Submitted:
01 January 2026
Posted:
04 January 2026
You are already at the latest version
Abstract
Keywords:
1. Introduction
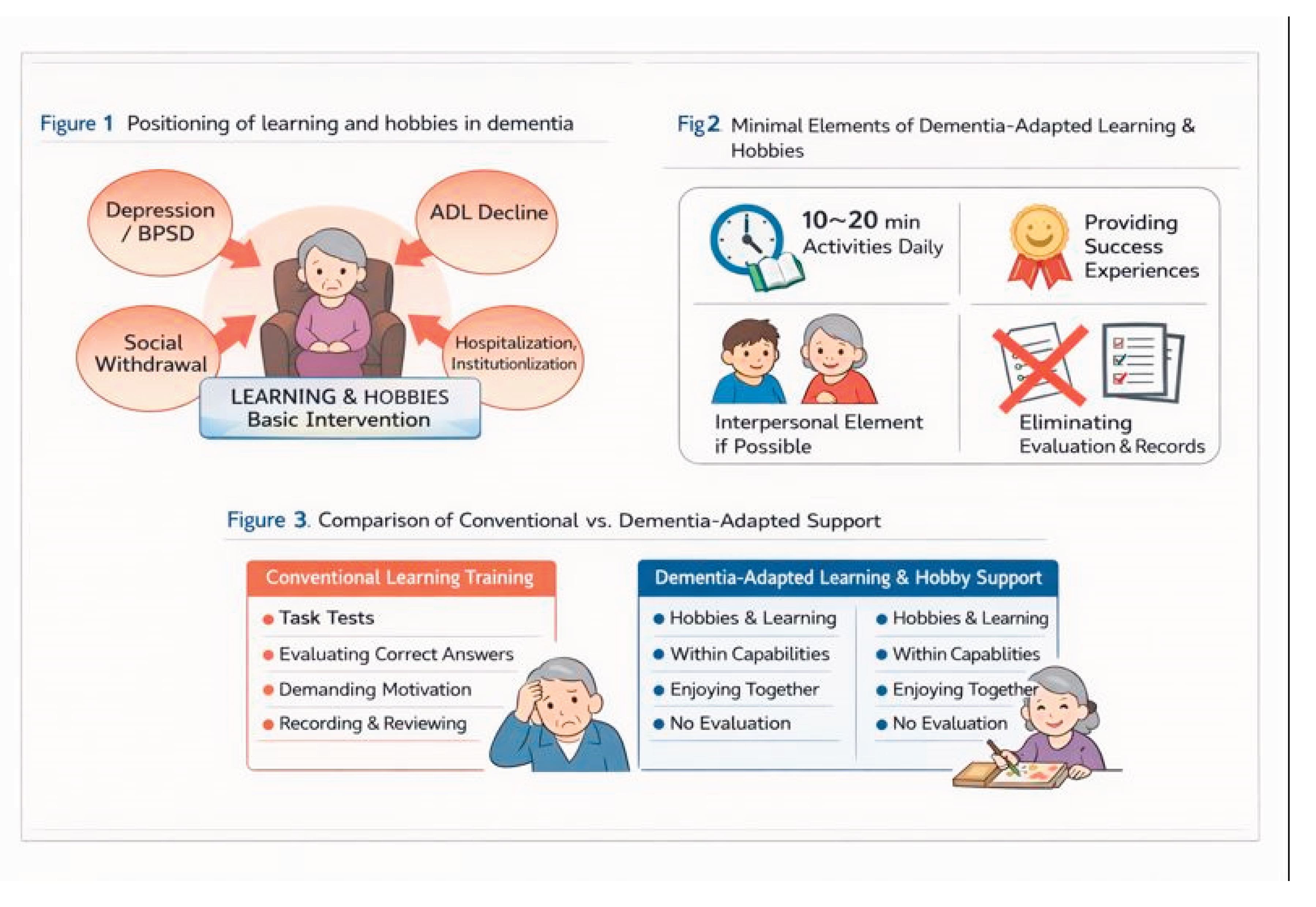
1.1. Redefining “Learning and Leisure Activities” in Dementia
1.2. Limitations of Conventional Cognitive Training and Learning Interventions
- (i)
- comprehension and memory;
- (ii)
- accurate task performance;
- (iii)
- continuous self-management; and
- (iv)
- tolerance for evaluation.
