghosh, S.; Prado, C.M. Consumption of a High-Protein Meal Replacement Leads to Higher Fat Oxidation, Suppression of Hunger, and Improved Metabolic Profile After an Exercise Session. Nutrients 2021, 13, 155. [Google Scholar] [CrossRef]
- Zauner, C.; Schneeweiss, B.; Kranz, A.; Madl, C.; Ratheiser, K.; Kramer, L.; Roth, E.; Schneider, B.; Lenz, K. Resting Energy Expenditure in Short-Term Starvation Is Increased as a Result of an Increase in Serum Norepinephrine. The American journal of clinical nutrition 2000, 71, 1511–1515. [Google Scholar] [CrossRef] [PubMed]
- Catenacci, V.A.; Pan, Z.; Ostendorf, D.; Brannon, S.; Gozansky, W.S.; Mattson, M.P.; Martin, B.; MacLean, P.S.; Melanson, E.L.; Troy Donahoo, W. A Randomized Pilot Study Comparing Zero-calorie Alternate-day Fasting to Daily Caloric Restriction in Adults with Obesity. Obesity 2016, 24, 1874–1883. [Google Scholar] [CrossRef] [PubMed]
- Thissen, J.-P.; Ketelslegers, J.-M.; Underwood, L.E. Nutritional Regulation of the Insulin-like Growth Factors. Endocrine reviews 1994, 15, 80–101. [Google Scholar] [CrossRef] [PubMed]
- Ho, K.Y.; Veldhuis, J.D.; Johnson, M.L.; Furlanetto, R.; Evans, W.S.; Alberti, K.; Thorner, M. Fasting Enhances Growth Hormone Secretion and Amplifies the Complex Rhythms of Growth Hormone Secretion in Man. The Journal of clinical investigation 1988, 81, 968–975. [Google Scholar] [CrossRef]
- Harvie, M.N.; Pegington, M.; Mattson, M.P.; Frystyk, J.; Dillon, B.; Evans, G.; Cuzick, J.; Jebb, S.A.; Martin, B.; Cutler, R.G. The Effects of Intermittent or Continuous Energy Restriction on Weight Loss and Metabolic Disease Risk Markers: A Randomized Trial in Young Overweight Women. International journal of obesity 2011, 35, 714–727. [Google Scholar] [CrossRef]
- Harvie, M.; Wright, C.; Pegington, M.; McMullan, D.; Mitchell, E.; Martin, B.; Cutler, R.G.; Evans, G.; Whiteside, S.; Maudsley, S. The Effect of Intermittent Energy and Carbohydrate Restriction v. Daily Energy Restriction on Weight Loss and Metabolic Disease Risk Markers in Overweight Women. British Journal of Nutrition 2013, 110, 1534–1547. [Google Scholar] [CrossRef]
- He, Z.; Xu, H.; Li, C.; Yang, H.; Mao, Y. Intermittent Fasting and Immunomodulatory Effects: A Systematic Review. Frontiers in Nutrition 2023, 10. [Google Scholar] [CrossRef] [PubMed]
- Lettieri-Barbato, D.; Cannata, S.M.; Casagrande, V.; Ciriolo, M.R.; Aquilano, K. Time-Controlled Fasting Prevents Aging-like Mitochondrial Changes Induced by Persistent Dietary Fat Overload in Skeletal Muscle. PLOS ONE 2018, 13, e0195912. [Google Scholar] [CrossRef]
- Singh, R.; Mohapatra, L.; Tripathi, A.S. Targeting Mitochondrial Biogenesis: A Potential Approach for Preventing and Controlling Diabetes. Future Journal of Pharmaceutical Sciences 2021, 7, 212. [Google Scholar] [CrossRef]
- Rojas-Morales, P.; León-Contreras, J.C.; Granados-Pineda, J.; Hernández-Pando, R.; Gonzaga, G.; Sánchez-Lozada, L.G.; Osorio-Alonso, H.; Pedraza-Chaverri, J.; Tapia, E. Protection against Renal Ischemia and Reperfusion Injury by Short-Term Time-Restricted Feeding Involves the Mitochondrial Unfolded Protein Response. Free Radical Biology and Medicine 2020, 154, 75–83. [Google Scholar] [CrossRef] [PubMed]
- Real-Hohn, A.; Navegantes, C.; Ramos, K.; Ramos-Filho, D.; Cahuê, F.; Galina, A.; Salerno, V.P. The Synergism of High-Intensity Intermittent Exercise and Every-Other-Day Intermittent Fasting Regimen on Energy Metabolism Adaptations Includes Hexokinase Activity and Mitochondrial Efficiency. PLOS ONE 2018, 13, e0202784. [Google Scholar] [CrossRef]
- Cheng, C.-W.; Adams, G.B.; Perin, L.; Wei, M.; Zhou, X.; Lam, B.S.; Da Sacco, S.; Mirisola, M.; Quinn, D.I.; Dorff, T.B.; et al. Prolonged Fasting Reduces IGF-1/PKA to Promote Hematopoietic-Stem-Cell-Based Regeneration and Reverse Immunosuppression. Cell Stem Cell 2014, 14, 810–823. [Google Scholar] [CrossRef]
- Sutton, E.F.; Beyl, R.; Early, K.S.; Cefalu, W.T.; Ravussin, E.; Peterson, C.M. Early Time-Restricted Feeding Improves Insulin Sensitivity, Blood Pressure, and Oxidative Stress Even without Weight Loss in Men with Prediabetes. Cell Metabolism 2018, 27, 1212–1221.e3. [Google Scholar] [CrossRef]
- Rajpal, A.; Ismail-Beigi, F. Intermittent Fasting and ‘Metabolic Switch’: Effects on Metabolic Syndrome, Prediabetes and Type 2 Diabetes. Diabetes, Obesity and Metabolism 2020, 22, 1496–1510. [Google Scholar] [CrossRef]
- Guo, Y.; Luo, S.; Ye, Y.; Yin, S.; Fan, J.; Xia, M. Intermittent Fasting Improves Cardiometabolic Risk Factors and Alters Gut Microbiota in Metabolic Syndrome Patients. The Journal of Clinical Endocrinology & Metabolism 2021, 106, 64–79. [Google Scholar] [CrossRef]
- Furmli, S.; Elmasry, R.; Ramos, M.; Fung, J. Therapeutic Use of Intermittent Fasting for People with Type 2 Diabetes as an Alternative to Insulin. Case Reports 2018, 2018, bcr. [Google Scholar] [CrossRef]
- Albosta, M.; Bakke, J. Intermittent Fasting: Is There a Role in the Treatment of Diabetes? A Review of the Literature and Guide for Primary Care Physicians. Clinical Diabetes and Endocrinology 2021, 7, 3. [Google Scholar] [CrossRef] [PubMed]
- Mattson, M.P.; Wan, R. Beneficial Effects of Intermittent Fasting and Caloric Restriction on the Cardiovascular and Cerebrovascular Systems. The Journal of Nutritional Biochemistry 2005, 16, 129–137. [Google Scholar] [CrossRef] [PubMed]
- Martin, B.; Mattson, M.P.; Maudsley, S. Caloric Restriction and Intermittent Fasting: Two Potential Diets for Successful Brain Aging. Ageing Research Reviews 2006, 5, 332–353. [Google Scholar] [CrossRef] [PubMed]
- Clifton, K.K.; Ma, C.X.; Fontana, L.; Peterson, L.L. Intermittent Fasting in the Prevention and Treatment of Cancer. CA: A Cancer Journal for Clinicians 2021, 71, 527–546. [Google Scholar] [CrossRef] [PubMed]
- Pietrocola, F.; Lachkar, S.; Enot, D.P.; Niso-Santano, M.; Pedro, J.M.B.-S.; Sica, V.; Izzo, V.; Maiuri, M.C.; Madeo, F.; Mariño, G.; et al. Spermidine Induces Autophagy by Inhibiting the Acetyltransferase EP300. Cell Death and Differentiation 2015, 22, 509. [Google Scholar] [CrossRef]
- Ali, M.A.; Poortvliet, E.; Strömberg, R.; Yngve, A. Polyamines in Foods: Development of a Food Database. Food & Nutrition Research 2011. [CrossRef]
- Madeo, F.; Hofer, S.J.; Pendl, T.; Bauer, M.A.; Eisenberg, T.; Carmona-Gutierrez, D.; Kroemer, G. Nutritional Aspects of Spermidine. Annual Review of Nutrition 2020, 40, 135–159. [Google Scholar] [CrossRef]
- Soda, K.; Kano, Y.; Sakuragi, M.; Takao, K.; Lefor, A.; Konishi, F. Long-Term Oral Polyamine Intake Increases Blood Polyamine Concentrations. J Nutr Sci Vitaminol (Tokyo) 2009, 55, 361–366. [Google Scholar] [CrossRef]
- Soda, K.; Uemura, T.; Sanayama, H.; Igarashi, K.; Fukui, T. Polyamine-Rich Diet Elevates Blood Spermine Levels and Inhibits Pro-Inflammatory Status: An Interventional Study. Med Sci (Basel) 2021, 9, 22. [Google Scholar] [CrossRef]
- Senekowitsch, S.; Wietkamp, E.; Grimm, M.; Schmelter, F.; Schick, P.; Kordowski, A.; Sina, C.; Otzen, H.; Weitschies, W.; Smollich, M. High-Dose Spermidine Supplementation Does Not Increase Spermidine Levels in Blood Plasma and Saliva of Healthy Adults: A Randomized Placebo-Controlled Pharmacokinetic and Metabolomic Study. Nutrients 2023, 15, 1852. [Google Scholar] [CrossRef]
- Madeo, F.; Eisenberg, T.; Pietrocola, F.; Kroemer, G. Spermidine in Health and Disease. Science 2018, 359, eaan2788. [Google Scholar] [CrossRef]
- Wirth, M.; Benson, G.; Schwarz, C.; Köbe, T.; Grittner, U.; Schmitz, D.; Sigrist, S.J.; Bohlken, J.; Stekovic, S.; Madeo, F.; et al. The Effect of Spermidine on Memory Performance in Older Adults at Risk for Dementia: A Randomized Controlled Trial. Cortex 2018, 109, 181–188. [Google Scholar] [CrossRef] [PubMed]
