1. Introduction
Irritable bowel syndrome (IBS) is a chronic gastrointestinal (GI) disorder that is characterized by relapsing abdominal pain, bloating, and changes in bowel habits which manifests as primarily constipation, diarrhea, or both [
1]. Although IBS is not classically defined as an inflammatory condition, it significantly impacts quality of life [
1]. The exact etiology of IBS remains elusive. It is thought to be multi-factorial, involving one or more of the following: genetics, diet, stress response, infections, alterations in gut motility, and changes in gut microbiome [
2]. The gut microbiome plays a significant role in GI disease and in modulating skin health; forming the basis of the emerging concept of the gut-skin axis [
3]. This concept explores the bidirectional relationship between skin health and the gut microbiome [
3]. A growing body of evidence supports an association between gut microbiome dysbiosis, IBS and various inflammatory skin disorders [
4,
5].
The mucosal lining of the gut epithelium is colonized with a variety of microorganisms including bacteria, fungi, and protozoa which aid in digestion, drug metabolism, the maintenance of gut mucosal barrier integrity, immunomodulation and pathogen protection [
5]. When the gut barrier is impaired, this allows pathogens to colonize the gut and potentially lead to an imbalance of gut flora [
3]. Alterations in microbial composition may trigger inflammation, oxidative stress and further increase intestinal permeability [
6]. Studies have demonstrated distinct differences in gut microbiome composition between IBS patients and healthy controls [
7], highlighting a potential role for microbial dysbiosis in IBS pathophysiology.
These findings parallel research in dermatology, where studies have identified differences in gut microbiome composition between healthy individuals and patients with certain inflammatory skin diseases [
4]. Further, there is a growing interest in the use of probiotics in dermatology, with early trials demonstrating that certain probiotics may improve skin outcomes [
8]. Together, these observations highlight the importance of understanding the role of gut microbiome dysbiosis in dermatology.
