1. Introduction
Extramammary Paget’s disease (EMPD) is a rare intraepithelial adenocarcinoma that primarily affects apocrine gland–bearing skin, most commonly the vulvar, perianal, and genital regions [
1]. First described by Crocker in 1889 [
2], EMPD represents a distinct clinical and pathological entity from mammary Paget’s disease, although both share histopathological features, including the presence of large, pale-staining Paget cells within the epidermis [
3]. EMPD predominantly affects postmenopausal women, particularly in the vulvar region [
4]. EMPD is a rare cutaneous adenocarcinoma that typically arises in older adults (around 50–80 years of age). Notably, its incidence and gender predilection vary by region and ethnicity: Western cohorts show a female predominance (EMPD is 2–7 times more common in women), whereas Asian populations show a male predominance (about 3.5:1 in favor of men). Indeed, Asian males have the highest reported incidence of EMPD. Commonly affected sites are the vulva in women and the penoscrotal or adjacent truncal areas in men; by contrast, cases in atypical locations (such as the suprapubic region) are seldom documented. This epidemiologic profile highlights why reporting a rare male case in an unusual location (suprapubic skin) is particularly valuable for the medical literature [
5].
Clinically, EMPD often presents as a slowly enlarging, erythematous, pruritic, and eczematous lesion, frequently leading to delayed diagnosis due to its nonspecific appearance and resemblance to benign dermatologic conditions such as dermatitis or fungal infections [
5]. Histopathological examination remains the gold standard for diagnosis [
6], with immunohistochemical staining aiding in differentiating primary EMPD from secondary involvement by underlying adnexal or visceral malignancies [
7].
In addition to a primary intraepidermal origin, EMPD-like lesions may also result from epidermotropic spread of malignant cells or direct extension from an underlying internal carcinoma [
8]. While surgical excision remains the mainstay of treatment, recurrence rates are high, and the disease can be associated with regional or distant metastasis in invasive cases [
9]. Given its rarity, heterogeneity in presentation, and potential for malignancy, EMPD continues to pose significant diagnostic and therapeutic challenges, warranting further investigation into its molecular biology, prognostic factors, and optimal management strategies.
2. Case Presentation
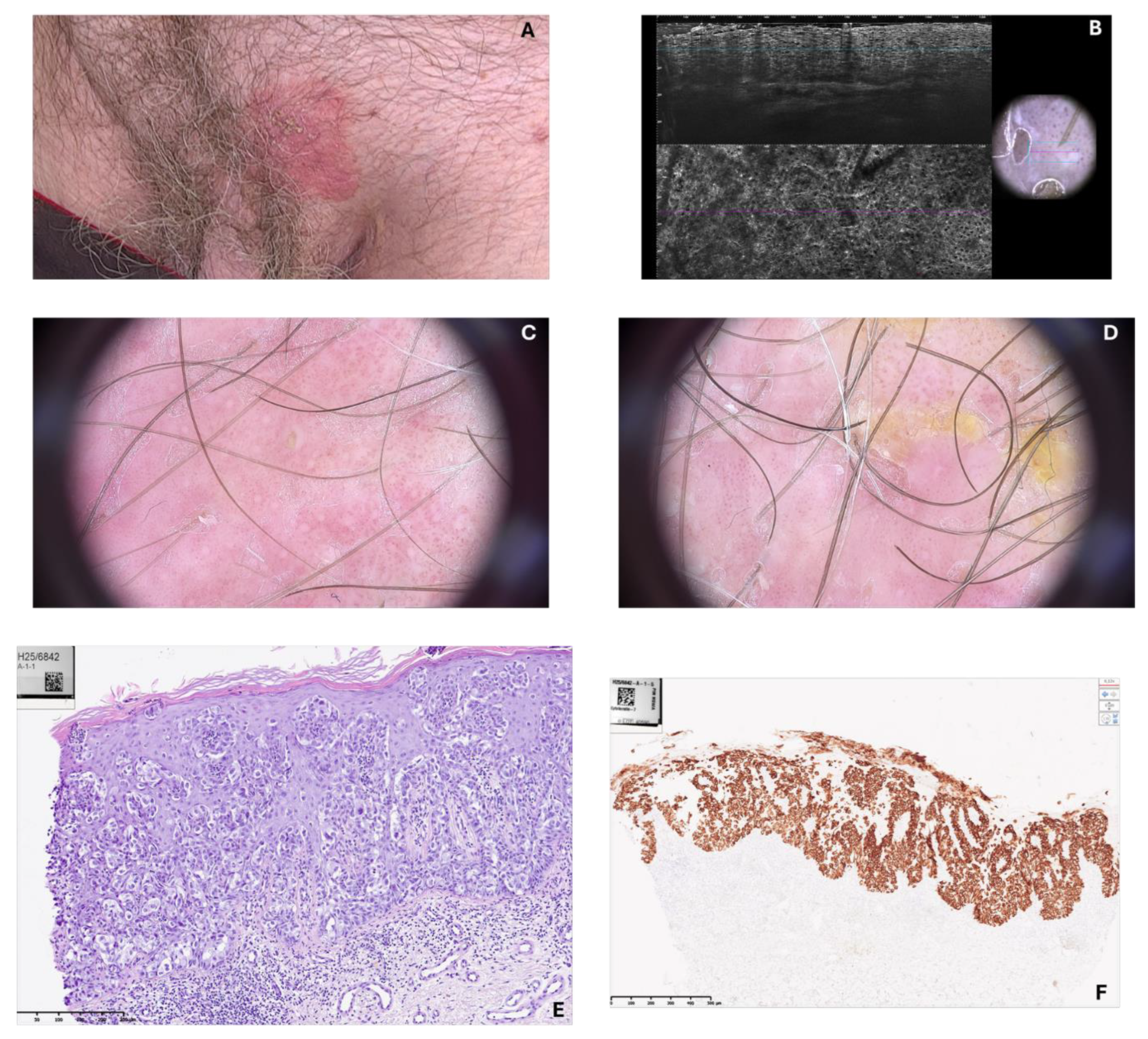
An 80-year-old male with a history of chronic comorbidities presented with a persistent erythematous and pruritic lesion located in the suprapubic region. The lesion had been present for several months and had gradually enlarged despite treatment with topical corticosteroids and antifungal agents administered under the initial presumption of dermatitis. On clinical examination, a well-demarcated erythematous plaque with superficial erosion and scaling, measuring approximately 7 × 6 cm, was observed on the suprapubic skin above the pubic symphysis. No inguinal lymphadenopathy was detected.
