1. Introduction
Dr. Franz Tappeiner (1816–1902) is recognized as a central figure in the emergence of Meran (Merano) as a 19th-century Alpine health resort [
1]. His impact extended far beyond Tappeiner championed the integration of climatic and landscape-based walking therapy (
Terrainkur), a model popularized by the Munich laryngologist Max Joseph Oertel [
2], alongside social hygiene, epidemic control, and civic health planning [
3,
4].
Its relevance has resurfaced considering modern challenges, such as chronic disease prevention, climate-responsive healthcare, and nature-based rehabilitation strategies, which increasingly echo historical practices once sidelined by biomedical reductionism [
5,
6]. His work during the 1855 cholera epidemic in Meran exemplifies early epidemiological communication and hygiene education, and his financing of the
Terrainkur walkway “Tappeiner Promenade” (Tappeinerweg) illustrates the concretization of nature as a therapeutic setting [
1,
7].
This article is published in conjunction with the commemoration of Tappeiner’s 210th birthday in 2026, which is being marked by a matinée event at Meran’s city library on 17 January 2026. Bringing together voices from cultural history, journalism, and medicine, the event frames Tappeiner as both a product and shaper of 19th-century modernity.
Drawing from both primary material (including educational records and local health policy initiatives) and secondary medical-historical research, this article reconstructs Tappeiner’s development as a physician and a civic actor. A historiographically informed perspective situates him within the epistemic landscape of medicine around 1850, a period marked by theoretical pluralism, diagnostic uncertainty, and competing paradigms of disease causation.
The goals of this study are threefold,
to contextualize Tappeiner’s medical and civic activity within 19th-century Central European health culture,
to evaluate his contributions considering modern public health discourse—particularly regarding environmental and preventive care,
and to assess the continued relevance of terrain-based and climate-responsive health models in rehabilitation and noncommunicable disease management today.
Rather than offering a chronological biography, this article proceeds thematically. It begins with a brief biographical sketch and historical context, proceeds to analyze prevailing medical theories and practices around 1850, and then turns to Tappeiner’s applied work in Meran, especially his roles in epidemic response, health education, and spatial-therapeutic innovation. The conclusion reflects on his enduring legacy in medical humanism and public health practice.
2. Biographical Sketch and Historical Context
2.1. Rural Origins and Academic Formation
Franz Tappeiner was born in 1816 in Laas (Lasa), a rural village in the Vinschgau valley of the historic Tyrol, today South Tyrol (Autonomous Province of Bolzano, Italy). Coming from a farming family, his path to the medical profession was marked by intellectual ambition and a remarkable educational trajectory for someone of a non-aristocratic background. After attending the Benedictine Gymnasium in Meran and completing his gymnasium and philosophical studies in Innsbruck, Tappeiner began his medical studies in 1836 at the University of Prague. He continued his medical education in Padua in 1837 and subsequently returned to Prague, before completing his studies in Vienna, where he came under the influence of leading figures of the Second Viennese Medical School. He attended clinical and pathological lectures by Joseph Škoda and Carl von Rokitansky, and dermatology lectures by Ferdinand von Hebra. These formative experiences combined the traditional framework of humoral theory with the emerging empirical-scientific approach to diagnosis and pathology. He was awarded a Doctor medicinae universae degree in 1843 [
1,
8].
In 1846, after completing his medical studies and initial clinical experience, Tappeiner moved to Meran to establish himself as a practicing physician in a town marked by post-revolutionary uncertainty, poverty, and inadequate public health infrastructure (
Figure 1). At that time, Meran lacked a proper hospital and was served only by a basic hospice and an old-age care facility. With few medical professionals and recurring epidemics worsened by inadequate sanitation, these conditions strengthened Tappeiner’s enduring dedication to public hygiene, modern medical infrastructure, and community-based health initiatives [
1,
8].
2.2. Political and Social Conditions in 19th-Century Tyrol
The period following the Napoleonic Wars saw Tyrol reintegrated into the Austrian Empire, experiencing both administrative modernization and growing nationalist sentiment [
9,
10]. The Vormärz era was marked by socio-political rigidity, as well as infrastructural and intellectual stirrings [
11]. In South Tyrol, the economy remained predominantly agrarian throughout the first half of the 19th century, with small-scale handicrafts often being integrated into agricultural households. However, by the late 1830s and the 1840s, urban centers such as Meran began to develop a civic bourgeoisie that was increasingly invested in public hygiene, education, and emerging medical modernity, particularly as the town gained recognition for its health-promoting climate and therapeutic potential [
1,
7,
12].
2.3. Medical Theory and Practice Circa 1850
Tappeiner practiced at a time when the epistemic foundations of medicine were in a state of flux. Germ theory had not yet been established—Koch’s postulates emerged only in the 1880s—and miasma theory, which attributed disease to harmful environmental vapors or “bad air,” remained dominant in European medical thinking [
13,
14]. Physicians believed that clean air, proper elevation, and natural environments were essential for preventing and curing illnesses, particularly respiratory and epidemic diseases [
15,
16]. This context explains Tappeiner’s therapeutic emphasis on mountain climates, fresh air, and atmospheric purity, aligning him with the broader 19th-century practices of climate therapy and high-altitude health resorts [
17,
18].
Contagionism often coexisted with miasmatic theory, with physicians viewing both "bad air" and direct transmission as pathogenic forces requiring ventilation and isolation [
19,
20]. "Heroic" treatments, such as bloodletting and purgatives, remained common based on humoral models [
21,
22], while balneological treatments reflected environmental healing beliefs [
23]. Pre-bacteriological hygiene entered institutions through hygiene chairs and sanitation protocols [
24,
25]. Limited pharmacological options have led to empirical yet theoretically speculative medicine [
26,
27].
Tappeiner’s adoption of terrain therapy, climate medicine, and public sanitation initiatives reveals a practitioner who was highly responsive to evolving conceptions of health. Rather than adhering rigidly to dogma, Tappeiner integrated empirical reasoning with a strong belief in environmental and social determinants, positioning himself at the forefront of mid-19th-century medicine.
3. Public Health Physician: Cholera, Hygiene, and Preventive Thinking
When Franz Tappeiner moved to Meran in 1846, he swiftly became a pivotal figure in the city’s medical and public spheres, influencing them for several years [
1]. His medical practice extended beyond the city limits, reaching rural communities in the Vinschgau (Venosta) and Passeier (Passiria) valleys. In an area lacking adequate sanitary facilities, hospitals, and sufficient medical staff, he combined his clinical duties with public efforts to enhance hygiene, prevent diseases, and promote public health. Tappeiner exemplified the physician-citizen model by merging practical medical care with a commitment to environmental and social concerns.
3.1. The 1855 Cholera Pamphlet: Community-Facing Medical Communication
Cholera posed a recurring threat to 19th-century Northern Italy, with severe outbreaks occurring in 1836 and 1855. In 1855, nearly 30,000 people died in Tuscany alone [
28], and Ferrara recorded over 2000 cases linked to poor housing conditions [
29]. In Bologna, the epidemic triggered a shift from clerical to medical administrative governance [
30]. Although data on South Tyrol are limited, the region lies within a vulnerable Alpine-Habsburg corridor. Nearby Carinthia and Carniola responded with quarantine regimes and lazarettos, reflecting the evolving epidemic governance [
31,
32,
33].
In response to the devastating cholera epidemic of 1855 [
28,
29,
30], Tappeiner published a leaflet titled “Some Words About Cholera for the Instruction and Reassurance of the Rural Population,” one of the rare examples of early medical outreach aimed directly at lay audiences in South Tyrol (
Supplementary Table S1) [
34]. The text was written during a time of widespread panic and misinformation, and it sought to calm fears and provide practical advice to the rural population, which he considered especially vulnerable to rumors and superstition.
Tappeiner employed a clear and accessible tone, consciously addressing the rural population in non-technical terms. His guidance reflected prevailing miasmatic assumptions: he recommended ventilation, personal hygiene, moderation in diet, and avoidance of cold or wet conditions to prevent the disease. He emphasized the early recognition of cholera symptoms, especially initial diarrhea, and encouraged prompt, self-administered treatment using simple remedies. Tappeiner also advised against extreme behaviors, such as excessive fear or restrictive eating, calling instead for calm, orderly conduct. His reassurance that cholera was not contagious in the traditional sense and his appeal to compassion for the sick reflect both his empirical orientation and early awareness of the psychosocial dimensions of health.
3.2. Hygiene, Early Intervention, and Behavioral Regulation
As discussed in
Section 2.3, miasmatic logic dominated mid-19th-century medicine. Within this framework, Tappeiner’s pamphlet advocated for prevailing medical paradigms. Contagionism emerged in hybrid models that linked disease spread to impure air [
35,
36]. Tappeiner’s emphasis on ventilation, cleanliness, and moderate eating aligns with contemporary preventive practices [
37]. His warnings against dietary excess and fear reflected humoral theories linking illness to imbalances and emotional disturbances [
38,
39,
40]. This guidance embodied the "dietetics of the soul" and recognized emotions as pathogenic factors [
39,
40]. The pamphlet transformed the physicians into public health advocates. Through practical guidance and promotion of collective responsibility, Tappeiner pioneered epidemic risk communication [
37,
41], combining authority with humility while emphasizing practical health protection measures.
3.3. Assessment from a Contemporary Perspective
Tappeiner’s 1855 cholera pamphlet constitutes a notably progressive contribution to public health communication, even when evaluated using contemporary standards. Although grounded in the miasmatic paradigm, it articulates principles that are now integral to modern outbreak guidance: clear, actionable messaging, behavior-oriented prevention, culturally embedded language, and an early form of community health literacy [
42,
43,
44]. His concise instructions on recognizing early symptoms, employing simple remedies, ensuring ventilation, and avoiding fear or excess reflected a pragmatic, experience-based approach to epidemic risk mitigation.
