Submitted:
27 November 2025
Posted:
28 November 2025
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
2.1. Theoretical Perspective
2.2. Study Design
2.3. Setting, Participants, and Recruitment
2.4. Data Collection
2.5. Data Analysis
2.6. Trustworthiness
2.7. Ethical Considerations
3. Results
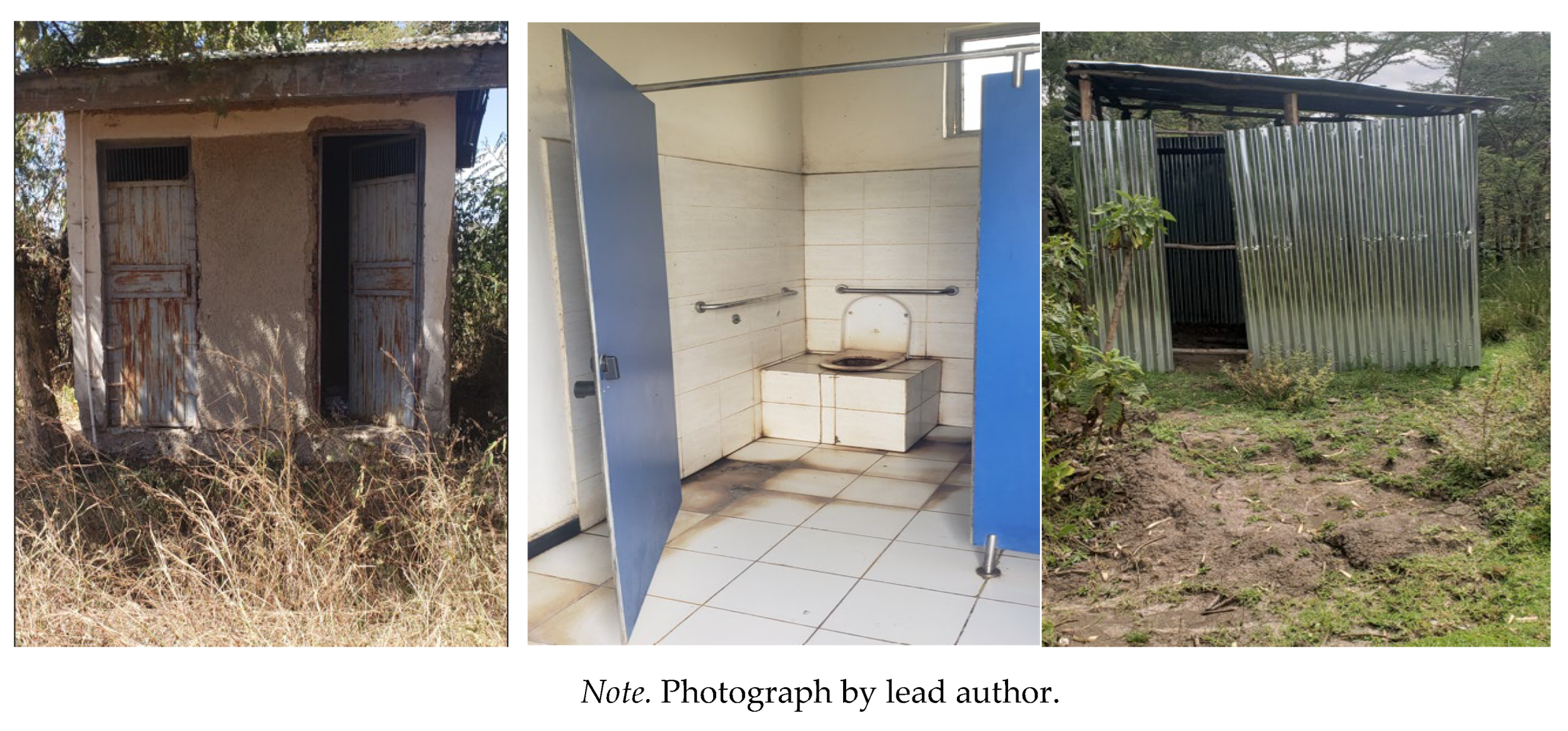
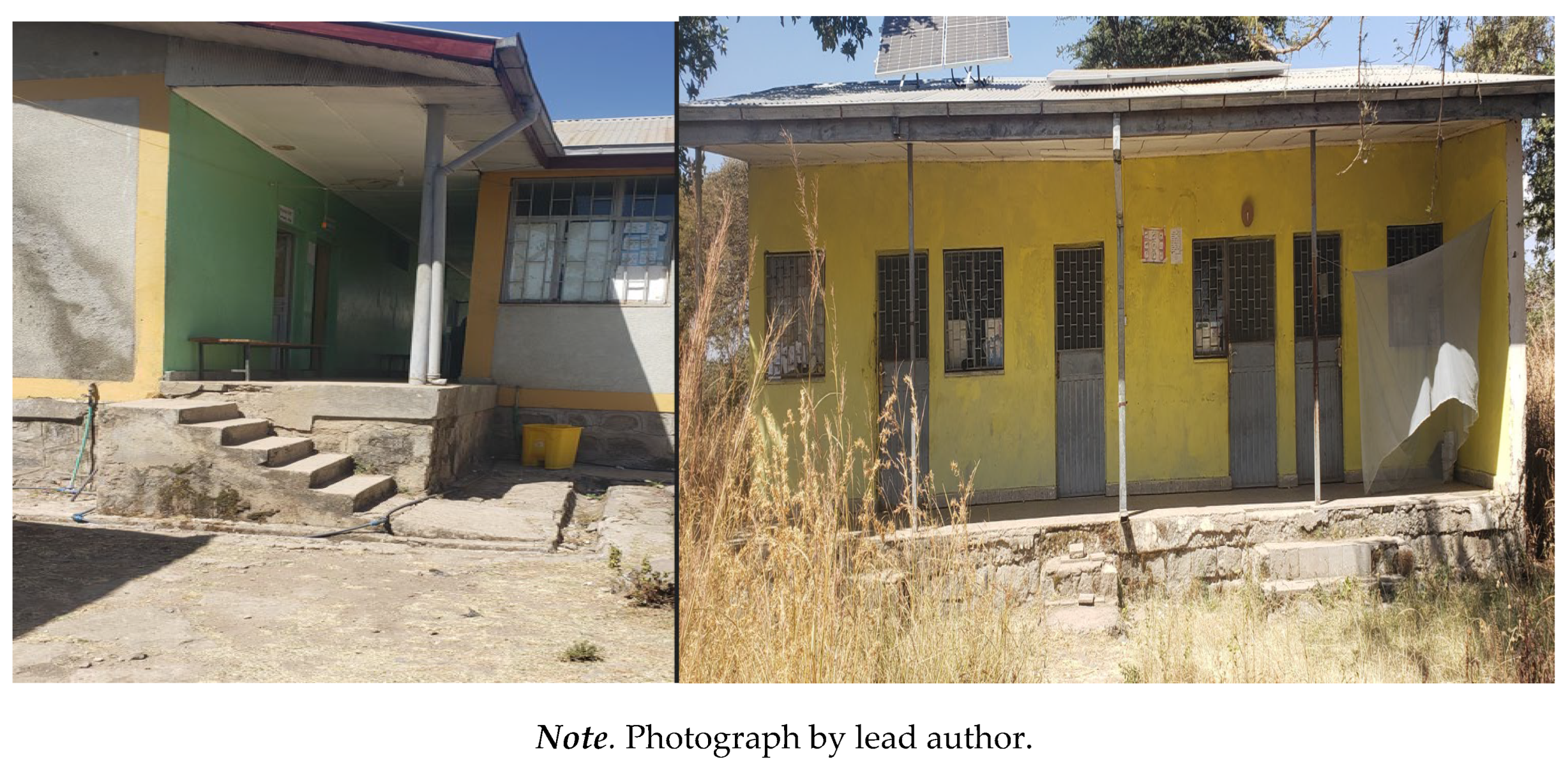
