1. Introduction
Preterm birth remains a major global health challenge. In 2020, an estimated 13.4 million babies, approximately 1 in 10 births worldwide, occurred before 37 weeks’ gestation, with little improvement in rates over the last decade [
1]. Prematurity is the leading cause of neonatal mortality and contributes substantially to morbidity, prolonged hospitalization, and long-term developmental impairment [
2]. Global neonatal mortality reached 2.3 million deaths in 2022, nearly half of all deaths among children under five [
2].
Epidemiological analyses consistently show that the burden of prematurity is high across countries and healthcare systems. A recent study reported a 23% prevalence of prematurity among all live births in a reference neonatal intensive care unit (NICU), identifying primigravidity and hypertensive disorders of pregnancy as major risk factors, whereas adequate prenatal care acted as a protective factor [
3]. These findings reinforce the multifactorial nature of prematurity and highlight the persistent global challenge of reducing both its incidence and its complications.
Among the clinical complications associated with prematurity, respiratory morbidity is particularly prevalent. Neonatal respiratory distress syndrome (RDS) remains one of the most frequent causes of acute respiratory failure in preterm infants, with incidence rates reaching 40–70% in very low birth-weight neonates depending on gestational age [
4]. Bronchopulmonary dysplasia (BPD), the main chronic sequela of prematurity, emerges from the interaction of lung immaturity, oxygen exposure, infection and ventilator-induced injury, often resulting in long-term respiratory impairment and increased healthcare utilization [
5].
Despite advances in antenatal corticosteroids, surfactant therapy, non-invasive ventilation and lung-protective strategies, the prevalence of these complications remains high [
6]. Consequently, current neonatal care increasingly emphasizes not only survival but also the prevention of lung injury, reduction of invasive ventilation, and optimization of long-term pulmonary development.
In this context, respiratory physiotherapy has gained attention as a non-pharmacological and non-invasive adjunct therapy aimed at improving ventilation distribution, enhancing secretion clearance and reducing work of breathing. Techniques such as prolonged slow expiration, expiratory flow increase, postural management and other gentle manual approaches have been examined in preterm infants with RDS or BPD. Previous evidence suggests potential benefits in oxygenation, respiratory and heart rate stabilization, reduction of atelectasis, decreased duration of mechanical ventilation and shorter hospitalization, generally without significant adverse events [
7,
8,
9,
10,
11].
Nevertheless, the evidence remains heterogeneous. Clinical trials report variable protocols, different treatment frequencies and inconsistent endpoints, limiting the ability to draw firm conclusions. Safety concerns persist, especially in extremely preterm infants, stemming from isolated reports of iatrogenic injuries with inappropriate or vigorous techniques [
12]. A recent systematic review found that respiratory physiotherapy consistently improved pulmonary mechanics, oxygenation and short-term physiological stability, but again emphasized the lack of standardized methodology and the need for high-quality long-term studies [
13].
Despite the growing interest and expanding literature, no consensus currently exists regarding which respiratory physiotherapy modalities should be routinely implemented, how they should be integrated with modern respiratory support or which preterm subgroups benefit most. Existing reviews often combine term and preterm infants, focus on only one technique or pre-date recent randomized trials.
The aim of this comprehensive review is to provide an updated and clinically oriented synthesis of respiratory physiotherapy techniques in preterm neonates with RDS or BPD, describing their mechanisms, effects on pulmonary function, physiological stability, respiratory support requirements and clinical outcomes, as well as their safety profile. Based on the available evidence, we hypothesize that well-structured respiratory physiotherapy may represent a safe and valuable adjunct to standard medical care.
2. Materials and Methods
2.1. Study Design
This study was conducted as a comprehensive literature review using a structured search strategy, while maintaining the flexibility of a narrative synthesis. The aim was to identify, summarize and critically discuss the clinical evidence on respiratory physiotherapy interventions in preterm infants diagnosed with RDS or BPD. This design enabled a rigorous and extensive exploration of the available literature without adhering to the procedural requirements of systematic reviews.
2.2. Search Strategy
A structured literature search was conducted between November 2024 and January 2025 in the following electronic databases: Web of Science (WOS), PubMed, Scopus, Cochrane Library, PEDro and ScienceDirect.
The search strategy combined Medical Subject Headings (MeSH) and free-text terms related to prematurity, neonatal respiratory disease and respiratory physiotherapy. MeSH terms included “preterm”, “premature”, “bronchopulmonary dysplasia”, “respiratory distress syndrome”, “hyaline membrane”, “pulmonary diseases”, “physical therapy”, and “physiotherapy”. To enhance sensitivity, additional free terms such as “respiratory diseases”, “rehabilitation”, and “chest physiotherapy” were incorporated.
Boolean operators were applied as follows: OR to combine synonyms or related concepts; AND to link population, condition and intervention terms.