- Schwarz, C.; Benson, G.S.; Horn, N.; Wurdack, K.; Grittner, U.; Schilling, R.; Märschenz, S.; Köbe, T.; Hofer, S.J.; Magnes, C.; et al. Effects of Spermidine Supplementation on Cognition and Biomarkers in Older Adults With Subjective Cognitive Decline: A Randomized Clinical Trial. JAMA Netw Open 2022, 5, e2213875. [Google Scholar] [CrossRef] [PubMed]
- Schwarz, C.; Stekovic, S.; Wirth, M.; Benson, G.; Royer, P.; Sigrist, S.J.; Pieber, T.; Dammbrueck, C.; Magnes, C.; Eisenberg, T.; et al. Safety and Tolerability of Spermidine Supplementation in Mice and Older Adults with Subjective Cognitive Decline. Aging 2018, 10, 19–33. [Google Scholar] [CrossRef] [PubMed]
- Ray, K. Caffeine Is a Potent Stimulator of Autophagy to Reduce Hepatic Lipid Content—a Coffee for NAFLD? Nat Rev Gastroenterol Hepatol 2013, 10, 563–563. [Google Scholar] [CrossRef]
- Pietrocola, F.; Malik, S.A.; Mariño, G.; Vacchelli, E.; Senovilla, L.; Chaba, K.; Niso-Santano, M.; Maiuri, M.C.; Madeo, F.; Kroemer, G. Coffee Induces Autophagy in Vivo. Cell Cycle 2014, 13, 1987–1994. [Google Scholar] [CrossRef]
- Ferraresi, A.; Titone, R.; Follo, C.; Castiglioni, A.; Chiorino, G.; Dhanasekaran, D.N.; Isidoro, C. The Protein Restriction Mimetic Resveratrol Is an Autophagy Inducer Stronger than Amino Acid Starvation in Ovarian Cancer Cells. Molecular Carcinogenesis 2017, 56, 2681–2691. [Google Scholar] [CrossRef]
- Josifovska, N.; Albert, R.; Nagymihály, R.; Lytvynchuk, L.; Moe, M.C.; Kaarniranta, K.; Veréb, Z.J.; Petrovski, G. Resveratrol as Inducer of Autophagy, Pro-Survival, and Anti-Inflammatory Stimuli in Cultured Human RPE Cells. Int J Mol Sci 2020, 21, 813. [Google Scholar] [CrossRef] [PubMed]
- Meng, T.; Xiao, D.; Muhammed, A.; Deng, J.; Chen, L.; He, J. Anti-Inflammatory Action and Mechanisms of Resveratrol. Molecules 2021, 26, 229. [Google Scholar] [CrossRef]
- Pasquereau, S.; Nehme, Z.; Haidar Ahmad, S.; Daouad, F.; Van Assche, J.; Wallet, C.; Schwartz, C.; Rohr, O.; Morot-Bizot, S.; Herbein, G. Resveratrol Inhibits HCoV-229E and SARS-CoV-2 Coronavirus Replication In Vitro. Viruses 2021, 13, 354. [Google Scholar] [CrossRef]
- Chen, K.; Zhao, H.; Shu, L.; Xing, H.; Wang, C.; Lu, C.; Song, G. Effect of Resveratrol on Intestinal Tight Junction Proteins and the Gut Microbiome in High-Fat Diet-Fed Insulin Resistant Mice. International Journal of Food Sciences and Nutrition 2020, 71, 965–978. [Google Scholar] [CrossRef]
- Chatam, O.; Chapnik, N.; Froy, O. Resveratrol Induces the Fasting State and Alters Circadian Metabolism in Hepatocytes. Plant Foods Hum Nutr 2022, 77, 128–134. [Google Scholar] [CrossRef]
- Park, D.; Jeong, H.; Lee, M.N.; Koh, A.; Kwon, O.; Yang, Y.R.; Noh, J.; Suh, P.-G.; Park, H.; Ryu, S.H. Resveratrol Induces Autophagy by Directly Inhibiting MTOR through ATP Competition. Scientific reports 2016, 6, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Hewlings, S.J.; Kalman, D.S. Curcumin: A Review of Its Effects on Human Health. Foods 2017, 6, 92. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.J.; Kim, N.-Y.; Suh, Y.-A.; Lee, C. Involvement of ROS in Curcumin-Induced Autophagic Cell Death. Korean J Physiol Pharmacol 2011, 15, 1–7. [Google Scholar] [CrossRef]
- Shakeri, A.; Cicero, A.F.G.; Panahi, Y.; Mohajeri, M.; Sahebkar, A. Curcumin: A Naturally Occurring Autophagy Modulator. J Cell Physiol 2019, 234, 5643–5654. [Google Scholar] [CrossRef] [PubMed]
- Anand, P.; Kunnumakkara, A.B.; Newman, R.A.; Aggarwal, B.B. Bioavailability of Curcumin: Problems and Promises. Mol. Pharmaceutics 2007, 4, 807–818. [Google Scholar] [CrossRef] [PubMed]
- Shoba, G.; Joy, D.; Joseph, T.; Majeed, M.; Rajendran, R.; Srinivas, P.S. Influence of Piperine on the Pharmacokinetics of Curcumin in Animals and Human Volunteers. Planta Med 1998, 64, 353–356. [Google Scholar] [CrossRef]
- Ferrari, E.; Bettuzzi, S.; Naponelli, V. The Potential of Epigallocatechin Gallate (EGCG) in Targeting Autophagy for Cancer Treatment: A Narrative Review. International Journal of Molecular Sciences 2022, 23, 6075. [Google Scholar] [CrossRef]
- Zhou, J.; Farah, B.L.; Sinha, R.A.; Wu, Y.; Singh, B.K.; Bay, B.-H.; Yang, C.S.; Yen, P.M. Epigallocatechin-3-Gallate (EGCG), a Green Tea Polyphenol, Stimulates Hepatic Autophagy and Lipid Clearance. PLOS ONE 2014, 9, e87161. [Google Scholar] [CrossRef]
- Rubinsztein, D.C.; Nixon, R.A. Rapamycin Induces Autophagic Flux in Neurons. Proceedings of the National Academy of Sciences 2010, 107, E181–E181. [Google Scholar] [CrossRef]
- Rangaraju, S.; Verrier, J.D.; Madorsky, I.; Nicks, J.; Dunn, W.A.; Notterpek, L. Rapamycin Activates Autophagy and Improves Myelination in Explant Cultures from Neuropathic Mice. J. Neurosci. 2010, 30, 11388–11397. [Google Scholar] [CrossRef]
- Sarkar, S.; Ravikumar, B.; Floto, R.A.; Rubinsztein, D.C. Rapamycin and MTOR-Independent Autophagy Inducers Ameliorate Toxicity of Polyglutamine-Expanded Huntingtin and Related Proteinopathies. Cell Death Differ 2009, 16, 46–56. [Google Scholar] [CrossRef] [PubMed]
- Sotthibundhu, A.; McDonagh, K.; von Kriegsheim, A.; Garcia-Munoz, A.; Klawiter, A.; Thompson, K.; Chauhan, K.D.; Krawczyk, J.; McInerney, V.; Dockery, P.; et al. Rapamycin Regulates Autophagy and Cell Adhesion in Induced Pluripotent Stem Cells. Stem Cell Res Ther 2016, 7, 166. [Google Scholar] [CrossRef]
- Lin, S.-R.; Fu, Y.-S.; Tsai, M.-J.; Cheng, H.; Weng, C.-F. Natural Compounds from Herbs That Can Potentially Execute as Autophagy Inducers for Cancer Therapy. Int J Mol Sci 2017, 18, 1412. [Google Scholar] [CrossRef] [PubMed]
- Martin-Rincon, M.; Morales-Alamo, D.; Calbet, J. a. L. Exercise-Mediated Modulation of Autophagy in Skeletal Muscle. Scandinavian Journal of Medicine & Science in Sports 2018, 28, 772–781. [Google Scholar] [CrossRef]
- He, C.; Bassik, M.C.; Moresi, V.; Sun, K.; Wei, Y.; Zou, Z.; An, Z.; Loh, J.; Fisher, J.; Sun, Q.; et al. Exercise-Induced BCL2-Regulated Autophagy Is Required for Muscle Glucose Homeostasis. Nature 2012, 481, 511–515. [Google Scholar] [CrossRef] [PubMed]
- Vainshtein, A.; Hood, D.A. The Regulation of Autophagy during Exercise in Skeletal Muscle. Journal of Applied Physiology 2016, 120, 664–673. [Google Scholar] [CrossRef]
- Summers, C.M.; Valentine, R.J. Acute Heat Exposure Alters Autophagy Signaling in C2C12 Myotubes. Frontiers in Physiology 2020, 10. [Google Scholar] [CrossRef]
- Moser, J.C.; Salvador, E.; Deniz, K.; Swanson, K.; Tuszynski, J.; Carlson, K.W.; Karanam, N.K.; Patel, C.B.; Story, M.; Lou, E.; et al. The Mechanisms of Action of Tumor Treating Fields. Cancer Research 2022, 82, 3650–3658. [Google Scholar] [CrossRef]
- He-Ling, D.; Hong-Yuan, W.; Zhen-Xiang, T.; Zhi, L.; Yi-Fen, W.; Jun, Z. Electrical Stimulation Induces Mitochondrial Autophagy via Activating Oxidative Stress and Sirt3 Signaling Pathway. Chinese Medical Journal 2021. [Google Scholar] [CrossRef]
- Lyamzaev, K.G.; Tokarchuk, A.V.; Panteleeva, A.A.; Mulkidjanian, A.Y.; Skulachev, V.P.; Chernyak, B.V. Induction of Autophagy by Depolarization of Mitochondria. Autophagy 2018, 14, 921–924. [Google Scholar] [CrossRef] [PubMed]
- Denaro, C.A.; Haloush, Y.I.; Hsiao, S.Y.; Orgera, J.J.; Osorio, T.; Riggs, L.M.; Sassaman, J.W.; Williams, S.A.; Monte Carlo, A.R.; Da Costa, R.T.; et al. COVID-19 and Neurodegeneration: The Mitochondrial Connection. Aging Cell 2022, 21, e13727. [Google Scholar] [CrossRef] [PubMed]
- Narendra, D.; Tanaka, A.; Suen, D.-F.; Youle, R.J. Parkin Is Recruited Selectively to Impaired Mitochondria and Promotes Their Autophagy. Journal of Cell Biology 2008, 183, 795–803. [Google Scholar] [CrossRef] [PubMed]
