1. Introduction
Epithelial ovarian carcinomas can be grouped into five main histologic subtypes by different histopathological features and molecular pathogenesis, high-grade serous, endometrioid, ovarian clear cell carcinoma (OCCC), mucinous and low-grade serous carcinomas, by different histopathological features and molecular pathogenesis [
1]. OCCC represents approximately 10% of all ovarian carcinomas, with an incidence ranging from 5 to 25% depending on geographic, ethnic and/or racial factors [
1,
2,
3]. The incidence of OCCC is gradually increasing in recent years in several countries, while currently the Asian women have the highest incidence. OCCC is the second most common histologic subtype of epithelial ovarian cancer after the serous type and typically occurs in younger women at an early stage [
4,
5,
6]. In a large cohort of young patients with stage I ovarian clear cell carcinoma, fertility-sparing surgery (FSS) was not associated with worse survival [
7]. However, OCCC has a great risk of recurrence and poor prognosis in comparison with other pathological types of epithelial ovarian carcinoma because of a relative resistance to first-line platinum-based chemotherapy [
8,
9] . Fertility preservation in patients with OCCC remains controversial due to its aggressive biological behavior and limited evidence supporting conservative management [
10]. Herein, we report a young patient with ovarian clear cell carcinoma who underwent a fertility-sparing operation, followed by six courses of combination chemotherapy with liposomal paclitaxel and carboplatin, and remained disease-free during follow-up and achieved a successful full-term pregnancy after in vitro fertilization and embryo transfer.
2. Case Presentation
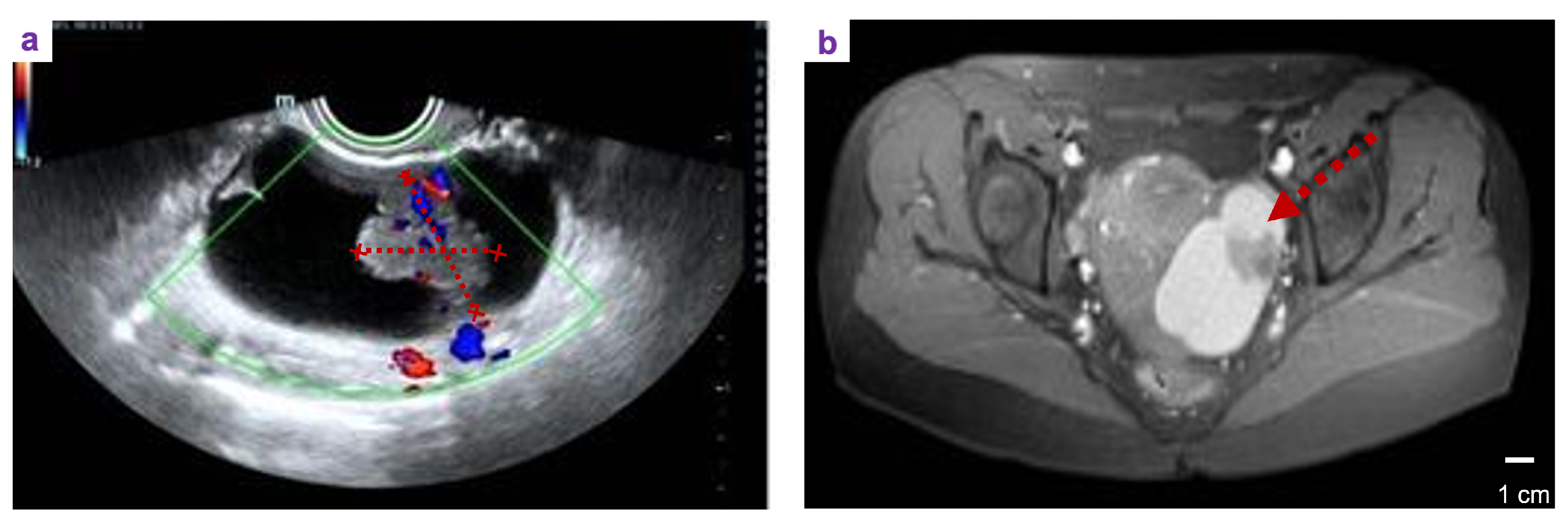
A 33 year-old female patient, unmarried, G0P0 came to the gynacological department with the main complaint of Left adnexal mass discovered on physical examination 7 days ago. She complained occasional mild lower-abdominal pain between menstruations, without bloating, weight loss, and abnormal vaginal bleeding. The past history did not show abnormalities. Her family history included her father suffered from hypertension and coronary heart disease, while her mother was healthy. At her first vist, a 7.5 × 4.4 cm mixed cystic-solid mass with nternal septations and vascularity was detected in her left adnexal region. (
Figure 1a). Furthermore, the left adnexal cystic-solid lesion and small uterine fibroid was confirmed by MRI scan (
Figure 1b). The laboratory result showd CA-125, CA-153, CA-199, HE4, CEA, AFP are all in normal range.