As an example, the search strategy used in WOS was as follows: (“premature” OR “preterm”) AND (“respiratory distress syndrome” OR “bronchopulmonary dysplasia” OR “hyaline membrane” OR “respiratory diseases” OR “pulmonary diseases”) AND (“physical therapy” OR “physiotherapy” OR “rehabilitation” OR “chest physiotherapy”)
2.3. Eligibility Criteria
Articles were selected based on predefined eligibility criteria.
Inclusion criteria:
Population: preterm infants (<37 weeks of gestation) with a medical diagnosis of RDS or BPD.
Intervention: any respiratory physiotherapy technique or modality.
Study design: randomized controlled trials.
Publication period: January 2014 to January 2025.
Language: English or Spanish.
Exclusion criteria:
Preterm infants presenting major comorbidities (e.g., congenital malformations, genetic syndromes, significant cardiovascular abnormalities).
Studies for which full-text access was not available.
2.4. Study Selection and Data Extraction
Study selection was performed by a single reviewer (P.R.R.), with a second reviewer (M.J.A.A.) consulted whenever uncertainty arose regarding eligibility.
Given the comprehensive and narrative nature of this review, studies were selected based on their relevance, clinical content and contribution to understanding the effects of respiratory physiotherapy on preterm infants with RDS or BPD.
All retrieved records were exported to Mendeley, where duplicate entries were identified and removed. Screening proceeded in two stages: (1) Title and abstract screening, to exclude clearly irrelevant studies or those not meeting basic eligibility criteria and (2) Full-text assessment, to confirm compliance with all inclusion and exclusion criteria.
For each included study, the following information was manually extracted: authorship, year of publication, sample size and characteristics, intervention details, outcome measures, principal findings and authors’ conclusions. Extracted data were compiled into a structured table to support qualitative synthesis and comparison across studies.
2.5. Quality Assessment
Although this comprehensive review did not include a formal risk-of-bias assessment credibility and reliability were ensured through the use of a structured search strategy and the inclusion of studies published exclusively in peer-reviewed scientific journals. This approach is consistent with the methodological expectations for comprehensive and narrative reviews, which emphasize breadth of coverage, critical interpretation and integration of evidence rather than quantitative synthesis.
2.6. Use of Generative Artificial Intelligence
Generative artificial intelligence (GenAI) tools were used exclusively for the creation of selected graphical elements associated with this review. GenAI was not used for data extraction, study screening, analysis or interpretation. All decisions regarding study inclusion, methodological assessment and evidence synthesis were made independently by the authors.
3. Manual Techniques for Enhancing Ventilatory Mechanics and Expiratory Flow
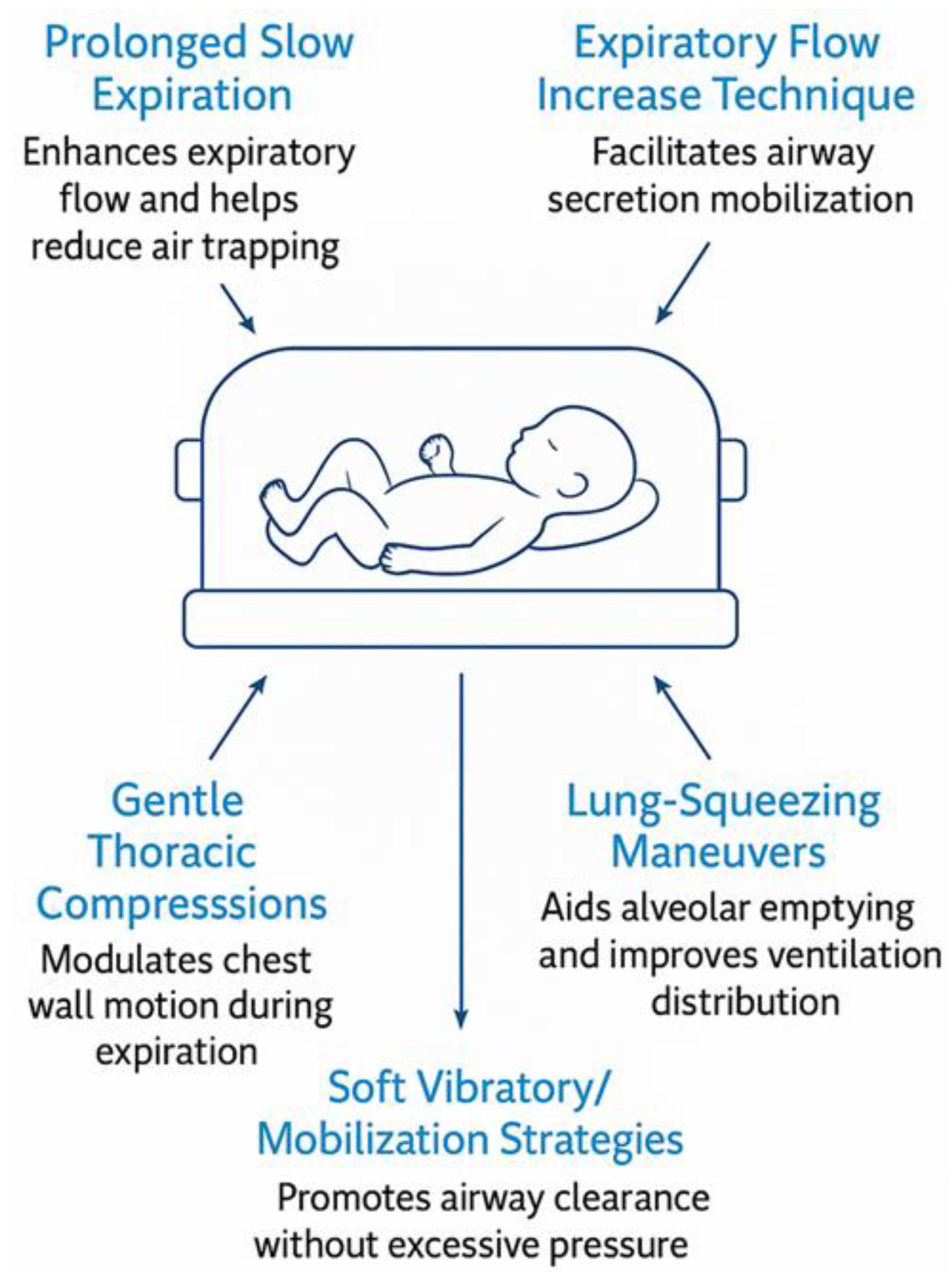
Manual respiratory physiotherapy techniques constitute the most extensively represented group of interventions among the studies included in this review. These techniques—applied with gentle, controlled maneuvers—seek to optimize expiratory flow, mobilize secretions, re-expand atelectatic areas and support more efficient ventilatory mechanics in premature infants with respiratory distress.
Across the analyzed trials, clinicians employed a variety of manual methods (
