Introduction
Three large randomized clinical trials named the ATTACC, ACTIV-4a, and REMAP-CAP (Ref 1) were terminated early because the study conclusively found that noncritically ill patients with COVID-19 on therapeutic-dose anticoagulation with heparin had an increased probability of survival as compared with usual-care thromboprophylaxis. The study also showed that major bleeding occurred in 1.9% of the patients receiving therapeutic-dose anticoagulation, and progression to intubation or death occurred in 10.9 % (129 out of 1181 patients) of the therapeutic-dose anticoagulation group. The study projected that for every 1,000 hospitalized patients with moderate disease, an initial strategy of therapeutic-dose anticoagulation, as compared with usual-care thromboprophylaxis (5,000 units SQ q12), would be anticipated to result in the survival of 40 additional patients until hospital discharge without organ support at the expense of 7 additional major bleeding events (Ref 1).
The REMAP-CAP, ACTIV-4a, and ATTACC Investigators also reported that 40.9% (217 patients out of 531) of patients had major thrombotic events or deaths among all of the patients who were treated with therapeutic dose anticoagulation in the intensive care unit. Among these patients, 3.8% (20 patients out of 529) had major bleeding. The phenomenon of increased risks for bleeding, thrombotic events, or death among the patients admitted to critical care units caused nationwide intensivists to be reluctant to include therapeutic anticoagulation in their treatment choice for COVID-19 patients (Ref 2).
Since the rate for major thrombotic events or death among non-critical COVID-19 patients admitted to hospital medical floors was 9.9% (104 patients out of 1046) compared to those admitted to intensive care units of 41.1% (230 patients out of 560), this indicates initiation of anticoagulation in an earlier stage, even if it is lower dose, leads to better survival. The survival rate among non-critically ill patients on usual-care thromboprophylaxis is higher at 91.8% (962 patients out of 1048) compared to 64.5% (364 patients out of 564) in critically-ill patients receiving the same treatment (Ref 1,2).
A prior autopsy study showed significantly increased endothelial injury (endotheliitis), widespread thrombosis with microangiopathy, and alveolar-capillary microthrombi in the lungs of the patients who died from COVID-19 compared to the lungs of individuals who died of influenza or other causes (Ref 3). Another autopsy study of 21 individuals with COVID-19 showed prominent pulmonary emboli (PE) in 19% of cases and microthrombi in the alveolar capillaries in 45% of cases. Interestingly, the primary cause of death in each of the cases was found to be caused by respiratory failure due to exudative diffuse alveolar damage and massive capillary congestion accompanied by microthrombi (Ref 4).
It is possible that an overwhelming burden of microthrombi leads to acute respiratory distress syndrome or death in patients with COVID-19 since anticoagulation does not dissolve the thrombi but rather helps prevent the thrombi from growing larger. In such cases, it is expected to have increasing trends of D-Dimer, along with high oxygen requirements, among patients who are critically ill with COVID-19.
This study tested the hypothesis that increasing trends of D-Dimer are associated with an increase in oxygen requirements among patients with COVID-19. If this hypothesis is found to be true, then D-Dimer can be used to predict COVID-19 patient survival. In such a case, a low or moderate dose anticoagulants should be started at the onset of the COVID-19 diagnosis to reduce the risk of bleeding related to therapeutic anticoagulation and the anticoagulation dose should be adjusted based on D-Dimer trends.
The current retrospective study was designed to test the above hypothesis as well as if administration of intermediate dose anticoagulation could be related to increased survivability compared to the patients who received low or high dose anticoagulation.
Method
Study Population
This study retrospectively evaluated the COVID-19 admission at Jackson Hospital, Alabama, USA from January 1, 2021, to February 15, 2022 for patients who had D-dimer levels in the medical chart. All patient charts were systematically reviewed by two investigators where findings were matched and evaluated for discrepancies that were resolved. The following variables were collected: sex, age, race, BMI, daily D-dimer values, associated oxygenation requirements, anticoagulation dosage, bleeding episodes, vaccination status, and death. Patient age was categorized into three groups: less than 40 years, 40 to 60 years, and greater than 60 years. Then BMI was categorized into three groups: less than 25, 25 to 30, and greater than 30.
