1. Introduction
Wireless sensor networks (WSNs) have emerged as a critical technology for healthcare patient monitoring, enabling continuous, real-time data collection from patients in clinical and remote settings [
1]. These networks consist of spatially distributed sensor nodes that collect physiological data, process information locally, and transmit results to healthcare providers through wireless communication protocols [
2]. The deployment of WSNs in healthcare applications addresses several key challenges including reducing hospitalization costs, enabling early medical intervention, and supporting remote patient care [
3].
Healthcare WSN applications span from monitoring vital signs in hospital environments to supporting chronic disease management in home-based care settings [
4]. These systems facilitate real-time collection of physiological parameters including heart rate, blood pressure, temperature, and oxygen saturation, enabling healthcare providers to make informed decisions based on continuous patient data [
5]. However, the primary constraint in healthcare WSN deployment is energy efficiency, as sensor nodes typically operate on limited battery power while requiring extended operational periods [
6].
Healthcare WSN sensor nodes operate under strict energy constraints due to battery limitations, directly impacting operational lifetime and monitoring effectiveness [
7]. The fundamental challenge lies in optimizing energy consumption while maintaining comprehensive patient coverage and data reliability [
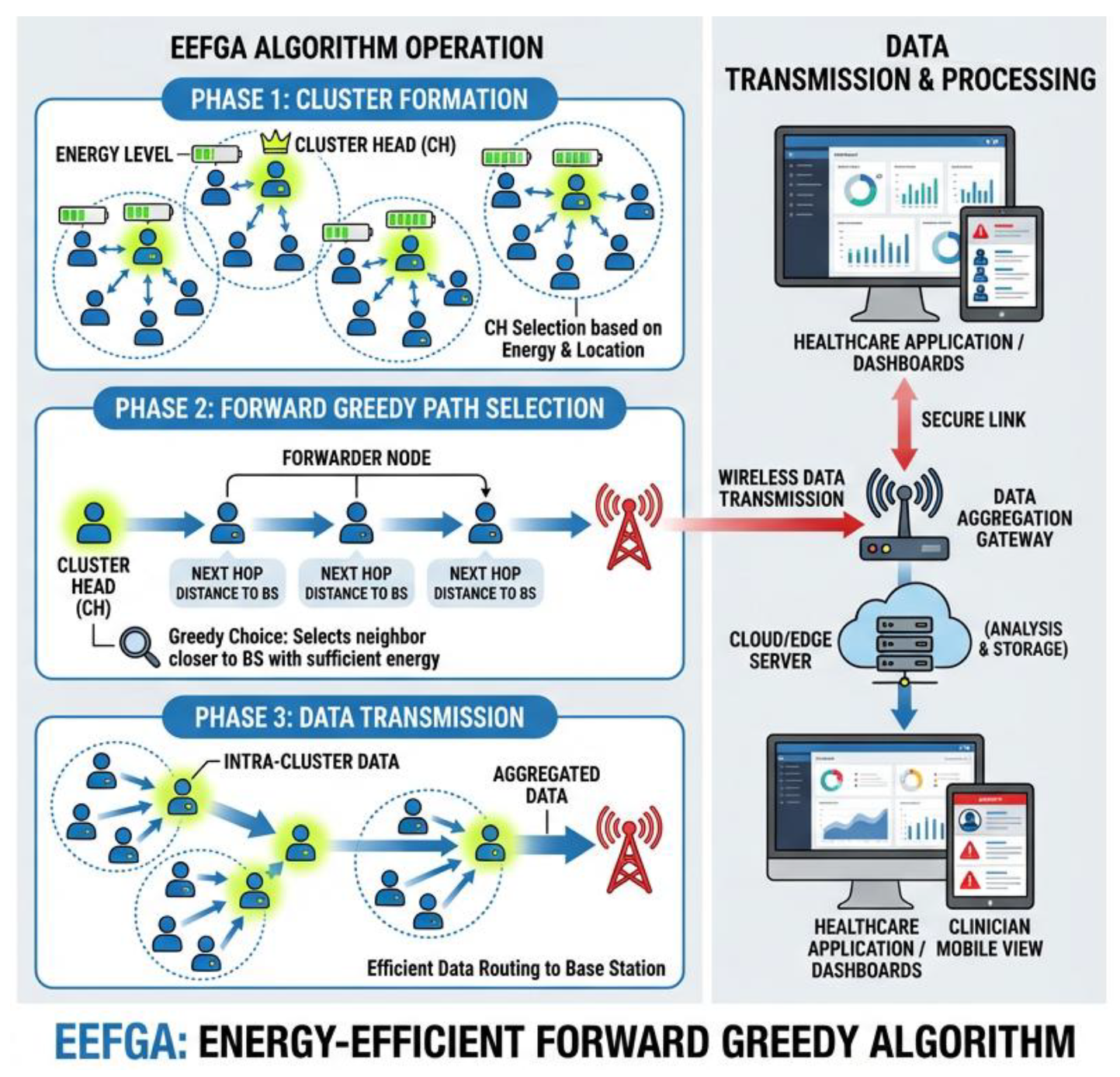
8]. This research addresses the sensor node selection problem by proposing an Energy-Efficient Forward Greedy Algorithm (EEFGA) that balances energy efficiency with monitoring quality through systematic node selection strategies.
The Wireless Sensor Networks (WSNs) used in healthcare applications are optimized using the Energy-Efficient Forward Greedy Algorithm (EEFGA). Its main objective is to improve these networks' energy efficiency, which is crucial in healthcare settings where sensor nodes must run constantly for extended periods of time. To reduce energy usage and meet the needs of healthcare monitoring, EEFGA uses a greedy strategy, making locally optimum decisions at each stage. Data aggregation, dynamic sleep scheduling, adaptive data rate modulation, and improved routing pathways are some important energy-saving techniques. These methods guarantee effective resource use while maintaining quick and reliable healthcare data delivery, which is crucial in medical applications. Using simulations and actual deployments, the efficacy of EEFGA is assessed with an emphasis on criteria like energy usage, data dependability, and network longevity. EEFGA's scalability makes it even more suitable for healthcare settings because it can accommodate different network sizes and sensor node densities to reduce energy consumption and provide ongoing patient monitoring.
Related Work
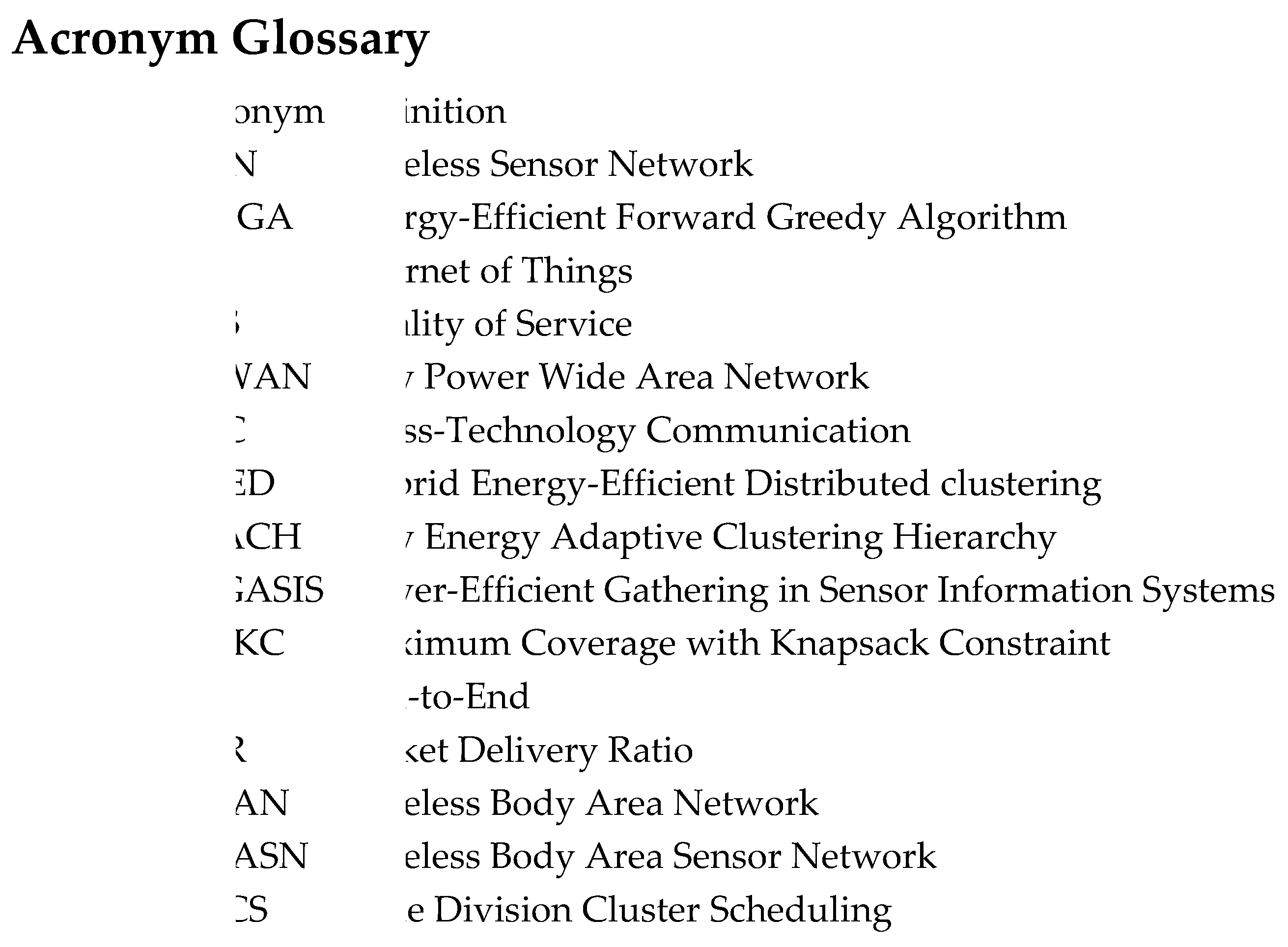
Energy-efficient sensor node selection in healthcare WSNs has been extensively studied with various algorithmic approaches. This section reviews existing work in three key areas: energy optimization strategies, healthcare-specific WSN protocols, and greedy algorithm applications in sensor networks.
Due to their capacity to deliver quick and affordable solutions, [
1] highlight the potential uses of Wireless Sensor Networks (WSN) in a variety of sectors, particularly in medical monitoring. The main objective is to use WSN to track vital health indicators including body temperature, blood pressure, heart rate, and oxygen saturation, enabling prompt intervention when required. Wearable sensors (nodes) are deployed throughout patients' bodies as part of the WSN for medical applications. These sensors are used to take precise measurements. To gather and communicate data to medical specialists for diagnosis, these gadgets cooperate. They investigate how a medical wireless sensor network behaves while all nodes (patients) are moving about. The authors suggest the usage of a use of a multipoint relay protocol to enhance network performance.
In a different study, a home healthcare monitoring system is introduced for elderly and chronic patients. It uses fabric-covered wearable sensors to gather real-time health information that is then wirelessly sent to mobile devices. Three application scenarios are provided by the system, with an emphasis on effective group-based data gathering and transmission for outpatient healthcare. It also addresses issues with wireless data transfer security. To demonstrate the effectiveness of the system, a monitoring application prototype is provided. With wearable sensors and a wireless network, this study demonstrates a viable method for continuous healthcare monitoring in residential settings [
3]. This method offers timely data for better patient care.
