1. Introduction
Multiple myeloma (MM) is a plasma cell malignancy accounting for approximately 10% of all hematologic neoplasms. It is characterized by clonal expansion of malignant plasma cells in the bone marrow, leading to end-organ damage such as bone lysis, anemia, renal insufficiency, and immune dysfunction. Over the past two decades, the therapeutic landscape has been transformed by the advent of proteasome inhibitors, immunomodulatory agents, and monoclonal antibodies, markedly improving survival and depth of response. A roadmap towards improving outcomes in multiple myeloma highlights how these novel agents have shifted standard-of-care paradigms [
2].
Despite these advances, autologous stem cell transplantation (ASCT) remains a foundational therapy for transplant-eligible patients, offering deeper remission and longer progression-free survival when integrated into modern regimens. The
2024 update on diagnosis, risk-stratification, and treatment emphasizes that even in the era of potent induction therapies, ASCT retains a critical role [
3].
The optimal timing of autologous stem cell transplantation (ASCT) in newly diagnosed multiple myeloma (MM) has been debated for decades. Clinical trials have typically endorsed early ASCT—performed within 12 months of diagnosis following induction therapy—as standard practice, citing improvements in response depth and progression-free survival [
4]. However, in real-world settings, practice often diverges from trial protocols. Some patients face delays due to comorbidities, organ dysfunction, or suboptimal response to induction therapy [
5]. Others confront logistical or socioeconomic hurdles, leading to postponed ASCT timing. In these scenarios, transplantation may be deferred, raising key questions about which clinical or biological factors most significantly contribute to treatment delay [
3,
6].
Current international guidelines continue to emphasize the importance of early autologous stem cell transplantation (ASCT) in transplant-eligible patients, yet they provide limited direction on how to prioritize or risk-stratify candidates based on the optimal timing of the procedure [
7]. To address this gap, several studies have investigated clinical predictors that may influence transplant timing, including disease burden at diagnosis—such as bone marrow plasma cell infiltration—disease stage, cytogenetic abnormalities, renal function, and patient-related characteristics such as age and performance status [
8].
The Revised Myeloma Comorbidity Index (R-MCI) was developed to quantify the cumulative comorbidity burden in multiple myeloma (MM) and to support individualized treatment planning. R-MCI incorporates five parameters—age, Eastern Cooperative Oncology Group (ECOG) performance status, renal function (eGFR), pulmonary function, and cytogenetic risk profile—creating a concise, disease-specific score that predicts outcomes more accurately than generic indices [
1]. Validated across independent MM cohorts, R-MCI has shown strong predictive value for overall survival and treatment tolerance and is increasingly used to guide therapy intensity in both clinical trials and real-world settings [
9]. However, its specific role in defining the timing of transplantation—rather than transplant eligibility alone—remains underexplored.
One particularly understudied factor is the
percentage of bone marrow plasma cells at diagnosis, often used as a surrogate for disease burden. While studies have shown that high plasma cell infiltration (e.g.,≥ 60%) is independently predictive of poorer progression-free survival and overall survival—even after adjusting for established prognostic markers—its direct influence on clinical decisions regarding early versus delayed ASCT remains unproven [
10]. Likewise, although transplant-timing studies, such as those by Blackburn et al., provide insights into predictive factors and barriers in real-world settings, the independent and combined roles of comorbidity scores, ISS staging, and plasma cell burden in dictating ASCT timing have not been conclusively delineated [
5].
Moreover, it remains uncertain whether the same clinical variables decisively influence the decision to proceed with ASCT at all. In routine clinical practice, a notable proportion of transplant-eligible patients may never receive transplantation due to clinical frailty, comorbidities, or failure to achieve disease control. For example, studies exploring barriers to ASCT report that logistic, financial, and cultural factors can discourage both physicians and patients from pursuing transplant [
11]. In addition, data from Tang et al. [
12] indicate that among transplant-eligible myeloma patients, those refusing or deemed unfit for ASCT had worse survival outcomes, emphasizing the clinical importance of understanding who proceeds to transplant and who does not.