In contrast to abstract or medicalized explanations, Tappeiner’s approach emphasized practical behavioral modifications, such as sanitary discipline, dietary moderation, and psychological calmness, which align closely with contemporary evidence on effective cholera communication strategies [
45,
46]. Presented in local accessible prose, this approach exemplifies a model of culturally appropriate and community-specific messaging endorsed by modern risk communication frameworks [
47,
48].
Although the absence of microbial contagion may appear to be a deficit, it must be understood within the epistemic constraints of the 1850s. Tappeiner’s trust in environmental control and behavioral measures was both scientifically coherent for the period and strategically effective within its historical framework. His intervention thus reflects an early instance of prevention-first, population-level health promotion, foreshadowing today WASH (Water, Sanitation, and Hygiene) logic and One Health paradigms [
46,
49].
4. The Researching Physician: Tappeiner Between Science and Practice
4.1. Scientific Inquiry Beyond Institutions
Despite being based outside the academic centers, Tappeiner undertook empirical investigations that reflected a rigorous scientific mindset. His meteorological recordings, climatological reports, and long-term observations of pulmonary patients exemplified an early form of translational research, turning local data into generalized health recommendations. His commitment to methodical, data-informed practice positions him within the lineage of “researching physicians” whose work bridges the bedside and benchside, clinic, and community.
4.2. Tuberculosis Transmission Experiments
Before the discovery of the tubercle bacillus in 1882, Franz Tappeiner had already positioned Meran as a favorable location for treating pulmonary diseases, especially phthisis, based on climatological and observational data. By the 1840s, Meran had begun attracting patients suffering from consumption (“Schwindsucht”), and Tappeiner’s publications played a central role in legitimizing its status as a therapeutic destination [
50,
51]. Although specialized sanatoria emerged only later, his advocacy for hygiene, outdoor exposure, and elevation helped lay the conceptual groundwork for Meran’s transformation into a tuberculosis health resort city. Notably, his direct involvement in climate medicine preceded his 1877 experimental work on tuberculosis transmission, reflecting a transition from empirical climatotherapy to pathogen-oriented investigation.
4.2.1. Experimental Proof of Airborne Transmission
Franz Tappeiner’s experimental studies on the transmission of tuberculosis were among the earliest systematic efforts to establish the infectivity of phthisis via inhalation and have since gained retrospective scientific recognition [
52]. Beginning in the summer of 1877, Tappeiner conducted a series of controlled inhalation experiments in Munich [
53], which were later replicated and extended in Meran and Berlin [
54,
55,
56]. These experiments involved the exposure of dogs—and in some cases rabbits—to aerosolized sputum from tuberculosis patients, vaporized with water in closed chambers. The animals subsequently developed miliary tuberculosis, demonstrating that the disease could be transmitted via airborne particles and supporting the identification of phthisis and tuberculosis as manifestations of the same contagious condition. Tappeiner emphasized that these findings were based not on isolated trials in Munich but on multiple replications across sites, including rural Meran, where he performed inhalation and oral exposure experiments [
55]. Notably, dogs fed tuberculous sputum did not develop tuberculosis, reinforcing inhalation as the critical transmission route [
53]. The specificity of the response was underscored by the absence of pathological changes in the control animals and the reproducibility of the results across species and locations.
4.2.2. Scientific Reception and Historical Positioning
These findings were first published in 1878 in the Virchow’s “Archiv für pathologische Anatomie und Physiologie und für klinische Medicin” [
53] after the first presentation at the “Versammlung deutscher Naturforscher und Ärzte” in Munich [
57]. Tappeiner’s work was further discussed in professional journals of the time [
58], including additional reports by colleagues such as Dr. Hausmann in Meran and in correspondence with contemporaries [
54,
55]. Rudolf Virchow, then one of the most authoritative figures in German medicine with whom Tappeiner replicated his findings in Berlin [
56], acknowledged the scientific rigor and relevance of Tappeiner’s experiments, lending further legitimacy to his contributions despite their rural, non-institutional origin [
6].
Importantly, Tappeiner’s experiments preceded Robert Koch’s identification of the tubercle bacillus in 1882 by five years. While Koch’s bacteriological breakthrough provided microbial proof, Tappeiner had already established a robust empirical model of airborne tuberculosis transmission. Reports from this period indicate that Koch referenced Tappeiner’s work in early lectures [
54], illustrating its integration into the evolving bacteriological discourse. Although not affiliated with an academic laboratory, Tappeiner’s research circulated within scientific networks and contributed foundational observational evidence for the airborne nature of infectious diseases.
4.2.3. Enduring Relevance and Validation Through Modern Research
Tappeiner’s experiments were controversial at the time [
54,
55], but have since been supported by microbiological and epidemiological research. Modern studies have confirmed that
Mycobacterium tuberculosis can survive in dried or heat-fixed sputum, retaining infectivity for several days. Laboratory data show viable bacilli persisting in unstained sputum smears for at least seven days [
59,
60] and in preserved samples for up to eight days [
61]. This supports the plausibility of infection risk via aerosolized and dried material.
Beyond viability, research has consistently demonstrated that indoor air quality critically influences the risk of transmission. Inadequate ventilation and overcrowding amplify the airborne spread of tuberculosis, particularly in healthcare settings, public transport, prisons, and housing with poor air exchange. Modeling and empirical studies suggest that improving natural or mechanical ventilation can reduce the transmission risk by up to 97% [
62,
63,
64]. Outbreak investigations have further shown transmission through shared indoor air without direct contact [
65]. These findings retrospectively validate the core aspects of Tappeiner’s observational and experimental approach. While working without bacteriological tools, his emphasis on inhalational pathways anticipated modern insights into the dynamics of airborne diseases. His tuberculosis research, though unconventional for its time, aligned closely with what would become established knowledge of environmental transmission and respiratory hygiene.
Tappeiner’s work exemplifies how physicians operating outside institutional research centers can nonetheless make foundational contributions to medical science. His tuberculosis experiments, anatomical investigations, and public health writings reflect a practitioner who was deeply committed to empirical observation, anatomical rigor, and innovative inquiry. Contemporary evidence supports the notion that such research engagement enhances clinical quality: physicians involved in research consistently demonstrate more critical thinking, stronger evidence appraisal, and more reflective and context-sensitive decision-making [
66,
67]. Research-active clinicians are also more likely to align care with real-world health needs and act as conduits for translating scientific knowledge into practice [
68,
69]. Although Tappeiner practiced far from academic centers, his integration of clinical experience with experimental reasoning aligns with modern understanding of how research-informed physicians advance both care and knowledge.
Tappeiner’s integration of observation, experimentation, and environmental reasoning shaped both his hygienic interventions and infrastructural legacy, as explored in the following chapters.
5. Public Health in Practice: From Hygiene to Therapeutic Landscapes
5.1. Hygienic Interventions and Preventive Thinking
Franz Tappeiner’s contributions to public health in Meran began with his proactive response to the cholera epidemic of 1855. His efforts extended beyond direct patient care and included public education initiatives. The pamphlet emphasized the importance of early symptom recognition, advocated straightforward behavioral and dietary interventions, and advised against panic. This approach was reflective of the prevailing miasmatic theory of disease while also highlighting the significance of behavioral prevention and emotional regulation.
Tappeiner’s methodology was founded upon the principles of education, environmental regulation, and social solidarity. He asserted that health should not be regarded as a private issue but as a matter of civic responsibility. Affluent citizens were encouraged to support the impoverished, medications were dispensed at no cost, and municipal authorities were urged to establish the essential infrastructure. His focus on clean water, well-ventilated housing, and systematic burial practices presaged numerous elements of institutional hygiene that emerged only in subsequent decades [
1].
Importantly, Tappeiner’s approach to preventive health extended beyond addressing acute epidemics. He consistently perceived health as being influenced by modifiable factors such as air, water, and behavior, and acted in accordance with this understanding. He endorsed early quarantine measures, advocated for waste management reforms, and promoted public access to medical information. Through these initiatives, Meran established a foundational framework for a health-conscious city, predating the formalization of such concepts in public health legislation [
1].
Tappeiner’s philosophy embodies an early iteration of what would subsequently be identified as “social hygiene”: a form of medicine intertwined with civic responsibility, moral conduct and environmental stewardship. His interventions established the foundation for Meran’s evolution from a provincial town into a therapeutic landscape characterized by health-oriented infrastructure rather than merely passive geography [
1].
