1. Introduction
Urinary incontinence (UI) is a prevalent condition that significantly impairs women’s quality of life by disrupting daily activities, social participation, and emotional well-being. Stress urinary incontinence (SUI), the most common subtype, typically results from pelvic floor weakness and urethral hypermobility, leading to involuntary urine leakage during physical exertion, coughing, or sneezing. When conservative approaches, such as pelvic floor muscle training or behavioral therapy, fail, surgical intervention becomes the preferred treatment option.[
1,
2,
3]
Over the past two decades, mid-urethral sling (MUS) procedures have become the gold standard for managing SUI, owing to their proven long-term efficacy and relatively low morbidity.[
4,
5,
6] However, ongoing concerns remain regarding mesh-related complications such as erosion, chronic pelvic pain, and voiding dysfunction, which may necessitate surgical revision.[
7] These complications have prompted both patients and surgeons to seek safer, less invasive alternatives.
The single-incision mini-sling (SIMS) procedure was developed to minimize tissue dissection and reduce the risk of complications while maintaining continence outcomes comparable to traditional MUS techniques. A multicenter randomized controlled trial reported that mini-slings provided non-inferior subjective success rates and comparable safety outcomes to standard midurethral slings.[
8] Furthermore, a recent meta-analysis confirmed that mini-slings were associated with shorter operative time, less postoperative pain, and similar efficacy, suggesting they may be a viable minimally invasive alternative.[
9]
Despite these advantages, mesh erosion and exposure remain significant postoperative concerns, with incidence rates varying widely depending on surgical technique, mesh material, and postoperative care.[
10] As such, real-world data assessing mini-sling outcomes in diverse clinical settings are valuable for better defining their overall risk–benefit profile.
In this context, the present retrospective study aimed to evaluate the outcomes of the mini-sling procedure in patients with urinary incontinence, focusing on objective parameters (mesh erosion rate, healing time, postoperative cough and pad tests) and subjective outcomes (patient satisfaction). By analyzing real-world data from a large patient cohort, this study aims to provide additional evidence regarding the safety and effectiveness of mini-sling surgery in contemporary clinical practice.
2. Materials and Methods
2.1. Study Design
This retrospective cohort study included 186 patients who underwent mini-sling surgery for urinary incontinence (UI) between January 2019 and January 2024. The analysis focused on mesh erosion, erosion healing time, preoperative and 6-month postoperative cough stress test and pad test results, and patient satisfaction scores. Patient satisfaction was rated on a 1–5 Likert scale, with 5 indicating the highest level of satisfaction. This study design enabled a comprehensive evaluation of both objective and patient-reported clinical outcomes associated with the mini-sling procedure.
The inclusion criteria comprised female patients aged over 18 years who underwent elective mini-sling surgery for urinary incontinence and had complete medical records available. Patients with incomplete or missing data in their electronic medical records were excluded from the study.
2.2. Data Collection
Demographic characteristics, duration and type of UI, and obstetric history were recorded. Clinical data included preoperative cough stress test and pad test results, 6-month postoperative cough and pad test outcomes, and patient satisfaction scores (1–5 scale, with 5 representing the highest satisfaction). Information on postoperative management, including the use of estriol cream, was also documented. Surgical complications—such as mesh erosion, reoperation rates, and erosion healing time—were evaluated through postoperative follow-up visits. All data were retrieved from electronic medical records and patient charts to ensure completeness and accuracy.
2.3. Follow-Up and Patient Report Outcomes
All postoperative evaluations at the 6-month follow-up were performed prospectively as part of the clinic’s routine postoperative assessment protocol. This included both objective outcome measures—such as the cough stress test and pad test—and patient-reported satisfaction. Objective tests were repeated at the scheduled 6-month visit, and patient satisfaction was recorded using a standardized 1–5 Likert scale (with 5 indicating the highest satisfaction). This structured and routine prospective follow-up ensured consistent measurement of both objective clinical outcomes and subjective patient-reported experiences, despite the overall retrospective design of the study.
2.4. Statistical Analyses and Tools
All statistical analyses were performed using Wistats v3.0 (WisdomEra Corp., Istanbul, Turkey), which integrates Python-based statistical and machine learning libraries. Descriptive statistics were used to summarize demographic and clinical data. Categorical variables were expressed as frequencies and percentages, whereas continuous variables were reported as mean values.