Figure 1) such as prolonged slow expiration (PLE), the Expiratory Flow Increase Technique (EFIT), gentle thoracic compressions, lung squeezing maneuvers, and soft vibratory or mobilization strategies (14–20). All of these were delivered in synchrony with spontaneous breathing, respecting the physiological fragility of the premature lung and aiming to modulate expiratory flow without generating excessive intrathoracic pressure.
In a randomized trial involving mechanically ventilated preterm infants, a research group in Brazil demonstrated that EFIT and conventional chest physiotherapy produced immediate improvements in oxygen saturation (SpO₂), decreased respiratory rate and reduced pain scores following treatment [
14]. Further physiological benefits were reported in a study led by an Indian neonatal team, where a single session of chest mobilization improved ventilatory patterns and reduced the work of breathing both in extubated and ventilated infants [
15].
Manual techniques were also applied with the goal of resolving atelectasis, a frequent complication in RDS. In a clinical investigation focused on lobar collapse, lung squeezing contributed to significant radiological improvement and better oxygenation profiles within 24 hours of treatment [
20]. Similarly, another trial conducted on extremely preterm infants with severe respiratory distress documented earlier normalization of breath sounds and improved ventilatory patterns when gentle chest physiotherapy techniques were used [
17].
It is important to note that all contemporary studies reported excellent safety, with no adverse events observed when techniques were performed by trained neonatal physiotherapists. Historical reports of rib fractures after vigorous compressions [
11] highlight the need for expertise, but they do not reflect current professional practice.
Overall, the evidence suggests that well-executed manual techniques can yield rapid and clinically meaningful improvements in oxygenation, thoracoabdominal synchrony, secretion mobilization and general respiratory stability.
4. Positioning and Postural Management in Respiratory Support
Positioning strategies represent some of the safest and most physiologically grounded interventions available for premature infants. Because neonatal ribcage structure, diaphragmatic function and lung compliance are highly sensitive to gravity, therapeutic positioning can markedly influence ventilation distribution and gas exchange.
Multiple studies show that specific postures lead to meaningful improvements in respiratory function (
Table 1). In a randomized clinical trial conducted in Indonesia, the quarter-prone position significantly increased SpO₂ in preterm infants receiving continuous positive airway pressure (CPAP), demonstrating more favorable lung recruitment than the supine posture [
22]. Comparable benefits were documented in a Brazilian study evaluating CPAP users, where prone and lateral positions promoted better thoracoabdominal synchrony and more homogeneous ventilation distribution [
29].
Earlier physiological evidence, such as research carried out in the United States with preterm infants hospitalized for lung disease, also indicated that prone positioning increases lung volumes and reduces areas of dorsal atelectasis compared with the supine position [
28]. These findings align with neonatal physiology: prone posture improves diaphragmatic efficiency, reduces anterior ribcage distortion and helps maintain functional residual capacity.
A particularly significant contribution comes from a multicenter clinical trial comparing conventional respiratory physiotherapy to an individualized postural care program. In this investigation, infants receiving tailored positioning strategies experienced a greater reduction in mechanical ventilation time than those assigned to chest physiotherapy, underscoring the therapeutic value of optimized posture even in critically ill infants [
19].
