Submitted:
05 May 2023
Posted:
09 May 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
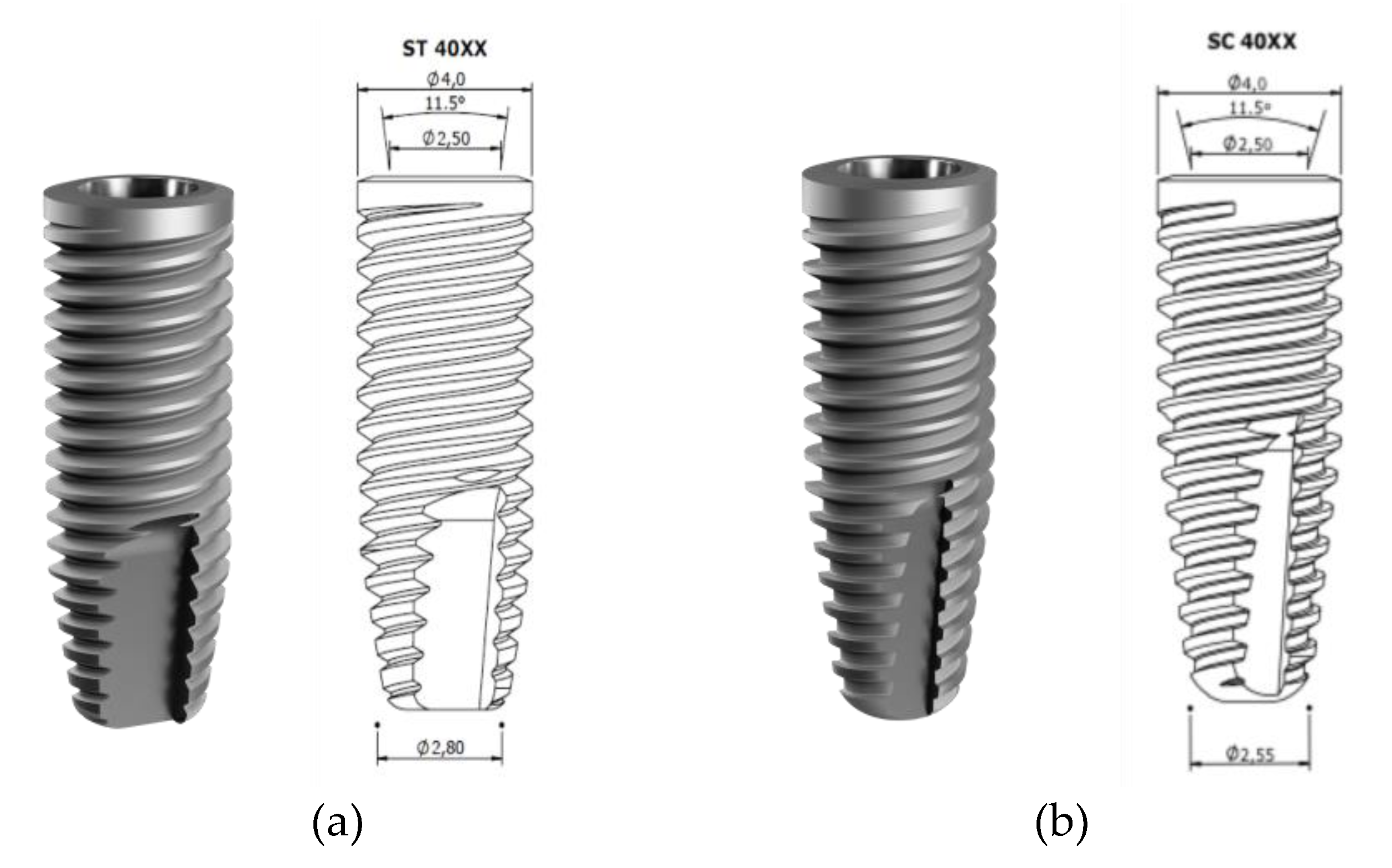
2. Materials and Methods
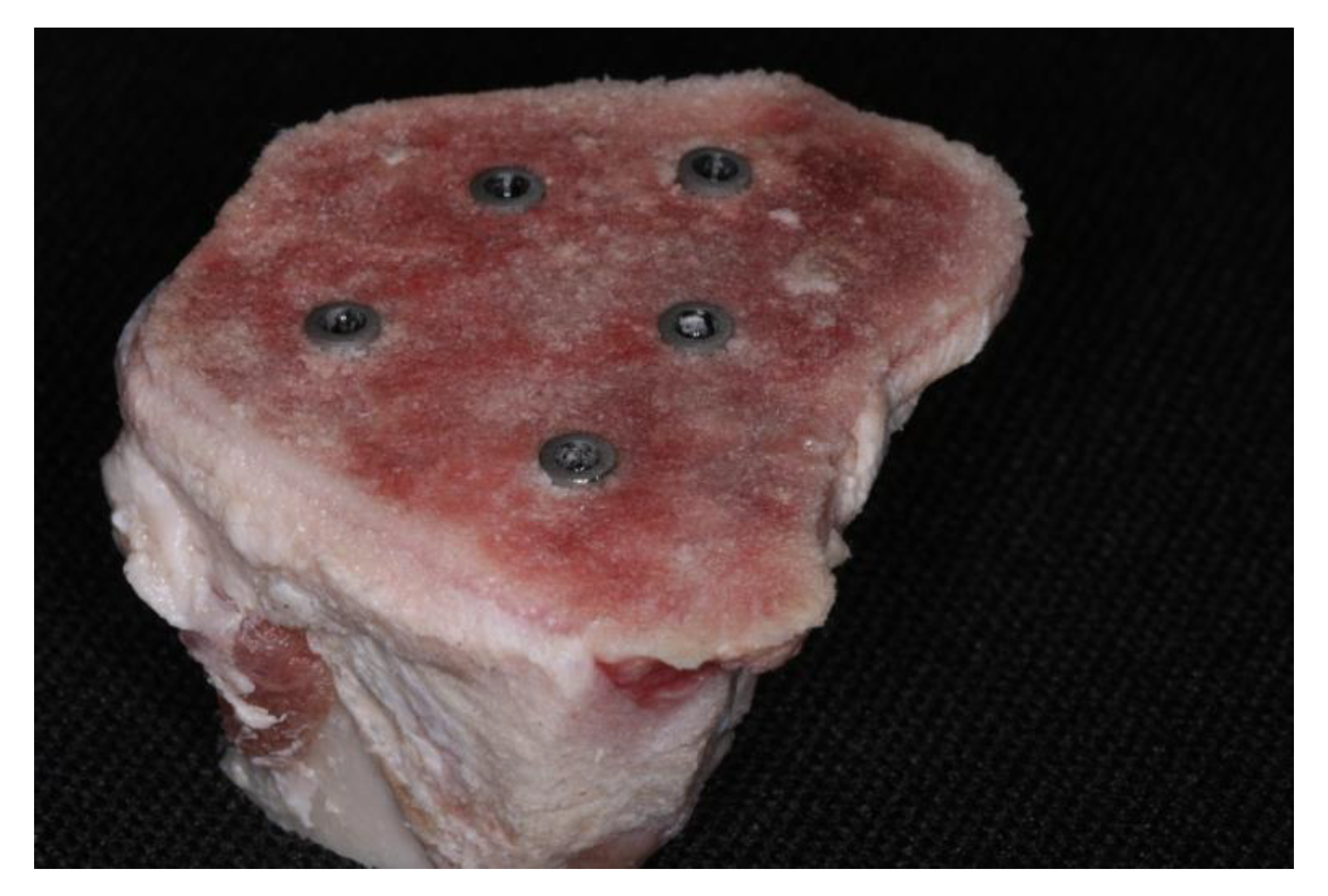
2.1. Sample Preparation
2.2. IT, ISQ, and RT assessment
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Cylindrical Conventional梅Group 1a 梅(sample number) | ISQ ( mean for each implant) | IT (Ncm) | RT (Ncm) |
|---|---|---|---|
| 1 | 49.5 | 20 | 10 |
| 2 | 51.5 | 15 | 10 |
| 3 | 54 | 30 | 20 |
| 4 | 50.5 | 15 | 5 |
| 5 | 46 | 10 | 5 |
| 6 | 49.5 | 20 | 10 |
| 7 | 44 | 10 | 5 |
| 8 | 44.5 | 15 | 5 |
| 9 | 46 | 15 | 5 |
| 10 | 50 | 15 | 10 |
| Cylindrical OD梅Group 1b梅(sample number) | ISQ (mean value for each implant) | IT (Ncm) | RT (Ncm) |
|---|---|---|---|
| 1 | 45.5 | 15 | 10 |
| 2 | 55 | 40 | 40 |
| 3 | 55.5 | 45 | 40 |
| 4 | 50 | 25 | 25 |
| 5 | 51 | 10 | 5 |
| 6 | 50.5 | 30 | 25 |
| 7 | 52 | 30 | 20 |
| 8 | 48.5 | 20 | 15 |
| 9 | 49 | 15 | 10 |
| 10 | 51 | 30 | 25 |
| Conical Conventional梅Group 2a梅(sample number) | ISQ (mean value for each implant) | IT (Ncm) | RT (Ncm) |
|---|---|---|---|
| 1 | 50 | 15 | 10 |
| 2 | 50 | 20 | 15 |
| 3 | 51 | 10 | 5 |
| 4 | 56.5 | 15 | 10 |
| 5 | 55.5 | 30 | 25 |
| 6 | 56 | 30 | 20 |
| 7 | 50.5 | 10 | 5 |
| 8 | 54.5 | 45 | 40 |
| 9 | 54.5 | 40 | 30 |
| 10 | 53 | 30 | 25 |
| Conical OD梅Group 2b梅(sample number) | ISQ (mean value for each implant) | IT (Ncm) | RT (Ncm) |
|---|---|---|---|
| 1 | 53.5 | 20 | 15 |
| 2 | 54.5 | 15 | 10 |
| 3 | 57.5 | 30 | 25 |
| 4 | 52 | 20 | 20 |
| 5 | 54 | 25 | 20 |
| 6 | 54.5 | 30 | 35 |
| 7 | 51.5 | 20 | 15 |
| 8 | 55.5 | 40 | 45 |
| 9 | 58.5 | 45 | 50 |
| 10 | 61.5 | 60 | 65 |
References
- Adell, R.; Lekholm, U.; Rockler, B.; Branemark, P.I. A 15-year study of osseointegrated implants in the treatment of the edentulous jaw. Int. J. Oral Surg. 1981, 10, 387–416. [Google Scholar] [CrossRef] [PubMed]
- Henry, P.J.; Laney, W.R.; Jemt, T.; Harris, D.; Krogh, P.H.; Polizzi, G.; Zarb, G.A.; Herrmann, I. Osseointegrated implants for single-tooth replacement: a prospective 5-year multicenter study. Int. J. Oral Maxillofac. Implants. 1996, 11, 450–455. [Google Scholar] [PubMed]
- Buser, D.; Sennerby, L.; De Bruyn, H. Modern implant dentistry based on osseointegration: 50 years of progress, current trends and open questions. Periodontol 2000. 2017, 73, 7–21. [Google Scholar] [CrossRef] [PubMed]
