Submitted:
11 November 2025
Posted:
12 November 2025
Read the latest preprint version here
Abstract
Keywords:
1. Introduction
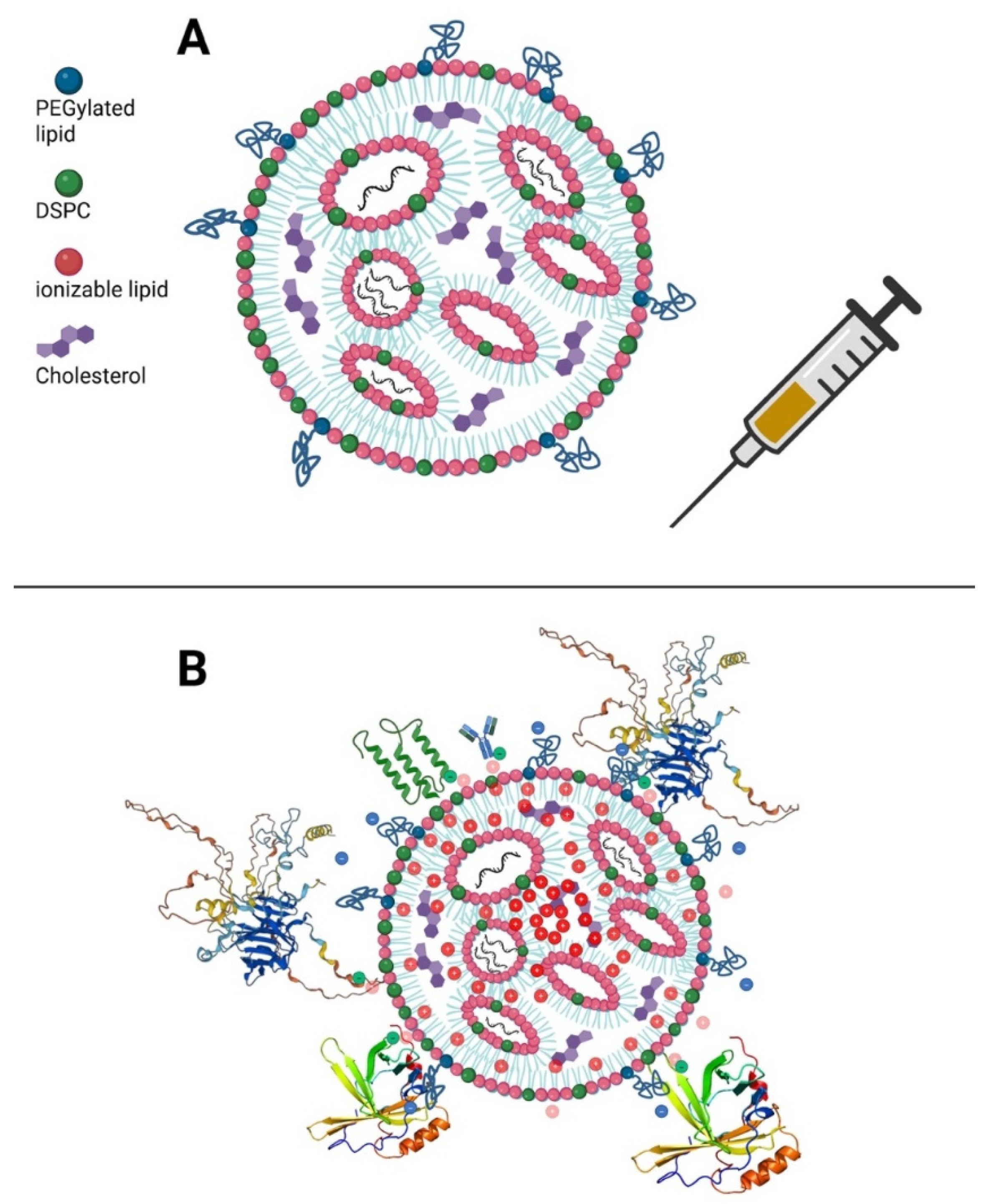
2. Lipid Nanoparticles for mRNA Delivery: Biological Properties and Effects on Cellular Systems
2.1. Factors Influencing Nanoparticle Bioactivity
2.2. LNP Biodistribution
2.3. Mechanisms of Uptake
2.4. Endosomal Escape and Membrane Destabilization Due to Ionizable Lipids
2.5. Spread to Distant Sites via Exosomes
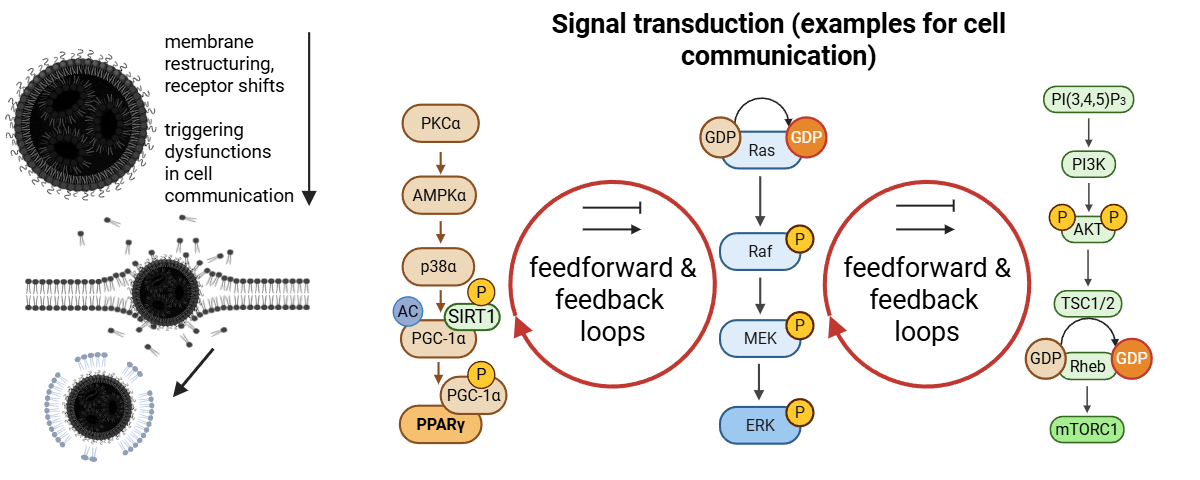
2.6. LNP Metabolism Leads to Oxidative Stress and Signaling Cascades
2.7. Activation of the Immune System
3. The Principles Behind How LNP-modRNA was Thought to Work
4. Omics: Evidence for Membrane Dysfunction Secondary to LNP Transfection
4.1. Ndeupen et al. - A Pioneering Omics Study
4.2. Upregulation of Multiple Inflammatory Markers
4.3. Downregulation of PPAR and AMPK Signaling
4.4. Downregulated Xenobiotic Metabolism by Cytochrome P450 Enzymes
4.5. Non-Canonical Transciptomics and Proteomic Alterations – Are the TLR4 Reactions Decoupled?
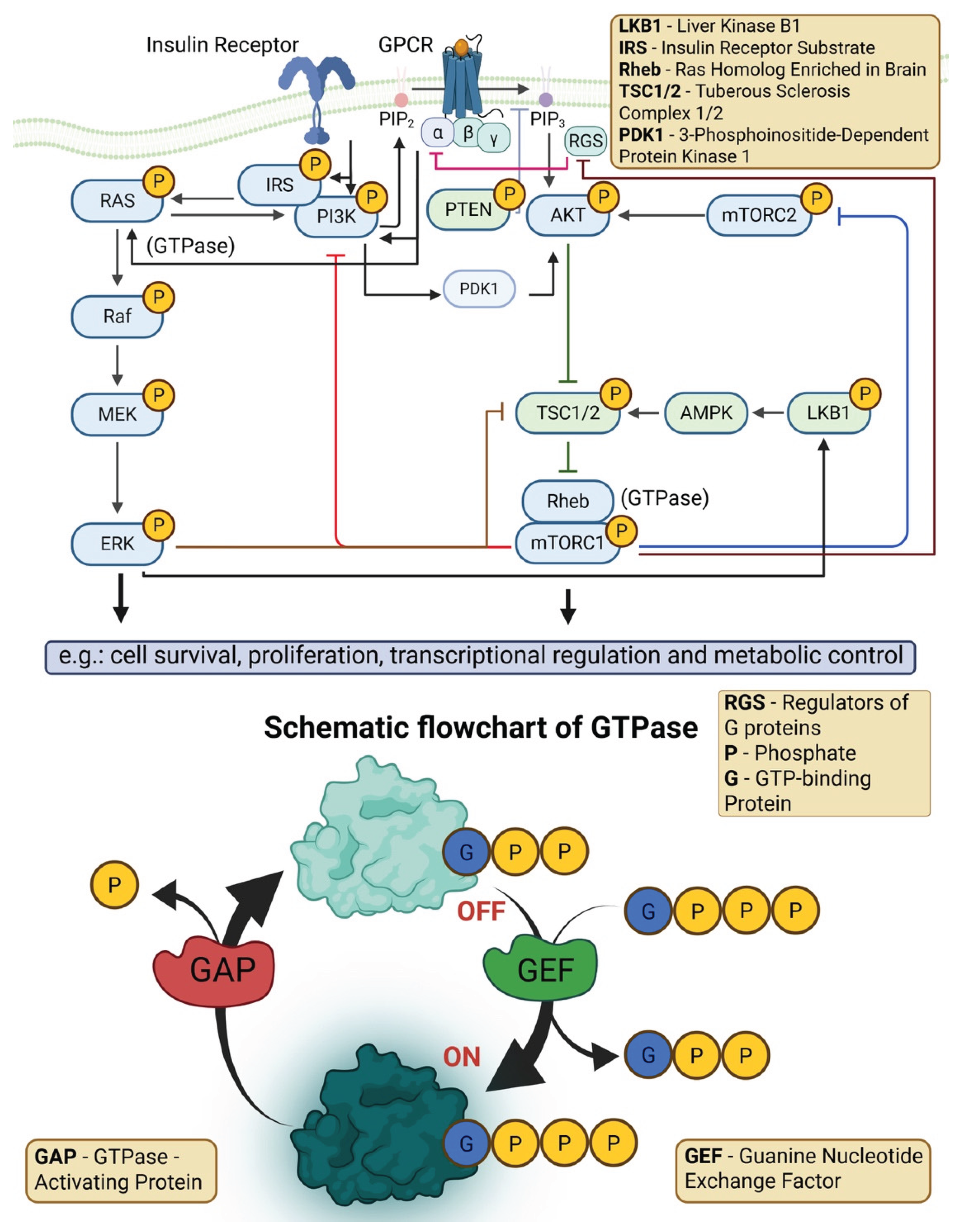
4.6. Dysregulation of MAPK/ERK, JAK-STAT, and other Signaling Pathways
4.7. Further Studies Using Single Cell Analyses Revealing Gender-Based Differences
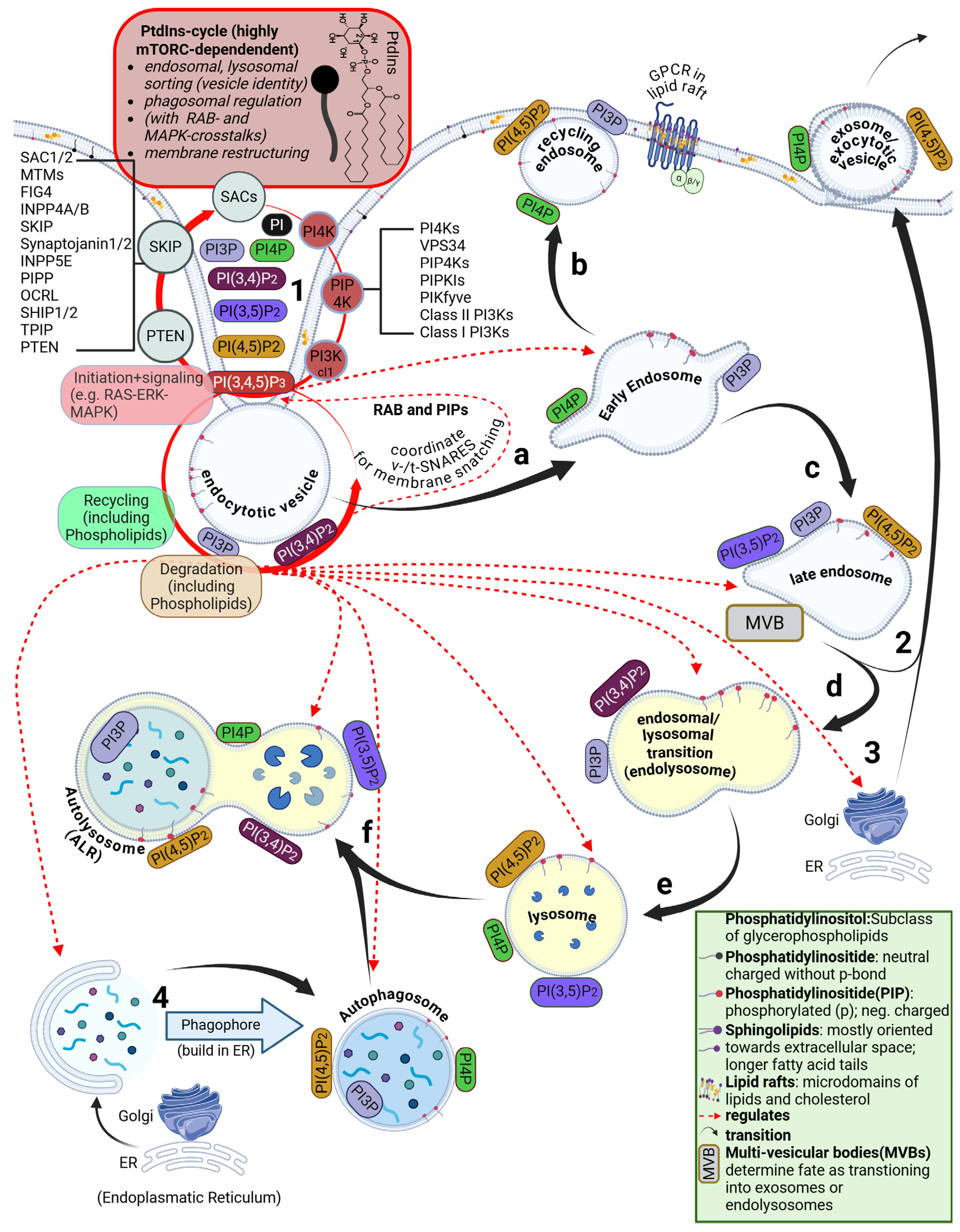
4.8. Disruption of the ESCRT Circuit and Phosphatidylinositol Signaling
4.9. Perturbations Originate at the Plasma Membrane and Disturb PtdIns Signaling Cascades
5. Breaching the Plasma Membrane: Important Roles for Phosphoinositides
5.1. Brief Overview of the Phosphatidylinositide Cycle
5.2. The Role of Lipid Rafts in LNP Uptake into Cells
5.3. Signaling Through Phosphorylation States of Phosphatidylinositols
5.4. Oxysterol-Binding Proteins (OSBs) and a Role for Cholesterol
5.5. How Does 1,2-distearoyl-sn-glycero-3-phosphocholine (DSPC) Affect the PI Cycle?
5.6. A Role for Lipid Impurities
5.7. Small Perturbations Can Lead to Major Shifts in PIP Signaling
6. Discussion
7. Conclusions
Supplementary Materials
Author Contributions
Use of Generative AI
Acknowledgements
Competing Interests
List of Abbreviations
| 4HNE | 4-Hydroxynonenal |
| AKT | Protein Kinase B |
| ALC-0315 | ionizable lipid,[(4-hydroxybutyl)azanediyl]di(hexane-6,1-diyl) bis(2-hexyldecanoate) |
| ALR | Autophagic Lysosome Reformation |
| AMPK | AMP-Activated Protein Kinase |
| APC | Antigen-Presenting Cell |
| AhR | Aryl Hydrocarbon Receptor |
| ApoE | Apolipoprotein E |
| BUB1 | Budding Uninhibited by Benzimidazoles 1 |
| C57BL/6 | C57 black 6: a common inbred mouse strain |
| CARPA | Complement Activation-Related Pseudoallergy |
| CCL2/3/4/7 | Chemokine Ligands |
| CDC25A | Cell Division Cycle 25A |
| CDP-DAG | Cytidine Diphosphate Diacylglycerol |
| CRP | C-Reactive Protein |
| CSF2RB | Colony Stimulating Factor 2 Receptor Beta |
| CYP1A2, CYP2C9, CYP2C19, CYP3A4 | Cytochrome Isoenzymes |
| CYP | Cytochrome P450 |
| DC | Dendritic Cell |
| DEPs | Differentially Expressed Proteins |
| DLin-MC3-DMA | ionizable lipid, (6Z,9Z,28Z,31Z)-Heptatriaconta-6,9,28,31-tetraen-19-yl 4-(dimethylamino)butanoate |
| DSPC | 1,2-Distearoyl-sn-glycero-3-Phosphocholine |
| E2F/E2F1/E2F8 | E2F Transcription Factor Family |
| EMA | European Medicines Agency |
| ER | Endoplasmic Reticulum |
| ERK | Extracellular Signal-Regulated Kinase |
| ESCRT | Endosomal Sorting Complex Required for Transport |
| FDR | False Discovery Rate |
| GM-CSF | Granulocyte-Macrophage Colony-Stimulating Factor |
| GPCR | G-Protein Coupled Receptor |
| GSEA | Gene Set Enrichment Analysis |
| HDL | High-Density Lipoprotein |
| IFN-γ | Interferon-γ |
| IL-1β, IL-2, IL-6, IL-17 | Interleukins |
| IRF | Interferon Regulatory Factor |
| IgE, IgM, IgG | Immunoglobulin Isotypes |
| JAK-STAT | Janus Kinase - Signal Transducer and Activator of Transcription |
| KEGG | Kyoto Encyclopedia of Genes and Genomes |
| KRAS | Kirsten Rat Sarcoma Oncogene |
| L-DMD | Lipid-Nanoparticle-Driven Membrane Dysfunction |
| LC3 | Microtubule-Associated Protein 1A/1B-Light Chain 3 |
| LDL-R | Low-Density Lipoprotein Receptor |
| LDL | Low-Density Lipoprotein |
| LNP | Lipid Nanoparticle |
| MAPK/ERK | The RAS–RAF–MEK–ERK Pathway |
| MAPK | Mitogen-Activated Protein Kinase |
| MC3 | ionizable lipid also known as D-Lin-MC3-DMA |
| MDDC | Monocyte-Derived Dendritic Cell |
| MSigDB | Molecular Signatures Database |
| MVB | Multivesicular Body |
| MyD88 | Myeloid Differentiation Primary Response 88 |
| NES | Normalized Enrichment Score |
| NF-κB | Nuclear Factor Kappa-Light-Chain-Enhancer of Activated B Cells |
| NIK/RELA/RELB | NF-κB Pathway Subunits |
| NLRP3 | NOD-Like Receptor Family Pyrin Domain Containing 3 |
| NOD | Nucleotide-Binding Oligomerization Domain |
| OSBP/OSH | Oxysterol-Binding Protein / Yeast Ortholog |
| PA | Phosphatidic Acid |
| PBMC | Peripheral Blood Mononuclear Cell |
| PBS | Phosphate-Buffered Saline |
| PC | Phosphatidylcholine |
| PEG | Polyethylene Glycol |
| PEGylated | Covalently Modified with Polyethylene Glycol |
| PET-CT | Positron Emission Tomography–Computed Tomography |
| PI3K | Phosphatidylinositol-3-Kinase |
| PI3P, PI4P, PI (4,5) P2, PI (3,4,5) P3 | Phosphorylated PI Species |
| PIP | Phosphoinositide |
| PPAR | Peroxisome Proliferator-Activated Receptor |
| PTEN | Phosphatase and Tensin Homolog |
| PtdIns/PI | Phosphatidylinositol |
| RE | Recycling Endosome |
| RES | Reticuloendothelial System |
| RIG-I | Retinoic Acid–Inducible Gene I |
| ROS | Reactive Oxygen Species |
| RRM2 | Ribonucleotide Reductase Regulatory Subunit M2 |
| SM-102 | ionizable lipid:1-Octylnonyl 8-[(2-hydroxyethyl)[6-oxo-6-(undecyloxy) hexyl]amino]octanoate |
| SPARKLE | Strategic Peptide Anchored Retained Kept after Lipid Elimination |
| STAT3/STAT5 | Signal Transducer and Activator of Transcription 3 / 5 |
| TBK1 | Tank-Binding Kinase 1 |
| TCA | Tricarboxylic Acid Cycle |
| TGF-β | Transforming Growth Factor β |
| TLR2/3/4/7/8/9 | Specific Toll-Like Receptor Types |
| TLR | Toll-Like Receptor |
| TNF-α | Tumor Necrosis Factor Alpha |
| TRIF | TLR4 Signaling Adaptors |
| Tm | Transition Temperature |
| V-ATPase | Vacuolar ATPase |
| WIPI2 | WD Repeat Domain Phosphoinositide-Interacting Protein 2 |
| WT | Wild Type |
| mRNA | Messenger Ribonucleic Acid |
| mTOR/mTORC1/mTORC2 | Mechanistic Target of Rapamycin (Complex 1 / 2) |
