1. Introduction
Sudden cardiac arrest affects around 30000 people every year in the UK. Of the 8-10% of patients who survive this event, around 70% experience fatigue, half have some degree of cognitive impairment and between 1/4 and a 1/3 experience significant symptoms of low mood, anxiety and/or post-traumatic stress disorder six months after the event [
1]. Recent guidelines [
1] position statements [
2,
3] and quality standards [
4]recommend the investigation of all these domains, before and after discharge. To date, however, no study has been published on the implementation of these guidelines in routine clinical practice.
Guidance on how to complete the screening is scant. European Resuscitation Council guidelines recommend performing “functional assessments of physical and non-physical impairment” before discharge from hospital: this refers to a wide range of (semi)structured evaluations aimed at understanding the patient's current capabilities and limitations, and to inform rehabilitation, discharge planning, and ongoing care. Their use has been relatively limited in published studies, with a few exception – namely, the Frenchay Activities Index (FI) [
5]¸the Katz Index of Independence in Activities of Daily Living [
6] the assessment of Motor and Process Skills (AMPS) and the Activities of Daily Living Interview (ADL-I) [
7,
8] which however are unlikely to be widely used in routine clinical practice where the assessment of ADLs is more often unstandardised, variable and informal.
ERC guidelines recommend using the MoCA (Montreal Cognitive Assessment) to formally evaluate cognition, and the IQCODE-CA (Informant Questionnaire of Cognitive decline in the Elderly—Cardiac Arrest version) and the CLCH-24 (Checklist Cognition and Emotion) to investigate informants’ and patients’ (respectively) insight into cognition and behaviour if required.
The HADS (Hospital Anxiety and Depression Scale) is also recommended for the screening of emotional problem and widely available. No specifically validated tool is recommended to assess fatigue, despite this being the most common complaint, with only a handful of tools having been used in the literature (Modified Fatigue Impact Scale; Fatigue Severity Scale; Patient-Reported Outcome Measurement Information System-Fatigue Scale; Multidimensional Fatigue Inventory (MFI-20) [
9,
10,
11])
In this context, working practices in the use of screening tools for cognition, mood and fatigue are largely understudied in the UK; unsurprisingly, no information is currently available on what tools are being used in different cardiac arrest centres (as defined in [