3.1. Physical and Environmental Barriers: “Every Negative Aspect is Stacked Against Us”: Challenges in Travelling to and Within Health Centers
3.2. Socioeconomic Marginalization: Financial Hardship and Poverty
3.3. Socio-Cultural Stigma and Attitudinal Barriers
3.3.1. Community Prejudice and Health Care Providers' Negative Attitude
3.3.2. Gendered Health Care Neglect and Domestic Burdens
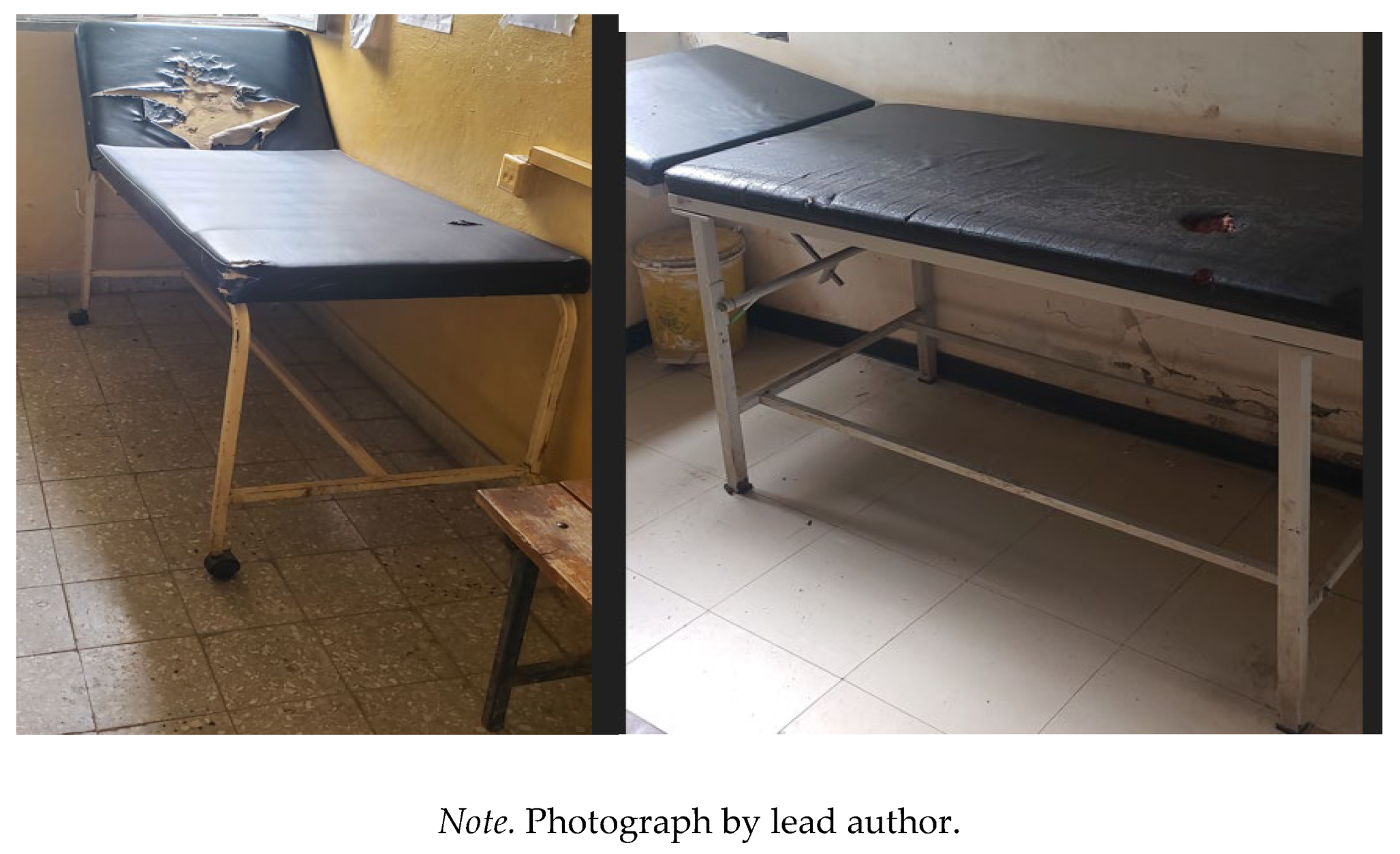
3.3.3. Systemic Weaknesses in Health Service Delivery: Gaps in Resources, Coordination, and Implementation
4. Discussion
4.1. Recommendations
4.2. Strengths and Limitations of the Study
4.3. Future Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Disability Language/Terminology Positionality Statement
References
- World Health Organization. Global report on health equity for persons with disabilities. Geneva, Swizerland: World Health Organization; 2022. Contract No.: Licence: CC BY-NC-SA 3.0 IGO.