| modRNA | Modified Messenger RNA |
| p53 | Tumour Suppressor Protein p53 |
| qPCR | Quantitative Polymerase Chain Reaction |
| siRNA | Small Interfering RNA |
| ζ | Zeta Potential (Surface Charge) |
References
- Khurana A, Allawadhi P, Khurana I, Allwadhi S, Weiskirchen R, Banothu AK, Chhabra D, Joshi K, Bharani KK. Role of nanotechnology behind the success of mRNA vaccines for COVID-19. Nano Today. 2021 Jun;38:101142. [CrossRef]
- Hald Albertsen C, Kulkarni JA, Witzigmann D, Lind M, Petersson K, Simonsen JB. The role of lipid components in lipid nanoparticles for vaccines and gene therapy. Adv Drug Deliv Rev 2022; 188: 114416. [CrossRef]
- Swetha K, Kotla NG, Tunki L, Jayaraj A, Bhargava SK, Hu H, Bonam SR, Kurapati R. Recent advances in the lipid nanoparticle-mediated delivery of mRNA vaccines. Vaccines (Basel). 2023 Mar 14;11(3):658. [CrossRef]
- Suk JS, Xu Q, Kim N, Hanes J, Ensign LM. PEGylation as a strategy for improving nanoparticle-based drug and gene delivery. Adv Drug Deliv Rev. 2016 Apr 1;99(Pt A):28-51. [CrossRef]
- Ju Y, Carreo JM, Simon V, Dawson K, Krammer F, Kent SJ. Impact of anti-PEG antibodies induced by SARS-CoV-2 mRNA vaccines. Nat Rev Immunol. 2023 Mar;23(3):135-136. [CrossRef]
- Zhou ZH, Stone CA Jr, Jakubovic B, Phillips EJ, Sussman G, Park J, Hoang U, Kirshner SL, Levin R, Kozlowski S. Anti-PEG IgE in anaphylaxis associated with polyethylene glycol. J Allergy Clin Immunol Pract. 2021 Apr;9(4):1731-1733.e3. [CrossRef]
- Kozma GT, Shimizu T, Ishida T, Szebeni J. Anti-PEG antibodies: Properties, formation, testing and role in adverse immune reactions to PEGylated nano-biopharmaceuticals. Adv Drug Deliv Rev. 2020;154-155:163-175. [CrossRef]
- Khalid MB, Frischmeyer-Guerrerio PA. The conundrum of COVID-19 mRNA vaccine-induced anaphylaxis. J Allergy Clin Immunol Glob. 2023 Feb;2(1):1-13. [CrossRef]
- Zelkoski AE, Lu Z, Sukumar G, Dalgard C, Said H, Alameh MG, Mitre E, Malloy AMW. Ionizable lipid nanoparticles of mRNA vaccines elicit NF-κB and IRF responses through toll-like receptor 4. NPJ Vaccines. 2025 Apr 17;10(1):73. [CrossRef]
- Lee Y, Jeong M, Park J, Jung H, Lee H. Immunogenicity of lipid nanoparticles and its impact on the efficacy of mRNA vaccines and therapeutics. Exp Mol Med. 2023 Oct;55(10):2085-2096. [CrossRef]
- Kimura S, Okada K, Matsubara N, Lyu F, Tsutsumi S, Kimura Y, Hashiya F, Inagaki M, Abe N, Abe H. In vivo demonstration of enhanced mRNA delivery by cyclic disulfide-containing lipid nanoparticles for facilitating endosomal escape. RSC Med Chem. 2025 Jun 27;16(9):4122-4137. [CrossRef]
- Gutschi LM, Seger F. Complexity, unpredictability and safety challenges of lipid nanoparticles. Zenodo preprint. Oct 13, 2025. [CrossRef]
- Boros LG, Kyriakopoulos AM, Brogna C, Piscopo M, McCullough PA, Seneff S. Long-lasting, biochemically modified mRNA, and its frameshifted recombinant spike proteins in human tissues and circulation after COVID-19 vaccination. Pharmacol Res Perspect. 2024 Jun;12(3):e1218. [CrossRef]
- Cordes J, Zhao S, Engel CM, Stingele J. Cellular responses to RNA damage. Cell. 2025 Feb 20;188(4):885-900. [CrossRef]
- Kaludercic N, Deshwal S, Di Lisa F. Reactive oxygen species and redox compartmentalization. Front Physiol. 2014 Aug 12;5:285. [CrossRef]
- Kim KQ, Burgute BD, Tzeng SC, Jing C, Jungers C, Zhang J, Yan LL, Vierstra RD, Djuranovic S, Evans BS, Zaher HS. N1-methylpseudouridine found within COVID-19 mRNA vaccines produces faithful protein products. Cell Rep. 2022 Aug 30;40(9):111300. [CrossRef]
- Röltgen K, Nielsen SCA, Silva O, Younes SF, Zaslavsky M, Costales C, Yang F, Wirz OF, Solis D, Hoh RA, Wang A, Arunachalam PS, Colburg D, Zhao S, Haraguchi E, Lee AS, Shah MM, Manohar M, Chang I, Gao F, Mallajosyula V, Li C, Liu J, Shoura MJ, Sindher SB, Parsons E, Dashdorj NJ, Dashdorj ND, Monroe R, Serrano GE, Beach TG, Chinthrajah RS, Charville GW, Wilbur JL, Wohlstadter JN, Davis MM, Pulendran B, Troxell ML, Sigal GB, Natkunam Y, Pinsky BA, Nadeau KC, Boyd SD. Immune imprinting, breadth of variant recognition, and germinal center response in human SARS-CoV-2 infection and vaccination. Cell. 2022 Mar 17;185(6):1025-1040.e14. [CrossRef]
- Kim W, Ly NK, He Y, Li Y, Yuan Z, Yeo Y. Protein corona: Friend or foe? Co-opting serum proteins for nanoparticle delivery. Adv Drug Deliv Rev. 2023 Jan;192:114635. [CrossRef]
- Suzuki Y, Ishihara H. Difference in the lipid nanoparticle technology employed in three approved siRNA (Patisiran) and mRNA (COVID-19 vaccine) drugs. Drug Metab Pharmacokinet. 2021 Dec;41:100424. [CrossRef]
- Buckley M, Araínga M, Maiorino L, Pires IS, Kim BJ, Michaels KK, Dye J, Qureshi K, Zhang YJ, Mak H, Steichen JM, Schief WR, Villinger F, Irvine DJ. Visualizing lipid nanoparticle trafficking for mRNA vaccine delivery in non-human primates. Mol Ther. 2025 Mar 5;33(3):1105-1117. [CrossRef]
- Sasaki K, Sato Y, Okuda K, Iwakawa K, Harashima H. mRNA-loaded lipid nanoparticles targeting dendritic cells for cancer immunotherapy. Pharmaceutics. 2022 Jul 28;14(8):1572. [CrossRef]
- Hassett KJ, Rajlic IL, Bahl K, White R, Cowens K, Jacquinet E, Burke KE. mRNA vaccine trafficking and resulting protein expression after intramuscular administration. Mol Ther Nucleic Acids. 2023 Nov 24;35(1):102083. [CrossRef]
- Maugeri M, Nawaz M, Papadimitriou A, Angerfors A, Camponeschi A, Na M, Hölttä M, Skantze P, Johansson S, Sundqvist M, Lindquist J, Kjellman T, Mrtensson I-L, Jin T, Sunnerhagen P, Ostman S, Lindfors L, Valadi H. Linkage between endosomal escape of LNP-mRNA and loading into EVs for transport to other cells. Nat Commun 2019; 10: 4333. [CrossRef]
- Inam W, Bhadane R, Akpolat RN, Taiseer RA, Filippov SK, Salo-Ahen OMH, Rosenholm JM, Zhang H. Interactions between polymeric nanoparticles and different buffers as investigated by zeta potential measurements and molecular dynamics simulations. View 2022; 3(4): 20210009. [CrossRef]
- Simak J, De Paoli S. The effects of nanomaterials on blood coagulation in hemostasis and thrombosis. Wiley Interdiscip Rev Nanomed Nanobiotechnol. 2017 Sep;9(5). [CrossRef]
- Brooks DE, Seaman GVF. The effect of neutral polymers on the electrokinetic potential of cells and other charged particles. I. Models for the zeta potential increase. J Colloid Interf Sci. 1973 ;43 (3):670-686.