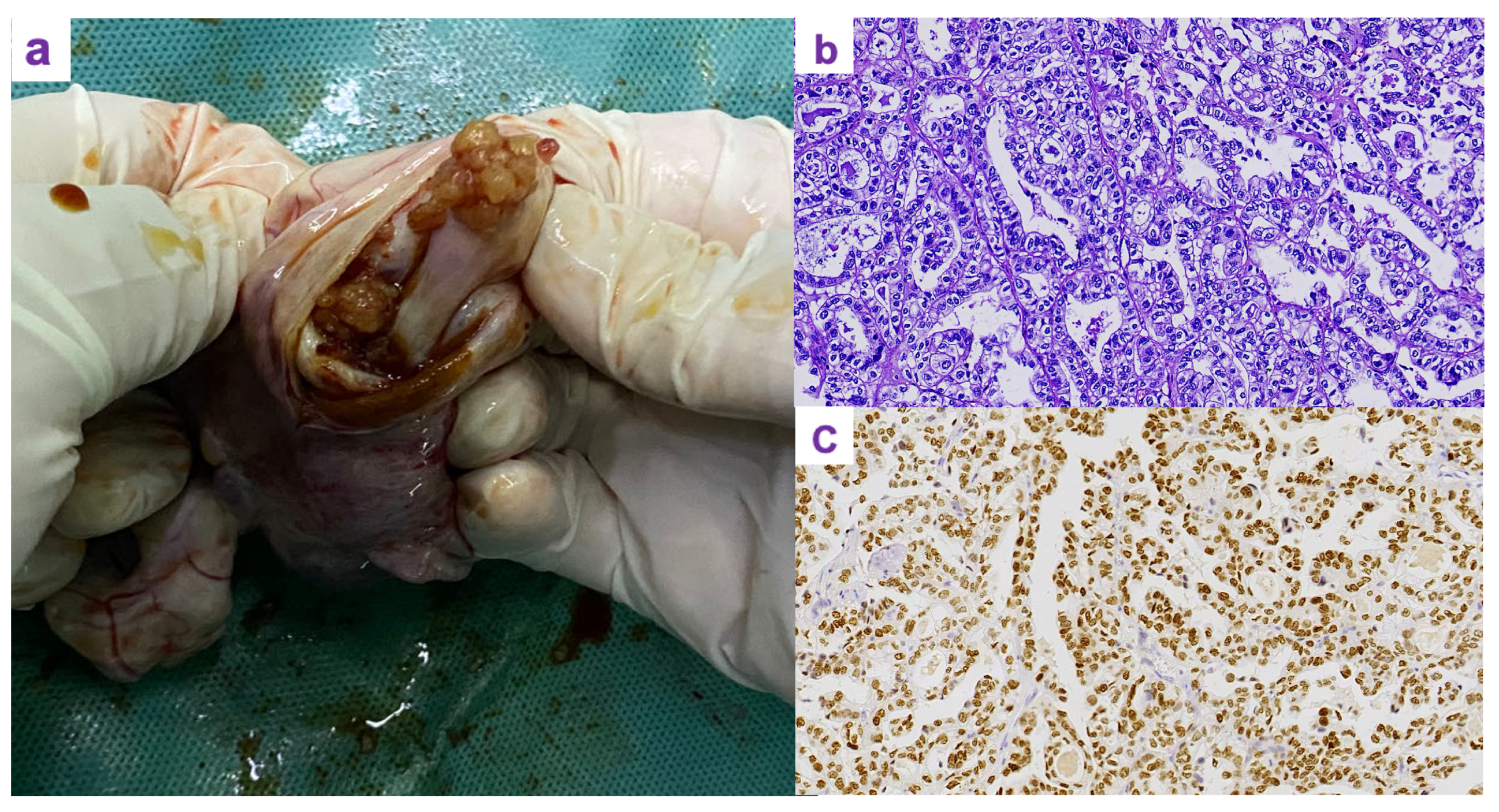
Due to the patient’s young age and early-stage disease, a laparotomic left salpingo-oophorectomy was performed. The ovarian mass was removed intact without rupture and then opened after excision. Grossly, the tumor consisted of a solid-cystic mass with a cystic wall encapsulating solid components (
Figure 2a). The specimen was submitted for intraoperative frozen section, which revealed features consistent with clear cell carcinoma. Immunohistochemical staining showed strong diffuse positivity for HNF-1
on DAB staining (
Figure 2b). The final histopathological examination confirmed the diagnosis of ovarian clear cell carcinoma, FIGO stage IA (pT1a N0 M0).