Despite these parallels, the relationship between IBS and dermatologic disease remains underexplored. We chose to investigate IBS as opposed to another GI disorder such as inflammatory bowel disease (IBD) due to the scarcity of research linking IBS and skin pathologies. In contrast, IBD is a chronic inflammatory disorder of the bowel with well documented cutaneous associations [
9,
10]. The robustness of current literature on IBD and skin diseases highlights an important gap: the association between IBS and skin pathology remains unclear and warrants further investigation.
In this retrospective cohort study, we aimed to investigate the association between IBS and the following inflammatory skin pathologies: acne vulgaris, psoriasis, atopic dermatitis, hidradenitis suppurativa, rosacea, vitiligo, alopecia areata, and urticaria. Using the global health database, TriNetX, we compared the prevalence of these dermatological conditions in those with IBS and those without IBS. We also performed reciprocal analyses comparing the prevalence of IBS in patients with each dermatological disease to those without.
2. Materials and Methods
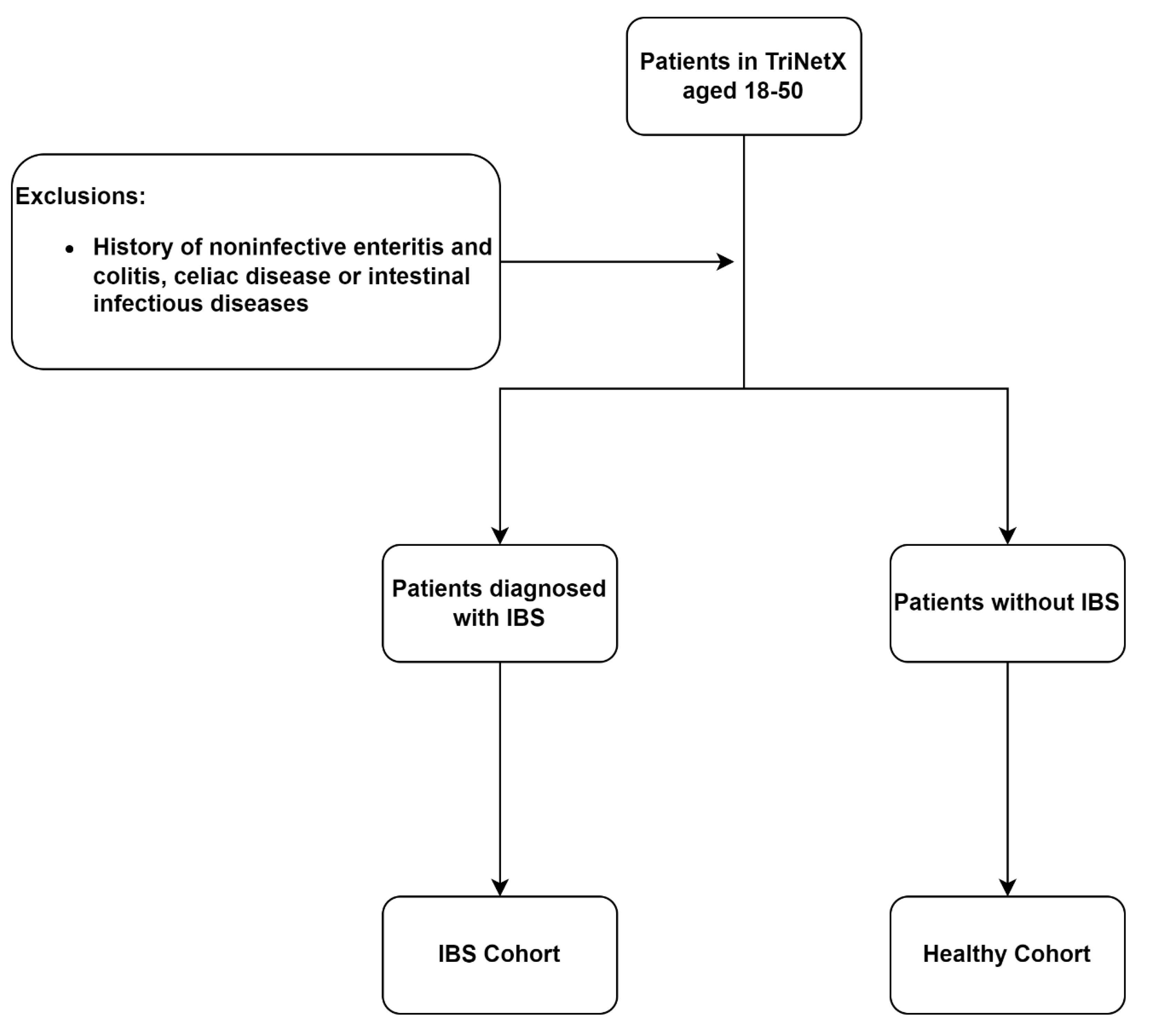
A retrospective cohort study was conducted using data from the US collaborative network on TriNetX. Patients were identified by using International Classification of Diseases, Tenth Revision, Clinical Modification codes, Current Procedural Terminology codes, Anatomical Therapeutic Chemical Classification System codes, and RxNorm codes (
Table 1). Patients were eligible if they were between the ages of 18-50. Patients with a history of IBD, celiac disease or infectious intestinal disease were excluded. To assess the epidemiologic association between IBS and dermatological disease, two primary cohorts were created: patients with IBS and non-IBS patients (
Figure 1). Cohorts were 1:1 propensity score matched by demographics, obesity, diabetes mellitus, tobacco use, alcohol use, generalized anxiety disorder and major depression disorder. The primary outcome in this analysis was the prevalence of acne vulgaris, psoriasis, atopic dermatitis, hidradenitis suppurativa, rosacea, vitiligo, alopecia areata, urticaria, 1-year after IBS diagnosis or 1-year following encounter for general adult medical examination without abnormal findings for healthy controls, assessed using Odds Ratios (OR) and 95% confidence intervals (CIs).