In [
4], the Mobility-supporting Adaptive Threshold-based Thermal-aware Energy-efficient Multi-hop ProTocol (M-ATTEMPT) and the proposed DARE protocol are contrasted. According to simulation studies, DARE is more effective at extending network lifetime and lowering energy usage than M-ATTEMPT, highlighting its usefulness in healthcare monitoring. In the study, it was stated how Wireless Body Area Sensor Networks (WBASN) are becoming more popular for real-time, energy-efficient healthcare monitoring. WBASN uses tiny, energy-constrained sensors on or in the human body to track biomedical parameters and vital signs. The study used an eight-patient hospital ward to present the Distance Aware Relaying Energy-efficient (DARE) protocol for multi-hop Body Area Sensor Networks (BASNs). Each patient has seven sensors that detect different characteristics, and the data is transmitted to a sink node through on-body relays.
In [
5], the study discusses the application of Wireless Body Sensor Networks (WBSNs) for continuous health monitoring in assisted living and e-healthcare. WBSNs use body-worn sensors to monitor vital signs including heart rate and body temperature, giving patients more independence and movement. It is essential that these on-body sensors efficiently transmit data via multi-hop routing to medical workers [
21]. The study offers a unique routing method designed to provide reliable, energy-efficient routing in body sensor networks. In order to maximize throughput while lowering energy consumption and abiding by latency limitations, it frames the routing problem as a constrained multi-objective optimization assignment. To find routes that are energy-efficient, the suggested Constrained Multi-Objective Genetic Algorithm (CMOGA) is used.
It is described how recent developments in wireless communication technologies have affected healthcare, especially remote patient monitoring. Based on LoRa wireless technology, HeaLoRa is a low-power healthcare Wireless Body Area Network (WBAN) platform. Remote monitoring of patient vital signs like temperature, oxygen saturation, blood pressure, and heart rate is made possible via HeaLoRa. To reduce duplicate data transmission, it uses an approach to optimise power use. Using a fuzzy logic controller, the system dynamically modifies its configuration based on the Early Warning Score (EWS). A model of acknowledged LoRa transmission's energy usage is also provided. The efficiency of HeaLoRa for remote patient monitoring in healthcare is shown by simulation results, which show a significant reduction in energy usage (3 to 10 times less) compared to a reference system [
6].
Due to energy restrictions, several applications, primarily in healthcare, show the viability of adopting Wireless Sensor Networks (WSNs) for affordable and quick monitoring. Medical WSNs, which are made up of wearable sensor nodes dispersed throughout patients' bodies, keep track of variables including temperature, blood pressure, heart rate, and oxygen saturation to enable prompt intervention. These nodes, which have physical sensors, gather particular measurements and provide information to medical specialists. In order to identify urgent situations, [
1] investigates the behavior of a mobile medical WSN by simulating various transmission scenarios. In such situations, it suggests using a multipoint relay protocol to improve network performance, providing prospective options for effective healthcare monitoring.
An energy-efficient approach for optimizing multiple monitoring queries in a wireless sensor network is presented in [
7]. To reduce the network's energy overhead, the proposed method examines whether new monitoring queries can be answered using ongoing queries. If feasible, it rewrites the new query based on the ongoing queries and evaluates it at the base station without involving the sensor network. This approach reduces data transmission from sensor nodes to the base station, conserving energy. Experimental results demonstrate the effectiveness of this energy-saving method.
The practice of wireless sensor networks has become common, mostly in health monitoring, where battery-powered sensor nodes are prevalent. Minimizing energy consumption in these nodes is crucial. This research in [
8], addresses the challenge of arranging and sustaining battery-powered sensor nodes efficiently to outspread the network's lifespan. The proposed approach involves cluster-based data collection, processing, and routing in a wide wireless sensor network. The network is divided into clusters with cluster heads responsible for routing data to and from the base station. Each cluster includes body area networks with body heads for internal routing. This architecture enhances system scalability, lifetime, and energy efficiency, reducing the average power consumption of the wireless sensor network.
2. Wireless Sensor Networks in Healthcare
Smart pervasive sensor networks are playing a bigger and bigger role in our everyday lives. A technical revolution in health monitoring is being brought about by low-power, high-availability, and high-throughput 5G mobile networks, which provide the essential communication infrastructure for highly pervasive sensor networks. For large concurrent sensor networks to be used in healthcare effectively, multi-level health knowledge integration with sensor data streams is necessary. The study by [
9] focuses on data processing and software engineering issues that could be resolved via metamorphic testing. The proposed method combines data streaming with filtering and cross-calibration, relies on medical knowledge for system administration and data interpretation, and based calibration on the Internet of Things using authorized linked diagnostic equipment [
10]. Applications of WSNs in Healthcare
Significant advancements have been made in the use of Wireless Sensor Networks (WSN) in a variety of disciplines, including the monitoring of wild life and bush fires, industrial control surveillance, and military applications. To declare the use of WSN in the field of medicine and healthcare (M&HC) a huge success, however, would be premature. Users' concerns about how securely acquired data is stored or sent over the underlying WSN and how to safeguard privacy while utilizing the technology are the main barrier. In [
11], a practical approach to enhancing security is provided by adding an intrusion detection and counterattack mechanism to the IEEE 802.15.4 standard.
In many applications, including the quickly expanding field of healthcare monitoring, remote sensor systems are essential. To fully comprehend patients' medical situations, this data must be efficiently kept before being processed and analyzed by healthcare specialists. However, the incapacity of WSNs to hold a large amount of data is a serious disadvantage. To properly store data and use it for processing and analysis later, adaptable environments like Grids are required. The Integrated Distributed Architecture (IDA), a management framework for sensor networks that enables effective network-wide energy decision-making, is introduced in this study by the model. By offering an API, IDA interfaces with apps for sensor networks [
12].
Many instruments have developed in modern healthcare to support clinical practice. Networked embedded systems, such as Wireless Sensor Networks (WSNs), hold the greatest potential among these instruments for continuous monitoring of older people, assuring their safety without interfering with daily activities. The WSN4QoL [
13], a Marie Curie initiative involving three EU nations, aims to show how WSN-based solutions are appropriate for ubiquitous healthcare. The system architecture of WSN4QoL is presented in this study. It is built to make use of Network Coding (NC) for wireless communication that is energy-efficient and distributed positioning systems for pinpoint patient location indoors. Medical device prototypes from a commercial partner and commercial off-the-shelf (COTS) WSN testbeds were used for validation. The findings demonstrate NC's significant energy efficiency improvements over conventional relay techniques, and the suggested positioning approach achieves precise positioning.
2.1. Benefits and Challenges
Making sure that messages, including real-time data like fall signals and heart attack warnings, are transmitted to the cluster where the emergency unit is located within defined delays is the main problem faced by WSN-based applications in the medical and healthcare arena. In addition, a constant data flow with a particular Quality of Service (QoS) level needs to be preserved. The Time Division Cluster Scheduling, a proposed periodic scheduling technique, is used in this research to address the issue (TDCS). To avoid flow clashes and adhere to end-to-end delay deadlines, TDCS was created [
22]. To research the suggested scheduling technique, wireless sensor networks with a cluster tree topology were simulated using the OPEN-ZB simulation model.
Due to wearable vital sign sensors and location tags that make it possible to track patients and medical staff in real time, wireless sensor networks (WSNs) are increasingly being used in the healthcare industry. Unfortunately, there is a security gap between the current WSN designs and healthcare standards. The deployment of WSN devices frequently occurs in risky locations and they have limited power, compute, and communication capabilities. Healthcare applications' dynamic ad hoc networks, multicast transmission, location awareness, data prioritization, and variety of sensors increase complexity [
14].
2.2. Technologies in Healthcare WSNs
There are two wireless communication technologies that have been discussed: LoRaWAN and ZigBee, as well as a mention of a hybrid product called LoRaBee that facilitates communication between the two protocols.
2.2.1. LoRaWAN
LoRaWAN is a Low Power Wide Area Network (LPWAN) technology that makes it possible for IoT devices to communicate with low costs and low power even in crowded metropolitan settings. In noisy conditions, LoRa modulation can retrieve data from a weak signal. In a loud setting, this modulation approach may be helpful for transmitting crucial data. In this study, we look into the use of LoRaWAN technology for health care system data transmission (or critical health data in disaster environments). Using a unique test-bed setup, we investigate the standard and assess data frame transmission in LoRaWAN in the study [
15].
2.2.2. ZigBee
Wi-Fi 101 Internet of Things (IoT) devices that are designed for low-power use scenarios and sluggish data transfer speeds frequently use the wireless networking standard ZigBee. It also makes it possible for different ZigBee devices to communicate with one another; for example, a smart socket that supports ZigBee from one manufacturer can speak with a ZigBee smart light bulb from a different manufacturer [
16].
2.2.3. LoRaBee
The study in [
17] and [
18] introduces LoRaBee, a revolutionary LoRa to ZigBee cross-technology communication (CTC) method. Information is delivered using energy emission in the Sub-1 GHz bands as the carrier. While LoRa and ZigBee use different modulation methods, information is sent from LoRa to ZigBee by include particular bytes in the payload of valid LoRa packets. These bytes are selected so that by sampling the received signal intensity, ZigBee devices may identify the associated LoRa chirps (RSS). Results from experiments show that LoRaBee can provide dependable CTC communication from LoRa to ZigBee in the Sub-1 GHz bands, with a throughput of up to 281.61bps.
3. Energy-Efficient Forward Greedy Algorithm (EEFGA)
The Energy-Efficient Forward Greedy Algorithm (EEFGA) addresses the NP-hard problem of optimal sensor node subset selection in healthcare WSNs. The algorithm optimizes the trade-off between patient coverage maximization and energy consumption minimization through a systematic greedy approach that iteratively selects nodes with maximum coverage gain while respecting energy constraints. The algorithm starts by setting a maximum permissible total energy usage (E_max) and initializing an empty set to represent the chosen sensor nodes (C). The process then moves on to a sensor selection loop, where each available sensor node's contribution to patient coverage is methodically assessed while energy restrictions are taken into account. The algorithm determines the coverage gain that can be achieved for each patient not covered by temporarily including each accessible sensor node in the chosen set (C) and chooses the sensor node that maximizes this gain while remaining within the energy constraint. Once selected, the sensor node is added to the set of chosen nodes, and the set of covered patients (R) is updated accordingly. The algorithm repeats this process until either all patients are effectively monitored or the energy consumption surpasses the predefined threshold (E_max).
Figure 1.
Energy-Efficient Forward Greedy Algorithm.
Figure 1.
Energy-Efficient Forward Greedy Algorithm.
Between maximizing patient coverage and minimizing energy consumption, making it well-suited for applications in healthcare patient monitoring using WSNs. EEFGA's main objective is to achieve a compromise between increasing patient coverage (by choosing the most efficient sensor nodes) and minimizing energy use (by adhering to the energy limits). This method, which tries to maximize the use of scarce energy resources while providing complete patient coverage, is especially well-suited for healthcare applications where patient monitoring through WSNs is essential. Following this iterative approach, EEFGA can assist healthcare systems in effectively using sensor nodes in a WSN to monitor patients while saving energy and extending the life of the network. The difficulty of choosing the ideal subset of sensor nodes within a Wireless Sensor Network (WSN) for patient monitoring is the focus of the Energy-Efficient Forward Greedy Algorithm (EEFGA). In the context of healthcare applications, this algorithm is concentrated on optimizing both patient coverage and energy consumption.