5.2. Climate Medicine and the Rise of Meran as a Health Destination
Prior to the establishment of the formal sanatorium system, Tappeiner played a pivotal role in establishing Meran as a site of therapeutic significance for individuals suffering from consumption [
70], a term historically associated with phthisis and later identified as pulmonary tuberculosis [
71]. Drawing from multi-year clinical observations and local meteorological data, he argued that Meran’s mild winters, moderate humidity, and stable barometric conditions created an optimal environment for respiratory recovery [
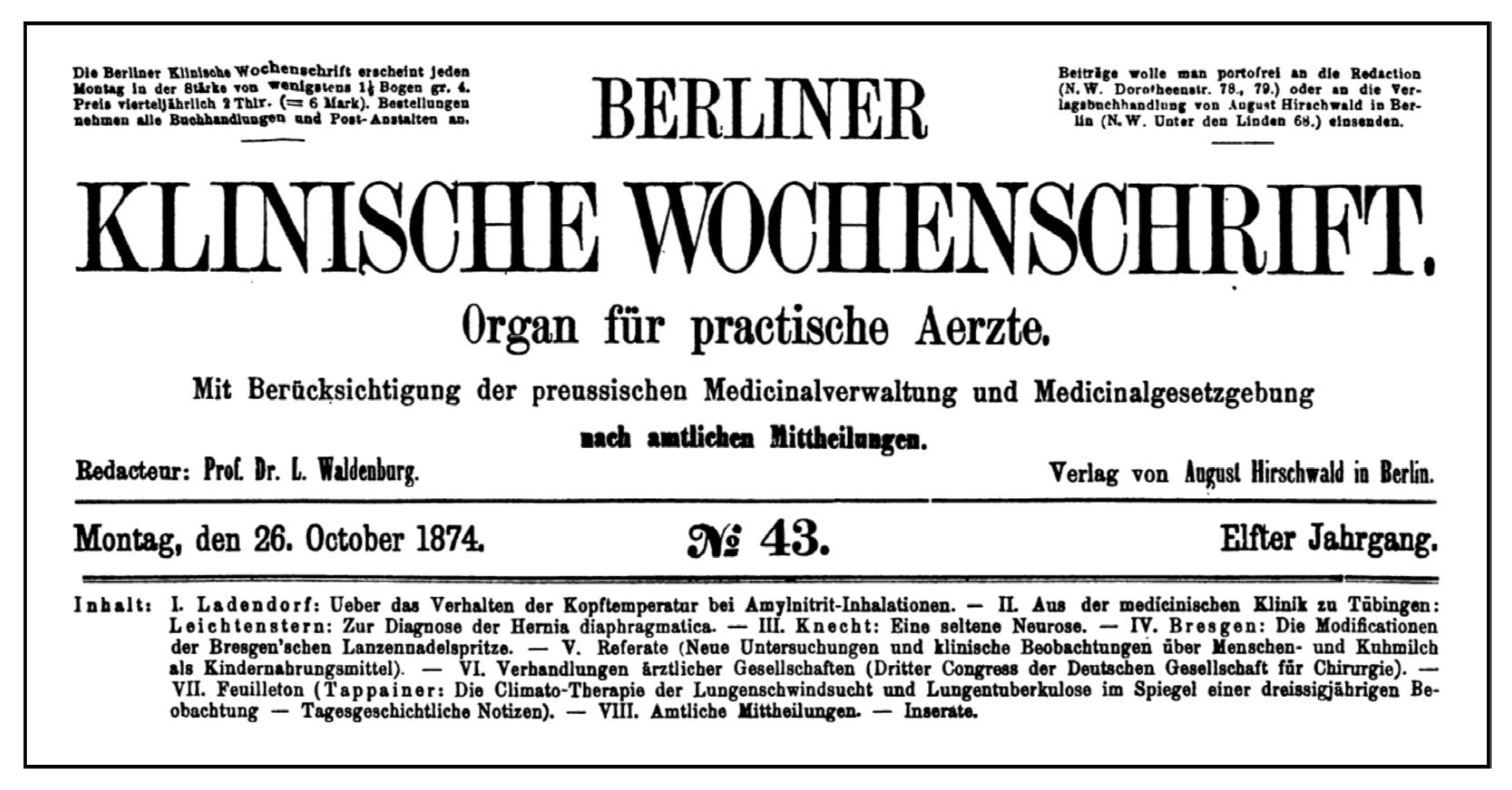
50]. His reasoning, published in “Die Climato-Therapie der Lungenkatharre und Lungenphthise im Spiegel einer dreißigjährigen Beobachtung” (The Climate Therapy of Pulmonary Catarrh and Pulmonary Phthisis in the Light of Thirty Years of Observation) in 1874 [
51], emphasized the role of empirical evidence gathered over decades of treating patients in Meran, rather than anecdotal reports or romanticized landscape depictions (
Figure 2).
His argument followed a clinical, observation-based logic. Tappeiner documented seasonal patterns in disease progression and differentiated the outcomes of patients wintering in Meran from those treated in northern or alpine regions, where harsh conditions often triggered relapses or accelerated decline in health. He proposed that early relocation to a climate-stable environment could delay deterioration—an idea aligned with the constitutional thinking of the time but reinforced by longitudinal outcomes [
51]. This climate-based rationale for pulmonary care played a key role in Meran’s rise as a therapeutic center before the bacteriological revolution in tuberculosis treatment.
Tappeiner’s contributions presaged the emergence of alpine sanatoria, such as those in Davos and Arosa, yet his methodology was conceptually distinct. He conceptualized climate as a modifiable determinant of health rather than merely a passive geographic asset. Instead of relying on enclosed institutions, he integrated medical reasoning with civic infrastructure and advocated for the development of walkways, green spaces, and enhanced ventilation. His design of Meran as a therapeutic urban landscape anticipated the now widely accepted public health principle that cities can be engineered to promote good health.
This conceptual framework resonates significantly with contemporary research on Urban Green and Blue Spaces (UGBS) as health assets. Current studies confirm that meticulously designed urban greenways and park systems, such as the Tappeiner Promenade, promote physical activity, enhance air quality, mitigate urban heat, and support mental well-being, particularly for socioeconomically disadvantaged groups [
72,
73,
74]. Furthermore, the present focus on integrating health objectives into urban planning, co-designing with citizens, and restoring ecological buffers aligns with the environmental foresight inherent in Tappeiner’s interventions [
75,
76,
77]. His work anticipated what is now recognized as preventive urbanism, in which spatial design, green infrastructure, and health equity are interconnected. By reimagining Meran as a walkable, ventilated, and restorative environment, Tappeiner conceptualized the city as a living therapeutic system—an idea that is only now being formalized in urban health and climate policies.
5.3. The Terrainkur as Visionary Preventive Medicine
In the 1880s, Tappeiner began engaging with the
Terrainkur, a physiologically grounded form of graded walking therapy systematically developed by von Oertel [
78]. Alongside Tappeiner, physicians such as Bernhard Mazegger jun. and Raphael Hausmann played intermediary roles in operationalizing
Terrainkur in Meran, linking Oertel’s physiological theory with local governance, alpine associations, and patient education [
79,
80]. Contemporary reporting in the Meraner Zeitung demonstrates that the introduction of the
Terrainkur in Meran was not confined to medical circles but actively communicated to the wider public [
80]. Detailed newspaper accounts explained its physiological rationale, therapeutic indications, and infrastructural realization, underscoring the high level of public engagement with health, prevention, and climate-based therapy in late-19th-century Meran.
The institutional involvement of the Alpine Club (Alpenverein) was pivotal for translating Oertel’s physiologically defined
Terrainkur into a reproducible, scalable public health infrastructure. By designing, marking, and maintaining graded paths according to medical specifications, the Alpine Club functioned as an early mediator between clinical prescription and spatial implementation [
79].
Rooted in cardiopulmonary physiology,
Terrainkur was originally designed for patients with chronic lung disease, anemia, early cardiac decompensation, and what Oertel described as fatty heart disease—a metabolic form of myocardial dysfunction responsive to structured physical exertion [
78]. Oertel’s approach emphasizes controlled ascents on defined gradients, with attention to pulse regulation, respiratory efficiency, and endurance building. The intervention aimed not only at somatic strengthening but also at optimizing oxygen uptake through prolonged exposure to open elevated air. Tappeiner, aware of the scientific underpinnings and therapeutic aims outlined by Oertel, strongly supported the integration of this regimen into the landscape of Meran, aligning it with his broader vision of preventive medicine and topography-based rehabilitation.
5.3.1. Therapeutic Landscapes and Environmental Reasoning
The development of the
Terrainkur walkway in the late 1880s marked a pivotal shift in Meran’s transformation into a modern health resort city. Sparked by the visit and influence of Oertel, the city embraced the principles of
Terrainkur as walking therapy. At the request of the health resort administration, Oertel served as consulting physician between 1886 and 1892, guiding the implementation of graded walking paths, standardized route markings, and medically supervised exercise protocols [
1,
81]. Combining elevation-adjusted gradients, curated vegetation, and broad accessibility, the promenade embodied an open-air alternative to closed sanatoria. Its design reflected a civic and ecological vision of public health, grounded in the conviction that structured movement in fresh air, especially during Meran’s dry winter climate, could improve cardiopulmonary and metabolic function.
Financed significantly through Tappeiner’s personal funds—amounting to 120,000 Kronen [
1], which corresponds to approximately 700,000 Euros today—and developed in consultation with local horticulturists, the promenade included a path that accommodated users with different physical abilities (
Figure 3). Its design reflects therapeutic logic: exposure to curated vegetation, elevation-adjusted movement, and panoramic views were intended to support vascular, pulmonary, and psychological health.
In contrast to enclosed, fee-based sanatoria that increasingly characterized tuberculosis treatment in alpine regions, the Tappeiner Promenade was freely accessible to all, irrespective of social class or diagnosis. Its design prioritized inclusion: the path’s gentle gradients and broad layout enabled use by wheelchair users and patients transported in rolling chairs or carts, with dedicated staff in Meran available to assist as attendants—ensuring that therapeutic walking was not restricted by mobility limitations. It functioned as both medical infrastructure and a civic statement, embedding prevention into daily life rather than isolating it within institutions.