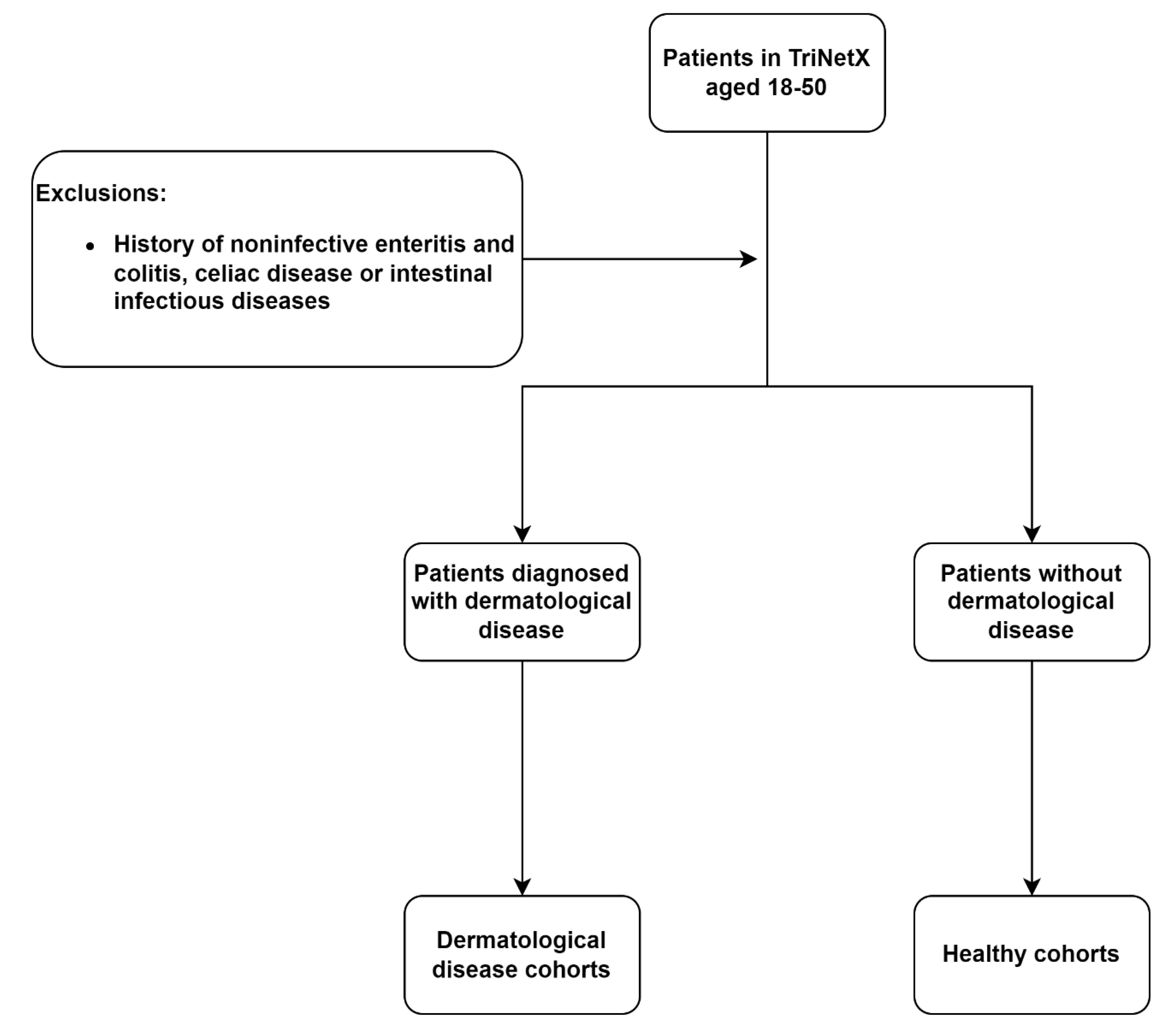
To confirm bidirectionality, reciprocal analyses were performed. Patients were considered eligible if they were between the ages of 18-50, excluding those with a history of IBD, celiac disease and infectious intestinal disease. Each analysis compared patients with dermatological disease (acne vulgaris, psoriasis, atopic dermatitis, hidradenitis suppurativa, rosacea, vitiligo, alopecia areata, urticaria) to patients without the corresponding disease (
Figure 2). All cohorts were 1:1 propensity score matched by demographics, obesity, diabetes mellitus, tobacco use, alcohol use, generalized anxiety, major depression disorder and systemic antibiotic use. Systemic antibiotic use was included as an additional matching variable in these analyses due to their potential to disrupt gut microbiota and confound the development of IBS. The primary endpoint of these analyses was the prevalence of IBS, 1-year following dermatological diagnosis or 1-year following encounter for general adult medical examination without abnormal findings for healthy controls, measured using ORs and 95% Cis.
