Submitted:
22 January 2026
Posted:
23 January 2026
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Distribution, Physiological Role, and Contribution to Atrial Fibrosis of Epicardial Adipose Tissue
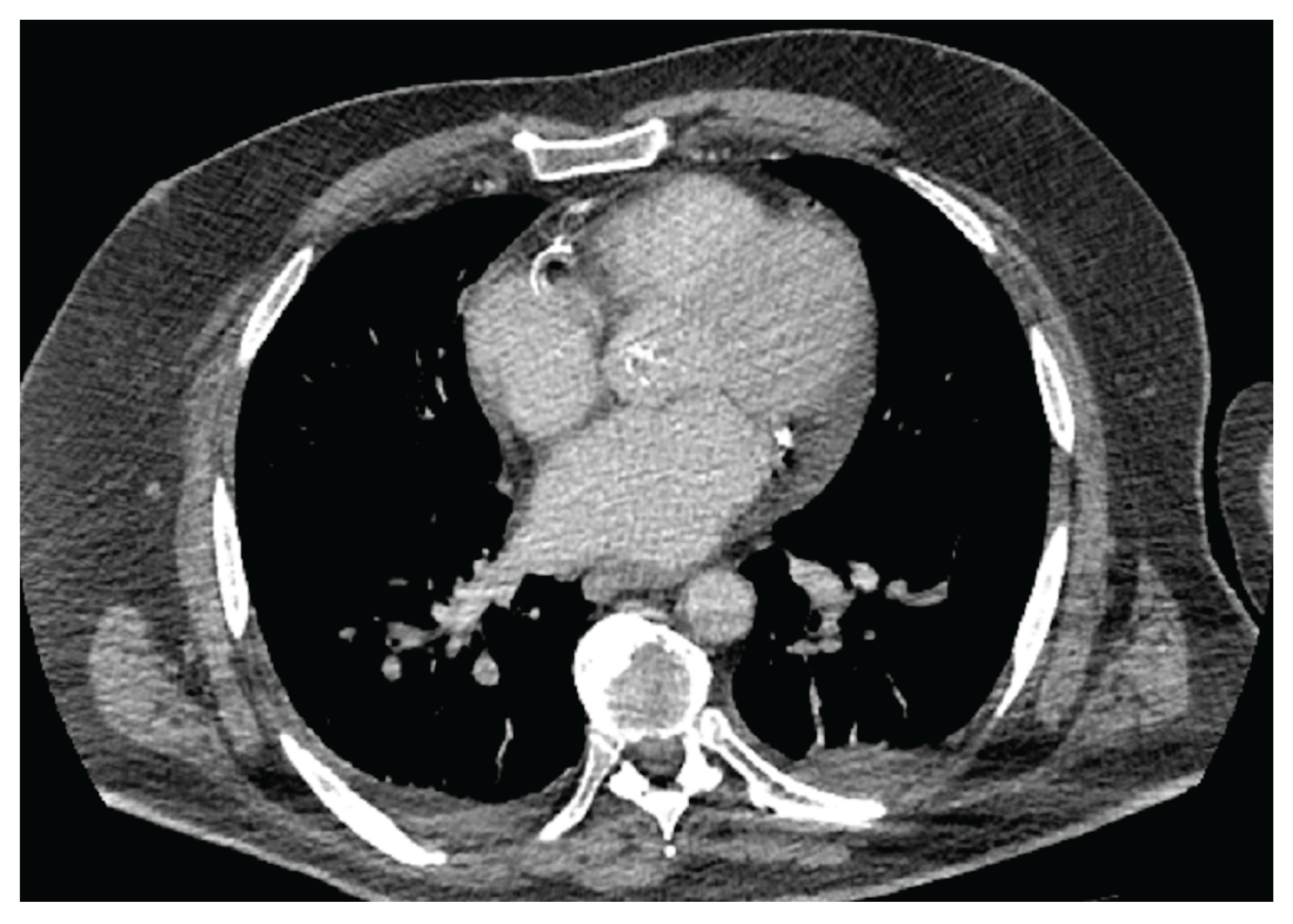
3. Cardiac CT and MRI in the Assessment of Epicardial Adipose Tissue
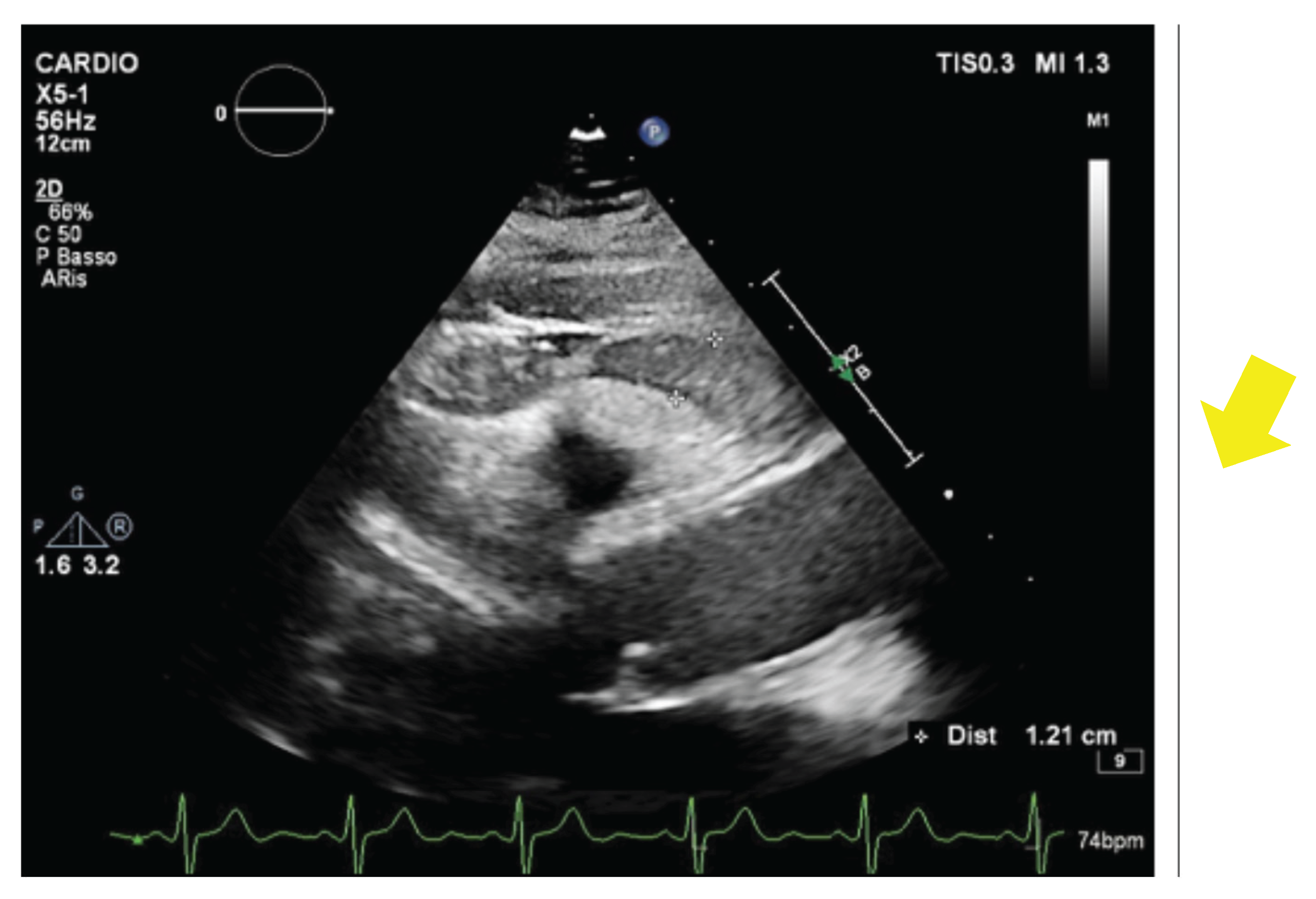
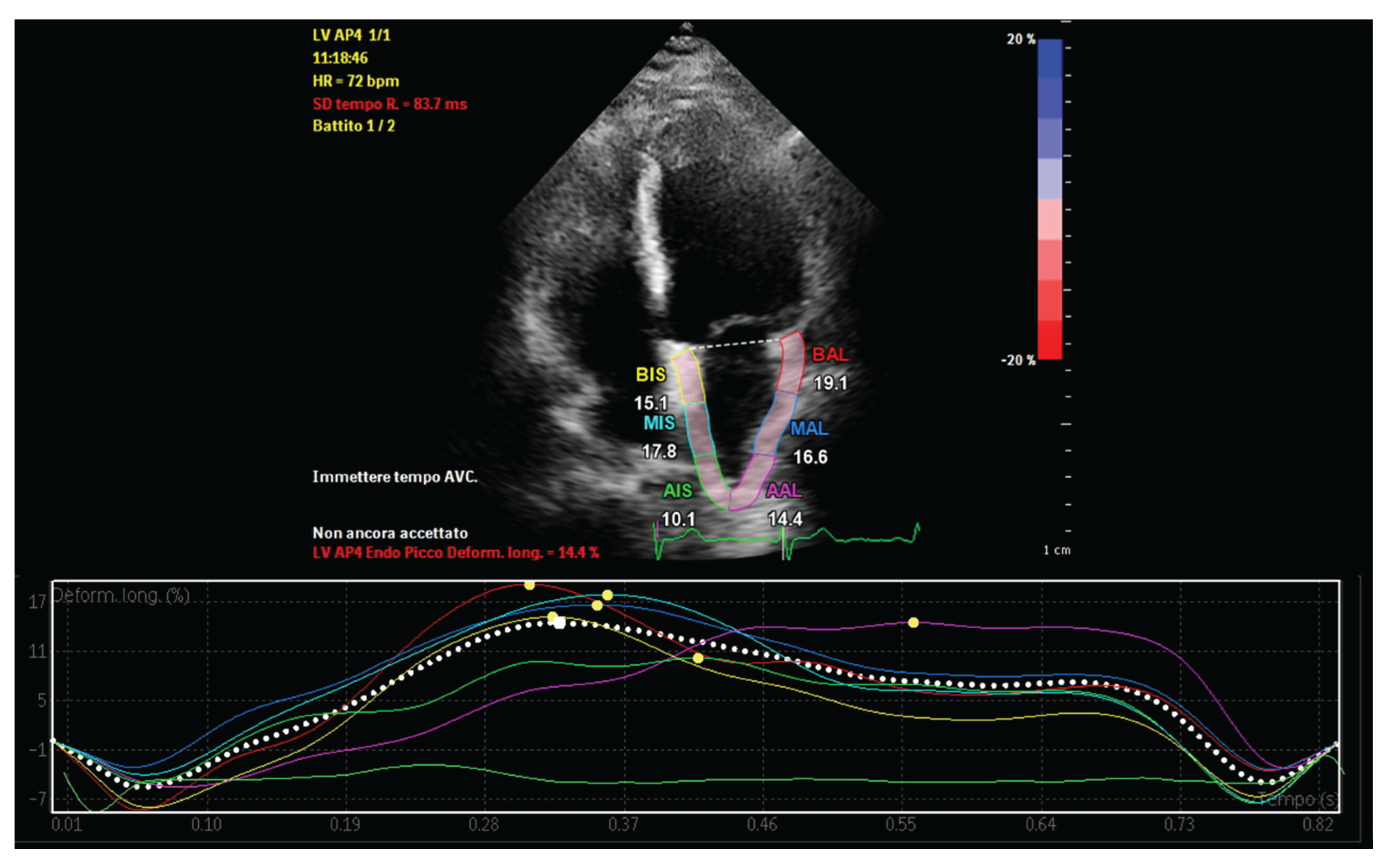
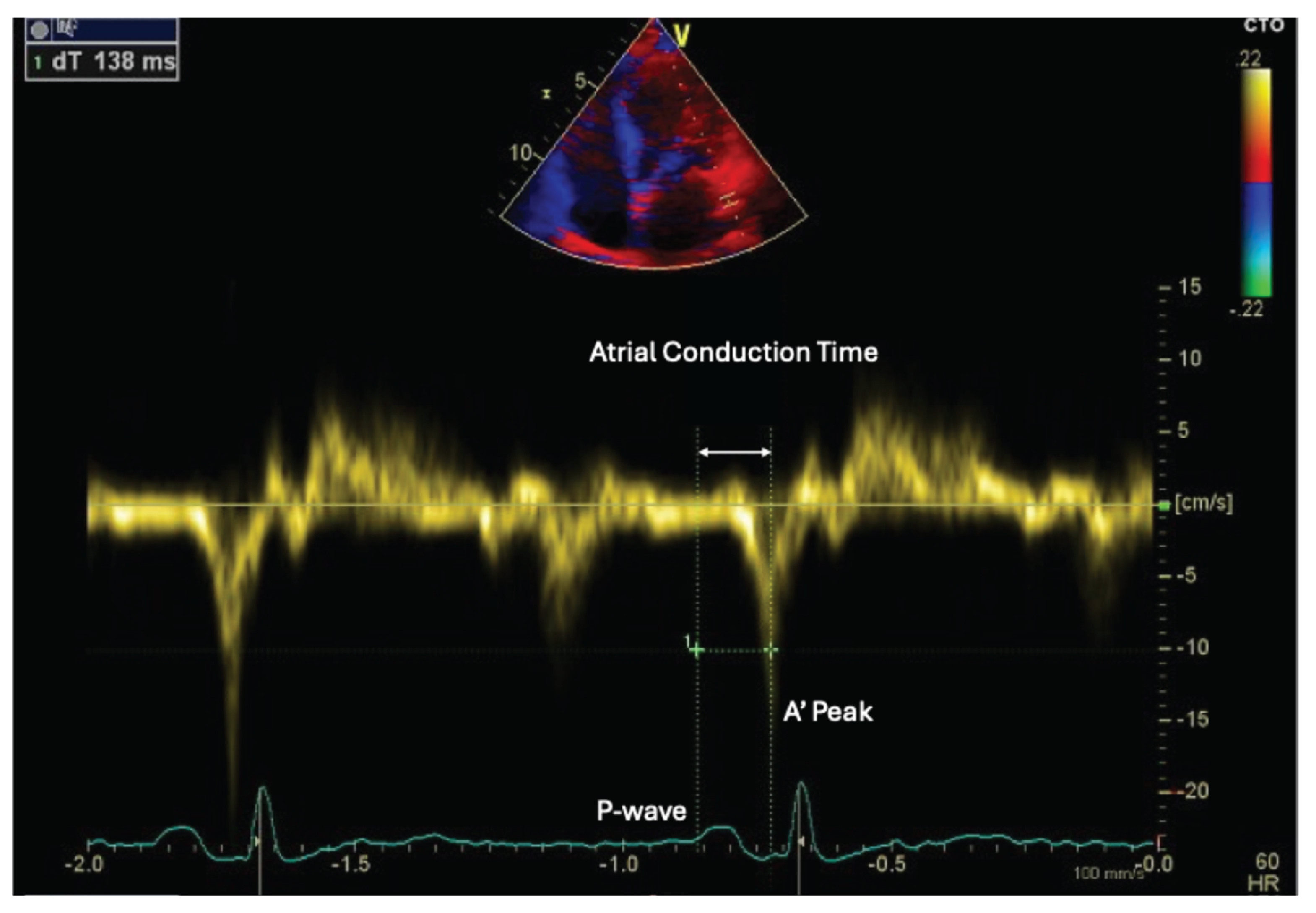
4. Echocardiographic Assessment of Atrial Function in Patients with Increased Epicardial Adipose Tissue
5. Electroanatomical Mapping of the Left Atrium
6. Posterior Wall Electroanatomical Ablation vs Cryoballoon PVI
7. Therapeutic Implications of GLP-1 Receptor Agonists and Dual GIP/GLP-1 Agonists
8. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| EAM EAT GLP-1 GIP LAA LGE PA-TDI PVI PWI VAT |
Electroanatomical mapping Epicardial adipose tissue Glucagon-like peptide-1 Glucose-dependent insulinotropic polypeptide Left atrial appendage Late gadolinium enhancement P-wave to A’-wave tissue Doppler imaging interval Pulmonary vein isolation Posterior wall isolation Visceral adipose tissue |
References
- Raggi, P; Stillman, AE. Clinical Role of Epicardial Adipose Tissue. Can J Cardiol 2025, 41(9), 1753–1763. [Google Scholar] [CrossRef] [PubMed]
- Iacobellis, G. Epicardial adipose tissue in contemporary cardiology. Nat Rev Cardiol 2022, 19(9), 593–606. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Şengül, C; Özveren, O. Epicardial adipose tissue: a review of physiology, pathophysiology, and clinical applications. Anadolu Kardiyol Derg 2013, 13(3), 261–5. [Google Scholar] [CrossRef] [PubMed]
- Bodenstab, ML; Varghese, RT; Iacobellis, G. Cardio-Lipotoxicity of Epicardial Adipose Tissue. Biomolecules 2024, 14(11), 1465. [Google Scholar] [CrossRef] [PubMed Central]
- Cacciapuoti, F; Caso, I; Crispo, S; Verde, N; Capone, V; Gottilla, R; Materazzi, C; Volpicelli, M; Ziviello, F; Mauro, C; et al. Linking Epicardial Adipose Tissue to Atrial Remodeling: Clinical Implications of Strain Imaging. Hearts 2025, 6(1), 3. [Google Scholar] [CrossRef]