- Wennerberg, A.; Albrektsson, T. Effects of titanium surface topography on bone integration: a systematic review. Clin. Oral Implant. Res. 2009, 20, 172–184. [Google Scholar] [CrossRef] [PubMed]
- Coelho, P.G.; Jimbo, R.; Tovar, N.; Bonfante, E.A. Osseointegration: hierarchical designing encompassing the macrometer, micrometer, and nanometer length scales. Dent Mater. 2015, 31, 37–52. [Google Scholar] [CrossRef] [PubMed]
- Svanborg, L.M.; Hoffman, M.; Andersson, M.; Currie, F.; Kjellin, P.; Wennerberg, A. The effect of hydroxyapatite nanocrystals on early bone formation surrounding dental implants. Int. J. Oral Maxillofac. Surg. 2011, 40, 308–315. [Google Scholar] [CrossRef] [PubMed]
- Gehrke, S.A.; Aramburú junior, J.; Pérez-Diaz, L.; Treichel, T.L.E.; Dedavid, B.A.; De Aza, P.N.; Prados-Frutos, J.C. New implant macrogeometry to improve and accelerate the osseointegration: an in vivo experimental study. Appl. Sci. 2019, 9, 3181. [Google Scholar] [CrossRef]
- Bonfante, E.A.; Jimbo, R.; Witek, L.; Tovar, N.; Neiva, R.; Torroni, A.; Coelho, P.G. Biomaterial and biomechanical considerations to prevent risks in implant therapy. Periodontol 2000. 2019, 81, 139–151. [Google Scholar] [CrossRef]
- Albrektsson, T.; Brånemark, P.I.; Hansson, H.A.; Lindström, J. Osseointegrated titanium implants. Requirements for ensuring a long-lasting, direct bone-to-implant anchorage in man. Acta Orthop. Scand. 1981, 52, 155–170. [Google Scholar] [CrossRef]
- Stavropoulos, A.; Nyengaard, J.R.; Lang, N.P. ; Karring. T. Immediate loading of single SLA implants: Drilling vs osteotomes for the preparation of the implant site. Clin. Oral Implant. Res 2008, 19, 55–65. [Google Scholar] [CrossRef]
- Coelho, P.G.; Jimbo, R. Osseointegration of metallic devices: Current trends based on implant hardware design. Arch. Biochem. Biophys. 2014, 561, 99–108. [Google Scholar] [CrossRef] [PubMed]
- Javed, F.; Romanos, G.E. The role of primary stability for successful immediate loading of dental implants. A literature review. J. Dent. 2010, 38, 612–620. [Google Scholar] [CrossRef] [PubMed]
- Campos, F.E.; Gomes, J.B.; Marin, C.; Teixeira, H.S.; Suzuki, M.; Witek, L.; Zanetta- Barbosa, D.; Coelho, P.G. Effect of drilling dimension on implant placement torque and early osseointegration stages: an experimental study in dogs. J. Oral Maxillofac. Surg. 2012, 70, e43–50. [Google Scholar] [CrossRef] [PubMed]
