Submitted:
05 November 2025
Posted:
10 November 2025
You are already at the latest version
Abstract
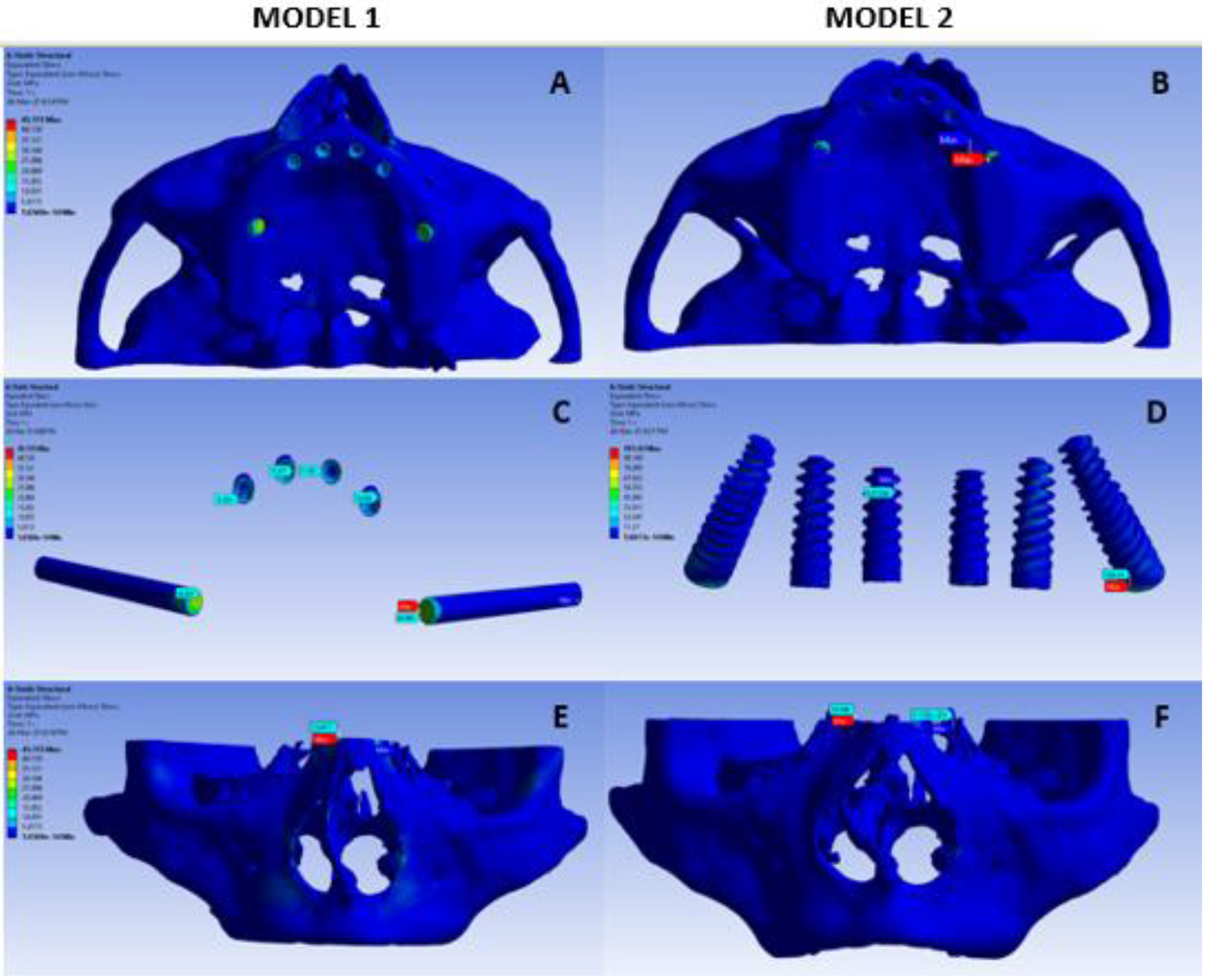
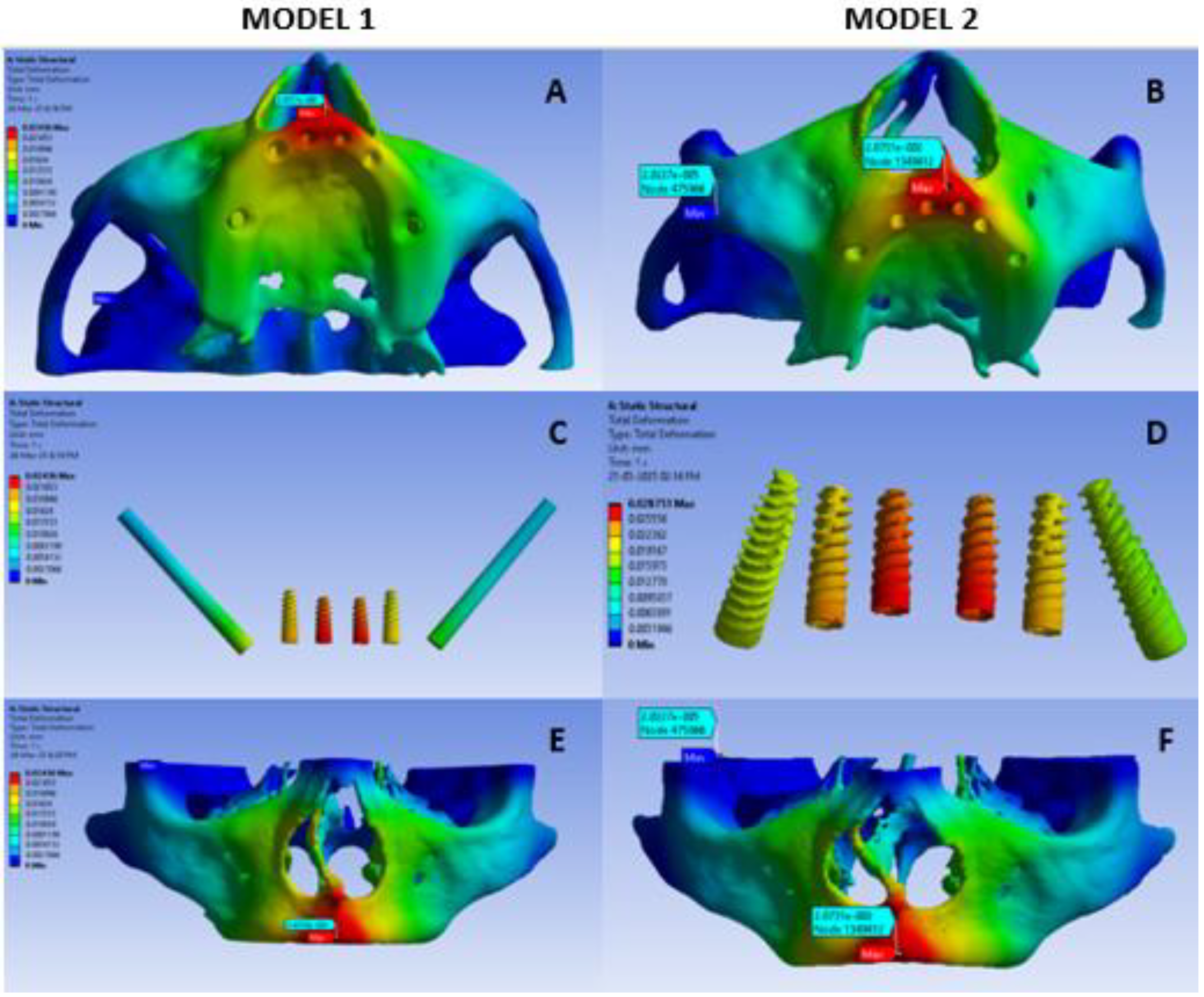
Background: All-on-6 implants are a reliable and efficient full-arch restoration option in patients with atrophic maxilla. Aim: The present study aimed to evaluate and compare the distribution of stress surrounding implants and adjacent osseous structures by utilizing all-on-six tilted and zygomatic methodologies in the maxillary region by using Finite element (FEA) analysis. Material and methods: Two finite element models were constructed with CT images of 50 years female. Model 1 was constructed with zygomatic implants, while model 2 was constructed with tilted implants.A vertical force of 150N on anterior component and 300N on posterior component were applied and maximum stress and deformation was assessed. Results: In the present study, the von Mises stress on the bone, implant and overall was higher in the tilted implant model than the zygomatic implant model. Conclusion: The findings of the present study suggests that zygomatic implants help distribute occlusal loads more favorably, especially under horizontal and combined loading conditions in all-on-six configuration.