- Yamano, K.; Youle, R.J. PINK1 Is Degraded through the N-End Rule Pathway. Autophagy 2013, 9, 1758–1769. [Google Scholar] [CrossRef] [PubMed]
- Kazlauskaite, A.; Kondapalli, C.; Gourlay, R.; Campbell, D.G.; Ritorto, M.S.; Hofmann, K.; Alessi, D.R.; Knebel, A.; Trost, M.; Muqit, M.M.K. Parkin Is Activated by PINK1-Dependent Phosphorylation of Ubiquitin at Ser65. Biochemical Journal 2014, 460, 127–141. [Google Scholar] [CrossRef]
- Shiba-Fukushima, K.; Arano, T.; Matsumoto, G.; Inoshita, T.; Yoshida, S.; Ishihama, Y.; Ryu, K.-Y.; Nukina, N.; Hattori, N.; Imai, Y. Phosphorylation of Mitochondrial Polyubiquitin by PINK1 Promotes Parkin Mitochondrial Tethering. PLOS Genetics 2014, 10, e1004861. [Google Scholar] [CrossRef]
- Koyano, F.; Okatsu, K.; Kosako, H.; Tamura, Y.; Go, E.; Kimura, M.; Kimura, Y.; Tsuchiya, H.; Yoshihara, H.; Hirokawa, T.; et al. Ubiquitin Is Phosphorylated by PINK1 to Activate Parkin. Nature 2014, 510, 162–166. [Google Scholar] [CrossRef]
- Kane, L.A.; Lazarou, M.; Fogel, A.I.; Li, Y.; Yamano, K.; Sarraf, S.A.; Banerjee, S.; Youle, R.J. PINK1 Phosphorylates Ubiquitin to Activate Parkin E3 Ubiquitin Ligase Activity. Journal of Cell Biology 2014, 205, 143–153. [Google Scholar] [CrossRef]
- Heo, J.-M.; Ordureau, A.; Paulo, J.A.; Rinehart, J.; Harper, J.W. The PINK1-PARKIN Mitochondrial Ubiquitylation Pathway Drives a Program of OPTN/NDP52 Recruitment and TBK1 Activation to Promote Mitophagy. Molecular Cell 2015, 60, 7–20. [Google Scholar] [CrossRef] [PubMed]
- Hu, Y.; Li, X.-C.; Wang, Z.; Luo, Y.; Zhang, X.; Liu, X.-P.; Feng, Q.; Wang, Q.; Yue, Z.; Chen, Z.; et al. Tau Accumulation Impairs Mitophagy via Increasing Mitochondrial Membrane Potential and Reducing Mitochondrial Parkin. Oncotarget 2016, 7, 17356–17368. [Google Scholar] [CrossRef] [PubMed]
- Georgakopoulos, N.D.; Wells, G.; Campanella, M. The Pharmacological Regulation of Cellular Mitophagy. Nat Chem Biol 2017, 13, 136–146. [Google Scholar] [CrossRef] [PubMed]
- Huang, R.; Xu, Y.; Wan, W.; Shou, X.; Qian, J.; You, Z.; Liu, B.; Chang, C.; Zhou, T.; Lippincott-Schwartz, J.; et al. Deacetylation of Nuclear LC3 Drives Autophagy Initiation under Starvation. Mol Cell 2015, 57, 456–466. [Google Scholar] [CrossRef] [PubMed]
- Schiavi, A.; Maglioni, S.; Palikaras, K.; Shaik, A.; Strappazzon, F.; Brinkmann, V.; Torgovnick, A.; Castelein, N.; De Henau, S.; Braeckman, B.P.; et al. Iron-Starvation-Induced Mitophagy Mediates Lifespan Extension upon Mitochondrial Stress in C. Elegans. Curr Biol 2015, 25, 1810–1822. [Google Scholar] [CrossRef] [PubMed]
- Jang, S.; Kang, H.T.; Hwang, E.S. Nicotinamide-Induced Mitophagy: Event Mediated by High NAD+/NADH Ratio and SIRT1 Protein Activation. J Biol Chem 2012, 287, 19304–19314. [Google Scholar] [CrossRef] [PubMed]
- Block, T.; Kuo, J. Rationale for Nicotinamide Adenine Dinucleotide (NAD+) Metabolome Disruption as a Pathogenic Mechanism of Post-Acute COVID-19 Syndrome. Clin Med�Insights�Pathol 2022, 15, 2632010X221106986. [Google Scholar] [CrossRef]
- Domi, E.; Hoxha, M.; Kolovani, E.; Tricarico, D.; Zappacosta, B. The Importance of Nutraceuticals in COVID-19: What’s the Role of Resveratrol? Molecules 2022, 27, 2376. [Google Scholar] [CrossRef]
- Wissler Gerdes, E.O.; Vanichkachorn, G.; Verdoorn, B.P.; Hanson, G.J.; Joshi, A.Y.; Murad, M.H.; Rizza, S.A.; Hurt, R.T.; Tchkonia, T.; Kirkland, J.L. Role of Senescence in the Chronic Health Consequences of COVID-19. Translational Research 2022, 241, 96–108. [Google Scholar] [CrossRef]
- Kang, J.-W.; Hong, J.-M.; Lee, S.-M. Melatonin Enhances Mitophagy and Mitochondrial Biogenesis in Rats with Carbon Tetrachloride-Induced Liver Fibrosis. Journal of Pineal Research 2016, 60, 383–393. [Google Scholar] [CrossRef]
- Chen, C.; Yang, C.; Wang, J.; Huang, X.; Yu, H.; Li, S.; Li, S.; Zhang, Z.; Liu, J.; Yang, X.; et al. Melatonin Ameliorates Cognitive Deficits through Improving Mitophagy in a Mouse Model of Alzheimer’s Disease. J Pineal Res 2021, 71, e12774. [Google Scholar] [CrossRef] [PubMed]
- Coto-Montes, A.; Boga, J.A.; Rosales-Corral, S.; Fuentes-Broto, L.; Tan, D.-X.; Reiter, R.J. Role of Melatonin in the Regulation of Autophagy and Mitophagy: A Review. Molecular and Cellular Endocrinology 2012, 361, 12–23. [Google Scholar] [CrossRef] [PubMed]
- Bertholet, A.M.; Delerue, T.; Millet, A.M.; Moulis, M.F.; David, C.; Daloyau, M.; Arnauné-Pelloquin, L.; Davezac, N.; Mils, V.; Miquel, M.C.; et al. Mitochondrial Fusion/Fission Dynamics in Neurodegeneration and Neuronal Plasticity. Neurobiology of Disease 2016, 90, 3–19. [Google Scholar] [CrossRef] [PubMed]
- Hattori, N.; Saiki, S.; Imai, Y. Regulation by Mitophagy. Int J Biochem Cell Biol 2014, 53, 147–150. [Google Scholar] [CrossRef]
- Jornayvaz, F.R.; Shulman, G.I. Regulation of Mitochondrial Biogenesis. Essays in Biochemistry 2010, 47, 69–84. [Google Scholar] [CrossRef]
- Hwang, P.S.; Machek, S.B.; Cardaci, T.D.; Wilburn, D.T.; Kim, C.S.; Suezaki, E.S.; Willoughby, D.S. Effects of Pyrroloquinoline Quinone (PQQ) Supplementation on Aerobic Exercise Performance and Indices of Mitochondrial Biogenesis in Untrained Men. Journal of the American College of Nutrition 2020, 39, 547–556. [Google Scholar] [CrossRef]
- Chung, N.; Park, J.; Lim, K. The Effects of Exercise and Cold Exposure on Mitochondrial Biogenesis in Skeletal Muscle and White Adipose Tissue. J Exerc Nutrition Biochem 2017, 21, 39–47. [Google Scholar] [CrossRef]
- Booth, F.W.; Ruegsegger, G.N.; Toedebusch, R.G.; Yan, Z. Chapter Six - Endurance Exercise and the Regulation of Skeletal Muscle Metabolism. In Progress in Molecular Biology and Translational Science; Bouchard, C., Ed.; Molecular and Cellular Regulation of Adaptation to Exercise; Academic Press, 2015; Vol. 135, pp. 129–151.
- Coyle, E.F. Physiological Determinants of Endurance Exercise Performance. Journal of Science and Medicine in Sport 1999, 2, 181–189. [Google Scholar] [CrossRef]
- Cattadori, G.; Di Marco, S.; Baravelli, M.; Picozzi, A.; Ambrosio, G. Exercise Training in Post-COVID-19 Patients: The Need for a Multifactorial Protocol for a Multifactorial Pathophysiology. Journal of Clinical Medicine 2022, 11, 2228. [Google Scholar] [CrossRef]
- Nisoli, E.; Clementi, E.; Paolucci, C.; Cozzi, V.; Tonello, C.; Sciorati, C.; Bracale, R.; Valerio, A.; Francolini, M.; Moncada, S.; et al. Mitochondrial Biogenesis in Mammals: The Role of Endogenous Nitric Oxide. Science 2003, 299, 896–899. [Google Scholar] [CrossRef]
- Leary, S.C.; Shoubridge, E.A. Mitochondrial biogenesis: Which part of “NO” do we understand? BioEssays 2003, 25, 538–541. [Google Scholar] [CrossRef] [PubMed]
- Shen, W.; Zhang, X.; Zhao, G.; Wolin, M.S.; Sessa, W.; Hintze, T.H. Nitric Oxide Production and NO Synthase Gene Expression Contribute to Vascular Regulation during Exercise. Med Sci Sports Exerc 1995, 27, 1125–1134. [Google Scholar] [CrossRef] [PubMed]
- Roberts, C.K.; Barnard, R.J.; Jasman, A.; Balon, T.W. Acute Exercise Increases Nitric Oxide Synthase Activity in Skeletal Muscle. American Journal of Physiology-Endocrinology and Metabolism 1999, 277, E390–E394. [Google Scholar] [CrossRef]
- Hazell, G.; Khazova, M.; Cohen, H.; Felton, S.; Raj, K. Post-Exposure Persistence of Nitric Oxide Upregulation in Skin Cells Irradiated by UV-A. Sci Rep 2022, 12, 9465. [Google Scholar] [CrossRef]
- Puyaubert, J.; Baudouin, E. New Clues for a Cold Case: Nitric Oxide Response to Low Temperature. Plant, Cell & Environment 2014, 37, 2623–2630. [Google Scholar] [CrossRef]
- Sánchez-Vicente, I.; Lorenzo, O. Nitric Oxide Regulation of Temperature Acclimation: A Molecular Genetic Perspective. Journal of Experimental Botany 2021, 72, 5789–5794. [Google Scholar] [CrossRef] [PubMed]