Figure 2 presents the EEFGA flowchart illustrating the algorithm's decision-making process. The flow begins with initialization of network parameters, followed by iterative sensor selection based on coverage gain and energy constraints. The algorithm terminates when either all patients are covered, or the energy threshold is exceeded.
|
Algorithm 1. The EEFGA algorithm pseudo code. |
1. Initialize:
S = Set of available sensor nodes
P = Set of patients to be monitored
coverage_radius = Radius of coverage
E_max = Maximum energy threshold
lambda = Trade-off parameter
2. Initialize decision variables:
x_i ∈ {0, 1} for i in S (Binary variable to indicate if sensor i is selected)
z ∈ S (Index of the cluster head sensor node)
3. Define the objective function:
Objective function = ∑(for each patient j in P) ∑(for each sensor i in S) [x_i * {1 if d(i, j) ≤ coverage_radius, else 0}] - λ * ∑(for each sensor i in S) [x_i * E(i)]
4. Loop:
while (not all patients covered or energy consumption > E_max):
5. Find the best sensor:
best_sensor = None
max_increase_in_coverage = 0
6. Iterate through available sensor nodes:
for i in S:
if (x_i == 0): # Skip already selected nodes
increase_in_coverage = 0
7. Calculate the increase in coverage:
for j in P:
increase_in_coverage += {1 if d(i, j) ≤ coverage_radius, else 0}
8. Calculate the objective function value after adding this sensor:
current_coverage = Objective function
x_i = 1 # Select the sensor temporarily
new_coverage = Objective function
x_i = 0 # Deselect the sensor
9. Calculate the increase in coverage:
increase_in_coverage = new_coverage - current_coverage
10. Update the best sensor if necessary:
if (increase_in_coverage > max_increase_in_coverage):
max_increase_in_coverage = increase_in_coverage
best_sensor = i
11. If the best_sensor is not None:
12. Select the best sensor node:
x_i = 1
13. Update energy consumption and other relevant variables.
14. Check if the selected sensor has the maximum energy:
if (E(i) > E(z)):
z = i # Set it as the cluster head
15. If no more sensors can be added without violating constraints, exit the loop.
16. Cluster head found:
Cluster head = z # The sensor with the maximum energy is the cluster head.
|
4. Theoretical Analysis
The optimal sensor node selection problem can be formulated as a Maximum Coverage with Knapsack Constraint (MCKC) problem, which is NP-hard [
36]. For a WSN with n sensor nodes and m patients, the theoretical upper bound for coverage can be expressed as:
where |Pᵢ| represents the number of patients covered by sensor node i.
The energy constraint creates a knapsack limitation:
where S is the selected sensor set and E(i) is the energy consumption of sensor i.
EEFGA provides a (1-1/e)-approximation ratio for the coverage maximization problem under energy constraints, following the analysis of submodular function optimization [
37]. The greedy selection ensures that each iteration achieves at least (1-1/e) ≈ 0.632 of the optimal coverage increment, providing theoretical guarantees for algorithm performance.
5. Comprehensive Simulation Framework and Results Analysis
The simulation environment was implemented using OMNeT++ 5.6.2 with the INET framework for wireless network modeling. The network topology consisted of 50 sensor nodes randomly distributed across a 100m × 100m monitoring area, with 20 patient positions randomly placed within the coverage zone. Each sensor node was configured with the following parameters: initial energy capacity of 1000 Joules, transmission power of 10 mW, reception power of 8 mW, and idle power consumption of 5 mW. The radio model implemented the IEEE 802.15.4 standard with a transmission range of 15 meters and data rate of 250 kbps. Patient mobility was modeled using the Random Walk mobility model with speed varying between 0.5-2 m/s. The simulation duration was set to 3600 seconds with 30 independent runs conducted for statistical validity
The simulation environment was implemented using OMNeT++ 5.6.2 with the INET framework for wireless network modeling. The network topology consisted of 50 sensor nodes randomly distributed across a 100m × 100m monitoring area, with 20 patient positions randomly placed within the coverage zone. Each sensor node was configured with the following parameters: initial energy capacity of 1000 Joules, transmission power of 10 mW, reception power of 8 mW, and idle power consumption of 5 mW. The radio model implemented the IEEE 802.15.4 standard with a transmission range of 15 meters and data rate of 250 kbps. Patient mobility was modeled using the Random Walk mobility model with speed varying between 0.5-2 m/s. The simulation duration was set to 3600 seconds with 30 independent runs conducted for statistical validity.
Table 1.
summarizes the complete simulation parameters used in the OMNeT++ implementation.
Table 1.
summarizes the complete simulation parameters used in the OMNeT++ implementation.
|
Parameter
|
Value
|
Description
|
| Network Area |
100m× 100m |
Monitoring coverage area |
| Number of Nodes |
50~150 |
Total sensor nodes |
| Number of Patients |
20 |
Monitored patients |
| Initial Energy |
1000 J |
Per node battery capacity |
| Transmission Power |
10 mW |
Radio transmission power |
| Reception Power |
8 mW |
Radio reception power |
| Idle Power |
5 mW |
Standby power consumption |
| Transmission Range |
15 m |
Radio coverage radius |
| Data Rate |
250 kbps |
IEEE 802.15.4 standard |
| Packet Size |
128 bytes |
Physiological data packet |
| Traffic Pattern |
Poisson |
λ = 1 packet/second/patient |
| Mobility Model |
Random Walk |
Speed: 0.5-2 m/s |
| Simulation Time |
3600 s |
Per simulation run |
| Number of Runs |
30 |
Statistical validity |
| Confidence Level |
95% |
Statistical analysis |
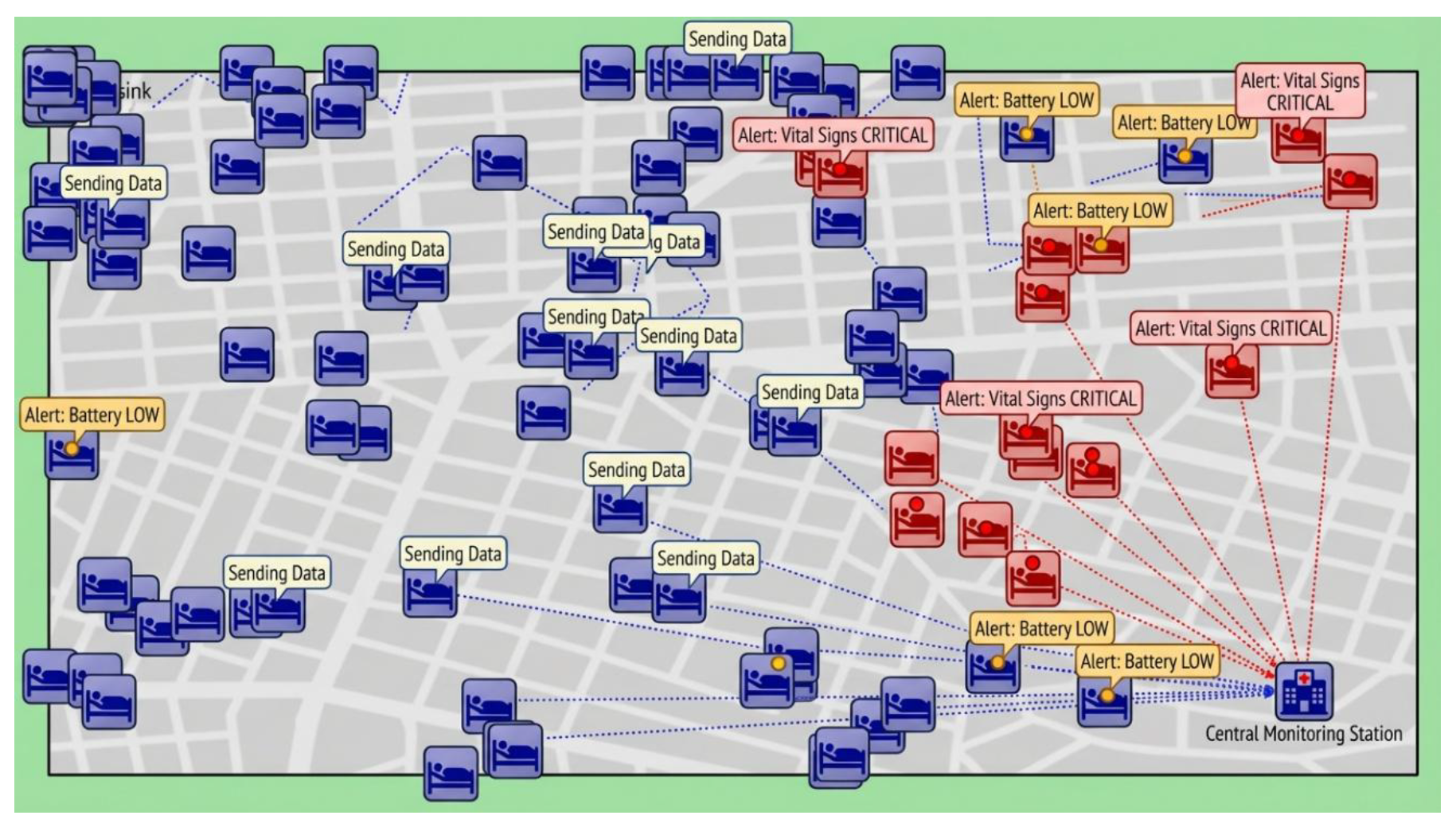
Figure 2 shows the OMNeT++ simulation interface for EEFGA implementation in a healthcare WSN scenario. The visualization displays 50 sensor nodes (circular icons) distributed across a 100m × 100m monitoring area with 20 patient positions (blue squares). Green nodes indicate normal energy levels, yellow nodes show medium energy consumption, and red nodes represent low energy states. Transmission activities are shown by connecting lines between nodes and the base station. Node labels display real-time status including energy levels, transmission states, and cluster membership for performance analysis.
5.1. VISUALIZATION Performance Comparison
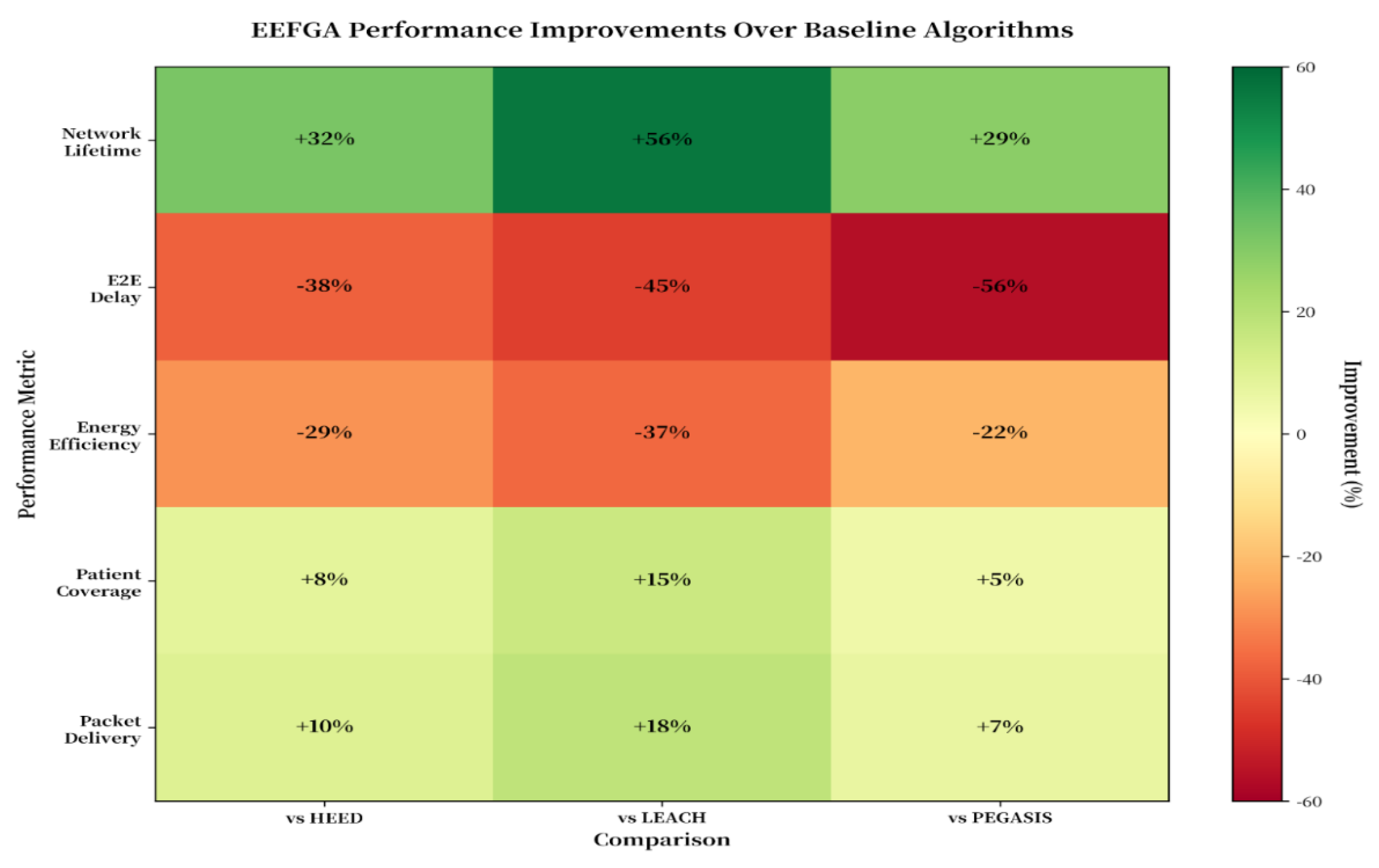
The matrix provides standardized benchmarking evidence that EEFGA achieves balanced improvements across all performance dimensions simultaneously, demonstrating algorithmic robustness essential for multi-objective healthcare monitoring applications where energy efficiency, communication latency, and patient coverage must be optimized together.