Keywords:
Introduction
Materials and Methods
- A.
- Model 1: Zygomatic Implants as Posterior Implants and Four Axial Implants in Anterior Maxilla
- B.
- Model 2: Tilted Implants as Posterior Implants and Four Axial Implant In Anterior Maxilla
Steps of Method
- 1.
- Case Selection
- 2.
- DICOM and STL Files conversion
- 3.
- Construction Of The Basic Finite Element Model Of Maxilla
- 4.
- Construction Of Maxillary Model With Implants
- 5.
- Occlusal Loading
- 6.
- Finite Element Analysis
Results
Discussion
Limitations
Future Perspective
Conclusion
Conflicts of Interest
References
- Blanc O, Shilo D, Weitman E, Capucha T, Rachmiel A. Extramaxillary Zygomatic Implants: An Alternative Approach for the Reconstruction of the Atrophic Maxilla. Ann Maxillofac Surg. 2020 Jan-Jun;10(1):127-132. [Medline: 32855928]. [CrossRef]
- Aalam AA, Krivitsky-Aalam A, Kurtzman GM, Mahesh L. The severely atrophic maxilla: Decision making with zygomatic and pterygoid dental implants. J Oral Biol Craniofac Res. 2023 Mar-Apr;13(2):202-206. [Medline: 37065973]. [CrossRef]
- Taruna M, Chittaranjan B, Sudheer N, Tella S, Abusaad M. Prosthodontic perspective to all-on-4® concept for dental implants. J Clin Diagn Res. 2014 Oct;8(10):ZE16-9. [Medline: 25478475]. [CrossRef]
- Gaviria L, Salcido JP, Guda T, Ong JL. Current trends in dental implants. J Korean Assoc Oral Maxillofac Surg. 2014 Apr;40(2):50-60.
- Arora A, Upadhyaya V, Parashar KR, Malik D. Evaluation of the effect of implant angulations and impression techniques on implant cast accuracy - An in vitro study. J Indian Prosthodont Soc. 2019 Apr-Jun;19(2):149-158.
- Solomon O, Chetrus V, Zaharescu A, Leata R, Ilie M, Covaci AM, Earar K. “ ALL-ON-6”, Advantages and disadvantages of this modern dental restoration solution. Romanian Journal of Oral Rehabilitation. 2024 Oct 1;16(4).
- Forna DA, Constantin BC, Mihali M, Tiutiucă C, Earar K. Complex maxillary and mandibular oral rehabilitation using the all-on-6 concept, case report. Romanian Journal of Oral Rehabilitation. 2023 Apr;15(2):204-12.
- Moraru MC, Buzduga CM, Gurzu IL, Mereuta VD, Ciurcanu OE, Balan M, Al Hage E. the advantage of the all-on-six and all-on-eight technique compared to the all-on-four technique. Romanian Journal of Oral Rehabilitation. 2024 Jan;16(1).
- Gümrükçü Z, Korkmaz YT. Influence of implant number, length, and tilting degree on stress distribution in atrophic maxilla: a finite element study. Medical & biological engineering & computing. 2018 Jun;56:979-89.
- Khatib I, Joshi NV, Rao P, Joshi M, Shetty A, Thorat V, Talreja P. Effect of Implant-Abutment Connection and Abutment Angulations on Peri-implant Stress Levels: A Finite Element Analysis Study. Compendium of continuing education in dentistry (Jamesburg, NJ: 1995). 2024;45(7):e5-9.
- de Souza Rendohl E, Brandt WC. Stress distribution with extra-short implants in an angled frictional system: A finite element analysis study. The Journal of Prosthetic Dentistry. 2020 Dec 1;124(6):728-e1.
- Venkat Ratna Nag P, Sarika P, Bhagwatkar T, Dhara V. Angulated implant a novel concept for rehabilitation of severe atrophic maxilla with 3 years follow up supported by Finite Element Analysis. J Osseointegr 2020;13(1):39-44.