3. Results
Over a 1-year period, the prevalence of acne vulgaris (OR: 0.78, CIs: 0.75-0.80) and vitiligo (OR: 0.78, CIs: 0.64-0.95) was lower in IBS patients compared to healthy controls. Psoriasis (OR: 1.14, CIs: 1.08-1.21), hidradenitis suppurativa (OR: 1.11, CIs: 1.03-1.20), rosacea (OR: 1.10, CIs: 1.03-1.18), and urticaria (OR: 1.27, CIs: 1.21-1.34) were more prevalent in IBS patients compared to healthy controls. No difference was observed for atopic dermatitis or alopecia areata (
Table 2).
In the reciprocal analysis, the prevalence of IBS was lower in alopecia areata patients (OR: 0.76, CIs: 0.64-0.90) compared to healthy controls after 1 year. The prevalence IBS was greater in patients with psoriasis (OR: 1.15, CIs: 1.07-1.23), rosacea (OR: 1.23, CIs: 1.15-1.31), and urticaria (OR: 1.06, CIs: 1.01-1.12) compared to their healthy control cohorts. No association was seen in patients with acne, atopic dermatitis, hidradenitis suppurativa, and vitiligo (
Table 3).
4. Discussion
The gut-skin axis refers to bidirectional communication between the GI tract and the skin [
11]. these two systems host a highly diverse microbiome, are involved in shaping the immune system, protecting against pathogens and maintaining a healthy barrier [
5]. Dysbiosis in the gut can disrupt immune homeostasis and lead to increased systemic inflammation [
4], which may contribute to the pathogenesis of inflammatory skin conditions including acne vulgaris, psoriasis, atopic dermatitis, hidradenitis suppurativa and rosacea [
5,
11].
Acne Vulgaris
The existing literature focused on the prevalence of IBS in acne vulgaris is controversial [
12,
13].
Demirbas and Elmas showed that IBS was significantly more common in patients with acne vulgaris compared to healthy controls [
13]. Additionally, they showed that patients with IBS had higher clinical severity, measured using the global acne grading system [
13] while
Daye et al showed no significant differences between acne vulgaris and healthy control groups and no relation between IBS and acne severity [
12]. Both studies utilize small single centered cohorts, while our study’s population was much larger. Our results suggested a potential inverse association with acne vulgaris between IBS patients and healthy controls, while the reciprocal analysis showed no association. Nonetheless, our results add to this mixed body of evidence and underscore the need for further research with granular adjustments for confounding factors.
Psoriasis
There was a bilateral positive association between psoriasis and IBS. While a prior study has also identified the association between psoriasis and IBS [
14], it featured a small cohort of approximately 300 participants [
14]. Furthermore, this study identified a higher frequency of IBS in psoriasis patients with psoriatic arthritis compared to psoriasis patients without psoriatic arthritis [
14]. Importantly, few studies have assessed the prevalence of psoriasis in IBS patients compared to healthy controls, while our large-scale retrospective analysis helps address this gap.
Atopic Dermatitis and Urticaria
Allergic diseases, such as atopic dermatitis and urticaria have been postulated to be connected to IBS by shared pathogenesis of microbial dysbiosis and increased mast cell activation [
15]. Although a recent meta-analysis reports a significant association between atopic dermatitis and IBS [
16], our analysis revealed no significant relationship. This discrepancy may be due to significant variations in diagnostic criteria for IBS, population characteristics and high heterogeneity (I² = 78%) seen in their study [
16] whereas our study focused on adults aged 18-50 with clear exclusions. Together, these findings suggest that the strength of atopic dermatitis and IBS may vary by factors such as age and geographic location and highlights the need for additional standardized studies to clarify the association.