- Jimbo, R.; Tovar, N.; Anchieta, R.B.; Machado, L.S.; Marin, C.; Teixeira, H.S.; Coelho, P.G. The combined effects of undersized drilling and implant macrogeometry on bone healing around dental implants: An experimental study. Int. J. Oral Maxillofac. Surg. 2014, 43, 1269–1275. [Google Scholar] [CrossRef] [PubMed]
- Summers, R.B. A new concept in maxillary implant surgery: The osteotome technique. Compendium. 1994, 15, 154–156. [Google Scholar]
- Büchter, A.; Lieinheinz, J.; Wiesmann, H.P.; Kersken, J.; Nienkemper, M.; von Weyhrother, H.; Joos, U.; Meyer, U. Biological and biomechanical evaluation of bone remodeling and implant stability after using an osteotome technique. Clin. Oral Implant. Res. 2005, 16, 1–8. [Google Scholar] [CrossRef]
- Wang, L.; Wu, Y.; Perez, K.C.; Hyman, S.; Brunski, J.B.; Tulu, U.; Bao, C.; Salmon, B.; Helms, J.Á. Effect of condensation on peri-implant bone density and remodeling. J. Dent. Res. 2017, 96, 413–420. [Google Scholar] [CrossRef]
- Huwais, S.; Meyer, E. A novel osseous densification approach in implant osteotomy preparation to increase biomechanical primary stability, bone mineral density, and bone-to-implant contact. Int. J. Oral Maxillofac. Implants. 2017, 32, 27–36. [Google Scholar] [CrossRef]
- Slete, F.B.; Olin, P.; Prasad, H. Histomorphometric comparison of 3 osteotomy techniques. Implant. Dent. 2018, 27, 424–428. [Google Scholar] [CrossRef]
- Lahens, B.; Neiva, R.; Tovar, N.; Alifarag, A.M.; Jimbo, R.; Bonfante, E.A.; Bowers, M.M.; Cuppini, M.; Freitas, H.; Witek, L.; Coelho, P.G. Biomechanical and histologic basis of osseodensification drilling for endosteal implant placement in low density bone. An experimental study in sheep. J. Mech. Behav. Biomed. Mater. 2016, 63, 56–65. [Google Scholar] [CrossRef]
- Trisi, P.; Berardini, M.; Falco, A.; Vulpiani, M.P. New osseodensification implant site preparation method to increase bone density in low-density bone: in vivo evaluation in sheep. Implant. Dent. 2016, 25, 24–31. [Google Scholar] [CrossRef] [PubMed]
- Witek, L.; Neiva, R.; Alifarag, A.; Shahraki, F.; Sayah, G.; Tovar, N.; Lopez, C.D.; Gil, L.; Coelho, P.G. Abscence of healing impairment in osteotomies prepared via osseodensification drilling. Int. J. Periodontics Restorative Dent. 2019, 39, 65–71. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, P.G.F.P.; Bergamo, E.T.P.; Neiva, R.; Bonfante, E.A.; Witek, L.; Tovar, N.; Coelho, P.G. Osseodensification outperforms conventional implant subtractive instrumentation: a study in sheep. Materials Science and Engineering C. 2018, 90, 300–307. [Google Scholar] [CrossRef] [PubMed]