12]) to screen survivors following an OHCA, their acceptability to patients and what type of barriers and facilitators can affect their routine use.
In this audit, we operationalised the 2021 ERC–ESICM post-resuscitation guidelines into five criteria and prospectively audited adherence across four centres in South-East England. The 2025 guidelines update preserves the same core elements (functional assessment before discharge; organised ≤3-month follow-up with cognitive, emotional, and fatigue screening; information/support for patients and co-survivors [
13]), so our endpoints remain aligned; the added emphasis on structured rehabilitation does not change them
2. Methods:
Structure of the clinical audit
Participating Organizations and Timeframe of Audit
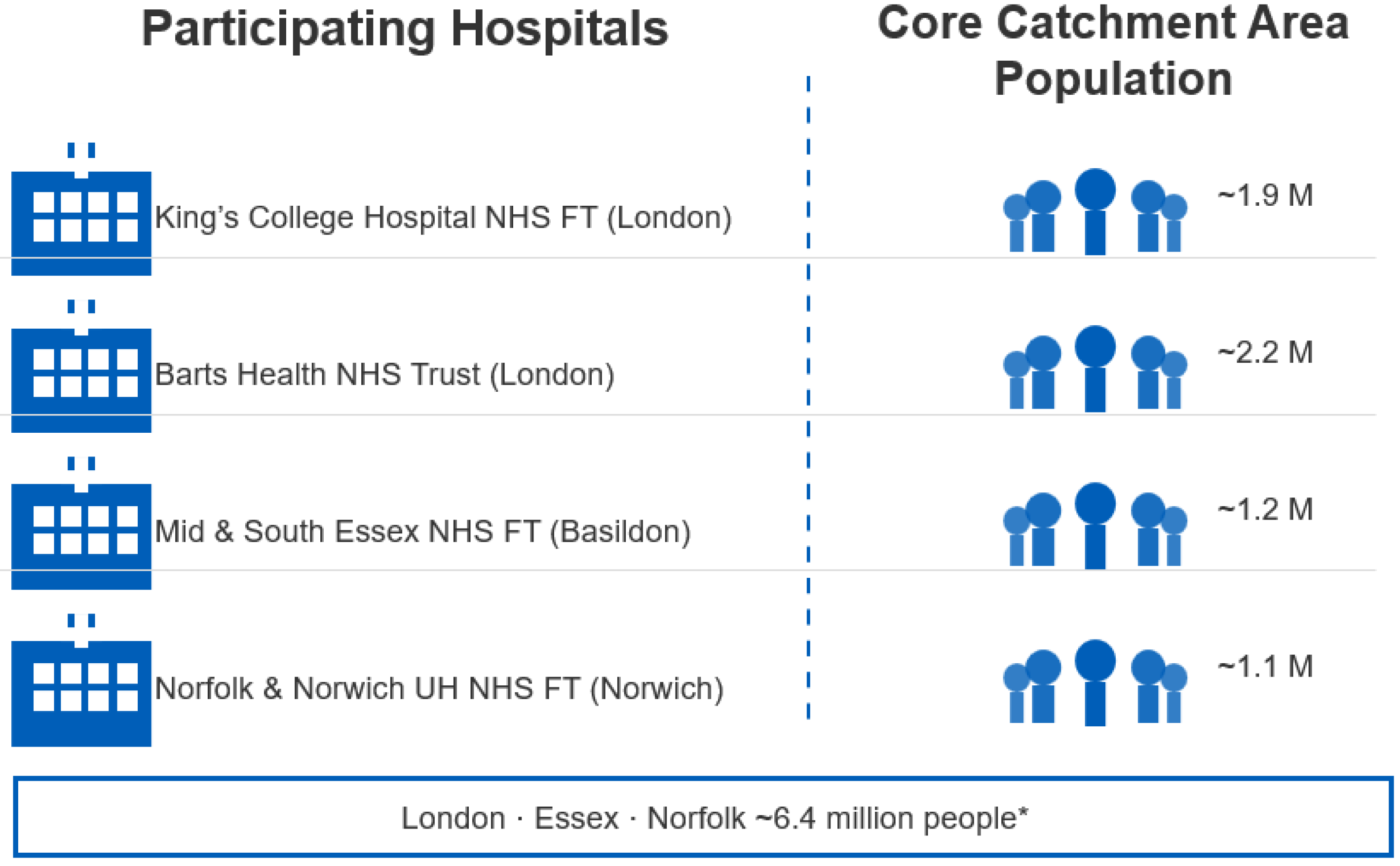
A multidisciplinary working group on ‘care and rehabilitation’ following OHCA first met in December 2022, comprising therapists from 4 different NHS Hospital Trusts in Southeast/Eastern England (King’s College Hospital NHS Foundation Trust; Barts Health NHS Trust; Mid and South Essex NHS Foundation Trust; Norfolk and Norwich University Hospital NHS Foundation Trust –
Figure 1). These specialized tertiary hospital units serve a large catchment area across London, Essex and Norfolk, covering a population of around 6.2 million people, and at the time had established pilot systems to complete pre-discharge and follow-up assessments for OHCA survivors.
To gain some system-level insights into the way these systems were structured and implemented, the group decided to engage in a prospective, multi-centre, 6-month audit of current practices in the assessment of cognition, mood, fatigue, and quality of life following an OHCA.
The audit was divided into pre-discharge and follow-up sections. All patients admitted between the 1st of June 2023 and the 30th November 2023 who were discharged alive from hospital were included in the audit; the follow-up section of the audit was completed when the last patient recruited was seen at follow-up (timing could vary depending on each individual centre’s practices in completing the follow-up).
Audit Criteria and Standards Used.
This audit assessed the compliance with European Resuscitation Council guidelines on post-resuscitation care. Two standards were specifically investigated:
Standard 1 – pre-discharge care “Providing information and performing functional assessments of physical and non-physical impairments before discharge from the hospital”.