- Packer, M. Epicardial Adipose Tissue May Mediate Deleterious Effects of Obesity and Inflammation on the Myocardium. J Am Coll Cardiol. 2018, 71(20), 2360–2372. [Google Scholar] [CrossRef] [PubMed]
- Conte, M; Petraglia, L; Cabaro, S; Valerio, V; Poggio, P; Pilato, E; Attena, E; Russo, V; Ferro, A; Formisano, P; Leosco, D; Parisi, V. Epicardial Adipose Tissue and Cardiac Arrhythmias: Focus on Atrial Fibrillation. Front Cardiovasc Med. 2022, 9, 932262. [Google Scholar] [CrossRef] [PubMed Central]
- Ma, M; Zheng, X; Wu, X; Xie, Q. Epicardial adipose tissue thickness on transthoracic echocardiography predicts 2-year incident atrial fibrillation in elderly hypertensive patients. Front Cardiovasc Med 2025, 12, 1650423. [Google Scholar] [CrossRef] [PubMed Central]
- Nakahara, S; Hori, Y; Kobayashi, S; Sakai, Y; Taguchi, I; Takayanagi, K; Nagashima, K; Sonoda, K; Kogawa, R; Sasaki, N; Watanabe, I; Okumura, Y. Epicardial adipose tissue-based defragmentation approach to persistent atrial fibrillation: its impact on complex fractionated electrograms and ablation outcome. Heart Rhythm 2014, 11(8), 1343–51. [Google Scholar] [CrossRef] [PubMed]
- Iacobellis, G. Epicardial Fat Inflammation and GLP-1/GIP Receptor Analogs: Are we Shifting our Perspective? Curr Cardiol Rep. 2025, 27(1), 161. [Google Scholar] [CrossRef] [PubMed]
- Hasebe, H; Yoshida, K; Nogami, A; Ieda, M. Difference in epicardial adipose tissue distribution between paroxysmal atrial fibrillation and coronary artery disease. Heart Vessels 2020, 35(8), 1070–1078. [Google Scholar] [CrossRef] [PubMed]
- Neeland, IJ; Zhu, F; Graca, G; Lymperopoulos, A; Iacobellis, G; Farzaneh, A; Bos, D; Ghanbari, M; Goldberger, JJ; Kavousi, M; Greenland, P. Metabolomics Profiling of Epicardial Adipose Tissue: MESA and the Rotterdam Study. J Am Heart Assoc. 2025, 14(13), e039750. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Cacciapuoti, F; Liguori, C; Nasti, R; Capone, V; Cacciapuoti, F. Unlocking the Mysteries of Epicardial Adipose Tissue: Implications of Cardiometabolic Syndrome. Research in Cardiovascular Medicine 2024, 13(2), 23–28. [Google Scholar] [CrossRef]