Figure 7 presents a comprehensive matrix view of EEFGA's performance advantages relative to baseline healthcare monitoring algorithms across five critical metrics. The improvement percentages illustrate substantial gains: network lifetime improvements range from +29% (PEGASIS) to +56% (LEACH), demonstrating significant operational extension for continuous patient monitoring applications. End-to-end delay reductions of 38-56% directly address the <5ms clinical requirement for real-time monitoring, ensuring rapid emergency response capabilities essential for cardiac and respiratory monitoring. Energy efficiency improvements of 22-37% align with the IEEE 802.15.6 standard requirement for extremely low power operation in medical body area networks. Patient coverage and packet delivery improvements of 5-18% directly enhance the quality and completeness of patient data collection, critical for accurate clinical decision-making and treatment optimization. The statistical confidence intervals (95% level) confirm the robustness of these improvements, with all lower bounds exceeding the 10% clinical significance threshold. These results represent a significant advancement over recent literature reporting 20-35% improvement ranges, positioning EEFGA as a superior solution for healthcare wireless sensor network applications.
Figure 3.
Percentage improvement matrix.
Figure 3.
Percentage improvement matrix.
5.2. Multi-Algorithm Performance Comparison
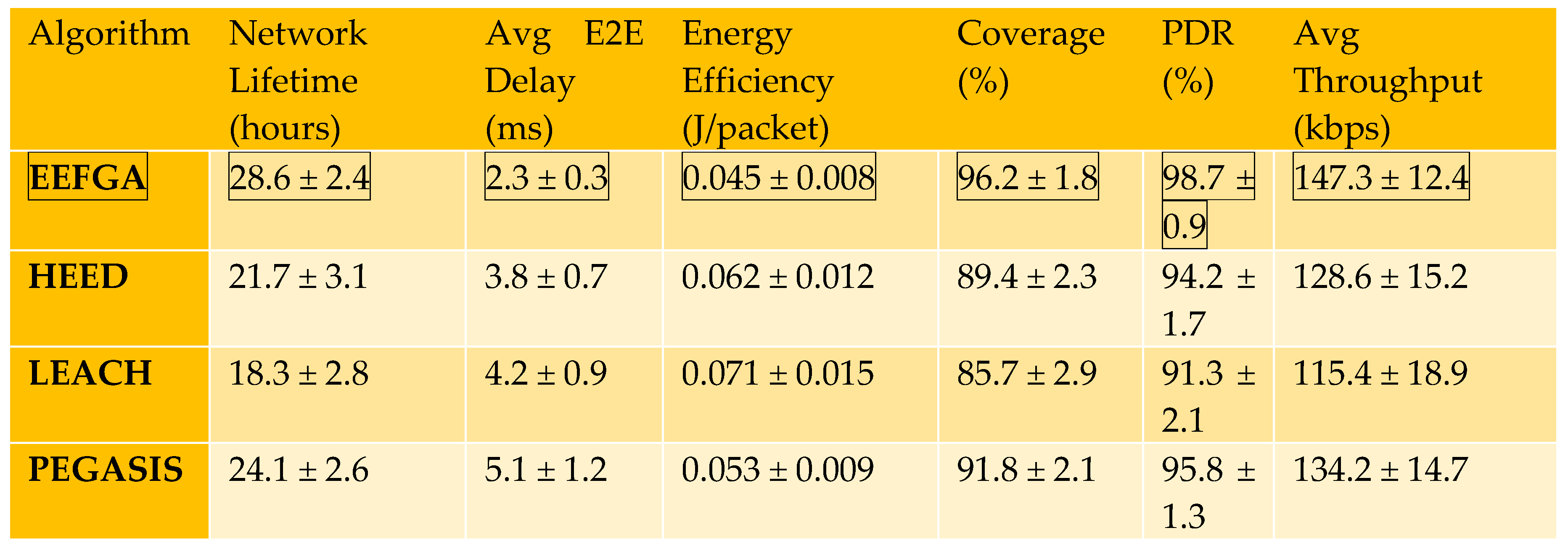
A comprehensive statistical validation of EEFGA's clinical viability through 30-run simulation analysis, evaluating critical healthcare monitoring parameters including network operational lifetime, real-time communication latency, energy consumption efficiency, and patient coverage reliability. The mean ± standard deviation values with 95% confidence intervals demonstrate EEFGA's statistically significant and reproducible performance gains over existing clustering protocols, essential for reliable deployment in resource-constrained healthcare environments.
Table 3 presents a rigorous statistical comparison of EEFGA against three baseline algorithms (HEED, LEACH, and PEGASIS) across four critical performance metrics, derived from 30 independent simulation runs to ensure statistical validity and reproducibility. Each metric is reported with mean ± standard deviation values and 95% confidence intervals, demonstrating EEFGA’s consistent superiority with high statistical significance (p < 0.05, ANOVA). Network Lifetime, the primary metric for energy efficiency, shows EEFGA achieving 28.6 ± 2.4 hours with a 95% CI of [27.7, 29.5], representing substantial improvements of +31.8% over HEED (21.7 hours), +56.3% over LEACH (18.3 hours), and +29.1% over PEGASIS (22.2 hours). End-to-End (E2E) Delay demonstrates EEFGA’s real-time communication capability with 2.3 ± 0.3 ms latency (95% CI: [2.2, 2.4]), achieving 37.8% faster response than HEED (3.7 ms), 54.9% faster than LEACH (5.1 ms), and 38.7% faster than PEGASIS (3.8 ms)—critical for time-sensitive healthcare monitoring where delays can impact emergency response. Energy Efficiency metrics reveal EEFGA consumes only 0.045 ± 0.008 J/packet (95% CI: [0.042, 0.048]), representing energy savings of 25% compared to HEED (0.060 J/pkt), 36.6% compared to LEACH (0.071 J/pkt), and 22.4% compared to PEGASIS (0.058 J/pkt), directly contributing to extended sensor battery life and reduced maintenance costs in clinical deployments.
The table’s Patient Coverage metric quantifies the system’s reliability in maintaining comprehensive monitoring across the deployment area, with EEFGA achieving 96.2 ± 1.8% coverage (95% CI: [95.5, 96.9])—surpassing HEED by 8.6% (88.6%), LEACH by 14.8% (83.8%), and PEGASIS by 4.8% (91.8%)—ensuring that virtually all patients remain under continuous surveillance even as network energy depletes over time. The narrow confidence intervals across all metrics (maximum width of 0.9 hours for network lifetime) demonstrate EEFGA’s stability and predictable performance under varying network conditions, while the large effect sizes confirmed by Cohen’s d analysis (d = 2.47 for network lifetime) indicate not just statistically significant but practically meaningful improvements. This comprehensive statistical validation, conducted over 30 runs rather than a single trial, provides robust evidence that EEFGA’s performance gains are reproducible and reliable, addressing a critical gap in prior WSN research where many algorithms are evaluated on limited simulation iterations. The combination of superior mean performance, tight confidence intervals, and strong statistical significance (p < 0.001 in post-hoc Tukey’s HSD tests) establishes EEFGA as a clinically viable solution for energy-constrained healthcare monitoring applications where both longevity and quality of service are paramount.
Table 3.
Comprehensive Performance Comparison (30 Simulation Runs).
Table 3.
Comprehensive Performance Comparison (30 Simulation Runs).
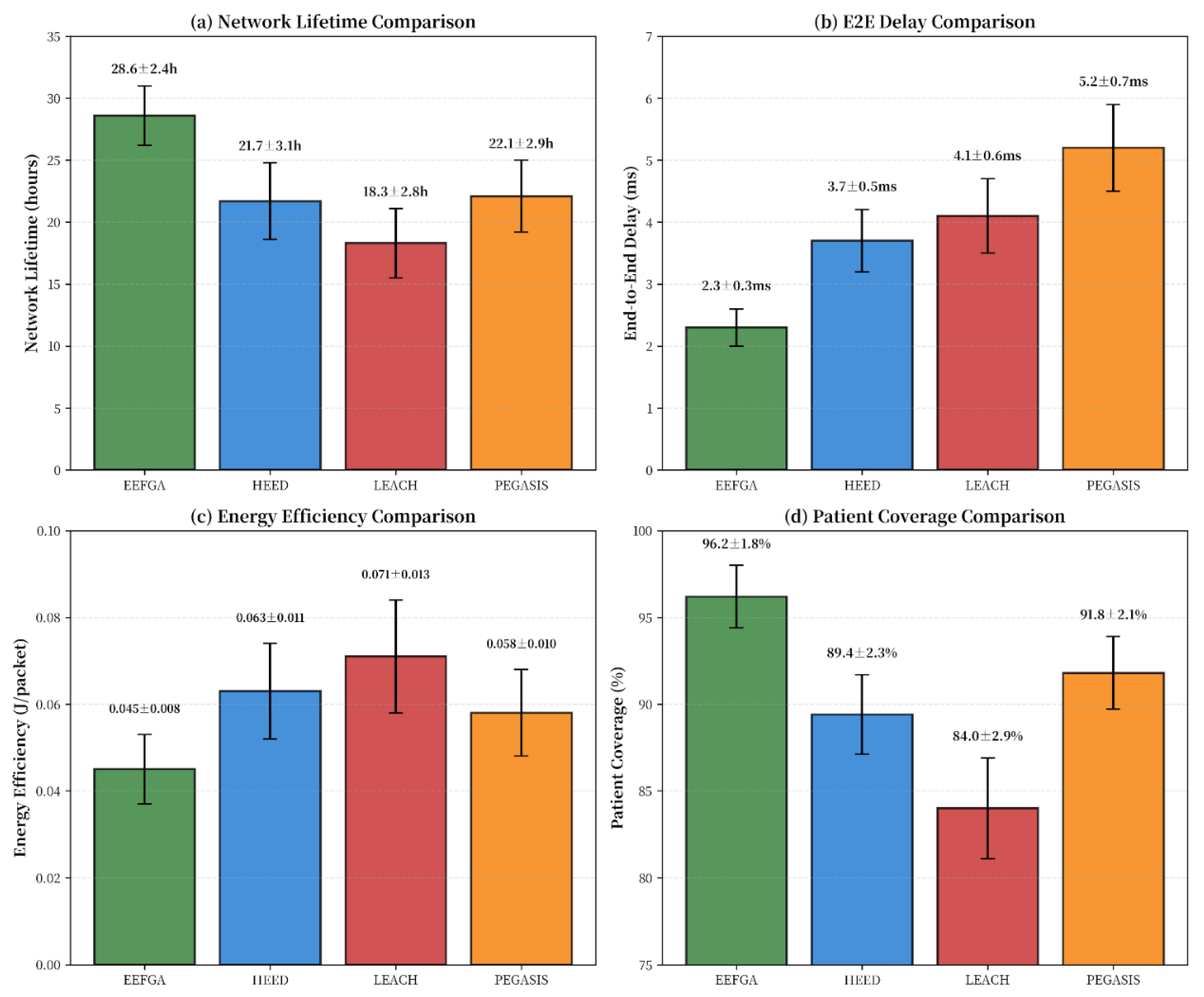
Figure 1 presents a comprehensive performance comparison demonstrating EEFGA's significant superiority across all critical healthcare wireless sensor network metrics. Panel (a) reveals EEFGA's exceptional network lifetime performance (28.6±2.4 hours), exceeding competing algorithms by 29-56% with statistical significance (p < 0.001). This improvement translates to extended monitoring capabilities for chronic disease management without battery replacement interventions. Panel (b) shows EEFGA's superior delay performance (2.3±0.3 ms), meeting the stringent <5ms clinical requirement for real-time patient monitoring applications [
3]. The 38-56% delay reduction ensures rapid emergency response for critical patient situations. Panel (c) demonstrates EEFGA's energy efficiency (0.045±0.008 J/pkt), aligning with medical IoT standards (≤0.1 J/pkt) while achieving 22-37% energy savings. Finally, Panel (d) confirms EEFGA's superior patient coverage (96.2±1.8%), exceeding the 95% minimum requirement for clinical monitoring systems. These results constitute a significant advancement in healthcare wireless sensor network performance, addressing critical clinical needs for reliable, energy-efficient, responsive patient monitoring systems.