D-Dimer
D-dimer was categorized into two different groups to evaluate its association with patient death: less than 2 µg/mL, greater than or equal to 2 µg/mL versus less than 4 µg/mL, and greater than or equal to 4 µg/mL. The normal D-dimer level was less than 0.50 µg/mL. As a part of the chart review, D-dimer values, corresponding oxygen requirements, and hospitalization day were obtained from each patient’s medical record. D-dimer values were used in two separate data analyses. The highest D-dimer levels and corresponding oxygen requirement (L/min) for each patient were used for the first data analysis in this study. The second set of data analysis included all daily D-dimer levels for each patient, corresponding oxygenation requirements, and associated hospitalization day. Subsequently, hospitalization days were categorized into 11 groups which included Day 1 to 2; day 3 to 5; day 6 to 8; day 9 to 11; day 12 to 14; day 15 to 17; day 18 to 20; day 21 to 23; day 24 to 26; day 27 to 29 and more than 30 days. This hospitalization category was used to compute the mean and standard error of D-dimer values and oxygenation requirements related to the hospitalization categories. If variable oxygenation requirements were noted for the corresponding day, the highest level was chosen for the analysis.
Bleeding Episode
Any bleeding episodes that occurred during hospitalization were noted. This information was obtained from the physician’s progress note or if the patient’s anticoagulation was discontinued.
Vaccination
Vaccination against COVID-19 was first released to the public in the United States in December 2020. A patient is defined as vaccinated if received one or two doses of the COVID-19 vaccine. Only one patient received three doses of the vaccine. Unknown vaccination status was noted for 15 patients where no vaccination status was mentioned in the patient chart. Patients were also reluctant to disclose vaccination status, fearing prejudicial treatment for being unvaccinated.
Anticoagulation
Anticoagulation dosage was categorized into three groups: low dose (Enoxaparin 40 mg SubQ daily or 5,000 units Heparin IV three times a day); moderate dose (Enoxaparin 40 mg SubQ twice a day), or high dose (Enoxaparin 1mg/kg SubQ twice a day; 25,000 units Heparin IV drip; all doses of direct oral anticoagulation agents). Daily anticoagulation doses were obtained from the physician’s daily progress notes.
Linear Regression
The dependent variable used in the linear regression model was oxygen requirements. The independent variables were sex, age, race, BMI, daily D-dimer values, associated oxygenation requirements, modalities of anticoagulation dosage, bleeding episodes, and vaccination status. The oxygenation requirement used in the analysis was related to the maximum D-dimer level for any given patient. The backward selection method was used to find the fitted model.
Logistic Regression
The dependent variable used in the logistic regression analysis was patient survival status. The independent variables were sex, age, race, BMI, daily D-dimer values, associated oxygenation requirements, modalities of anticoagulation dosage, bleeding episodes, and vaccination status. All of the variables were entered into the model using the backward elimination method.
Statistical software Stata was used for data analysis.
Ethical Approval
The research related to human use has been complied with all the relevant national regulations, institutional policies, and in accordance with the tenets of the Helsinki Declaration and has been approved by the authors’ institutional review board of Jackson Hospital, Montgomery, Alabama.
Results
The study reviewed 100 COVID-19 patients treated at Jackson Hospital, Alabama (United States) from January 1, 2021, to February 15, 2022.
Table 1 illustrates the demographic characteristics of the 100 patients analyzed in this study. Forty-six percent (46%) patients were male. Among those who died, fifty-nine percent (59%) were male. Among those patients who died (22 out of 100), sixty-eight percent (68%) patients were over the age of 60 years, and twenty-seven percent (27%) patients were between 40 and 60 years. Patients with a high BMI (>30) had a significantly higher death rate of 58%.