Videodermoscopy revealed a sharply circumscribed erythematous area with irregular whitish scaling and superficial erosion, suggestive of an intraepidermal neoplastic process. Line-Field Confocal Optical Coherence Tomography (LC-OCT) further demonstrated the presence of large, atypical cells with abundant pale cytoplasm distributed within the epidermis, corresponding to Paget cells, and confirmed the dermoscopic suspicion. A punch biopsy was subsequently performed, and histopathological analysis was conducted. The hematoxylin and eosin stained section demonstrates marked histopathological changes within the epidermis. There was a prominent infiltration of epidermis by large, atypical cells, occurring both singly and in cohesive nests. The cells were distinguished by abundant, pale cytoplasm and large, pleomorphic nuclei. Some nuclei appeared vesicular with prominent nucleoli. The cells were scattered throughout all layers of epidermis in a “pagetoid” distribution. The underlying dermis exbibited superficial, perivascular inflammatory infiltrate. No invasion of dermal stroma was evident. Immunohistochemical staining for Cytokeratin 7 demonstrated strong and diffuse cytoplasmic positivity within the large, atypical intraepidermal cells.
In sharp contrast, the adjacent non-neoplastic keratynocytes of the epidermis were negative. The staining pattern effectively highlighted the full extent of the neoplastic infiltration and confirms the Paget cells – a finding characteristic for this disease. Representative videodermoscopy, LC-OCT, and histopathology images are provided (
Figure 1).
The patient subsequently underwent wide local excision with appropriate clinical margins hisopathologically free of lesions. The postoperative course was uneventful. Patient continues to be monitored under regular dermatological surveillance (videodermoscopy) for over 1 year now with no sings of recurrence.
3. Discussion
Extramammary Paget’s disease (EMPD) is a rare neoplasm that usually affects apocrine gland–bearing areas such as the vulva, scrotum, penis, and perianal region [
10]. Suprapubic localization, as in our case, is exceedingly uncommon and only sporadically described in the literature. The atypical clinical location, combined with the nonspecific erythematous and eczematous appearance, often results in delayed diagnosis and inappropriate initial treatment, as occurred in this patient, who was first managed with topical corticosteroids and antifungal agents.
Videodermoscopy and LC-OCT proved being valuable in this case, supporting the suspicion of intraepidermal neoplasia and guiding the decision to perform a diagnostic biopsy. Although histopathology remains the gold standard, the integration of non-invasive imaging modalities such as dermoscopy and LC-OCT may facilitate earlier recognition of EMPD and reduce diagnostic delays.