- Ilinskaya AN, Dobrovolskaia MA. Nanoparticles and the blood coagulation system. Part II: safety concerns. Nanomedicine (Lond). 2013 Jun;8(6):969-81. [CrossRef]
- Omo-Lamai S, Zamora ME, Patel MN, Wu J, Nong J, Wang Z, Peshkova A, Majumder A, Melamed JR, Chase LS, Essien EO, Weissman D, Muzykantov VR, Marcos-Contreras OA, Myerson JW, Brenner JS. Physicochemical targeting of lipid nanoparticles to the lungs induces clotting: Mechanisms and solutions. Adv Mater. 2024 Jun;36(26):e2312026. [CrossRef]
- Bekal S, Husari G, Okura M, Huang CA, Bukari MS. Thrombosis development after mRNA COVID-19 vaccine administration: A Case Series. Cureus. 2023 Jul 4;15(7):e41371. [CrossRef]
- Kent SJ, Li S, Amarasena TH, Reynaldi A, Lee WS, Leeming MG, O'Connor DH, Nguyen J, Kent HE, Caruso F, Juno JA, Wheatley AK, Davenport MP, Ju Y. Blood distribution of SARS-CoV-2 lipid nanoparticle mRNA vaccine in humans. ACS Nano. 2024 Oct 1;18(39):27077-27089. [CrossRef]
- Ren Y, Lin L, Abdallah M, Zhu X, Liu H, Fabb SA, Payne TJ, Pouton CW, Johnston APR, Trevaskis NL. Impact of ionizable lipid type on the pharmacokinetics and biodistribution of mRNA-lipid nanoparticles after intravenous and subcutaneous injection. J Control Release. 2025 Aug 10;384:113945. [CrossRef]
- Luo J, Molbay M, Chen Y, Horvath I, Kadletz K, Kick B, Zhao S, Al-Maskari R, Singh I, Ali M, Bhatia HS, Minde DP, Negwer M, Hoeher L, Calandra GM, Groschup B, Su J, Kimna C, Rong Z, Galensowske N, Todorov MI, Jeridi D, Ohn TL, Roth S, Simats A, Singh V, Khalin I, Pan C, Arús BA, Bruns OT, Zeidler R, Liesz A, Protzer U, Plesnila N, Ussar S, Hellal F, Paetzold J, Elsner M, Dietz H, Erturk A. Nanocarrier imaging at single-cell resolution across entire mouse bodies with deep learning. Nat Biotechnol. 2025 Jan 14. Epub ahead of print. [CrossRef]
- Di J, Du Z, Wu K, Jin S, Wang X, Li T, Xu Y. Biodistribution and non-linear gene expression of mRNA LNPs affected by delivery route and particle size. Pharm Res. 2022 Jan;39(1):105-114. [CrossRef]
- Dey AK, Nougarède A, Clément F, Fournier C, Jouvin-Marche E, Escudé M, Jary D, Navarro FP, Marche PN. Tuning the immunostimulation properties of cationic lipid nanocarriers for nucleic acid delivery. Front Immunol. 2021 Aug 23;12:722411. [CrossRef]
- Zhang W, Liu R, Chen Y, Wang M, Du J. Crosstalk between oxidative stress and exosomes. Oxid Med Cell Longev. 2022 Aug 30;2022:3553617. [CrossRef]
- Wei C, Zhu Y, Lu X, Goodier KD, Yu D, Liu X, Choy J, Calderón AT, Ma J, Su Y, Lin J, Li S, Schneck JP, Murphy SC, Mao H-Q. Systemic trafficking of mRNA lipid nanoparticle vaccine following intramuscular injection generates potent tissue-specific T cell response. bioRxiv Preprint. April 24, 2025. [CrossRef]
- Balcorta HV, Mata Corral MY, Gallegos A, Chavez J, Perez J, Balivada S, Natividad-Diaz SL, Poon W. Development of chemical tags for universal lipid nanoparticle visualization and tracking in 2D and 3D imaging. Nano Lett. 2025 May 14;25(19):7682-7689. [CrossRef]
- Yamamoto K, Mashiba T, Takano K, Suzuki T, Kami M, Takita M, Kusumi E, Mizuno Y, Hamaki T. A case of exacerbation of subclinical hyperthyroidism after first administration of BNT162b2 mRNA COVID-19 vaccine. Vaccines (Basel). 2021 Sep 29;9(10):1108. [CrossRef]
- Hummel A, Oniszczuk J, Kervella D, Charbit M, Guerrot D, Testa A, Philipponnet C, Chauvet C, Guincestre T, Brochard K, Benezech A, Figueres L, Belenfant X, Guarnieri A, Demoulin N, Benetti E, Miglinas M, Dessaix K, Morelle J, Angeletti A, Sellier-Leclerc AL, Ranchin B, Goussard G, Hudier L, Bacchetta J, Servais A, Audard V. Idiopathic nephrotic syndrome relapse following COVID-19 vaccination: a series of 25 cases. Clin Kidney J. 2022 May 6;15(8):1574-1582. [CrossRef]
- Malayala SV, Papudesi BN, Sharma R, Vusqa UT, Raza A. A case of idiopathic thrombocytopenic purpura after booster dose of BNT162b2 (Pfizer-Biontech) COVID-19 vaccine. Cureus. 2021 Oct 23;13(10):e18985. [CrossRef]
- Shumnalieva R, Ravichandran N, Hannah J, Javaid M, Darooka N, Roy D, Gonzalez DE, Velikova T, Milchert M, Kuwana M, Joshi M, Gracia-Ramos AE, Boyd P, Yaadav P, Cheng K, Kobert L, Cavagna L, Sen P, Day J, Makol A, Gutiérrez CET, Caballero-Uribe CV, Saha S, Parodis I, Dey D, Nikiphorou E, Distler O, Kadam E, Tan AL, Shinjo SK, Ziade N, Knitza J, Chinoy H, Aggarwal R, Agarwal V, Gupta L; COVAD Study Group. Characteristics of emerging new autoimmune diseases after COVID-19 vaccination: A sub-study by the COVAD group. Int J Rheum Dis. 2024 May;27(5):e15180. [CrossRef]
- Broachwala M, Banks DW, Jevotovsky DS, Oehlermarx W, Durbhakula S. Burning mouth syndrome following Covid vaccination: A case report. Clin Case Rep. 2025 Apr 29;13(5):e70329. [CrossRef]
- Fraiman J, Erviti J, Jones M, Greenland S, Whelan P, Kaplan RM, Doshi P. Serious adverse events of special interest following mRNA COVID-19 vaccination in randomized trials in adults. Vaccine. 2022 Sep 22;40(40):5798-5805. [CrossRef]
- Faksova K, Walsh D, Jiang Y, Griffin J, Phillips A, Gentile A, Kwong JC, Macartney K, Naus M, Grange Z, Escolano S, Sepulveda G, Shetty A, Pillsbury A, Sullivan C, Naveed Z, Janjua NZ, Giglio N, Perälä J, Nasreen S, Gidding H, Hovi P, Vo T, Cui F, Deng L, Cullen L, Artama M, Lu H, Clothier HJ, Batty K, Paynter J, Petousis-Harris H, Buttery J, Black S, Hviid A. COVID-19 vaccines and adverse events of special interest: A multinational Global Vaccine Data Network (GVDN) cohort study of 99 million vaccinated individuals. Vaccine. 2024 Apr 2;42(9):2200-2211. [CrossRef]
- Kim HJ, Kim MH, Choi MG, Chun EM. 1-year risks of cancers associated with COVID-19 vaccination: a large population-based cohort study in South Korea. Biomark Res. 2025 Sep 26;13(1):114. [CrossRef]
- Abbasi R, Shineh G, Mobaraki M, Doughty S, Tayebi L. Structural parameters of nanoparticles affecting their toxicity for biomedical applications: a review. Journal of Nanoparticle Research 2023; 25(3): 43. [CrossRef]
- Yuan Z, Yan R, Fu Z, Wu T, Ren C. Impact of physicochemical properties on biological effects of lipid nanoparticles: Are they completely safe. Sci Total Environ. 2024 Jun 1;927:172240. [CrossRef]
- Szebeni J, Kiss B, Bozó T, Turjeman K, Levi-Kalisman Y, Barenholz Y, Kellermayer M. Insights into the structure of Comirnaty COVID-19 vaccine: A theory on soft, partially bilayer-covered nanoparticles with hydrogen bond-stabilized mRNA-lipid complexes. ACS Nano. 2023 Jul 25;17(14):13147-13157. [CrossRef]
- Brader ML, Williams SJ, Banks JM, Hui WH, Zhou ZH, Jin L. Encapsulation state of messenger RNA inside lipid nanoparticles. Biophys J. 2021 Jul 20;120(14):2766-2770. [CrossRef]
- Münter R, Larsen JB, Andresen TL. The vast majority of nucleic acid-loaded lipid nanoparticles contain cargo. J Colloid Interface Sci. 2024 Nov 15;674:139-144. [CrossRef]
- Li S, Hu Y, Li A, Lin J, Hsieh K, Schneiderman Z, Zhang P, Zhu Y, Qiu C, Kokkoli E, Wang TH, Mao HQ. Payload distribution and capacity of mRNA lipid nanoparticles. Nat Commun. 2022 Sep 23;13(1):5561. [CrossRef]
- Chen X, Ye Y, Li M, Zuo T, Xie Z, Ke Y, Cheng H, Hong L, Liu Z. Structural characterization of mRNA lipid nanoparticles (LNPs) in the presence of mRNA-free LNPs. J Control Release. 2025 Oct 10;386:114082. [CrossRef]
- Rampado R, Crotti S, Caliceti P, Pucciarelli S, Agostini M. Recent advances in understanding the protein corona of nanoparticles and in the formulation of "stealthy" nanomaterials. Front Bioeng Biotechnol. 2020 Apr 3;8:166. [CrossRef]
- Sun Y, Zhou Y, Rehman M, Wang YF, Guo S. Protein corona of nanoparticles: Isolation and analysis. Chem Bio Eng. 2024 Oct 3;1(9):757-772. [CrossRef]
- Voke E, Arral M, Squire HJ, Lin TJ, Coreas R, Lui A, Iavarone AT, Pinals RL, Whitehead KA, Landry M. Protein corona formed on lipid nanoparticles compromises delivery efficiency of mRNA cargo. bioRxiv [Preprint]. 2025 Jan 24:2025.01.20.633942. [CrossRef]
- Sebastiani F, Yanez Arteta M, Lerche M, Porcar L, Lang C, Bragg RA, Elmore CS, Krishnamurthy VR, Russell RA, Darwish T, Pichler H, Waldie S, Moulin M, Haertlein M, Forsyth VT, Lindfors L, Cárdenas M. Apolipoprotein E binding drives structural and compositional rearrangement of mRNA-containing lipid nanoparticles. ACS Nano. 2021 Apr 27;15(4):6709-6722. [CrossRef]
- Liu K, Nilsson R, Lázaro-Ibáñez E, Duàn H, Miliotis T, Strimfors M, Lerche M, Salgado Ribeiro AR, Ulander J, Lindén D, Salvati A, Sabirsh A. Multiomics analysis of naturally efficacious lipid nanoparticle coronas reveals high-density lipoprotein is necessary for their function. Nat Commun. 2023 Jul 6;14(1):4007. [CrossRef]
- Hosseini-Kharat M, Bremmell KE, Prestidge CA. Why do lipid nanoparticles target the liver? Understanding of biodistribution and liver-specific tropism. Mol Ther Methods Clin Dev. 2025 Feb 15;33(1):101436. [CrossRef]
- Therapeutic Goods Administration. Nonclinical Evaluation Report BNT162b2 [mRNA] COVID-19 vaccine (COMIRNATY). Health, Ed.; Department of Health and Aged Care. https://www.tga.gov.au/sites/default/files/foi-2389-06.pdf, 2021; Vol. FOI 2389.