- Zhen, J.; Lu, H.; Wang, X.Q.; Vaziri, N.D.; Zhou, X.J. Upregulation of Endothelial and Inducible Nitric Oxide Synthase Expression by Reactive Oxygen Species. American Journal of Hypertension 2008, 21, 28–34. [Google Scholar] [CrossRef]
- Kauser, K.; Rubanyi, G.M. Potential Cellular Signaling Mechanisms Mediating Upregulation of Endothelial Nitric Oxide Production by Estrogen. Journal of Vascular Research 2008, 34, 229–236. [Google Scholar] [CrossRef]
- Laufs, U.; La Fata, V.; Plutzky, J.; Liao, J.K. Upregulation of Endothelial Nitric Oxide Synthase by HMG CoA Reductase Inhibitors. Circulation 1998, 97, 1129–1135. [Google Scholar] [CrossRef]
- Kato, H.; Tanaka, G.; Masuda, S.; Ogasawara, J.; Sakurai, T.; Kizaki, T.; Ohno, H.; Izawa, T. Melatonin Promotes Adipogenesis and Mitochondrial Biogenesis in 3T3-L1 Preadipocytes. Journal of Pineal Research 2015, 59, 267–275. [Google Scholar] [CrossRef]
- Niu, Y.-J.; Zhou, W.; Nie, Z.-W.; Shin, K.-T.; Cui, X.-S. Melatonin Enhances Mitochondrial Biogenesis and Protects against Rotenone-Induced Mitochondrial Deficiency in Early Porcine Embryos. Journal of Pineal Research 2020, 68, e12627. [Google Scholar] [CrossRef] [PubMed]
- Cardinali, D.P.; Brown, G.M.; Pandi-Perumal, S.R. Possible Application of Melatonin in Long COVID. Biomolecules 2022, 12, 1646. [Google Scholar] [CrossRef]
- Lewis Luján, L.M.; McCarty, M.F.; Di Nicolantonio, J.J.; Gálvez Ruiz, J.C.; Rosas-Burgos, E.C.; Plascencia-Jatomea, M.; Iloki Assanga, S.B. Nutraceuticals/Drugs Promoting Mitophagy and Mitochondrial Biogenesis May Combat the Mitochondrial Dysfunction Driving Progression of Dry Age-Related Macular Degeneration. Nutrients 2022, 14, 1985. [Google Scholar] [CrossRef] [PubMed]
- Chodari, L.; Dilsiz Aytemir, M.; Vahedi, P.; Alipour, M.; Vahed, S.Z.; Khatibi, S.M.H.; Ahmadian, E.; Ardalan, M.; Eftekhari, A. Targeting Mitochondrial Biogenesis with Polyphenol Compounds. Oxidative Medicine and Cellular Longevity 2021, 2021, e4946711. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Galilea, M.; Pérez-Matute, P.; Prieto-Hontoria, P.L.; Houssier, M.; Burrell, M.A.; Langin, D.; Martínez, J.A.; Moreno-Aliaga, M.J. α-Lipoic Acid Treatment Increases Mitochondrial Biogenesis and Promotes Beige Adipose Features in Subcutaneous Adipocytes from Overweight/Obese Subjects. Biochim Biophys Acta 2015, 1851, 273–281. [Google Scholar] [CrossRef]
- Shen, W.; Hao, J.; Feng, Z.; Tian, C.; Chen, W.; Packer, L.; Shi, X.; Zang, W.; Liu, J. Lipoamide or Lipoic Acid Stimulates Mitochondrial Biogenesis in 3T3-L1 Adipocytes via the Endothelial NO Synthase-CGMP-Protein Kinase G Signalling Pathway: Lipoamide, Lipoic Acid and Mitochondrial Biogenesis. British Journal of Pharmacology 2011, 162, 1213–1224. [Google Scholar] [CrossRef]
- Shen, W.; Liu, K.; Tian, C.; Yang, L.; Li, X.; Ren, J.; Packer, L.; Cotman, C.W.; Liu, J. R-Alpha-Lipoic Acid and Acetyl-L-Carnitine Complementarily Promote Mitochondrial Biogenesis in Murine 3T3-L1 Adipocytes. Diabetologia 2008, 51, 165–174. [Google Scholar] [CrossRef]
- Nicassio, L.; Fracasso, F.; Sirago, G.; Musicco, C.; Picca, A.; Marzetti, E.; Calvani, R.; Cantatore, P.; Gadaleta, M.N.; Pesce, V. Dietary Supplementation with Acetyl-l-Carnitine Counteracts Age-Related Alterations of Mitochondrial Biogenesis, Dynamics and Antioxidant Defenses in Brain of Old Rats. Exp Gerontol 2017, 98, 99–109. [Google Scholar] [CrossRef]
- Pesce, V.; Nicassio, L.; Fracasso, F.; Musicco, C.; Cantatore, P.; Gadaleta, M.N. Acetyl-L-Carnitine Activates the Peroxisome Proliferator-Activated Receptor-γ Coactivators PGC-1α/PGC-1β-Dependent Signaling Cascade of Mitochondrial Biogenesis and Decreases the Oxidized Peroxiredoxins Content in Old Rat Liver. Rejuvenation Res 2012, 15, 136–139. [Google Scholar] [CrossRef]
- Pesce, V.; Fracasso, F.; Cassano, P.; Lezza, A.M.S.; Cantatore, P.; Gadaleta, M.N. Acetyl-L-Carnitine Supplementation to Old Rats Partially Reverts the Age-Related Mitochondrial Decay of Soleus Muscle by Activating Peroxisome Proliferator-Activated Receptor Gamma Coactivator-1alpha-Dependent Mitochondrial Biogenesis. Rejuvenation Res 2010, 13, 148–151. [Google Scholar] [CrossRef] [PubMed]
- Hao, J.; Shen, W.; Yu, G.; Jia, H.; Li, X.; Feng, Z.; Wang, Y.; Weber, P.; Wertz, K.; Sharman, E.; et al. Hydroxytyrosol Promotes Mitochondrial Biogenesis and Mitochondrial Function in 3T3-L1 Adipocytes. The Journal of Nutritional Biochemistry 2010, 21, 634–644. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.; Chen, D.; Xie, Q.; Yang, Y.; Shen, W. Nebivolol Stimulates Mitochondrial Biogenesis in 3T3-L1 Adipocytes. Biochem Biophys Res Commun 2013, 438, 211–217. [Google Scholar] [CrossRef]
- Valenti, D.; De Rasmo, D.; Signorile, A.; Rossi, L.; de Bari, L.; Scala, I.; Granese, B.; Papa, S.; Vacca, R.A. Epigallocatechin-3-Gallate Prevents Oxidative Phosphorylation Deficit and Promotes Mitochondrial Biogenesis in Human Cells from Subjects with Down’s Syndrome. Biochimica et Biophysica Acta (BBA) - Molecular Basis of Disease 2013, 1832, 542–552. [Google Scholar] [CrossRef]
- Lee, M.-S.; Shin, Y.; Jung, S.; Kim, Y. Effects of Epigallocatechin-3-Gallate on Thermogenesis and Mitochondrial Biogenesis in Brown Adipose Tissues of Diet-Induced Obese Mice. Food & Nutrition Research 2017.
- Ha, T.; Kim, M.K.; Park, K.; Jung, W.; Choo, H.; Chong, Y. Structural Modification of (−)-Epigallocatechin Gallate (EGCG) Shows Significant Enhancement in Mitochondrial Biogenesis. J. Agric. Food Chem. 2018, 66, 3850–3859. [Google Scholar] [CrossRef]
- Rehman, H.; Krishnasamy, Y.; Haque, K.; Thurman, R.G.; Lemasters, J.J.; Schnellmann, R.G.; Zhong, Z. Green Tea Polyphenols Stimulate Mitochondrial Biogenesis and Improve Renal Function after Chronic Cyclosporin A Treatment in Rats. PLOS ONE 2013, 8, e65029. [Google Scholar] [CrossRef]
- Rasbach, K.A.; Schnellmann, R.G. Isoflavones Promote Mitochondrial Biogenesis. J Pharmacol Exp Ther 2008, 325, 536–543. [Google Scholar] [CrossRef]
- Henagan, T.M.; Cefalu, W.T.; Ribnicky, D.M.; Noland, R.C.; Dunville, K.; Campbell, W.W.; Stewart, L.K.; Forney, L.A.; Gettys, T.W.; Chang, J.S.; et al. In Vivo Effects of Dietary Quercetin and Quercetin-Rich Red Onion Extract on Skeletal Muscle Mitochondria, Metabolism, and Insulin Sensitivity. Genes Nutr 2014, 10, 2. [Google Scholar] [CrossRef] [PubMed]
- You, Y.; Liang, C.; Han, X.; Guo, J.; Ren, C.; Liu, G.; Huang, W.; Zhan, J. Mulberry Anthocyanins, Cyanidin 3-Glucoside and Cyanidin 3-Rutinoside, Increase the Quantity of Mitochondria during Brown Adipogenesis. Journal of Functional Foods 2017, 36, 348–356. [Google Scholar] [CrossRef]
- You, Y.; Yuan, X.; Lee, H.J.; Huang, W.; Jin, W.; Zhan, J. Mulberry and Mulberry Wine Extract Increase the Number of Mitochondria during Brown Adipogenesis. Food Funct. 2015, 6, 401–408. [Google Scholar] [CrossRef]
- Gomes, J.V.P.; Rigolon, T.C.B.; Souza, M.S. da S.; Alvarez-Leite, J.I.; Lucia, C.M.D.; Martino, H.S.D.; Rosa, C. de O.B. Antiobesity Effects of Anthocyanins on Mitochondrial Biogenesis, Inflammation, and Oxidative Stress: A Systematic Review. Nutrition 2019, 66, 192–202. [Google Scholar] [CrossRef] [PubMed]
- Su, K.-Y.; Yu, C.Y.; Chen, Y.-W.; Huang, Y.-T.; Chen, C.-T.; Wu, H.-F.; Chen, Y.-L.S. Rutin, a Flavonoid and Principal Component of Saussurea Involucrata, Attenuates Physical Fatigue in a Forced Swimming Mouse Model. International Journal of Medical Sciences 2014, 11, 528–537. [Google Scholar] [CrossRef] [PubMed]