Standard 2 – post-discharge care “Systematic follow-up of all cardiac arrest survivors within 3 months following hospital discharge, which should, at least, include cognitive screening, screening for emotional problems and fatigue, and the provision of information and support for patients and their family”
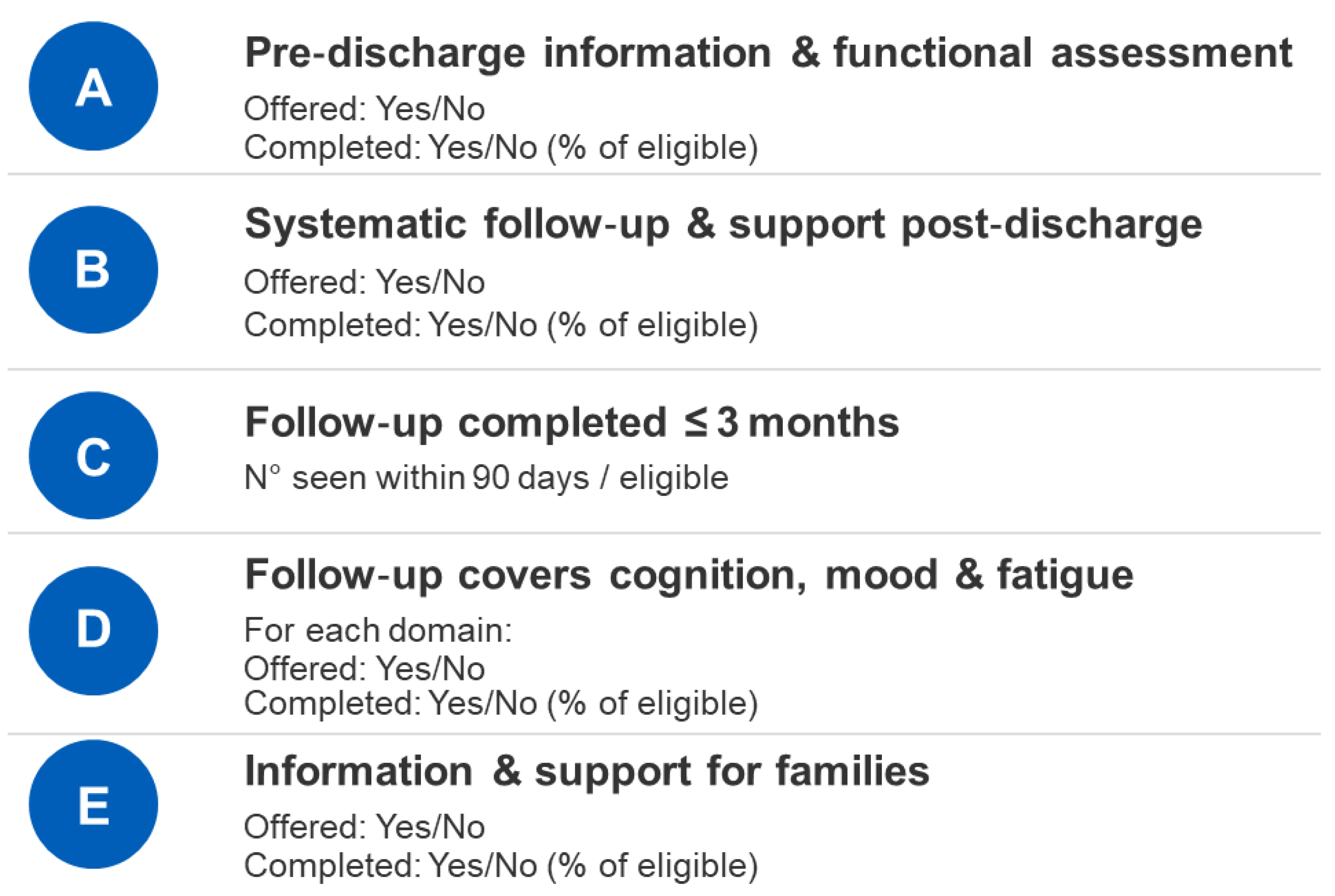
These standards were operationalised into 5 measurable criteria, based on documentation of whether an action was offered and/or completed. Completion rates are reported as the percentage of patients who received the action out of those eligible. Follow-up involved provision of information and support. Subcomponents of follow-up – cognitive, emotional, fatigue screening and family support – are reported separately (
Figure 2)
In addition to measuring adherence to the above criteria, we also recorded reasons for failure to complete an assessment.
Ethics
According to guidance published by the Healthcare Quality Improvement Partnership, this project was classified as a clinical audit and registered at MSE (Mid and South Essex NHS Trust) with reference number CTCCA103 in October 2023. No ethics application was required as patients continued to receive standard clinical care without any modification or intervention beyond routine practice.