2. Constraints in Learning and Leisure Activity Interventions
2.1. Cognitive Constraints: Difficulties in Comprehension, Memory, and Self-Regulation
2.2. Emotional Constraints: Failure Experiences Trigger BPSD
2.3. Implementation Constraints: Care Burden and Daily Care Pathways
3. Distinguishing Active Ingredients from Excessive Burden
3.1. Core Active Ingredients
- Maintenance of engagement: Prevents fixation of disengagement and apathy
- Securing successful experiences (achievement/pleasure): Preserves reward systems and self-efficacy
- Addition of social context (interpersonal elements when feasible): Simultaneously promotes stimulation, arousal, and emotional stability
- Minimal repeatable units: Even short activities that can be performed “every day”
3.2. Excessive Implementation Burdens to Be Removed
- Evaluation of correct answers or achievement levels (test-like formats)
- Requiring motivation or sustained willingness from the person
- Complex rules or tasks requiring memory
- Decision-making burdens caused by offering multiple choices
- Obligatory recording, scoring, or reflection
4. Dementia-Adaptive Minimal Model of Learning and Leisure Activities
4.1. Minimal Component ①: 10–20 Minutes per Day of “Meaningful Activity” (Including Leisure)
- Leisure: coloring, origami, gardening, partial sewing tasks, arranging a shogi board, simple musical instruments, singing
- Roles: assisting with meal setup, folding towels, sorting, wiping, arranging
- Language: reading aloud, short read-aloud sessions, reminiscence using old photographs
- Sensory: keeping rhythm, hand and finger movements (focus on process rather than completion)
4.2. Minimal Component ②: Difficulty Set to Ensure Successful Experiences (“Leaning Toward Can-Do”)
- Early termination is acceptable; completion is not required
- Demonstrate and perform together rather than explaining verbally
- Do not correct mistakes; do not evaluate outcomes based on product quality
4.3. Minimal Component ③: Interpersonal Elements When Possible (One-to-One Is Sufficient)
4.4. Minimal Component ④: Removal of Evaluation and Self-Management Demands (Shifting Responsibility to the Environment)
5. Implementation Protocol (Summary)
- Frequency: Daily (short duration)
- Format: Same time, same place, same tools (predictability)
- Leader: Caregiver-led (does not assume user initiative)
- Recording: Simple ○/× check only (no evaluation)
6. Implications for Research, Practice, and Policy
7. Conclusion
Appendix
- disengagement
- apathy
- activity avoidance
- emotional instability
- behavioral and psychological symptoms of dementia (BPSD)
- care staff working in residential care facilities or home-care settings
- family caregivers supporting people with dementia
- medical and welfare professionals seeking to integrate learning and leisure activities into daily care without excessive burden
- This manual is not a clinical trial protocol, but an implementation guide for routine care.
- It does not claim therapeutic efficacy or cognitive improvement from learning or leisure activities.
- People with mild to moderate dementia
- Individuals who respond to simple verbal cues, imitation, or non-verbal guidance
- Individuals capable of engaging in short-duration activities in daily life
- Persistent severe agitation, refusal, or irritability that prevents safe implementation
- Marked exacerbation of BPSD triggered by activity-related stimulation
- Medically unstable conditions such as acute delirium, severe pain, or significant physical illness
- Final decisions should always prioritize clinical judgment.
- Even in advanced dementia, this program may be adaptively applied as presence-affirming activities when outcomes or responses are not demanded.