- Hamidie, R.D.R.; Yamada, T.; Ishizawa, R.; Saito, Y.; Masuda, K. Curcumin Treatment Enhances the Effect of Exercise on Mitochondrial Biogenesis in Skeletal Muscle by Increasing CAMP Levels. Metabolism - Clinical and Experimental 2015, 64, 1334–1347. [Google Scholar] [CrossRef] [PubMed]
- Rashedinia, M.; Saberzadeh, J.; Khosravi Bakhtiari, T.; Hozhabri, S.; Arabsolghar, R. Glycyrrhizic Acid Ameliorates Mitochondrial Function and Biogenesis Against Aluminum Toxicity in PC12 Cells. Neurotox Res 2019, 35, 584–593. [Google Scholar] [CrossRef] [PubMed]
- Mogalli, R.; Matsukawa, T.; Shimomura, O.; Isoda, H.; Ohkohchi, N. Cyanidin-3-Glucoside Enhances Mitochondrial Function and Biogenesis in a Human Hepatocyte Cell Line. Cytotechnology 2018, 70, 1519–1528. [Google Scholar] [CrossRef]
- Kou, G.; Li, Z.; Wu, C.; Liu, Y.; Hu, Y.; Guo, L.; Xu, X.; Zhou, Z. Citrus Tangeretin Improves Skeletal Muscle Mitochondrial Biogenesis via Activating the AMPK-PGC1-α Pathway In Vitro and In Vivo: A Possible Mechanism for Its Beneficial Effect on Physical Performance. J. Agric. Food Chem. 2018, 66, 11917–11925. [Google Scholar] [CrossRef]
- Lee, M.-S.; Kim, Y. Effects of Isorhamnetin on Adipocyte Mitochondrial Biogenesis and AMPK Activation. Molecules 2018, 23, 1853. [Google Scholar] [CrossRef]
- Dusabimana, T.; Kim, S.R.; Kim, H.J.; Park, S.W.; Kim, H. Nobiletin Ameliorates Hepatic Ischemia and Reperfusion Injury through the Activation of SIRT-1/FOXO3a-Mediated Autophagy and Mitochondrial Biogenesis. Exp Mol Med 2019, 51, 1–16. [Google Scholar] [CrossRef]
- Hiramitsu, M.; Shimada, Y.; Kuroyanagi, J.; Inoue, T.; Katagiri, T.; Zang, L.; Nishimura, Y.; Nishimura, N.; Tanaka, T. Eriocitrin Ameliorates Diet-Induced Hepatic Steatosis with Activation of Mitochondrial Biogenesis. Sci Rep 2014, 4, 3708. [Google Scholar] [CrossRef]
- Tsutsumi, R.; Yoshida, T.; Nii, Y.; Okahisa, N.; Iwata, S.; Tsukayama, M.; Hashimoto, R.; Taniguchi, Y.; Sakaue, H.; Hosaka, T.; et al. Sudachitin, a Polymethoxylated Flavone, Improves Glucose and Lipid Metabolism by Increasing Mitochondrial Biogenesis in Skeletal Muscle. Nutrition & Metabolism 2014, 11, 32. [Google Scholar] [CrossRef]
- Yamamoto, H.; Morino, K.; Mengistu, L.; Ishibashi, T.; Kiriyama, K.; Ikami, T.; Maegawa, H. Amla Enhances Mitochondrial Spare Respiratory Capacity by Increasing Mitochondrial Biogenesis and Antioxidant Systems in a Murine Skeletal Muscle Cell Line. Oxidative Medicine and Cellular Longevity 2016, 2016, e1735841. [Google Scholar] [CrossRef]
- Kim, H.-L.; Park, J.; Park, H.; Jung, Y.; Youn, D.-H.; Kang, J.; Jeong, M.-Y.; Um, J.-Y. Platycodon Grandiflorum A. De Candolle Ethanolic Extract Inhibits Adipogenic Regulators in 3T3-L1 Cells and Induces Mitochondrial Biogenesis in Primary Brown Preadipocytes. J. Agric. Food Chem. 2015, 63, 7721–7730. [Google Scholar] [CrossRef] [PubMed]
- Ajaz, S.; McPhail, M.J.; Singh, K.K.; Mujib, S.; Trovato, F.M.; Napoli, S.; Agarwal, K. Mitochondrial Metabolic Manipulation by SARS-CoV-2 in Peripheral Blood Mononuclear Cells of Patients with COVID-19. American Journal of Physiology-Cell Physiology 2021, 320, C57–C65. [Google Scholar] [CrossRef] [PubMed]
- Abramczyk, H.; Brozek-Pluska, B.; Beton, K. Decoding COVID-19 MRNA Vaccine Immunometabolism in Central Nervous System: Human Brain Normal Glial and Glioma Cells by Raman Imaging 2022, 2022.03.02.482639.
- Nunn, A.V.W.; Guy, G.W.; Brysch, W.; Bell, J.D. Understanding Long COVID; Mitochondrial Health and Adaptation—Old Pathways, New Problems. Biomedicines 2022, 10, 3113. [Google Scholar] [CrossRef]
- Díaz-Resendiz, K.J.G.; Benitez-Trinidad, A.B.; Covantes-Rosales, C.E.; Toledo-Ibarra, G.A.; Ortiz-Lazareno, P.C.; Girón-Pérez, D.A.; Bueno-Durán, A.Y.; Pérez-Díaz, D.A.; Barcelos-García, R.G.; Girón-Pérez, M.I. Loss of Mitochondrial Membrane Potential (ΔΨm) in Leucocytes as Post-COVID-19 Sequelae. Journal of Leukocyte Biology 2022, 112, 23–29. [Google Scholar] [CrossRef]
- Guntur, V.P.; Nemkov, T.; de Boer, E.; Mohning, M.P.; Baraghoshi, D.; Cendali, F.I.; San-Millán, I.; Petrache, I.; D’Alessandro, A. Signatures of Mitochondrial Dysfunction and Impaired Fatty Acid Metabolism in Plasma of Patients with Post-Acute Sequelae of COVID-19 (PASC). Metabolites 2022, 12, 1026. [Google Scholar] [CrossRef]
- Prasada Kabekkodu, S.; Chakrabarty, S.; Jayaram, P.; Mallya, S.; Thangaraj, K.; Singh, K.K.; Satyamoorthy, K. Severe Acute Respiratory Syndrome Coronaviruses Contributing to Mitochondrial Dysfunction: Implications for Post-COVID Complications. Mitochondrion 2023, 69, 43–56. [Google Scholar] [CrossRef]
- Mikirova, N.; Casciari, J.; Rogers, A.; Taylor, P. Effect of High-Dose Intravenous Vitamin C on Inflammation in Cancer Patients. Journal of Translational Medicine 2012, 10, 189. [Google Scholar] [CrossRef]
- Kc, S.; Càrcamo, J.M.; Golde, D.W. Vitamin C Enters Mitochondria via Facilitative Glucose Transporter 1 (Gluti) and Confers Mitochondrial Protection against Oxidative Injury. The FASEB Journal 2005, 19, 1657–1667. [Google Scholar] [CrossRef]
- Carr, A.C.; Maggini, S. Vitamin C and Immune Function. Nutrients 2017, 9, 1211. [Google Scholar] [CrossRef]
- Vineetha, R.C.; Mathews, V.V.; Nair, R.H. Chapter 28 - Ascorbic Acid and the Mitochondria. In Mitochondrial Physiology and Vegetal Molecules; de Oliveira, M.R., Ed.; Academic Press, 2021; pp. 613–624 ISBN 978-0-12-821562-3.
- Otten, A.T.; Bourgonje, A.R.; Peters, V.; Alizadeh, B.Z.; Dijkstra, G.; Harmsen, H.J.M. Vitamin C Supplementation in Healthy Individuals Leads to Shifts of Bacterial Populations in the Gut-A Pilot Study. Antioxidants (Basel) 2021, 10, 1278. [Google Scholar] [CrossRef] [PubMed]
- Giannos, P.; Prokopidis, K. Gut Dysbiosis and Long COVID-19: Feeling Gutted. J Med Virol 2022, 94, 2917–2918. [Google Scholar] [CrossRef] [PubMed]
- Ancona, G.; Alagna, L.; Alteri, C.; Palomba, E.; Tonizzo, A.; Pastena, A.; Muscatello, A.; Gori, A.; Bandera, A. Gut and Airway Microbiota Dysbiosis and Their Role in COVID-19 and Long-COVID. Frontiers in Immunology 2023, 14. [Google Scholar] [CrossRef]
- Vollbracht, C.; Kraft, K. Feasibility of Vitamin C in the Treatment of Post Viral Fatigue with Focus on Long COVID, Based on a Systematic Review of IV Vitamin C on Fatigue. Nutrients 2021, 13, 1154. [Google Scholar] [CrossRef]
- Izzo, R.; Trimarco, V.; Mone, P.; Aloè, T.; Capra Marzani, M.; Diana, A.; Fazio, G.; Mallardo, M.; Maniscalco, M.; Marazzi, G.; et al. Combining L-Arginine with Vitamin C Improves Long-COVID Symptoms: The LINCOLN Survey. Pharmacol Res 2022, 183, 106360. [Google Scholar] [CrossRef]
- Tosato, M.; Calvani, R.; Picca, A.; Ciciarello, F.; Galluzzo, V.; Coelho-Júnior, H.J.; Di Giorgio, A.; Di Mario, C.; Gervasoni, J.; Gremese, E.; et al. Effects of L-Arginine Plus Vitamin C Supplementation on Physical Performance, Endothelial Function, and Persistent Fatigue in Adults with Long COVID: A Single-Blind Randomized Controlled Trial. Nutrients 2022, 14, 4984. [Google Scholar] [CrossRef]
- Rushworth, G.F.; Megson, I.L. Existing and Potential Therapeutic Uses for N-Acetylcysteine: The Need for Conversion to Intracellular Glutathione for Antioxidant Benefits. Pharmacology & Therapeutics 2014, 141, 150–159. [Google Scholar] [CrossRef]
- Cnubben, N.H.P.; Rietjens, I.M.C.M.; Wortelboer, H.; van Zanden, J.; van Bladeren, P.J. The Interplay of Glutathione-Related Processes in Antioxidant Defense. Environmental Toxicology and Pharmacology 2001, 10, 141–152. [Google Scholar] [CrossRef] [PubMed]
- Tenório, M.C. dos S.; Graciliano, N.G.; Moura, F.A.; Oliveira, A.C.M. de; Goulart, M.O.F. N-Acetylcysteine (NAC): Impacts on Human Health. Antioxidants 2021, 10, 967. [Google Scholar] [CrossRef] [PubMed]