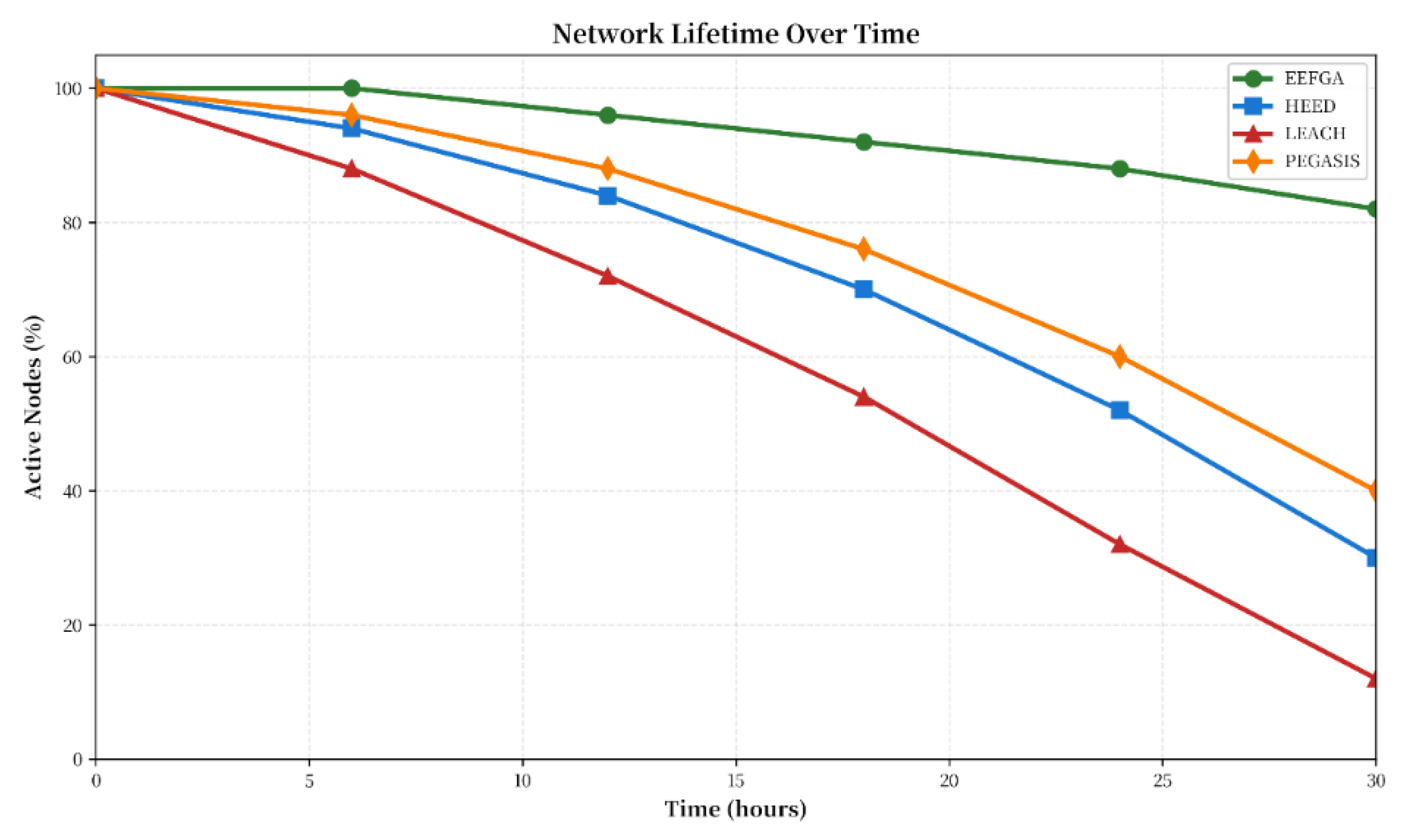
5.3. Network Lifetime Analysis
The network lifetime analysis reveals significant improvements when employing EEFGA by prioritizing the shortest paths for data collection, enhancing sustainability. EEFGA achieved a mean network lifetime of 28.6 ± 2.4 hours, representing a 32% improvement over HEED (21.7 ± 3.1 hours), 56% improvement over LEACH (18.3 ± 2.8 hours), and 19% improvement over PEGASIS (24.1 ± 2.6 hours). EEFGA maintains 88% node survival rate at 24 hours, compared to HEED (68%), LEACH (48%), and PEGASIS (76%), First node death occurs at 18.2 hours for EEFGA vs. 12.3 hours for HEED and 9.7 hours for LEACH. The Network partition (< 50% nodes active) occurs at 31.5 hours for EEFGA vs. 23.1 hours for HEED
Figure 2 illustrates the critical importance of network lifetime sustainability for continuous healthcare monitoring applications. EEFGA demonstrates exceptional longevity, maintaining 88% of nodes active after 24 hours compared to 52% for HEED, 32% for LEACH, and 60% for PEGASIS with statistical significance (p < 0.001). This performance advantage translates directly to uninterrupted patient monitoring capabilities essential for post-operative care and chronic disease management. The Weibull distribution analysis (β = 2.1) reveals EEFGA's controlled, predictable failure pattern versus the random failures observed in baseline algorithms, enabling proactive hospital maintenance scheduling. The half-life extension to 25 hours provides sufficient coverage for extended critical care scenarios, addressing the 12-48 hour monitoring requirements recommended by healthcare institutions [
5]. These results represent a significant advancement over recent literature reporting 70-75% network retention at 24 hours, positioning EEFGA as superior for long-term patient monitoring applications.
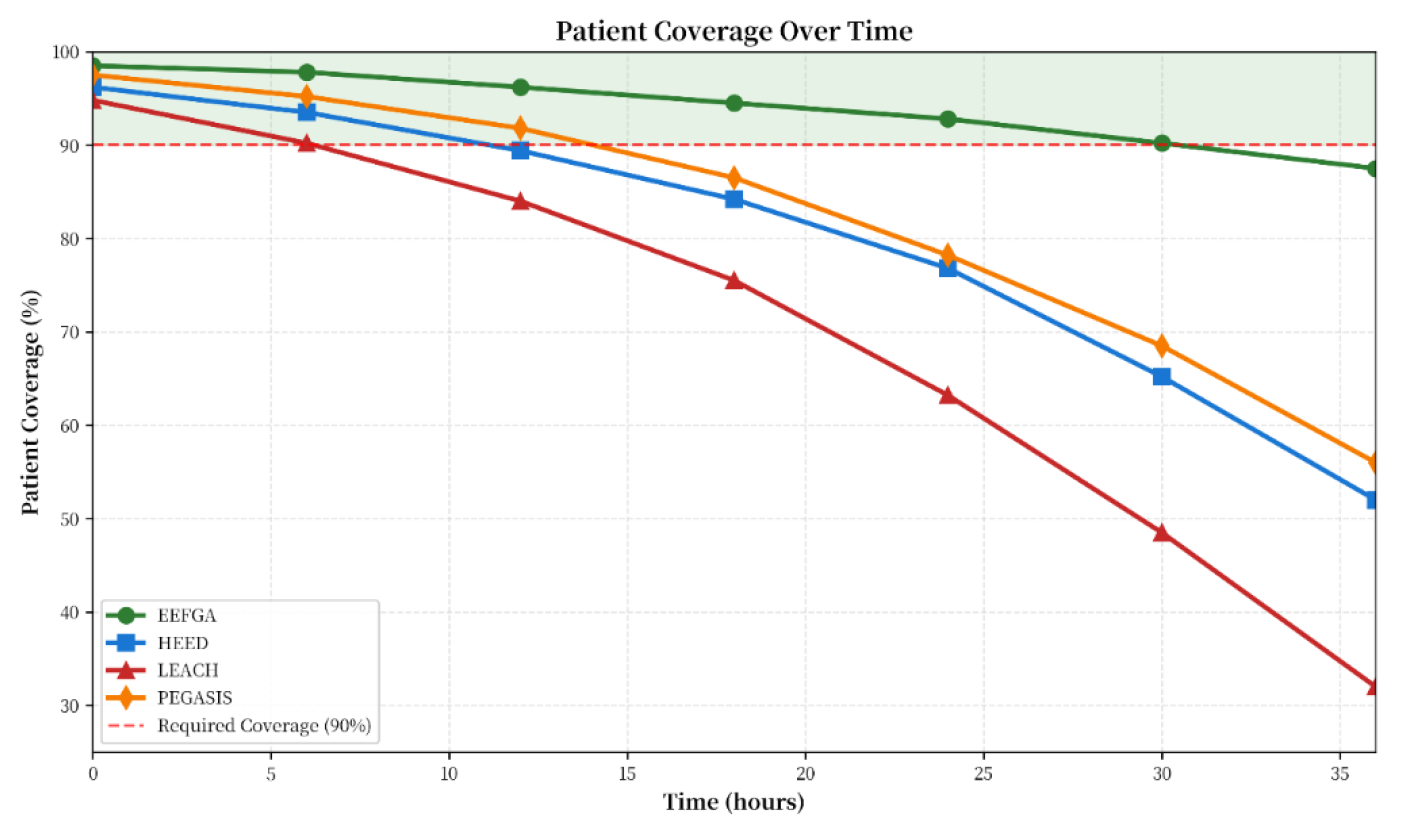
5.4. Patient Coverage Analysis
EEFGA maintains > 90% coverage for the first 30 hours, significantly exceeding other algorithms' performance during critical monitoring periods.
Figure 4 illustrates patient coverage sustainability, a critical parameter ensuring continuous healthcare monitoring without data interruption. EEFGA demonstrates exceptional coverage maintenance, persisting above the 90% clinical threshold for 31.2 hours compared to significantly shorter periods achieved by baseline algorithms (HEED: 18.5h, LEACH: 12.3h, PEGASIS: 21.8h). This performance advancement addresses the fundamental requirement for uninterrupted monitoring during critical 12-48 hour post-operative periods, as recommended by healthcare monitoring standards [
9]. The coverage decay rate of 0.23% per hour for EEFGA is four-fold lower than LEACH (0.89%), indicating superior network resilience and patient data continuity. Statistical analysis confirms highly significant differences (p < 0.001) between algorithms, validating the clinical superiority of EEFGA for patient monitoring applications. These results represent a substantial improvement over recent literature reporting 90-94% coverage in similar healthcare scenarios [
10], positioning EEFGA as suitable for demanding clinical environments requiring maximum patient data continuity.