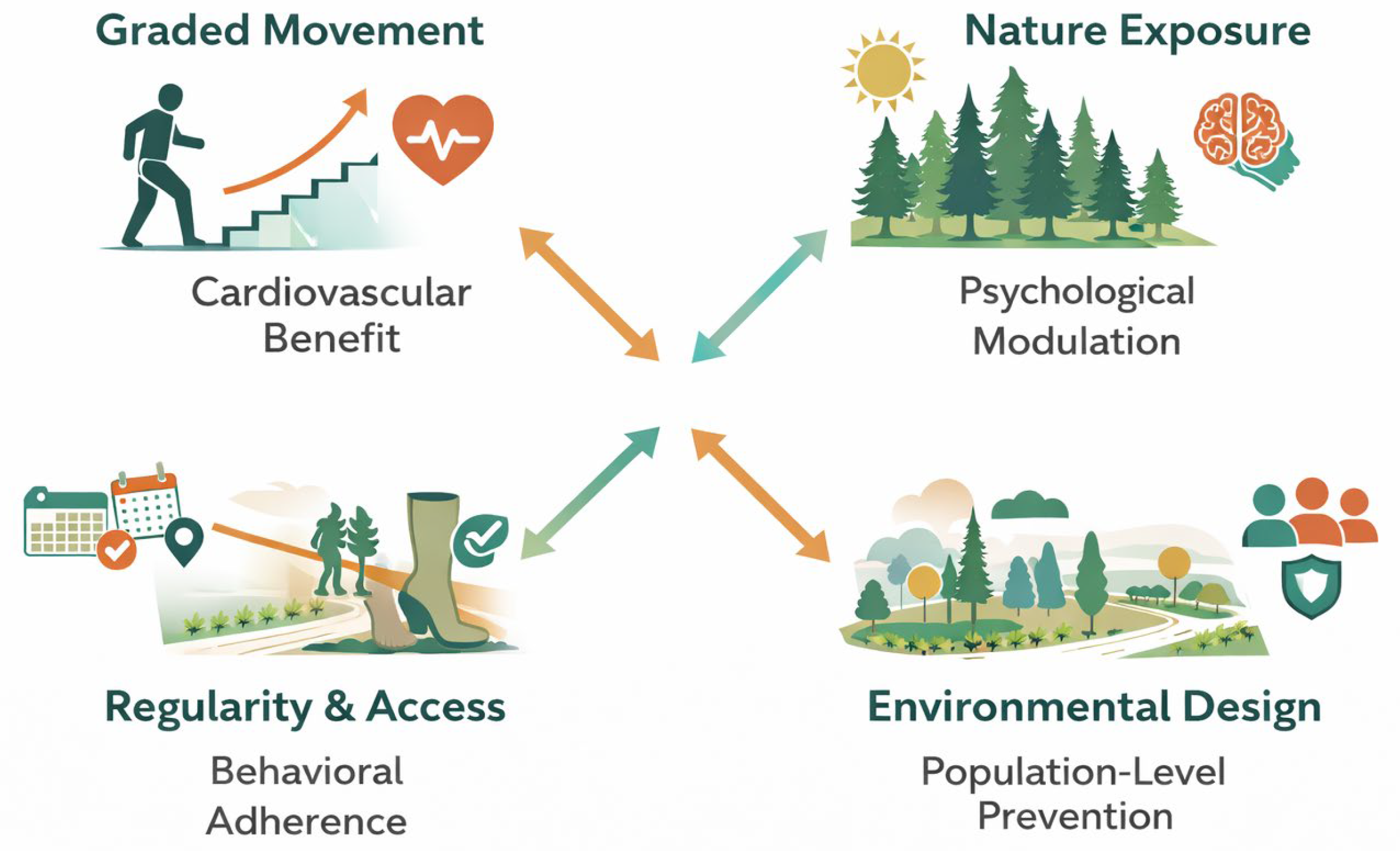
5.3.2. Terrainkur and Modern Rehabilitation Science
The approach of Oertel anticipated core elements of modern exercise prescription, including workload stratification, dose–response logic, and outcome monitoring [
79], principles that now underpin cardiac and pulmonary rehabilitation. Contemporary rehabilitation medicine has reaffirmed many of the principles embedded in the
Terrainkur [
82].
Walking at low to moderate intensity yields significant benefits across cardiovascular, metabolic, and psychological domains, thereby affirming its pivotal role in preventive and rehabilitative medicine [
83,
84]. In adults who were previously inactive but are otherwise healthy, walking programs have been shown to reduce systolic and diastolic blood pressure, body fat, and fasting glucose levels, while enhancing maximal oxygen uptake (VO₂max) and overall fitness. For patients with coronary artery disease, structured walking therapy—particularly when supervised—has been demonstrated to decrease cardiovascular mortality, hospitalizations, and myocardial infarction, and to result in measurable improvements in functional capacity and quality of life [
85,
86,
87]. Notably, Nordic walking has surpassed conventional rehabilitation in enhancing functional capacity and walking distance [
88].
In populations affected by obesity and metabolic syndrome, walking interventions have been shown to significantly enhance body mass index (BMI), insulin sensitivity, and inflammatory profiles. For instance, postmenopausal women with obesity exhibit reductions in high-sensitivity C-reactive protein (hs-CRP), Interleukin-6 (IL-6), and Tumor Necrosis Factor Alpha (TNF-α) following 12 weeks of moderate walking, suggesting vascular benefits and a decreased risk of cardiovascular disease [
89]. Both children and adults experience metabolic benefits, as evidenced by the reductions in fasting insulin and lipid ratios observed across various trials [
90,
91].
From a psychological perspective, walking is significantly correlated with reduced stress, anxiety, and depressive symptoms and enhances subjective well-being and quality of life. These effects are particularly pronounced in natural environments; "green" walking or park-based programs demonstrate greater improvements in mood and tension reduction than indoor or urban settings [
92,
93,
94]. Additionally, app-based and home-guided walking programs enhance accessibility, yielding comparable psychological benefits and high adherence rates to traditional walking programs.
Table 1 summarizes the key health effects of low- to moderate-intensity walking across the cardiovascular, metabolic, and psychological domains. Collectively, these findings illustrate that walking is a potent, scalable, and empirically supported intervention that demonstrates efficacy across a range of populations and conditions. Its integration into structured public health strategies, including terrain-based therapies such as
Terrainkur, anticipates and aligns with contemporary rehabilitation medicine. Tappeiner’s vision—encompassing tailored exertion, exposure to nature, and civic infrastructure as preventive medicine—is thus substantiated by a robust, contemporary evidence.
5.4. Climate Medicine and Post-Tuberculosis Urban Health
Tappeiner’s initial endeavors to position Meran as a destination for individuals with respiratory conditions—grounded in meteorological analysis and longitudinal patient documentation [
51]—foreshadowed contemporary methodologies that consider climate and topography as adjustable therapeutic resources. Currently, evidence supports the short-term effectiveness of low-altitude, clean-air environments in enhancing pulmonary function in patients with asthma and chronic obstructive pulmonary disease (COPD) [
95]. Furthermore, prolonged exposure to variations in temperature, precipitation, and biometeorological conditions continues to be acknowledged as a significant determinant of chronic respiratory morbidity and exacerbations [
96,
97,
98], thereby affirming Tappeiner’s assertion that Meran’s therapeutic efficacy was contingent upon climatic conditions and thus temporally constrained.
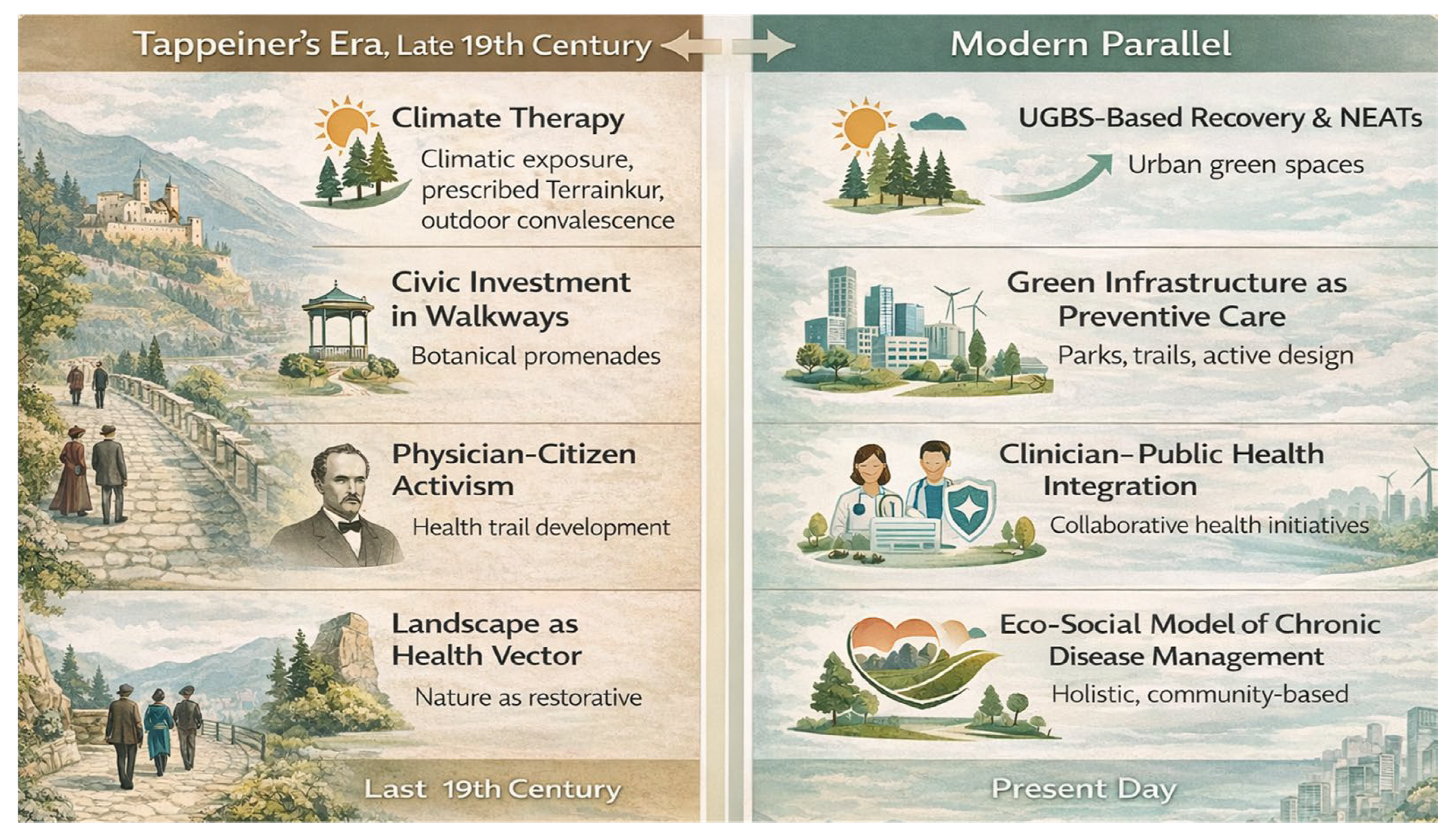
His subsequent transition towards terrain-based interventions, particularly through the establishment of the Tappeiner Promenade, signified a strategic reorientation of Meran’s role in health. As the town’s efficacy in treating infectious diseases diminished, Tappeiner reconceptualized it as a locus for recovery, prevention, and lifestyle-focused therapy, an approach that closely aligns with contemporary strategies for chronic disease prevention. Modern public health increasingly prioritizes contextual behavior change, incorporating geography, environmental stimuli, and social infrastructure to design interventions that are both place-sensitive and scalable [
99]. Nature-based and adventure therapies (NEATs), although not yet fully integrated into health systems, formally build upon this rationale by combining outdoor terrain with behavioral support to manage non-communicable diseases [
100]. Techniques for behavior change, such as goal setting, monitoring, and knowledge shaping, are essential components of successful lifestyle interventions and are increasingly employed in low-resource settings [
101,
102].