Data analysis and Interpretation
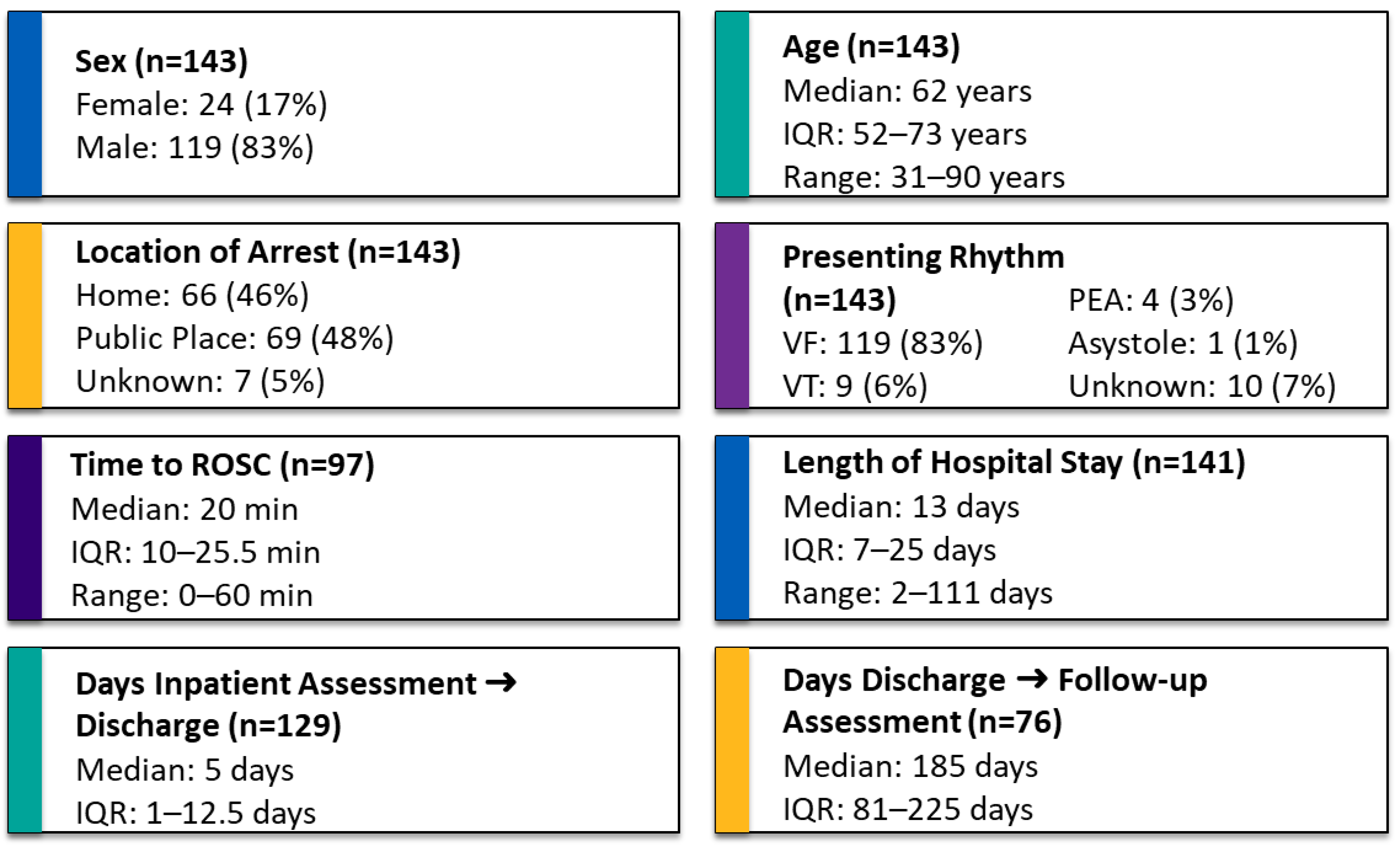
Descriptive statistics were used to characterize patient demographics, clinical features, and the frequency of assessments completed pre-discharge and during follow-up. Continuous variables (e.g., age, length of hospital stay, days from hospital discharge to follow-up) were summarized using medians and interquartile ranges (IQR), reflecting the non-normal distribution typically seen in clinical audit data. Categorical variables (e.g., sex, location of arrest, presenting rhythm) were summarized using frequencies and percentages.
Compliance with the predefined audit criteria was calculated and expressed as percentages to illustrate performance against standards. Analysis of assessment completion rates distinguished between pre-discharge and post-discharge phases, with additional stratification by assessment type (cognitive screening, emotional problems, fatigue).
Reasons for non-completion of assessments were categorized and quantified separately for inpatient and mapped onto the Theoretical Domains Framework (TDF). This integrative tool provides a structured approach for systematically identifying barriers and facilitators to implementation, mapping these to evidence-based intervention strategies, and evaluating mechanisms of change within complex healthcare settings [
14]
Comparative analyses between centres were not performed as the audit’s main objective was to highlight practice variations collectively and generate shared learning rather than evaluate individual centre performance.
All statistical analyses were performed using SPSS version 29.0.1.