3. Results
Detailed descriptive statistics for the mini-sling procedure are presented in
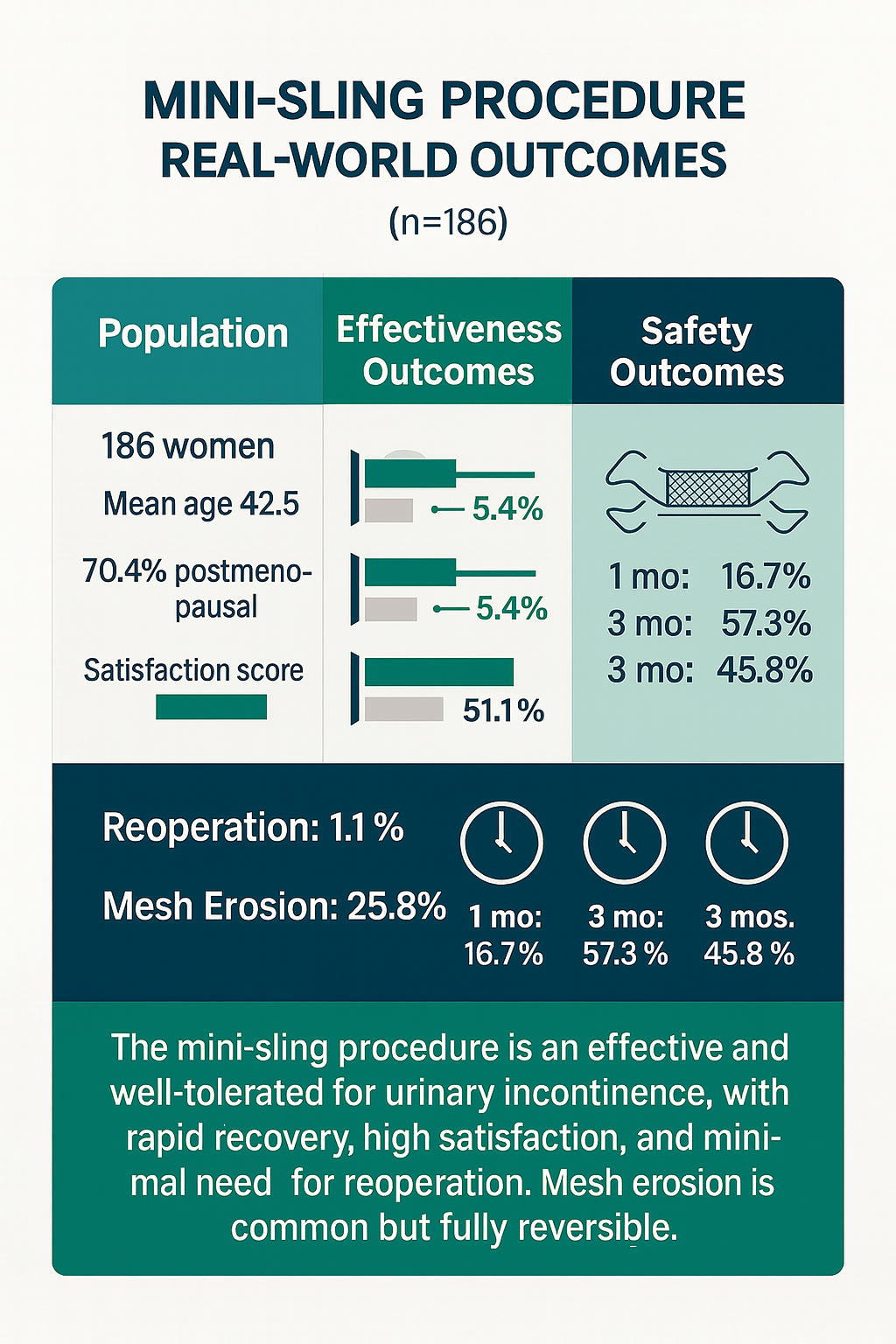
Table 1. The mean age of the patients was 42.5 years (range: 28–44), and the mean duration of the procedure was 18.1 minutes (range: 14–22). Most patients were postmenopausal (70.4%), and over half (58.1%) had urinary incontinence for more than five years. Stress urinary incontinence was the predominant type, observed in 83.9% of the cohort. Baseline demographic and clinical characteristics are summarized visually in
Figure 1.
Preoperative test results and postoperative clinical outcomes are presented in
Table 2. The cough stress test and preoperative pad test were positive in all patients. At the 6-month follow-up, postoperative urinary incontinence scores demonstrated a significant improvement. The rate of positive pad tests decreased from 100% preoperatively to 5.4% postoperatively, and nearly identical improvement was observed in cough stress test results. Detailed objective cure outcomes and postoperative complications are illustrated in
Figure 2.