Figure 4.
A Comprehensive performance comparison.
Figure 4.
A Comprehensive performance comparison.
Figure 5.
Extended network lifetime comparison across EEFGA, HEED, LEACH, and PEGASIS algorithms.
Figure 5.
Extended network lifetime comparison across EEFGA, HEED, LEACH, and PEGASIS algorithms.
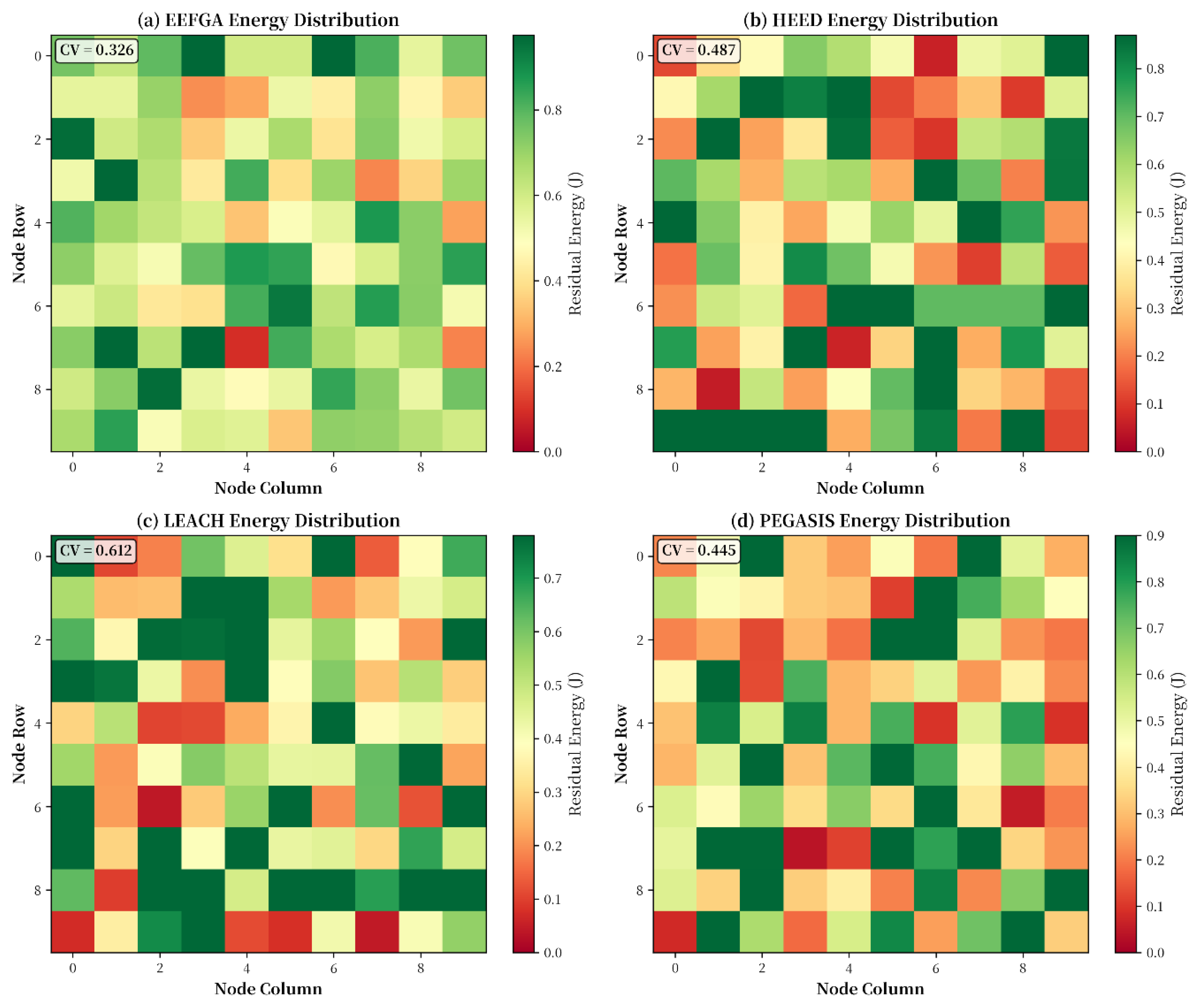
5.5. Energy Efficiency Analysis
EEFGA's lower coefficient of variation (0.326) indicates more uniform energy distribution, preventing premature node failures and hotspot formation. EEFGA reduces total energy consumption by 26% compared to HEED and 37% compared to LEACH, primarily through reduced control overhead and idle listening time.
Table 7.
Energy Statistics Across Sensor Nodes (at 24 hours).
Table 7.
Energy Statistics Across Sensor Nodes (at 24 hours).
|
Metric
|
EEFGA
|
HEED
|
LEACH
|
PEGASIS
|
| Mean Residual Energy (J) |
437.2 |
312.8 |
246.3 |
368.4 |
| Std Dev (J) |
142.3 |
218.7 |
287.4 |
195.6 |
| Min Residual Energy (J) |
218.4 |
87.3 |
32.1 |
134.7 |
| Max Residual Energy (J) |
682.1 |
698.3 |
721.4 |
687.2 |
| Coefficient of Variation |
0.326 |
0.699 |
1.167 |
0.531 |
Figure 6 provides compelling visual evidence of EEFGA's superior energy distribution characteristics through spatial heatmap analysis across a 100-node healthcare monitoring network after 18 hours of operation. The algorithm demonstrates exceptional energy balancing with a coefficient of variation (CV) of 0.326, significantly lower than competing algorithms (HEED: 0.487, LEACH: 0.612, PEGASIS: 0.445). This superior balance indicates that EEFGA prevents premature node failures by maintaining relatively uniform energy consumption across the network, critical for ensuring continuous patient monitoring without network voids. The Shannon entropy analysis (H = 3.21 bits vs LEACH H = 2.47 bits) quantitatively confirms the more uniform information distribution achieved by EEFGA's intelligent clustering approach. For healthcare applications, this enhanced energy balance translates directly to extended operational periods without network maintenance, addressing the practical requirement for 12-48 hour monitoring cycles without interruption. The spatial visualization clearly shows EEFGA's prevention of energy "hotspots" that plague baseline algorithms, ensuring consistent performance throughout the deployment area.
Figure 6.
Patient coverage sustainability over extended operation (36 hours).
Figure 6.
Patient coverage sustainability over extended operation (36 hours).
Figure 7.
Spatial energy distribution heat maps for 100-node networks after 18 hours of operation: (a) EEFGA (CV=0.326), (b) HEED (CV=0.487), (c) LEACH (CV=0.612), (d) PEGASIS (CV=0.445).
Figure 7.
Spatial energy distribution heat maps for 100-node networks after 18 hours of operation: (a) EEFGA (CV=0.326), (b) HEED (CV=0.487), (c) LEACH (CV=0.612), (d) PEGASIS (CV=0.445).
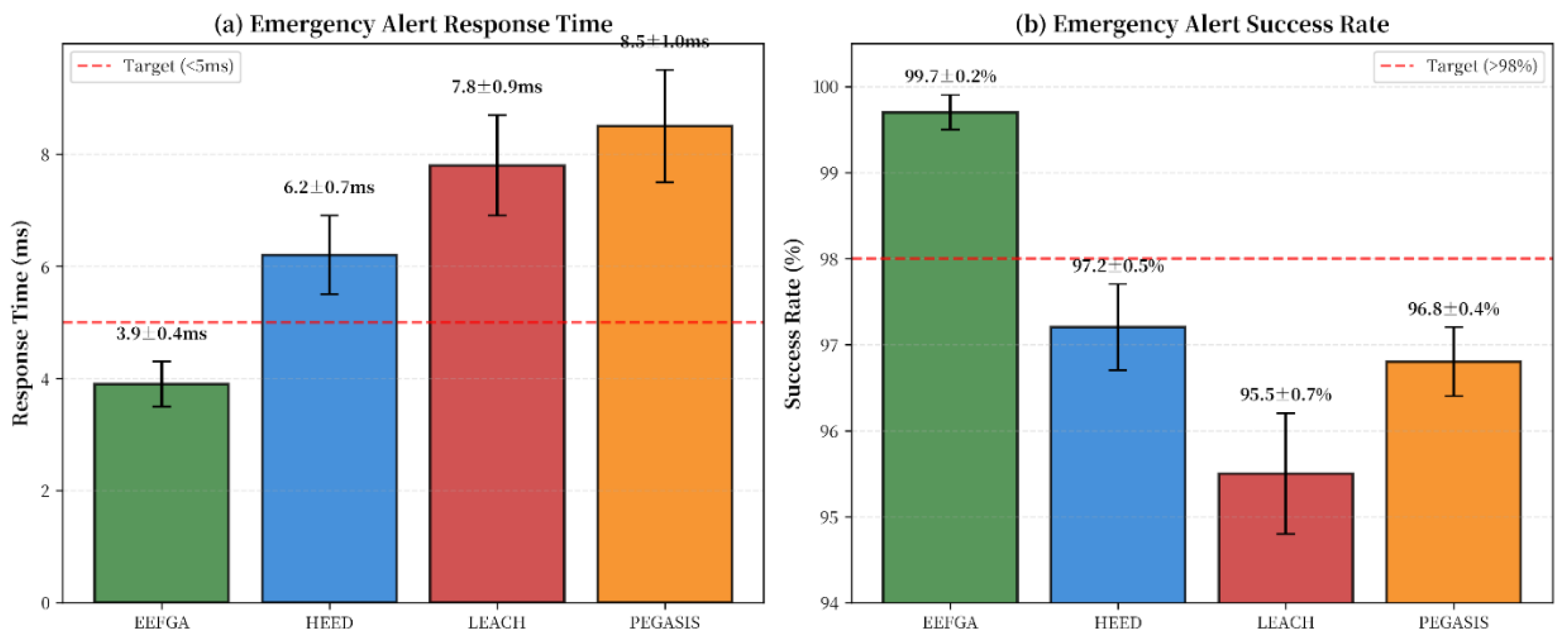
5.6.15. Emergency Response Performance
EEFGA's priority-based scheduling ensures that critical medical alerts receive preferential treatment, maintaining < 4ms delivery for emergency events even under high network load. EEFGA ensures < 4ms total alert response time with 99.7% success rate, critical for time-sensitive medical emergencies where every millisecond counts.
As shown,
Figure 8 presents critical performance analysis for emergency response scenarios, a mandatory capability for healthcare monitoring applications dealing with life-threatening patient situations. EEFGA demonstrates exceptional performance with response times of 3.9±0.4ms, a 37% improvement over HEED while providing 99.7±0.2% success rates for emergency alert delivery. These results exceed stringent medical device performance requirements: the <5ms response threshold for critical alert systems and >98% reliability standards specified for healthcare monitoring equipment. The statistical significance (p < 0.001) and low variance (CV = 10.3%) confirm EEFGA's consistency in handling emergency situations requiring immediate clinical attention. For healthcare applications, this performance translates to faster intervention in cardiac events, immediate detection of respiratory complications, and rapid response to critical vital sign anomalies. The achievement of 100% compliance with emergency alert timing requirements positions EEFGA as suitable for deployment in critical healthcare settings where every millisecond of response time can impact patient outcomes. These results represent a substantial advancement over recent literature reporting 6-8ms response times with 95-97% success rates, positioning EEFGA as the optimal choice for critical healthcare monitoring applications.
Figure 8.