3. Results:
A total of 143 OHCA patients were discharged alive from hospital across the 4 sites during the 6 months of this audit. Descriptive variables are presented in
Table 1. Normality testing using the Kolmogorov-Smirnov test indicated that time to ROSC, length of hospital stay, days from inpatient assessment to hospital discharge, and days from hospital discharge to follow-up were not normally distributed (p <0.001), whereas the assumption of normality could not be rejected for age (p=0.2)
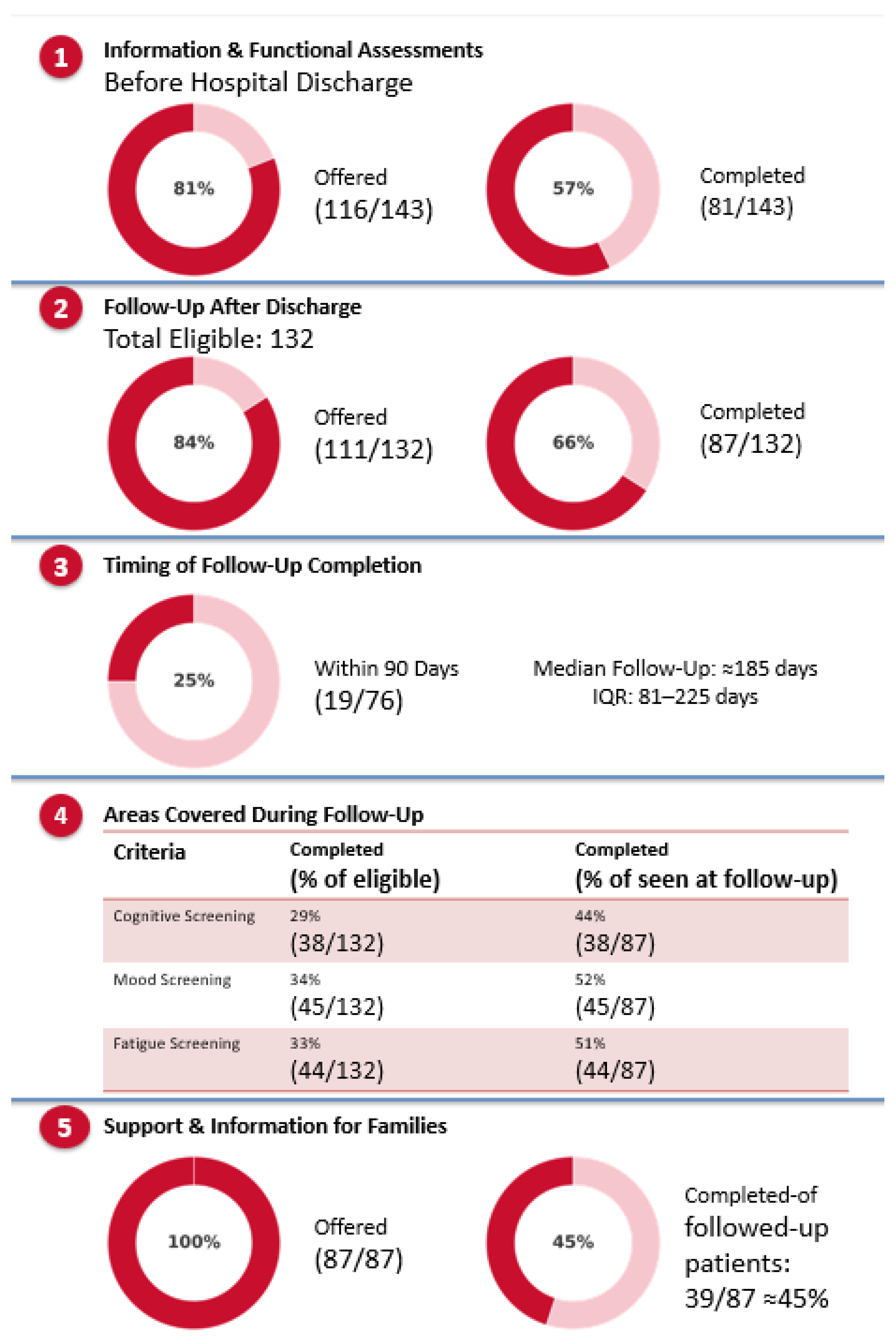
Before discharge, the audit evaluated whether patients received information and a functional assessment addressing physical and non-physical impairments. Out of 143 patients, assessments were fully completed for 81 individuals (57%). In an additional 35 cases, attempts were made—however patients either declined (3), were discharged before the assessment could be administered/finished (17), or they were unable to complete the process due to significant cognitive impairment (15). In 27 cases, clinicians relied on other formal or informal observations – including standardized paper-and-pencil tasks – rather than on functional assessment, which were therefore not completed
With regard to the follow-up, the audit tracked the provision of information and support for survivors of cardiac arrest. Of the 143 patients, 11 were recorded as having passed away, 24 were not invited to participate due to local hospital policies (that is, patient discharged out of area, or not admitted to ICU), and 21 follow-ups were attempted but ultimately not completed, either because they did not attend or could not be contacted. However, only 19 out of 76 patients with available data were followed up within the recommended three-month period, amounting to just 25% meeting this target, while the median follow-up occurred much later, at approximately 185 days after discharge [IQR 81 to 225] (
Figure 3)
With respect to the content of the follow-ups completed, only around half of them included cognitive screening (44%), screening of emotional problems (52% )or assessment of fatigue (51%) as recommended by ERC guidelines. This was most often due to patients declining standardized assessments and self-reporting ‘no problems’ in these areas. Other reasons included discretionary decision by clinicians not to administer the assessment, lack of time, or patients cognition too severely impaired (flowchart in
Figure 4).