- Do not require comprehension, memory retention, or learning outcomes
- Do not evaluate correctness, completeness, or improvement
- Do not correct, instruct, compare, or reprimand
- Immediately reduce or stop the activity if anxiety, confusion, or refusal is observed
- Fix activity content, timing, and procedures as much as possible
- Avoid framing activities as special events
- Do not assume motivation, judgment, or self-management by the person
- Consider support successful even if the person does not actively “participate”
- Learning and leisure activities: daily, 10–20 minutes
- Interpersonal interaction (when feasible): short one-to-one engagement
- Verbal prompting and initiation: embedded within routine daily care
- Familiar living environments
- Quiet settings that avoid excessive stimulation
- Minimal preparation, movement, and choice requirements
- Prevent fixation of disengagement and apathy
- Maintain daytime activity levels and emotional stability
- Fix activities that the individual has previously enjoyed or resists least
- Do not require completion, understanding, or measurable outcomes
- Leisure: coloring, origami, knitting, gardening (watering only), singing
- Learning-like activities: reading aloud, short read-aloud sessions, simple calculation-like tasks
- Role-based activities: folding towels, sorting, arranging, wiping
- “Let’s try this together for a little while.”
- “It’s okay to stop at any time.”
- Prevent refusal or BPSD triggered by failure experiences
- Reduce difficulty to a clearly achievable level
- Treat incomplete or partial engagement as success
- Correcting mistakes
- Referring to improvement or performance outcomes
- Support attention, arousal, and emotional stability
- Engage together in a one-to-one format
- Emphasize parallel or supportive presence
- Do not force group participation
- Do not check whether the person remembers or understands
- Cognitive training or test-like learning formats
- Interventions that evaluate correctness, achievement, or outcomes
- Persuasive approaches aimed at eliciting motivation or willingness
- Interactions requiring decision-making through choice presentation
- This is not an exclusion of learning stimuli per se, but a restructuring of format.
- This manual does not constitute an intervention study designed to quantitatively verify the effectiveness of a specific learning program.
- Its primary aim is to present an implementation framework adapted to the cognitive and emotional constraints of dementia, based on existing theoretical, review, and implementation studies.
- Duration (shortening is acceptable)
- Activity content (simplification)
- Amount of interpersonal stimulation
- Clear anxiety, refusal, or agitation
- Increased fatigue or confusion
- Signs of BPSD exacerbation
- Physical risks are extremely low
- The greatest risk is accumulation of failure experiences
- Do not demand perfect implementation or consistent success
- 9. Consistency with Existing Evidence
- Associations between apathy, reduced activity, and functional decline
- Findings on apathy reduction through non-pharmacological interventions
- Relationships between social engagement and cognitive or functional decline
- Supplementary material describing intervention content
- Documentation of implementation methods and fidelity
- Simplified manuals for care staff
- Guides for family caregivers
- Shared reference materials for care policy discussions
References
- Brodaty, H.; Burns, K. Nonpharmacological management of apathy in dementia: A systematic review. American Journal of Geriatric Psychiatry 2012, 20(7), 549–564. [Google Scholar] [CrossRef] [PubMed]
- Desai, R.; Leung, W. G.; Fearn, C.; John, A.; Stott, J.; Spector, A. Effectiveness of cognitive stimulation therapy (CST) for mild to moderate dementia: A systematic review and meta-analysis. Ageing Research Reviews 97 2024, 102312. [Google Scholar] [CrossRef] [PubMed]
- Fratiglioni, L.; Paillard-Borg, S.; Winblad, B. An active and socially integrated lifestyle in late life might protect against dementia. The Lancet Neurology 2004, 3(6), 343–353. [Google Scholar] [CrossRef] [PubMed]
- Kuiper, J. S.; Zuidersma, M.; Oude Voshaar, R. C.; et al. Social relationships and cognitive decline: A systematic review and meta-analysis. Ageing Research Reviews 22 2015, 39–57. [Google Scholar] [CrossRef] [PubMed]
- Robert, P.; Onyike, C. U.; Leentjens, A. F.; Dujardin, K.; Aalten, P.; Starkstein, S.; et al. Proposed diagnostic criteria for apathy in Alzheimer’s disease and other neuropsychiatric disorders. European Psychiatry 2009, 24(2), 98–104. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2026 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