In redefining Meran, Tappeiner shifted the focus from acute respiratory care to the management of chronic diseases through landscape-mediated approaches. This redefinition anticipates contemporary evidence-based spatial and behavioral strategies, as illustrated in
Figure 4. His early vision recognized that both the environment and infrastructure serve not only as therapeutic contexts but also as active determinants of long-term health outcomes.
6. The Visionary: Integrating Clinical Insight, Environment, and Social Responsibility
A newspaper article published on Tappeiner’s 80th birthday in 1896 illustrates the extent to which his medical and civic work had entered public consciousness. The Meraner Zeitung portrayed him not merely as a successful physician, but as a moral authority and civic benefactor whose preventive, hygienic, and infrastructural initiatives were widely perceived as foundational for Meran’s transformation into a health resort [
70]. This public framing underscores the societal resonance of preventive medicine and environmental health strategies in late-19th-century Meran.
Tappeiner’s trajectory—from tuberculosis care to terrain-based rehabilitation—embodied a synthesis of empirical medicine, environmental sensibility, and social equity. His efforts did not follow institutional blueprints; rather, they arose from situated practices, informed observations, and responsiveness to public needs.
In his writings and interventions, Tappeiner consistently argued for an expanded role for the physician—not limited to curative care, but extending into the design of spaces, communication of risk, and democratization of prevention. He financed public infrastructure, distributed cholera pamphlets, documented meteorological-health correlations, and transformed his town into a health-promoting landscape.
Current public health frameworks increasingly endorse cross-sectoral collaboration, ecological determinants of health, and participatory civic engagement. In this respect, Tappeiner’s legacy extends well beyond mere historical curiosity. He emerges as a prescient model for integrating clinical practice, scientific reasoning, and civic ethics in public health. His work exemplifies what current scholarship calls the “clinician-citizen”—a physician whose responsibilities extend from bedside to policy, grounded in public health ethics and social accountability [
103,
104].
Tappeiner’s projects, such as advocating hygiene ordinances, supporting worker welfare, and investing in shared green spaces, directly anticipated today’s eco-social frameworks that view the environment, social equity, and health as interdependent systems [
105,
106]. His role in building the Tappeiner Promenade exemplifies this synthesis: a project shaped by environmental foresight, clinical insight, and civic commitment, realized through cooperation with local stakeholders. This aligns with modern calls for transdisciplinary, place-based health promotion, where municipalities, civil society, and health actors co-create public health infrastructure [
107,
108].
The Tappeiner Promenade—still in daily use—is not merely a historical artifact but a living embodiment of “health citizenship.” As a designed landscape that invites movement, reflection, and recovery, it resonates with current thinking around green citizen initiatives as health-promoting and place-making interventions. [
109]. It stands as a testament to how public health can be materially expressed as walkable terrain, civic space, and social infrastructure, all shaped by scientific care and public commitment (
Figure 5).
7. Conclusions
Franz Tappeiner’s contributions extend beyond his clinical achievements and the enduring physical infrastructure of the promenade bearing his name. He exemplified a model of medical practice characterized by scientific rigor and civic engagement, aligning with the 21st-century public health paradigm. This paradigm emphasizes climate-sensitive, behaviorally structured, and environmentally integrated approaches to the prevention and care of adults.
This paper documents Tappeiner’s progression from a provincial physician addressing epidemic threats to an empirical researcher, urban health strategist, and pioneer in spatially grounded rehabilitation. His interventions against cholera and tuberculosis anticipated bacteriological reasoning before its widespread acceptance. His work in climate therapy and subsequent advocacy for structured terrain-based movement illustrate a strategic transition from managing infectious diseases to facilitating long-term recovery.
This trajectory parallels the contemporary shift toward preventing noncommunicable diseases through ecological and behavioral interventions. Through initiatives such as the Tappeiner Promenade—co-designed, municipally integrated, and personally financed—he operationalized the concept of the city as preventive infrastructure. This walkway represents an early example of health-promoting urban design, consistent with current evidence on green spaces, therapeutic landscapes, and walkability as social determinants of health.
In an era marked by chronic disease burden and climate disruption, Tappeiner’s integrated model of medicine, environment, and civic design offers enduring guidance. His legacy invites a redefinition of the physician’s role, not only as a healer but as a co-architect of the social, spatial, and environmental conditions that enable health across the life course.
Supplementary Materials
The following supporting information can be downloaded at: Preprints.org.
Author Contributions
Conceptualization, P.R., U.K., D.H. and C.J.W.; methodology, P.R. and C.J.W.; investigation, P.R. and C.J.W.; writing—original draft preparation, C.J.W.; writing—review and editing, P.R., U.K. and D.H.; supervision, D.H. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data were created.
Acknowledgments
During the preparation of this manuscript, the authors used ChatGPT-5.2 (OpenAI, San Francisco, CA, USA) and Consensus (Consensus, Inc., Cambridge, MA, USA) for the purposes of language refinement, figure concept development and generation, content synthesis, and structuring of scientific tables and graphics, and literature search and summarization, respectively. The authors have reviewed and edited the output and take full responsibility for the content of this publication.
Conflicts of Interest
P.R. and U.K. have edited a book publication on Franz Tappeiner and hold associated authorship agreements. P.R. is also active as a tourism expert with historical expertise and undertakes public and private commissions related to the city of Meran. P.R. and D.H. declare no potential conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| BMI |
Body Mass Index |
| COPD |
Chronic Obstructive Pulmonary Disease |
| CV |
Cardiovascular |
| HOMA-IR |
Homeostatic Model Assessment of Insulin Resistance |
| NEATs |
Nature-, Eco-, and Adventure-Based Therapies |
| QoL |
Quality of Life |
| UGBS |
Urban Green and Blue Spaces |
| VO2max |
Maximal Oxygen Uptake |
| WASH |
Water, Sanitation, and Hygiene |
References
- Kindl, U.; Rina, P. Franz Tappeiner. Kurarzt und Mäzen – Medico e Mecenate; Merabilia: Bozen, Italien; Athesia, 2017; ISBN 978-88-6839-249-9. [Google Scholar]
- Wormer, E.J. Oertel, Max Joseph. Neue Deutsche Biographie 1999, 19, 450. Available online: https://www.deutsche-biographie.de/pnd117106259.html#ndbcontent (accessed on 7 January 2026).
- Rosen, G. A History of Public Health; Johns Hopkins University Press: Baltimore, MA, USA, 2015; ISBN 1-4214-1601-8. [Google Scholar]
- Weindling, P. Health, Race and German Politics between National Unification and Nazism, 1870-1945; Cambridge University Press: Cambridge, England, UK, 1989; ISBN 0-521-42397-X. [Google Scholar]
- Egger, G.J.; Binns, A.F.; Rossner, S.R. The Emergence of “Lifestyle Medicine” as a Structured Approach for Management of Chronic Disease. Med J Aust 2009, 190, 143–145. [Google Scholar] [CrossRef] [PubMed]
- Guthrie, G. Definition of Lifestyle Medicine. In Lifestyle Medicine, Third Edition; CRC Press: Boca Raton, FL, United States, 2019. [Google Scholar]
- Brigo, F.; Martini, M. Franz Tappeiner (1816-1902): The Physician Who Became Headhunter. Portrait of a Leading Figure in 19th Century Anthropology. J Med Biogr 2024, 32, 32–35. [Google Scholar] [CrossRef] [PubMed]
- Austrian Centre for Digital Humanities and Cultural Heritage. Tappeiner von Tappein, Franz Edler (1816–1902), Mediziner, Botaniker und Anthropologe. Available online: https://biographien.ac.at/ID-0.3914478-1 (accessed on 10 January 2026).
- Wandruszka, A.; Urbanitsch, P. “Die” Habsburgermonarchie 1848-1918: 6: Die Habsburgermonarchie Im System Der Internationalen Beziehungen; Verlag der Österreichischen Akademie der Wissenschaften, 1973; Vol. 2, ISBN 3-7001-2084-2. [Google Scholar]
- Judson, P.M. The Habsburg Empire: A New History; Harvard University Press: Cambridge, MA, United States, 2016; ISBN 0-674-96932-4. [Google Scholar]
- Okey, R. The Habsburg Monarchy: From Enlightenment to Eclipse; Macmillan Martins Press: New York, NY, USA, 2001. [Google Scholar]
- Köfler, W. Verwaltungsgeschichte Tirols. Available online: https://www.tirol.gv.at/fileadmin/themen/kunst-kultur/landesarchiv/downloads/verwaltungsgeschichte.PDF (accessed on 1 January 2026).