- Atkuri, K.R.; Mantovani, J.J.; Herzenberg, L.A.; Herzenberg, L.A. N-Acetylcysteine—a Safe Antidote for Cysteine/Glutathione Deficiency. Current Opinion in Pharmacology 2007, 7, 355–359. [Google Scholar] [CrossRef]
- Aparicio-Trejo, O.E.; Reyes-Fermín, L.M.; Briones-Herrera, A.; Tapia, E.; León-Contreras, J.C.; Hernández-Pando, R.; Sánchez-Lozada, L.G.; Pedraza-Chaverri, J. Protective Effects of N-Acetyl-Cysteine in Mitochondria Bioenergetics, Oxidative Stress, Dynamics and S-Glutathionylation Alterations in Acute Kidney Damage Induced by Folic Acid. Free Radical Biology and Medicine 2019, 130, 379–396. [Google Scholar] [CrossRef]
- Kumar, P.; Liu, C.; Hsu, J.W.; Chacko, S.; Minard, C.; Jahoor, F.; Sekhar, R.V. Glycine and N-Acetylcysteine (GlyNAC) Supplementation in Older Adults Improves Glutathione Deficiency, Oxidative Stress, Mitochondrial Dysfunction, Inflammation, Insulin Resistance, Endothelial Dysfunction, Genotoxicity, Muscle Strength, and Cognition: Results of a Pilot Clinical Trial. Clinical and Translational Medicine 2021, 11, e372. [Google Scholar] [CrossRef] [PubMed]
- Barbagallo, M.; Veronese, N.; Dominguez, L.J. Magnesium in Aging, Health and Diseases. Nutrients 2021, 13, 463. [Google Scholar] [CrossRef]
- Nouri-Majd, S.; Ebrahimzadeh, A.; Mousavi, S.M.; Zargarzadeh, N.; Eslami, M.; Santos, H.O.; Taghizadeh, M.; Milajerdi, A. Higher Intake of Dietary Magnesium Is Inversely Associated With COVID-19 Severity and Symptoms in Hospitalized Patients: A Cross-Sectional Study. Frontiers in Nutrition 2022, 9. [Google Scholar] [CrossRef]
- Racay, P. Effect of Magnesium on Calcium-Induced Depolarisation of Mitochondrial Transmembrane Potential. Cell Biology International 2008, 32, 136–145. [Google Scholar] [CrossRef]
- Pilchova, I.; Klacanova, K.; Tatarkova, Z.; Kaplan, P.; Racay, P. The Involvement of Mg2+ in Regulation of Cellular and Mitochondrial Functions. Oxidative Medicine and Cellular Longevity 2017, 2017, e6797460. [Google Scholar] [CrossRef]
- Di, Y.; He, Y.-L.; Zhao, T.; Huang, X.; Wu, K.-W.; Liu, S.-H.; Zhao, Y.-Q.; Fan, M.; Wu, L.-Y.; Zhu, L.-L. Methylene Blue Reduces Acute Cerebral Ischemic Injury via the Induction of Mitophagy. Mol Med 2015, 21, 420–429. [Google Scholar] [CrossRef]
- Tucker, D.; Lu, Y.; Zhang, Q. From Mitochondrial Function to Neuroprotection—an Emerging Role for Methylene Blue. Mol Neurobiol 2018, 55, 5137–5153. [Google Scholar] [CrossRef]
- Poteet, E.; Winters, A.; Yan, L.-J.; Shufelt, K.; Green, K.N.; Simpkins, J.W.; Wen, Y.; Yang, S.-H. Neuroprotective Actions of Methylene Blue and Its Derivatives. PLOS ONE 2012, 7, e48279. [Google Scholar] [CrossRef] [PubMed]
- Chuang, S.-T.; Papp, H.; Kuczmog, A.; Eells, R.; Condor Capcha, J.M.; Shehadeh, L.A.; Jakab, F.; Buchwald, P. Methylene Blue Is a Nonspecific Protein–Protein Interaction Inhibitor with Potential for Repurposing as an Antiviral for COVID-19. Pharmaceuticals 2022, 15, 621. [Google Scholar] [CrossRef] [PubMed]
- Kidd, S.A.; Lancaster, P. a. L.; Anderson, J.C.; Boogert, A.; Fisher, C.C.; Robertson, R.; Wass, D.M. Fetal Death After Exposure to Methylene Blue Dye During Mid-Trimester Amniocentesis in Twin Pregnancy. Prenatal Diagnosis 1996, 16, 39–47. [Google Scholar] [CrossRef]
- Gillman, P.K. CNS Toxicity Involving Methylene Blue: The Exemplar for Understanding and Predicting Drug Interactions That Precipitate Serotonin Toxicity. J Psychopharmacol 2011, 25, 429–436. [Google Scholar] [CrossRef] [PubMed]
- Brasche, S.; Bischof, W. Daily Time Spent Indoors in German Homes – Baseline Data for the Assessment of Indoor Exposure of German Occupants. International Journal of Hygiene and Environmental Health 2005, 208, 247–253. [Google Scholar] [CrossRef]
- Dörre, W.H. Time-Activity-Patterns of Some Selected Small Groups as a Basis for Exposure Estimation: A Methodological Study. J Expo Anal Environ Epidemiol 1997, 7, 471–491. [Google Scholar]
- Wang, S.-J.; Chen, M.-Y. The Effects of Sunlight Exposure Therapy on the Improvement of Depression and Quality of Life in Post-Stroke Patients: A RCT Study. Heliyon 2020, 6, e04379. [Google Scholar] [CrossRef]
- Lindqvist, P.G.; Epstein, E.; Nielsen, K.; Landin-Olsson, M.; Ingvar, C.; Olsson, H. Avoidance of Sun Exposure as a Risk Factor for Major Causes of Death: A Competing Risk Analysis of the Melanoma in Southern Sweden Cohort. J Intern Med 2016, 280, 375–387. [Google Scholar] [CrossRef]
- Holick, M.F. Chapter 4 - Photobiology of Vitamin D. In Vitamin D (Fourth Edition); Feldman, D., Ed.; Academic Press, 2018; pp. 45–55 ISBN 978-0-12-809965-0.
- Walski, T.; Dąbrowska, K.; Drohomirecka, A.; Jędruchniewicz, N.; Trochanowska-Pauk, N.; Witkiewicz, W.; Komorowska, M. The Effect of Red-to-near-Infrared (R/NIR) Irradiation on Inflammatory Processes. Int J Radiat Biol 2019, 95, 1326–1336. [Google Scholar] [CrossRef]
- Begum, R.; Calaza, K.; Kam, J.H.; Salt, T.E.; Hogg, C.; Jeffery, G. Near-Infrared Light Increases ATP, Extends Lifespan and Improves Mobility in Aged Drosophila Melanogaster. Biology Letters 2015, 11, 20150073. [Google Scholar] [CrossRef] [PubMed]
- Hobday, R.A.; Cason, J.W. The Open-Air Treatment of PANDEMIC INFLUENZA. Am J Public Health 2009, 99, S236–S242. [Google Scholar] [CrossRef] [PubMed]
- Tsai, S.-R.; Hamblin, M.R. Biological Effects and Medical Applications of Infrared Radiation. J Photochem Photobiol B 2017, 170, 197–207. [Google Scholar] [CrossRef] [PubMed]
- Shamloo, S.; Defensor, E.; Ciari, P.; Ogawa, G.; Vidano, L.; Lin, J.S.; Fortkort, J.A.; Shamloo, M.; Barron, A.E. The Anti-Inflammatory Effects of Photobiomodulation Are Mediated by Cytokines: Evidence from a Mouse Model of Inflammation. Frontiers in Neuroscience 2023, 17. [Google Scholar] [CrossRef]
- Nguyen, L.M.-D.; Malamo, A.G.; Larkin-Kaiser, K.A.; Borsa, P.A.; Adhihetty, P.J. Effect of Near-Infrared Light Exposure on Mitochondrial Signaling in C2C12 Muscle Cells. Mitochondrion 2014, 14, 42–48. [Google Scholar] [CrossRef]
- Díaz-Resendiz, K.J.G.; Covantes-Rosales, C.E.; Benítez-Trinidad, A.B.; Navidad-Murrieta, M.S.; Razura-Carmona, F.F.; Carrillo-Cruz, C.D.; Frias-Delgadillo, E.J.; Pérez-Díaz, D.A.; Díaz-Benavides, M.V.; Zambrano-Soria, M.; et al. Effect of Fucoidan on the Mitochondrial Membrane Potential (ΔΨm) of Leukocytes from Patients with Active COVID-19 and Subjects That Recovered from SARS-CoV-2 Infection. Marine Drugs 2022, 20, 99. [Google Scholar] [CrossRef]
- Vásquez-Reyes, S.; Velázquez-Villegas, L.A.; Vargas-Castillo, A.; Noriega, L.G.; Torres, N.; Tovar, A.R. Dietary Bioactive Compounds as Modulators of Mitochondrial Function. The Journal of Nutritional Biochemistry 2021, 96, 108768. [Google Scholar] [CrossRef]
- Forbes-Hernández, T.Y.; Giampieri, F.; Gasparrini, M.; Mazzoni, L.; Quiles, J.L.; Alvarez-Suarez, J.M.; Battino, M. The Effects of Bioactive Compounds from Plant Foods on Mitochondrial Function: A Focus on Apoptotic Mechanisms. Food and Chemical Toxicology 2014, 68, 154–182. [Google Scholar] [CrossRef]
- Rai, P.K.; Russell, O.M.; Lightowlers, R.N.; Turnbull, D.M. Potential Compounds for the Treatment of Mitochondrial Disease. British Medical Bulletin 2015, 116, 5–18. [Google Scholar] [CrossRef]
- McCreary, M.R.; Schnell, P.M.; Rhoda, D.A. Randomized Double-Blind Placebo-Controlled Proof-of-Concept Trial of Resveratrol for Outpatient Treatment of Mild Coronavirus Disease (COVID-19). Sci Rep 2022, 12, 10978. [Google Scholar] [CrossRef]
- Mittra, I.; Souza, R. de; Bhadade, R.; Madke, T.; Shankpal, P.D.; Joshi, M.; Qayyumi, B.; Bhattacharjee, A.; Gota, V.; Gupta, S.; et al. Resveratrol and Copper for Treatment of Severe COVID-19: An Observational Study (RESCU 002) 2020, 2020.07.21.20151423.
- Vahedian-Azimi, A.; Abbasifard, M.; Rahimi-Bashar, F.; Guest, P.C.; Majeed, M.; Mohammadi, A.; Banach, M.; Jamialahmadi, T.; Sahebkar, A. Effectiveness of Curcumin on Outcomes of Hospitalized COVID-19 Patients: A Systematic Review of Clinical Trials. Nutrients 2022, 14, 256. [Google Scholar] [CrossRef]
- Pawar, K.S.; Mastud, R.N.; Pawar, S.K.; Pawar, S.S.; Bhoite, R.R.; Bhoite, R.R.; Kulkarni, M.V.; Deshpande, A.R. Oral Curcumin With Piperine as Adjuvant Therapy for the Treatment of COVID-19: A Randomized Clinical Trial. Frontiers in Pharmacology 2021, 12. [Google Scholar] [CrossRef] [PubMed]
- Bettuzzi, S.; Gabba, L.; Cataldo, S. Efficacy of a Polyphenolic, Standardized Green Tea Extract for the Treatment of COVID-19 Syndrome: A Proof-of-Principle Study. COVID 2021, 1, 2–12. [Google Scholar] [CrossRef]
- Camell, C.D.; Yousefzadeh, M.J.; Zhu, Y.; Prata, L.G.P.L.; Huggins, M.A.; Pierson, M.; Zhang, L.; O’Kelly, R.D.; Pirtskhalava, T.; Xun, P.; et al. Senolytics Reduce Coronavirus-Related Mortality in Old Mice. Science 2021, 373, eabe4832. [Google Scholar] [CrossRef]
- Hu, Q.; Zhang, Q.-Y.; Peng, C.-F.; Ma, Z.; Han, Y.-L. Efficiency of Nicotinamide-Based Supportive Therapy in Lymphopenia for Patients with Ordinary or Severe COVID-19: A Randomized Controlled Trial. Medicine (Baltimore) 2022, 101, e31138. [Google Scholar] [CrossRef]
- Khalaji, A.; Behnoush, A.H.; Alilou, S.; Rezaee, M.; Peiman, S.; Sahebkar, A. Adjunctive Therapy with Lipid-Lowering Agents in COVID-19: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Lipids Health Dis 2023, 22, 61. [Google Scholar] [CrossRef]
- Lan, S.-H.; Lee, H.-Z.; Chao, C.-M.; Chang, S.-P.; Lu, L.-C.; Lai, C.-C. Efficacy of Melatonin in the Treatment of Patients with COVID-19: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Journal of Medical Virology 2022, 94, 2102–2107. [Google Scholar] [CrossRef]
- Pattnaik, B.R.; Bhatraju, N.; Kashyap, S.; Verma, U.; Madan, K.; Guleria, R.; Agrawal, A.; Mohan, A. Effect of a Nutraceutical Drug in COPD Condition: A Pilot Study of in Vitro, in Vivo and Clinical Trial. European Respiratory Journal 2022, 60. [Google Scholar] [CrossRef]
- Barbara, C.; Clavario, P.; De Marzo, V.; Lotti, R.; Guglielmi, G.; Porcile, A.; Russo, C.; Griffo, R.; Mäkikallio, T.; Hautala, A.J.; et al. Effects of Exercise Rehabilitation in Patients with Long Coronavirus Disease 2019. European Journal of Preventive Cardiology 2022, 29, e258–e260. [Google Scholar] [CrossRef] [PubMed]
- Nopp, S.; Moik, F.; Klok, F.A.; Gattinger, D.; Petrovic, M.; Vonbank, K.; Koczulla, A.R.; Ay, C.; Zwick, R.H. Outpatient Pulmonary Rehabilitation in Patients with Long COVID Improves Exercise Capacity, Functional Status, Dyspnea, Fatigue, and Quality of Life. Respiration 2022, 101, 593–601. [Google Scholar] [CrossRef]
- Romanet, C.; Wormser, J.; Fels, A.; Lucas, P.; Prudat, C.; Sacco, E.; Bruel, C.; Plantefève, G.; Pene, F.; Chatellier, G.; et al. Effectiveness of Exercise Training on the Dyspnoea of Individuals with Long COVID: A Randomised Controlled Multicentre Trial. Annals of Physical and Rehabilitation Medicine 2023, 66, 101765. [Google Scholar] [CrossRef] [PubMed]
- Winchester, S.; John, S.; Jabbar, K.; John, I. Clinical Efficacy of Nitric Oxide Nasal Spray (NONS) for the Treatment of Mild COVID-19 Infection. Journal of Infection 2021, 83, 237–279. [Google Scholar] [CrossRef]
- Zhong, M.; Sun, A.; Xiao, T.; Yao, G.; Sang, L.; Zheng, X.; Zhang, J.; Jin, X.; Xu, L.; Yang, W.; et al. A Randomized, Single-Blind, Group Sequential, Active-Controlled Study to Evaluate the Clinical Efficacy and Safety of α-Lipoic Acid for Critically Ill Patients With Coronavirus Disease 2019 (COVID-19). Frontiers in Medicine 2022, 8. [Google Scholar] [CrossRef] [PubMed]
- Altay, O.; Arif, M.; Li, X.; Yang, H.; Aydın, M.; Alkurt, G.; Kim, W.; Akyol, D.; Zhang, C.; Dinler-Doganay, G.; et al. Combined Metabolic Activators Accelerates Recovery in Mild-to-Moderate COVID-19. Advanced Science 2021, 8, 2101222. [Google Scholar] [CrossRef] [PubMed]
- Li, C.; Ou, R.; Wei, Q.; Shang, H. Carnitine and COVID-19 Susceptibility and Severity: A Mendelian Randomization Study. Frontiers in Nutrition 2021, 8. [Google Scholar] [CrossRef]
- Negro, R.W.D.; Turco, P.; Povero, M. Nebivolol: An Effective Option against Long-Lasting Dyspnoea Following COVID-19 Pneumonia - a Pivotal Double-Blind, Cross-over Controlled Study. Multidisciplinary Respiratory Medicine 2022, 17. [Google Scholar] [CrossRef]
- Cheema, H.A.; Sohail, A.; Fatima, A.; Shahid, A.; Shahzil, M.; Ur Rehman, M.E.; Awan, R.U.; Chinnam, S.; Nashwan, A.J. Quercetin for the Treatment of COVID-19 Patients: A Systematic Review and Meta-Analysis. Reviews in Medical Virology 2023, 33, e2427. [Google Scholar] [CrossRef]
- Gomaa, A.A.; Mohamed, H.S.; Abd-ellatief, R.B.; Gomaa, M.A.; Hammam, D.S. Advancing Combination Treatment with Glycyrrhizin and Boswellic Acids for Hospitalized Patients with Moderate COVID-19 Infection: A Randomized Clinical Trial. Inflammopharmacol 2022, 30, 477–486. [Google Scholar] [CrossRef]
- Banerjee, S.; Baidya, S.K.; Adhikari, N.; Ghosh, B.; Jha, T. Glycyrrhizin as a Promising Kryptonite against SARS-CoV-2: Clinical, Experimental, and Theoretical Evidences. Journal of Molecular Structure 2023, 1275, 134642. [Google Scholar] [CrossRef]
- Gomaa, A.A.; Abdel-Wadood, Y.A.; Gomaa, M.A. Glycyrrhizin and Boswellic Acids, the Golden Nutraceuticals: Multitargeting for Treatment of Mild–Moderate COVID-19 and Prevention of Post-COVID Cognitive Impairment. Inflammopharmacol 2022, 30, 1977–1992. [Google Scholar] [CrossRef]
- Semmarath, W.; Mapoung, S.; Umsumarng, S.; Arjsri, P.; Srisawad, K.; Thippraphan, P.; Yodkeeree, S.; Dejkriengkraikul, P. Cyanidin-3-O-Glucoside and Peonidin-3-O-Glucoside-Rich Fraction of Black Rice Germ and Bran Suppresses Inflammatory Responses from SARS-CoV-2 Spike Glycoprotein S1-Induction In Vitro in A549 Lung Cells and THP-1 Macrophages via Inhibition of the NLRP3 Inflammasome Pathway. Nutrients 2022, 14, 2738. [Google Scholar] [CrossRef]
- Jaimes-Gualdrón, T.; Flórez-Álvarez, L.; Zapata-Cardona, M.I.; Rojano, B.A.; Rugeles, M.T.; Zapata-Builes, W. Corozo (Bactris Guineensis) Fruit Extract Has Antiviral Activity in Vitro against SARS-CoV-2. Functional Foods in Health and Disease 2022, 12, 534–546. [Google Scholar] [CrossRef]
- Dabholkar, N.; Gorantla, S.; Dubey, S.K.; Alexander, A.; Taliyan, R.; Singhvi, G. Repurposing Methylene Blue in the Management of COVID-19: Mechanistic Aspects and Clinical Investigations. Biomedicine & Pharmacotherapy 2021, 142, 112023. [Google Scholar] [CrossRef]
- Hamidi-Alamdari, D.; Hafizi-Lotfabadi, S.; Bagheri-Moghaddam, A.; Safari, H.; Mozdourian, M.; Javidarabshahi, Z.; Peivandi-Yazdi, A.; Ali-Zeraati, A.; Sedaghat, A.; Poursadegh, F.; et al. Methylene Blue for Treatment of Hospitalized COVID-19 Patients: A Randomized, Controlled, Open-Label Clinical Trial, Phase 2. Revista de investigación clínica 2021, 73, 190–198. [Google Scholar] [CrossRef]
- Patidar, V.; Sharma, A.; Bhoraskar, S.; Tripathi, A.P.; Dhaneriya, S. The Role of Nebulized Methylene Blue [NMB] in The Management of COVID-19 Cases: An Observational Study. International Journal of Medical Arts 2022, 4, 2129–2132. [Google Scholar] [CrossRef]