- Vyas, V; Sandhar, B; Keane, JM; Wood, EG; Blythe, H; Jones, A; Shahaj, E; Fanti, S; Williams, J; Metic, N; Efremova, M; Ng, HL; Nageswaran, G; Byrne, S; Feldhahn, N; Marelli-Berg, F; Chain, B; Tinker, A; Finlay, MC; Longhi, MP. Tissue-resident memory T cells in epicardial adipose tissue comprise transcriptionally distinct subsets that are modulated in atrial fibrillation. Nat Cardiovasc Res. 2024, 3(9), 1067–1082. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Carena, MC; Badi, I; Polkinghorne, M; Akoumianakis, I; Psarros, C; Wahome, E; Kotanidis, CP; Akawi, N; Antonopoulos, AS; Chauhan, J; Sayeed, R; Krasopoulos, G; Srivastava, V; Farid, S; Walcot, N; Douglas, G; Channon, KM; Casadei, B; Antoniades, C. Role of Human Epicardial Adipose Tissue-Derived miR-92a-3p in Myocardial Redox State. J Am Coll Cardiol. 2023, 82(4), 317–332. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Sha, R; Baines, O; Hayes, A; Tompkins, K; Kalla, M; Holmes, AP; O'Shea, C; Pavlovic, D. Impact of Obesity on Atrial Fibrillation Pathogenesis and Treatment Options. J Am Heart Assoc. 2024, 13(1), e032277. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Nakatani, Y; Sakamoto, T; Yamaguchi, Y; Tsujino, Y; Kinugawa, K. Epicardial adipose tissue affects the efficacy of left atrial posterior wall isolation for persistent atrial fibrillation. J Arrhythm. 2020, 36(4), 652–659. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Huber, AT; Fankhauser, S; Wittmer, S; Chollet, L; Lam, A; Maurhofer, J; Madaffari, A; Seiler, J; Servatius, H; Haeberlin, A; Noti, F; Brugger, N; von Tengg-Kobligk, H; Gräni, C; Roten, L; Tanner, H; Reichlin, T. Epicardial adipose tissue dispersion at CT and recurrent atrial fibrillation after pulmonary vein isolation. Eur Radiol 2024, 34(8), 4928–4938. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Trimarchi, G; Carerj, ML; Zito, C; Bella, GD; Taverna, G; Cusmà Piccione, M; Crea, P; Lo Giudice, S; Buonpane, A; Bonanni, M; Restelli, D; Paradossi, U; Monteleone, A; Micari, A; Carerj, S. Epicardial Adipose Tissue: A Multimodal Imaging Diagnostic Perspective. Medicina (Kaunas) 2025, 61(6), 961. [Google Scholar] [CrossRef] [PubMed Central]