- Sellers, C. To Place or Not to Place: Toward an Environmental History of Modern Medicine. Bull Hist Med 2018, 92, 1–45. [Google Scholar] [CrossRef] [PubMed]
- Lupton, D. Immunities in the COVID Age: A Sociomaterial and More-than-Human Perspective. Soc Theory Health 2025, 23, 10. [Google Scholar] [CrossRef]
- Svarverud, R. Ventilation for the Nation: Fresh Air, Sunshine, and the Warfare on Germs in China’s National Quest for Hygienic Modernity, 1849-1949. Environ Hist 2020, 26, 307–329. [Google Scholar] [CrossRef]
- Morris, R.E. The Victorian ‘Change of Air’as Medical and Social Construction. J Tour Hist 2018, 10, 49–65. [Google Scholar] [CrossRef]
- French, A. Sites of Re-Enchantment: Sacred Space and Nature in Early 20th Century Europe. Religions 2022, 13, 110. [Google Scholar] [CrossRef]
- Savioz, A. The Arve Valley and Environmental Health: From Therapeutic Imagination to Eco-Anxiety. J Alp Res 2022, 110, 3. [Google Scholar] [CrossRef]
- Drakman, A. When Filth Became Dangerous: The Miasmatic and Contagionistic Origins of Nineteenth-Century Cleanliness Practices among Swedish Provincial Doctors. Med Hist 2025, 69, 22–38. [Google Scholar] [CrossRef]
- Worboys, M. Spreading Germs: Disease Theories and Medical Practice in Britain, 1865-1900; Cambridge University Press: Cambridge, England, UK, 2000; ISBN 0-521-77302-4. [Google Scholar]
- Sakalauskaitė-Juodeikienė, E. “Heroic” Medicine in Neurology: A Historical Perspective. Eur J Neurol 2024, 31, e16135. [Google Scholar] [CrossRef] [PubMed]
- Kasting, N.W. A Rationale for Centuries of Therapeutic Bloodletting: Antipyretic Therapy for Febrile Diseases. Perspect Biol Med 1990, 33, 509–516. [Google Scholar] [CrossRef] [PubMed]
- Orsini, D.; Cristina, M.L.; Spagnolo, A.M.; Minet, C.; Sartini, M.; Parrella, R.; Bragazzi, N.L.; Martini, M. Healthcare Settings and Infection Prevention: Today’s Procedures in Light of the “Instructions for Disinfection” Issued During the 1817 Typhus Epidemic in the Grand Duchy of Tuscany (Pre-Unification Italy). Epidemiologia (Basel) 2025, 6, 5. [Google Scholar] [CrossRef] [PubMed]
- Loconsole, M. Origins and Developments of Experimental Hygiene in Italy (1876–1899). Luigi Pagliani’s Contribution. Hist Eur Ideas 2025, 51, 820–846. [Google Scholar] [CrossRef]
- Poczai, P.; Karvalics, L.Z. The Little-Known History of Cleanliness and the Forgotten Pioneers of Handwashing. Front Public Health 2022, 10, 979464. [Google Scholar] [CrossRef]
- Schickore, J.; Schickore, J. Parasites, Pepsin, Pus, and Postulates: Jakob Henle’s Essay on Miasma, Contagium, and Miasmatic-Contagious Diseases in Its Original Contexts. Bull Hist Med 2022, 96, 612–638. [Google Scholar] [CrossRef]
- Matthews, R.A. The Origins of the Treatment of Uncertainty in Clinical Medicine. Part 1: Ancient Roots, Familiar Disputes. J R Soc Med 2020, 113, 193–196. [Google Scholar] [CrossRef]
- Fornaciari, A. Death in the Time of Pandemic: A Tuscan Cholera Cemetery at Benabbio (1855). Hist Arch 2023, 57, 1254–1268. [Google Scholar] [CrossRef]
- Scapoli, C.; Guidi, E.; Angelini, L.; Stefanati, A.; Gregorio, P. Sociomedical Indicators in the Cholera Epidemic in Ferrara of 1855. Eur J Epidemiol 2003, 18, 617–621. [Google Scholar] [CrossRef]
- Di Cimbrini, T.; Musella, A.M.; Corsi, C. Accounting for and of the Epidemic in Bologna in 1855: The Medicus-Politicus in the Papal States. Account Hist 2024, 29, 123–155. [Google Scholar] [CrossRef]
- Keber, K. Carniola’s Defense Mechanism for Protection against the First Cholera Epidemic in Europe. Kronika 2022, 70. [Google Scholar] [CrossRef]
- Promitzer, C. Vorwegnahme und Ernstfall: Emotionale Regime in den Jahren der zweiten Cholerapandemie am Beispiel Kärntens. Virus 2023, 22, 67–88. [Google Scholar] [CrossRef]
- Bratož, U. Med kugo in kolero: Karantenski ukrepi v severnem Jadranu. Kronika 2025, 73, 61–78. [Google Scholar] [CrossRef]
- Tappeiner, F. Einige Worte über die Cholera zur Belehrung und Beruhigung für das Landvolk; Eberle’sche Buchdruckerei: Bozen, 1855. [Google Scholar]
- Jimenez, J.L.; Marr, L.C.; Randall, K.; Ewing, E.T.; Tufekci, Z.; Greenhalgh, T.; Tellier, R.; Tang, J.W.; Li, Y.; Morawska, L. What Were the Historical Reasons for the Resistance to Recognizing Airborne Transmission during the COVID-19 Pandemic? Indoor Air 2022, 32, e13070. [Google Scholar] [CrossRef] [PubMed]
- Kinzelbach, A. Infection, Contagion, and Public Health in Late Medieval and Early Modern German Imperial Towns. J Hist Med Allied Sci 2006, 61, 369–389. [Google Scholar] [CrossRef]
- Armston-Sheret, E. Nourishing Food, Clean Air and Exercise: Medical Debates over Environment and Polar Hygiene on Robert Falcon Scott’s British National Antarctic Expedition, 1901-1904. Med Hist 2024, 68, 308–324. [Google Scholar] [CrossRef]
- Bretelle-Establet, F.; Gaille, M.; Katouzian-Safadi, M. Introduction. In Making Sense of Health, Disease, and the Environment in Cross-Cultural History: The Arabic-Islamic World, China, Europe, and North America; Bretelle-Establet, F., Gaille, M., Katouzian-Safadi, M., Eds.; Springer International Publishing: Cham, 2019; pp. 1–23. ISBN 978-3-030-19082-8. [Google Scholar]
- Iranzadasl, M.; Karimi, Y.; Moadeli, F.; Pasalar, M. Persian Medicine Recommendations for the Prevention of Pandemics Related to the Respiratory System: A Narrative Literature Review. Integr Med Res 2021, 10, 100483. [Google Scholar] [CrossRef]
- Tinková, D. Empirical Psychology and Dietetics of the Soul: Between Medicine and Philosophy. Cent Eur Cult 2024, 4, 41–71. [Google Scholar] [CrossRef]
- Drakman, A. When Filth Became Dangerous: The Miasmatic and Contagionistic Origins of Nineteenth-Century Cleanliness Practices among Swedish Provincial Doctors. Med Hist 2025, 69, 22–38. [Google Scholar] [CrossRef]
- Adera, N.G.; Ketema, B.; Girma, E. Effectiveness and Quality of Risk Communication Process in Ethiopia: The Case of Risk Communication during Cholera Outbreak in Addis Ababa, Ethiopia. PLoS One 2022, 17, e0265203. [Google Scholar] [CrossRef]
- Tutu, R.A.; Gupta, S.; Elavarthi, S.; Busingye, J.D.; Boateng, J.K. Exploring the Development of a Household Cholera-Focused Health Literacy Scale in James Town, Accra. J Infect Public Health 2019, 12, 62–69. [Google Scholar] [CrossRef]
- Nutbeam, D.; McGill, B.; Premkumar, P. Improving Health Literacy in Community Populations: A Review of Progress. Health Promot Int 2018, 33, 901–911. [Google Scholar] [CrossRef]
- Mohamed, M.G.; Dabou, E.A.A.; Abdelsamad, S.; Elsalous, S.H. Cholera Outbreaks: Public Health Implications, Economic Burden, and Preventive Strategies. AIMS Public Health 2025, 12, 767–795. [Google Scholar] [CrossRef] [PubMed]
- Budge, S.; Ambelu, A.; Bartram, J.; Brown, J.; Hutchings, P. Environmental Sanitation and the Evolution of Water, Sanitation and Hygiene. Bull World Health Organ 2022, 100, 286–288. [Google Scholar] [CrossRef] [PubMed]
- Gobena, D.; Gudina, E.K.; Fetensa, G.; Degfie, T.T.; Debela, T.; Tamiru, A.; Bayissa, Z.B.; Diriba, D.; Sarbessa, T.; Bekele, D.; et al. Risk Communication and Community Engagement (RCCE) Implementations to Control Cholera Outbreak in Oromia Region, Ethiopia. Trop Med Health 2025, 53, 4. [Google Scholar] [CrossRef] [PubMed]
- Ramírez, A.S.; Ramondt, S.; Van Bogart, K.; Perez-Zuniga, R. Public Awareness of Air Pollution and Health Threats: Challenges and Opportunities for Communication Strategies To Improve Environmental Health Literacy. J Health Commun 2019, 24, 75–83. [Google Scholar] [CrossRef]