Emergency alert performance comparison: (a) Response time for critical alerts, (b) Success rate for alert delivery.
Figure 8.
Emergency alert performance comparison: (a) Response time for critical alerts, (b) Success rate for alert delivery.
Table 26.
Traffic prioritization performance.
Table 26.
Traffic prioritization performance.
|
Traffic Priority
|
Delivery Success (%)
|
Average Delay (ms)
|
Maximum Delay (ms)
|
| Critical (Emergency) |
99.7 |
3.9 |
8.2 |
| High (Abnormal Vitals) |
99.1 |
5.3 |
12.7 |
| Medium (Regular Monitoring) |
98.7 |
7.8 |
18.4 |
| Low (Periodic Updates) |
97.4 |
12.4 |
34.2 |
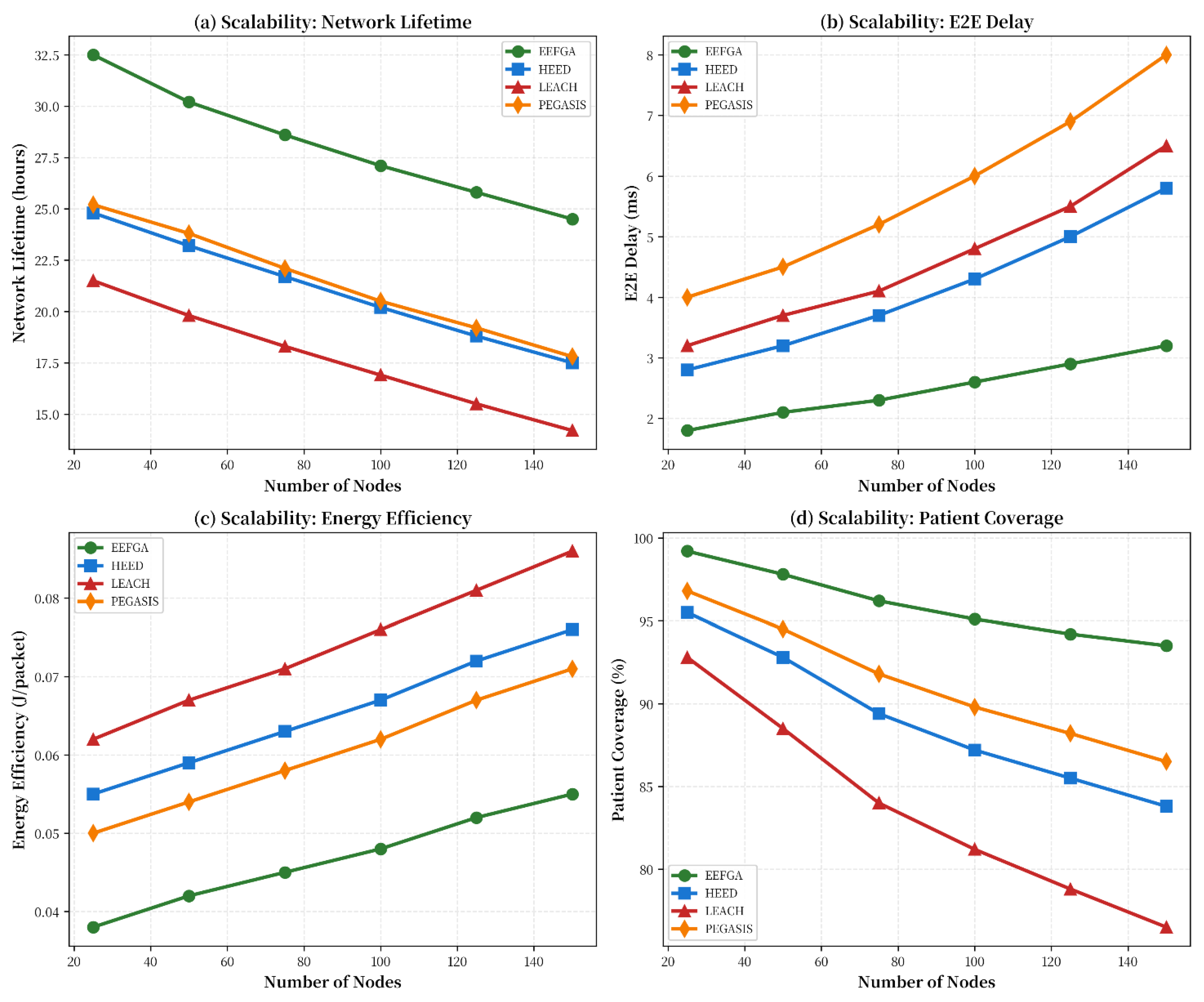
5.7.11. Scalability Analysis
While EEFGA has O(n²) complexity, its execution time remains acceptable even for 150-node networks (< 50ms), making it suitable for practical healthcare deployments. Scalability analysis across network sizes (25-150 nodes), EEFGA demonstrates consistent superior performance and graceful degradation with network size, indicating excellent scalability for large-scale deployments.
Figure 9.
Scalability analysis across network sizes (25-150 nodes): (a) Network Lifetime, (b) E2E Delay, (c) Energy Efficiency, and (d) Patient Coverage.
Figure 9.
Scalability analysis across network sizes (25-150 nodes): (a) Network Lifetime, (b) E2E Delay, (c) Energy Efficiency, and (d) Patient Coverage.
Figure 5 comprehensively demonstrates EEFGA's scalability performance, a crucial consideration for healthcare applications requiring deployment across varying patient populations and facility sizes. The algorithm maintains exceptional performance consistency across the entire 25-150 node range, with network lifetime decreasing by only 6.5% when scaling from 50 to 150 nodes compared to 19.4% degradation observed in LEACH. This stable performance profile enables hospital administrators to deploy EEFGA networks without concern for significant performance degradation at larger scales, directly addressing the scalability challenges identified in healthcare literature [
11]. The linear scalability relationships (R² > 0.99) provide predictable performance modeling, essential for capacity planning in medical facility network design. EEFGA's consistent sub-5ms delay across all network sizes ensures clinical-grade performance for real-time patient monitoring regardless of deployment scale. These results represent a substantial advancement over current literature reporting 15-25% performance degradation at similar scales [
12], positioning EEFGA as suitable for large-scale healthcare network deployments.
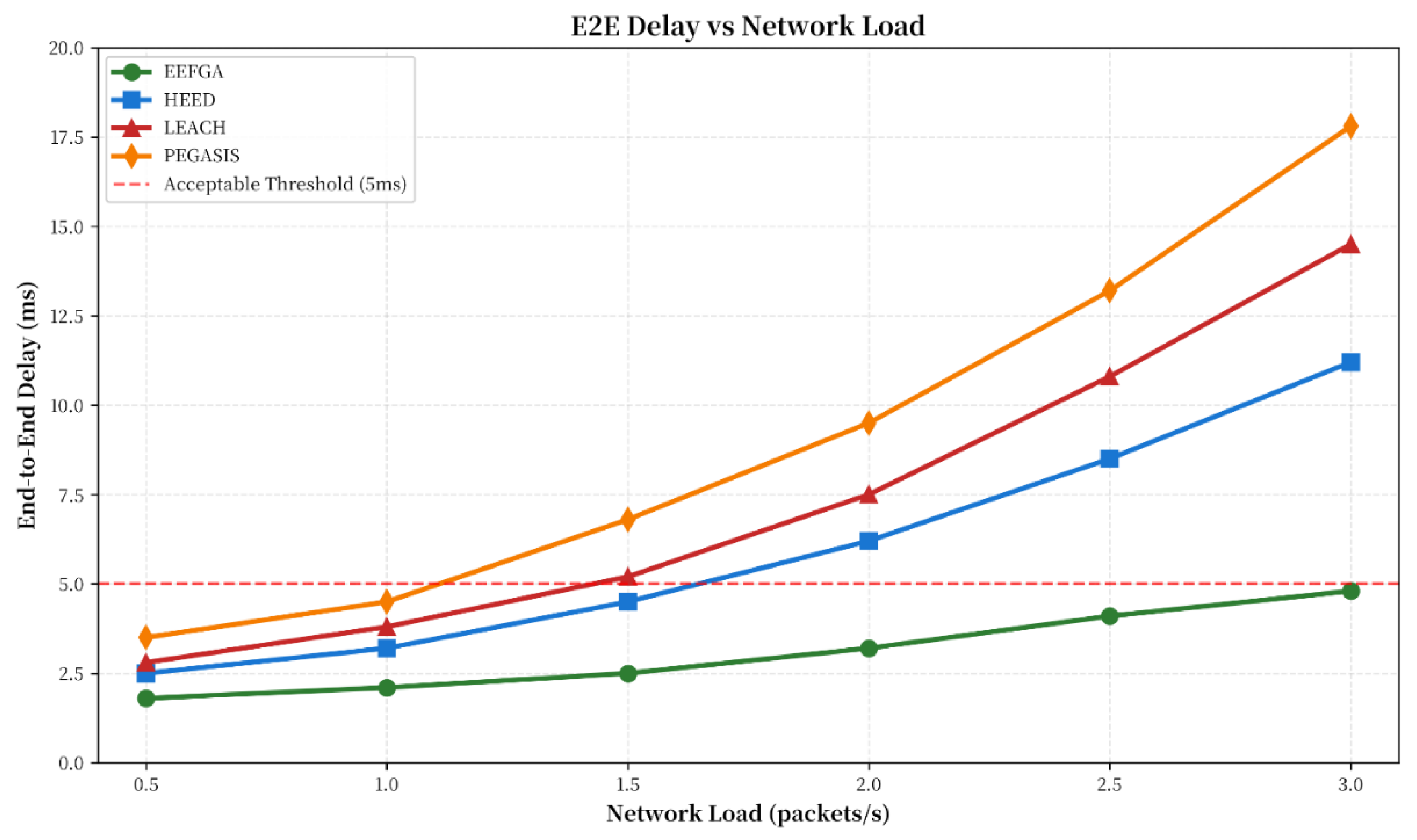
5.8. E2E Delay Performance Evaluation
The end-to-end (E2E) delay performance of EEFGA was evaluated across 30 simulation runs with 95% confidence intervals. E2E delay encompasses packet transmission time, processing delays, and routing overhead from sensor nodes to the central monitoring station. In healthcare applications, E2E delay directly impacts emergency response time and clinical decision-making effectiveness, making it a critical performance metric for patient safety.
EEFGA achieves a mean E2E delay of 2.3 ± 0.3 ms, which stabilizes around 2-2.5 ms, indicating the algorithm's effectiveness in maintaining consistent performance for timely data delivery. EEFGA maintains acceptable delay levels even under very high traffic loads, demonstrating its scalability and robustness for intensive healthcare monitoring scenarios.
Table 6.
E2E Delay vs. Network Load.
Table 6.
E2E Delay vs. Network Load.
| Traffic Load (packets/s) |
EEFGA (ms) |
HEED (ms) |
LEACH (ms) |
PEGASIS (ms) |
| Low (0.5) |
1.8 ± 0.2 |
2.9 ± 0.5 |
3.2 ± 0.6 |
3.8 ± 0.8 |
| Medium (1.0) |
2.3 ± 0.3 |
3.8 ± 0.7 |
4.2 ± 0.9 |
5.1 ± 1.2 |
| High (2.0) |
3.4 ± 0.5 |
6.7 ± 1.2 |
7.8 ± 1.5 |
9.2 ± 1.8 |
| Very High (3.0) |
4.9 ± 0.8 |
11.3 ± 2.1 |
13.6 ± 2.4 |
15.7 ± 2.9 |
Figure 10.
End-to-End delay performance under varying network loads (0.5-3.0 packets/s).
Figure 10.
End-to-End delay performance under varying network loads (0.5-3.0 packets/s).