- Neves AR, Queiroz JF, Costa Lima SA, Figueiredo F, Fernandes R, Reis S. Cellular uptake and transcytosis of lipid-based nanoparticles across the intestinal barrier: Relevance for oral drug delivery. J Colloid Interface Sci. 2016 Feb 1;463:258-65. [CrossRef]
- Haghighi E, Abolmaali SS, Dehshahri A, Mousavi Shaegh SA, Azarpira N, Tamaddon AM. Navigating the intricate in-vivo journey of lipid nanoparticles tailored for the targeted delivery of RNA therapeutics: a quality-by-design approach. J Nanobiotechnology. 2024 Nov 14;22(1):710. [CrossRef]
- Khare P, Edgecomb SX, Hamadani CM, Tanner EEL, S Manickam D. Lipid nanoparticle-mediated drug delivery to the brain. Adv Drug Deliv Rev. 2023 Jun;197:114861. [CrossRef]
- Chen J, Xu Y, Zhou M, Xu S, Varley AJ, Golubovic A, Lu RXZ, Wang KC, Yeganeh M, Vosoughi D, Li B. Combinatorial design of ionizable lipid nanoparticles for muscle-selective mRNA delivery with minimized off-target effects. Proc Natl Acad Sci U S A. 2023 Dec 12;120(50):e2309472120. [CrossRef]
- Younis MA, Sato Y, Elewa YHA, Kon Y, Harashima H. Self-homing nanocarriers for mRNA delivery to the activated hepatic stellate cells in liver fibrosis. J Control Release. 2023 Jan;353:685-698. [CrossRef]
- Naasani, I. Establishing the pharmacokinetics of genetic vaccines is essential for maximising their safety and efficacy. Clin Pharmacokinet. 2022 Jul;61(7):921-927. [CrossRef]
- European Medical Assessment. 2020. https://www.ema.europa.eu/en/documents/assessment-report/comirnaty-epar-public-assessment-report en.pdf.
- Akhter MH, Khalilullah H, Gupta M, Alfaleh MA, Alhakamy NA, Riadi Y, Md S. Impact of protein corona on the biological identity of nanomedicine: Understanding the fate of nanomaterials in the biological milieu. Biomedicines. 2021 Oct 19;9(10):1496. [CrossRef]
- Behzadi S, Serpooshan V, Tao W, Hamaly MA, Alkawareek MY, Dreaden EC, Brown D, Alkilany AM, Farokhzad OC, Mahmoudi M. Cellular uptake of nanoparticles: journey inside the cell. Chem Soc Rev. 2017 Jul 17;46(14):4218-4244. [CrossRef]
- Lavington S, Watts A. Lipid nanoparticle technologies for the study of G protein-coupled receptors in lipid environments. Biophys Rev. 2020 Nov 19;12(6):1287–302. [CrossRef]
- Chatterjee S, Kon E, Sharma P, Peer D. Endosomal escape: A bottleneck for LNP-mediated therapeutics. Proc Natl Acad Sci U S A. 2024 Mar 12;121(11):e2307800120. [CrossRef]
- Sengottiyan S, Mikolajczyk A, Jagiełło K, Swirog M, Puzyn T. Core, coating, or corona? The importance of considering protein coronas in nano-QSPR modeling of zeta potential. ACS Nano. 2023 Feb 14;17(3):1989-1997. [CrossRef]
- Fell VHK, Kramer T, Heindl A, Merkel OM. Prediction of the apparent pKa value of lipid nanoparticles by density functional theory. ACS Mater Au. 2025 Feb 27;5(3):451-457. [CrossRef]
- Johansson JM, Du Rietz H, Hedlund H, Eriksson HC, Oude Blenke E, Pote A, Harun S, Nordenfelt P, Lindfors L, Wittrup A. Cellular and biophysical barriers to lipid nanoparticle mediated delivery of RNA to the cytosol. Nat Commun. 2025 Jul 1;16(1):5354. [CrossRef]
- Ermilova I, Swenson J. Ionizable lipids penetrate phospholipid bilayers with high phase transition temperatures: perspectives from free energy calculations. Chem Phys Lipids. 2023 Jul;253:105294. [CrossRef]
- Er-Rafik M, Ferji K, Combet J, Sandre O, Lecommandoux S, Schmutz M, Le Meins J-F, Marques CM. Tear of lipid membranes by nanoparticles. Soft Matter 2022; 18(17): 3318-3322. [CrossRef]
- Pilkington EH, Suys EJA, Trevaskis NL, Wheatley AK, Zukancic D, Algarni A, Al-Wassiti H, Davis TP, Pouton CW, Kent SJ, Truong NP. From influenza to COVID-19: Lipid nanoparticle mRNA vaccines at the frontiers of infectious diseases. Acta Biomater. 2021 Sep 1;131:16-40. [CrossRef]
- Müller JA, Schäffler N, Kellerer T, Schwake G, Ligon TS, Rädler JO. Kinetics of RNA-LNP delivery and protein expression. Eur J Pharm Biopharm. 2024 Apr;197:114222. [CrossRef]
- Aliakbarinodehi N, Niederkofler S, Emilsson G, Parkkila P, Olsén E, Jing Y, Sjöberg M, Agnarsson B, Lindfors L, Höök F. Time-resolved inspection of ionizable lipid-facilitated lipid nanoparticle disintegration and cargo release at an early endosomal membrane mimic. ACS Nano. 2024 Aug 27;18(34):22989-23000. [CrossRef]
- Schlich M, Palomba R, Costabile G, Mizrahy S, Pannuzzo M, Peer D, Decuzzi P. Cytosolic delivery of nucleic acids: The case of ionizable lipid nanoparticles. Bioeng Transl Med. 2021 Mar 20;6(2):e10213. [CrossRef]
- Sabnis S, Kumarasinghe ES, Salerno T, Mihai C, Ketova T, Senn JJ, Lynn A, Bulychev A, McFadyen I, Chan J, Almarsson Ö, Stanton MG, Benenato KE. A novel amino lipid series for mRNA delivery: Improved endosomal escape and sustained pharmacology and safety in non-human primates. Mol Ther. 2018 Jun 6;26(6):1509-1519. [CrossRef]
- Paramasivam P, Franke C, Stöter M, Höijer A, Bartesaghi S, Sabirsh A, Lindfors L, Arteta MY, Dahlén A, Bak A, Andersson S, Kalaidzidis Y, Bickle M, Zerial M. Endosomal escape of delivered mRNA from endosomal recycling tubules visualized at the nanoscale. J Cell Biol. 2022 Feb 7;221(2):e202110137. [CrossRef]
- Sahay G, Querbes W, Alabi C, Eltoukhy A, Sarkar S, Zurenko C, Karagiannis E, Love K, Chen D, Zoncu R, Buganim Y, Schroeder A, Langer R, Anderson DG. Efficiency of siRNA delivery by lipid nanoparticles is limited by endocytic recycling. Nat Biotechnol. 2013 Jul;31(7):653-8. [CrossRef]
- Bitounis D, Jacquinet E, Rogers MA, Amiji MM. Strategies to reduce the risks of mRNA drug and vaccine toxicity. Nat Rev Drug Discov. 2024 Apr;23(4):281-300. [CrossRef]
- Moghimi SM, Simberg D. Pro-inflammatory concerns with lipid nanoparticles. Mol Ther. 2022 Jun 1;30(6):2109-2110. [CrossRef]
- Bates SM, Munson MJ, Trovisco V, Pereira S, Miller SR, Sabirsh A, Betts CJ, Blenke EO, Gay NJ. The kinetics of endosomal disruption reveal differences in lipid nanoparticle induced cellular toxicity. J Control Release. 2025 Oct 10;386:114047. [CrossRef]
- Su J, Song Y, Zhu Z, Huang X, Fan J, Qiao J, Mao F. Cell-cell communication: new insights and clinical implications. Signal Transduct Target Ther. 2024 Aug 7;9(1):196. [CrossRef]
- Bansal S, Perincheri S, Fleming T, Poulson C, Tiffany B, Bremner RM, Mohanakumar T. Cutting edge: Circulating exosomes with COVID spike protein are induced by BNT162b2 (Pfizer-BioNTech) vaccination prior to development of antibodies: A novel mechanism for immune activation by mRNA vaccines. J Immunol. 2021 Nov 15;207(10):2405-2410. [CrossRef]
- Kammerer USV, Steger K. BioNTech RNA-based COVID-19 injections contain large amounts of residual DNA including an SV40 promoter/enhancer Sequence. Journal of Science, Public Health Policy and the Law 2024; v5.2019-2024.
- Sahin U, Karikó K, Türeci Ö. mRNA-based therapeutics--developing a new class of drugs. Nat Rev Drug Discov. 2014 Oct;13(10):759-80. [CrossRef]
- Jörgensen AM, Wibel R, Bernkop-Schnürch A. Biodegradable cationic and ionizable cationic lipids: A roadmap for safer pharmaceutical excipients. Small. 2023 Apr;19(17):e2206968. [CrossRef]
- Knaggs KLM, Sun Y, Walz BA, Pang J, Khan OF. The role of excipients in lipid nanoparticle metabolism: implications for enhanced therapeutic effect. Ther Deliv. 2025 Jul;16(7):687-700. [CrossRef]
- Packer M, Gyawali D, Yerabolu R, Schariter J, White P. A novel mechanism for the loss of mRNA activity in lipid nanoparticle delivery systems. Nat Commun 2021; 12(1): 6777. [CrossRef]
- Moderna. Moderna Science and Technology Day. 2022. Available online: https://s29.q4cdn.com/435878511/files/doc_presentations/2022/05/Science-Day-2022-Master-Slides-FINAL-(05.17_7am).pdf, 2022 (accessed on 28 February 2023).
- USFDA. Letter to Pfizer: Children’s vaccination, authorization of formulation change. US Food and Drug Administration: https://cacmap.fda.gov/media/150386/download, 2021.
- Maelfait J, Liverpool L, Rehwinkel J. Nucleic acid sensors and programmed cell death. J Mol Biol. 2020 Jan 17;432(2):552-568. [CrossRef]
- Fritz KS, Petersen DR. An overview of the chemistry and biology of reactive aldehydes. Free Radic Biol Med. 2013 Jun;59:85-91. [CrossRef]
- Dalleau S, Baradat M, Guéraud F, Huc L. Cell death and diseases related to oxidative stress: 4-hydroxynonenal (HNE) in the balance. Cell Death Differ. 2013 Dec;20(12):1615-30. [CrossRef]
- Hashiba K, Taguchi M, Sakamoto S, Otsu A, Maeda Y, Ebe H, Okazaki A, Harashima H, Sato Y. Overcoming thermostability challenges in mRNA-lipid nanoparticle systems with piperidine-based ionizable lipids. Commun Biol. 2024 May 10;7(1):556. [CrossRef]
- Wang W, Deng S, Lin J, Ouyang D. Modeling on in vivo disposition and cellular transportation of RNA lipid nanoparticles via quantum mechanics/physiologically-based pharmacokinetic approaches. Acta Pharm Sin B. 2024 Oct;14(10):4591-4607. [CrossRef]
- Yu Z, Li Q, Wang J, Yu Y, Wang Y, Zhou Q, Li P. Reactive oxygen species-related nanoparticle toxicity in the biomedical field. Nanoscale Res Lett. 2020 May 20;15(1):115. [CrossRef]
- Atianand MK, Fitzgerald KA. Molecular basis of DNA recognition in the immune system. J Immunol. 2013 Mar 1;190(5):1911-8. [CrossRef]
- Szebeni J, Simberg D, González-Fernández Á, Barenholz Y, Dobrovolskaia MA. Roadmap and strategy for overcoming infusion reactions to nanomedicines. Nat Nanotechnol. 2018 Dec;13(12):1100-1108. [CrossRef]
- Bakos T, Mészáros T, Kozma GT, Berényi P, Facskó R, Farkas H, Dézsi L, Heirman C, de Koker S, Schiffelers R, Glatter KA, Radovits T, Szénási G, Szebeni J. mRNA-LNP COVID-19 vaccine lipids induce complement activation and production of proinflammatory cytokines: Mechanisms, effects of complement inhibitors, and relevance to adverse reactions. Int J Mol Sci. 2024 Mar 22;25(7):3595. [CrossRef]
- Euopean Medicines Agency. Onpattro: European Public Assessment Report (EPAR) EMA/554262/2018. CHMP, Ed.; Amsterdam, NL, 2018.