Our results showed a bilateral association between IBS and urticaria. Previous studies have also demonstrated a higher prevalence of IBS in urticaria patients compared to healthy controls [
17,
18]. However, the existing literature on the prevalence of urticaria in IBS patients is limited.
Hidradenitis Suppurativa
Our study suggested that hidradenitis suppurativa is more common in patients with IBS than those without. However, there was no difference in the occurrence of IBS in patients with hidradenitis suppurativa compared to healthy controls. In contrast,
Demirbas et al found that IBS occurred more frequently in hidradenitis suppurativa than those without [
19]. These results underscore the need for further research on this topic to clarify the association between hidradenitis suppurativa and IBS.
Rosacea
Our results suggested a bilateral positive association between IBS and rosacea. The current literature supports our findings with studies showing a significantly higher incidence [
20] and prevalence [
21,
22] of IBS in rosacea patients compared to healthy controls.
Jo et al, demonstrated that there was a 21% increased risk of developing IBS compared to controls [
20]. The team also noted that chronicity of rosacea appeared to further increase IBS risk [
20]. The association of rosacea is not limited to IBS; rosacea patients showed increased occurrences of other gastrointestinal diseases such as IBD, celiac disease, gastroesophageal reflux disease and Helicobacter pylori associated disease [
21,
22], suggesting a greater gastrointestinal involvement. However, there are limited studies examining the occurrence of rosacea in IBS compared to those without.
Vitiligo and Alopecia Areata
Vitiligo and alopecia areata, unlike the other dermatological conditions examined in the study, are autoimmune skin diseases which share overlapping pathogenesis [
23,
24,
25]. Current epidemiological data suggests a significant risk of co-occurrence bilaterally [
26,
27]. However, there is limited research on how IBS relates to both vitiligo and alopecia areata.
Our study suggested that vitiligo occurs less frequently in IBS patients than those without, yet the reciprocal analysis revealed no difference in IBS prevalence among vitiligo patients compared to healthy controls. While research examining the direct relationship between the two are limited, existing literature suggests that vitiligo patients may have an altered gut microbiome [
28,
29,
30,
31]. Despite this, our study suggests no clear association between vitiligo and IBS.
The results from our study showed no difference between the IBS patients and healthy controls on the prevalence of alopecia areata. However, in the reciprocal analysis, IBS appeared to occur less frequently in alopecia areata patients compared to those without. These results challenge prior research which demonstrate a strong bidirectional association between alopecia areata and IBS [
32]. Several methodological factors may account for this divergence. Our study excluded patients who have history of celiac, IBD and infectious gastroenteritis, conditions which share a substantial clinical overlap with IBS [
33]. In addition, we controlled for major depression and generalized anxiety disorder, psychiatric conditions that are robustly associated with both IBS and alopecia areata [
34,
35,
36,
37]. Without these design features, prior associations may have been inflated. Nonetheless, this inconsistency highlights the need for further research with clear diagnostic criteria and attention to psychiatric and other lifestyle confounders.
5. Conclusions
In our large-scale retrospective study, we examined the dermatological comorbidities of IBS patients compared to healthy controls, and performed a reciprocal analysis, a perspective which is underexamined. We identified three dermatological conditions, psoriasis, rosacea, urticaria, that show bilateral positive associations with IBS, suggesting a gut-skin link. Conversely, conditions like acne vulgaris and hidradenitis suppurativa, which showed asymmetric associations, should be interpreted cautiously and may be due to confounding factors. Atopic dermatitis showed no reproducible relationship with IBS in our study, despite prior meta-analysis reporting positive associations. This discrepancy may reflect differences in study design, population characteristics and diagnostic criteria. Autoimmune conditions such as vitiligo and alopecia areata also showed no consistent relationship, suggesting that the gut-skin axis may not equally influence all dermatologic diseases.
Limitations to our study include potential misclassification of International Classification of Diseases, Tenth Revision, Clinical Modification codes, selection bias and confounding variables such as diet, lifestyle and disease severity that are not adequately captured by large databases such as TriNetX.