Positioning therefore emerges as a foundational respiratory support tool non-invasive, physiologically sound and applicable to virtually all preterm infants, particularly those in whom excessive handling must be avoided.
5. Reflex-Based and Neurodevelopmental Approaches
Reflex-based approaches, particularly those inspired by Vöjta therapy, aim to activate innate neuromotor patterns that facilitate respiratory muscle engagement. By stimulating specific trigger zones, these methods seek to influence not only the respiratory system but also global motor organization and autonomic regulation. One of the most relevant contributions in this area comes from a Spanish research team who applied Vöjta reflex rolling to preterm infants with RDS or BPD. Their work showed improvements in oxygenation, reduction in respiratory distress signs and enhanced neuromotor organization shortly after therapy sessions [
23]. These effects suggest that reflex-based interventions may support respiratory mechanics through improved intercostal activation and diaphragmatic recruitment (
Figure 2).
Additional insight comes from a randomized trial combining lung squeezing with reflex rolling, where the intervention produced greater increases in SpO₂ than lung squeezing alone [
14]. This suggests a potential synergistic effect when respiratory techniques are integrated with reflex-based neuromotor activation.
Although the evidence base remains smaller than for manual or postural techniques, the available data indicate that reflex-based interventions may be particularly beneficial in infants with altered thoracoabdominal synchrony, weak respiratory muscle recruitment or delayed neuromotor development.
6. Multimodal Rehabilitation Strategies Integrating Respiratory, Postural and Motor Components
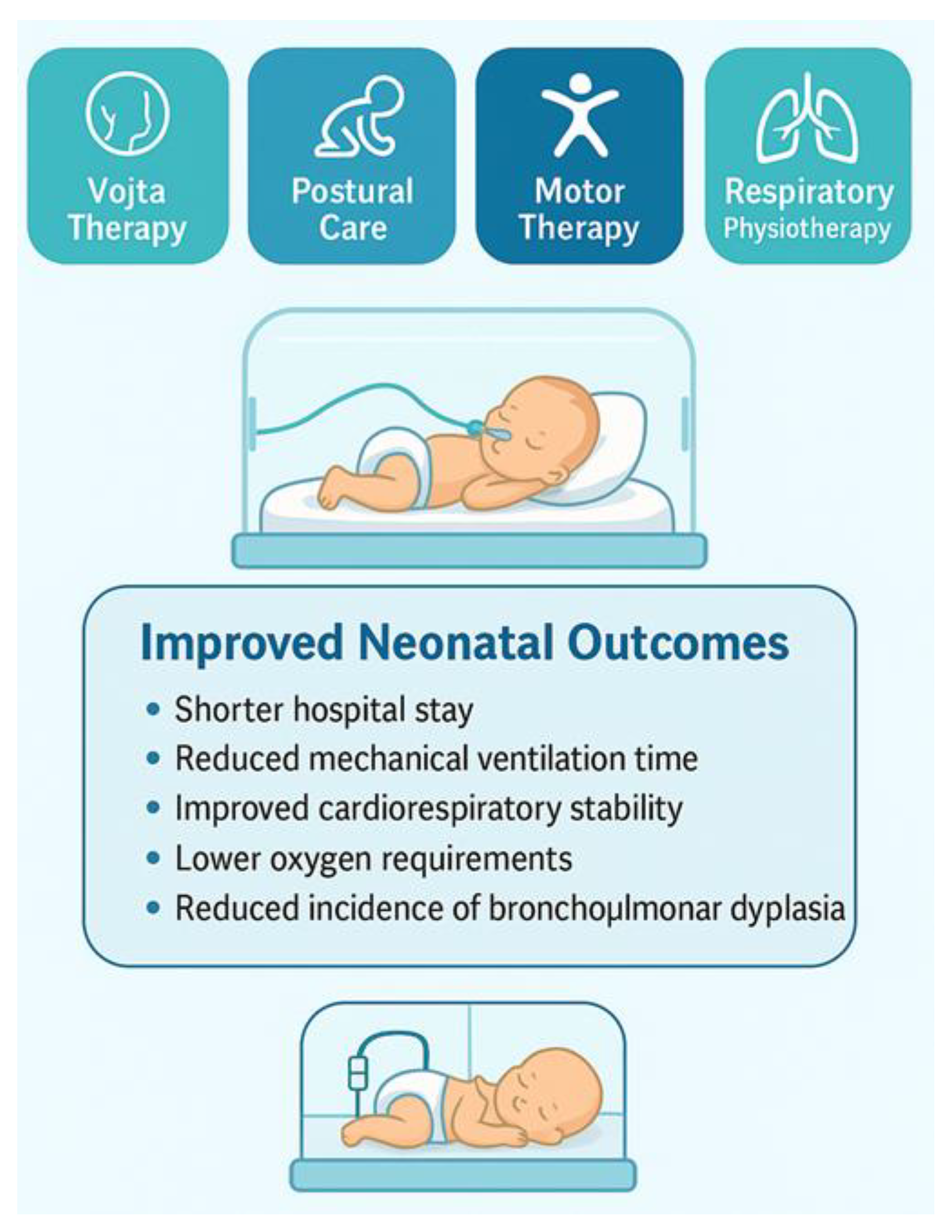
Some of the most promising interventions identified in this review are those that combine respiratory physiotherapy with broader developmental and postural strategies. These multimodal approaches aim to address the complex physiological and neuromotor needs of premature infants more comprehensively than isolated methods.