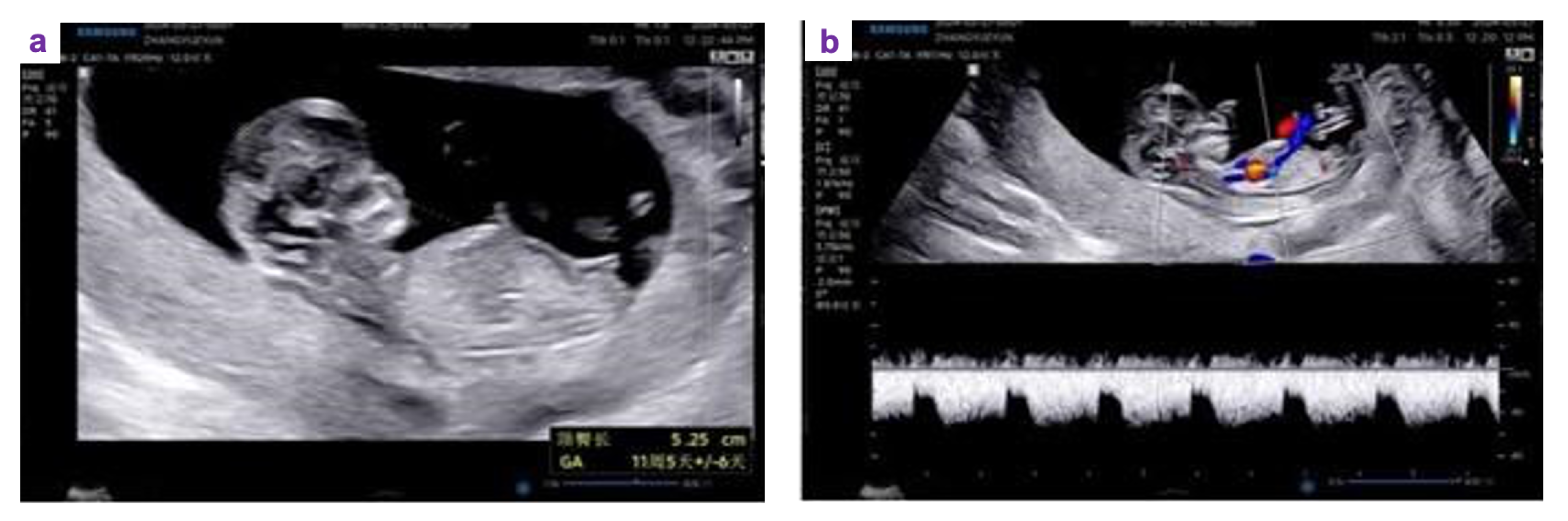
Six courses of paclitaxel (175 mg/m2)/carboplatin (AUC 6) in combination with adjuvant chemotherapy were administered smoothly. To protect ovarian function during chemotherapy, gonadotropin-releasing hormone agonist (GnRH-a, leuprolide depot) was administered every 28 days for a total of six doses. Regular monitoring of clinical presentation was performed every three months after completion of chemotherapy. The tumor markers were all within the normal range. Approximately one year after completing chemotherapy, the patient underwent in vitro fertilization and embryo transfer (IVF-ET). A successful pregnancy was achieved after the second embryo transfer. The ultrasound examination demonstrated a viable intrauterine pregnancy with normal fetal development (
Figure 3).
3. Discussion
In this case report, we described a rare but encouraging case of successful pregnancy following FSS and adjuvant chemotherapy in a patient with OCCC. This outcome is remarkable given that OCCC is typically considered a high-risk histologic subtype with limited data supporting fertility preservation. FSS appears to be a safe alternative for young women (<45 years old) with FIGO stage I ovarian clear cell carcinoma who wish to preserve fertility. In a cohort of 47 patients comparing FSS with radical surgery, the mean time to recurrence was 19 months after FSS and 20 months after radical surgery (P = 0.935). The sites of recurrence were comparable between the two groups. Moreover, there were no significant differences in 5-year disease-free survival (77% vs. 84%; P = 0.849) or 5-year overall survival (91% vs. 88%; P = 0.480).[
10,
11].