- Qadeer, I. India’s COVID-19 Pandemic Experience: Lessons and the Way Forward. Vantage J Themat Anal 2021, 2, 6–21. [Google Scholar] [CrossRef]
- Reimer, H. Klimatische Winterkurorte mit besonderer Rücksicht auf die Winterstationen der Schweiz, Tirols, Oberitaliens und des südlichen Frankreichs: Ein Leitfaden für Aerzte u. Laien; Georg Reimer: Berlin, 1869; ISBN 978-3-11-125982-6. [Google Scholar]
- 51; Tappeiner, F. Die Klimato-Therapie der Lungenschwindsucht und Lungentuberkulose im Spiegel einer 30jährigen Betrachtung. Berl Klin Wochenschr 1874, 11, 546–547. [Google Scholar]
- Brigo, F.; Riccardi, N.; Martini, M. Franz Tappeiner (1816-1902) and His Pioneering Studies on Tuberculosis. Tuberculosis (Edinb) 2022, 132, 102160. [Google Scholar] [CrossRef]
- Tappeiner, F. Ueber eine neue Methode Tuberculose zu erzeugen. Arch Pathol Anat Physiol Klin Med 1878, 74, 393–400. [Google Scholar] [CrossRef]
- Hausmann, R. Entwicklungsgang und gegenwärtiger Stand der experimentellen Tuberkulose. Wien Med Presse 1883, 24, 51–53. [Google Scholar]
- Tappeiner, F. Zur Tuberkulosefrage: Offenes Schreiben an Herrn Dr. Arnold Spina. Wien Med Presse 1883, 24, 334–336. [Google Scholar]
- Tappeiner, F. Neue experimentelle Beiträge zur Inhalationstuberculose der Hunde. Arch Pathol Anat Physiol Klin Med 1880, 82, 353–359. [Google Scholar] [CrossRef]
- Tappeiner, F. Neue Methode, bei Tieren durch Einatmung frischer, zersteubter phtisischer Sputa allgemeine Miliartuberkulose zu Erzeugen; Amtlicher Bericht der 50; Versammlung deutscher Naturforscher und Ärzte: München, Deutschland, 1877. [Google Scholar]
- Sauggman, C. Zur Frage der Bedeutung der Tröpfcheninfektion für die Verbreitung der Tuberkulose. Z Tuberk Heilstattenwe 1904, 6, 125–139. [Google Scholar]
- Cardoso, C.L.; Giacomelli, L.R.B.; Helbel, C.; Sant’Ana, J.J.; Martins, F.M.; Barreto, A.M.W. Survival of Tubercle Bacilli in Heat-Fixed and Stained Sputum Smears. Mem. Inst. Oswaldo Cruz 2001, 96, 277–280. [Google Scholar] [CrossRef]
- Allen, B.W. Survival of Tubercle Bacilli in Heat-Fixed Sputum Smears. J Clin Pathol 1981, 34, 719–722. [Google Scholar] [CrossRef]
- Smithwick, R.W.; Stratigos, C.B.; David, H.L. Use of Cetylpyridinium Chloride and Sodium Chloride for the Decontamination of Sputum Specimens That Are Transported to the Laboratory for the Isolation of Mycobacterium Tuberculosis. J Clin Microbiol 1975, 1, 411–413. [Google Scholar] [CrossRef]
- Escombe, A.R.; Ticona, E.; Chávez-Pérez, V.; Espinoza, M.; Moore, D.A.J. Improving Natural Ventilation in Hospital Waiting and Consulting Rooms to Reduce Nosocomial Tuberculosis Transmission Risk in a Low Resource Setting. BMC Infect Dis 2019, 19, 88. [Google Scholar] [CrossRef]
- Deol, A.K.; Shaikh, N.; Middelkoop, K.; Mohlamonyane, M.; White, R.G.; McCreesh, N. Importance of Ventilation and Occupancy to Mycobacterium Tuberculosis Transmission Rates in Congregate Settings. BMC Public Health 2022, 22, 1772. [Google Scholar] [CrossRef]
- Banholzer, N.; Middelkoop, K.; Schmutz, R.; Leukes, J.; Zürcher, K.; Egger, M.; Wood, R.; Fenner, L. Infection Prevention and Control Measures during the COVID-19 Pandemic and Airborne Tuberculosis Transmission during Primary Care Visits in South Africa. Int J Infect Dis 2025, 156, 107921. [Google Scholar] [CrossRef]
- Turner, R.D.; Chiu, C.; Churchyard, G.J.; Esmail, H.; Lewinsohn, D.M.; Gandhi, N.R.; Fennelly, K.P. Tuberculosis Infectiousness and Host Susceptibility. J Infect Dis 2017, 216, S636–S643. [Google Scholar] [CrossRef]
- Gonzalez-Perez, O.; Ramos-Remus, C. The Importance of Physician Engagement in Medical Research. Front Med (Lausanne) 2025, 12, 1537023. [Google Scholar] [CrossRef] [PubMed]
- Worley, E.; Suh, E.H.; Abrukin, L.; DeFilippo, M.; Kamler, J.J.; Polavarapu, M.; Wyer, P.C. Harnessing Residents’ Practice-Based Inquiries to Enhance Research Literacy: The Thoughtful Reading of Evidence into Clinical Settings (T-RECS) Initiative. West J Emerg Med 2025, 26, 564–568. [Google Scholar] [CrossRef] [PubMed]
- Matheson, M.; Skinner, I.W.; Vehagen, A.; Auliffe, S.M.; Malliaras, P. Barriers and Enablers of Primary Healthcare Professionals in Health Research Engagement: A Systematic Review of Qualitative Studies. Nurs Health Sci 2025, 27, e70022. [Google Scholar] [CrossRef] [PubMed]
- Bhaskar, S.M.M. Medicine Meets Science: The Imperative of Scientific Research and Publishing for Physician-Scientists. Indian J Radiol Imaging 2025, 35, S9–S17. [Google Scholar] [CrossRef]
- Meraner Zeitung Dr. Franz Tappeiner. Meraner Zeitung 1896, 30, 1.
- Hetherington, H.W. The Diagnosis and Management of Latent, Suspected and Early Clinical Tuberculosis. JAMA 1937, 109, 1952. [Google Scholar] [CrossRef]
- Hunter, R.F.; Nieuwenhuijsen, M.; Fabian, C.; Murphy, N.; O’Hara, K.; Rappe, E.; Sallis, J.F.; Lambert, E.V.; Duenas, O.L.S.; Sugiyama, T.; et al. Advancing Urban Green and Blue Space Contributions to Public Health. Lancet Public Health 2023, 8, e735–e742. [Google Scholar] [CrossRef]
- Markevych, I.; Schoierer, J.; Hartig, T.; Chudnovsky, A.; Hystad, P.; Dzhambov, A.M.; de Vries, S.; Triguero-Mas, M.; Brauer, M.; Nieuwenhuijsen, M.J.; et al. Exploring Pathways Linking Greenspace to Health: Theoretical and Methodological Guidance. Environ Res 2017, 158, 301–317. [Google Scholar] [CrossRef]
- Wicki, B. The Main Task of Urban Public Health: Narrowing the Health Gap Between the Poor and the Rich. Int J Public Health 2022, 67, 1605084. [Google Scholar] [CrossRef]
- Hunter, R.F.; Cleland, C.; Cleary, A.; Droomers, M.; Wheeler, B.W.; Sinnett, D.; Nieuwenhuijsen, M.J.; Braubach, M. Environmental, Health, Wellbeing, Social and Equity Effects of Urban Green Space Interventions: A Meta-Narrative Evidence Synthesis. Environ Int 2019, 130, 104923. [Google Scholar] [CrossRef]
- Diener, A.; Mudu, P. How Can Vegetation Protect Us from Air Pollution? A Critical Review on Green Spaces’ Mitigation Abilities for Air-Borne Particles from a Public Health Perspective - with Implications for Urban Planning. Sci Total Environ 2021, 796, 148605. [Google Scholar] [CrossRef] [PubMed]
- Misiak, B.; Karska, J.; Kowalski, S.; Courtet, P.; Volpe, U.; Schouler-Ocak, M.; Destoop, M.; Adorjan, K.; Kraxner, F.; Buwalda, V.J.A.; et al. Urban Mental Health: A Position Paper of the European Psychiatric Association. Eur Psychiatry 2025, 68, e127. [Google Scholar] [CrossRef] [PubMed]
- Oertel, M.J. Ueber Terrain-Curorte zur Behandlung von Kranken mit Kreislaufs-Störungen, Kraftabnahme des Herzmuskels, ungenügenden Compensationen bei Herzfehlern, Fettherz und Fettsucht, Veränderungen im Lungenkreislauf etc. insbesondere als Winter-Stationen in Südtirol (Meran-Mais, Bozen-Gries, Arco) zur Orientirung für Aerzte und Kranke.; F.C.W. Vogel: Leipzig, Deutschland, 1886. [Google Scholar]
- Kornprobst, R. Dr. Bernhard Mazegger Senior und Junior — Wegbereiter für den Kurort Meran-Mais; Kleinode Merans; Heimatschutzverein Meran: Meran, 2025. [Google Scholar]
- Hausmann, R.; Mazegger, B., Jr. Erfahrungen über Terrain-Kuren in Meran-Mais. Meraner Zeitung 1889, 23, 3. [Google Scholar]
- Payer, P. Gehen im Grünen — Wohldosiert! Entstehung und Verbreitung von „Terrainkuren“. In Grün in der Stadt. Vom Hortus conclusus zum Urban gardening; Pühringer, A., Gräf, H.T., Eds.; StudienVerlag: Wien-Innsbruck, Österreich, 2023; pp. 343–362. [Google Scholar]
- Schuh, A.; Schnizer, W.; Dirnagl, K. Terrainkuren und ihre Grenzen. HeilbadKurort 1985, 126–127. [Google Scholar]