- Alamdari, D.H.; Moghaddam, A.B.; Amini, S.; Keramati, M.R.; Zarmehri, A.M.; Alamdari, A.H.; Damsaz, M.; Banpour, H.; Yarahmadi, A.; Koliakos, G. Application of Methylene Blue -Vitamin C –N-Acetyl Cysteine for Treatment of Critically Ill COVID-19 Patients, Report of a Phase-I Clinical Trial. European Journal of Pharmacology 2020, 885, 173494. [Google Scholar] [CrossRef]
- Mahale, N.; Godavarthy, P.; Marreddy, S.; Gokhale, S.D.; Funde, P.; Rajhans, P.A.; Akole, P.V.; Pawar, B.; Bhurke, B.; Dalvi, P.; et al. Intravenous Methylene Blue as a Rescue Therapy in the Management of Refractory Hypoxia in COVID-19 ARDS Patients: A Case Series. Indian J Crit Care Med 2021, 25, 934–938. [Google Scholar] [CrossRef] [PubMed]
- Yella, S.H.T.; Yella, S.S.T.; Sasanka, K.S.B.S.K.; Thangaraju, P. Does Methylene Blue Satisfy an Option in COVID-19 ARDS. Infectious Disorders - Drug TargetsDisorders) 2022, 22, 62–65. [Google Scholar] [CrossRef] [PubMed]
- Henry, M.; Summa, M.; Patrick, L.; Schwartz, L. A Cohort of Cancer Patients with No Reported Cases of SARS-CoV-2 Infection: The Possible Preventive Role of Methylene Blue. Substantia 2020, 888–888. [Google Scholar] [CrossRef]
- Rawat, D.; Roy, A.; Maitra, S.; Gulati, A.; Khanna, P.; Baidya, D.K. Vitamin C and COVID-19 Treatment: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Diabetes & Metabolic Syndrome: Clinical Research & Reviews 2021, 15, 102324. [Google Scholar] [CrossRef]
- Hemilä, H.; de Man, A.M.E. Vitamin C and COVID-19. Frontiers in Medicine 2021, 7. [Google Scholar] [CrossRef] [PubMed]
- Assimakopoulos, S.F.; Aretha, D.; Komninos, D.; Dimitropoulou, D.; Lagadinou, M.; Leonidou, L.; Oikonomou, I.; Mouzaki, A.; Marangos, M. N-Acetyl-Cysteine Reduces the Risk for Mechanical Ventilation and Mortality in Patients with COVID-19 Pneumonia: A Two-Center Retrospective Cohort Study. Infectious Diseases 2021, 53, 847–854. [Google Scholar] [CrossRef]
- Paraskevas, T.; Kantanis, A.; Karalis, I.; Michailides, C.; Karamouzos, V.; Koniari, I.; Pierrakos, C.; Velissaris, D. N-Acetylcysteine Efficacy in Patients Hospitalized with COVID-19 Pneumonia: A Systematic Review and Meta-Analysis. Romanian Journal of Internal Medicine 2023, 61, 41–52. [Google Scholar] [CrossRef]
- La Carrubba, A.; Veronese, N.; Di Bella, G.; Cusumano, C.; Di Prazza, A.; Ciriminna, S.; Ganci, A.; Naro, L.; Dominguez, L.J.; Barbagallo, M.; et al. Prognostic Value of Magnesium in COVID-19: Findings from the COMEPA Study. Nutrients 2023, 15, 830. [Google Scholar] [CrossRef]
- Segev, A.; Sagir, A.; Matetzky, S.; Segev, A.; Atar, S.; Shechter, M. Admission Serum Magnesium Levels Is Associated with Short and Long-Term Clinical Outcomes in COVID-19 Patients. Nutrients 2023, 15, 2016. [Google Scholar] [CrossRef] [PubMed]
- Pulido Perez, P.; Póndigo de los Angeles, J.A.; Perez Peralta, A.; Ramirez Mojica, E.; Torres Rasgado, E.; Hernandez-Hernandez, M.E.; Romero, J.R. Reduction in Serum Magnesium Levels and Renal Function Are Associated with Increased Mortality in Obese COVID-19 Patients. Nutrients 2022, 14, 4054. [Google Scholar] [CrossRef]
- Díez, J.J.; Iglesias, P.; García, A.; Martín-Casasempere, I.; Bernabéu-Andréu, F.A. Serum Calcium, Magnesium, and Phosphorus Levels in Patients with COVID-19: Relationships with Poor Outcome and Mortality. Horm Metab Res 2023, 55, 31–39. [Google Scholar] [CrossRef] [PubMed]
- Guerrero-Romero, F.; Mercado, M.; Rodriguez-Moran, M.; Ramírez-Renteria, C.; Martínez-Aguilar, G.; Marrero-Rodríguez, D.; Ferreira-Hermosillo, A.; Simental-Mendía, L.E.; Remba-Shapiro, I.; Gamboa-Gómez, C.I.; et al. Magnesium-to-Calcium Ratio and Mortality from COVID-19. Nutrients 2022, 14, 1686. [Google Scholar] [CrossRef]
- Tian, J.; Tang, L.; Liu, X.; Li, Y.; Chen, J.; Huang, W.; Liu, M. Populations in Low-Magnesium Areas Were Associated with Higher Risk of Infection in COVID-19’s Early Transmission: A Nationwide Retrospective Cohort Study in the United States. Nutrients 2022, 14, 909. [Google Scholar] [CrossRef] [PubMed]
- Tan, C.W.; Ho, L.P.; Kalimuddin, S.; Cherng, B.P.Z.; Teh, Y.E.; Thien, S.Y.; Wong, H.M.; Tern, P.J.W.; Chandran, M.; Chay, J.W.M.; et al. Cohort Study to Evaluate the Effect of Vitamin D, Magnesium, and Vitamin B12 in Combination on Progression to Severe Outcomes in Older Patients with Coronavirus (COVID-19). Nutrition 2020, 79–80, 111017. [Google Scholar] [CrossRef] [PubMed]
- Nejatifard, M.; Asefi, S.; Jamali, R.; Hamblin, M.R.; Fekrazad, R. Probable Positive Effects of the Photobiomodulation as an Adjunctive Treatment in COVID-19: A Systematic Review. Cytokine 2021, 137, 155312. [Google Scholar] [CrossRef] [PubMed]
- Vetrici, M.A.; Mokmeli, S.; Bohm, A.R.; Monici, M.; Sigman, S.A. Evaluation of Adjunctive Photobiomodulation (PBMT) for COVID-19 Pneumonia via Clinical Status and Pulmonary Severity Indices in a Preliminary Trial. J Inflamm Res 2021, 14, 965–979. [Google Scholar] [CrossRef] [PubMed]
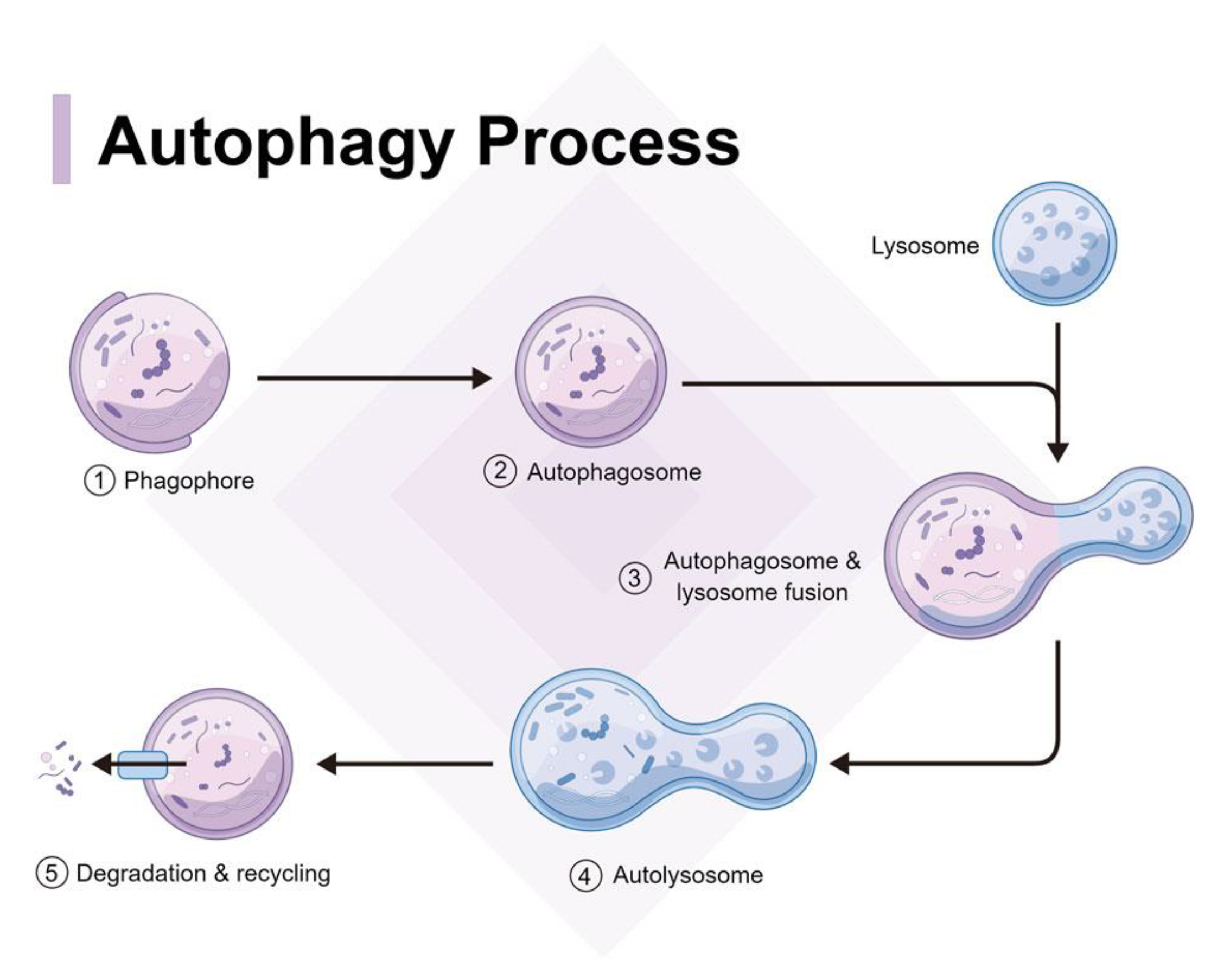
| Spiritual Tradition | World Region | Fasting Rituals |
|---|---|---|
| Islam | Middle East, Africa, Asia, and beyond | Ramadan: Observing a month-long fast from sunrise to sunset as a religious obligation [6]. |
| Christianity | Europe, Americas, Africa, Asia, and beyond | Lent: Fasting for a period of 40 days leading up to Easter, often involving specific dietary restrictions [6]. |
| Buddhism | East Asia, Southeast Asia, South Asia | Uposatha: Observing monthly fasting days to purify the mind and reaffirm spiritual commitments [6]. |
| Hinduism | South Asia, Southeast Asia, Mauritius | Ekadashi: Fasting on the 11th day of each lunar fortnight, abstaining from grains and certain foods [6]. |
| Judaism | Middle East, Europe, Americas, Africa, Asia | Yom Kippur: Observing a 24-hour fast as a day of atonement and repentance [6]. |
| Bahá'í Faith | Global | Nineteen-Day Fast: Fasting from sunrise to sunset during the last month of the Bahá'í calendar [6]. |
| Jainism | India, East Africa | Ayambil: Observing a one-day fast by consuming only boiled water and specific foods. [3] |
| Native American | Americas | Vision Quest: Fasting and solitary retreat to seek spiritual guidance and connection with nature.Sun dance: Fasting and dancing, without water for multiple straight days [4]Plant dietas: Preparation for ceremony [5] |
| Sufism | Middle East, South Asia, North Africa, Europe | Chilla: Engaging in extended periods of fasting and meditation for spiritual growth and purification. [7] |
| Mormonism(Church of Latter Day Saints) | North America | Fasting one day each month [6] |
| Medical Tradition | Region | Fasting Rituals |
| Ayurveda | India, South Asia | Upavasa: Observing occasional fasting as a means to cleanse the body, balance doshas, and support digestion [10]. |
| Traditional Chinese Medicine | China, East Asia | Daoist Fasting: Engaging in intermittent or prolonged fasting to restore harmony and promote vitality [11]. |
| Naturopathy | Europe, Global | Juice Fasting: Consuming only fresh fruit or vegetable juices for a specific duration to support detoxification and rejuvenation [12]. |
| Siddha Medicine | India | Ekadashi Fasting: Observing fasting on specific lunar days to eliminate toxins, promote purification, and enhance energy levels [13]. |
| Western Medicine | Global | Preoperative Fasting: Temporarily refraining from food and drink before surgical procedures to minimize the risk of complications [14]. |
| Greek Medicine | Ancient Greece, Mediterranean | Fasting was used in the treatment of epilepsy [15]. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