OCCC is considered relatively insensitive to chemotherapy compared with other histologic subtypes of epithelial ovarian cancer. In a cohort of 27 patients with stage III/IV OCCC and residual disease after surgery, the response rate to platinum-based chemotherapy was only 11.1% [
8]. In the recurrent or relapsed setting, reported response rates are as low as 6–8%. Retrospective data indicates that the median overall survival of patients with platinum-sensitive OCCC is approximately 16 months, whereas that of patients with platinum-resistant disease is only 7 months [
9]. These findings underscore the need for novel targeted therapies to improve outcomes in OCCC.
Pregnancy after fertility-sparing surgery has been encouraged for patients with stage IA/IC low-grade epithelial ovarian cancer (EOC). In one cohort of 40 patients (mean age 28 years; range 18–44 years), histologic subtypes included mucinous (47.5%), clear cell (22.5%), endometrioid (20%), and serous carcinoma (10%). Laparoscopic surgery was performed in 40% of cases, and 67.5% of patients received adjuvant chemotherapy. Among those who attempted conception (13 patients, 32.5%), eight (61.5%) achieved spontaneous pregnancy, resulting in five live births (three term and two preterm), one fetal loss, one intrauterine fetal death, and one fetal anomaly. Notably, no tumor recurrence occurred during pregnancy [
12].
In this case, the patient received six cycles of paclitaxel (175 mg/m²) and carboplatin (AUC 6) as adjuvant chemotherapy, which were completed without complications. Three months after completion of treatment, all laboratory parameters had returned to normal. Concurrently, a gonadotropin-releasing hormone agonist (GnRH-a; leuprolide depot) was administered every 28 days for a total of six doses to protect ovarian function. Although the benefit of adjuvant chemotherapy for stage IA–IC1 ovarian clear cell carcinoma (OCCC) remains uncertain because of the relative chemoresistance of this subtype compared with other forms of epithelial ovarian cancer, chemotherapy was administered in this case in view of the potential risk of microscopic residual disease and the inherently aggressive biological behavior of OCCC. According to current clinical guidelines, adjuvant chemotherapy is routinely recommended for patients with stage IC2 disease or higher. Previous studies have demonstrated the limited responsiveness of OCCC to platinum-based chemotherapy. For instance, among 27 patients with stage III/IV OCCC and residual disease, the response rate to platinum-based therapy was only 11.1% [
8], while in the recurrent or relapsed setting, response rates have been reported to be as low as 6–8%. These findings emphasize the need for more effective and targeted treatment strategies for this histologic subtype.
4. Conclusions
In conclusion, this case highlights a rare but encouraging instance of successful pregnancy following FSS and adjuvant chemotherapy in a patient with OCCC. Despite being a high-risk histologic subtype with relative chemoresistance and limited evidence supporting fertility preservation, favorable oncologic and reproductive outcomes can be achieved in carefully selected patients with early-stage disease and thorough surgical staging. Adjuvant chemotherapy was administered in this case to mitigate the potential risk of microscopic residual disease, reflecting a cautious yet individualized treatment approach. The preservation of ovarian function and achievement of a successful pregnancy without tumor recurrence support the feasibility of fertility-sparing management in young women with stage IA–IC1 OCCC. However, given the limited data and the aggressive nature of OCCC,FSS should only be considered in strictly selected cases, accompanied by comprehensive counseling and close long-term surveillance. Further multi-center studies and long-term follow-up are warranted to refine patient selection criteria and optimize both oncologic safety and reproductive outcomes.
Author Contributions
SW: conceptualization; Validation; Investigation; Writing - original draft ; Writing - review and editing; Visualization. QL: Validation; Investigation; Writing - original draft ; Writing - review and editing, Visualization. BZ: Conceptualization; Validation; Investigation; Writing - original draft ; Writing - review and editing; Visualization; Supervision; FZ: Conceptualization; Validation; Investigation; Writing - original draft ; Writing - review and editing; Visualization; Supervision
Funding
This research received no external funding.
Institutional Review Board Statement
Ethical review and approval were waived for this study, as it describes a single-patient case report considered non-research. The report contains no identifiable personal information.