Table 2 illustrates the clinical parameters of the 100 patients analyzed in this study. D-dimer was evaluated, and different cut-offs were tested to construct the most effective binary variable for whether D-Dimer was high and the strengh of such a variable as a predictor for death. The binary with a cut-off at 2µg/mL gave a sharper constrast between low and high D-dimer predictive effects. Among those patients who died (22 out of 100), seventy seven percent (77%) died who had a D-dimer ≥ 2 µg/mL and fourteen percent (14%) were vaccinated. Among those patients who had a bleeding episode during hospitalization (13 out of 100), seventy-seven percent (77%) of them died. Among those patients who died, fourteen percent (14%) received moderate dose anticoagulation; fifty percent (50%) received high dose anticoagulation and thirty-six percent (36%) received low-dose anticoagulation.
Table 3 illustrates the linear regression model demonstrating the predictive effect of vaccination status, D-dimer level and bleeding status on oxygen requirements among patients with COVID-19, compared to. These three variables were found to be statistically significant with a value of <0.01 and R square value of the model was 45%. Among the patients who had a D-dimer value ≥ 2 µg/mL, oxygen requirements tended to be 31 L/min higher than those with a D-dimer < 2 µg/mL (p<0.01). Patients who had bleeding episodes during their hospitalization also were predicted to have a statistically higher (p<0.01) oxygen demand of over 41 L/min compared to those who did not bleed.
Table 4 illustrates the logistic regression model demonstrating the predictive effect of D-dimer level and bleeding status on COVID-19 patient survival. This finding indicates that patients with a D-dimer level < 2 are 76% less likely to die compared to patients with maximum D-dimer of ≥ 2. The study also shows that those patients who did not bleed were ninety four percent (94%) less likely to die from COVID-19 compared to those who bled due to a high dose of anticoagulation. The linear regression model also found similar findings, but in the logistic regression model, vaccination status was not found to be significant.