Lastly, an attempt was made to invite a survivor’s family member in all cases, however only 39/87 (45%) attended.
From the original cohort of 143 patients, 11 (7.7%) were deceased at follow-up, leaving 132 survivors. Contact was attempted for 108 patients (81.8% of survivors), resulting in 87 completed assessments (80.6% of those contacted). Among these 87 assessed patients, cognitive assessments were completed in 38 (43.7%), mood screenings in 45 (51.7%), and fatigue screenings in 44 (50.6%). Reasons for non-completion across domains included assessments not being offered, time constraints, patient decline, cognitive impairment, and assessments deemed unnecessary by the clinician.
4. Discussion
In this prospective audit we investigated compliance with post-resuscitation ERC guidelines across four tertiary cardiac arrest centres in the southeast of England that were, at the time, providing both in-patient and follow-up care. Guidelines were operationalised into five measurable criteria, and compliance was evaluated by collecting additional information on implementation barriers when a standard could not be followed or was not adhered to. We also reported the percentages of assessments attempted but ultimately unsuccessful, with a view to provide insights into real-life implementation challenges. In this discussion, we classify barriers using the Theoretical Domains Framework – an established taxonomy in implementation research that helps identify reasons why things do not happen in practice.
Pre-Discharge Care
In terms of pre-discharge care, the discrepancy between completed and offered assessments was due mainly to four factors: patients’ level of cognitive impairment, patients declining the assessment, clinicians not having enough time to complete them, and assessments not being offered as judged unnecessary.
In this cohort, a poor neurological outcome was relatively uncommon – only 15/143 (9.5%) of patients showed marked neurological impairment; this is in line with data from Western countries, where withdrawal of life sustaining treatment is routinely practiced [
15]. Arguably, the multidimensional complexity of rehabilitation and information needs of this cohort of survivors is unique, and best served by access to specialist rehabilitation as advocated by NICE Guideline NG211 (2022 – “Rehabilitation after traumatic injury”) or by the Royal College of Physicians Disorders of Consciousness Guidelines (2020 – “Prolonged disorders of consciousness following sudden onset brain injury).
In the larger group of survivors with less significant neurological and cognitive problems, the second, third and fourth factor can be mapped respectively to the “Beliefs about consequences (patient-related)”, “Environmental context and resources” and “Beliefs about consequences (clinician-related)” TDF domain. Whilst the former was a minor barrier in this audit, the second affected a larger proportion of patients. Suggested mitigation measures include adding a checklist item to the discharge summary, flagging patients at risk of being discharged early, and/or increasing capacity in the system by providing additional administration or clinician time (Table 2)
With regard to assessments not being offered as judged unnecessary, this could largely be due to clinicians relying on other formal or informal observations – including standardized paper-and-pencil tasks – and stemming from the belief that additional assessments would not add value. Although adding this task as part of a standard operating procedure could help overcome this barrier, clinical staff would need to perceive the utility of this approach for it to be sustainable in the long term.
Post-Discharge Care
Inconsistent provision of follow-up care was due to several factors, largely mapping to three TDF domains – namely “Environmental context and resources”, “Beliefs about consequences / motivation (patient-related)” and “Social Influences”.
Issues related to “Environmental context and resources” involved, for instance, local operational procedures that did not mandate a follow-up for patients not admitted to ICU or discharged outside the hospital’s catchment area, resulting in 16.8% (21/132) of them not being offered a follow-up appointment at all. During the appointment, specific assessments were at times not administered due to them not being part of the follow-up workflow but rather discretionary for the clinicians completing them (15, 8 and 4 patients not offered cognitive, mood and fatigue assessment respectively). Administration of assessments was also occasionally hindered by lack of clinic time (6, 5 and 4 patients with respect to cognitive, mood and fatigue). A wider issue was found regarding the availability of follow-up slots, resulting in only a quarter of appointments being completed within the recommended 90 days, with a median time of around 6 months.
Regarding the second domain, of the patients offered an appointment, around a fifth were either non-contactable, or did not attend the appointment (24/111). When an appointment was attended (87), a sizeable proportion of patients (~28-29%) declined specific aspects of the assessment (standardized cognitive assessment; mood and fatigue screening), suggesting that patient-related motivational factors play a significant role – that is, patients do not perceive a possible benefit or fear experiencing an additional burden of care. However, it is also possible that patients may have declined or avoided follow-up assessments due to cultural norms, social stigma, lack of family support, language barriers, or financial/practical difficulties that influenced their willingness to engage (therefore mapping onto the “Social influences” domain). Similar factors also likely played a role in the reduced attendance of relatives of OHCA survivors; although relatives of all patients reviewed in the clinic (N = 87) were invited to the follow-up, only 39 (45%) attended. None of the hospitals had any provision for inviting relatives when the patient declined to be involved or was not contactable (
Table 2)
Limitations
This audit has several limitations. First, it was observational and non-comparative in design. While it allowed for the prospective collection of implementation data across multiple centres, it did not aim to evaluate the effectiveness of specific interventions, compare performance between sites, or assess clinical outcomes. As such, findings should be interpreted as descriptive of current practice rather than indicative of impact.