In this retrospective observational study, we aimed to evaluate both transplant eligibility and timing in patients with multiple myeloma. Specifically, we assessed whether plasma cell infiltration at diagnosis, R-MCI score, ISS stage, age, and other clinical characteristics are associated with the likelihood of receiving ASCT. Among those who underwent transplantation, we further analyzed which of these variables influenced whether ASCT was performed early (≤12 months) or delayed (>12 months) after diagnosis. By exploring both the eligibility and timing dimensions, this study seeks to clarify the real-world determinants of ASCT decision-making and help inform individualized treatment planning in clinical practice.
2. Materials and Methods
This retrospective observational study was conducted at Marmara University Pendik Training and Research Hospital, a tertiary referral center located in Istanbul, Turkey. Adult patients diagnosed with MM between January 2015, and June 2025 were identified through institutional records. Ethical approval was obtained from the local institutional review board, and the study was conducted by the principles of the Declaration of Helsinki.
A total of 150 patients diagnosed with MM between January 2015, and June 2025 were identified. Of these, 13 were excluded due to missing data on one or more key clinical variables (age, ECOG performance status, eGFR, DLCO, cytogenetic profile, or bone marrow plasma cell percentage), yielding a final analysis cohort of 137 patients. Among them, 61 patients underwent ASCT, while 76 did not receive transplantation during follow-up. All patients had received standard induction regimens containing proteasome inhibitors and/or immunomodulatory agents before assessment for transplant eligibility.
For patients who underwent ASCT, the time interval between initial diagnosis and the transplantation procedure was calculated. Transplant timing was categorized as either early (≤12 months from diagnosis) or delayed (>12 months), based on current clinical practice patterns and literature-supported thresholds [
13]. This categorization reflects real-world clinical dynamics in which transplant timing may be influenced by disease stabilization, treatment response, or comorbidity burden.
Clinical and laboratory variables recorded at diagnosis comprised age, sex, ECOG, bone marrow plasma cell infiltration percentage, ISS stage, eGFR, and diffusing capacity of carbon monoxide DLCO. Cytogenetic risk status (standard vs. high risk, e.g. del(17p), t(4;14), t(14;16)) was documented when available. These parameters were then used to calculate the R-MCI according to the scoring scheme outlined in
Table 1. Total R-MCI scores ranged from 0 to 9 and were stratified as low risk (0–3), intermediate risk (4–6), or high risk (7–9). These scores were then incorporated, alongside the other clinical variables, into subgroup comparisons and multivariate logistic regression analyses to identify predictors of ASCT eligibility and timing.
All statistical analyses were performed using IBM SPSS Statistics (version 26.0; IBM Corp., Armonk, NY, USA). Continuous variables were expressed as medians with interquartile ranges (IQR), and categorical variables as counts with corresponding percentages. Between-group comparisons were conducted using the Mann–Whitney U test for continuous variables and the chi-square or Fisher’s exact test, as appropriate, for categorical variables. Variables with a p-value <0.10 in univariate analyses were entered into the multivariate logistic regression model to identify independent predictors of transplant timing. A two-sided p-value <0.05 was considered statistically significant.
The study protocol was approved by the Marmara University Faculty of Medicine Ethics Committee for Drug and Non-Drug Medical Device Research (Protocol No: 09.2025-25-0796) and conducted in accordance with the Declaration of Helsinki.
3. Results
3.1. Patient Characteristics
A total of 150 patients diagnosed with multiple myeloma between January 2015 and June 2025 were identified, of whom 137 were included in this retrospective analysis after excluding 13 patients with missing data on key clinical variables. The median age at diagnosis was 64 years (IQR: 57–71), and 57.7% (n=79) were female. The median bone marrow plasma cell infiltration at diagnosis was 60% (IQR: 30–80). Based on the ISS, 26 patients (19.0%) were classified as Stage I, 36 (26.3%) as Stage II, and 64 (46.7%) as Stage III. Staging information was unavailable in 11 patients.
