1. Introduction
Fournier's gangrene is a rare yet highly aggressive disease, characterized by necrotizing fasciitis affecting the external genitalia, perineum, or perianal area. This rapidly spreading condition requires urgent medical attention and timely interventions to prevent life-threatening complications [
1].
Fournier's gangrene typically arises from local infections in the genital or perianal region and can rapidly progress to severe tissue necrosis, systemic sepsis, and even multiple organ failure.
Patients with predisposing factors, such as diabetes mellitus, immunosuppression, chronic alcoholism, obesity, and peripheral vascular disease, are at a higher risk of developing Fournier's gangrene. Additionally, individuals with underlying colorectal malignancies may be more susceptible to this condition.
The treatment for Fournier's gangrene involves aggressive resuscitation, administration of broad-spectrum antibiotics, and surgical debridement. Early and extensive surgical debridement is essential to control infection and prevent further spread. Multiple debridement procedures may be necessary to ensure complete removal of infected tissue [
2].
Following debridement, patients develop large perineal defects that require reconstruction. Some reconstructive procedures are used in Fournier’s gangrene to provide skin coverage with functional and cosmetic results and less morbidity. The choice of reconstruction method depends on several factors, such as the location and size of the defect and patient's medical condition [
3].
Herein, we present a case of Fournier's gangrene caused by underlying colon cancer in a patient scheduled for chemotherapy.
2. Case Description
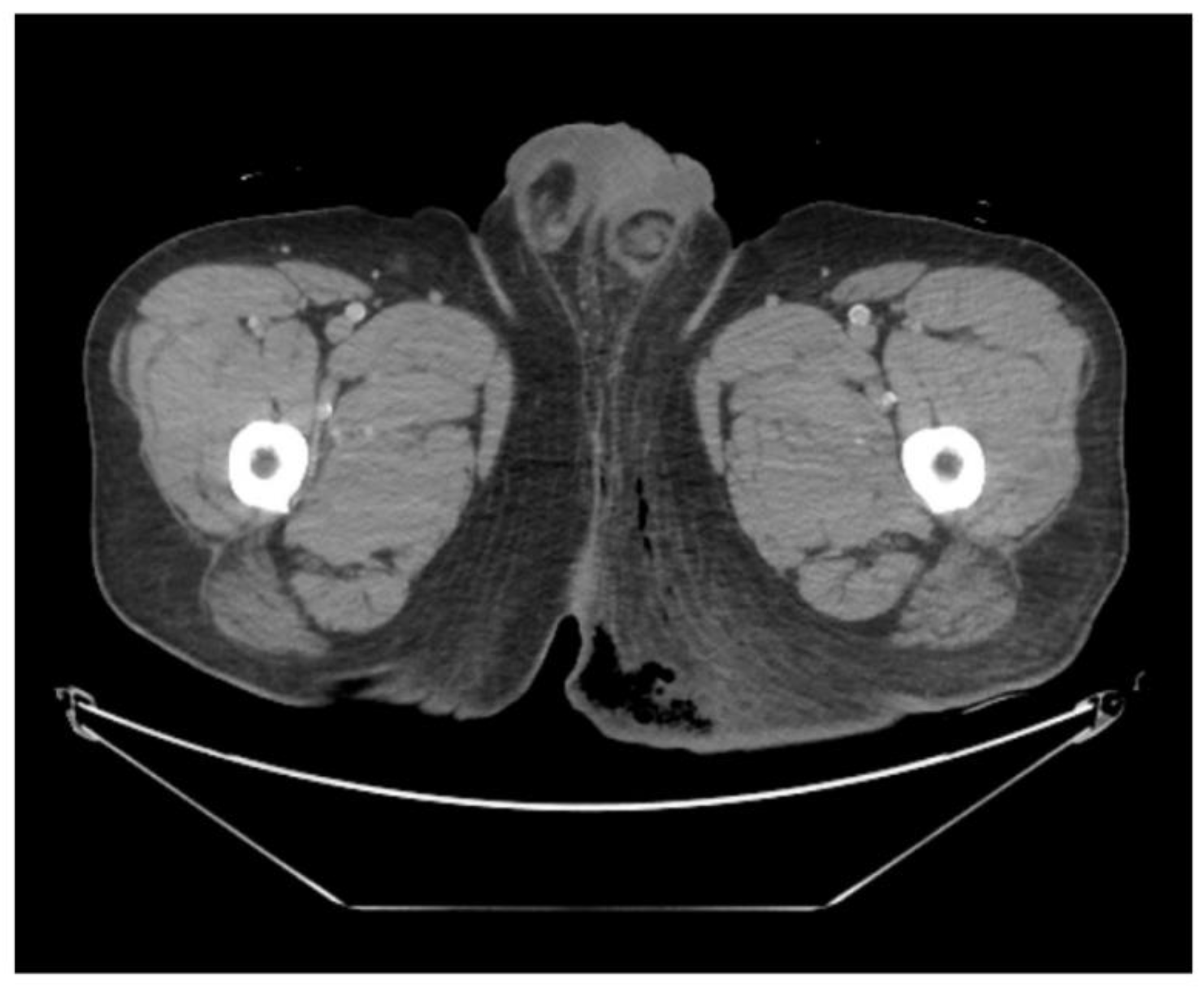
A man in his 40s presented to the emergency department complaining of severe perineal pain and pus discharge from multiple sites in the perineum. The patient had undergone surgery for fistula at another clinic a week ago. He reported a medical history of diabetes, hypertension, and heavy alcohol consumption. Physical examination revealed an edematous scrotum with a foul-smelling exudate. Pelvic computed tomography (CT) revealed air collection in the buttock area, indicating Fournier's gangrene (
Figure 1). Due to the aggressive nature of the condition and the development of sepsis, broad-spectrum antibiotics were promptly initiated. Subsequently, the patient underwent radical debridement in both the General Surgery and Urology departments.