- Wang J, Ding Y, Chong K, Cui M, Cao Z, Tang C, Tian Z, Hu Y, Zhao Y, Jiang S. Recent advances in lipid nanoparticles and their safety concerns for mRNA delivery. Vaccines (Basel). 2024 Oct 8;12(10):1148. [CrossRef]
- Zhang L, Ren F, Zhang X, Wang X, Shi H, Zhou L, Zheng S, Chen Y, Chen D, Li L, Zhao C, Duan Z. Peroxisome proliferator-activated receptor alpha acts as a mediator of endoplasmic reticulum stress-induced hepatocyte apoptosis in acute liver failure. Dis Model Mech. 2016 Jul 1;9(7):799-809. [CrossRef]
- Popovics H, Mikone K, Mozes M, Kwon J-Y, Hansmann G, Kokeny G. P0721 PPAR-gamma activation inhibits TGF-beta induced renal complement and galectin-3 expression in vivo and in vitro, Nephrology Dialysis Transplantation 2020; 35(Suppl 3): gfaa142.P0721. [CrossRef]
- Kong Y, Wang N, Tong Z, Wang D, Wang P, Yang Q, Yan X, Song W, Jin Z, Zhang M. Role of complement factor D in cardiovascular and metabolic diseases. Front Immunol. 2024 Oct 2;15:1453030. [CrossRef]
- Dai W, Xing M, Sun L, Lv L, Wang X, Wang Y, Pang X, Guo Y, Ren J, Zhou D Lipid nanoparticles as adjuvant of norovirus VLP vaccine augment cellular and humoral immune responses in a TLR9- and type I IFN-dependent pathway. J virology 2024; 98(12): e0169924. [CrossRef]
- Chaudhary N, Kasiewicz LN, Newby AN, Arral ML, Yerneni SS, Melamed JR, LoPresti ST, Fein KC, Strelkova Petersen DM, Kumar S, Purwar R, Whitehead KA. Amine headgroups in ionizable lipids drive immune responses to lipid nanoparticles by binding to the receptors TLR4 and CD1d. Nat Biomed Eng. 2024 Nov;8(11):1483-1498. [CrossRef]
- Means N, Elechalawar CK, Chen WR, Bhattacharya R, Mukherjee P. Revealing macropinocytosis using nanoparticles. Mol Aspects Med. 2022 Feb;83:100993. [CrossRef]
- Baimanov D, Wang J, Liu Y, Zheng P, Yu S, Liu F, Wang J, Boraschi D, Zhao Y, Chen C, Wang L. Identification of cell receptors responsible for recognition and binding of lipid nanoparticles. Journal of the American Chemical Society 2025; 147(9): 7604-7616. [CrossRef]
- Paunovska K, Da Silva Sanchez AJ, Lokugamage MP, Loughrey D, Echeverri ES, Cristian A, Hatit MZC, Santangelo PJ, Zhao K, Dahlman JE. The extent to which lipid nanoparticles require apolipoprotein E and low-density lipoprotein receptor for delivery changes with ionizable lipid structure. Nano Lett. 2022 Dec 28;22(24):10025-10033. [CrossRef]
- Karikó K, Ni H, Capodici J, Lamphier M, Weissman D. mRNA is an endogenous ligand for Toll-like receptor 3. J Biol Chem. 2004 Mar 26;279(13):12542-50. [CrossRef]
- Karikó K, Muramatsu H, Welsh FA, Ludwig J, Kato H, Akira S, Weissman D. Incorporation of pseudouridine into mRNA yields superior nonimmunogenic vector with increased translational capacity and biological stability. Mol Ther. 2008 Nov;16(11):1833-40. [CrossRef]
- Karikó K, Buckstein M, Ni H, Weissman D. Suppression of RNA recognition by Toll-like receptors: the impact of nucleoside modification and the evolutionary origin of RNA. Immunity. 2005 Aug;23(2):165-75. [CrossRef]
- Monroe J, Eyler DE, Mitchell L, Deb I, Bojanowski A, Srinivas P, Dunham CM, Roy B, Frank AT, Koutmou KS. N1-Methylpseudouridine and pseudouridine modifications modulate mRNA decoding during translation. Nat Commun. 2024 Sep 16;15(1):8119. [CrossRef]
- Przybylski S, Gasch M, Marschner A, Ebert M, Ewe A, Helmig G, Hilger N, Fricke S, Rudzok S, Aigner A, Burkhardt J. Influence of nanoparticle-mediated transfection on proliferation of primary immune cells in vitro and in vivo. PLoS One. 2017 May 2;12(5):e0176517. [CrossRef]
- Guo X, Wang H, Li Y, Leng X, Huang W, Ma Y, Xu T, Qi X. Transfection reagent Lipofectamine triggers type I interferon signaling activation in macrophages. Immunol Cell Biol. 2019 Jan;97(1):92-96. doi: 10.1111/imcb.12194. Epub 2018 Aug 31. Erratum in: Immunol Cell Biol. 2020 Jan;98(1):88. [CrossRef]
- Choe U, Yu L, Wang TTY. Selected lipid-based transfection reagents activate NF-κB and MAP kinases signaling pathways, induced cytokines mRNA expression in human THP-1 macrophage. Anal Biochem. 2019 May 15;573:73-76. [CrossRef]
- Connors J, Joyner D, Mege NJ, Cusimano GM, Bell MR, Marcy J, Taramangalam B, Kim KM, Lin PJC, Tam YK, Weissman D, Kutzler MA, Alameh MG, Haddad EK. Lipid nanoparticles (LNP) induce activation and maturation of antigen presenting cells in young and aged individuals. Commun Biol. 2023 Feb 17;6(1):188. doi: 10.1038/s42003-023-04555-1. Erratum in: Commun Biol. 2025 Feb 22;8(1):285. [CrossRef]
- Korzun T, Moses AS, Jozic A, Grigoriev V, Newton S, Kim J, Diba P, Sattler A, Levasseur PR, Le N, Singh P, Sharma KS, Goo YT, Mamnoon B, Raitmayr C, Mesquita Souza AP, Taratula OR, Sahay G, Taratula O, Marks DL. Lipid nanoparticles elicit reactogenicity and sickness behavior in mice via toll-like receptor 4 and myeloid differentiation protein 88 axis. ACS Nano. 2024 Sep 10;18(36):24842-24859. [CrossRef]
- Kawai T, Akira S. Toll-like receptors and their crosstalk with other innate receptors in infection and immunity. Immunity. 2011 May 27;34(5):637-50. [CrossRef]
- Ding X, Jin S, Tong Y, Jiang X, Chen Z, Mei S, Zhang L, Billiar TR, Li Q. TLR4 signaling induces TLR3 up-regulation in alveolar macrophages during acute lung injury. Sci Rep 2017; 7: 34278. [CrossRef]
- Nouri-Shirazi M, Tamjidi S, Nourishirazi E, Guinet E. Combination of TLR8 and TLR4 agonists reduces the degrading effects of nicotine on DC-NK mediated effector T cell generation. Int Immunopharmacol. 2018 Aug;61:54-63. [CrossRef]
- Kim HJ, Kim H, Lee JH, Hwangbo C. Toll-like receptor 4 (TLR4): new insight immune and aging. Immun Ageing. 2023 Nov 24;20(1):67. [CrossRef]
- Alhamdan F, Bayarsaikhan G, Yuki K. Toll-like receptors and integrins crosstalk. Front Immunol. 2024 Jun 10;15:1403764. [CrossRef]
- Ghosh TK, Mickelson DJ, Solberg JC, Lipson KE, Inglefield JR, Alkan SS. TLR-TLR cross talk in human PBMC resulting in synergistic and antagonistic regulation of type-1 and 2 interferons, IL-12 and TNF-alpha. Int Immunopharmacol. 2007 Aug;7(8):1111-21. [CrossRef]
- Xu XH, Shah PK, Faure E, Equils O, Thomas L, Fishbein MC, Luthringer D, Xu XP, Rajavashisth TB, Yano J, Kaul S, Arditi M. Toll-like receptor-4 is expressed by macrophages in murine and human lipid-rich atherosclerotic plaques and upregulated by oxidized LDL. Circulation. 2001 Dec 18;104(25):3103-8. [CrossRef]
- Hovland A, Jonasson L, Garred P, Yndestad A, Aukrust P, Lappegård KT, Espevik T, Mollnes TE. The complement system and toll-like receptors as integrated players in the pathophysiology of atherosclerosis. Atherosclerosis. 2015 Aug;241(2):480-94. [CrossRef]
- Luo L, Wall AA, Tong SJ, Hung Y, Xiao Z, Tarique AA, Sly PD, Fantino E, Marzolo MP, Stow JL. TLR crosstalk activates LRP1 to recruit Rab8a and PI3Kγ for suppression of inflammatory responses. Cell Rep. 2018 Sep 11;24(11):3033-3044. [CrossRef]
- Köberlin MS, Heinz LX, Superti-Furga G. Functional crosstalk between membrane lipids and TLR biology. Curr Opin Cell Biol. 2016 Apr;39:28-36. [CrossRef]
- Kornilov FD, Shabalkina AV, Lin C, Volynsky PE, Kot EF, Kayushin AL, Lushpa VA, Goncharuk MV, Arseniev AS, Goncharuk SA, Wang X, Mineev KS. The architecture of transmembrane and cytoplasmic juxtamembrane regions of Toll-like receptors. Nat Commun. 2023 Mar 17;14(1):1503. [CrossRef]
- Ndeupen S, Qin Z, Jacobsen S, Bouteau A, Estanbouli H, Igyártó BZ. The mRNA-LNP platform's lipid nanoparticle component used in preclinical vaccine studies is highly inflammatory. iScience. 2021 Dec 17;24(12):103479. [CrossRef]
- Finney, DJ. The median lethal dose and its estimation. Arch Toxicol. 1985 Feb;56(4):215-8. [CrossRef]
- Avila AM, Bebenek I, Bonzo JA, Bourcier T, Davis Bruno KL, Carlson DB, Dubinion J, Elayan I, Harrouk W, Lee SL, Mendrick DL, Merrill JC, Peretz J, Place E, Saulnier M, Wange RL, Yao J, Zhao D, Brown PC. An FDA/CDER perspective on nonclinical testing strategies: Classical toxicology approaches and new approach methodologies (NAMs). Regul Toxicol Pharmacol. 2020 Jul;114:104662. [CrossRef]
- Li, GM. Mechanisms and functions of DNA mismatch repair. Cell Res. 2008 Jan;18(1):85-98. [CrossRef]
- Molnár T., Mázló A., Tslaf V., Szöllősi A.G., Emri G., Koncz G. Current translational potential and underlying molecular mechanisms of necroptosis. Cell Death Dis. 2019;10. [CrossRef]
- Park BK, Pirmohamed M, Kitteringham NR. The role of cytochrome P450 enzymes in hepatic and extrahepatic human drug toxicity. Pharmacol Ther. 1995;68(3):385-424. [CrossRef]
- Guo Q, Jin Y, Chen X, Ye X, Shen X, Lin M, Zeng C, Zhou T, Zhang J. NF-κB in biology and targeted therapy: new insights and translational implications. Signal Transduct Target Ther. 2024 Mar 4;9(1):53. [CrossRef]
- Parameswaran N, Patial S. Tumor necrosis factor-α signaling in macrophages. Crit Rev Eukaryot Gene Expr. 2010;20(2):87-103. [CrossRef]
- Mills KHG. IL-17 and IL-17-producing cells in protection versus pathology. Nat Rev Immunol. 2023 Jan;23(1):38-54. [CrossRef]
- Wicherska-Pawłowska K, Wróbel T, Rybka J. Toll-like receptors (TLRs), NOD-like receptors (NLRs), and RIG-I-like receptors (RLRs) in innate immunity. TLRs, NLRs, and RLRs ligands as immunotherapeutic agents for hematopoietic diseases. Int J Mol Sci. 2021 Dec 13;22(24):13397. [CrossRef]
- Mohan GS, Kumar R. Impairment of tricarboxylic acid cycle (TCA) cycle in Alzheimer's disease: Mechanisms, implications, and potential therapies. Aging Dis. 2025 May 29;16(5):2553-2574. [CrossRef]
- Lee, Y. Roles of circadian clocks in cancer pathogenesis and treatment. Exp Mol Med 2021; 53: 1529–1538. [CrossRef]
- Dunn WG, McLoughlin MA, Vassiliou GS. Clonal hematopoiesis and hematological malignancy. J Clin Invest. 2024 Oct 1;134(19):e180065. [CrossRef]
- Zheng Y, Sun L, Jiang T, Zhang D, He D, Nie H. TNFα promotes Th17 cell differentiation through IL-6 and IL-1β produced by monocytes in rheumatoid arthritis. J Immunol Res. 2014;2014:385352. [CrossRef]
- Marasco MR, Conteh AM, Reissaus CA, Cupit JE 5th, Appleman EM, Mirmira RG, Linnemann AK. Interleukin-6 reduces β-cell oxidative stress by linking autophagy with the antioxidant response. Diabetes. 2018 Aug;67(8):1576-1588. [CrossRef]
- Deretic V, Saitoh T, Akira S. Autophagy in infection, inflammation and immunity. Nat Rev Immunol. 2013 Oct;13(10):722-37. [CrossRef]
- Chi DS, Fitzgerald SM, Pitts S, Cantor K, King E, Lee SA, Huang SK, Krishnaswamy G. MAPK-dependent regulation of IL-1- and beta-adrenoreceptor-induced inflammatory cytokine production from mast cells: implications for the stress response. BMC Immunol. 2004 Sep 21;5:22. [CrossRef]