- Koutouzis, T.; Huwais, S.; Hasan, F.; Trahan, W.; Waldrop, T.; Neiva, R. Alveolar ridge expansion by osseodensificaton-mediated plastic deformation and compaction autografting: a multicenter retrospective study. Implant. Dent. 2019, 28, 349–355. [Google Scholar] [CrossRef] [PubMed]
- Huwais, S.; Mazor, Z.; Ioannou, A.L.; Gluckman, H.; Neiva, R. A multicenter retrospective clinical study with up-to-5-year follow-up utilizing a method that enhances bone density and allows for transcrestal sinus augmentation through compacting grafting. Int, J. Oral Maxillofac. Implants. 2018, 33, 1305–1311. [Google Scholar] [CrossRef] [PubMed]
- de Carvalho Formiga, M.; Grzech-Leśniak, K.; Moraschini, V.; Shibli, J.A.; Neiva, R. Effects of osseodensification on immediate implant placement: retrospective analysis of 211 implants. Materials 2022, 15, 3539. [Google Scholar] [CrossRef] [PubMed]
- Stacchi, C.; Troiano, G.; Montaruli, G.; Mozzati, M.; Lamazza, L.; Antonelli, A.; Giudice, A.; Lombardi, T. Changes in implant stability using different site preparation techniques: Osseodensification drills versus piezoelectric surgery. A multi-center prospective randomized controlled clinical trial. Clin. Implant. Dent. Relat. Res 2023, 25, 133–140. [Google Scholar] [CrossRef]
- Misch, C.E. Contemporary Implant Dentistry, 2nd ed.; Mosby: St. Louis MO, USA, 1993. [Google Scholar]
- Cáceres, F.; Troncoso, C.; Silva, R.; Pinto, N. Effects of osseodensification protocol on insertion, removal torques, and resonance frequency analysis of BioHorizons® conical implants. An ex vivo study. J. Oral Biol. Craniofac. Res. 2020, 10, 625–628. [Google Scholar] [CrossRef]
- The jamovi project (2022). jamovi. (Version 2.3) [Computer Software]. Available online: https://www.jamovi.org. (accessed on 25.03.2023).
- R Core Team (2021). R: A Language and environment for statistical computing. (Version 4.1) [Computer software]. Available online: https://cran.r-project.org. (accessed on 25.03.2023).
- Walt, S.; Colbert, S.C.; Varoquaux, G. NumPy: Array computation for Python. 2023, Versão 1.15. NumPy. [Software]. Available online: : https://numpy.org/. (accessed on 25.03.2023).
- Python software foundation. Python Language Site: Documentation, 2020. Página de documentação. Available online: https://www.python.org/doc/. (accessed on 25.03.2023).