Informed Consent Statement
Written informed consent was obtained from the patient for publication of this case report and any accompanying images
Data Availability Statement
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Acknowledgments
The authors would like to thank the colleagues from the Departments of Pathology and Ultrasound in the Affiliated Weihai Second Municipal Hospital of Qingdao University for their valuable assistance.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Prat, J.; D’Angelo, E.; Espinosa, I. Ovarian carcinomas: at least five different diseases with distinct histological features and molecular genetics. Human pathology 2018, 80, 11–27. [Google Scholar] [CrossRef] [PubMed]
- Pozzati, F.; Moro, F.; Pasciuto, T.; Gallo, C.; Ciccarone, F.; Franchi, D.; Mancari, R.; Giunchi, S.; Timmerman, D.; Landolfo, C.; et al. Imaging in gynecological disease (14): clinical and ultrasound characteristics of ovarian clear cell carcinoma. Ultrasound in Obstetrics & Gynecology 2018, 52, 792–800. [Google Scholar] [CrossRef] [PubMed]
- Kato, N.; Sato, Y.; Kamataki, A.; Fukase, M.; Uchigasaki, S.; Kurose, A. PIK3CA hotspot mutations and cyclooxygenase-2 expression in ovarian clear cell carcinomas: a close association with stromal features. Human Pathology 2019, 86, 32–37. [Google Scholar] [CrossRef] [PubMed]
- Phung, M.T.; Pearce, C.L.; Meza, R.; Jeon, J. Trends of ovarian cancer incidence by histotype and race/ethnicity in the United States 1992–2019. Cancer research communications 2023, 3, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.I.; Ha, H.I.; Eoh, K.J.; Lim, J.; Won, Y.J.; Lim, M.C. Trends in the incidence and survival rates of primary ovarian clear cell carcinoma compared to ovarian serous carcinoma in Korea. Frontiers in Oncology 2022, 12, 874037. [Google Scholar] [CrossRef] [PubMed]
- Chiang, Y.C.; Chen, C.A.; Chiang, C.J.; Hsu, T.H.; Lin, M.C.; You, S.L.; Cheng, W.F.; Lai, M.S. Trends in incidence and survival outcome of epithelial ovarian cancer: 30-year national population-based registry in Taiwan. Journal of gynecologic oncology 2013, 24, 342. [Google Scholar] [CrossRef] [PubMed]
- Nasioudis, D.; Mulugeta-Gordon, L.; McMinn, E.; Frey, M.K.; Chapman-Davis, E.; Holcomb, K. Fertility sparing surgery for patients with FIGO stage I clear cell ovarian carcinoma: a database analysis and systematic review of the literature. International Journal of Gynecological Cancer 2020, 30, 1372–1377. [Google Scholar] [CrossRef] [PubMed]
- Kajiyama, H.; Shibata, K.; Mizuno, M.; Yamamoto, E.; Fujiwara, S.; Umezu, T.; Suzuki, S.; Nakanishi, T.; Nagasaka, T.; Kikkawa, F. Postrecurrent oncologic outcome of patients with ovarian clear cell carcinoma. International journal of gynecological cancer 2012, 22, 801–806. [Google Scholar] [CrossRef] [PubMed]
- Takano, M.; Sugiyama, T.; Yaegashi, N.; Sakuma, M.; Suzuki, M.; Saga, Y.; Kuzuya, K.; Kigawa, J.; Shimada, M.; Tsuda, H.; et al. Low response rate of second-line chemotherapy for recurrent or refractory clear cell carcinoma of the ovary: a retrospective Japan Clear Cell Carcinoma Study. International Journal of Gynecological Cancer 2008, 18, 937–942. [Google Scholar] [CrossRef] [PubMed]
- Park, J.Y.; Suh, D.S.; Kim, J.H.; Kim, Y.M.; Kim, Y.T.; Nam, J.H. Outcomes of fertility-sparing surgery among young women with FIGO stage I clear cell carcinoma of the ovary. International Journal of Gynecology & Obstetrics 2016, 134, 49–52. [Google Scholar] [CrossRef] [PubMed]
- Prodromidou, A.; Theofanakis, C.; Thomakos, N.; Haidopoulos, D.; Rodolakis, A. Fertility sparing surgery for early-stage clear cell carcinoma of the ovary; A systematic review and analysis of obstetric outcomes. European Journal of Surgical Oncology 2021, 47, 1286–1291. [Google Scholar] [CrossRef] [PubMed]
- Yin, J.; Wang, Y.; Shan, Y.; Li, Y.; Jin, Y.; Pan, L. Pregnancy and oncologic outcomes of early stage low grade epithelial ovarian cancer after fertility sparing surgery: a retrospective study in one tertiary hospital of China. Journal of Ovarian Research 2019, 12, 44. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).