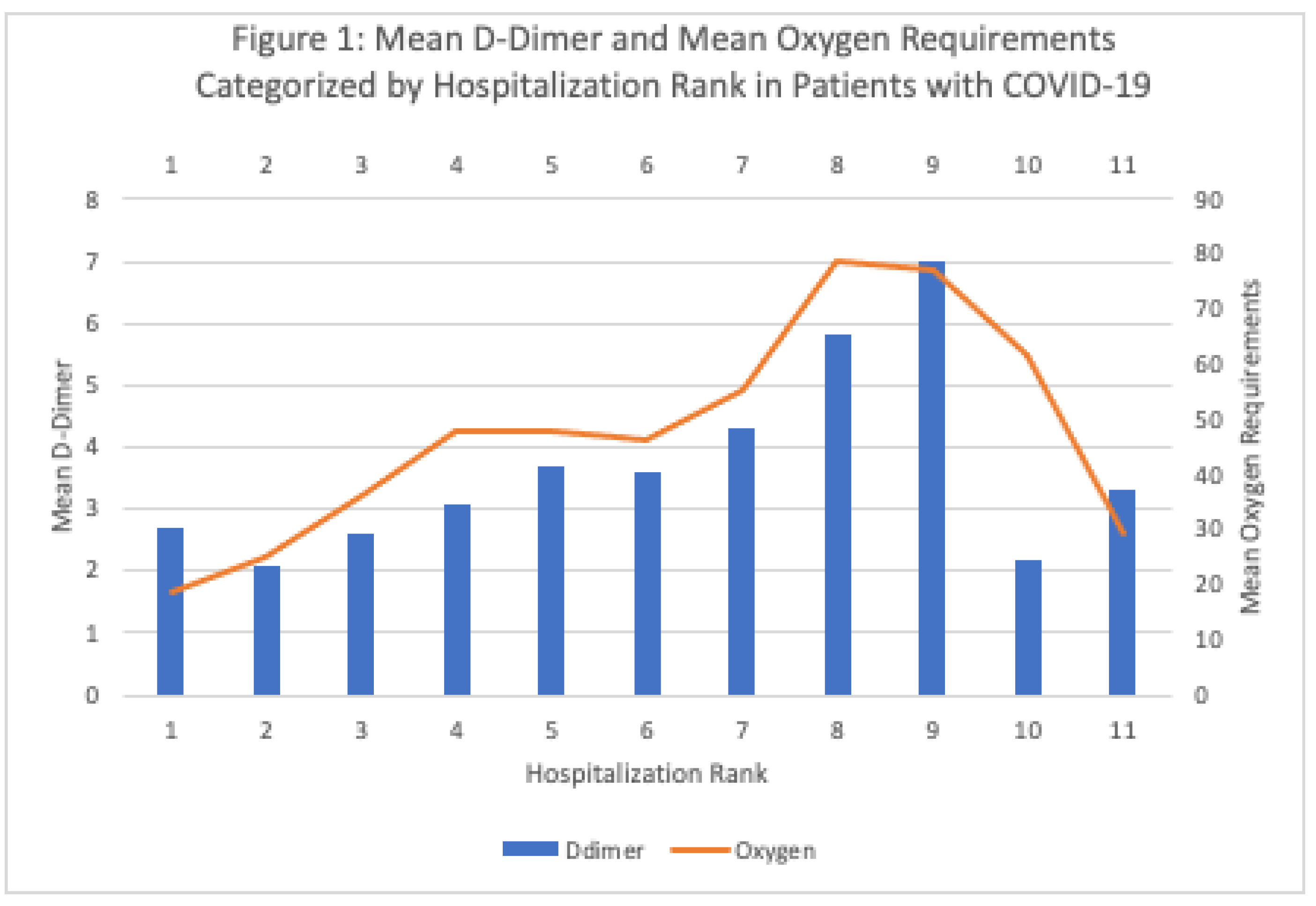
Table 5 illustrates the analysis of the mean D-dimer and corresponding oxygen requirements where D-dimer levels were categorized into eleven hospital days categories (ranks). The D-dimer levels were noted to follow a similar trend in which the values peaked at the maximum point of illness at around day 24 to day 26 and decreased subsequently. The associated oxygen requirements follow the same trend like the D-dimer values during hospitalization. The lowest mean oxygen requirement was during the hospital days 1 and 2 at a value of 18.6 L/min with a corresponding D-dimer mean value of 2.7 μg/mL. The peak mean oxygen requirement was during the hospital days 21 and 23 at a value of 78.9 L/min with a corresponding D-dimer mean value of 5.8 μg/mL. The peak D-dimer level was during hospital days 24 to 26 at a value of 7.0 μg/mL with a corresponding oxygen requirement of 77.1 L/min.
Figure 1 illustrates the trend of rising D-dimer values corresponding to hospitalization days and oxygenation demand until a peak is reached where the D-dimer value rapidly decreases along with the oxygenation demand.
Discussion
Whereas the three randomized clinical trials, ATTACC, ACTIV-4a, and REMAP-CAP only checked a baseline D-dimer, this study evaluated only those patients who had multiple D-dimer tests during the course of hospitalization. The study suggests that daily D-dimer trend is the direct indicator of patients’ prognosis in patients with COVID-19. This study also found that a D-dimer level ≥ 2 µg/mL is strongly associated with increased death in the multivariate logistic regression model (p-value <0.05) and increased oxygenation requirements in the multivariate linear regression model (p-value <0.01). The study found that seventy seven percent (77%) of the patients who had a D-dimer ≥ 2 µg/mL, died during hospitalization. In this study, the oxygen requirements and D-dimer trends were found following similar trends and directions both in univariate and multivariate linear analysis. In a previous study, this trend held consistent at the individual level (Ref 6).