- Gandhi, Y.; Padhye, N. Comparison of insertion torque, implant stability quotient and removal torque, in two different implant designs with and without osseodensification. - An ex vivo bench top study. J. Oral Biol. Craniofac. Res. 2023, 13, 249–252. [Google Scholar] [CrossRef]
- Di Stefano, D.A.; Arosio, P.; Perrotti, V.; Iezzi, G.; Scarano, A.; Piattelli, A. Correlation between Implant Geometry, bone density, and the insertion torque/depth integral: a study on bovine ribs. Dent. J. 2019, 7, 25. [Google Scholar] [CrossRef]
- Naves, M.M.; Menezes, H.H.M.; Magalhães, D.; Ferreira, J.A.; Ribeiro, S.F.; de Mello, J.D.; Costa, H.L. Effect of macrogeometry on the surface topography of dental implants. Int. J. Maxillofac. Implants. 2015, 30, 789–799. [Google Scholar] [CrossRef] [PubMed]
- Javed, F.; Ahmed, H.B.; Crespi, R.; Romanos, G.E. Role of primary stability for successful osseointegratation of dental implants: Factors of influence and evaluation. Interv. Med. Appl. Sci. 2013, 5, 162–167. [Google Scholar] [CrossRef] [PubMed]
- Lachmann, S.; Laval, J.Y.; Axmann, D.; Weber, H. Influence of implant geometry on primary insertion stability and simulated peri-implant bone loss: An in vitro study using resonance frequency analysis and damping capacity assessment. Int. J. Oral Maxillofac. Implants. 2011, 26, 347–355. [Google Scholar] [PubMed]
- Elias, C.N.; Rocha, F.A.; Nascimento, A.L.; Coelho, P.G. Influence of implant shape morphology, surgical technique and bone quality on the primary stability of dental implants. J. Mech. Behav. Biomed. Mater. 2012, 16, 169–180. [Google Scholar] [CrossRef] [PubMed]
- Punnoose, K.; Kumar, G.A.B.M.; Govindarajulu, R.V.A.A.E.; Babu, J.S.C.S.; Nayyar, A.S. Osseodensification implant site preparation technique and subsequent implant stability: A pilot study. J. Orthod. Sci. 2022, 11, 50. [Google Scholar] [CrossRef] [PubMed]