Nearly all patients (96.8%) had a history of vaginal delivery. Mesh erosion occurred in 25.8% of patients; however, all cases healed completely within three months, with reoperation required in only two patients (1.1%). At the 6-month evaluation, 63.4% of patients reported the highest satisfaction score. Healing trajectories and patient-reported satisfaction outcomes are shown in
Figure 3.
4. Discussion
This study provides valuable real-world evidence on the clinical outcomes of the mini-sling procedure in patients with urinary incontinence. The analysis of 186 patients demonstrated that the mini-sling approach yields high efficacy and patient satisfaction with an acceptable safety profile. Although the overall design was retrospective, routine prospective 6-month follow-up strengthened the reliability of objective and patient-reported outcomes. At the 6-month follow-up, 63.4% of patients reported the highest satisfaction score, while the positive pad test rate decreased dramatically from 100% preoperatively to 5.4% postoperatively. Although mesh erosion occurred in 25.8% of cases, all instances resolved completely within three months. These findings highlight that the mini-sling represents an effective and well-tolerated treatment option for urinary incontinence, contributing meaningful evidence to the ongoing discussion on less invasive sling techniques.
The favorable results of our study are consistent with previous reports evaluating mini-sling outcomes. Abdel-Fattah et al. demonstrated that mini-sling surgery was non-inferior to the standard mid-urethral sling (SMUS) in patient-reported success after 15 months of follow-up.[
11] Similarly, the U.S. Food and Drug Administration’s summary of 36-month outcomes confirmed that mini-sling systems exhibit comparable efficacy and adverse event profiles to conventional mid-urethral slings.[
12] Zhou et al. reported in a recent meta-analysis that single-incision mini-sling (SIMS) procedures achieve objective cure rates similar to SMUS, while offering shorter operative times and fewer intraoperative complications.[
9] Our findings of high patient satisfaction and marked reduction in incontinence symptoms are further supported by long-term studies. In a 10-year follow-up of the Altis® single-incision sling, 75.4% of patients achieved complete continence and 84.6% reported significant improvement in quality of life.[
13] Similarly, in a 4–7-year evaluation of a surgeon-tailored mini-sling, objective cure rates exceeded 90% at the final follow-up, demonstrating sustained long-term efficacy.[
14] These data suggest that the improvements seen in our 6-month results are likely to remain stable over time with appropriate patient selection and follow-up.
The mesh erosion rate in our study (25.8%) appears higher than in other reports, where erosion or exposure rates typically range between 3% and 12%. For example, the Altis® series reported only 3.2% mesh erosion over an average of 85 months[
13], while the Ophira sling study reported erosion in 11.3% of patients at a mean follow-up of 30 months.[
15] In contrast, our short-term erosion cases all resolved within three months, underscoring the importance of early detection and conservative management. Differences in device design, mesh material, surgical technique, patient estrogen status, and vaginal delivery history may account for the differing erosion rates reported across studies. Long-term registry data also provide a broader safety perspective. Funk et al. reported a 3.7% sling revision/removal rate over nine years, with 60% of revisions due to mesh erosion [
16], while Dejene et al. found a 15-year revision rate of 7.9%.[
17] These long-term data emphasize that although erosion is a known complication, its impact can be minimized through careful surgical technique and close follow-up. In a comprehensive meta-analysis comparing SIMS and MUS, single-incision mini-slings were found to be non-inferior regarding objective cure rates, with shorter operative times and similar rates of complications such as urgency or pain.[
18] The NEJM randomized controlled trial further confirmed this non-inferiority in both short- and medium-term follow-up.[
11] Collectively, these findings reinforce that the mini-sling procedure achieves comparable functional outcomes to traditional mid-urethral slings, while potentially reducing operative invasiveness and recovery time.
From a clinical standpoint, the substantial improvement in objective continence measures and high patient satisfaction observed in this cohort supports the mini-sling as a practical minimally invasive option for women seeking surgical treatment for stress urinary incontinence. The minimal dissection required may be advantageous for patients aiming for faster postoperative recovery or those with comorbidities that increase surgical risk. Furthermore, the complete resolution of all mesh erosions within three months highlights the importance of structured early follow-up and suggests that many short-term complications can be effectively managed without reoperation. For clinicians, these findings reinforce that appropriate patient selection—considering factors such as estrogen status, parity, and tissue quality—combined with standardized postoperative care may optimize outcomes and minimize complications. Overall, the mini-sling technique fits well within contemporary trends favoring reduced invasiveness while maintaining high therapeutic efficacy.