- Yang HT, Cohen P, Rousseau S. IL-1beta-stimulated activation of ERK1/2 and p38alpha MAPK mediates the transcriptional up-regulation of IL-6, IL-8 and GRO-alpha in HeLa cells. Cell Signal. 2008 Feb;20(2):375-80. [CrossRef]
- Tengesdal IW, Dinarello A, Powers NE, Burchill MA, Joosten LAB, Marchetti C, Dinarello CA. Tumor NLRP3-derived IL-1β drives the IL-6/STAT3 axis resulting in sustained MDSC-mediated immunosuppression. Front Immunol. 2021 Aug 31;12:661323. [CrossRef]
- Li H, Wu M, Zhao X. Role of chemokine systems in cancer and inflammatory diseases. MedComm (2020). 2022 Jun 8;3(2):e147. [CrossRef]
- Unver, N. Macrophage chemoattractants secreted by cancer cells: Sculptors of the tumor microenvironment and another crucial piece of the cancer secretome as a therapeutic target. Cytokine Growth Factor Rev. 2019 Dec;50:13-18. [CrossRef]
- Nakatsumi H, Matsumoto M, Nakayama KI. Noncanonical pathway for regulation of CCL2 expression by an mTORC1-FOXK1 axis promotes recruitment of tumor-associated macrophages. Cell Rep. 2017 Nov 28;21(9):2471-2486. [CrossRef]
- Huda N, Khambu B, Liu G, Nakatsumi H, Yan S, Chen X, Ma M, Dong Z, Nakayama KI, Yin XM. Senescence connects autophagy deficiency to inflammation and tumor progression in the liver. Cell Mol Gastroenterol Hepatol. 2022;14(2):333-355. [CrossRef]
- Forster III J, Nandi D, Kulkarni A. mRNA-carrying lipid nanoparticles that induce lysosomal rupture activate NLRP3 inflammasome and reduce mRNA transfection efficiency. Biomater Sci. 2022 Sep 27;10(19):5566-5582. [CrossRef]
- Shin JN, Rao L, Sha Y, Abdel Fattah E, Hyser J, Eissa NT. p38 MAPK activity is required to prevent hyperactivation of NLRP3 inflammasome. J Immunol. 2021 Jul 15;207(2):661-670. [CrossRef]
- Lv JM, Gao YL, Wang LY, Li BD, Shan YL, Wu ZQ, Lu QM, Peng HY, Zhou TT, Li XM, Zhang LM. Inhibition of the P38 MAPK/NLRP3 pathway mitigates cognitive dysfunction and mood alterations in aged mice after abdominal surgery plus sevoflurane. Brain Res Bull. 2024 Oct 15;217:111059. [CrossRef]
- Sozio MS, Lu C, Zeng Y, Liangpunsakul S, Crabb DW. Activated AMPK inhibits PPAR-α and PPAR-γ transcriptional activity in hepatoma cells. Am J Physiol Gastrointest Liver Physiol. 2011 Oct;301(4):G739-47. [CrossRef]
- Sun H, Zhu X, Lin W, Zhou Y, Cai W, Qiu L. Interactions of TLR4 and PPARγ, dependent on AMPK signalling pathway contribute to anti-inflammatory effects of vaccariae hypaphorine in endothelial cells. Cell Physiol Biochem. 2017;42(3):1227-1239. [CrossRef]
- Harada K, Isse K, Kamihira T, Shimoda S, Nakanuma Y. Th1 cytokine-induced downregulation of PPARγ in human biliary cells relates to cholangitis in primary biliary cirrhosis. Hepatology. 2005 Jun;41(6):1329-38. [CrossRef]
- Yin R, Dong YG, Li HL. PPARγ phosphorylation mediated by JNK MAPK: a potential role in macrophage-derived foam cell formation. Acta Pharmacol Sin. 2006 Sep;27(9):1146-52. [CrossRef]
- Su AC, Zhang LY, Zhang JG, Hu YY, Liu XY, Li SC, Xian XH, Li WB, Zhang M. The regulation of autophagy by p38 MAPK-PPARγ signaling during the brain ischemic tolerance induced by cerebral ischemic preconditioning. DNA Cell Biol. 2022 Sep;41(9):838-849. [CrossRef]
- Ballav S, Biswas B, Sahu VK, Ranjan A, Basu S. PPARγ partial agonists in disease-fate decision with special reference to cancer. Cells. 2022 Oct 13;11(20):3215. [CrossRef]
- Zhao M, Ma J, Li M, Zhang Y, Jiang B, Zhao X, Huai C, Shen L, Zhang N, He L, Qin S. Cytochrome P450 enzymes and drug metabolism in humans. Int J Mol Sci. 2021 Nov 26;22(23):12808. [CrossRef]
- Liu F, Aulin LBS, Manson ML, Krekels EHJ, van Hasselt JGC. Unraveling the effects of acute inflammation on pharmacokinetics: A model-based analysis focusing on renal glomerular filtration rate and cytochrome P450 3A4-mediated metabolism. Eur J Drug Metab Pharmacokinet. 2023 Nov;48(6):623-631. [CrossRef]
- Stanke-Labesque F, Gautier-Veyret E, Chhun S, Guilhaumou R; French Society of Pharmacology and Therapeutics. Inflammation is a major regulator of drug metabolizing enzymes and transporters: Consequences for the personalization of drug treatment. Pharmacol Ther. 2020 Nov;215:107627. [CrossRef]
- Bayraktar İ, Yalçın N, Demirkan K. The potential interaction between COVID-19 vaccines and clozapine: A novel approach for clinical trials. Int J Clin Pract. 2021 Aug;75(8):e14441. [CrossRef]
- Imai T, Ochiai S, Ishimaru T, Daitoku H, Miyagawa Y, Fukuhara R, Boku S, Takebayashi M. A case report: Clozapine-induced leukopenia and neutropenia after mRNA COVID-19 vaccination. Neuropsychopharmacol Rep. 2022 Jun;42(2):238-240. [CrossRef]
- Thompson D, Delorme CM, White RF, Honer WG. Elevated clozapine levels and toxic effects after SARS-CoV-2 vaccination. J Psychiatry Neurosci. 2021 Mar 5;46(2):E210-E211. [CrossRef]
- Eiermann B, Engel G, Johansson I, Zanger UM, Bertilsson L. The involvement of CYP1A2 and CYP3A4 in the metabolism of clozapine. Br J Clin Pharmacol. 1997 Nov;44(5):439-46. [CrossRef]
- Villemure S, Trenaman SC, Goralski KB. The impact of COVID-19 infection on cytochrome P450 3A4-mediated drug metabolism and drug interactions. Expert Opin Drug Metab Toxicol. 2023 Jan-Jun;19(6):329-332. [CrossRef]
- Lim SYM, Al Bishtawi B, Lim W. Role of cytochrome P450 2C9 in COVID-19 treatment: Current status and future directions. Eur J Drug Metab Pharmacokinet. 2023 May;48(3):221-240. [CrossRef]
- Szychowski KA, Skóra B, Wójtowicz AK. Engagement of peroxisome proliferator-activated receptor γ (PPARγ) and mammalian target of rapamycin (mTOR) in the triclosan-induced disruption of Cyp450 enzyme activity in an in vitro model of mouse embryo fibroblasts (3T3-L1). Toxicology. 2025 Feb;511:154031. [CrossRef]
- Hossam Abdelmonem B, Abdelaal NM, Anwer EKE, Rashwan AA, Hussein MA, Ahmed YF, Khashana R, Hanna MM, Abdelnaser A. Decoding the role of CYP450 enzymes in metabolism and disease: A comprehensive review. Biomedicines. 2024 Jul 2;12(7):1467. [CrossRef]
- Koozi H, Lengquist M, Frigyesi A. C-reactive protein as a prognostic factor in intensive care admissions for sepsis: A Swedish multicenter study. J Crit Care. 2020 Apr;56:73-79. [CrossRef]
- Lenoir C, Rollason V, Desmeules JA, Samer CF. Influence of inflammation on cytochromes P450 activity in adults: A systematic review of the literature. Front Pharmacol. 2021 Nov 16;12:733935. [CrossRef]
- Yang M, Lu Y, Piao W, Jin H. The Translational Regulation in mTOR Pathway. Biomolecules. 2022 Jun 8;12(6):802. [CrossRef]
- Shveygert M, Kaiser C, Bradrick SS, Gromeier M. Regulation of eukaryotic initiation factor 4E (eIF4E) phosphorylation by mitogen-activated protein kinase occurs through modulation of Mnk1-eIF4G interaction. Mol Cell Biol. 2010 Nov;30(21):5160-7. [CrossRef]
- Lin Y, Bian L, Zhu G, Zhang B. Vitronectin promotes proliferation and metastasis of cervical cancer cells via the epithelial-mesenchymal transition. Front Oncol. 2024 Dec 9;14:1466264. [CrossRef]
- Gao P, Lu Y, Tang K, Wang W, Wang T, Zhu Y, Zhao J, Mao Y. Ficolin-1 ameliorates pulmonary fibrosis via directly binding to TGF-β1. J Transl Med. 2024 Nov 21;22(1):1051. [CrossRef]
- Knabl L, Lee HK, Wieser M, Mur A, Zabernigg A, Knabl L Sr, Rauch S, Bock M, Schumacher J, Kaiser N, Furth PA, Hennighausen L. BNT162b2 vaccination enhances interferon-JAK-STAT-regulated antiviral programs in COVID-19 patients infected with the SARS-CoV-2 Beta variant. Commun Med (Lond). 2022;2(1):17. [CrossRef]
- Burotto M, Chiou VL, Lee JM, Kohn EC. The MAPK pathway across different malignancies: a new perspective. Cancer. 2014 Nov 15;120(22):3446-56. [CrossRef]
- Panwar V, Singh A, Bhatt M, Tonk RK, Azizov S, Raza AS, Sengupta S, Kumar D, Garg M. Multifaceted role of mTOR (mammalian target of rapamycin) signaling pathway in human health and disease. Signal Transduct Target Ther. 2023 Oct 2;8(1):375. [CrossRef]
- Yu H, Lin L, Zhang Z, Zhang H, Hu H. Targeting NF-κB pathway for the therapy of diseases: mechanism and clinical study. Signal Transduct Target Ther. 2020 Sep 21;5(1):209. [CrossRef]
- McCubrey JA, Steelman LS, Chappell WH, Abrams SL, Montalto G, Cervello M, Nicoletti F, Fagone P, Malaponte G, Mazzarino MC, Candido S, Libra M, Bäsecke J, Mijatovic S, Maksimovic-Ivanic D, Milella M, Tafuri A, Cocco L, Evangelisti C, Chiarini F, Martelli AM. Mutations and deregulation of Ras/Raf/MEK/ERK and PI3K/PTEN/Akt/mTOR cascades which alter therapy response. Oncotarget. 2012 Sep;3(9):954-87. [CrossRef]
- Nigam M, Punia B, Dimri DB, Mishra AP, Radu AF, Bungau G. Reactive oxygen species: A double-edged sword in the modulation of cancer signaling pathway dynamics. Cells. 2025 Aug 6;14(15):1207. [CrossRef]
- Cui D, Qu R, Liu D, Xiong X, Liang T, Zhao Y. The cross talk between p53 and mTOR pathways in response to physiological and genotoxic stresses. Front Cell Dev Biol. 2021 Nov 18;9:775507. [CrossRef]
- Bassermann F, Eichner R, Pagano M. The ubiquitin proteasome system - implications for cell cycle control and the targeted treatment of cancer. Biochim Biophys Acta. 2014 Jan;1843(1):150-62. [CrossRef]
- Chen Y, Gong W, Dai W, Jiang H, Xu X. E2F1/2/4 mRNA is associated with immune infiltration and are potential biomarkers for the prognosis of human gastric carcinoma. Transl Cancer Res. 2021 Jun;10(6):2801-2811. [CrossRef]
- Daigh LH, Saha D, Rosenthal DL, Ferrick KR, Meyer T. Uncoupling of mTORC1 from E2F activity maintains DNA damage and senescence. Nat Commun 2024; 15: 9181. [CrossRef]
- Zhang Y, Hao X, Han G, Lu Y, Chen Z, Zhang L, Wu J, Wang X. E2F1-mediated GINS2 transcriptional activation promotes tumor progression through PI3K/AKT/mTOR pathway in hepatocellular carcinoma. Am J Cancer Res. 2022 Apr 15;12(4):1707-1726.
- Calzone L, Gelay A, Zinovyev A, Radvanyi F, Barillot E. A comprehensive modular map of molecular interactions in RB/E2F pathway. Mol Syst Biol. 2008;4:173. [CrossRef]
- Bertonnier-Brouty L, Andersson J, Kaprio T, Hagström J, Bsharat S, Asplund O, Hatem G, Haglund C, Seppänen H, Prasad RB, Artner I. E2F transcription factors promote tumorigenicity in pancreatic ductal adenocarcinoma. Cancer Med. 2024 May;13(9):e7187. [CrossRef]
- Wasserman D, Nachum S, Cohen M, Enrico TP, Noach-Hirsh M, Parasol J, Zomer-Polak S, Auerbach N, Sheinberger-Chorni E, Nevenzal H, Levi-Dadon N, Wang X, Lahmi R, Michaely E, Gerber D, Emanuele MJ, Tzur A. Cell cycle oscillators underlying orderly proteolysis of E2F8. Mol Biol Cell. 2020 Apr 1;31(8):725-740. [CrossRef]
- Timmers C, Sharma N, Opavsky R, Maiti B, Wu L, Wu J, Orringer D, Trikha P, Saavedra HI, Leone G. E2f1, E2f2, and E2f3 control E2F target expression and cellular proliferation via a p53-dependent negative feedback loop. Mol Cell Biol. 2007 Jan;27(1):65-78. doi: 10.1128/MCB.02147-05. Erratum in: Mol Cell Biol. 2012 May;32(9):1758.