- Orth, C.; Haas, A.N.; Peruzzo, D.C.; Carvahlo da Silva, R.; Mesquita de Carvahlo, P.F.; de Barros Carrilho, G.P.; Joly, C.J. Primary stability of dental implants installed using Osseodensification or bone expansion drilling systems: a comparative clinical study. J. Int. Acad. Periodontol. 2022, 24, 165–174. [Google Scholar]
- de Carvalho Formiga, M.; Gehrke, A.F.; De Bortoli, J.P.; Gehrke, S.A. Can the design of the instruments used for undersized osteotomies influence the initial stability of implants installed in low-density bone? An in vitro pilot study. PLoS One. 2021, 16, e0257985. [Google Scholar] [CrossRef]
- Yamaguchi, Y.; Shiota, M.; Munakata, M.; Kasugai, S.; Ozeki, M. Effect of implant design on primary stability using torque-time curves in artificial bone. Int. J. Implant. Dent. 2015, 1, 21. [Google Scholar] [CrossRef]
- Turkylmaz, I.; Aksoy, U.; McGlumphy, E.A. Two alternative surgical techniques for enhancing primary implant stability in the posterior maxilla: a clinical study including bone density, insertion torque, and resonance frequency analysis data. Clin. Implant. Dent. Relat. Res. 2008, 10, 231–237. [Google Scholar] [CrossRef]
- Gehrke, S.A.; Treichel, T.L.E.; Perez-Diaz, L.; Calvo-Guirado, J.L.; Aramburú Júnior, J.; Mazón, P.; de Aza, P.N. Impact of different titanium implant thread designs on bone healing: a biomechanical and histometric study with as animal model. J. Clin. Med. 2019, 8, 777. [Google Scholar] [CrossRef]
- Steigenga, J.; Al-Shammari, K.; Misch, C.; Nociti, F.H.; Wang, H.L. Effects of implant thread geometry on percentage of osseointegration and resistance to reverse torque in the tibia of rabbits. J. Periodontol 2004, 75, 1233–1241. [Google Scholar] [CrossRef] [PubMed]