This study has several limitations that should be acknowledged. First, its retrospective design may introduce selection and information bias, particularly in the reporting of complications and follow-up data. Second, the 6-month follow-up period limits the assessment of long-term efficacy, recurrence, or delayed complications. Third, the absence of a control group—such as patients undergoing SMUS procedures—prevents direct comparative interpretation. Fourth, details on the management of mesh erosions (e.g., surgical vs. conservative approaches) were not systematically analyzed. Lastly, patient heterogeneity in demographic and clinical variables (e.g., Body Mass Index, menopausal status, parity) could have influenced outcomes but was not examined through subgroup analysis.
5. Conclusions
In conclusion, the mini-sling procedure appears to be a promising and well-tolerated minimally invasive approach for the treatment of urinary incontinence. The marked improvement in pad test results, high patient satisfaction, and minimal need for reoperation support its clinical utility. Although mesh erosion was relatively frequent, complete healing within three months suggests that the complication is manageable with proper postoperative care. These findings are in line with large randomized and meta-analytic studies demonstrating comparable outcomes to traditional sling procedures, supporting the mini-sling as a reliable alternative for appropriately selected patients. Nevertheless, future multicenter prospective studies with longer follow-up and comparative designs are warranted to validate these findings and identify predictors of long-term success and complications.
Author Contributions
Conceptualization, İÖ and AÖ; Methodology, İÖ and AÖ; Investigation, İÖ and AÖ; Resources, İÖ and AÖ; Data Curation, İÖ and AÖ; Writing – Original Draft Preparation, İÖ; Writing – Review & Editing, İÖ and AÖ; Visualization, İÖ; Supervision, İÖ;.
Funding
None of the authors has any potential financial conflict of interest related to this manuscript.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board (or Ethics Committee) of Beykoz State Hospital (protocol code BEYKOZ DH 54 and 2022-08-09). Ethical review and approval were waived for this study due to its retrospective design and the use of anonymized data collected as part of routine clinical care, in accordance with institutional policies and national regulations.
Informed Consent Statement
Not applicable.
Data Availability Statement
The dataset generated and analyzed in this study is publicly available on the Istinye University Dataset Sharing Platform. Anonymized data can be accessed at the following link:
https://dataset.istinye.edu.tr/dataset?did=58. All data were fully anonymized in accordance with ethical regulations. Access is provided for research purposes through a controlled-access system under the platform’s standard licensing and data-sharing policies.
Acknowledgments
We would like to thank the Artificial Intelligence Research And Application Center of Istinye University (
https://yzaum.istinye.edu.tr/) for their support in the technical assessment of the manuscript, including verification of data integrity and plagiarism screening prior to submission. We also extend our appreciation to the Ditako Data Analytics Team (
https://ditako.com) for providing professional data analytics services that contributed to the robustness of the results.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
| UI |
Urinary Incontinence |
| SUI |
Stress urinary incontinence |
| MUS |
Mid-urethral sling |
| SMUS |
Standard mid-urethral sling |
| SIMS |
Single-incision mini-sling |
| FDA |
U.S. Food and Drug Administration |
References
- Richter, H.E.; Albo, M.E.; Zyczynski, H.M.; Kenton, K.; Norton, P.A.; Sirls, L.T.; Kraus, S.R.; Chai, T.C.; Lemack, G.E.; Dandreo, K.J.; et al. Retropubic versus Transobturator Midurethral Slings for Stress Incontinence. N. Engl. J. Med. 2010, 362, 2066–2076. [CrossRef]