Second, the lack of standardisation across centres limited internal consistency. Variations in how assessments were administered, documented, or prioritised reflected local resource constraints and existing workflows, making direct comparisons between sites inappropriate. This heterogeneity is informative but constrains generalisability.
Third, selection bias may have influenced follow-up data. Although 132 patients were eligible for follow-up, only 108 were invited, with some patients excluded due to local referral procedures—for example, those not admitted to ICU or discharged outside a hospital's catchment area. This may have skewed findings toward those more likely to engage with services.
Forth, while the audit captured which tools were used, it did not assess how consistently or accurately they were applied, or whether staff received training. The psychometric robustness of these tools in this context was also not examined, and some are not specifically recommended for OHCA survivors.
Finally, the audit did not include any formal measures of acceptability, burden, or perceived utility of assessments from the perspectives of patients, relatives, or clinicians. These insights are critical for guiding meaningful quality improvement and ensuring that interventions are not only deliverable but valued by those involved.
In addition, this audit was conducted at four large hospital trusts that already had infrastructure in place to offer post-resuscitation follow-up care and had expressed an interest in improving practice. As such, these centres likely represent a best-case scenario within the wider system. The level of care delivered across all trusts nationally—many of which may lack structured follow-up pathways or access to rehabilitation staff—is likely to be lower. This selection bias should be considered when interpreting the findings and planning for wider implementation.
5. Conclusions
This multicentre prospective audit provides insights into the current implementation of post-resuscitation ERC guidelines across four specialist centres in southeast England. By operationalising guidelines into measurable criteria, we identified specific areas of incomplete adherence and, crucially, barriers mapped to the Theoretical Domains Framework (TDF).
Barriers related to Environmental context and resources were particularly prominent, notably affecting timely assessments both pre-discharge and during follow-up. Limited staff availability, short hospital stays, and fragmented or inconsistent follow-up procedures indicate the need for organisational strategies such as standardising assessment workflows, clarifying responsibilities, embedding assessment tasks into routine discharge summaries, and ensuring sufficient clinical and administrative capacity.
Clinician- and patient-related factors, mapped primarily onto the domain of Beliefs about consequences, also significantly influenced guideline adherence. Clinicians occasionally considered additional formal assessments unnecessary, relying instead on informal evaluations or prior documentation, suggesting that targeted education and training may be essential. Patients and relatives frequently declined or did not engage with offered assessments, highlighting a need for approaches that enhance their understanding of the value of follow-up and reduce perceived burden, such as framing assessments as routine care, providing early informational interventions, or offering flexible attendance formats (e.g., telehealth options).
Future improvement efforts should leverage these TDF insights, prioritizing interventions that directly target the identified behavioural domains. This could include operational changes (e.g., protected time for follow-up assessments, increase clinic capacity), targeted training and education programs to shift clinician perceptions and behaviours, and improved patient and relative communication strategies. Adopting a structured, theory-informed approach offers the greatest potential to enhance guideline adherence, ensuring comprehensive, equitable, and sustainable rehabilitation care following cardiac arrest.
Supplementary Materials
The following supporting information can be downloaded at the website of this paper posted on Preprints.org.
Author Contributions
Conceptualization (idea formulation), M.M.; methodology (study design and audit framework), M.M., A.S., M.K., C.K., S.M.; validation (cross-checking and verification of data and interpretations), M.M.; formal analysis (data processing and summary statistics), M.M.; investigation (data collection and site coordination), M.K., A.S., S.M., J.D., U.S. and C.K.; data curation (data entry and quality control), M.M. and C.K., writing – original draft preparation (manuscript drafting), M.M.; writing—review and editing (critical revision and approval of the final text), M.K., A.S., C.K., N.G., N.P., and T.R.K.; visualization (figure design and layout), M.M.; supervision (oversight and guidance), T.R.K. and N.G.; project administration (coordination across sites), M.M.; funding acquisition (resources and support), none. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and registered as a clinical audit at Mid and South Essex NHS Foundation Trust (reference number CTCCA103, October 2023). Ethical approval was not required as the project met criteria for clinical audit under the UK Health Research Authority and Healthcare Quality Improvement Partnership guidance.
Informed Consent Statement
Not applicable. This study involved analysis of anonymised audit data and did not include identifiable human participants.
Data Availability Statement
The aggregated, anonymised audit dataset underlying this study is available from the corresponding author upon reasonable request and subject to local information governance approvals. No publicly archived datasets were generated.