A particularly notable example is a structured early rehabilitation program implemented in a neonatal unit in China, which included respiratory physiotherapy, neuromotor stimulation, postural management and orofacial therapy. Infants receiving this combined intervention showed significantly shorter hospital stays, reduced oxygen supplementation and fewer days of mechanical ventilation. The program also yielded a lower incidence of BPD, making it one of the most impactful interventions identified [
21].
Another relevant contribution originates from a Brazilian study exploring the combination of chest physiotherapy with motor stimulation activities. This integrated approach produced stronger improvements in cardiovascular and respiratory stability than respiratory techniques alone, suggesting that the synergy between motor control and respiratory mechanics can enhance physiological regulation [
27].
Such evidence highlights the potential of multimodal strategies to improve clinical outcomes by addressing not only the respiratory system but also neuromotor maturation, behavioral state organization and overall cardiorespiratory stability (
Figure 3).
7. Synthesis of Evidence Across Respiratory Physiotherapy Modalities
When integrating findings across all included trials, several consistent patterns emerge regarding the effects of respiratory physiotherapy in preterm infants:
7.1. Immediate Physiological Benefits
Increases in SpO₂ (14–20, 22)
Reductions in RR and improved heart rate stability (16–18)
Better breath sounds and improved auscultatory findings (14, 20)
Improved respiratory support parameters
Faster radiological resolution of atelectasis (14, 20)
Decreased FiO₂ requirements (19, 22)
Enhanced ventilatory patterns in ventilated preterm infants (15, 17)
7.2. Medium- to Long-Term Clinical Improvements in Multimodal Programs
Decreased hospitalization duration (13, 21, 23)
Reduced mechanical ventilation days (13, 23)
Lower incidence of BPD in one comprehensive intervention trial [
21]
7.3. Safety
All modern studies reported excellent tolerance and no significant adverse events, reinforcing that physiotherapy techniques—when performed appropriately—are safe for preterm infants. Historical concerns stem from outdated techniques no longer representative of current practice [
11].
8. Discussion
The purpose of this comprehensive review was to integrate current evidence on respiratory physiotherapy in preterm infants with RDS or BPD, clarifying its physiological effects, clinical relevance and safety. Overall, the findings suggest that respiratory physiotherapy, whether through manual expiratory modulation, postural strategies or neurodevelopmentally oriented techniques, can produce meaningful short-term improvements in gas exchange, ventilation efficiency, secretion clearance and physiological stability. Although variability between trials prevents firm conclusions regarding superiority of one technique over another, the consistency of observed benefits reinforces its potential role as an adjunctive therapy within neonatal respiratory care.
The observations of this review align with findings from earlier systematic and narrative reviews on neonatal respiratory physiotherapy. Over the past decade, only three systematic reviews have addressed this topic in depth, highlighting both the scarcity of high-quality evidence and the persistent heterogeneity of methodologies. A recent synthesis, published in 2023 [
24] included a mix of randomized clinical trials, quasi-experimental studies and case–control designs, reporting improvements in oxygenation and respiratory effort following physiotherapy interventions. Another sytematic review, focused largely on postural and airway-clearance approaches, incorporated randomized and crossover trials and concluded that physiotherapy may reduce respiratory workload and facilitate ventilation in premature infants [
25]. These trends are consistent with the findings of this comprehensive review.
The methodological approaches of previous reviews also anticipated some of the challenges encountered here. Earlier syntheses relied on broad tools to appraise study quality [
24,
25], highlighting risks of bias and variability in intervention delivery. The present review confirms these limitations: although the evidence supports potential clinical benefits, the methodological heterogeneity of primary studies continues to impede more definitive recommendations.
Across the literature, respiratory and motor physiotherapy techniques have demonstrated beneficial effects on cardiorespiratory stability, in preterm neonates. Research integrating thoracic and motor stimulation showed improvements in cardiovascular parameters and secretion clearance in preterm infants with RDS, supporting the physiological rationale for combining respiratory and motor components in neonatal care [
27]. Similarly, a case report examining thoracic compressions and the EFIT described notable improvements in bronchial secretion clearance in infants with acute respiratory deterioration [
30], which aligns with trends observed in several randomized trials.