Following serial debridement at the General Surgery Department, the patient was referred to the Plastic and Reconstructive Surgery Department for infection control and reconstruction of the extensive perineal defect (
Figure 2). Negative pressure wound therapy (NPWT) was used to aid in wound healing and reduce defect size. During the course of NPWT for 4 weeks, a decrease in wound size and formation of healthy granulation tissue without any signs of infection was observed (
Figure 3). During follow up, abdominal CT revealed a suspicious region consistent with colon cancer. Further pathological examinations confirmed the diagnosis of rectosigmoid colon cancer. The General Surgery (GS) team strategized a treatment plan involving colostomy and stoma surgery to address the underlying colon cancer. Following surgery, the patient was scheduled to undergo chemotherapy as part of a comprehensive treatment approach. This integrated strategy aimed to manage both Fournier's gangrene and the underlying cancer, maximizing the chances of a successful outcome for the patient.
Under general anesthesia, the GS team performed further debridement and colostomy. Because of the extensive defect measuring 25 x 11 cm from the scrotum to the posterior anal area, we opted for a deep external pudendal artery perforator (DEPAP) flap for reconstruction. The DEPAP flap, based on the posterior pudendal thigh flap, offers well-vascularized tissue ideal for wound healing and minimizes the risk of complications. The perforator was explored and identified in the septum of the groin crease, using a handheld Doppler. Flap elevation began at the distal end of the subfascial plane. Dissection was carefully performed to preserve the integrity of the perforator and surrounding vascular structures. The flap was dissected from the medial thigh to the posterior scrotal level. Once the DEPAP flap was adequately dissected, it was transposed to cover the extensive perineal defect resulting from the previous surgeries. The DEPAP flap is a fasciocutaneous flap that enables direct closure of the donor site. The flap was positioned and secured to the surrounding healthy tissue with meticulous suturing to ensure proper wound closure and minimize tension on the flap (Figure 4).
3. Results
The patient was placed in the supine position with the thigh adducted to relieve tension for 7 days to minimize movement. Drains were removed without any observed side effects such as hematoma or infection; therefore, we encouraged the patient to start walking gradually after 7 days. Since no adverse effect was noted, the patient was discharged from the hospital 14 days after suture removal. The DEPAP flap surgery was successful, and the flap survived without any functional impairment for 9 months postoperatively. The patient showed satisfactory postoperative progress during this period (
Figure 5).
4. Discussion
Fournier’s gangrene is an infrequent yet life-threatening emergency characterized by swiftly spreading necrotizing infections affecting the perineum and external genitalia. This condition is often polymicrobial and encompasses bacteria, posing a substantial risk if not promptly and effectively managed [
4].
Early diagnosis is pivotal for improving patient outcomes. The clinical symptoms of Fournier’s gangrene include intense pain, erythema, edema, and crepitus in the affected areas. Patients may also manifest systemic signs of infection, such as fever, tachycardia, and leukocytosis [
5]. A heightened level of suspicion is crucial, especially in individuals with predisposing factors, such as diabetes mellitus, immunosuppression, and underlying colorectal malignancies, as they are at an elevated risk of developing Fournier’s gangrene [
6].
The initial management of Fournier’s gangrene involves aggressive resuscitation with broad-spectrum antibiotics administration. Surgical intervention is the cornerstone of the treatment for Fournier’s gangrene. Emergency debridement of necrotic tissue is essential to control the infection and prevent further spread. Therefore, serial debridement may be necessary in such cases. However, these procedures often lead to defects in the perineal area [
7]. Reconstruction of scrotal defects after surgical debridement is typically achieved using skin grafts or flaps. However, no consensus on the optimal method of defect reconstruction exists [
8]. The choice of the reconstructive procedure should hinge on the location and size of the defect, patient’s medical condition, and surgeon’s experience [
3].
Fournier’s gangrene is associated with rectosigmoid colon cancer and further complicates the reconstruction process. To address the extensive defect resulting from debridement and colostomy, using a flap is considered an appropriate reconstructive option [
9]. Among the available options, perforator flaps have the advantages of preserving muscle function, reducing donor-site morbidity, versatility in replacing various areas, faster recovery times, and aesthetically pleasing results while preserving a natural appearance [
10]. For defects extending from the scrotum to the posterior anal area, the DEPAP flap is selected owing to its various advantages.