R-MCI, incorporating age, performance status, renal and pulmonary function, and cytogenetic risk, was calculated in all patients. The median R-MCI score was 0 (IQR: 0–1), indicating a predominantly low-risk cohort.
ASCT was performed in 61 patients (44.5%), whereas 76 patients (55.5%) did not undergo transplantation during follow-up. All patients received standard induction therapy, which included proteasome inhibitors and/or immunomodulatory agents, before transplant evaluation.
3.2. Comparison Between Transplanted and Non-Transplanted Patients
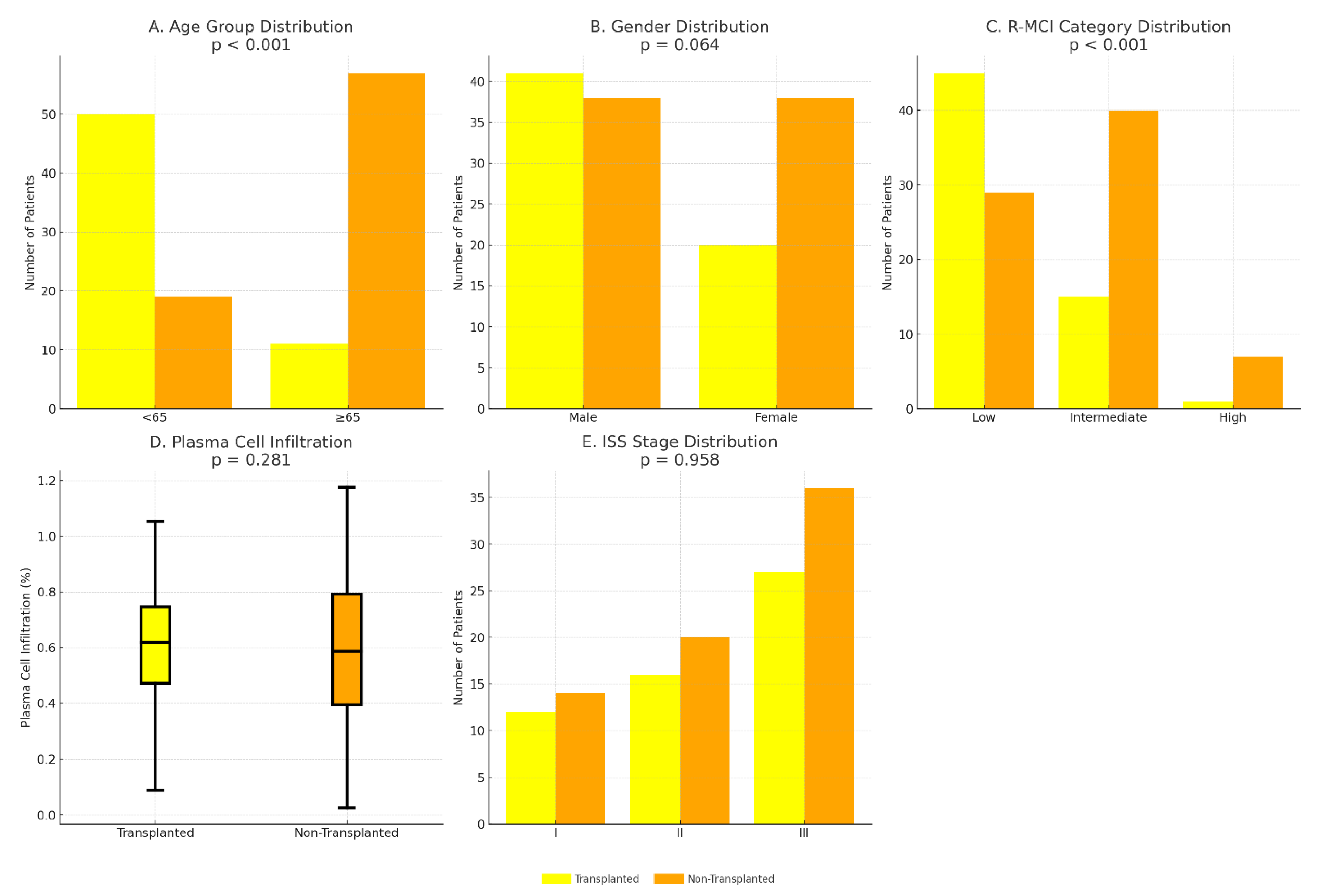
The proportion of patients aged < 65 years was significantly higher in the ASCT group than in the non-transplanted group (82.0% vs. 25.0%, p < 0.001), indicating that younger age strongly determined transplant eligibility. Similarly, the median R-MCI score was significantly lower among transplanted patients (0 [IQR 0–1] vs. 1 [IQR 0–2], p < 0.001), highlighting the influence of comorbidity burden on the decision to proceed with ASCT. In contrast, no significant differences were observed between the two groups in terms of female sex distribution (33% vs. 50%, p = 0.064), bone marrow plasma cell infiltration (median 60% vs. 57%, p = 0.281), or ISS stage distribution (p = 0.958). These comparisons are summarized in
Table 2 and illustrated in
Figure 1A–E.