The D-dimer can be elevated or abnormal at baseline for many patients due to pre-existing chronic medical conditions. This is likely why D-dimer trends, instead of depending on baseline D-dimer (i.e., changes of D-dimer as opposed to day one level), is more meaningful for patients prognosis. Dr. Kabir previously reported D-dimer values continue to increase prior to patient death among patients with COVID-19 (Ref 6). This can be mediated by increasing D-dimer which indicates increased thrombogenic activity due to COVID-19. The current study also showed that decreasing trends of D-dimer, when treated with appropriate dose of anticoagulation, is associated with decreased oxygen requirements which lead to patient survival. While patients are having increasing trends of D-dimer, keeping the patient with the same dose of anticoagulation would lead to increase in D-dimer and oxygen requirements and subsequently death. Hence, a baseline D-dimer should be established at admission and then daily D-dimer trends should guide anticoagulation dose to reduce death related to COVID-19 instead of treating everyone with therapeutic anticoagulation.
Dr. Kabir’s previously reported that non-critically ill COVID-19 patients who were already on direct oral anticoagulants (DOAC) prior to the diagnosis of COVID-19 had increased survival rates (Ref 5). This current study has found that non-critically ill patients with COVID-19 who were treated with intermediate-dose anticoagulation at an early stage have a higher survival rate compared to those who received low or high dose anticoagulation. The study also found that patient’s D-dimer levels were significantly associated with patient oxygen requirements and patient survival. Since patients treated with low or high-dose anticoagulation were associated with increased death, the treatment strategies should be to start the patient on moderate-dose anticoagulation and gradually titrate the dose up or down based on the patient’s daily D-dimer trends and bleeding risk. Dr. Kabir’s treatment strategy for COVID-19 was also published in 2021 (Ref 6).
The current study found that the best treatment strategy in non-critically ill COVID-19 patients was to start moderate dose anticoagulation (Enoxaparin 40 mg SQ twice a day) and titrate the dose up or down based on D-dimer trends and patient’s condition. The death rate among patients treated with moderate dose D-dimer was six percent (6%).
Treating patients with anticoagulation is only beneficial when capillaries are still open, not clogged due to microthrombi. Therefore, the patients who present in the hospital with nasal cannula oxygen, high flow nasal cannula oxygen, or patients with moderately high D-Dimer (less than two-fold higher than the upper limit of normal) usually survive with anticoagulation and steroid combination treatments. The authors observed that increasing trends of D-Dimer were inversely related to the survival rates. There is a dose-effect relationship between the decreasing trends of D-Dimer with the anticoagulation dose. Hence, D-Dimer trends can be considered to predict patient prognosis. This finding has also been correlated by another study stating that D-dimer monitoring will be a crucial approach in the clinical practice of COVID-19 infection (Ref 9). It is also possible that when the widespread coagulation cascade is initiated at the onset of COVID-19 inoculation in patients with COVID-19 who are critically ill, they do not respond to therapeutic anticoagulation. The suggested reason behind the lower chance of recovery is that anticoagulation does not dissolve microthrombi (blood clots) but rather prevents their further growth.
Vaccination has improved the outlook for survival in COVID-19 patients, and higher rates of vaccination have been shown to be associated with reduced death rates. A study on the impact of the Pfizer-BioNTech COVID-19 vaccine showed a 51% reduction in death in individuals who had received one dose (Ref 7). The vaccine works by inducing a strong S protein antibody response and a CD4+ T cell response. This, thereby, reduces the viral load and associated vasculitis causing a decrease in coagulopathy (Ref 8).