The DEPAP flap offers several benefits over alternative reconstruction techniques. It provides well-vascularized tissue with a color similar to that of the perineal area, diminishing the risk of flap failure. Additionally, the DEPAP flap has potential sensory characteristics and shares the same nerve supply, enhancing functional outcomes. Notably, the operative time for DEPAP flaps is shorter than that for free flaps, thus minimizing surgical complexity [
11].
Overall, the DEPAP flap proved to be a reliable and effective option for reconstructing extensive perineal defects in this challenging case. Its success underscores the importance of considering individual patient factors and selecting an appropriate reconstruction method to achieve optimal outcomes.
5. Conclusions
Fournier’s gangrene is rare in patients with underlying colon cancer scheduled for chemotherapy. The comprehensive treatment approach involving colostomy and subsequent chemotherapy aims to manage both Fournier's gangrene and the underlying cancer, thus enhancing the chances of a successful outcome for the patient. However, this treatment process limits the perineal reconstruction method for defects.
A DEPAP flap offers a reliable solution, providing well-vascularized tissue to promote wound healing and minimize complications. This flap, based on the posterior pudendal thigh flap, demonstrated its efficacy in the present case, leading to successful reconstruction without functional impairment.
Author Contributions
Conceptualization, D.G.K. and K.A.L.; methodology, K.A.L.; software, K.A.L.; validation, K.A.L.; formal analysis, K.A.L.; investigation, D.G.K. and K.A.L.; resources, D.G.K. and K.A.L.; data curation, K.A.L.; writing—original draft preparation, D.G.K. and K.A.L.; writing—review and editing, D.G.K. and K.A.L.; visualization, D.G.K. and K.A.L.; supervision, K.A.L.; project administration, K.A.L.; funding acquisition, K.A.L. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Institutional Review Board of [Institution Name] (IRB No. 2023-12-028-002). Written informed consent was obtained from the patient to publish this paper.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The sharing of data is carried out in accordance with the consent provided by participants on the use of confidential data.
Acknowledgments
During the preparation of this manuscript, the authors used no tool.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Basoglu, M.; Ozbey, I.; Atamanalp, S.S.; Yildirgan, M.I.; Aydinli, B.; Polat, O.; Ozturk, G.; Peker, K.; Onbas, O.; Oren, D. Management of Fournier’s gangrene: review of 45 cases. Surg Today 2007, 37, 558–563. [CrossRef]
- Somville, F.; Swerts, S.; Vandamme, S.; Monsieurs, K. Fournier’s gangrene: a fulminant subcutaneous infection. Acta Chir Belg 2016, 116, 178–183. [CrossRef]
- Insua-Pereira, I.; Ferreira, P.C.; Teixeira, S.; Barreiro, D.; Silva, Á. Fournier’s gangrene: a review of reconstructive options. Cent European J Urol 2020, 73, 74–79. [CrossRef]
- Kordahi, A.M.; Suliman, A.S. A case of Fournier’s gangrene. EPlasty 2017, 17, ic25. PMID: 28959375, PMCID: PMC5609248.
- Singh, A.; Ahmed, K.; Aydin, A.; Khan, M.S.; Dasgupta, P. Fournier’s gangrene. A clinical review. Arch Ital Urol Androl 2016, 88, 157–164. [CrossRef]
- Bruketa, T.; Majerovic, M.; Augustin, G. Rectal cancer and Fournier’s gangrene - current knowledge and therapeutic options. World J Gastroenterol 2015, 21, 9002–9020, PMID: 26290629, PMCID: PMC4533034. [CrossRef]
- Lewis, G.D.; Majeed, M.; Olang, C.A.; Patel, A.; Gorantla, V.R.; Davis, N.; Gluschitz, S. Fournier’s gangrene diagnosis and treatment: A systematic review. Cureus 2021, 13, e18948, PMID: 34815897, PMCID: PMC8605831. [CrossRef]
- Karian, L.S.; Chung, S.Y.; Lee, E.S. Reconstruction of defects after Fournier gangrene: a systematic review. EPlasty 2015, 15, e18.
- Ossibi, P.E.; Souiki, T.; ibn Majdoub, K.; Toughrai, I.; Laalim, S.A.; Mazaz, K.; Tenkorang, S.; Farih, M.H. Fournier gangrene: rare complication of rectal cancer. Pan Afr Med J 2015, 20, 288. [CrossRef]
- Saint-Cyr, M.; Schaverien, M.V.; Rohrich, R.J. Perforator flaps: history, controversies, physiology, anatomy, and use in reconstruction. Plast Reconstr Surg 2009, 123, 132e–145e. [CrossRef]
- AbdAlmoktader, M.A. Abstract: deep external peudendal artery (DEPA) perforator flap for phalloplasty a single stage sensate phallus. Plast Reconstr Surg Glob Open 2018, 6, 186–187. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).