Conventional respiratory physiotherapy, autogenic drainage and prolonged slow expiration have also been shown to assist in reducing ventilatory support requirements and reversing atelectasis. These effects are coherent with clinical improvements documented in studies employing positive expiratory pressure devices, where enhancements in respiratory parameters and gradual reductions in oxygen dependence were observed throughout the course of hospitalization [
31].
Nevertheless, not all physiological markers responded uniformly across studies. For example, while some investigations documented improvements in the fraction of FiO₂ after physiotherapy, others reported no significant changes likely reflecting differences in therapeutic intensity, duration or underlying lung pathology rather than contradictory evidence. Pain and discomfort also appeared unaffected by gentle, developmentally respectful techniques, reinforcing their suitability for fragile preterm infants [
32].
Postural interventions likewise demonstrated promising effects. A study investigating various body positions in preterm infants receiving pressure CPAP reported improvements in oxygenation and ventilation distribution [
33], supporting the inclusion of postural optimization within multimodal rehabilitation strategies. The consistency between postural and manual approaches highlights the interdependence of thoracic mechanics, diaphragmatic function and global respiratory efficiency in premature newborns.
Safety remains a central concern in the application of respiratory physiotherapy in preterm neonates. Although historical cases described iatrogenic rib fractures following inappropriate chest physiotherapy techniques [
11], no such adverse events were reported in recent trials employing gentle, synchronized, developmentally guided interventions. This shift reflects an evolution in neonatal physiotherapy practice, prioritizing controlled expiratory flow modulation and biomechanically safe handling. The absence of increased intracranial hemorrhage risk in infants treated with early combined rehabilitation further supports the safety of physiotherapy in this population [
21].
8.1. Limitations
Several limitations must be acknowledged. First, although the search strategy was structured and conducted across major biomedical databases, exhaustive systematic retrieval was not the goal of this article type; therefore, some relevant studies may not have been captured. Second, the underlying evidence remains constrained by small sample sizes, single-center designs and short follow-up, limiting generalizability and preventing conclusions about long-term respiratory or neurodevelopmental outcomes. Third, substantial heterogeneity exists in intervention protocols, treatment duration and outcome measures, precluding quantitative synthesis. Finally, without a formal risk-of-bias assessment, interpretations must rely on qualitative appraisal and consistency of findings rather than hierarchical evidence grading.
8.2. Clinical Implications
The findings of this review have practical significance for neonatal care teams. Gentle respiratory physiotherapy, delivered by clinicians trained in neonatal respiratory management, can support lung function, assist in secretion clearance, stabilize oxygenation and reduce respiratory workload in preterm infants. When integrated into multimodal rehabilitation strategies that include postural alignment, sensorimotor stimulation and individualized respiratory support, respiratory physiotherapy may help decrease the duration of mechanical ventilation, minimize pulmonary complications and enhance early functional stability. These benefits reinforce the value of incorporating respiratory physiotherapy within multidisciplinary neonatal intensive care pathways, always prioritizing safety, synchrony with spontaneous breathing and individualized assessment.
9. Conclusions
Respiratory physiotherapy emerges as a valuable adjunct within the multidisciplinary management of preterm infants with respiratory distress syndrome or bronchopulmonary dysplasia. The techniques described in the literature consistently demonstrate short-term improvements in oxygenation, ventilation distribution, secretion clearance and overall physiological stability.
When delivered with appropriate clinical expertise, these interventions appear safe even in extremely preterm and medically fragile infants.
Despite encouraging evidence, the field remains characterized by methodological heterogeneity, variability in treatment protocols and limited sample sizes. These factors constrain definitive conclusions regarding the optimal techniques, timing and dosing of physiotherapy interventions.
The available evidence positions respiratory physiotherapy as a promising, non-pharmacological and non-invasive strategy that can complement respiratory support and medical and nurse cares, help reduce complications and potentially contribute to improved early respiratory outcomes in preterm infants.
10. Future Directions
Future research on respiratory physiotherapy in preterm infants must prioritize methodological rigor, standardized intervention protocols and long-term outcome assessment. High-quality randomized clinical trials, with adequately powered sample sizes, are needed to determine the relative effectiveness of specific techniques, establish optimal treatment frequency and dosing and clarify which physiological subgroups derive the greatest benefit. Harmonizing definitions, intervention components and outcome measures across studies would facilitate comparability and allow for more robust meta-analytic integration.
A deeper understanding of the mechanistic effects of respiratory physiotherapy is also required. Advanced imaging modalities, lung function monitoring and real-time assessments of thoracoabdominal synchrony could help elucidate how manual and postural interventions modulate respiratory biomechanics in preterm infants with immature lung structure.
Longitudinal studies are essential to determine whether early physiotherapy contributes to sustained improvements beyond acute physiological stabilization, including long-term pulmonary function, neuromotor development, hospitalization trajectories and healthcare utilization.
As neonatal care increasingly embraces individualized and family-centered models, evaluating the feasibility of physiotherapy protocols across diverse clinical settings, including low-resource environments, will also be critical.