3.3. Transplant Timing: Early vs. Delayed ASCT
Among the 61 patients who underwent ASCT, 26 (42.6%) received transplantation within 12 months of diagnosis (early ASCT), while 35 (57.4%) had delayed transplantation (more than 12 months).
No univariate differences were observed in age (median 57 vs. 60 years; p = 0.677), R-MCI score (median 0 vs. 1; p = 0.235), plasma cell infiltration (median 60% vs. 70%; p = 0.615), or sex (p = 0.989).
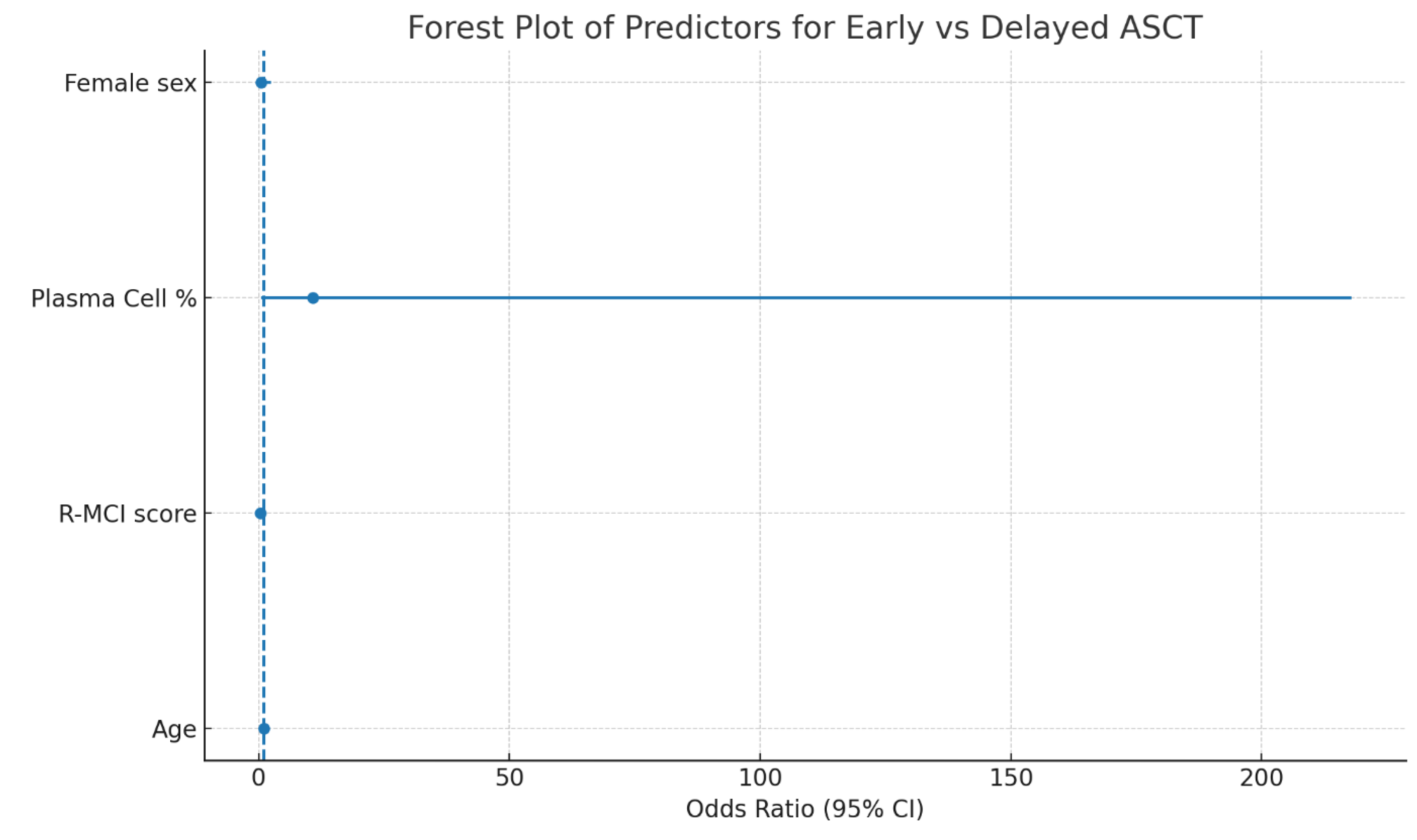
In multivariate logistic regression analysis (
Table 3,
Figure 2), only R-MCI score remained an independent predictor of ASCT timing: each one-point increase in R-MCI was associated with a 73% reduction in the odds of early transplantation (OR 0.267; 95% CI 0.067–1.058; p = 0.060), whereas age, plasma cell percentage, and sex were not significant.
4. Discussion
In this comprehensive single-center cohort, our data demonstrate that patient-related characteristics—particularly age and comorbidity burden—are the primary drivers of both eligibility for and timing of ASCT. The marked difference in transplant rates between patients aged <65 and ≥65 years (82.0% vs. 25.0%,
p < 0.001) suggests that chronological age remains a potent, though imperfect, surrogate for physiological reserve in clinical decision-making. More importantly, the significantly lower R-MCI scores among transplanted patients (median 0 vs. 1;
p < 0.001) indicate that structured comorbidity indices may offer a more nuanced assessment of patient fitness beyond age alone. These findings are consistent with recent literature emphasizing functional and organ-specific assessments over rigid age cut-offs in transplant algorithms [