Histopathological and immunohistochemical evaluation are essential not only to confirm the diagnosis but also to differentiate primary EMPD from secondary involvement by underlying visceral malignancies. In our patient, the immunoprofile (CK7+, CKPan+, PAS+, GATA3+, CK20-, CDX2-, Sox10-, HMB-45-, and PRAME-) excluded colorectal carcinoma, supporting the diagnosis of primary EMPD.
Wide local excision remains the standard of care for EMPD, but high recurrence rates have been reported due to subclinical extension of tumor cells beyond clinically visible margins. Mohs micrographic surgery has been advocated as an alternative for reducing recurrence [
9], though its availability is limited. Intraoperative frozen section analysis may serve as a practical compromise to ensure margin clearance. The reconstruction with a local advancement flap provided a satisfactory cosmetic and functional outcome, with no recurrence observed during follow-up.
This case emphasizes the importance of considering EMPD in the differential diagnosis of persistent, treatment-resistant lesions in atypical sites such as the suprapubic region. Early biopsy, aided by non-invasive imaging techniques, and careful immunohistochemical characterization are critical for accurate diagnosis and appropriate treatment planning.
4. Conclusions
We report a rare case of primary extramammary Paget’s disease localized to the suprapubic region in a male patient. This case highlights the diagnostic challenges posed by EMPD, particularly in unusual anatomical locations where it may mimic benign dermatoses. Non-invasive imaging modalities such as dermoscopy and LC-OCT can facilitate timely recognition and guide biopsy. Wide local excision remains an effective treatment, though long-term follow-up is mandatory due to the risk of recurrence. Clinicians should maintain a high index of suspicion for EMPD in chronic, unresponsive lesions of the suprapubic area, and a multidisciplinary approach is essential to optimize patient outcomes.
Author Contributions
Writing, M.K. and P.S.; review and editing, M.K. and P.S.; histopathology, Mał. Koł.; visualization, M.K. and P.S.; supervision, I.W. All authors contributed significantly to the work and approved the final version.
Funding
This research received no external funding.
Institutional Review Board Statement
Ethical review and approval were waived for this study due to its nature as a single-patient case report describing standard-of-care treatment, which does not require prior Ethics Committee/IRB approval under local regulations and institutional policy.
Informed Consent Statement
Written informed consent has been obtained from the patient to publish this paper.
Data Availability Statement
Data are available on request from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| EMPD |
Extramammary Paget’s disease |
| LC-OCT |
Line-Field Confocal Optical Coherence Tomography |
| CK7 |
Cytokeratin 7 |
References
- Lopes Filho, L.L., et al., Mammary and extramammary Paget’s disease. Anais brasileiros de dermatologia, 2015. 90(2): p. 225-231.
- Crocker, H.R., Paget’s disease affecting the scrotum and penis. Trans. Pathol. Soc. Lond., 1889. 40: p. 187-191.
- St Claire, K., et al., Extramammary paget disease. Dermatology online journal, 2019. 25(4).
- Hashimoto, H. and T. Ito, Current Management and Treatment of Extramammary Paget’s Disease. Current Treatment Options in Oncology, 2022. 23(6): p. 818-830. [CrossRef]
- Shah, R.R., et al., Extramammary Paget disease. Part I. epidemiology, pathogenesis, clinical features, and diagnosis. Journal of the American Academy of Dermatology, 2024. 91(3): p. 409-418. [CrossRef]
- Bayan, C.A., et al., A review of non-invasive imaging in extramammary Paget’s disease. Journal of the European Academy of Dermatology and Venereology, 2018. 32(11): p. 1862-1873. [CrossRef]
- Perrotto, J., et al., The role of immunohistochemistry in discriminating primary from secondary extramammary Paget disease. The American journal of dermatopathology, 2010. 32(2): p. 137-143. [CrossRef]
- Ishizuki, S. and Y. Nakamura, Extramammary Paget’s disease: diagnosis, pathogenesis, and treatment with focus on recent developments. Current Oncology, 2021. 28(4): p. 2969-2986. [CrossRef]
- Wollina, U., et al., Surgical treatment for extramammary Paget’s disease. Current treatment options in oncology, 2018. 19(6): p. 27. [CrossRef]
- Kyriazanos, I.D., et al., Extra-mammary Paget’s disease of the perianal region: a review of the literature emphasizing the operative management technique. Surgical oncology, 2011. 20(2): p. e61-e71. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).