- United Nations Ethiopia. International Day of Persons with Disabilities marked with a call to accelerate efforts to ensure disability inclusion: UN Ethiopia; 2024 [Available from: https://ethiopia.un.org/en/286846-international-day-persons-disabilities-marked-call-accelerate-efforts-ensure-disability.
- United Nations Population Fund (UNFPA). Ethiopia: Population data portal: United Nations Population Fund; 2025 [Available from: https://www.unfpa.org/data/world-population/ET.
- Krahn GL, Walker DK, Correa-De-Araujo R. Persons With Disabilities as an Unrecognized Health Disparity Population. American Journal of Public Health. 2015;105(S2):S198-S206.
- Vergunst R, Swartz L, Mji G, MacLachlan M, Mannan H. ‘You must carry your wheelchair’ – barriers to accessing healthcare in a South African rural area. Global Health Action. 2015;8(1):29003.
- Mahmoudi E, Meade MA. Disparities in access to health care among adults with physical disabilities: analysis of a representative national sample for a ten-year period. Disabil Health J. 2015;8(2):182-90.
- Krahn GL, Walker DK, Correa-De-Araujo R. Persons with disabilities as an unrecognized health disparity population. Am J Public Health. 2015;105 Suppl 2(Suppl 2):S198-206.
- Gréaux M, Moro MF, Kamenov K, Russell AM, Barrett D, Cieza A. Health equity for persons with disabilities: a global scoping review on barriers and interventions in healthcare services. Int J Equity Health. 2023;22(1):236.
- United Nations. Convention on the Rights of Persons with Disabilities and Optional Protocol. In: (Ed.) UN, editor. New York: : United Nations; 2006. p. 18.
- United Nations. Transforming our world: the 2030 Agenda for Sustainable Development New York2015 [.
- Ratification of the Convention on the Rights of Persons with Disabilities Proclamation No. 676/2010, (2010).
- Federal Democratic Republic of Ethiopia. Ethiopian Building Proclamation No. 624/2009. . 2009.
- Ethiopian Health Insurance Agency. Community-Based Health Insurance Evaluation Report. Addis Ababa, Ethiopia: Ethiopian Health Insurance Agency; 2022.
- United Nations Department of Economic and Social Affairs. UN Disability and Development Report - Realizing the SDG by, for and with persons with disabilities. New York: UN; 2019.
- Damtew B, Yigezu M. Perspectives of care providers on obstacles to healthcare access for people with disabilities in Ethiopia: a qualitative investigation. BMC Health Serv Res. 2024;24(1):1290.
- Tesfaye T, Woldesemayat EM, Chea N, Wachamo D. Accessing Healthcare Services for People with Physical Disabilities in Hawassa City Administration, Ethiopia: A Cross-Sectional Study. Risk Manag Healthc Policy. 2021;14:3993-4002.
- Fekadu H, Mekonnen W, Adugna A, Kloos H, Hailemariam D. Barriers to equitable healthcare services for under-five children in Ethiopia: a qualitative exploratory study. BMC Health Services Research. 2024;24(1):613.
- Gebrekirstos LG, Lencha TT, Asgedom YS, Wube TB. Prevalence and factors associated with violence; perceived social support and health access among people with disabilities in rural districts of southern Ethiopia: mixed study. Journal of Multidisciplinary Healthcare. 2023:2921-36.
- Dagnachew N, Meshesha SG, Mekonen ZT. A qualitative exploration of barriers in accessing community pharmacy services for persons with disability in Addis Ababa, Ethiopia: a cross sectional phenomenological study. BMC health services research. 2021;21(1):467.
- Kemal S. Assessment of Barriers of Accessing Primary Health Care Services For Persons with Hearing, Visual and Physical Impairments in Gulele Sub City of Addis Ababa, AAU. Accessed on. 2017;12.