- Labrie, J.; Fischer, K.; van der Vaart, C.H. Health-Related Quality of Life. The Effect of Pelvic Floor Muscle Training and Midurethral Sling Surgery: A Systematic Review. Int. Urogynecology J. 2012, 23, 1155–1162. [CrossRef]
- Pandey, D.; Maturi, C.; Dhakar, B.P.S.; Jain, G.; Kyalakond, K. Interventions and Quality of Life in Stress Urinary Incontinence. Gynecol. Minim. Invasive Ther. 2019, 8, 106–112. [CrossRef]
- Dejene, S.Z.; Funk, M.J.; Pate, V.; Wu, J.M. Long-Term Outcomes After Midurethral Mesh Sling Surgery for Stress Urinary Incontinence. Female Pelvic Med. Reconstr. Surg. 2022, 28, 188–193. [CrossRef]
- Tommaselli, G.A.; Di Carlo, C.; Formisano, C.; Fabozzi, A.; Nappi, C. Medium-Term and Long-Term Outcomes Following Placement of Midurethral Slings for Stress Urinary Incontinence: A Systematic Review and Metaanalysis. Int. Urogynecology J. 2015, 26, 1253–1268. [CrossRef]
- Valadez, L.; Frilot, C.F.; Gomelsky, A. Long-Term Outcomes of Transobturator Midurethral Slings: A Critical Evaluation of a Real-World Population. Neurourol. Urodyn. 2020, 39, 2463–2470. [CrossRef]
- Farag, F.; Osman, N.I.; Pang, K.H.; Castro-Diaz, D.; Chapple, C.R.; Cruz, F.; Gamé, X.; Goldman, H.; Greenwell, T.; Hampel, C.; et al. Complications of Synthetic Midurethral Slings: Is There a Relevant Discrepancy Between Observational Data and Clinical Trials? Eur. Urol. Focus 2024, 10, 535–550. [CrossRef]
- Abdel-Fattah, M.; Cooper, D.; Davidson, T.; Kilonzo, M.; Boyers, D.; Bhal, K.; McDonald, A.; Wardle, J.; N’Dow, J.; MacLennan, G.; et al. Single-Incision Mini-Slings versus Standard Synthetic Mid-Urethral Slings for Surgical Treatment of Stress Urinary Incontinence in Women: The SIMS RCT. Health Technol. Assess. Winch. Engl. 2022, 26, 1–190. [CrossRef]
- Zhou, Y.; Chai, Y.; Zhang, Y.; Zhou, Z. Application of Single-Incision Mini-Sling Surgery versus Standard Mid-Urethral Sling Surgery in Female Stress Urinary Incontinence: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Int. J. Surg. Lond. Engl. 2025, 111, 5518–5534. [CrossRef]
- Bueno Garcia Reyes, P.; Hashim, H. Mesh Complications: Best Practice in Diagnosis and Treatment. Ther. Adv. Urol. 2020, 12, 1756287220942993. [CrossRef]
- Abdel-Fattah, M.; Cooper, D.; Davidson, T.; Kilonzo, M.; Hossain, M.; Boyers, D.; Bhal, K.; Wardle, J.; N’Dow, J.; MacLennan, G.; et al. Single-Incision Mini-Slings for Stress Urinary Incontinence in Women. N. Engl. J. Med. 2022, 386, 1230–1243. [CrossRef]
- Health, C. for D. and R. Stress Urinary Incontinence: Surgical Mesh Considerations and Recommendations. FDA 2024.
- Quintana Franco, L.M.; González López, R.; Garde García, H.; De Palacio Fraguas, A.; González Enguita, C. Long-Term Outcomes of the Altis® Single-Incision Sling: Up to 10 Years’ Follow-Up. Int. Urogynecology J. 2024, 35, 1021–1026. [CrossRef]
- Uysal, D.; Güven, C.M.; Akgün Kavurmaci, S.; Sivaslioğlu, A.A. Long-Term Efficacy of the Single-Incision Mini-Sling Procedure Using Surgeon-Tailored Mesh. Eur. J. Obstet. Gynecol. Reprod. Biol. 2023, 287, 59–62. [CrossRef]
- Golbasi, C.; Taner, C.E.; Golbasi, H. Long-Term Outcomes and Quality of Life Effects of Single Incision Mini Sling Procedure in Stress Urinary Incontinence Patients. Eur. J. Obstet. Gynecol. Reprod. Biol. 2019, 234, 10–13. [CrossRef]
- Funk, M.J.; Siddiqui, N.Y.; Pate, V.; Amundsen, C.L.; Wu, J.M. Sling Revision/Removal for Mesh Erosion and Urinary Retention: Long-Term Risk and Predictors. Am. J. Obstet. Gynecol. 2013, 208, 73.e1-73.e7. [CrossRef]
- DEJENE, S.Z.; FUNK, M.J.; PATE, V.; WU, J.M. Long-Term Outcomes Following Midurethral Mesh Sling Surgery for Stress Urinary Incontinence. Female Pelvic Med. Reconstr. Surg. 2022, 28, 188–193. [CrossRef]
- Patel, T.; Sugandh, F.; Bai, S.; Varrassi, G.; Devi, A.; Khatri, M.; Kumar, S.; Dembra, D.; Dahri, S. Single Incision Mini-Sling Versus Mid-Urethral Sling (Transobturator/Retropubic) in Females With Stress Urinary Incontinence: A Systematic Review and Meta-Analysis. Cureus 2023, 15, e37773. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).