- Shivakumar S, Kudagi VS, Talwade P. Applications of finite element analysis in dentistry: A review. Journal of International Oral Health. 2021 Sep 1;13(5):415-22.
- Piccioni MA, Campos EA, Saad JR, de Andrade MF, Galvão MR, Abi Rached A. Application of the finite element method in dentistry. Revista Sul-Brasileira de Odontologia. 2013;10(4):369-77.
- Tezerişener HA, Özalp Ö, Altay MA, Sindel A. Comparison of stress distribution around all-on-four implants of different angulations and zygoma implants: a 7-model finite element analysis. BMC oral health. 2024 Feb 3;24(1):176.
- Pellizzer EP, Falcón-Antenucci RM, de Carvalho PSP, Sánchez DMIK, Rinaldi GAT, de Aguirre CC, et al. Influence of implant angulation with different crowns on stress distribution. J Craniofac Surg. 2011;22(2):434–7.
- Silva GC, Mendonca JA, Lopes LR, Landre Jr J. Stress patterns on implants in prostheses supported by four or six implants: a three-dimensional finite element analysis. International Journal of Oral & Maxillofacial Implants. 2010 Apr 1;25(2).
- Bedrossian, E. Rehabilitation of the edentulous maxilla with the zygoma concept: a 7-year prospective study. Int J Oral Maxillofac Implants. 2010;25(6):1213–21.
- Abouelhuda AM, Ibrahim AM, Elkenawy MH, Hegazy SA. Maxillary All-on-6 Treatment Using Zygomatic Implants. Bone Loss Evaluation by CBCT: 3-Year Follow-up. International Journal of Prosthodontics. 2025 Jan 1;38(1).
- Yemenoglu H, Beder M, Yaylacı M, Dizdar A, Alkurt M, Naralan ME, Yaylacı EU, Özdemir ME, Öztürk Ş, Yeşil Z. Evaluation of prostheses retained zygomatic and dental implants in large defects in the maxilla due to tumors or major trauma by biomechanical 3- dimensional finite element analysis. BMC Oral Health. 2025 Jan 19;25(1):99. [CrossRef] [PubMed] [PubMed Central]
- Saleh Saber F, Ghasemi S, Koodaryan R, Babaloo A, Abolfazli N. The Comparison of Stress Distribution with Different Implant Numbers and Inclination Angles In All-on-four and Conventional Methods in Maxilla: A Finite Element Analysis. J Dent Res Dent Clin Dent Prospects. 2015 Fall;9(4):246-53. [CrossRef]
- Jaiswal SB, Jain S, Jain V, Grover RK, Kale AA, Talreja L. Evaluation and Comparison of Stresses Between All-on-4 and All-on-6 Treatment Concepts With Three Different Prosthetic Materials in the Maxilla: A Finite Element Analysis Study. Cureus. 2024 Oct 13;16(10).
| Material | Young’s Modulus(MPa) | Poisson’s Ratio | Tensile Yield Strength(MPa) |
|---|---|---|---|
| Titanium | 110000 | 0.35 | 834 |
| Cortical bone | 13700 | 0.3 | 114 |
| Cancellous bone | 1370 | 0.3 | 52 |
| MODEL 1 | MODEL 2 | ||||
|---|---|---|---|---|---|
| Sr. No. | Sensor Name | Minimum | Maximum | Minimum | Maximum |
| 1 | Von Mises Stress Overall(MPa) | MPa | 45.155 MPa | MPa | 101.43 MPa |
| 2 | Von Mises Stress Implant(MPa) | MPa | 44.869 MPa | 0.97MPa | 100.29 MPa |
| 3 | Von Mises Stress Bone(MPa) | MPa5 | 18.418 MPa | MPa | 19.54 MPa |
| 4 | Total Deformation(mm) | 0 mm | 0.024 mm | 0 mm | 0.028 mm |
| 5 | Implant Deformation(mm) | 0.0036 mm | 0.023 mm | 0.016 mm | 0.027 mm |
| 6 | Bone Deformation(mm) | 0 mm | 0.024 mm | 0 mm | 0.028 mm |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