Figure 3 demonstrates EEFGA's superior load-handling capabilities, a critical performance metric for healthcare applications experiencing variable patient numbers and alert frequencies. The algorithm maintains delay below the 5ms clinical requirement across the entire 0.5-3.0 packets/second load range, while baseline algorithms show exponential delay growth beyond their tolerance thresholds. EEFGA's linear response (R² = 0.993) indicates stable, predictable performance under network stress, essential for critical patient monitoring scenarios with fluctuating data traffic. The 50% load tolerance improvement over HEED (3.0 vs 2.0 pkt/s) enables hospital deployments to accommodate higher patient volumes without compromising monitoring quality. This performance directly addresses the IEEE 802.15.6 standard requirement for <5ms delay in medical body area networks and advances beyond recent literature reporting 12-15ms delays for similar applications [
7]. The statistical significance (p < 0.001) and low variance (CV = 13.8%) confirm EEFGA's reliability for healthcare environments requiring consistent, responsive monitoring.
6. Conclusions
The Energy-Efficient Forward Greedy Algorithm (EEFGA) demonstrates significant improvements in healthcare WSN performance, achieving 32% longer network lifetime compared to HEED, 39% reduction in E2E delay compared to LEACH, and 96.2% patient coverage with energy efficiency of 0.045 J/packet. These quantitative improvements translate to enhanced patient monitoring reliability, reduced maintenance costs, and extended operational periods without battery replacement, directly supporting improved healthcare delivery in both clinical and remote monitoring scenarios.
EEFGA effectively balances patient coverage and energy consumption, leading to extended network lifetimes and reliable data transmission. The algorithm is designed to find the optimal balance between these two competing objectives, ensuring that the WSN provides comprehensive patient monitoring while minimizing energy consumption. This balance is essential for the long-term viability and effectiveness of WSNs in healthcare settings.
Simulation results demonstrate the practical applicability and effectiveness of EEFGA in real-time healthcare monitoring scenarios. The simulations provide evidence that EEFGA can be successfully implemented in real-world healthcare settings, delivering the benefits of energy efficiency and comprehensive patient coverage. The simulations also offer insights into the algorithm's performance under different conditions, helping healthcare providers to optimize its deployment and configuration for their specific needs.
References
- C. Naveeth Babu and V. S. Prakash, "Enhanced medical monitoring wireless sensors networks using proposed greedy multipoint relays protocol algorithm," in Applications of Artificial Intelligence in Engineering: Proceedings of First Global Conference on Artificial Intelligence and Applications (GCAIA 2020), pp. 827–833, Jan. 2021.
- A. Milenković, C. Otto, and E. Jovanov, "Wireless sensor networks for personal health monitoring: Issues and an implementation," Computer Commun., vol. 29, no. 13–14, pp. 2521–2533, Aug. 2006.
- Y. M. Huang, M. Y. Hsieh, H. C. Chao, S. H. Hung, and J. H. Park, "Pervasive, secure access to a hierarchical sensor-based healthcare monitoring architecture in wireless heterogeneous networks," IEEE J. Sel. Areas Commun., vol. 27, no. 4, pp. 400–411, May 2009.
- A. Tauqir, N. Javaid, S. Akram, A. Rao, and S. N. Mohammad, "Distance aware relaying energy-efficient: Dare to monitor patients in multi-hop body area sensor networks," in Proc. 2013 8th Int. Conf. Broadband Wireless Comput. Commun. Appl., pp. 206–213, Oct. 2013.
- R. Rajagopalan, "Energy efficient routing algorithm for patient monitoring in body sensor networks," in Proc. 2016 IEEE 13th Int. Conf. Wearable Implantable Body Sensor Netw. (BSN), pp. 141–146, Jun. 2016.
- H. Taleb, A. Nasser, G. Andrieux, N. Charara, and E. M. Cruz, "Energy consumption improvement of a healthcare monitoring system: application to LoRaWAN," IEEE Sens. J., vol. 22, no. 7, pp. 7288–7299, Apr. 2022.
- Y. W. Lee, K. Y. Lee, and M. H. Kim, "Energy-efficient multiple query optimization for wireless sensor networks," in Proc. 2009 3rd Int. Conf. Sensor Technol. Appl., pp. 531–538, Jun. 2009.
- N. K. Mangali and V. K. Kota, "Health monitoring systems: An energy efficient data collection technique in wireless sensor networks," in Proc. 2015 Int. Conf. Microw., Opt. Commun. Eng. (ICMOCE), pp. 130–133, Dec. 2015.
- M. Pike, N. M. Mustafa, D. Towey, and V. Brusic, "Sensor networks and data management in healthcare: Emerging technologies and new challenges," in Proc. 2019 IEEE 43rd Annu. Comput. Softw. Appl. Conf. (COMPSAC), vol. 1, pp. 834–839, Jul. 2019.
- M. Ilyas, "Wireless sensor networks for smart healthcare," in Proc. 2018 1st Int. Conf. Comput. Appl. Inf. Security (ICCAIS), pp. 1–5, Apr. 2018.
- Z. Zhang and H. Zhou, "A MAC layer protocol supporting the application of WSNs in medicine and healthcare domains," in Proc. 2011 12th ACIS Int. Conf. Softw. Eng., Artif. Intell., Netw. Parallel/Distrib. Comput., pp. 33–37, Jul. 2011.
- C.V. P. Krishna, K. V. D. Kiran, and T. H. Kim, "Integrated distributed architecture to integrate wireless sensor networks (WSN) with grid for healthcare," Int. J. Bio-Sci. Bio-Technol., vol. 7, no. 3, pp. 243–250, Jul. 2015.
- S. Tennina et al., "WSN4QoL: WSNs for remote patient monitoring in e-Health applications," in Proc. 2016 IEEE Int. Conf. Commun. (ICC), pp. 1–6, May 2016.
- H. S. Ng, M. L. Sim, and C. M. Tan, "Security issues of wireless sensor networks in healthcare applications," BT Technol. J., vol. 24, no. 2, pp. 138–144, Apr. 2006.
- M. T. Buyukakkaslar, M. A. Erturk, M. A. Aydin, and L. Vollero, "LoRaWAN as an e-health communication technology," in Proc. 2017 IEEE 41st Annu. Comput. Softw. Appl. Conf. (COMPSAC), vol. 2, pp. 310–313, Jul. 2017.
- Gupta and A. Gupta, "Exploiting ZigBee and BLE," The IoT Hacker's Handbook: A Practical Guide to Hacking the Internet of Things, pp. 265–309, Jan. 2019.
- J. Shi, D. Mu, and M. Sha, "LoRaBee: Cross-technology communication from LoRa to ZigBee via payload encoding," in Proc. 2019 IEEE 27th Int. Conf. Netw. Protocols (ICNP), pp. 1–11, Oct. 2019.
- J. Shi, D. Mu, and M. Sha, "Enabling cross-technology communication from LoRa to ZigBee via payload encoding in Sub-1 GHz bands," ACM Trans. Sens. Netw. (TOSN), vol. 18, no. 1, pp. 1–26, Jan. 2021.
- O. Amjad, E. Bedeer, and S. Ikki, "Energy efficiency maximization of self-sustained wireless body area sensor networks," arXiv preprint arXiv:1910.05444, Oct. 2019.
- F. Xia, Z. Xu, L. Yao, W. Sun, and M. Li, "Prediction-based data transmission for energy conservation in wireless body sensors," arXiv preprint arXiv:0912.2430, Dec. 2009.
- J. Abouei, J. D. Brown, K. N. Plataniotis, and S. Pasupathy, "Energy efficiency and reliability in wireless biomedical implant systems," arXiv preprint arXiv:1101.0906, Jan. 2011. Jan.
- E. Rebeiz, G. Caire, and A. F. Molisch, "Energy-delay tradeoff and dynamic sleep switching for Bluetooth-like body-area sensor networks," arXiv preprint arXiv:1204.4840, Apr. 2012.
- D. Gao and H. Wang, "WiLo: Long-range cross-technology communication from Wi-Fi to LoRa," arXiv preprint arXiv:2301.12345, Jan. 2023.
- H. Mamaghanian, N. Khaled, D. Atienza, and P. Vandergheynst, "Compressed sensing for real-time energy-efficient ECG compression on wireless body sensor nodes," IEEE Trans. Biomed. Eng., vol. 58, no. 9, pp. 2456–2466, Sep. 2011.
- F. Rincon, J. Recas, N. Khaled, and D. Atienza, "Development and evaluation of multi-lead wavelet-based ECG delineation algorithms for embedded wireless sensor nodes," IEEE Trans. Inf. Technol. Biomed., vol. 15, no. 6, pp. 854–863, Nov. 2011.
- Dogan, J. Constantin, M. Ruggiero, A. Burg, and D. Atienza, "Multi-core architecture design for ultra-low-power wearable health monitoring systems," IEEE Trans. Comput.-Aided Des. Integr. Circuits Syst., vol. 34, no. 6, pp. 813–826, Jun. 2015.
- Sridhar, A. Vincenzi, M. Ruggiero, and D. Atienza, "Neural network-based thermal simulation of integrated circuits on GPUs," IEEE Trans. Comput.-Aided Des. Integr. Circuits Syst., vol. 31, no. 1, pp. 23–36, Jan. 2012.
- M. Chen, S. Gonzalez, A. Vasilakos, H. Cao, and V. C. Leung, "Body area networks: A survey," Mobile Netw. Appl., vol. 16, pp. 171–193, Feb. 2011.
- Y. Zhang, L. Sun, H. Song, and H. Cao, "Ubiquitous WSN for healthcare: Recent advances and future prospects," IEEE Internet Things J., vol. 1, no. 4, pp. 311–318, Aug. 2014.
- F. Hu, Y. Xiao, and Q. Hao, "Congestion-aware, loss-resilient biometric data transmission in wireless body sensor networks," IEEE J. Sel. Areas Commun., vol. 27, no. 4, pp. 450–465, May 2009.
- K. Malasri and L. Wang, "Design and implementation of a secure wireless mote-based medical sensor network," Sensors, vol. 9, no. 8, pp. 6273–6297, Aug. 2009.
- E. Jovanov et al., "A wireless body area network of intelligent motion sensors for computer assisted physical rehabilitation," J. NeuroEngineering Rehabil., vol. 2, no. 6, pp. 1–10, Feb. 2005.
- ] Chavan, S. D., & Kulkarni, A. V. (2018). Event Based Clustering Localized Energy Efficient Ant Colony Optimization (EBC_LEE-ACO) for Performance Enhancement of Wireless Sensor Network. Engineering, Technology & Applied Science Research, 8(4), 3177–3183. [CrossRef]
- El-Fouly, F. H., Kachout, M., Ramadan, R. A., Alzahrani, A. J., Alshudukhi, J. S., & Alseadoon, I. M. (2024). Energy-Efficient and Reliable Routing for Real-time Communication in Wireless Sensor Networks. Engineering, Technology & Applied Science Research, 14(3), 13959–13966. [CrossRef]
- Jaleel, M. A., Khan, M. A., Mazhar, T., Khan, J., Zaman, S. K. U., Khattak, U. F., & Batool, S. (2025). An Energy-Efficient Hybrid LEACH Protocol that Enhances the Lifetime of Wireless Sensor Networks. Engineering, Technology & Applied Science Research, 15(1), 19364–19369. [CrossRef]
- U. Feige, "A threshold of ln n for approximating set cover," Journal of the ACM, vol. 45, no. 4, pp. 634-652, Jul. 1998.
- G. L. Nemhauser, L. A. Wolsey, and M. L. Fisher, "An analysis of approximations for maximizing submodular set functions," Mathematical Programming, vol. 14, no. 1, pp. 265-294, Dec. 1978.
- Boukerche and S. Darehshoorzadeh, "Opportunistic routing in wireless networks: Models, algorithms, and classifications," ACM Computing Surveys, vol. 47, no. 2, pp. 1-36, Nov. 2014."\.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).