- Spitschak A, Dhar P, Singh KP, Casalegno Garduño R, Gupta SK, Vera J, Musella L, Murr N, Stoll A, Pützer BM. E2F1-induced autocrine IL-6 inflammatory loop mediates cancer-immune crosstalk that predicts T cell phenotype switching and therapeutic responsiveness. Front Immunol. 2024 Oct 31;15:1470368. [CrossRef]
- Li J, Ran C, Li E, Gordon F, Comstock G, Siddiqui H, Cleghorn W, Chen HZ, Kornacker K, Liu CG, Pandit SK, Khanizadeh M, Weinstein M, Leone G, de Bruin A. Synergistic function of E2F7 and E2F8 is essential for cell survival and embryonic development. Dev Cell. 2008 Jan;14(1):62-75. [CrossRef]
- Zheng J, Huang J, Xia J, Zhou W, Dai L, Lin S, Gao L, Zou C. Transcription factor E2F8 is a therapeutic target in the basal-like subtype of breast cancer. Front Oncol. 2023 Feb 6;13:1038787. [CrossRef]
- Vigo E, Müller H, Prosperini E, Hateboer G, Cartwright P, Moroni MC, Helin K. CDC25A phosphatase is a target of E2F and is required for efficient E2F-induced S phase. Mol Cell Biol. 1999 Sep;19(9):6379-95. [CrossRef]
- Delgado M, Washam CL, Urbaniak A, Heflin B, Storey AJ, Lan RS, Mackintosh SG, Tackett AJ, Byrum SD, Chambers TC. Phosphoproteomics provides novel insights into the response of primary acute lymphoblastic leukemia cells to microtubule depolymerization in G1 phase of the cell cycle. ACS Omega. 2021 Sep 16;6(38):24949-24959. [CrossRef]
- Knapp JD, Bhargava A. BNT162b2 mRNA vaccine-induced sex differences in the single-cell transcriptome of peripheral blood mononuclear cells in healthy adults bioRxiv Preprint. Oct 3, 2023. [CrossRef]
- Ezine E, Lebbe C, Dumaz N. Unmasking the tumourigenic role of SIN1/MAPKAP1 in the mTOR complex 2. Clin Transl Med. 2023 Oct;13(10):e1464. [CrossRef]
- Hickey TE, Mudunuri U, Hempel HA, Kemp TJ, Roche NV, Talsania K, Sellers BA, Cherry JM, Pinto LA. Proteomic and serologic assessments of responses to mRNA-1273 and BNT162b2 vaccines in human recipient sera. Front Immunol. 2025 Jan 27;15:1502458. [CrossRef]
- Savelsbergh A, Mohr D, Wilden B, Wintermeyer W, Rodnina MV. Stimulation of the GTPase activity of translation elongation factor G by ribosomal protein L7/12. J Biol Chem. 2000 Jan 14;275(2):890-4. [CrossRef]
- Chang EC, Philips MR. Spatial segregation of Ras signaling: New evidence from fission yeast. Cell Cycle. 2006 Sep;5(17):1936-9. [CrossRef]
- Fadhal, E. The significance of key proteins in the RAS signaling pathway: Implications for cancer and therapeutic targets. OBM Genetics 2024; 8(2): 236. [CrossRef]
- Lin Y, Parajón E, Yuan Q, Ye S, Qin G, Deng Y, Borleis J, Koyfman A, Iglesias PA, Konstantopoulos K, Robinson DN, Devreotes PN. Ras-mediated dynamic and biphasic regulation of cell migration. Proc Natl Acad Sci U S A. 2025 Jul 29;122(30):e2503847122. [CrossRef]
- Chippalkatti R, Parisi B, Kouzi F, Laurini C, Ben Fredj N, Abankwa DK. RAS isoform specific activities are disrupted by disease associated mutations during cell differentiation. Eur J Cell Biol. 2024 Jun;103(2):151425. [CrossRef]
- Wang YF, Dong ZK, Jin WL. Hijacking homeostasis: the brain-body neural circuitry in tumor pathogenesis and emerging therapeutic frontiers. Mol Cancer. 2025 Jul 25;24(1):206. [CrossRef]
- Peng Q, Li X, Fang C, Zhu C, Wang T, Yin B, Dong X, Guo H, Liu Y, Zhang K. Disrupting calcium homeostasis and glycometabolism in engineered lipid-based pharmaceuticals propel cancer immunogenic death. Acta Pharm Sin B. 2025 Mar;15(3):1255-1267. [CrossRef]
- Gulluni F, Martini M, Hirsch E. Cytokinetic Abscission: Phosphoinositides and ESCRTs direct the final cut. J Cell Biochem. 2017 Nov;118(11):3561-3568. doi: 10.1002/jcb.26066. Erratum in: J Cell Biochem. 2024 Aug;125(8):e30626. [CrossRef]
- Tan X, Thapa N, Choi S, Anderson RA. Emerging roles of PtdIns(4,5)P2--beyond the plasma membrane. J Cell Sci. 2015 Nov 15;128(22):4047-56. [CrossRef]
- Ajazi A, Bruhn C, Shubassi G, Lucca C, Ferrari E, Cattaneo A, Bachi A, Manfrini N, Biffo S, Martini E, Minucci S, Vernieri C, Foiani M. Endosomal trafficking and DNA damage checkpoint kinases dictate survival to replication stress by regulating amino acid uptake and protein synthesis. Dev Cell. 2021 Sep 27;56(18):2607-2622.e6. [CrossRef]
- Hurley JH, Coyne AN, Miączyńska M, Stenmark H. The expanding repertoire of ESCRT functions in cell biology and disease. Nature 2025; 642: 877–888. [CrossRef]
- Zhu L, Jorgensen JR, Li M, Chuang YS, Emr SD. ESCRTs function directly on the lysosome membrane to downregulate ubiquitinated lysosomal membrane proteins. Elife. 2017 Jun 29;6:e26403. [CrossRef]
- Jia S, Yang Y, Liu J, Wang Z, Bai L. PPARγ controls ESCRT-dependent fibroblast-like synoviocyte exosome biogenesis and alleviates chondrocyte osteoarthritis mediated by exosomal ANXA1. J Orthop Translat. 2025 Jun 27;53:187-205. [CrossRef]
- Simonsen, JB. A perspective on bleb and empty LNP structures. J Control Release. 2024 Sep;373:952-961. [CrossRef]
- Schoenmaker L, Witzigmann D, Kulkarni JA, Verbeke R, Kersten G, Jiskoot W, Crommelin DJA. mRNA-lipid nanoparticle COVID-19 vaccines: Structure and stability. Int J Pharm. 2021 May 15;601:120586. [CrossRef]
- Liao S, Wang S, Wadhwa A, Birkenshaw A, Fox K, Cheng MHY, Casmil IC, Magana AA, Bathula NV, Ho CH, Cheng JY, Foster LJ, Harder KW, Ross CJD, Cullis PR, Blakney AK. Transfection potency of lipid nanoparticles containing mRNA depends on relative loading levels. ACS Appl Mater Interfaces. 2025 Jan 15;17(2):3097-3105. [CrossRef]
- Lonez C, Vandenbranden M, Ruysschaert JM. Cationic liposomal lipids: from gene carriers to cell signaling. Prog Lipid Res. 2008 Sep;47(5):340-7. [CrossRef]
- Lonez C, Vandenbranden M, Ruysschaert JM. Cationic lipids activate intracellular signaling pathways. Adv Drug Deliv Rev. 2012 Dec;64(15):1749-58. [CrossRef]
- Qin Z, Bouteau A, Herbst C, Igyártó BZ. Pre-exposure to mRNA-LNP inhibits adaptive immune responses and alters innate immune fitness in an inheritable fashion. PLoS Pathog. 2022 Sep 2;18(9):e1010830. [CrossRef]
- Sellegounder D, Ferrucci L, Anbazhagan R, Basisty N. Editorial: Molecular crosstalk between endocrine factors, paracrine signals, and the immune system during aging. Front Endocrinol (Lausanne). 2023 Apr 21;14:1203755. [CrossRef]
- Panariti A, Miserocchi G, Rivolta I. The effect of nanoparticle uptake on cellular behavior: disrupting or enabling functions? Nanotechnol Sci Appl. 2012 Sep 7;5:87-100. [CrossRef]
- Voigt J, Christensen J, Shastri VP. Differential uptake of nanoparticles by endothelial cells through polyelectrolytes with affinity for caveolae. Proc Natl Acad Sci U S A. 2014 Feb 25;111(8):2942-7. [CrossRef]
- Wang T, Bai J, Jiang X, Nienhaus GU. Cellular uptake of nanoparticles by membrane penetration: a study combining confocal microscopy with FTIR spectroelectrochemistry. ACS Nano. 2012 Feb 28;6(2):1251-9. [CrossRef]
- Gerelli, Y. Chapter Three: Exploring interactions between lipid membranes and nanoparticles through neutron and X-ray reflectometry techniques. In A. Iglič, M. Rappolt, & P. Losada-Pérez (Eds.), Advances in Biomembranes and Lipid Self-Assembly 2023; 38: 37–61. Academic Press. [CrossRef]
- Lavagna E, Barnoud J, Rossi G, Monticelli L. Size-dependent aggregation of hydrophobic nanoparticles in lipid membranes. Nanoscale 2020; 12: 9452–9461. [CrossRef]
- Cooper, GM. The Cell: A Molecular Approach. 2nd edition. Sunderland (MA): Sinauer Associates; 2000.
- Hammond GRV, Burke JE. Novel roles of phosphoinositides in signaling, lipid transport, and disease. Curr Opin Cell Biol. 2020 Apr;63:57-67. [CrossRef]
- Skotland T, Sandvig K. The role of PS 18:0/18:1 in membrane function. Nat Commun. 2019 Jun 21;10(1):2752. [CrossRef]
- Heimburg, T. The excitable fluid mosaic. Biochim Biophys Acta Biomembr. 2023 Mar;1865(3):184104. [CrossRef]
- Lupyan D, Mezei M, Logothetis DE, Osman R. A molecular dynamics investigation of lipid bilayer perturbation by PIP2. Biophys J. 2010 Jan 20;98(2):240-7. [CrossRef]
- Pike, LJ. Lipid rafts: bringing order to chaos. J Lipid Res. 2003 Apr;44(4):655-67. [CrossRef]
- Levin R, Grinstein S, Schlam D. Phosphoinositides in phagocytosis and macropinocytosis. Biochim Biophys Acta. 2015 Jun;1851(6):805-23. [CrossRef]
- Weiner OD, Neilsen PO, Prestwich GD, Kirschner MW, Cantley LC, Bourne HR. A PtdInsP(3)- and Rho GTPase-mediated positive feedback loop regulates neutrophil polarity. Nat Cell Biol. 2002 Jul;4(7):509-13. [CrossRef]
- Guan K, Curtis ER, Lew DJ, Elston TC. Particle-based simulations reveal two positive feedback loops allow relocation and stabilization of the polarity site during yeast mating. PLoS Comput Biol. 2023 Oct 2;19(10):e1011523. [CrossRef]
- Fallahi-Sichani M, Linderman JJ. Lipid raft-mediated regulation of G-protein coupled receptor signaling by ligands which influence receptor dimerization: a computational study. PLoS One. 2009 Aug 11;4(8):e6604. [CrossRef]
- Wang X, Shi X, Wang R. Regulating mRNA endosomal escape through lipid rafts: A review. Int J Pharm. 2025 Apr 30;675:125571. [CrossRef]
- Posor Y, Jang W, Haucke V. Phosphoinositides as membrane organizers. Nat Rev Mol Cell Biol. 2022 Dec;23(12):797-816. [CrossRef]
- van Meer G, Voelker DR, Feigenson GW. Membrane lipids: where they are and how they behave. Nat Rev Mol Cell Biol. 2008 Feb;9(2):112-24. [CrossRef]
- Lolicato F, Nickel W, Haucke V, Ebner M. Phosphoinositide switches in cell physiology - From molecular mechanisms to disease. J Biol Chem. 2024 Mar;300(3):105757. [CrossRef]
- Balla, T. Phosphoinositides: tiny lipids with giant impact on cell regulation. Physiol Rev. 2013 Jul;93(3):1019-137. [CrossRef]
- Eramo MJ, Mitchell CA. Regulation of PtdIns(3,4,5)P3/Akt signalling by inositol polyphosphate 5-phosphatases. Biochem Soc Trans. 2016 Feb;44(1):240-52. [CrossRef]
- Xu S, Cao B, Xuan G, Xu S, An Z, Zhu C, Li L, Tang C. Function and regulation of Rab GTPases in cancers. Cell Biol Toxicol. 2024 May 2;40(1):28. [CrossRef]
- Koike S, Jahn R. Rab GTPases and phosphoinositides fine-tune SNAREs dependent targeting specificity of intracellular vesicle traffic. Nat Commun. 2024 Mar 20;15(1):2508. [CrossRef]
- Nishimura T, Gecht M, Covino R, Hummer G, Surma MA, Klose C, Arai H, Kono N, Stefan CJ. Osh proteins control nanoscale lipid organization necessary for PI(4,5)P2 synthesis. Mol Cell. 2019 Sep 5;75(5):1043-1057.e8. [CrossRef]
- Heckle LA, Kozminski KG. Osh-dependent and -independent regulation of PI4P levels during polarized growth of Saccharomyces cerevisiae. Molecular Biology of the Cell Sep 2023; 34(11). [Epub ahead of print].
- Raychaudhuri S, Prinz WA. The diverse functions of oxysterol-binding proteins. Annu Rev Cell Dev Biol. 2010;26:157-77. [CrossRef]
- Omo-Lamai S, Wang Y, Patel MN, Essien E-O, Shen M, Majumdar A, Espy C, Wu J, Channer B, Tobin M, Murali S, Papp TE, Maheshwari R, Wang L, Chase LS, Zamora ME, Arral ML, Marcos-Contreras OA, Myerson JW, Hunter CA, Tsourkas A, Muzykantov V, Brodsky I, Shin S, Whitehead KA, Gaskill P, Discher D, Parhiz H, Brenner JS. Lipid nanoparticle-associated inflammation is triggered by sensing of endosomal damage: Engineering endosomal escape without side effects. bioRxiv preprint. April 18, 2024. [CrossRef]
- Cheng Y, Zhao E, Yang X, Luo C, Zi G, Wang R, Xu Y, Peng B. Entrapment of lipid nanoparticles in peripheral endosomes but not lysosomes impairs intracellular trafficking and endosomal escape. Int J Pharm. 2025 Jan 25;669:125024. [CrossRef]
- Puranik A, Lenehan PJ, Silvert E, Niesen MJM, Corchado-Garcia J, O'Horo JC, Virk A, Swift MD, Gordon JE, Speicher LL, Geyer HL, Kremers W, Halamka J, Badley AD, Venkatakrishnan AJ, Soundararajan V. Comparative effectiveness of mRNA-1273 and BNT162b2 against symptomatic SARS-CoV-2 infection. Med. 2022 Jan 14;3(1):28-41.e8. [CrossRef]
- Granados-Riveron JT, Aquino-Jarquin G. Engineering of the current nucleoside-modified mRNA-LNP vaccines against SARS-CoV-2. Biomed Pharmacother. 2021 Oct;142:111953. [CrossRef]
- Harvey RD, Ara N, Heenan RK, Barlow DJ, Quinn PJ, Lawrence MJ. Stabilization of distearoylphosphatidylcholine lamellar phases in propylene glycol using cholesterol. Mol Pharm. 2013 Dec 2;10(12):4408-17. Epub 2013 Nov 19. [CrossRef]
- Skotland T, Kavaliauskiene S, Sandvig K. The role of lipid species in membranes and cancer-related changes. Cancer Metastasis Rev. 2020 Jun;39(2):343-360. [CrossRef]
- Li J, Wang X, Zhang T, Wang C, Huang Z, Luo X, Deng Y. A review on phospholipids and their main applications in drug delivery systems. Asian Journal of Pharmaceutical Sciences 2015; 10(2): 81-98. [CrossRef]
- McMaster, CR. From yeast to humans - roles of the Kennedy pathway for phosphatidylcholine synthesis. FEBS Lett. 2018 Apr;592(8):1256-1272. [CrossRef]
- Cummings R, Parinandi N, Wang L, Usatyuk P, Natarajan V. Phospholipase D/phosphatidic acid signal transduction: role and physiological significance in lung. Mol Cell Biochem. 2002 May-Jun;234-235(1-2):99-109.