- Oja, P.; Kelly, P.; Murtagh, E.M.; Murphy, M.H.; Foster, C.; Titze, S. Effects of Frequency, Intensity, Duration and Volume of Walking Interventions on CVD Risk Factors: A Systematic Review and Meta-Regression Analysis of Randomised Controlled Trials among Inactive Healthy Adults. Br J Sports Med 2018, 52, 769–775. [Google Scholar] [CrossRef]
- Ungvari, Z.; Fazekas-Pongor, V.; Csiszar, A.; Kunutsor, S.K. The Multifaceted Benefits of Walking for Healthy Aging: From Blue Zones to Molecular Mechanisms. Geroscience 2023, 45, 3211–3239. [Google Scholar] [CrossRef]
- Dibben, G.O.; Faulkner, J.; Oldridge, N.; Rees, K.; Thompson, D.R.; Zwisler, A.-D.; Taylor, R.S. Exercise-Based Cardiac Rehabilitation for Coronary Heart Disease: A Meta-Analysis. Eur Heart J 2023, 44, 452–469. [Google Scholar] [CrossRef]
- Nagyova, I.; Jendrichovsky, M.; Kucinsky, R.; Lachytova, M.; Rus, V. Effects of Nordic Walking on Cardiovascular Performance and Quality of Life in Coronary Artery Disease. Eur J Phys Rehabil Med 2020, 56, 616–624. [Google Scholar] [CrossRef]
- Hu, Y.; Li, L.; Wang, T.; Liu, Y.; Zhan, X.; Han, S.; Huang, L. Comparison of Cardiac Rehabilitation (Exercise + Education), Exercise Only, and Usual Care for Patients with Coronary Artery Disease: A Non-Randomized Retrospective Analysis. Pharmacol Res Perspect 2021, 9, e00711. [Google Scholar] [CrossRef]
- Reed, J.L.; Terada, T.; Cotie, L.M.; Tulloch, H.E.; Leenen, F.H.; Mistura, M.; Hans, H.; Wang, H.-W.; Vidal-Almela, S.; Reid, R.D.; et al. The Effects of High-Intensity Interval Training, Nordic Walking and Moderate-to-Vigorous Intensity Continuous Training on Functional Capacity, Depression and Quality of Life in Patients with Coronary Artery Disease Enrolled in Cardiac Rehabilitation: A Randomized Controlled Trial (CRX Study). Prog Cardiovasc Dis 2022, 70, 73–83. [Google Scholar] [CrossRef]
- Son, W.-H.; Park, H.-T.; Jeon, B.H.; Ha, M.-S. Moderate Intensity Walking Exercises Reduce the Body Mass Index and Vascular Inflammatory Factors in Postmenopausal Women with Obesity: A Randomized Controlled Trial. Sci Rep 2023, 13, 20172. [Google Scholar] [CrossRef] [PubMed]
- Giovanelli, L.; Bernardelli, G.; Facchetti, S.; Malacarne, M.; Vandoni, M.; Carnevale Pellino, V.; Zuccotti, G.; Calcaterra, V.; Lucini, D. Metabolic Improvement after Exercise Training in Children with Obesity: Possible Role of the Six-Minute Walking Test. PLoS One 2025, 20, e0320209. [Google Scholar] [CrossRef] [PubMed]
- Sandsdal, R.M.; Juhl, C.R.; Jensen, S.B.K.; Lundgren, J.R.; Janus, C.; Blond, M.B.; Rosenkilde, M.; Bogh, A.F.; Gliemann, L.; Jensen, J.-E.B.; et al. Combination of Exercise and GLP-1 Receptor Agonist Treatment Reduces Severity of Metabolic Syndrome, Abdominal Obesity, and Inflammation: A Randomized Controlled Trial. Cardiovasc Diabetol 2023, 22, 41. [Google Scholar] [CrossRef] [PubMed]
- Murphy, M.; Nevill, A.; Neville, C.; Biddle, S.; Hardman, A. Accumulating Brisk Walking for Fitness, Cardiovascular Risk, and Psychological Health. Med Sci Sports Exerc 2002, 34, 1468–1474. [Google Scholar] [CrossRef]
- Limonti, F.; Gigliotti, A.; Cecere, L.; Varvaro, A.; Bosco, V.; Mazzotta, R.; Gravante, F.; Ramacciati, N. Evaluating the Efficacy and Impact of Home-Based Cardiac Telerehabilitation on Health-Related Quality of Life (HRQOL) in Patients Undergoing Percutaneous Coronary Intervention (PCI): A Systematic Review. J Clin Med 2025, 14, 4971. [Google Scholar] [CrossRef]
- Lee, Y.J.; Kwon, E.J.; Park, D.-I.; Park, S.H.; Hwang, S.W.; Ye, B.D. Effectiveness of an App-Based Walking Program for Obese Patients with Inflammatory Bowel Disease in Korea: A Single-Blind Parallel-Group Randomized Clinical Trial. BMC Gastroenterol 2025, 25, 417. [Google Scholar] [CrossRef]
- Droli, M.; Basan, L.; Vassallo, F.G. Positioning Climate Therapy Stays as a Health Tourism Product: An Evidence-Based Approach. Emerg Sci J 2022, 6, 256–272. [Google Scholar] [CrossRef]
- Romaszko-Wojtowicz, A.; Dragańska, E.; Doboszyńska, A.; Glińska-Lewczuk, K. Impact of Seasonal Biometeorological Conditions and Particulate Matter on Asthma and COPD Hospital Admissions. Sci Rep 2025, 15, 450. [Google Scholar] [CrossRef]
- Koskela, H.O.; Kaulamo, J.T.; Lätti, A.M. The Associations of Long-Term Temperature and Precipitation with Chronic Respiratory Symptoms: Projections for the Changing Climate. Lung 2024, 203, 7. [Google Scholar] [CrossRef]
- Li, D.; Dong, J.; Liu, X.; Ge, J.; Shu, J.; Zhu, L.; Bao, H. Exploring the Impact of Three Meteorological Factors and Their Specific Effect Sizes on Chronic Obstructive Pulmonary Disease Admission in Qingyang, China. Sci Rep 2025, 15, 24803. [Google Scholar] [CrossRef] [PubMed]
- Barber, B.V.; Kephart, G.; Martin-Misener, R.; Vallis, M.; Matthews, S.; Atkins, L.; Cassidy, C.; Curran, J.; Rainham, D. Integrating Health Geography and Behavioral Economic Principles to Strengthen Context-Specific Behavior Change Interventions. Transl Behav Med 2024, 14, 257–272. [Google Scholar] [CrossRef] [PubMed]
- Buckley, R.C.; Brough, P. Nature, Eco, and Adventure Therapies for Mental Health and Chronic Disease. Front Public Health 2017, 5, 220. [Google Scholar] [CrossRef] [PubMed]
- Nadal, I.P.; Angkurawaranon, C.; Singh, A.; Choksomngam, Y.; Sadana, V.; Kock, L.; Wattanapisit, A.; Wiwatkunupakarn, N.; Kinra, S. Effectiveness of Behaviour Change Techniques in Lifestyle Interventions for Non-Communicable Diseases: An Umbrella Review. BMC Public Health 2024, 24, 3082. [Google Scholar] [CrossRef]
- Paul, B.; Kirubakaran, R.; Isaac, R.; Dozier, M.; Grant, L.; Weller, D. RESPIRE Collaboration A Systematic Review of the Theory of Planned Behaviour Interventions for Chronic Diseases in Low Health-Literacy Settings. J Glob Health 2023, 13, 04079. [Google Scholar] [CrossRef]
- Unger, J.-P.; Morales, I.; De Paepe, P.; Roland, M. Integrating Clinical and Public Health Knowledge in Support of Joint Medical Practice. BMC Health Serv Res 2020, 20, 1073. [Google Scholar] [CrossRef]
- Essel, K.; Akselrod, H.; Batra, S.; Dawes, C.; Zaidi, Z.; Deyton, L. Training Socially Accountable Clinician-Citizens: Integrating Clinical Public Health Education in a Medical School Curriculum. Med Educ Online 2025, 30, 2469972. [Google Scholar] [CrossRef]
- Morrison, J.; Tumas, N.; Moreno Mattar, O.; Gutiérrez-Zamora Navarro, M.; Pericas, J.M.; Martínez Herrera, E.; Cash-Gibson, L.; Caroz Armayones, J.M.; Ruisoto, P.; Zografos, C.; et al. Bridging Sectors and Disciplines to Gain a Critical Understanding of the Eco-Social Determinants of Health Inequities: The ESDHI-EU Conference. Int J Soc Determinants Health Health Serv 2025, 55, 388–401. [Google Scholar] [CrossRef]
- Willetts, L. Environmental Defenders: Public Health Champions. Lancet Planet Health 2022, 6, e938–e940. [Google Scholar] [CrossRef]
- de Montigny, J.G.; Desjardins, S.; Bouchard, L. The Fundamentals of Cross-Sector Collaboration for Social Change to Promote Population Health. Glob Health Promot 2019, 26, 41–50. [Google Scholar] [CrossRef]
- Calancie, L.; Frerichs, L.; Davis, M.M.; Sullivan, E.; White, A.M.; Cilenti, D.; Corbie-Smith, G.; Hassmiller Lich, K. Consolidated Framework for Collaboration Research Derived from a Systematic Review of Theories, Models, Frameworks and Principles for Cross-Sector Collaboration. PLoS One 2021, 16, e0244501. [Google Scholar] [CrossRef]
- van Bommel, M.N.; Derkzen, M.L.; Vaandrager, L. Greening for Meaning: Sense of Place in Green Citizen Initiatives in the Netherlands. Wellbeing Space Soc 2025, 8, 100240. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |