1. Introduction
Morphological variations in the human skeleton, particularly those observed in accessory bones (secondary ossicles), fusion defects, and other rare anatomical anomalies, are of notable interest in anthropological and clinical contexts [
1,
2,
3]. The study of foot bones enables anthropologists to identify unique skeletal characteristics, such as anatomical variants and fusion patterns. When these characteristics are correlated with clinical evidence, they can be used to ascertain individual identity [
4]. In clinical terms, such analyses can also provide insights into locomotor function, congenital or developmental anomalies, degenerative changes, and trauma patterns. Variations in foot morphology include bipartitions, bony fusions, sesamoid bones, and accessory ossicles [
2,
5,
6].
A comprehensive understanding of tarsal anomalies is of paramount importance for both clinicians and orthopedical researchers, as it offers invaluable insights into a multitude of aspects, including clinical assessments, diagnostic processes, and treatment planning [
1,
2,
7,
8,
9]. Anatomical variants in the tarsal region frequently manifest as deviations in the number, shape, size, or position of the bones [
10], being often identified fortuitously, which complicates the process of determining their etiology and morphological significance.
Accessory ossicles, also known as accessory or supernumerary bones, represent skeletal variations that are typically small in size. While often asymptomatic, they can occasionally be associated with pain or functional impairment [
2,
11]. These ossicles can occur as additional independent elements or as abnormal subdivisions of existing bones [
12,
13]. These subdivisions have their origin in either the incomplete fusion of the secondary ossification centers or the atypical division of the primary ossification centers [
1]. The presentation of accessory ossicles is heteroclite, manifesting as unilateral or bilateral formations. In certain cases, the ossicles can fuse with adjacent bones [
14].
Early research focused on foot anatomical variants relied heavily on cadaveric dissections, which provided critical insights into their anatomy and prevalence [
10,
15,
16,
17,
18,
19]. Although symptomatic ossicles are considered uncommon, recent literature indicates an increasing number of cases describing associated pain syndromes and degenerative changes [
2,
9,
11,
12,
14,
20,
21,
22,
23].
The reported prevalence of accessory ossicles of the foot varies considerably across studies, that likely stem from multiple biases, as highlighted by Silva and Curate [
3], and include differences in the type of sample or imaging technique, the non-detection of asymptomatic cases in clinical settings, and inconsistencies in prevalence estimation (per foot or per individual).
The aim of the present study is to record the frequency of six accessory foot ossicles (os trigonum, os calcaneum secundarium, navicular accessory bone, os sustentaculum, os vesalianum, and os intermetatarseum) in a Portuguese sample from the 21st Century Identified Skeletal Collection (CISC/XXI). In addition to frequency, patterns of co-occurrence, laterality, and potential differences by biological sex and age were also assessed.
2. Materials and Methods
Study Sample
The analysis was conducted on the 21st Century Identified Skeleton Collection (CISC/XXI), housed at the University of Coimbra (Forensic Anthropology Laboratory, Department of Life Sciences, Coimbra, Portugal). This collection consists of 302 adult skeletons (162 females; 140 males) from the
Cemitério dos Capuchos (Santarém), belonging to individuals exhumed between 1999 and 2016. All individuals died between 1982 and 2012 [
24,
25].
The study sample consisted of 162 adult individuals (82 females; 80 males), with ages at death ranging from 25 to 101 years old (average age at death = 75.0 years; SD=15.8).
Statistical Analysis
The frequencies of each accessory ossicle were calculated, and reported as prevalences in percentage (per individual and per foot). A chi-square test of independence (X2) was conducted under the null hypothesis that the proportion of individuals with an accessory ossicle is the same in both sexes. Laterality was also assessed with a chi-square test. A student’s t-test (independent samples) was employed to assess the null hypothesis that the average age at death is identical in individuals with and without accessory foot ossicles. Normality of the sample was evaluated with a Q-Q plot, and homoscedasticity with a Levene’s test. The critical p-value for rejecting the null hypothesis was set at p < 0.05. All statistical analyses were performed using Jamovi (v. 2.3.28).
3. Results
Of the 162 skeletons analyzed, 35 individuals (21.6%; 35/162), 13 females (15.9%; 13/82) and 22 males (27.5%; 22/80) exhibit at least one accessory ossicle. There is no statistically significant association between sex and the presence of accessory foot bones (X²: 2.082, df=1, p=0.149). A small difference was recorded in the mean ages at death of individuals with (mean = 71.5 years old; SD = 16.9) and without (mean = 76.1 years old; SD = 15.4) accessory ossicles, but the difference is not statistically significant (t-test: 1.55, df = 161, p = 0.123).
No co-occurrence of accessory foot bones was recorded. The prevalence of the observed ossicles of the foot per individual is summarized in
Table 1. Similarly, the prevalence of ossicles in each foot is shown in
Table 2 and
Table 3.
Os Trigonum
The most frequently observed accessory bone was
os trigonum, present in 15 individuals (9.3%, 15/162;
Table 2). The prevalence is 8.5% in females (7/82) and 10.0% in males (8/80), with no significant differences by sex (
X2: 0.745, df=1, p= 0.388). Six individuals (40%, 6/15), three females and three males, present with the ossicle bilaterally (
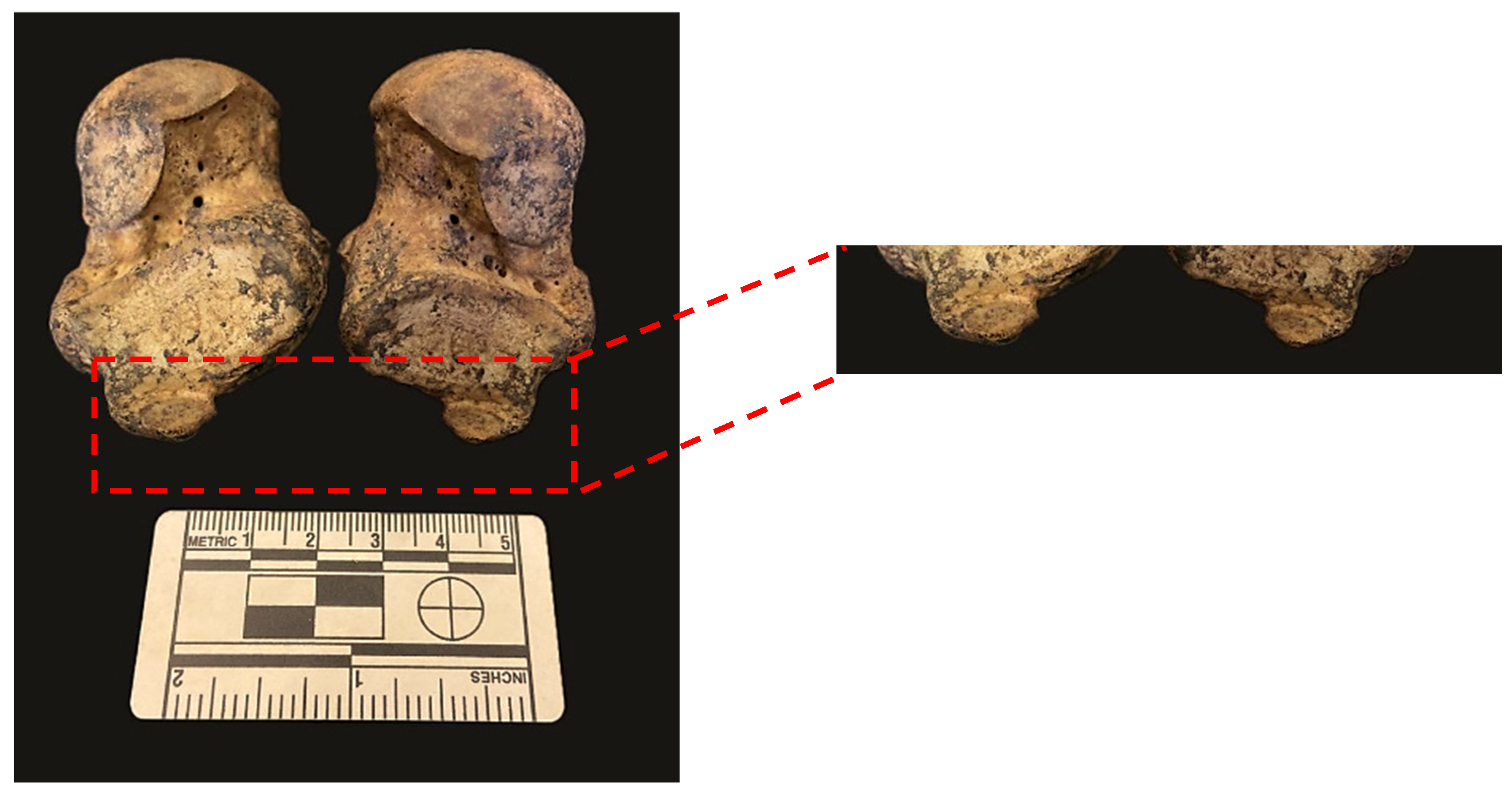
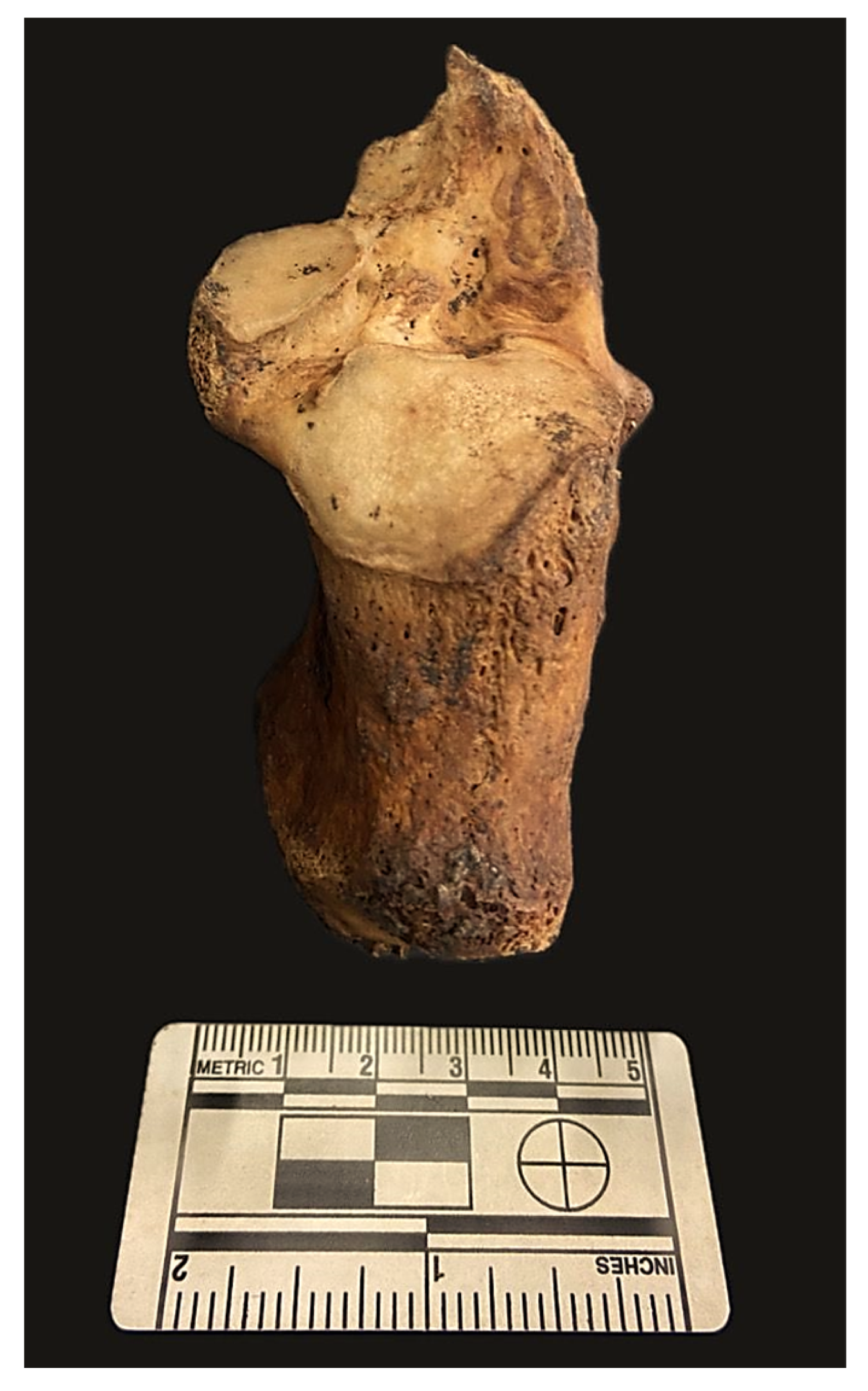
Figure 1).
Of the 15 individuals presenting with this ossicle, 14 (93.3%; 14/15) exhibit a fused
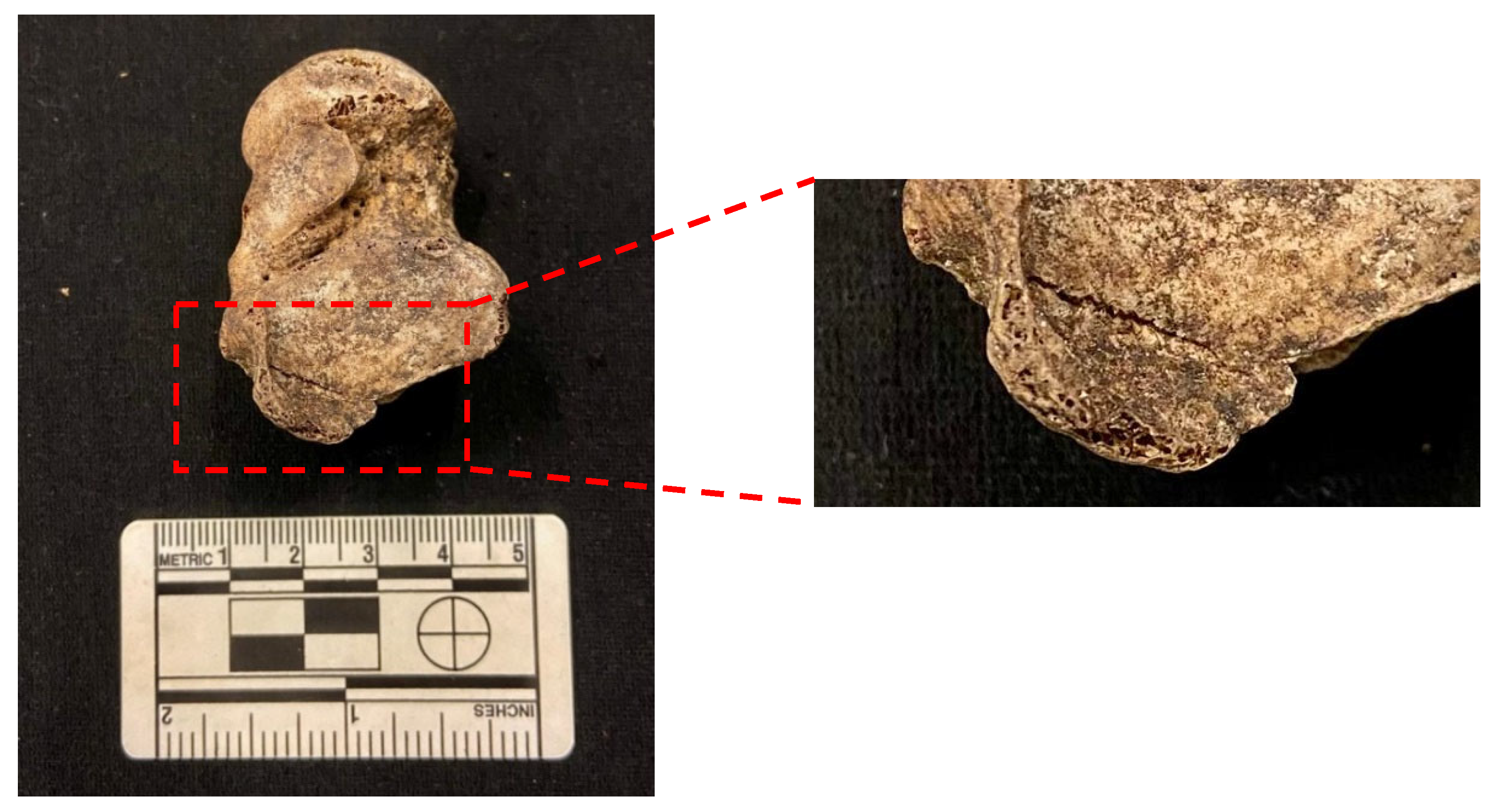
os trigonum. Two individuals (a male and a female) show bilateral fusion of this ossicle (
Figure 2). A unilateral fusion of this accessory bone was recorded in six males (three on the left foot and three on the right foot) and six females (four on the left foot and two on the right foot) (
Figure 3).
The prevalence of this ossicle is 7.1% (11/154) for the left foot (
Table 2), 6.3% in females (5/79) and 8.0% in males (6/75). Five of the affected women (100%, 5/5) and four men (66.7%, 4/6) present with a fused
os trigonum on the left foot. In the right foot, the prevalence is 6.5% (10/155), five females (6.4%, 5/78) and five males (6.5%, 5/77,
Table 3). Three females (60.0%; 3/5) and four males (80.0%; 4/5) show a fused
os trigonum in the right foot. This ossicle was observed bilaterally in 40% (6/15) of the individuals. Five (55.6%; 5/9) unilateral cases were found in the left foot and four (44.4%; 4/9) in the right foot. Only one free ossicle was detected, specifically in the right foot of a male subject (
Figure 4).
Calcaneum Secundarium
Calcaneum secundarium (CS) is the second most prevalent ossicle observed in this study, with a total prevalence per individual of 6.9% (11/159) (
Table 1). The ossicle is present in three females (3.8%; 3/80) and eight males (10.1%; 8/80), but the difference between sexes is not statistically significant (
X2: 2.51; df=1; p=0.113). Three individuals, one female and two males, exhibit the ossicle bilaterally (27.3%; 3/11;
Figure 5).
On the left foot, the prevalence is 3.2% (5/154,
Table 3), 1.3% in females (1/77) and 5.2% in males (4/77). The prevalence in the right foot is 5.8% (9/155, Table 4), 3.8% in females (3/78) and 7.8% in males (6/77). This accessory bone is expressed bilaterally in 27.3% of individuals. The majority of unilateral cases (75%; 6/8) were observed in the right foot, while only two left unilateral cases were recorded (25%; 2/8) (
Figure 6).
A statistically significant association was observed between laterality and the presence of calcaneum secundarium (X2: 39.2, df=1, p= < 0.001), with a higher prevalence in the right foot. The most common location of this ossicle is on the anterior facet of the calcaneus, specifically on the anteromedial aspect. Of the nine calcanei with CS, five exhibit separate facets, while the remaining four show a continuous facet.
Os Sustentaculum
This ossicle was not identified in any of the 163 individuals under study.
Os Vesalianum
This accessory bone was observed only in the right foot of one female (CISC/XXI/25), (0.6%, 1/159,
Table 1 and
Table 3).
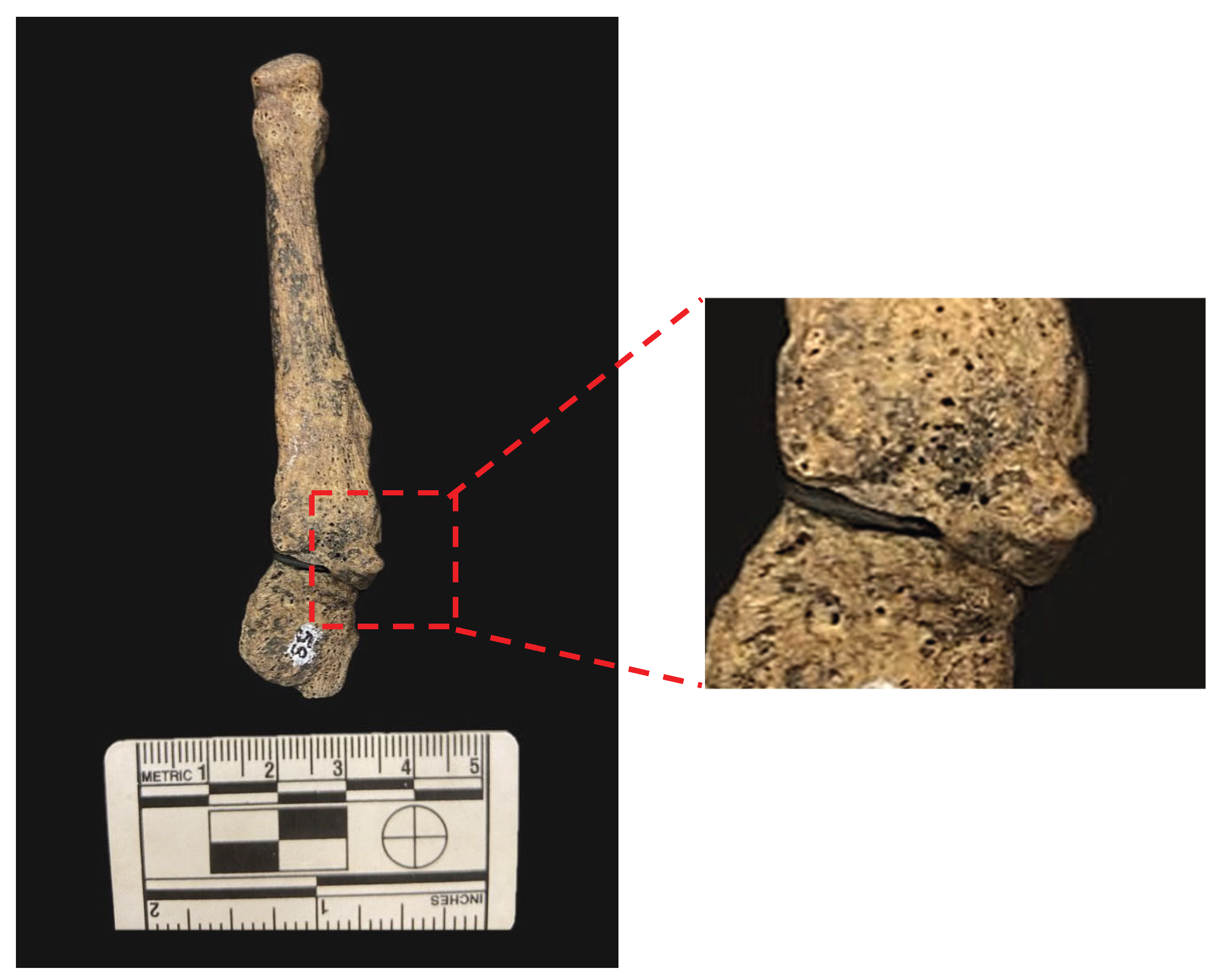
Accessory Navicular Bone
A Type II accessory navicular was identified in the right foot of one male (CISC/XXI/72) (0.6%, 1/160;
Table 1 and
Table 3;
Figure 7).
4. Discussion
This study reports a 21.4% prevalence (35/163) of accessory tarsal ossicles in a reference sample of Portuguese skeletal remains, a frequency broadly consistent with, though slightly higher than, that observed in a chronologically earlier Portuguese sample ([
3]: 18.3%; 89/486). Seemingly, there were no changes over a relatively short period of time in the frequency of accessory tarsal ossicles in the Portuguese population – a particular interesting feature when accounting for the changing political and socioeconomic circumstances of the country [
26]. The prevalence range reported in the broader literature spans from 18.0% to 40.2% [
12,
14,
27,
28,
29], reflecting significant morphological variability across populations and diverse methodological approaches.
Non-anatomical factors may account for the relatively low frequency observed in our study, particularly the application of different study methodologies and samples [
3], and the observation of distinct types of ossicles [
30], including those associated with the tibia and fibula. Variation in the preservation and completeness of foot bones within the CISC/XXI may have constrained the identification of smaller ossicles. In addition, taphonomic alterations and the lack of specialized recovery procedures during the exhumation of the individual that compose the reference skeletal collection [
25] could have further contributed to underrepresentation of these small and fragile bone variants.
The results corroborate previous findings that accessory ossicles are distributed similarly across sexes, with no statistically significant differences observed between males (27.5%) and females (15.7%)—a pattern consistently noted in other studies [
3,
12,
14,
28,
31]. The co-occurrence of accessory foot bones was not observed. In fact, co-occurrence is not frequent [
3,
16], varying from 1.6% to 10.6% [
3,
12,
14,
28,
31]. Usually, age is not considered as a demographic factor in the appearance or expression of foot ossicles and, as in this study, it is similar in both affected and non-affected individuals [
3].
These findings reinforce the importance of accounting for anatomical variations in both clinical and anthropological contexts. Accessory ossicles, particularly in the tarsus, may mimic pathological conditions on radiographic imaging or influence biomechanical interpretations in bioarcheological reconstructions.
Os Trigonum
Os trigonum is one of the most thoroughly documented in both anthropological and clinical literature [
1,
2,
3,
12,
14,
31]. Cerrato et al. [
32] noted that individuals engaged in activities involving repeated plantar flexion (including, e.g., dancers [
33]) are more likely to develop or retain this ossicle, suggesting a functional or biomechanical component in its manifestation. Studies based on medical imaging consistently report higher prevalence rates when compared to direct skeletal analyses . In the present sample, 15 (9.3 %) individuals presented with
os trigonum. Previous research studies report prevalence rates between 0.8% and 25.0%, varying by population and employed methodology [
2,
3,
10,
14,
16,
20,
27,
28,
29,
34,
35,
36].
The observed prevalence in the CISC/XXI skeletal sample supports the empirical hypothesis that medical imaging-based studies can overestimate the presence of the
os trigonum, possibly due to its cartilaginous or partially ossified form in living individuals, which may not always persist or be recovered in dry bone collections. As previously noted, comparisons across studies require particular caution, as data collection methods vary considerably [
3]. Most radiographic studies classify only unfused
os trigonum as present, whereas osteological studies involving dissection or dry bone analysis can include both unfused and fused forms. The interpretation of fused cases is not always straightforward – particularly in distinguishing an enlarged posterolateral process of the talus from a completely fused
os trigonum in the absence of a visible fusion line [
37]. To avoid misclassification in this study, only cases with a clearly identifiable fusion line or sulcus were recorded as positive findings.
Regarding laterality, both the present study and previous literature suggest that
os trigonum is predominantly unilateral, but without a noticeable propensity for the left or right foot. Bilaterality appears to be less common, with most studies estimating bilateral occurrence in only 5–10% of cases [
3,
12,
14,
16]. As with other accessory tarsal ossicles, no significant sex differences were observed in the present sample, a finding consistent with previous studies [
3,
12].
Calcaneum Secundarium
The prevalence of the
calcaneum secundarium varies widely in the literature, ranging from 0.1% to 11.8% [
3,
14,
35,
36,
38]. This variability can be attributed to differences in diagnostic methods, study populations, and inclusion criteria. In the present osteological sample, individual prevalence was 6.9 %. Silva [
36] reported a prevalence of 11.8 % in a prehistoric Portuguese sample, significantly higher than in other populations such as four non-industrial groups (4.4 %) and an early 20th-century U.S. sample (1.9 %) [
39]. Population homogeneity due to geographic isolation and/or marriage customs may account for the elevated rate in the prehistoric sample [
36].
The relative uncommonness of CS partly explains the lack of robust data regarding laterality and sex distribution. In this study, CS was observed in three females (3.8 %) and eight males (10.1 %), with no statistically significant sex difference. Only three individuals – one female and two males – presented bilateral CS (27.3 %, 3/11). A statistically significant association was found between CS presence and laterality, with a higher frequency on the right foot. However, earlier studies, such as Pfitzner’s [
10], described a tendency for bilateral occurrence, suggesting potential population-specific patterns.
The most common location for CS was the anterior facet of the calcaneus, specifically on the anteromedial aspect. Nine calcanei with CS had continuous facets, while five showed separate ones. Anderson [
17] associated CS with separated facets, whereas Mann [
39] found it more commonly associated with continuous facets. Future studies could clarify this relationship and offer further insights into the interaction between facet morphology and the presence of CS.
Os Sustentaculum
Os sustentaculum is generally asymptomatic and clinically insignificant but, in certain cases, it can become symptomatic [
2]. This accessory ossicle was not observed in the sample from the CISC/XXI, aligning with its rarity, as reported prevalences fluctuate between 0% and 1.0% [
1,
10,
28,
30,
40]. The first documented instance of this ossicle was by Pfitzner in 1896, who recorded a frequency of 0.5% in dissected feet [
10].
Os Vesalianum
Os vesalianum is a rare ossicle located at the proximal base of the fifth metatarsal within the
peroneus brevis tendon [
3,
41]. It was first identified by Andreas Vesalius in the
De Humani Corporis Fabrica [
3], and later studied by Pfitzner [
10] and Dwight [
15]. Its prevalence ranges from 0% to 5.9% [
3,
10,
14,
27,
28,
29,
42]. In this study, the ossicle was identified in a single female individual (1.3%) on the right foot.
This ossicle is typically round or oval and can articulate with the proximal end of the fifth metatarsal. In the present case, the ossicle showed well-defined cortical margins. Some studies suggest that it is slightly more common in males [
28,
42].
Accessory Navicular
The accessory navicular – also referred to as os
tibiale externum or
naviculare secundarium – is located medially to the navicular tuberosity [
1]. It is one of the most common accessory foot bone in clinical settings and is usually asymptomatic. When symptomatic, it often manifests during childhood or early adulthood as localized medial foot pain [
43]. Prevalence ranges from 1.2% to 28.3% in medical studies [
10,
14,
16,
27,
38,
44,
45,
46]. In anatomical and archaeological collections, however, lower prevalence rates are consistently observed, varying from 1.0% to 5.0% [
3,
47,
48]. In the present study, this ossicle was identified in only one male individual (0.6%), located on the right foot. The ossicle corresponded to a Type II accessory navicular – the most common of the three types and the most easily recognizable in human skeletal remains [
47].
Some studies convey a higher frequency in females [
43,
49,
50], while others report no significant differences between sexes [
3,
44,
47]. Similarly, reported patterns of lateralization differ across studies: while some authors describe a bilateral predominance [
10,
49,
51], others have found no consistent asymmetry [
44,
45].
5. Conclusions
The identification and documentation of accessory foot ossicles in reference skeletal collections are essential for advancing both anthropological and clinical knowledge of foot anatomy. The present study, based on the 21st Century Identified Skeletal Collection, provides updated data on the prevalence and distribution of these anatomical variants in a modern Portuguese sample. The results show a relatively low prevalence of these ossicles that is similar to a chronologically older sample from Portugal. Limitations of this study include potential underrepresentation due to preservation variability, taphonomic loss, and differences in recording methods. Despite these constraints, this research highlights the relevance of studying accessory foot ossicles in reference skeletal collections as sustained interdisciplinary investigations (integrating skeletal, clinical, and imaging approaches) can advance the scientific understanding of these anatomical variants and their effects on human variation and health.
Author Contributions
Conceptualization, F.C. and A.M.S.; methodology, L.S., F.C. and A.M.S.; validation, F.C. and A.M.S.; formal analysis, L.S.; data curation, L.S.; writing—original draft preparation, L.S., F.C. and A.M.S.; writing—review and editing, L.S., F.C. and A.M.S.; supervision, F.C. and A.M.S. All authors have read and agreed to the published version of the manuscript.
Funding
The co-authors Francisco Curate and Ana Maria Silva were financed by the R&D Unit Research Centre for Anthropology and Health, with the reference UIDB/00283/2020, funded by the Foundation for Science and Technology (FCT/MCTES) through national funds (PIDDAC) (https://doi.org/10.54499/UIDB/00283/2020).
Institutional Review Board Statement
Research clearance was granted by the curator and the Scientific Commission of the Laboratory of Forensic Anthropology (21st Century Identified Skeletal Collection).
Informed Consent Statement
Human skeletal remains prevail as a material embodiment of once-living people but informed consent is not an issue since the individuals included in the study are long deceased.
Data Availability Statement
Data generated during this study are available upon reasonable request.
Acknowledgments
We are indebted to the curator of the CISC/XXI, Professor Maria Teresa Ferreira.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Kelikian, A.; Sarrafian, S.K. Sarrafian’s Anatomy of the Foot and Ankle: Descriptive, Topographic, Functiona; Lippincott Williams & Wilkins: Philadelphia, 2011; Vol. 102. [Google Scholar]
- Mellado, J.M.; Ramos, A.; Salvadó, E.; Camins, A.; Danús, M.; Saurí, A. Accessory Ossicles and Sesamoid Bones of the Ankle and Foot: Imaging Findings, Clinical Significance and Differential Diagnosis. Eur. Radiol. 2003, 13. [Google Scholar] [CrossRef]
- Silva, A.M.; Curate, F. Accessory Foot Bones in a Portuguese Identified Skeletal Collection. Sci. Rep. 2024, 14. [Google Scholar] [CrossRef] [PubMed]
- Verna, E.; Piercecchi-Marti, M.D.; Chaumoitre, K.; Adalian, P. Relevance of Discrete Traits in Forensic Anthropology: From the First Cervical Vertebra to the Pelvic Girdle. Forensic Sci. Int. 2015, 253, 134.e1–134.e7. [Google Scholar] [CrossRef] [PubMed]
- Silva, A.M.; Silva, A.L. Unilateral Non-Osseous Calcaneonavicular Coalition: Report of a Portuguese Archeological Case. Anthropol. Sci. 2010, 118, 61–64. [Google Scholar] [CrossRef]
- Curate, F.; Silva, A.M. Developmental Anomalies of the Foot Bones: Coalitions and Bipartitions in the Coimbra Identified Skeletal Collection. Int. J. Osteoarchaeol. 2025, 35. [Google Scholar] [CrossRef]
- Rühli, F.J.; Solomon, L.B.; Henneberg, M. High Prevalence of Tarsal Coalitions and Tarsal Joint Variants in a Recent Cadaver Sample and Its Possible Significance. Clin. Anat. 2003, 16, 411–415. [Google Scholar] [CrossRef]
- Summers, A. Accessory Ossicles and Sesamoid Bones: Recognition and Treatment. Emerg. Nurse 2015, 22, 27–32. [Google Scholar] [CrossRef]
- Lawson, J.P. Symptomatic Radiographic Variants in Extremities. Radiology 1985, 157, 625–631. [Google Scholar] [CrossRef]
- Pfitzner, W. Beiträge Zur Kenntniss Des Menschlichen Extremitätenskelets. Morphol. Arb. 1896, 6. [Google Scholar]
- Krapf, D.; Krapf, S.; Wyss, C. Calcaneus Secundarius - A Relevant Differential Diagnosis in Ankle Pain: A Case Report and Review of the Literature. J. Med. Case Rep. 2015, 9. [Google Scholar] [CrossRef]
- Coskun, N.; Yuksel, M.; Cevener, M.; Arican, R.Y.; Ozdemir, H.; Bircan, O.; Sindel, T.; Ilgi, S.; Sindel, M. Incidence of Accessory Ossicles and Sesamoid Bones in the Feet: A Radiographic Study of the Turkish Subjects. Surg. Radiol. Anat. 2009, 31, 19–24. [Google Scholar] [CrossRef]
- Silva, A.M. Non-Osseous Calcaneonavicular Coalition in the Portuguese Prehistoric Population: Report of Two Cases. Int. J. Osteoarchaeol. 2005, 15, 449–453. [Google Scholar] [CrossRef]
- Candan, B.; Torun, E.; Dikici, R. The Prevalence of Accessory Ossicles, Sesamoid Bones, and Biphalangism of the Foot and Ankle: A Radiographic Study. Foot Ankle Orthop. 2022, 7. [Google Scholar] [CrossRef]
- Dwight, T. A Clinical Atlas, Variations of the Bones of the Hands and Feet; Lippincott Williams & Wilkins: Philadelphia, 1907. [Google Scholar]
- Heimerzheim, A. Über Einige Akzessorische Fußwurzelknochen Nebst Ihrer Chirurgischen Bedeutung. Dtsch. Zeitschrift für Chir. 1925, 190, 96–112. [Google Scholar] [CrossRef]
- Anderson, T. Calcaneus Secundarius: An Osteo-archaeological Note. Am. J. Phys. Anthropol. 1988, 77, 529–531. [Google Scholar] [CrossRef]
- Heikel, H.V.A. Coalitio Calcaneo-Navicularis and Calcaneus Secundarius: A Clinical and Radiographic Study of Twenty-Three Patients. Acta Orthop. 1962, 32, 72–84. [Google Scholar] [CrossRef]
- Henderson, R.S. Os Intermetatarseum and a Possible Relationship to Hallux Valgus. J. Bone Joint Surg. Br. 1963, 45 B, 117–121. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.H.; Kyung, M.G.; Cho, Y.J.; Go, T.W.; Lee, D.Y. Prevalence of Accessory Bones and Tarsal Coalitions Based on Radiographic Findings in a Healthy, Asymptomatic Population. CiOS Clin. Orthop. Surg. 2020, 12, 245–251. [Google Scholar] [CrossRef] [PubMed]
- Debnar, M.; Kopp, L.; Baba, V.; Rammelt, S. Accessory Bones at the Foot and Ankle: A Comprehensive Review. Fuss und Sprunggelenk 2023, 21, 121–137. [Google Scholar] [CrossRef]
- Vaz, A.; Trippia, C.R. Small but Troublesome: Accessory Ossicles with Clinical Significance. Radiol. Bras. 2018, 51, 248–256. [Google Scholar] [CrossRef] [PubMed]
- McAlister, J.E.; Urooj, U. Os Trigonum Syndrome. Clin. Podiatr. Med. Surg. 2021, 38, 279–290. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, M.T.; Coelho, C.; Makhoul, C.; Navega, D.; Gonçalves, D.; Cunha, E.; Curate, F. New Data about the 21st Century Identified Skeletal Collection (University of Coimbra, Portugal). Int. J. Legal Med. 2021, 135, 1087–1094. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, M.T.; Vicente, R.; Navega, D.; Gonçalves, D.; Curate, F.; Cunha, E. A New Forensic Collection Housed at the University of Coimbra, Portugal: The 21st Century Identified Skeletal Collection. Forensic Sci. Int. 2014, 245, 202.e1–202.e5. [Google Scholar] [CrossRef]
- Maranho, R.; Ferreira, M.T.; Curate, F. Secular Trends in the Size and Shape of the Scapula among the Portuguese between the 19th and the 21st Centuries. Biology (Basel). 2023, 12, 928. [Google Scholar] [CrossRef]
- Cilli, F.; Akçaoglu, M. The Incidence of Accessory Bones of the Foot and Their Clinical Significance. Acta Orthop. Traumatol. Turc. 2005, 39, 243–246. [Google Scholar]
- Kalbouneh, H.; Alajoulin, O.; Shawaqfeh, J.; Mustafa, A.; Jaber, S.; Zaben, S.; Zapen, J.; Alsalem, M. Accessory Ossicles in the Region of the Foot and Ankle: An Epidemiologic Survey in a Jordanian Population. Med. 2021, 57, 1–10. [Google Scholar] [CrossRef]
- Vasiljevic, V.; Markovic, L.; Vasic-Vilic, J.; Mihajlovic, D.; Nikolic, B.; Milosevic, S. Accessory Bones of the Feet: Radiological Analysis of Frequency. Vojnosanit. Pregl. 2010, 67, 469–472. [Google Scholar] [CrossRef]
- Keles-Celik, N.; Kose, O.; Sekerci, R.; Aytac, G.; Turan, A.; Güler, F. Accessory Ossicles of the Foot and Ankle: Disorders and a Review of the Literature. Cureus 2017, 9, e1881. [Google Scholar] [CrossRef]
- Kir, H.; Kandemir, S.; Olgaç, M.; Yıldırım, O.; Şen, G. The Incidence and Distribution of Accessory Ossicles of the Foot. Med. Bull. Sisli Etfal Hosp. 2011, 45, 44–47. [Google Scholar]
- Cerrato, R.; Myerson, M.S.; Jeng, C. The Symptomatic Os Trigonum: A Study of 27 Cases. Foot Ankle Int. 2006, 27, 42–47. [Google Scholar] [CrossRef]
- Marotta, J.J.; Micheli, L.J. Os Trigonum Impingement in Dancers. Am. J. Sports Med. 1992, 20, 533–536. [Google Scholar] [CrossRef]
- Stieda, L. Ueber Secundäre Fusswurzelknochen. Arch. für Anat. Physiol. und Wissenschaftliche Med. 1869, 108–111. [Google Scholar]
- Koo, B.S.; Song, Y.; Lee, S.; Sung, Y.K.; Sung, I.H.; Jun, J.B. Prevalence and Distribution of Sesamoid Bones and Accessory Ossicles of the Foot as Determined by Digital Tomosynthesis. Clin. Anat. 2017, 30, 1072–1076. [Google Scholar] [CrossRef] [PubMed]
- Silva, A.M. Foot Anomalies in the Late Neolithic/Chalcolithic Population Exhumed from the Rock Cut Cave of São Paulo 2 (Almada, Portugal). Int. J. Osteoarchaeol. 2011, 21, 420–427. [Google Scholar] [CrossRef]
- Zwiers, R.; Baltes, T.P.A.; Opdam, K.T.M.; Wiegerinck, J.I.; van Dijk, C.N. Prevalence of Os Trigonum on CT Imaging. Foot Ankle Int. 2018, 39, 338–342. [Google Scholar] [CrossRef] [PubMed]
- Tsuruta, T.; Shiokawa, Y.; Kato, A.; Matsumoto, T.; Yamazoe, Y.; Oike, T.; Sugiyama, T.; Saito, M. Radiological Study of the Accessory Skeletal Elements in the Foot and Ankle. J. Japanese Orthop. Assoc. 1981, 55, 357–370. [Google Scholar] [CrossRef]
- Mann, R.W. Calcaneus Secundarius: Description and Frequency in Six Skeletal Samples. Am. J. Phys. Anthropol. 1990, 81, 17–25. [Google Scholar] [CrossRef]
- Bencardino, J.; Rosenberg, Z.S.; Beltran, J.; Sheskier, S. Os Sustentaculi: Depiction on MR Images. Skeletal Radiol. 1997, 26, 505–506. [Google Scholar] [CrossRef] [PubMed]
- De Castro Correia, M.; Rodrigues Lopes, T. Knowing Your Accessory Foot Ossicles and Avoiding Misdiagnoses: A Case Report of Painful Os Vesalianum Pedis. Cureus 2022, 14, 11–13. [Google Scholar] [CrossRef]
- Pitchandi, M.; Mallikarjun, A.; Bhuvaneswari, V. Radiological Study on the Incidence and Clinical Importance of Os Vesalianum of 5th Metatarsal Bone. Int. J. Anatomy, Radiol. Surg. 2019, 8, 9–11. [Google Scholar]
- Ugolini, P.A.; Raikin, S.M. The Accessory Navicular. Foot Ankle Clin. 2004, 9, 165–180. [Google Scholar] [CrossRef]
- Keles Coskun, N.; Arican, R.Y.; Utuk, A.; Ozcanli, H.; Sindel, T. The Incidence of Accessory Navicular Bone Types in Turkish Subjects. Surg. Radiol. Anat. 2009, 31, 675–679. [Google Scholar] [CrossRef] [PubMed]
- Geist, E.S. Supernumerary Bones of the Foot — a Röntgen Study of the Feet of One Hundred Normal Individuals. J. Bone Jt. Surg. 1915, 2, 413–414. [Google Scholar]
- Bizarro, A.H. On Sesamoid and Supernumerary Bones of the Limbs. J. Anat. 1921, 55, 256–268. [Google Scholar]
- Offenbecker, A.M.; Case, D.T. Accessory Navicular: A Heritable Accessory Bone of the Human Foot. Int. J. Osteoarchaeol. 2012, 22, 158–167. [Google Scholar] [CrossRef]
- Burnett, S.E. Developmental Variation in South African Bantu: Variant Co-Occurrence and Skeletal Asymmetry, Arizona State University, 2005.
- Mygind, H.B. The Accessory Tarsal Scaphoid: Clinical Features and Treatment. Acta Orthop. 1953, 23, 142–151. [Google Scholar] [CrossRef] [PubMed]
- Mosel, L.D.; Kat, E.; Voyvodic, F. Imaging of the Symptomatic Type II Accessory Navicular Bone. Australas. Radiol. 2004, 48, 267–271. [Google Scholar] [CrossRef]
- Shands, A.R.; Wentz, I.J. Congenital Anomalies, Accessory Bones, and Osteochondritis in the Feet of 850 Children. Surg. Clin. North Am. 1953, 33, 1643–1666. [Google Scholar] [CrossRef]
- Gruber, W. Vorläufige Mittheilung Über Die Secundären Fusswurzelknochen Des Menschen. Arch. für Anat. Physiol. Wissenschaftliche Medizin 1864, 31, 286–290. [Google Scholar]
- Case, D.T.; Ossenberg, N.S.; Burnett, S.E. Os Intermetatarseum: A Heritable Accessory Bone of the Human Foot. Am. J. Phys. Anthropol. 1998, 107, 199–209. [Google Scholar] [CrossRef]
Figure 1.
Inferior view of the left and right talus, respectively, of a female individual (CISC/XXI29) with os trigonum. The left bone exhibits a fused ossicle, while the right presents a free ossicle.
Figure 1.
Inferior view of the left and right talus, respectively, of a female individual (CISC/XXI29) with os trigonum. The left bone exhibits a fused ossicle, while the right presents a free ossicle.
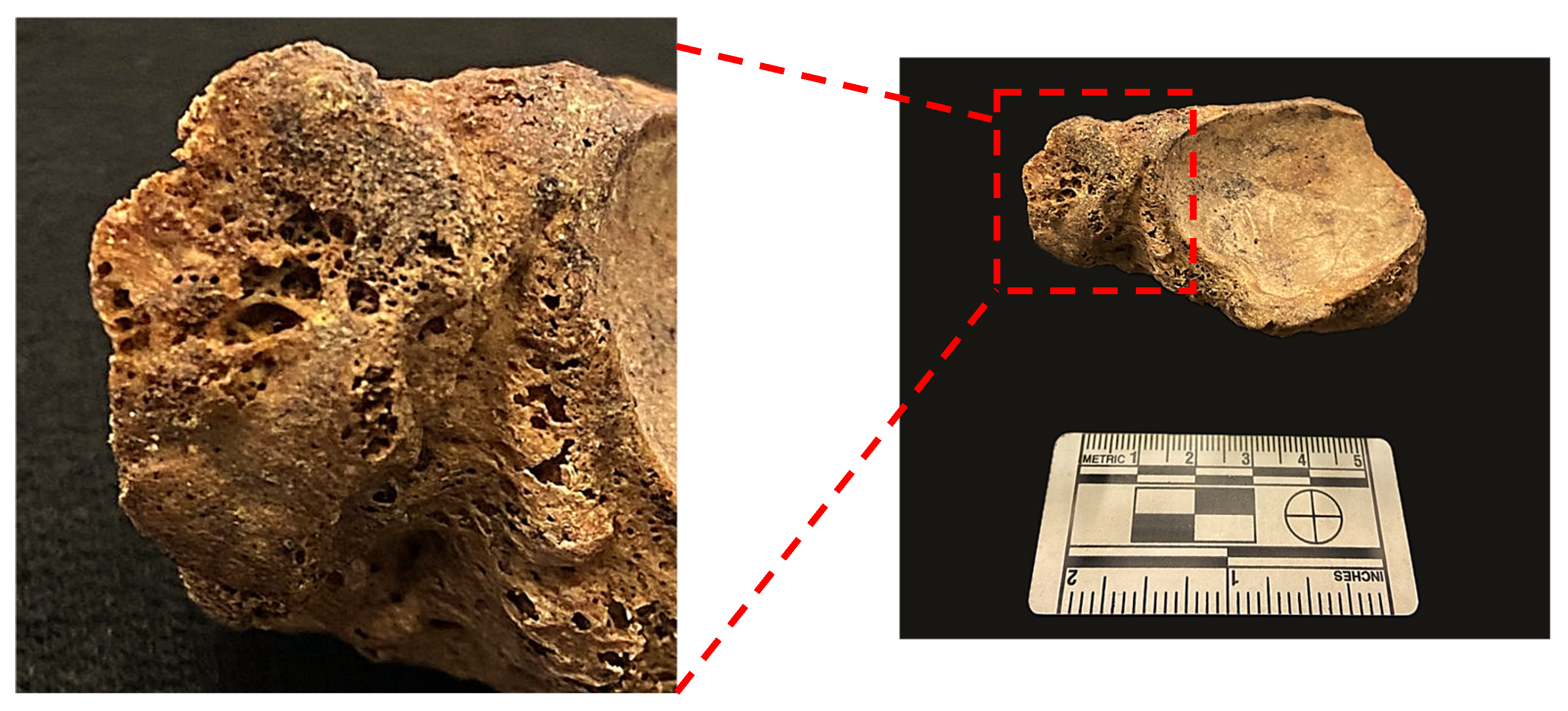
Figure 2.
Inferior view of the left and right talus of a female individual (CISC/XXI/299) illustrating bilateral, fused, os trigonum.
Figure 2.
Inferior view of the left and right talus of a female individual (CISC/XXI/299) illustrating bilateral, fused, os trigonum.
Figure 3.
Inferior view of the left talus of a female individual (CISC/XXI/59) with unilateral fusion of os trigonum. Note the fusion line in the close up.
Figure 3.
Inferior view of the left talus of a female individual (CISC/XXI/59) with unilateral fusion of os trigonum. Note the fusion line in the close up.
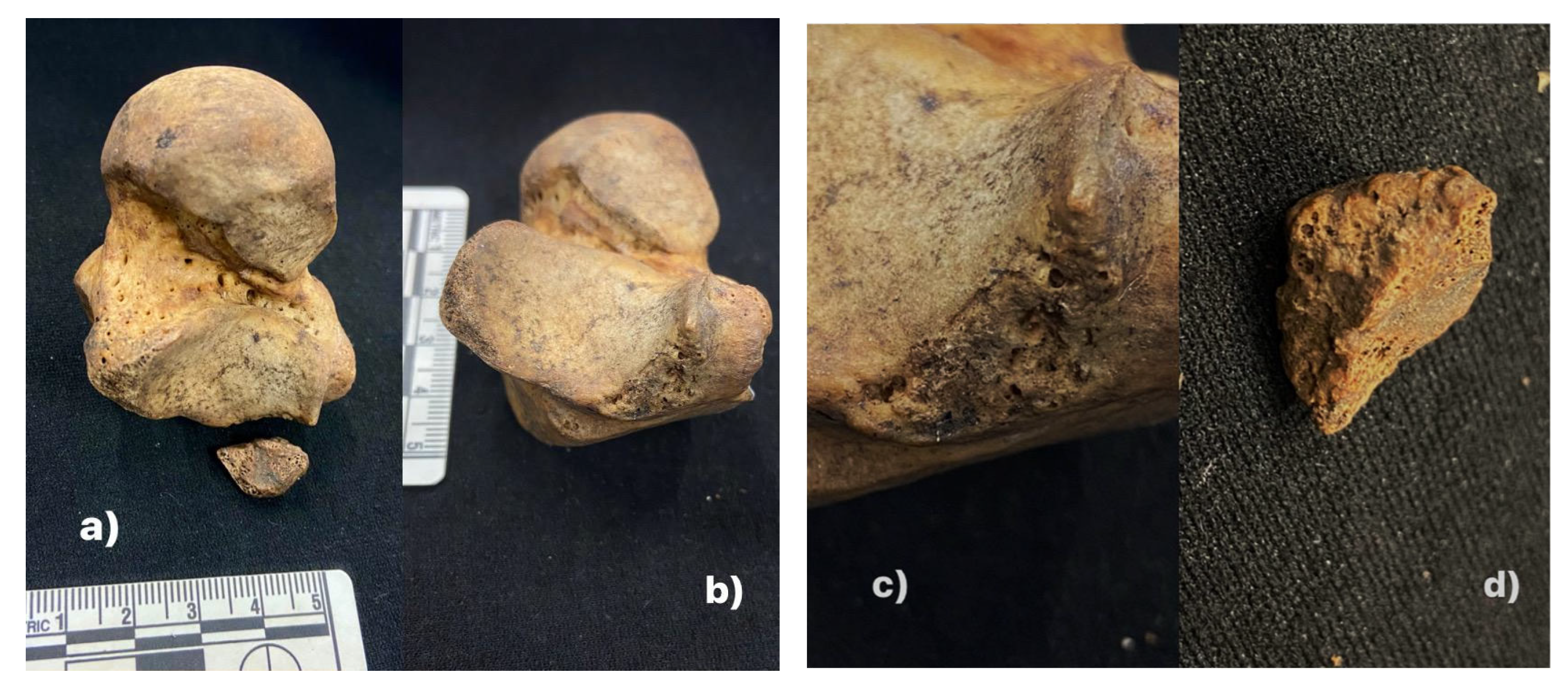
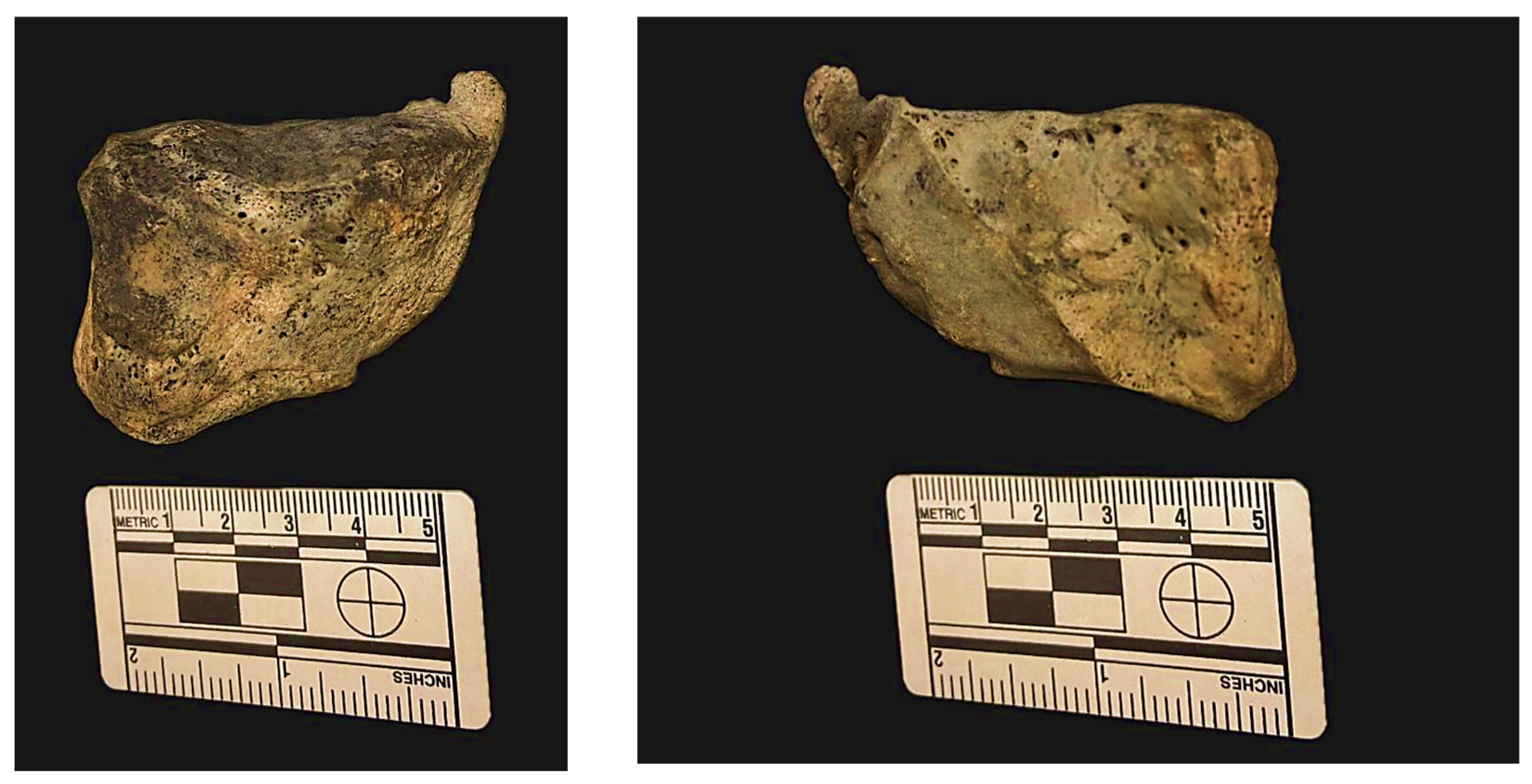
Figure 4.
a) and b) Inferior view of the right talus of a male individual (CISC/XXI/114) with the ossicle free; c) Infero-medial view. Note the triangular shape and d) The free os trigonum.
Figure 4.
a) and b) Inferior view of the right talus of a male individual (CISC/XXI/114) with the ossicle free; c) Infero-medial view. Note the triangular shape and d) The free os trigonum.
Figure 5.
Bilateral case of calcaneum secundarium in a male individual (CISC/XXI/109). Detailed view of the anteromedial aspect of the calcaneus. Note that the anterior and medial facets are continuous.
Figure 5.
Bilateral case of calcaneum secundarium in a male individual (CISC/XXI/109). Detailed view of the anteromedial aspect of the calcaneus. Note that the anterior and medial facets are continuous.
Figure 6.
Superior view of the right calcaneus of a male individual (CISC/XXI/252). The anterior and medial facets are separated.
Figure 6.
Superior view of the right calcaneus of a male individual (CISC/XXI/252). The anterior and medial facets are separated.
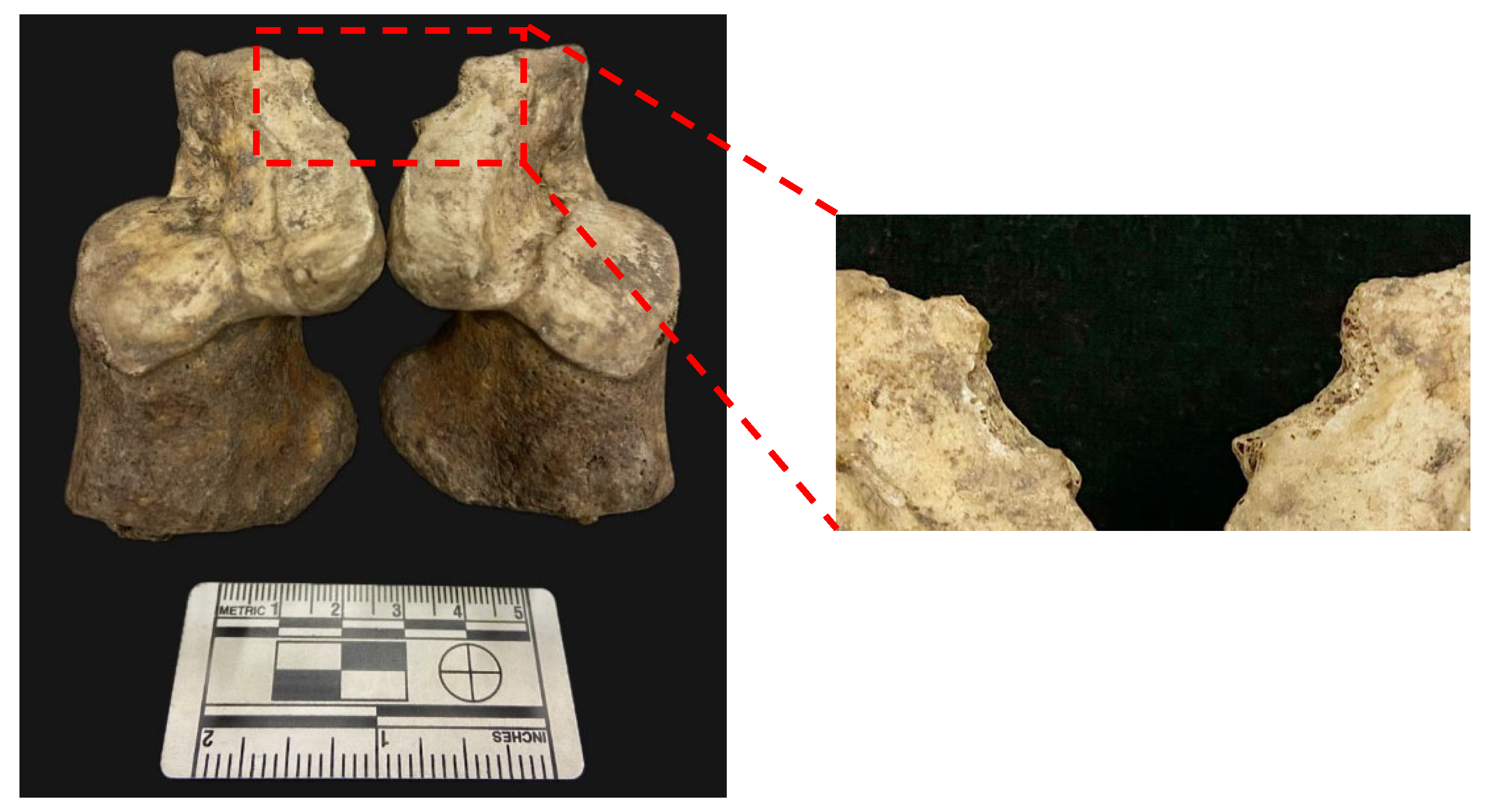
Figure 7.
Right navicular bone of a male individual (CISC/XXI/72), showing a unilateral case of Type II accessory navicular bone. On the close-up (left), note the flattened and porous surfaces of the bone.
Figure 7.
Right navicular bone of a male individual (CISC/XXI/72), showing a unilateral case of Type II accessory navicular bone. On the close-up (left), note the flattened and porous surfaces of the bone.
Figure 8.
Distal and proximal view of the left medial cuneiform of a male individual (CISC/XXI/14) with a fused os intermetatarseum.
Figure 8.
Distal and proximal view of the left medial cuneiform of a male individual (CISC/XXI/14) with a fused os intermetatarseum.
Figure 9.
Proximal view of the 2nd right metatarsal of a male individual (CISC/XXI/58), showing the presence of a fused os intermetatarseum.
Figure 9.
Proximal view of the 2nd right metatarsal of a male individual (CISC/XXI/58), showing the presence of a fused os intermetatarseum.
Table 1.
Prevalence of foot ossicles per individual in the CISC/XXI sample (n: individuals with foot ossicles, N: sample size).
Table 1.
Prevalence of foot ossicles per individual in the CISC/XXI sample (n: individuals with foot ossicles, N: sample size).
| |
Females |
Males |
Total |
| |
Prevalence |
n/N |
Prevalence |
n/N |
Prevalence |
n/N |
| Os trigonum |
8.5 |
7/82 |
10.0 |
8/80 |
9.3 |
15/162 |
| Calcaneum secundarium |
3.8 |
3/80 |
10.1 |
8/79 |
6.9 |
11/159 |
| Accessory navicular bone |
0.0 |
0/80 |
1.3 |
1/80 |
0.6 |
1/160 |
| Os sustentaculum |
0.0 |
0/80 |
0.0 |
0/80 |
0.0 |
0/160 |
| Os vesalianum |
1.3 |
1/80 |
0.0 |
0/79 |
0.6 |
1/159 |
| Os intermetatarseum |
2.5 |
2/79 |
6.6 |
5/76 |
4.5 |
7/155 |
Table 2.
Prevalence of foot ossicles in the CISC/XXI sample (left foot; n: individuals with foot ossicles, N: sample size).
Table 2.
Prevalence of foot ossicles in the CISC/XXI sample (left foot; n: individuals with foot ossicles, N: sample size).
| |
Females |
Males |
Total |
| |
Prevalence |
n/N |
Prevalence |
n/N |
Prevalence |
n/N |
| Os trigonum |
6.3 |
5/79 |
8.0 |
6/75 |
7.1 |
11/154 |
| Calcaneum secundarium |
1.3 |
1/77 |
5.2 |
4/77 |
3.2 |
5/154 |
| Accessory navicular bone |
0.0 |
0/74 |
0.0 |
0/69 |
0.0 |
0/143 |
| Os sustentaculum |
0.0 |
0/76 |
0.0 |
0/77 |
0.0 |
0/153 |
| Os vesalianum |
0.0 |
0/73 |
0.0 |
0/70 |
0.0 |
0/143 |
| Os intermetatarseum |
2.7 |
2/73 |
2.9 |
2/70 |
2.8 |
4/143 |
Table 3.
Prevalence of foot in the CISC/XXI sample (right foot; n: individuals with foot ossicles, N: sample size).
Table 3.
Prevalence of foot in the CISC/XXI sample (right foot; n: individuals with foot ossicles, N: sample size).
| |
Females |
Males |
Total |
| |
Prevalence |
n/N |
Prevalence |
n/N |
Prevalence |
n/N |
| Os trigonum |
6.4 |
5/78 |
5.2 |
5/77 |
6.5 |
10/155 |
| Calcaneum secundarium |
3.8 |
3/78 |
7.8 |
6/77 |
5.8 |
9/155 |
| Accessory navicular bone |
0.0 |
0/74 |
1.3 |
1/76 |
0.7 |
1/150 |
| Os sustentaculum |
0.0 |
0/80 |
0.0 |
0/80 |
0.0 |
0/160 |
| Os vesalianum |
1.3 |
1/80 |
0.0 |
0/79 |
0.6 |
1/159 |
| Os intermetatarseum |
2.5 |
2/79 |
6.6 |
5/76 |
4.5 |
7/155 |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).