Author Contributions
Conceptualization, P.R.-R. and M.J.A.-A.; methodology, P.R.-R., M.J.A.-A., R.L.-R. and A.P.-C.; validation, P.R.-R. and M.J.A.-A.; formal analysis, M.J.A.-A., R.L.-R. and A.P.-C.; investigation, P.R.-R., M.J.A.-A., R.L.-R. and A.P.-C.; resources, P.R.-R., M.J.A.-A., R.L.-R. and A.P.-C.; data curation, R.L.-R..; writing—original draft preparation, P.R.-R. and M.J.A.-A..; writing—review and editing, P.R.-R., M.J.A.-A., R.L.-R., A.P.-C..; visualization, P.R.-R., M.J.A.-A., R.L.-R. and A.P.-C.; supervision, M.J.A.-A., R.L.-R. and A.P.-C. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
No applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data were created.
Acknowledgments
During the preparation of this manuscript, the authors used ChatGPT (OpenAI, GPT-5.1 model) to assist with the generation of illustrative concepts for figures. All content produced with the assistance of this tool was critically reviewed, verified and edited by the authors, who take full responsibility for the accuracy, integrity and originality of the final publication.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| MDPI |
Multidisciplinary Digital Publishing Institute |
| DOAJ |
Directory of open access journals |
| TLA |
Three letter acronym |
| LD |
Linear dichroism |
References
- Ohuma EO, Moller A-B, Bradley E, Chakwera S, Hussain-Alkhateeb L, Lewin A, et al. National, regional, and global estimates of preterm birth in 2020, with trends from 2010: a systematic analysis. Lancet. 2023;402(10409):1261–71. [CrossRef]
- World Health Organization. Newborn mortality: Key facts [Internet]. Geneva: WHO; 2024 [consulted 12 May 2025]. Available from: https://www.who.int/news-room/fact-sheets/detail/newborn-mortality.
- Barreto MGP, Manso MC, Barreto RP, Barreto RP, Vasconcelos LMT, Silva C. Frequency and Risk Factors Associated with Prematurity: A Cohort Study in a Neonatal Intensive Care Unit. J Clin Med. 2024;13:4437.
- Yadav S, Lee B. Neonatal respiratory distress syndrome. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2025.
- Kalikkot Thekkeveedu R, Guaman MC, Shivanna B. Bronchopulmonary dysplasia: A review of pathogenesis and pathophysiology. Respir Med. 2017;132:170–7. [CrossRef]
- Igual-Blasco A, Piñero-Peñalver J, Fernández-Rego FJ, Torró-Ferrero G, Pérez-López J. Effects of chest physiotherapy in preterm infants with respiratory distress syndrome: a systematic review. Healthcare (Basel). 2023;11(8):1091. [CrossRef]
- Tana M, Bottoni A, Cota F, Papacci P, Di Polito A, Campagnola B, et al. Respiratory physiotherapy versus an individualized postural care program for reducing mechanical ventilation in preterm infants: a randomised controlled trial. Trials. 2021;22(1):1761. [CrossRef]
- Macedo JC de, Olivo CR, Barnabé V, Dias ED, Moraes ÍAP de, Tibério I de FLC, et al. Short-term effects of conventional chest physiotherapy and expiratory flow increase technique on respiratory parameters, heart rate, and pain in mechanically ventilated premature neonates: A randomized controlled trial. Healthcare (Basel). 2024;12(23):2408.
- De Abreu LC, Valenti VE, de Oliveira AG, Leone C, Siqueira AA, Herreiro D, et al. Chest-associated motor physiotherapy improves cardiovascular variables in newborns with respiratory distress syndrome. Int Arch Med. 2011;4(1):37. [CrossRef]
- Gomez-Conesa A, Fernández Rego FJ, Agüera Arenas JJ. Vojta therapy in the reduction of perinatal risk in preterm infants with respiratory distress syndrome and bronchopulmonary dysplasia. Physiotherapy. 2016;102:e199. [CrossRef]
- Chanelière C, Moreux N, Pracros J-P, Bellon G, Reix P. Rib fractures after chest physiotherapy: a report of 2 cases. Arch Pediatr. 2006;13(11):1410–2.
- Nunes A de M, Fernandes ATSF, de Castro Silva AT, Pereira SA. Effects of respiratory physiotherapeutic interventions on pulmonary mechanics, vital parameters and pain in newborns: a systematic review. Can J Respir Ther. 2025;61:145–56.