9,
14,
15]
Contrary to expectations based on historical trial data, neither baseline tumor burden—reflected by bone marrow plasma cell infiltration—nor ISS stage distribution differed significantly between groups, suggesting that modern induction regimens may attenuate the prognostic weight of initial disease load when selecting transplant candidates [
16]. Although univariate analyses did not identify clear differences in timing of ASCT (≤ 12 months vs. > 12 months) based on age, R-MCI, or disease metrics, our multivariate model showed a non-significant trend toward delayed transplantation with increasing R-MCI (OR 0.267; 95% CI 0.067–1.058; p = 0.060). This finding may suggest that comorbidity burden not only influences the decision to proceed with ASCT but could also inform the strategic scheduling of high-dose therapy, perhaps allowing time for comorbidity optimization or deeper remission before transplant [
17,
18,
19].
Our findings highlight a potential role for R-MCI in shared decision-making discussions. By quantifying comorbidity burden, clinicians can more transparently communicate risks and benefits to patients, tailor pre-transplant interventions (e.g., rehabilitation, nutritional support), and set realistic expectations regarding timing and outcomes [
20,
21]. Although our study did not reveal a statistically significant association between ISS stage and the decision to proceed with transplantation, this does not diminish the prognostic importance of ISS; in fact, current international guidelines continue to strongly recommend early ASCT in patients with high ISS stage [
3,
7].