- West, HW; Siddique, M; Williams, MC; Volpe, L; Desai, R; Lyasheva, M; Thomas, S; Dangas, K; Kotanidis, CP; Tomlins, P; Mahon, C; Kardos, A; Adlam, D; Graby, J; Rodrigues, JCL; Shirodaria, C; Deanfield, J; Mehta, NN; Neubauer, S; Channon, KM; Desai, MY; Nicol, ED; Newby, DE; Antoniades, C; ORFAN Investigators. Deep-Learning for Epicardial Adipose Tissue Assessment With Computed Tomography: Implications for Cardiovascular Risk Prediction. JACC Cardiovasc Imaging 2023, 16(6), 800–816. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Umar, A; Hocking, J; Massin, SZ; Suszko, A; Wintersperger, BJ; Chauhan, VS. Association of Cardiac CT-Derived Epicardial Adipose Tissue With Atrial Fibrillation in Patients Without Left Atrial Fibrosis as Defined by Endocardial Voltage Mapping. J Cardiovasc Electrophysiol. 2025, 36(2), 489–500. [Google Scholar] [CrossRef] [PubMed]
- Duca, F; Mascherbauer, K; Donà, C; Koschutnik, M; Binder, C; Nitsche, C; Halavina, K; Beitzke, D; Loewe, C; Bartko, P; Waldmann, E; Mascherbauer, J; Hengstenberg, C; Kammerlander, A. Association of epicardial adipose tissue on magnetic resonance imaging with cardiovascular outcomes: Quality over quantity? Obesity (Silver Spring). 2024, 32(9), 1670–1679. [Google Scholar] [CrossRef] [PubMed]
- Firouznia, M; Ylipää, E; Henningsson, M; Carlhäll, CJ. Poincare guided geometric UNet for left atrial epicardial adipose tissue segmentation in Dixon MRI images. Sci Rep. 2025, 15(1), 25549. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Skoda, I; Henningsson, M; Stenberg, S; Sundin, J; Carlhäll, CJ. Simultaneous Assessment of Left Atrial Fibrosis and Epicardial Adipose Tissue Using 3D Late Gadolinium Enhanced Dixon MRI. J Magn Reson Imaging 2022, 56(5), 1393–1403. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Eroğlu, S. How do we measure epicardial adipose tissue thickness by transthoracic echocardiography? Anatol J Cardiol 2015, 15(5), 416–9. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Nabati, M; Moradgholi, F; Moosazadeh, M; Parsaee, H. The correlation between epicardial fat thickness and longitudinal left atrial reservoir strain in patients with type 2 diabetes mellitus and controls. Ultrasound J 2023, 15(1), 37. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Müller, P; Weijs, B; Bemelmans, NMAA; Mügge, A; Eckardt, L; Crijns, HJGM; Bax, JJ; Linz, D; den Uijl, DW. Echocardiography-derived total atrial conduction time (PA-TDI duration): risk stratification and guidance in atrial fibrillation management. Clin Res Cardiol. 2021, 110(11), 1734–1742. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Karsum, EH; Andersen, DM; Modin, D; Biering-Sørensen, SR; Mogelvang, R; Jensen, G; Schnohr, P; Gislason, G; Biering-Sørensen, T. The prognostic value of left atrial dyssynchrony measured by speckle tracking echocardiography in the general population. Int J Cardiovasc Imaging 2021, 37(5), 1679–1688. [Google Scholar] [CrossRef] [PubMed]
- Cacciapuoti, F; Caso, I; Gottilla, R; Minicucci, F; Volpicelli, M; Caso, P. Left Atrial Mechanics and Remodeling in Paroxysmal Atrial Fibrillation: Introducing the EASE Score for Pre-Ablation Risk Prediction. Med Sci (Basel) 2025, 13(3), 131. [Google Scholar] [CrossRef] [PubMed Central]
- Zghaib, T; Ipek, EG; Zahid, S; Balouch, MA; Misra, S; Ashikaga, H; Berger, RD; Marine, JE; Spragg, DD; Zimmerman, SL; Zipunnikov, V; Trayanova, N; Calkins, H; Nazarian, S. Association of left atrial epicardial adipose tissue with electrogram bipolar voltage and fractionation: Electrophysiologic substrates for atrial fibrillation. Heart Rhythm 2016, 13(12), 2333–2339. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Shao, Y; Chen, L; Chen, W; Sang, C; Xu, C; Zhang, C. Left atrial epicardial adipose tissue is associated with low voltage zones in the left atrium in patients with non-valvular atrial fibrillation. Front Cardiovasc Med. 2022, 9, 924646. [Google Scholar] [CrossRef] [PubMed Central]