- Pothier D, Devlin R. Critical Disability Theory: Essays in Philosophy, Politics, Policy, and Law. Vancouver: UBC Press; 2006.
- Hosking DL. Critical disability theory. 4th Biennial Disability Studies Conference; 2008; Lancaster University, UK: (Leave blank unless formally published); 2008.
- Crenshaw K. Demarginalizing the intersection of race and sex: A Black feminist critique of antidiscrimination doctrine, feminist theory and antiracist politics. University of Chicago Legal Forum. 1989;1989(1):139–67.
- Hill Collins P. Intersectionality as critical social theory. Durham: Duke University Press; 2019.
- McCall L. Complex Inequality: Gender, Class and Race in the New Economy: Taylor & Francis; 2002.
- Collins PH, Bilge S. Intersectionality: John Wiley & Sons; 2020.
- Stake RE. Qualitative case studies. 2005.
- Central Statistical Agency (CSA) [Ethiopia] and ICF. Ethiopia Demographic and Health Survey. Addis Ababa, Ethiopia, and Rockville, Maryland, USA; 2017.
- Colorafi KJ, Evans B. Qualitative Descriptive Methods in Health Science Research. Herd. 2016;9(4):16-25.
- Neergaard MA, Olesen F, Andersen RS, Sondergaard J. Qualitative description – the poor cousin of health research? BMC Medical Research Methodology. 2009;9(1):52.
- Gill P, Stewart K, Treasure E, Chadwick B. Methods of data collection in qualitative research: interviews and focus groups. British Dental Journal. 2008;204(6):291-5.
- Kitzinger J. Qualitative Research: Introducing focus groups. BMJ. 1995;311(7000):299.
- Braun V, Clarke V, Hayfield N, Davey L, Jenkinson E. Doing reflexive thematic analysis. Supporting research in counselling and psychotherapy: Qualitative, quantitative, and mixed methods research: Springer; 2023. p. 19-38.
- Tracy SJ. Qualitative quality: Eight “big-tent” criteria for excellent qualitative research. Qualitative inquiry. 2010;16(10):837-51.
- Jacobson D, Mustafa N. Social identity map: A reflexivity tool for practicing explicit positionality in critical qualitative research. International journal of qualitative methods. 2019;18:1609406919870075.
- Lundberg DJ, Chen JA. Structural ableism in public health and healthcare: a definition and conceptual framework. The Lancet Regional Health - Americas. 2024;30:100650.
- Eide AH, Muderedzi JT, Braathen SH, Stray-Pedersen B. Exploring structural violence in the context of disability and poverty in Zimbabwe. African Journal of Disability. 2017;6(1):1-9.
- Pinilla-Roncancio M, Cedeño-Ocampo G. Multidimensional poverty among persons with disabilities in Colombia: Inequalities in the distribution of deprivations at the municipality level. PLoS One. 2023;18(6):e0286983.
- Groce N, Kett M. Youth with disabilities. Youth with Disabilities (2014) Working Paper. 2014;23.
- Alshami A, Nashwan A. Healthcare Access for People with Disabilities in LMICs. Healthcare Access for People with Disabilities in LMICs. Singapore: Springer Nature Singapore; 2025. p. 13-21.
- Hashemi G, Wickenden M, Bright T, Kuper H. Barriers to accessing primary healthcare services for people with disabilities in low and middle-income countries, a Meta-synthesis of qualitative studies. Disabil Rehabil. 2022;44(8):1207-20.
- Dassah E, Aldersey HM, McColl MA, Davison C. Health care providers’ and persons with disabilities’ recommendations for improving access to primary health care services in rural northern Ghana: A qualitative study. PLOS ONE. 2022;17(9):e0274163.
- Halvorsen T, Munthali A, Braathen SH, Rød JK, Eide AH. Using locational data in a novel mixed-methods sequence design: Identifying critical health care barriers for people with disabilities in Malawi. Social Science & Medicine. 2021;283:114127.
- Pucchio AMR, Stranges S, Ali S. Disability and unmet need for health care in Canada: Findings from the Canadian Community Health Survey. Disability and Health Journal. 2025:101846.
- Ganle JK, Otupiri E, Obeng B, Edusie AK, Ankomah A, Adanu R. Challenges Women with Disability Face in Accessing and Using Maternal Healthcare Services in Ghana: A Qualitative Study. PLOS ONE. 2016;11(6):e0158361.