Our results suggest that in physiologically fit patients with preserved organ function and good performance status, the recommendation for early ASCT in high ISS disease remains highly relevant; however, with modern therapies, this decision can be further individualized by incorporating factors such as comorbidity profile, depth of treatment response, and patient preference [
16,
22]. The deep remissions and organ function recovery achieved with contemporary induction regimens may partially mitigate the adverse impact of high disease stage on transplant candidacy. Therefore, while ISS remains a critical determinant in transplant planning, integrating it with comorbidity indices such as R-MCI, depth of response, and patient preference could support a more nuanced and patient-centered approach to ASCT timing and eligibility [
23,
24,
25].
Interestingly, baseline bone marrow plasma cell percentage did not differ significantly between transplanted and non-transplanted patients, nor between early and delayed ASCT groups. This observation aligns with some recent real-world studies suggesting that, in the era of highly effective induction regimens, initial marrow plasma cell burden may have a diminished impact on transplant candidacy and timing compared to earlier treatment eras. It is plausible that modern therapies, by rapidly reducing tumor burden and achieving deep remissions, mitigate the prognostic weight traditionally attributed to baseline plasma cell infiltration [
26,
27].
Taken together, these observations highlight the complementary value of integrating structured comorbidity assessment tools such as the R-MCI alongside established disease staging systems like the ISS to individualize ASCT planning. Such an approach may ensure that transplant candidacy and timing reflect not only disease burden but also each patient’s unique physiological reserve and treatment response. Future prospective multicenter studies incorporating robust survival endpoints and comprehensive molecular risk stratification will be instrumental in validating these findings and informing next-generation transplant timing algorithms.
Limitations
This study’s retrospective, single-center design introduces potential selection bias and limits generalizability across diverse practice settings. Cytogenetic and molecular risk data were not consistently available, potentially underrepresenting the impact of high-risk abnormalities on transplant decisions. Additionally, we did not evaluate long-term outcomes—such as progression-free or overall survival—relative to the timing of ASCT, which restricts interpretation of the clinical benefit associated with early versus delayed transplantation. Socioeconomic factors, depth of response to induction therapy, logistical constraints, and individual patient preferences were not captured in our dataset. They may have importantly influenced both the eligibility and scheduling of ASCT. Despite these limitations, our findings provide valuable real-world insights into the pivotal role of comorbidity assessment in transplant decision-making.
5. Conclusion
In real-world practice, patient fitness—defined by age and comorbidity burden via the R-MCI—appears to play a more prominent role than traditional disease burden metrics in determining both eligibility for and timing of ASCT in multiple myeloma. Although our study did not demonstrate a statistically significant association between ISS stage and transplant decisions, this finding does not diminish the prognostic significance of ISS; current guidelines continue to strongly recommend early ASCT in patients with high ISS stage. Our results suggest that in physiologically fit patients with preserved organ function and good performance status, the recommendation for early ASCT in high ISS disease remains highly relevant; however, with modern therapies, this decision can be further individualized by incorporating factors such as comorbidity profile, depth of treatment response, and patient preference.
Incorporating structured comorbidity assessment tools into transplant decision workflows, alongside established disease staging systems, may enhance individualized patient selection and optimize the timing of high-dose therapy. Prospective, multicenter studies incorporating comprehensive molecular profiling and survival analyses will be instrumental in developing new transplant decision-making algorithms that integrate both R-MCI and ISS.
Author Contributions
O.C. conceived and designed the study, performed data analysis, and drafted the manuscript. N.N., A.B., D.D., and A.M.Y. contributed to data collection and curation. A.F.Y. provided critical review and intellectual input. A.T.T., I.A., and T.T. supervised the study and offered methodological guidance. All authors read and approved the final version of the manuscript.
Acknowledgments
The authors would like to thank all colleagues involved in data collection and manuscript preparation.
Funding Information: No funding was received for this study.
Declaration of Competing Interests : The authors declare no competing financial or non-financial interests.
Data Accessibility Statement : The datasets generated and analyzed during the current study are available from the corresponding author upon reasonable request. Due to patient privacy and ethical restrictions, data are not publicly available.
Indicated Consent of the Patient: Before their participation, all study participants gave their informed consent.