- Wagner K, Brezesinski G. Phospholipase D activity is regulated by product segregation and the structure formation of phosphatidic acid within model membranes. Biophys J. 2007 Oct 1;93(7):2373-83. [CrossRef]
- Bruntz RC, Lindsley CW, Brown HA. Phospholipase D signaling pathways and phosphatidic acid as therapeutic targets in cancer. Pharmacol Rev. 2014 Oct;66(4):1033-79. [CrossRef]
- Semenkovich CF, Goldberg AC, Goldberg IJ. Disorders of Lipid Metabolism. Chapter 37 in Melmed S, Polonsky KS, Larsen PR, Kronenberg HM, Eds. Williams Textbook of Endocrinology (Thirteenth Edition). Elsevier 2016: 1660-1700. [CrossRef]
- Blunsom NJ, Cockcroft S. Phosphatidylinositol synthesis at the endoplasmic reticulum. Biochim Biophys Acta Mol Cell Biol Lipids. 2020 Jan;1865(1):158471. [CrossRef]
- Pearce B, Jakobson K, Morrow C, Murphy S. Phosphatidic acid promotes phosphoinositide metabolism and DNA synthesis in cultured cortical astrocytes. Neurochem Int. 1994 Feb;24(2):165-71. [CrossRef]
- Quick J, Santos ND, Cheng MHY, Chander N, Brimacombe CA, Kulkarni J, van der Meel R, Tam YYC, Witzigmann D, Cullis PR. Lipid nanoparticles to silence androgen receptor variants for prostate cancer therapy. J Control Release. 2022 Sep;349:174-183. [CrossRef]
- Jeschek D, Lhota G, Wallner J, Vorauer-Uhl K. A versatile, quantitative analytical method for pharmaceutical relevant lipids in drug delivery systems. J Pharm Biomed Anal. 2016 Feb 5;119:37-44. [CrossRef]
- Rezaei S, Blick EE, Mineart KP, Kelley EG. Chapter Three - Linking chemical degradation and physical instability of lipid vesicles. Advances in Biomembranes and Lipid Self-Assembly 2025; 41: 47-64. [CrossRef]
- Sarkar S, Carroll B, Buganim Y, Maetzel D, Ng AH, Cassady JP, Cohen MA, Chakraborty S, Wang H, Spooner E, Ploegh H, Gsponer J, Korolchuk VI, Jaenisch R. Impaired autophagy in the lipid-storage disorder Niemann-Pick type C1 disease. Cell Rep. 2013 Dec 12;5(5):1302-15. [CrossRef]
- Dall'Armi C, Devereaux KA, Di Paolo G. The role of lipids in the control of autophagy. Curr Biol. 2013 Jan 7;23(1):R33-45. [CrossRef]
- Zhang S, Peng X, Yang S, Li X, Huang M, Wei S, Liu J, He G, Zheng H, Yang L, Li H, Fan Q. The regulation, function, and role of lipophagy, a form of selective autophagy, in metabolic disorders. Cell Death Dis. 2022 Feb 8;13(2):132. [CrossRef]
- Jarocki M, Turek K, Saczko J, Tarek M, Kulbacka J. Lipids associated with autophagy: mechanisms and therapeutic targets. Cell Death Discov. 2024 Oct 30;10(1):460. [CrossRef]
- Karim M, Mishra M, Lo CW, Saul S, Cagirici HB, Gourdelier M, Ghita L, Ojha A, Tran DHN, Agrawal A, McGraw C, East MP, Gammeltoft KA, Sahoo MK, Mooney NA, Johnson GL, Das S, Leyssen P, Neyts J, Chiu W, Cohen CA, Bukh J, Gottwein J, Dye JM, Neff N, Jackson PK, Pinsky BA, Laitinen T, Pantsar T, Poso A, Zanini F, De Jonghe S, Asquith CRM, Einav S. PIP4K2C inhibition reverses autophagic flux impairment induced by SARS-CoV-2. Nat Commun. 2025 Jul 10;16(1):6397. [CrossRef]
- Haucke V, Kozlov MM. Membrane remodeling in clathrin-mediated endocytosis. J Cell Sci. 2018 Sep 3;131(17):jcs216812. [CrossRef]
- Rigby RE, Rehwinkel J. RNA degradation in antiviral immunity and autoimmunity. Trends Immunol. 2015 Mar;36(3):179-88. [CrossRef]
- Acevedo-Whitehouse K, Bruno R. Potential health risks of mRNA-based vaccine therapy: A hypothesis. Med Hypotheses. 2023 Feb;171:111015. [CrossRef]
- Fung SYS, Xǔ XJ, Wu M. Nonlinear dynamics in phosphoinositide metabolism. Curr Opin Cell Biol. 2024 Jun;88:102373. [CrossRef]
- Thiemicke A, Neuert G. Rate thresholds in cell signaling have functional and phenotypic consequences in non-linear time-dependent environments. Front Cell Dev Biol. 2023 Mar 21;11:1124874. [CrossRef]
- Hou X, Chen Y, Carrillo ND, Cryns VL, Anderson RA, Sun J, Wang S, Chen M. Phosphoinositide signaling at the cytoskeleton in the regulation of cell dynamics. Cell Death Dis. 2025 Apr 14;16(1):296. [CrossRef]
- Adhikari H, Cullen PJ. Role of phosphatidylinositol phosphate signaling in the regulation of the filamentous-growth mitogen-activated protein kinase pathway. Eukaryot Cell. 2015 Apr;14(4):427-40. [CrossRef]
- Wang L, Eghtesad S, Clemens PR. Migration of dendritic cells from murine skeletal muscle. Immunobiology. 2011 Jan-Feb;216(1-2):195-9. [CrossRef]
- Woodland DL, Kohlmeier JE. Migration, maintenance and recall of memory T cells in peripheral tissues. Nat Rev Immunol. 2009 Mar;9(3):153-61. [CrossRef]
- Zhang Y, Garcia-Ibanez L, Ulbricht C, Lok LSC, Pike JA, Mueller-Winkler J, Dennison TW, Ferdinand JR, Burnett CJM, Yam-Puc JC, Zhang L, Alfaro RM, Takahama Y, Ohigashi I, Brown G, Kurosaki T, Tybulewicz VLJ, Rot A, Hauser AE, Clatworthy MR, Toellner KM. Recycling of memory B cells between germinal center and lymph node subcapsular sinus supports affinity maturation to antigenic drift. Nat Commun. 2022 May 5;13(1):2460. [CrossRef]
- Chazaud, B. Inflammation and skeletal muscle regeneration: Leave it to the macrophages! Trends Immunol. 2020 Jun;41(6):481-492. [CrossRef]
- Sackstein R, Schatton T, Barthel SR. T-lymphocyte homing: an underappreciated yet critical hurdle for successful cancer immunotherapy. Lab Invest. 2017 Jun;97(6):669-697. [CrossRef]
- Simonis A, Theobald SJ, Koch AE, Mummadavarapu R, Mudler JM, Pouikli A, Göbel U, Acton R, Winter S, Albus A, Holzmann D, Albert MC, Hallek M, Walczak H, Ulas T, Koch M, Tessarz P, Hänsel-Hertsch R, Rybniker J. Persistent epigenetic memory of SARS-CoV-2 mRNA vaccination in monocyte-derived macrophages. Mol Syst Biol. 2025 Apr;21(4):341-360. [CrossRef]
- Ochoa D, Bradley D, Beltrao P. Evolution, dynamics and dysregulation of kinase signalling. Curr Opin Struct Biol. 2018 Feb;48:133-140. [CrossRef]
- Pelley, JW. Membranes and Intracellular Signal Transduction. Chapter 5 in Pelley JW, Ed. Elsevier's Integrated Biochemistry. Mosby, 2007, 37-46. [CrossRef]
- Grecco HE, Schmick M, Bastiaens PI. Signaling from the living plasma membrane. Cell. 2011 Mar 18;144(6):897-909. [CrossRef]
- Mukherjee A, Huang Y, Elgeti J, Oh S, Abreu JG, Neliat AR, Schüttler J, Su DD, Dupre C, Benites NC, Liu X, Peshkin L, Barboiu M, Stocker H, Kirschner MW, Basan M. Membrane potential mediates the cellular response to mechanical pressure. bioRxiv [Preprint]. 2024 Nov 13:2023.11.02.565386. [CrossRef]
- Szischik CL, Reves Szemere J, Balderrama R, Sánchez de la Vega C, Ventura AC. Transient frequency preference responses in cell signaling systems. npj Syst Biol Appl 2024; 10: 86. [CrossRef]
- Cobb MH, Goldsmith EJ. Dimerization in MAP-kinase signaling. Trends Biochem Sci. 2000 Jan;25(1):7-9. [CrossRef]
- Fossett, N. Signal transduction pathways, intrinsic regulators, and the control of cell fate choice. Biochim Biophys Acta. 2013 Feb;1830(2):2375-84. [CrossRef]
- Landry BD, Clarke DC, Lee MJ. Studying Cellular Signal Transduction with OMIC Technologies. J Mol Biol. 2015 Oct 23;427(21):3416-40. [CrossRef]
- Vijay S, Gujral TS. Non-linear deep neural network for rapid and accurate prediction of phenotypic responses to kinase inhibitors. iScience. 2020 May 22;23(5):101129. [CrossRef]
- Jiang Y, AkhavanAghdam Z, Li Y, Zid BM, Hao N. A protein kinase A-regulated network encodes short- and long-lived cellular memories. Sci Signal. 2020 May 19;13(632):eaay3585. [CrossRef]
- Ghomlaghi M, Hart A, Hoang N, Shin S, Nguyen LK. Feedback, Crosstalk and competition: ingredients for emergent non-linear behaviour in the PI3K/mTOR signalling network. Int J Mol Sci. 2021 Jun 28;22(13):6944. [CrossRef]
- Veres T, Kerestély M, Kovács BM, Keresztes D, Schulc K, Seitz E, Vassy Z, Veres DV, Csermely P. Cellular forgetting, desensitisation, stress and ageing in signalling networks. When do cells refuse to learn more? Cell Mol Life Sci. 2024 Feb 19;81(1):97. [CrossRef]
- Rauch N, Rukhlenko OS, Kolch W, Kholodenko BN. MAPK kinase signalling dynamics regulate cell fate decisions and drug resistance. Curr Opin Struct Biol. 2016 Dec;41:151-158. [CrossRef]
- Lavoie H, Gagnon J, Therrien M. ERK signalling: a master regulator of cell behaviour, life and fate. Nat Rev Mol Cell Biol 2020; 21: 6070632. [CrossRef]
- Parres-Gold J, Levine M, Emert B, Stuart A, Elowitz MB. Contextual computation by competitive protein dimerization networks. Cell. 2025 Apr 3;188(7):1984-2002.e17. [CrossRef]
- Avraham R, Yarden Y. Feedback regulation of EGFR signalling: decision making by early and delayed loops. Nat Rev Mol Cell Biol. 2011 Feb;12(2):104-17. [CrossRef]
- Wen PJ, Osborne SL, Meunier FA. Phosphoinositides in neuroexocytosis and neuronal diseases. Curr Top Microbiol Immunol. 2012;362:87-98. [CrossRef] [PubMed]
- Tsuruta, F. New insights into the functions of PtdIns(3,5)P2 in the pathogenisis of neurodegenerative disorders. Neural Regen Res. 2016 Feb;11(2):240-1. [CrossRef]
- Houthaeve G, De Smedt SC, Braeckmans K, De Vos WH. The cellular response to plasma membrane disruption for nanomaterial delivery. Nano Converg. 2022 Feb 1;9(1):6. [CrossRef]
| Pathway | Direction of NES | Consequences/Biological Function |
| Mismatch repair | Downregulated | DNA repair inefficiency; Promotion of tumorigenesis [137] |
| Phagosome | Upregulated | Induction of phagocytosis and autophagy |
| Necroptosis | Upregulated | Inflammatory form of cell death associated with many human diseases [138] |
| Apoptosis | Upregulated | Induction of programmed cell death |
| Metabolism of xenobiotics by cytochrome P450 | Downregulated | Impaired cytochrome P450 activity in the liver may lead to increased drug toxicity [139] |
| NF-κB | Upregulated | A key regulator of the immune system, inflammation, cell survival, and stress responses [140] |
| TNF | Upregulated | A powerful pro-inflammatory agent that regulates many facets of macrophage function [141] |
| IL-17 | Upregulated | Promotes proinflammatory cytokine production, neutrophil recruitment, tissue remodeling, and antimicrobial defenses [142] |
| Toll-like receptors, RIG-1-like receptors, Nod-like receptors | Upregulated | These receptors activate inflammatory and immune responses [143] |
| TCA cycle | Downregulated | Impaired TCA cycle is a feature of Alzheimer’s disease [144] |
| Circadian rhythm | Downregulated | Dysregulation of circadian rhythms increases cancer susceptibility [145] |
| Hematopoetic cell lineage | Upregulated | Increased clonal hematopoiesis leads to hematological malignancy [146] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