- Liu Y, Li ZF, Zhong YH, Zhao ZH, Deng WX, Chen LL, et al. Early combined rehabilitation intervention to improve the short-term prognosis of premature infants. BMC Pediatr. 2021;21(1):269. [CrossRef]
- Probst VS, Soares DS, Escobar VC, et al. Effect of bucket hydrotherapy on clinical parameters in infants with bronchopulmonary dysplasia: A pilot randomized clinical trial. Can J Respir Ther. 2025;61. [CrossRef]
- Mendoza JC, Roberts JL, Cook LN. Postural effects on pulmonary function and heart rate of preterm infants with lung disease. J Pediatr. 1991;118(3):445–8. [CrossRef]
- Brunherotti MA, Martinez EZ, Martinez FE. Effect of body position on preterm newborns receiving continuous positive airway pressure. Acta Paediatr. 2014;103(3):e101–5. [CrossRef]
- Hough JL, Johnston L, Brauer SG, Woodgate PG, Pham TMT, Schibler A. Effect of body position on ventilation distribution in preterm infants on continuous positive airway pressure. Pediatr Crit Care Med. 2012;13(4):446–51. [CrossRef]
- Kole J, Metgud D. Effect of lung squeeze technique and reflex rolling on oxygenation in preterm neonates with respiratory problems: A randomized controlled trial. Indian J Health Sci Biomed Res. 2014;7(1):15.
- Thacker NJ, Patel SB, Patel NS. Effect of lung squeezing technique for correcting atelectasis in mechanically ventilated preterm infants with respiratory distress syndrome. Int J Allied Med Sci Clin Res. 2014;2(4):433–8.
- Utario Y, Rustina Y, Waluyanti FT. The quarter prone position increases oxygen saturation in premature infants using continuous positive airway pressure. Compr Child Adolesc Nurs. 2017;40:95–101. [CrossRef]
- Gomez-Conesa A, Fernández Rego FJ, Agüera Arenas JJ. Vojta therapy in the reduction of perinatal risk in preterm infants with respiratory distress syndrome and bronchopulmonary dysplasia. Physiotherapy. 2016;102:e199. [CrossRef]
- Tavares AB, Treichel L, Ling CC, Scopel GG, Lukrafka JL. Fisioterapia respiratória não altera agudamente os parâmetros fisiológicos ou os níveis de dor em prematuros com síndrome do desconforto respiratório internados em unidade de terapia intensiva. Fisioter Pesqui. 2019;26(4):373–9.
- Mehta Y, Shetye J, Nanavati R, Mehta A. Physiological effects of a single chest physiotherapy session in mechanically ventilated and extubated preterm neonates. J Neonatal Perinatal Med. 2016;9(4):371–6. [CrossRef]
- Igual-Blasco A, Piñero-Peñalver J, Fernández-Rego FJ, Torró-Ferrero G, Pérez-López J. Effects of chest physiotherapy in preterm infants with respiratory distress syndrome: a systematic review. Healthcare (Basel). 2023;11(8):1091. [CrossRef]
- Bhandari AP, Nnate DA, Vasanthan L, Konstantinidis M, Thompson J. Positioning for acute respiratory distress in hospitalised infants and children. Cochrane Database Syst Rev. 2022;6(6):CD003645. [CrossRef]
- Ferguson KN, Roberts CT, Manley BJ, Davis PG. Intervenciones para mejorar las tasas de extubación exitosa en bebés prematuros: una revisión sistemática y un metanálisis. JAMA Pediatr. 2017;171(2):165–74.
- De Abreu LC, Valenti VE, de Oliveira AG, Leone C, Siqueira AA, Herreiro D, et al. Chest-associated motor physiotherapy improves cardiovascular variables in newborns with respiratory distress syndrome. Int Arch Med. 2011;4(1):37. [CrossRef]
- Aherrao S, Sharath HV. Effect of thoracic squeezing technique and expiratory flow increase technique on neonates with neonatal respiratory distress syndrome: a case report. Cureus. 2024;16(9):e68702. [CrossRef]
- Ferrara PE, Gatto DM, Codazza S, Zordan P, Stefinlongo G, Di Polito A, et al. PEP mask therapy for the rehabilitation of a pre-term infant with respiratory distress syndrome: a case report. Eur J Phys Rehabil Med. 2023;59(3):436–9. [CrossRef]
- Tavares AB, Treichel L, Ling CC, Scopel GG, Lukrafka JL. Fisioterapia respiratória não altera agudamente os parâmetros fisiológicos ou os níveis de dor em prematuros com síndrome do desconforto respiratório internados em unidade de terapia intensiva. Fisioter Pesqui. 2019;26(4):373–9.
- Hough JL, Johnston L, Brauer SG, Woodgate PG, Pham TMT, Schibler A. Effect of body position on ventilation distribution in preterm infants on continuous positive airway pressure. Pediatr Crit Care Med. 2012;13(4):446–51. [CrossRef]
- Chanelière C, Moreux N, Pracros J-P, Bellon G, Reix P. Rib fractures after chest physiotherapy: a report of 2 cases. Arch Pediatr. 2006;13(11):1410–2.
- Nunes A de M, Fernandes ATSF, de Castro Silva AT, Pereira SA. Effects of respiratory physiotherapeutic interventions on pulmonary mechanics, vital parameters and pain in newborns: a systematic review. Can J Respir Ther. 2025;61:145–56.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).