Ethics Approval Statement: The study titled “Determinants of Eligibility and Timing of Autologous Transplantation in Multiple Myeloma: The Role of R-MCI and Diagnostic Plasma Cell Burden” was approved by the Marmara University Faculty of Medicine, Ethics Committee for Drug and Non-Drug Medical Device Research (Protocol No: 09.2025-25-0796). The study was conducted in accordance with the ethical principles outlined in the Declaration of Helsinki, and written informed consent was obtained from all participants.
Clinical Trial Registration: This study was not registered as a clinical trial, as it did not meet the criteria requiring registration.
Disclaimer For Use of External Material: In this investigation, no materials were replicated from outside sources.
References
- Engelhardt M, Domm A-S, Dold SM, Ihorst G, Reinhardt H, Zober A, et al. A concise revised Myeloma Comorbidity Index as a valid prognostic instrument in a large cohort of 801 multiple myeloma patients. haematologica. 2017;102(5):910.
- Mohty M, Facon T, Malard F, Harousseau J-L. A roadmap towards improving outcomes in multiple myeloma. Blood Cancer Journal. 2024;14(1):135.
- Rajkumar SV. Multiple myeloma: 2024 update on diagnosis, risk-stratification, and management. American Journal of Hematology. 2024;99(9):1802-24.
- Richardson PG, Jacobus SJ, Weller EA, Hassoun H, Lonial S, Raje NS, et al. Triplet therapy, transplantation, and maintenance until progression in myeloma. New England Journal of Medicine. 2022;387(2):132-47.
- Blackburn L, Mansour A, Zhao Q, Cottini F, Khan A, Bumma N, et al. Real World Predictors, Timing, and Outcomes of Autologous Stem Cell Transplantation in Patients with Multiple Myeloma. Hemato. 2024;5(4):407-19.
- Lupak O, Xiaoxia H, Xie P, Thanikachalam K, Jabbour-Aida H, Farhan S, et al. Disparities in utilization of autologous stem cell transplantation as consolidative therapy for multiple myeloma: a single institution retrospective review. Clinical Lymphoma Myeloma and Leukemia. 2021;21(8):e680-e5.
- Dimopoulos MA, Terpos E, Boccadoro M, Moreau P, Mateos M-V, Zweegman S, et al. EHA–EMN Evidence-Based Guidelines for diagnosis, treatment and follow-up of patients with multiple myeloma. Nature Reviews Clinical Oncology. 2025:1-21.
- Facon T, Dimopoulos MA, Meuleman N, Belch A, Mohty M, Chen W-M, et al. A simplified frailty scale predicts outcomes in transplant-ineligible patients with newly diagnosed multiple myeloma treated in the FIRST (MM-020) trial. Leukemia. 2020;34(1):224-33.
- Mian H, Wildes TM, Vij R, Pianko MJ, Major A, Fiala MA. Dynamic frailty risk assessment among older adults with multiple myeloma: A population-based cohort study. Blood cancer journal. 2023;13(1):76.
- Al Saleh AS, Parmar HV, Visram A, Muchtar E, Buadi FK, Go RS, et al. Increased bone marrow plasma-cell percentage predicts outcomes in newly diagnosed multiple myeloma patients. Clinical Lymphoma Myeloma and Leukemia. 2020;20(9):596-601.
- Bashir Q, Braunstein M, Buck T, Chmielewski C, Hartmann B, Janakiram M, et al. Overcoming barriers to autologous stem cell transplantation in multiple myeloma: recommendations from a multidisciplinary roundtable discussion. Transplantation and Cellular Therapy. 2023;29(11):666-73.
- Tang HKK, Fung CY, Hwang YY, Lee H, Lau G, Yip SF, et al. Prognostic factors in 448 newly diagnosed multiple myeloma receiving bortezomib-based induction: impact of ASCT, transplant refusal and high-risk MM. Bone Marrow Transplantation. 2024;59(5):660-9.
- Kumar L, Hussain MM, Chethan R, Sahoo RK, Malik PS, Sharma OD, et al. Multiple myeloma: impact of time to transplant on the outcome. Clinical Lymphoma Myeloma and Leukemia. 2022;22(9):e826-e35.