Our findings add to the ongoing discourse on the connection between IBS, the gut microbiome and dermatology. Future research should explore biologic mechanisms underlying the gut-skin axis. Clinicians who treat IBS as well as those who treat dermatologic conditions, should be aware of this bidirectional association so appropriate care and/or referrals can be directed to optimize care.
Author Contributions
A.Y.L. was responsible for the conceptualization, methodology, analysis and writing/editing of this manuscript. N.M. and N.H. contributed to researching and writing of this manuscript. D.J. and D.P. provided conceptual guidance, supervised the study design and analysis. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Data Availability Statement
The data presented in this study are available upon request from the corresponding author due to institutional and ethical restrictions. The data was obtained from TriNetX, a global federated health research network and access is subject to data use agreements and institutional review.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Canavan C, West J, Card T. The epidemiology of irritable bowel syndrome. Clin Epidemiol. [CrossRef]
- Ford AC, Sperber AD, Corsetti M, Camilleri M. Irritable bowel syndrome. The Lancet, 1026. [CrossRef]
- Thye AY-K, Bah Y-R, Law JW-F, et al. Gut–skin axis: Unravelling the connection between the gut microbiome and psoriasis. Biomedicines, 1037. [CrossRef]
- Ryguła I, Pikiewicz W, Grabarek BO, Wójcik M, Kaminiów K. The role of the gut microbiome and microbial dysbiosis in common skin diseases. International Journal of Molecular Sciences, 1984. [CrossRef]
- De Pessemier B, Grine L, Debaere M, Maes A, Paetzold B, Callewaert C. Gut–skin axis: Current knowledge of the interrelationship between microbial dysbiosis and skin conditions. Microorganisms. [CrossRef]
- Potrykus M, Czaja-Stolc S, Stankiewicz M, Kaska Ł, Małgorzewicz S. Intestinal microbiota as a contributor to chronic inflammation and its potential modifications. Nutrients, 3839. [CrossRef]
- Wang L, Alammar N, Singh R, et al. Gut microbial dysbiosis in the irritable bowel syndrome: A systematic review and meta-analysis of case-control studies. J Acad Nutr Diet. [CrossRef]
- Yu Y, Dunaway S, Champer J, Kim J, Alikhan A. Changing our microbiome: Probiotics in dermatology. Br J Dermatol. [CrossRef]
- He R, Zhao S, Cui M, et al. Cutaneous manifestations of inflammatory bowel disease: Basic characteristics, therapy, and potential pathophysiological associations. Frontiers in Immunology. [CrossRef]
- Antonelli E, Bassotti G, Tramontana M, et al. Dermatological manifestations in inflammatory bowel diseases. Journal of Clinical Medicine. [CrossRef]
- Jimenez-Sanchez M, Celiberto LS, Yang H, Sham HP, Vallance BA. The gut-skin axis: A bi-directional, microbiota-driven relationship with therapeutic potential. Gut Microbes. [CrossRef]
- Daye M, Cihan FG, Işık B, Hafızoğlu B. Evaluation of bowel habits in patients with acne vulgaris. Int J Clin Pract, 1490. [CrossRef]
- Demirbaş A, Elmas Ö F. The relationship between acne vulgaris and irritable bowel syndrome: A preliminary study. J Cosmet Dermatol. [CrossRef]
- Unal G, Marakoglu K, Eryilmaz M, Unal M, Kulahci O. Skin and gut: Psoriasis and irritable bowel syndrome. Is there an association? Annals of Medical Research. [CrossRef]
- Loo EXL, Wang Y, Siah KTH. Association between irritable bowel syndrome and allergic diseases: To make a case for aeroallergen. Int Arch Allergy Immunol. [CrossRef]
- Lin DK, Chang HC. Association of atopic dermatitis or allergic rhinitis with irritable bowel syndrome: A systematic review and meta-analysis. Allergy, 2025. [CrossRef]