- Tonko, JB; Silberbauer, J; Lambiase, PD. Peak frequency analysis for epicardial contact mapping: How (in)frequent is epicardial adipose tissue? Heart Rhythm 2024, 21(10), 1898–1899. [Google Scholar] [CrossRef] [PubMed]
- Firouznia, M; Molnar, D; Edin, C; Hjelmgren, O; Östgren, CJ; Lundberg, P; Henningsson, M; Bergström, G; Carlhäll, CJ. Head-to-Head Comparison between MRI and CT in the Evaluation of Volume and Quality of Epicardial Adipose Tissue. Radiol Cardiothorac Imaging 2025, 7(4), e240531. [Google Scholar] [CrossRef] [PubMed]
- Qiu, B; Li, F; Sang, C; Shen, J; Shao, Y; Chen, W; Hu, X; Li, C; Hu, C; Zhang, C; Wang, Z; Chen, M. Combination of Epicardial Adipose Tissue and Left Atrial Low-Voltage Areas Predicting Atrial Fibrillation Recurrence after Radiofrequency Ablation. Cardiology 2025, 150(1), 48–55. [Google Scholar] [CrossRef] [PubMed]
- Cacciapuoti, F; Gottilla, R; Caso, I; Crispo, S; Pirozzi, C; Minicucci, F; Volpicelli, M. One size does not fit all: Echocardiography as a decision-making tool in atrial fibrillation management – A case series. J Cardiovasc Echography 2025, 35, 403–9. [Google Scholar]
- Sperling, JS; Delurgio, DL; Svinarich, JT. Posterior left atrial epicardial adipose tissue: scope of the problem and impact of new technology. Curr Opin Cardiol 2022, 37(1), 54–61. [Google Scholar] [CrossRef] [PubMed]
- van Rosendael, AR; Dimitriu-Leen, AC; van Rosendael, PJ; Leung, M; Smit, JM; Saraste, A; Knuuti, J; van der Geest, RJ; van der Arend, BW; van Zwet, EW; Scholte, AJ; Delgado, V; Bax, JJ. Association Between Posterior Left Atrial Adipose Tissue Mass and Atrial Fibrillation. Circ Arrhythm Electrophysiol 2017, 10(2), e004614. [Google Scholar] [CrossRef] [PubMed]
- Momot, K; Pruc, M; Rodkiewicz, D; Koźluk, E; Krauz, K; Piątkowska, A; Zalewska, Z; Buksińska-Lisik, M; Szarpak, L; Mamcarz, A. Predictive Value of Epicardial Adipose Tissue Parameters Measured by Cardiac Computed Tomography for Recurrence of Atrial Fibrillation After Pulmonary Vein Isolation. J Clin Med. 2025, 14(19), 6963. [Google Scholar] [CrossRef] [PubMed Central]