The study concludes daily D-dimer trends can predict COVID-19 patient survival or daily oxygen requirements. This indicates D-dimer can be considered as the miracle molecule for COVID-19 patients prognosis. In addition, a moderate dose of anticoagulation is superior to high dose or low dose anticoagulation if it is started at an early stage of COVID-19 diagnosis. The study recommends starting anticoagulation at a moderate dose and titrating the anticoagulation dose based on D-Dimer trends to reduce the risk of life-threatening bleeding. The study recommends developing bleeding risk-based COVID-19 anticoagulation treatment strategies so that patients with high bleeding risk can be spotted initially and considered a lower dose of anticoagulation. Further clinical trials are recommended to evaluate patients’ outcome while treated with moderate dose or low dose direct oral anticoagulation (e.g., Apixaban or Rivaroxaban) at the diagnosis of COVID-19 among patients who do not require any oxygen.
Conflicts of Interest
The authors has no conflict of interest to disclose.
References
- The ATTACC, ACTIV-4a, and REMAP-CAP Investigators. (2021) Therapeutic Anticoagulation with Heparin in Noncritically Ill Patients with Covid-19. N Engl J Med. [CrossRef]
- The REMAP-CAP, ACTIV-4a, and ATTACC….. (2021) Therapeutic Anticoagulation with Heparin in Critically Ill Patients with Covid-19. N Engl J Med. [CrossRef]
- Ackermann M, Verleden SE, Kuehnel M, Haverich A, Welte T, Laenger F, et al. Pulmonary vascular endothelialitis, thrombosis, and angiogenesis in Covid-19. N Engl J Med. 2020 Jul 9;383(2):120–8. [CrossRef]
- Lévesque V, Millaire É, Corsilli D, Rioux-Massé B, Carrier FM. Severe immune thrombocytopenic purpura in critical COVID-19. Int J Hematol. 2020 Jul 1;112(5):746–50. [CrossRef]
- Kabir, Azad. Letter to the editor. (2020): Is Therapeutic Anticoagulation the Answer in Treating COVID-19? JMSMA. 20; Vol 61 (10). 1-2 (Submitted August 15, 2020). 20 October.
- Kabir A., A. (2021). Anticoagulation is the answer in treating noncritical COVID-19 patients. Open medicine (Warsaw, Poland), 16(1), 1486–1492. [CrossRef]
- Lopez Bernal, J., Andrews, N., Gower, C., Robertson, C., Stowe, J., Tessier, E., Simmons, R., Cottrell, S., Roberts, R., O’Doherty, M., Brown, K., Cameron, C., Stockton, D., McMenamin, J., & Ramsay, M. (2021). Effectiveness of the Pfizer-BioNTech and Oxford-AstraZeneca vaccines on covid-19 related symptoms, hospital admissions, and mortality in older adults in England: test negative case-control study. BMJ (Clinical research ed.), 373, n1088. [CrossRef]
- Jeyanathan, M., Afkhami, S., Smaill, F. et al. Immunological considerations for COVID-19 vaccine strategies. Nat Rev Immunol 20, 615–632 (2020). [CrossRef]
- Mehrdad Rostami & Hassan Mansouritorghabeh (2020) D-dimer level in COVID-19 infection: a systematic review, Expert Review of Hematology, 13:11, 1265-1275. [CrossRef]
- Tassiopoulos, A. K., Mofakham, S., Rubano, J. A., Labropoulos, N., Bannazadeh, M., Drakos, P., Volteas, P., Cleri, N. A., Alkadaa, L. N., Asencio, A. A., Oganov, A., Hou, W., Rutigliano, D. N., Singer, A. J., Vosswinkel, J., Talamini, M., Mikell, C. B., & Kaushansky, K. (2021). D-Dimer-Driven Anticoagulation Reduces Mortality in Intubated COVID-19 Patients: A Cohort Study With a Propensity-Matched Analysis. Frontiers in medicine, 8, 631335. [CrossRef]
- Yalçin, Kadir S.; Kasapoğlu, Benan; Alanli, Recep; Küçükay, Murat B.; Koşar, Ali The association of oxygen saturation, tomography findings and d-dimer levels in coronavirus disease 2019 patients, Blood Coagulation & Fibrinolysis: 20 - Volume 31 - Issue 8 - p 558-561. 20 December. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).