- Fang ZY, Zhang HT, Lu C, Lu QM, Yu CH, Wang HY. Association between allergic diseases and irritable bowel syndrome: A retrospective study. Int Arch Allergy Immunol. [CrossRef]
- Shalom G, Magen E, Babaev M, et al. Chronic urticaria and irritable bowel syndrome: A cross-sectional study of 11 271 patients. Br J Dermatol. [CrossRef]
- Demi̇rbaş A, Elmas ÖF, Eker Hy, et al. The relationship between hidradenitis suppurativa and irritable bowel syndrome: A cross-sectional study. Turkish Journal of Medical Sciences. [CrossRef]
- Jo YW, Min JH, Kwon JW, Her Y. Rosacea and its potential role in the development of irritable bowel syndrome: Insights from the korean national health insurance service-national sample cohort. J Korean Med Sci, e: 2025;40(21), 2025. [CrossRef]
- Egeberg A, Weinstock LB, Thyssen EP, Gislason GH, Thyssen JP. Rosacea and gastrointestinal disorders: A population-based cohort study. Br J Dermatol. [CrossRef]
- Piontkowski AJ, Sharma D, Ungar B. Rosacea and gastrointestinal diseases: A case-control study in the all of us database. Dermatology. [CrossRef]
- Harris, JE. Vitiligo and alopecia areata: Apples and oranges? Exp Dermatol. [CrossRef]
- Rork JF, Rashighi M, Harris JE. Understanding autoimmunity of vitiligo and alopecia areata. Curr Opin Pediatr. [CrossRef]
- Yamaguchi HL, Yamaguchi Y, Peeva E. Pathogenesis of alopecia areata and vitiligo: Commonalities and differences. Int J Mol Sci, 2024. [CrossRef]
- Krajewski PK, Jastrząb B, Szepietowski JC, Jankowska-Konsur A, Saceda Corralo D. Immune-mediated disorders in patients with alopecia areata: Systematic review and meta-analysis. Int J Dermatol, 2025. [CrossRef]
- Lee JH, Ju HJ, Seo JM, et al. Comorbidities in patients with vitiligo: A systematic review and meta-analysis. J Invest Dermatol, 20 May. [CrossRef]
- Bzioueche H, Simonyté Sjödin K, West CE, et al. Analysis of matched skin and gut microbiome of patients with vitiligo reveals deep skin dysbiosis: Link with mitochondrial and immune changes. J Invest Dermatol, 2280. [CrossRef]
- Ni Q, Ye Z, Wang Y, et al. Gut microbial dysbiosis and plasma metabolic profile in individuals with vitiligo. Front Microbiol, 5922. [CrossRef]
- Ni Q, Xia L, Huang Y, et al. Gut microbiota dysbiosis orchestrates vitiligo-related oxidative stress through the metabolite hippuric acid. Microbiome, 6 May. [CrossRef]
- Yuan C, Liu L, Zeng D, Yuan J, Guo L, Zhang J. Exploring the influence of gut microbiota metabolites on vitiligo through the gut-skin axis. Front Microbiol, 1566. [CrossRef]
- Dai YX, Tai YH, Chang YT, Chen TJ, Chen MH. Bidirectional association between alopecia areata and irritable bowel syndrome: A nationwide population-based cohort study. Australas J Dermatol, 20 May. [CrossRef]
- Aziz I, Simrén M. The overlap between irritable bowel syndrome and organic gastrointestinal diseases. Lancet Gastroenterol Hepatol. [CrossRef]
- Midenfjord I, Polster A, Sjövall H, Törnblom H, Simrén M. Anxiety and depression in irritable bowel syndrome: Exploring the interaction with other symptoms and pathophysiology using multivariate analyses. Neurogastroenterol Motil, 1361. [CrossRef]
- Staudacher HM, Mikocka-Walus A, Ford AC. Common mental disorders in irritable bowel syndrome: Pathophysiology, management, and considerations for future randomised controlled trials. Lancet Gastroenterol Hepatol, 20 May. [CrossRef]
- Zamani M, Alizadeh-Tabari S, Zamani V. Systematic review with meta-analysis: The prevalence of anxiety and depression in patients with irritable bowel syndrome. Aliment Pharmacol Ther. [CrossRef]
- Vallerand IA, Lewinson RT, Parsons LM, et al. Assessment of a bidirectional association between major depressive disorder and alopecia areata. JAMA Dermatology. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).