- Liang, JJ; Elafros, MA; Muser, D; Pathak, RK; Santangeli, P; Supple, GE; Schaller, RD; Frankel, DS; Dixit, S. Comparison of Left Atrial Bipolar Voltage and Scar Using Multielectrode Fast Automated Mapping versus Point-by-Point Contact Electroanatomic Mapping in Patients With Atrial Fibrillation Undergoing Repeat Ablation. J Cardiovasc Electrophysiol. 2017, 28(3), 280–288. [Google Scholar] [CrossRef] [PubMed]
- Mumtaz, M; Jabeen, S; Danial, A; Chaychi, MTM; Zaheer, MK; Mumtaz, A; Mumtaz, T; Herweg, B. Adjunct posterior wall isolation reduces the recurrence of atrial fibrillation in patients undergoing cryoballoon ablation: A systematic review and meta-analysis. J Cardiovasc Electrophysiol. 2023, 34(10), 2043–2052. [Google Scholar] [CrossRef] [PubMed]
- Lee JM, Shim J, Park J, Yu HT, Kim TH, Park JK, Uhm JS, Kim JB, Joung B, Lee MH, Kim YH, Pak HN; POBI-AF Investigators. The Electrical Isolation of the Left Atrial Posterior Wall in Catheter Ablation of Persistent Atrial Fibrillation. JACC Clin Electrophysiol Erratum in: JACC Clin Electrophysiol. 2023 Jan;9(1):145. doi: 10.1016/j.jacep.2022.12.001. PMID: 31753429. 2019, 5(11), 1253–1261. [Google Scholar] [CrossRef]
- Anagnostopoulos, I; Kousta, M; Kossyvakis, C; Paraskevaidis, NT; Vrachatis, D; Deftereos, S; Giannopoulos, G. Epicardial Adipose Tissue and Atrial Fibrillation Recurrence following Catheter Ablation: A Systematic Review and Meta-Analysis. J Clin Med. 2023, 12(19), 6369. [Google Scholar] [CrossRef] [PubMed Central]
- Kistler, PM; Chieng, D; Sugumar, H; Ling, LH; Segan, L; Azzopardi, S; Al-Kaisey, A; Parameswaran, R; Anderson, RD; Hawson, J; Prabhu, S; Voskoboinik, A; Wong, G; Morton, JB; Pathik, B; McLellan, AJ; Lee, G; Wong, M; Finch, S; Pathak, RK; Raja, DC; Sterns, L; Ginks, M; Reid, CM; Sanders, P; Kalman, JM. Effect of Catheter Ablation Using Pulmonary Vein Isolation With vs Without Posterior Left Atrial Wall Isolation on Atrial Arrhythmia Recurrence in Patients With Persistent Atrial Fibrillation: The CAPLA Randomized Clinical Trial. JAMA 2023, 329(2), 127–135. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ding, Y; Lin, F; Liu, Z; Zhou, X; Liang, X. Targeting Epicardial/Pericardial Adipose Tissue in Cardiovascular Diseases: A Novel Therapeutic Strategy. Rev Cardiovasc Med. 2025, 26(3), 26128. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Wiszniewski, K; Grudniewska, A; Szabłowska-Gadomska, I; Pilichowska-Paszkiet, E; Zaborska, B; Zgliczyński, W; Dudek, P; Bik, W; Sota, M; Mrozikiewicz-Rakowska, B. Epicardial Adipose Tissue-A Novel Therapeutic Target in Obesity Cardiomyopathy. Int J Mol Sci 2025, 26(16), 7963. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Myasoedova, VA; Parisi, V; Moschetta, D; Valerio, V; Conte, M; Massaiu, I; Bozzi, M; Celeste, F; Leosco, D; Iaccarino, G; Genovese, S; Poggio, P. Efficacy of cardiometabolic drugs in reduction of epicardial adipose tissue: a systematic review and meta-analysis. Cardiovasc Diabetol 2023, 22(1), 23. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Yaribeygi, H; Maleki, M; Nasimi, F; Jamialahmadi, T; Stanford, FC; Sahebkar, A. Benefits of GLP-1 Mimetics on Epicardial Adiposity. Curr Med Chem. 2023, 30(37), 4256–4265. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Aronne, LJ; Horn, DB; le Roux, CW; Ho, W; Falcon, BL; Gomez Valderas, E; Das, S; Lee, CJ; Glass, LC; Senyucel, C; Dunn, JP. SURMOUNT-5 Trial Investigators. Tirzepatide as Compared with Semaglutide for the Treatment of Obesity. N Engl J Med. 2025, 393(1), 26–36. [Google Scholar] [CrossRef] [PubMed]
- Brachs, S; Soll, D; Beer, F; Huckauf, N; Konkar, A; Spranger, J; Rütten, H; Mai, K. Hormonal regulation of human adipose tissue lipolysis: impact of adipose GIP system in overweight and obesity. Eur J Endocrinol 2025, 192(2), 91–99. [Google Scholar] [CrossRef] [PubMed]
- Rosenkilde, MM; George, JT; Véniant, MM; Holst, JJ. GIP Receptor Antagonists in the Pharmacotherapy of Obesity: Physiologic, Genetic, and Clinical Rationale. Diabetes 2025, 74(8), 1334–1338. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2026 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