- Engelhardt M, Ihorst G, Duque-Afonso J, Wedding U, Spät-Schwalbe E, Goede V, et al. Structured assessment of frailty in multiple myeloma as a paradigm of individualized treatment algorithms in cancer patients at advanced age. Haematologica. 2020;105(5):1183.
- Sverrisdóttir IS, Rögnvaldsson S, Thorsteinsdottir S, Gíslason GK, Aspelund T, Turesson I, et al. Comorbidities in multiple myeloma and implications on survival: a population-based study. European journal of haematology. 2021;106(6):774-82.
- Palumbo A, Bringhen S, Ludwig H, Dimopoulos MA, Bladé J, Mateos MV, et al. Personalized therapy in multiple myeloma according to patient age and vulnerability: a report of the European Myeloma Network (EMN). Blood, The Journal of the American Society of Hematology. 2011;118(17):4519-29.
- Dhakal B, Szabo A, Chhabra S, Hamadani M, D’Souza A, Usmani SZ, et al. Autologous transplantation for newly diagnosed multiple myeloma in the era of novel agent induction: a systematic review and meta-analysis. JAMA oncology. 2018;4(3):343-50.
- Lee N, Moon S, Lee J, Park H, Kong S, Bang S, et al. Discrepancies between the percentage of plasma cells in bone marrow aspiration and BM biopsy: Impact on the revised IMWG diagnostic criteria of multiple myeloma. Blood Cancer Journal. 2017;7(2):e530-e.
- Schoeller K, Ihorst G, Scheubeck S, Holler M, Woerner SM, Reinhardt H, et al. The Revised Myeloma Comorbidity Index (R-MCI) as a promising approach for predicting overall (os)-and progression-free (pfs) survival and optimizing therapy strategies in multiple myeloma (mm) patients (pts)-comparative analysis of 5 comorbidity indices (ci), including retro-and prospective applicability. Blood. 2019;134:3474.
- Dreyling E, Ihorst G, Reinhardt H, Räder J, Holler M, Herget G, et al. Optimizing individualized therapy decision-making in multiple myeloma (MM): integration and impact of the Revised Myeloma Comorbidity Index in the MM-tumor board. Annals of Hematology. 2025;104(1):593-603.
- Agarwal M. Multiple myeloma: treatment is getting individualized. Indian Journal of Hematology and Blood Transfusion. 2016;32(1):3-9.
- Pawlyn C, Davies FE. Toward personalized treatment in multiple myeloma based on molecular characteristics. Blood, The Journal of the American Society of Hematology. 2019;133(7):660-75.
- Ebraheem MS, Chakraborty R, Rochwerg B, Visram A, Mohyuddin GR, Venner CP, et al. Quadruplet regimens for patients with newly diagnosed multiple myeloma: a systematic review and meta-analysis. Blood advances. 2024;8(23):5993-6002.
- Shah GL, Seier K, Devlin SM, Chung DJ, Scordo M, Hultcrantz M, et al. Depth of response and outcomes in patients with multiple myeloma undergoing autologous stem cell transplantation. Blood. 2018;132:4619.
- Ebraheem M, Kumar SK, Dispenzieri A, Jevremovic D, Buadi FK, Dingli D, et al. Deepening responses after upfront autologous stem cell transplantation in patients with newly diagnosed multiple myeloma in the era of novel agent induction therapy. Transplantation and Cellular Therapy. 2022;28(11):760. e1-. e5.
- Vij R, Kumar S, Zhang M-J, Zhong X, Huang J, Dispenzieri A, et al. Impact of pretransplant therapy and depth of disease response before autologous transplantation for multiple myeloma. Biology of Blood and Marrow Transplantation. 2015;21(2):335-41.
- Popat R, Counsell N, de Tute R, De-Silva D, Phillips EH, Cavenagh JD, et al. Using depth of response to stratify patients to front line autologous stem cell transplant: results of the phase II PADIMAC myeloma trial. British Journal of Haematology. 2021;193(3):e19-e22.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).