Acknowledgments
The authors thank all clinicians and therapists across the participating centres for their invaluable support in data collection and local audit registration. During the preparation of this manuscript, the authors used ChatGPT (GPT-5, OpenAI) to assist with language editing and structural refinement. The authors have reviewed and edited all AI-generated content and take full responsibility for the final version of this publication.
Conflicts of Interest
The authors declare no conflicts of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
References
- Nolan JP, Sandroni C, Böttiger BW, Cariou A, Cronberg T, Friberg H, et al. European Resuscitation Council and European Society of Intensive Care Medicine Guidelines 2021: Post-resuscitation care. Resuscitation 2021;161:220–69. [CrossRef]
- Sawyer KN, Camp-Rogers TR, Kotini-Shah P, Del Rios M, Gossip MR, Moitra VK, et al. Sudden Cardiac Arrest Survivorship: A Scientific Statement from the American Heart Association. Circulation 2020:E654–85. [CrossRef]
- Mion M, Simpson R, Johnson T, Oriolo V, Gudde E, Rees P, et al. British Cardiovascular Intervention Society Consensus Position Statement on Out-of-hospital Cardiac Arrest 2: Post-discharge Rehabilitation. Interventional Cardiology: Reviews, Research, Resources 2022. [CrossRef]
- Resuscitation Council UK. Quality Standards: Survivors | Resuscitation Council UK 2024. https://www.resus.org.uk/library/quality-standards-cpr/quality-standards-survivors (accessed September 30, 2024).
- Moulaert VRMP, Wachelder EM, Verbunt JA, Derick T W, Van Heugten CM. Determinants of quality of life in survivors of cardiac arrest. J Rehabil Med 2010. [CrossRef]
- Geri G, Dumas F, Bonnetain F, Bougouin W, Champigneulle B, Arnaout M, et al. Predictors of long-term functional outcome and health-related quality of life after out-of-hospital cardiac arrest. Resuscitation 2017;113:77–82. [CrossRef]
- Elisabet E, Waehrens E, Eastwood G, Kristensen LQ, Eiskjaer H, Van Tulder M, et al. Early ADL ability assessment and cognitive screening as markers of post-discharge outcomes after surviving an out-of-hospital cardiac arrest. A prospective cohort study. Resuscitation 2025;0:110653. [CrossRef]
- Christensen J, Eskildsen SJ, Gregers Winkel B, Kofoed Dichman C, Wagner MK. Motor and process skills in activities of daily living in survivors of out-of-hospital cardiac arrest: a cross-sectional study at hospital discharge. European Journal of Cardiovascular Nursing 2021;20:775–81. [CrossRef]
- Kim YJ, Rogers JC, Raina KD, Callaway CW, Rittenberger JC, Leibold M Lou, et al. An intervention for cardiac arrest survivors with chronic fatigue: A feasibility study with preliminary outcomes. Resuscitation 2016;105:109–15. [CrossRef]
- Joshi VL, Tang LH, Kim YJ, Wagner MK, Nielsen JF, Tjoernlund M, et al. Promising results from a residential rehabilitation intervention focused on fatigue and the secondary psychological and physical consequences of cardiac arrest: The SCARF feasibility study. Resuscitation 2022;173:12–22. [CrossRef]
- Joshi VL, Tang LH, Mikkelsen TB, Nielsen JF, Zinckernagel L, Borregaard B, et al. Does time heal fatigue, psychological, cognitive and disability problems in people who experience an out-of-hospital cardiac arrest? Results from the DANCAS survey study. Resuscitation 2023;182. [CrossRef]
- Boulton AJ, Abelairas-Gómez C, Olaussen A, Skrifvars MB, Greif R, Yeung J. Cardiac arrest centres for patients with non-traumatic cardiac arrest: A systematic review. Resuscitation 2024;203:110387. [CrossRef]
- Nolan J.P.; Sandroni C.; Cariou A.; Cronberg T.; D’Arrigo S.; Haywood K.; Hoedemaekers A.; Lilja G.; Nikolaou N.; Olasveengen T.M.; Robba C.; Skrifvars M.B.; Swindell P.; Soar J. European Resuscitation Council and European Society of Intensive Care Medicine Guidelines 2025: Post-Resuscitation Care. Intensive Care Med. 2025; Online ahead of print. [CrossRef]
- Michie S, Johnston M, Abraham C, Lawton R, Parker D, Walker A. Making psychological theory useful for implementing evidence based practice: A consensus approach. Qual Saf Health Care 2005;14:26–33. [CrossRef]
- Gräsner J-T, Herlitz J, M Tjelmeland IB, Wnent J, Lilja G, Bein B, et al. Epidemiology of cardiac arrest in Europe. Resuscitation 2021;161:61–79.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).