- Ssemata AS, Smythe T, Sande S, Menya A, Hameed S, Waiswa P, et al. Exploring the barriers to healthcare access among persons with disabilities: a qualitative study in rural Luuka district, Uganda. BMJ Open. 2024;14(11):e086194.
- Oliver M. The Politics of Disablement: Red Globe Press London; 1990.
- Rotoli J, Poffenberger C, Backster A, Sapp R, Modi P, Stehman CR, et al. From inequity to access: Evidence-based institutional practices to enhance care for individuals with disabilities. AEM Educ Train. 2023;7(Suppl 1):S5-s14.
- Hall MC. Critical Disability Theory. The Stanford Encyclopedia of Philosophy [Internet]. 2019.
- Titchkosky T. The Question of Access: Disability, Space, Meaning: University of Toronto Press; 2011.
- Mitra S, Posarac A, Vick B. Disability and Poverty in Developing Countries: A Multidimensional Study. World Development. 2013;41:1-18.
- Trani J-F, Loeb M. Poverty and disability: A vicious circle? Evidence from Afghanistan and Zambia. Journal of International Development. 2012;24(S1):S19-S52.
- Banks LM, Kuper H, Polack S. Poverty and disability in low- and middle-income countries: A systematic review. PLOS ONE. 2017;12(12):e0189996.
- International Labour Organization. Ethiopia Country Profile: Employment of People with Disabilities – The Impact of Legislation2004. Geneva: International Labour Organization; 2004.
- Soltani S, Takian A, Akbari Sari A, Majdzadeh R, Kamali M. Financial Barriers to Access to Health Services for Adult People with Disability in Iran: The Challenges for Universal Health Coverage. Iran J Public Health. 2019;48(3):508-15.
- Rahman M, Rana MS, Rahman MM, Khan MN. Healthcare services access challenges and determinants among persons with disabilities in Bangladesh. Scientific Reports. 2024;14(1):19187.
- Park S, Stimpson JP. Health Care Expenses and Financial Hardship Among Medicare Beneficiaries With Functional Disability. JAMA Netw Open. 2024;7(6):e2417300.
- Nguyen L, Lee JT, Hulse ESG, Hoang MV, Kim GB, Le DB. Health Service Utilization and Out-of-Pocket Expenditure Associated with the Continuum of Disability in Vietnam. International Journal of Environmental Research and Public Health. 2021;18(11):5657.
- Ssemata AS, Smythe T, Sande S, Menya A, Hameed S, Waiswa P, et al. Engaging community groups to enhance healthcare access for persons with disabilities in rural Uganda: A qualitative exploration. PLOS Glob Public Health. 2025;5(3):e0003140.
- World Health Organization & World Bank. World Report on Disability. 2011.
- Jin S, Sun Y, Tao J, Tian L, Lin J, Qian D. Medical expenditure and its inequity for people with disabilities: Evidence from the CHARLS 2018 data. Front Public Health. 2022;10:977150.
- Federal Ministry of Health. Health Care Financing Strategy 2022-2031. 2022.
- Alshami A, Nashwan A. Healthcare Access for People with Disabilities in LMICs. 2025. p. 13-21.
- Ministry of Labour and Social Affairs. National Plan of Action of Persons with Disabilities (2012-2021). . Addis Ababa: Government of Ethiopia; 2012.
- Koch R, Nkurunziza T, Rudolfson N, Nkurunziza J, Bakorimana L, Irasubiza H, et al. Does community-based health insurance protect women from financial catastrophe after cesarean section? A prospective study from a rural hospital in Rwanda. BMC Health Services Research. 2022;22(1):717.
- Atakorah YB, Arthur E, Osei-Fosu AK, Novignon J. The impact of Ghana’s national health insurance exemption policies on healthcare-seeking behaviour. SSM - Health Systems. 2024;3:100035.
- Tangcharoensathien V, Tisayaticom K, Suphanchaimat R, Vongmongkol V, Viriyathorn S, Limwattananon S. Financial risk protection of Thailand’s universal health coverage: results from series of national household surveys between 1996 and 2015. International Journal for Equity in Health. 2020;19(1):163.