- Tumedei, M.; Petrini, M.; Pietropaoli, D.; Cipollina, A. The influence of the implant microgeometry on insertion torque, removal torque, and periotest implant primary stability: a mechanical simulation on high-density artificial bone. Symetry. 2021, 13, 776. [Google Scholar] [CrossRef]
- Comuzzi, L.; Tumedei, M.; De Angelis, F.; Lorusso, F.; Piattelli, A.; Iezzi, G. Influence of the dental implant macrogeometry and threads design on primary stability: an in vitro simulation on artificial bone blocks. Comput. Methods. Biomech. Biomed. Engin. 2021, 24, 1242–1250. [Google Scholar] [CrossRef] [PubMed]
- Comuzzi, L.; Tumedei, M.; D'Arcangelo, C.; Piattelli, A.; Iezzi, G. An in vitro analysis on polyurethane foam blocks of the Insertion Torque (IT) values, Removal Torque Values (RTVs), and Resonance Frequency Analysis (RFA) values in tapered and cylindrical Implants. Int. J. Environ. Res. Public Health. 2021, 18, 9238. [Google Scholar] [CrossRef]
- Romeo, D.; Chochlidakis, K.; Barmak, A.B.; Agliardi, E.; Lo Russo, L.; Ercoli, C. Insertion and removal torque of dental implants placed using different drilling protocols: An experimental study on artificial bone substitutes. J. Prosthodont. 2022. [Google Scholar] [CrossRef]
- Frizzera, F.; Spin-Neto, R.; Padilha, V.; Nicchio, N.; Ghiraldini, B.; Bezerra, F.; Marcantonio Jr, E. Effect of osseodensification on the increase in ridge thickness and the prevention of buccal peri-implant defects: an in vitro randomized split mouth pilot study. BMC Oral Health. 2022, 22, 233. [Google Scholar] [CrossRef]
- Bergamo, E.T.P.; Zahoui, A.; Barrera, R.B.; Huwais, S.; Coelho, P.G.; Karateew, E.D.; Bonfante, E.A. Osseodensification effect on implants primary and secondary stability: Multicenter controlled clinical trial. Clin. Implant. Dent. Relat. Res. 2021, 23, 317–328. [Google Scholar] [CrossRef]