- Iezzoni LI, Long-Bellil LM. Training physicians about caring for persons with disabilities: "Nothing about us without us!". Disabil Health J. 2012;5(3):136-9.
- Sapp RW, Sebok-Syer SS, Gisondi MA, Rotoli JM, Backster A, McClure Poffenberger C. The Prevalence of Disability Health Training and Residents With Disabilities in Emergency Medicine Residency Programs. AEM Educ Train. 2021;5(2):e10511.
| Participants* | Gender | Age | Marital Status | Educational Status | Job (Means of Income) | Disability Type and Cause | Assistive Devices | |
|---|---|---|---|---|---|---|---|---|
| Shashie | F | 29 | Single | HSC | Hand Sewing | Congenital; Weak leg, Vision and hearing impairment | Walking Stick | |
| Kokit | F | 20 | Single | Grade 3 | Student | Congenital; Paralyzed legs | Wheelchair | |
| Kid | F | 31 | Single | College | Library assistant | Congenital; Weak and shortened hands | None | |
| Liya | F | 30 | Single | College | Selling local alcohol | Congenital; Weak and shortened hands | None | |
| Alex | M | 52 | Married | HSC | Barber | Acquired; Leg paralysis; childhood disease | Walking Stick | |
| Kal | M | 28 | Single | NFE | Shoeshine boy | Acquired; Unequal legs due to a fall in childhood age | Crutch | |
| Yibe | M | 66 | Married | NFE | Farmer | Congenital; Hand deformity | None | |
| Degu | M | 48 | Married | ESC | Farmer | Acquired; Disease (tuberculosis) Leg disability |
Walking Stick | |
| Maru | M | 37 | Widowed | NFE | Farmer | Acquired; Disease (leg amputation) | Crutch | |
| Mazi | F | 35 | Married | NFE | Selling goods | Congenital; leg deformity | Walking Stick | |
| Tasew | M | 42 | Married | ESC | Farmer | Acquired; Disease (unknown), leg deformity and weakness | Walking Stick | |
| Sis | F | 30 | Single | ESC | Hand Sewing | Congenital; Paralyzed legs | Wheelchair | |
| Baye | M | 29 | Married | HSC | Barber | Acquired; Leg shortening; unknown childhood disease | Crutch | |
| Nega | M | 45 | Married | ESC | Merchant | Acquired; Injury (amputation) | Crutch |
| Criteria | Strategies |
|---|---|
| Worthy Topic | Given the increasing prevalence of disabilities in Ethiopia and the limited research on their experiences with health care access, this study is timely and relevant. |
| Rich Rigour | Sufficient data were collected (14 individual interviews and a focus group with 7 participants); Synergy between design (case study) and methods (interview and focus group), CDT and intersectionality, and an iterative, six-phase reflexive thematic analysis was performed. |
| Sincerity | The first author engaged in self-reflective practices through journaling and by creating a ‘social identity map,’ a visual tool developed by Jacobson and Mustafa [35] to better understand his social position and the influence of power and privilege in relation to the participants and the study context. |
| Credibility | Participant stories were detailed verbatim, and a combination of individual interviews and one focus group were used to garner data to identify common findings. Two compatible theoretical lenses, intersectionality and CDT were applied. Moreover, during the focus group, the participants reviewed preliminary themes developed from the individual interviews and confirmed that interpretations resonated with their lived experiences. |
| Resonance | The study's findings can be applied to similar settings, such as sub-Saharan Africa. To enhance transferability, a detailed ‘thick description’ of the research context, participants, procedures and findings has been included, allowing readers to assess the potential applicability of insights to comparable environments. |
| Significant Contribution | In practice, the findings inform actionable policy recommendations, such as integrating disability indicators into Ethiopia’s community-based health insurance scheme. Also, the findings highlight an under-researched area within the Ethiopian context (practical significance) and provide a way to promote political and critical awareness (moral significance). |
| Ethics | Procedural ethics were followed (ethics approval obtained), and data were protected on a secure university server accessible only to the authors. |
| Meaningful Coherence | There is coherence between the research question, design, data collection, data analysis, and findings. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