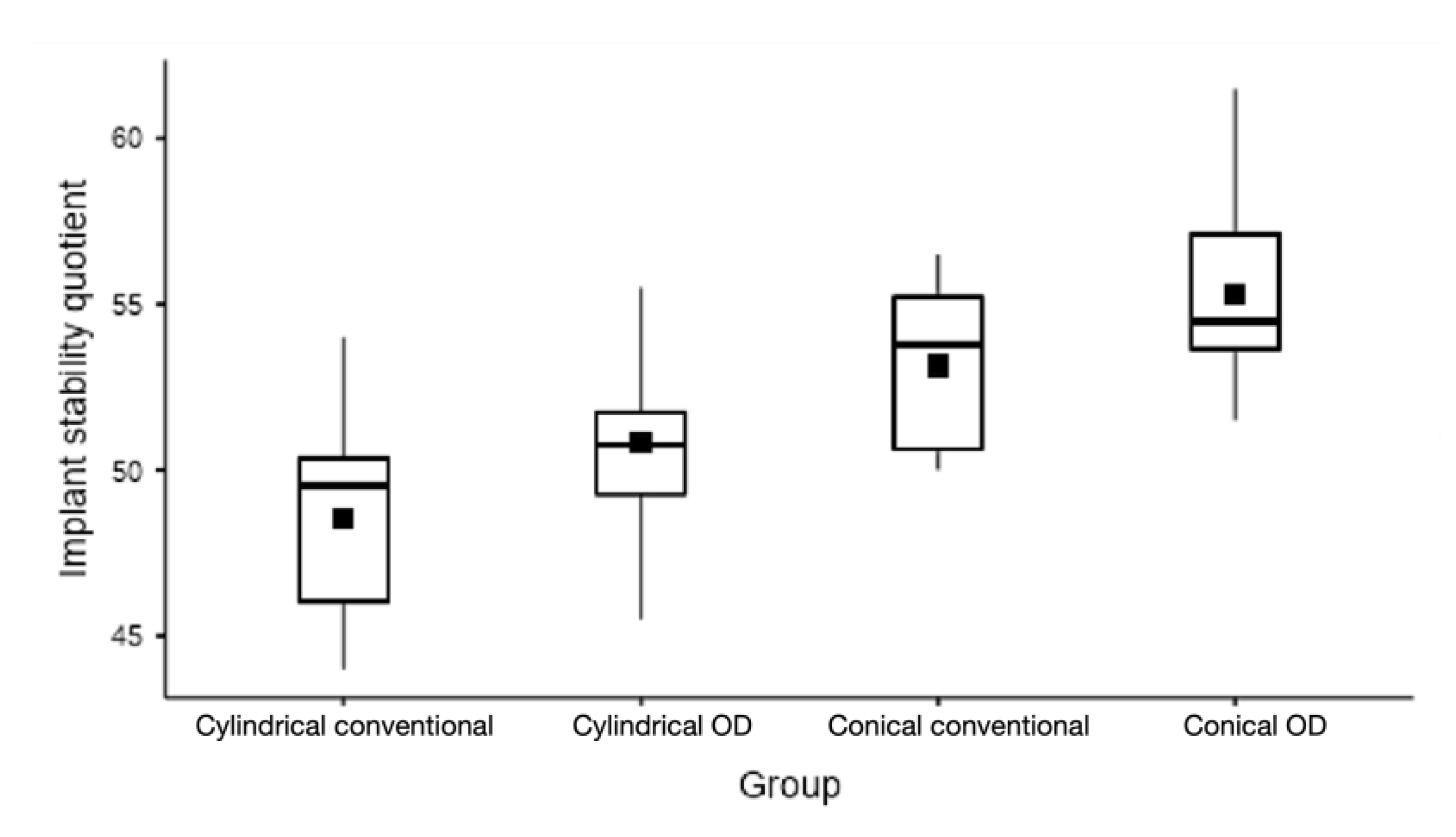
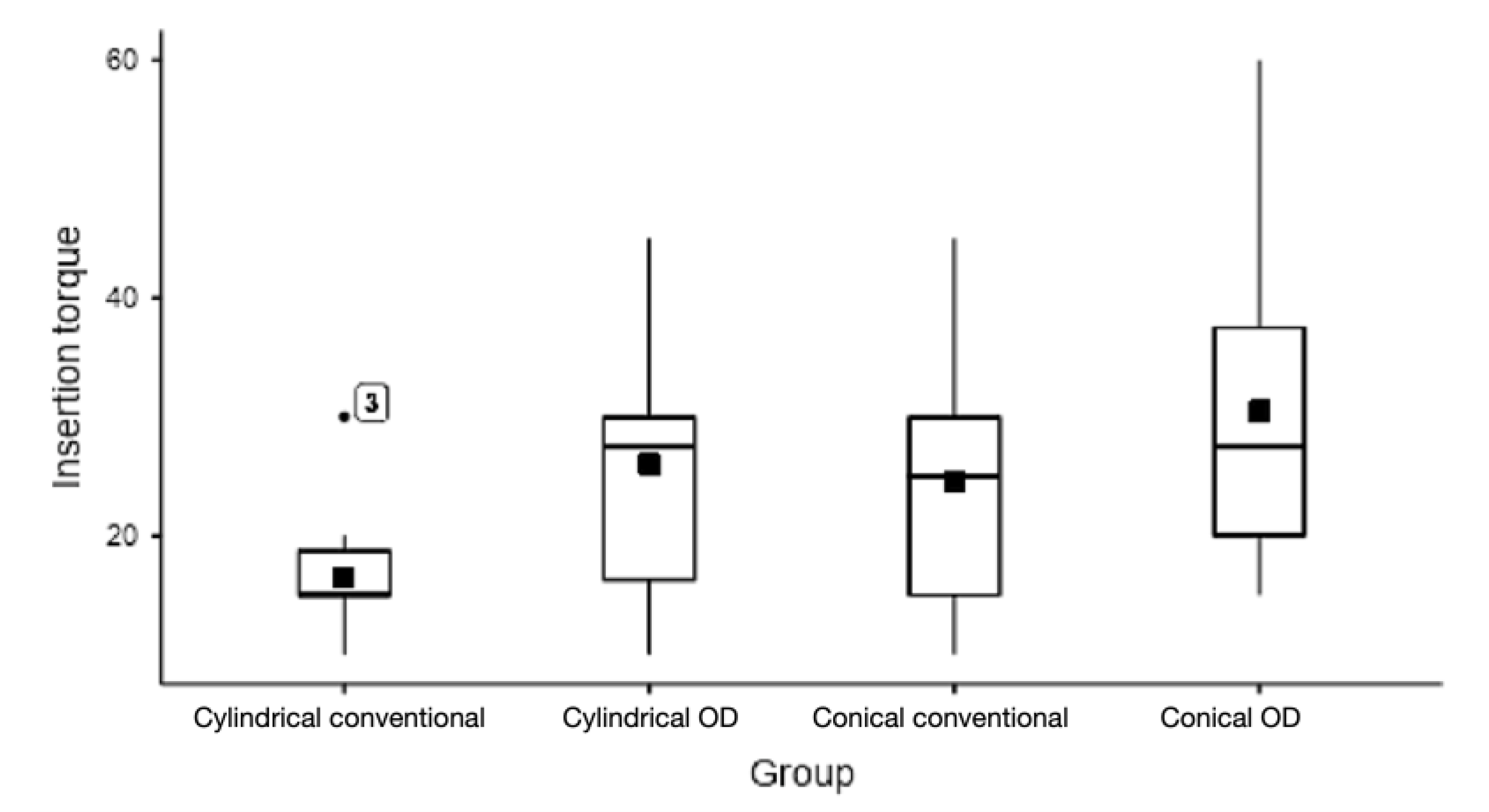
| Parameter | Group | Mean ± SD | Median ± IQR | Minimum | Maximum | ANOVA | |
|---|---|---|---|---|---|---|---|
| P-Value | |||||||
| ISQ | 1a | Cylindrical conventional | 48.6 ± 3.3 | 49.5 ± 4.4 | 44.0 | 54.0 | 0.0001 |
| 1b | Cylindrical OD | 50.8 ± 3.0 | 50.8 ± 2.5 | 45.5 | 55.5 | ||
| 2a | Conical conventional | 53.2 ± 2.6 | 53.8 ± 4.6 | 50.0 | 56.5 | ||
| 2b | Conical OD | 55.3 ± 3.1 | 54.5 ± 3.5 | 51.5 | 61.5 | ||
| IT | 1a | Cylindrical conventional | 16.5 ± 5.8 | 15.0 ± 3.8 | 10.0 | 30.0 | 0.0619 |
| 1b | Cylindrical OD | 26.0 ± 11.3 | 27.5 ± 13.8 | 10.0 | 45.0 | ||
| 2a | Conical conventional | 24.5 ± 12.4 | 25.0 ± 15.0 | 10.0 | 45.0 | ||
| 2b | Conical OD | 30.5 ± 14.0 | 27.5 ± 17.5 | 15.0 | 60.0 | ||
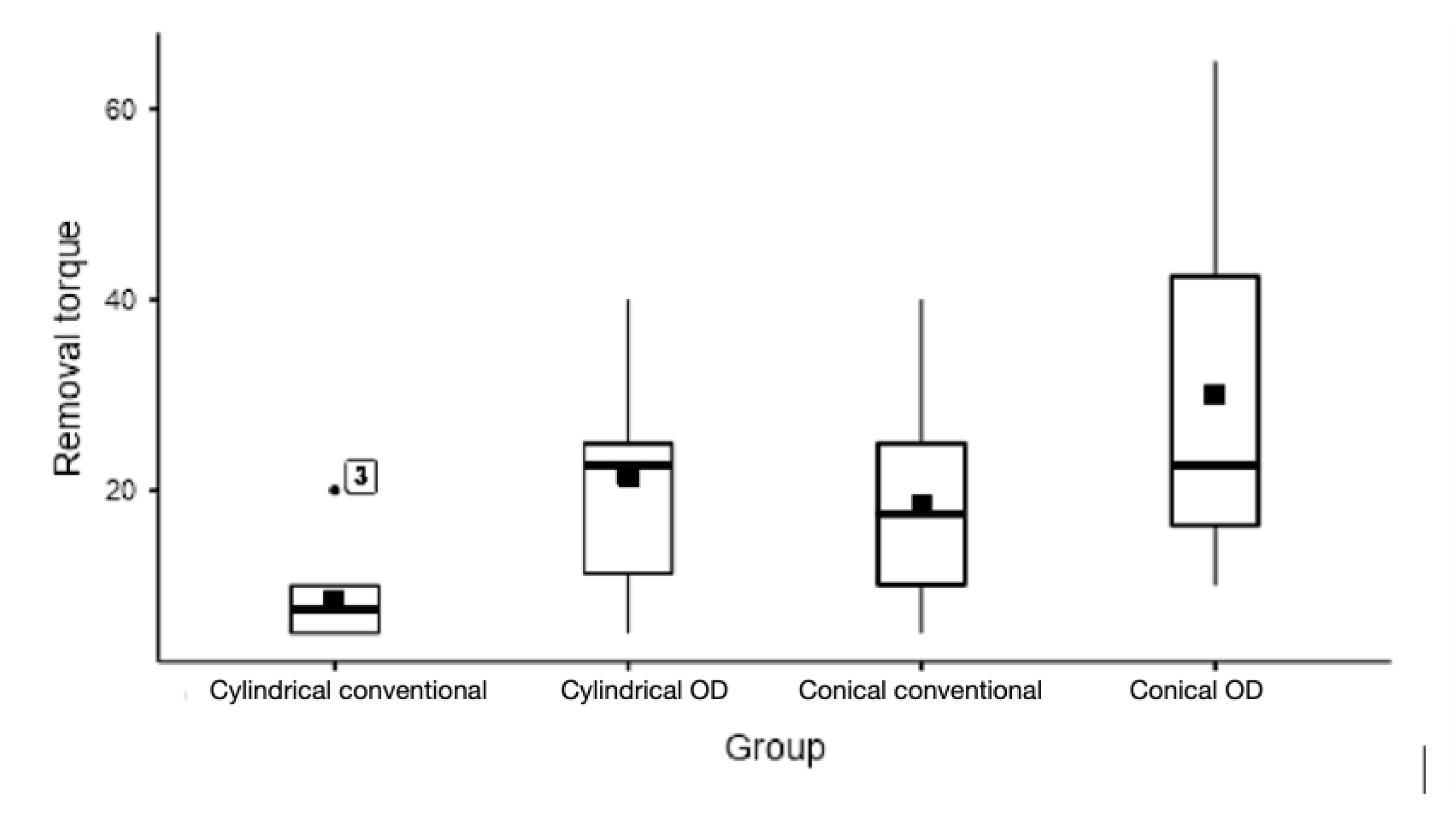
| RT | 1a | Cylindrical conventional | 8.5 ± 4.7 | 7.5 ± 5.0 | 5.0 | 20.0 | 0.0017 |
| 1b | Cylindrical OD | 21.5 ± 12.0 | 22.5 ± 13.8 | 5.0 | 40.0 | ||
| 2a | Conical conventional | 18.5 ± 11.6 | 17.5 ± 15.0 | 5.0 | 40.0 | ||
| 2b | Conical OD | 30.0 ± 18.1 | 22.5 ± 26.3 | 10.0 | 65.0 | ||
| Comparison | ISQ* | IT* | RT** | |||||
|---|---|---|---|---|---|---|---|---|
| Mean Diff. | P_Value | Mean Diff. | P_Value | Mean Diff. | P_Value | |||
| 1a vs 2a | -4.6 | 0.008 | -8.0 | 0.400 | -10.0 | 0.105 | ||
| 1a vs 1b | -2.3 | 0.346 | -9.5 | 0.254 | -13.0 | 0.035 | ||
| 1a vs 2b | -6.8 | 0.000 | -14.0 | 0.062 | -21.5 | 0.019 | ||
| 2a vs 1b | -2.4 | 0.309 | 1.5 | 0.991 | 3.0 | 0.940 | ||
| 2a vs 2b | -2.2 | 0.378 | -6.0 | 0.638 | -11.5 | 0.360 | ||
| 1b vs 2b | -4.5 | 0.009 | -4.5 | 0.809 | -8.5 | 0.614 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





