Submitted:
10 October 2025
Posted:
14 October 2025
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Methodology
2.1. Service Development and Implementation
2.2. Study Design
2.3. Data Collection Tool
- Describing experience with shared decision-making.
- Information pharmacists provided about the service and the role of urinalysis point-of-care testing.
- Advice pharmacists provided on managing current symptoms, safety netting and preventing future infections.
- Level of information pharmacists provided in relation to antimicrobial stewardship.
- Reported future healthcare behaviour.
2.4. Population and Sampling
2.5. Recruitment
2.6. Data Analysis
- The patient experience of shared decision-making in the service.
- The patient experience of information pharmacists provided about the service and the role of urinalysis point-of-care testing.
- The patient experience of advice pharmacists provided on managing current symptoms, safety netting and preventing future infection.
- The level of information pharmacists provided in relation to antimicrobial stewardship.
- The impact of patient experience on reported future healthcare behaviour.
3. Results
3.1. Patient Experience with the Service and its Delivery
3.2. Health-Seeking Behaviour

3.3. Free-Text Comments
4. Discussion
4.1. Strengths and limitations
5. Conclusions
References
- European Association of Urology. Urological Infections. Available online: https://uroweb.org/guidelines/urological-infections (accessed 24 September 2025).
- National Institute for Health and Clinical Excellence. Common infections: urinary tract infection Data focused commentary: management of acute uncomplicated urinary tract infection. 2009. Available online: http://www.npc.nhs.uk/therapeutics/common_infections/uti/resources/dfc_common_infect_uti.pdf (accessed 22 July 2025).
- Welsh Pharmaceutical Committee. Pharmacy: Delivering a Healthier Wales. 2019. Available online: https://www.rpharms.com/Portals/0/RPS%20document%20library/Open%20access/Wales/Pharmacy%20Delivering%20A%20Healthier%20Wales%20Summary%20Guide.pdf?ver=iavNxXa-P_IL3d1KpbznTQ%3d%3d (accessed 22 July 2025).
- Welsh Medicines Advice Centre. Common Ailments Service - Information for Members of the Public. 2025. Available online: https://www.wmic.wales.nhs.uk/common-ailments-service/ (accessed online 01 October 2025).
- White, J.; James, R.; Kennerley, Z. Bevan Commission. HDUHB Community Pharmacy Urinary Tract Infections Testing and Treatment Service. 2022. Available online: https://bevancommission.org/hduhb-community-pharmacy-uti-urinary-tract-infections-testing-and-treatment-service/ (accessed 22 July 2025).
- UK Health Security Agency and NHS England. Urinary tract infection: diagnostic tools for primary care. 2025. Available online: https://www.gov.uk/government/publications/urinary-tract-infection-diagnosis (accessed 22 July 2025).
- All Wales Medicines Strategy Group. All Wales Common Ailments Service Formulary. 2025. Available online: https://awttc.nhs.wales/files/guidelines-and-pils/all-wales-common-ailments-service-formulary-apr-2025-pdf/ (accessed 24 September 2025).
- Royal Pharmaceutical Society. The pharmacy contribution to antimicrobial stewardship. 2017. Available online: https://www.rpharms.com/Portals/0/RPS%20document%20library/Open%20access/Policy/AMS%20policy.pdf (accessed 15 July 2025).
- Community pharmacy Scotland. NHS Pharmacy First Scotland Service. 2024. Available online: https://static1.squarespace.com/static/6465418b5e15221808eb56ea/t/67d062a6f003ea30bd458230/1741709990897/24.07.24_Pharmacy_First_FAQs_Flowchart_and_Scenarios_V3.pdf (accessed 22 July 2025).
- NHS England. Pharmacy First. Available online: https://www.england.nhs.uk/primary-care/pharmacy/pharmacy-services/pharmacy-first/#:~:text=The%20benefits%20of%20Pharmacy%20First&text=It%20includes%20the%20supply%20of,issues%20before%20they%20get%20worse. (accessed 22 July 2025).
- Department of Health Northern Ireland. Local pharmacies can help with Urinary Tract Infections. 2023. Available online: https://www.health-ni.gov.uk/news/local-pharmacies-can-help-urinary-tract-infections#:~:text=The%20service%20is%20part%20of,or%20large%20quantities%20of%20urine (accessed 24 September 2025).
- Hind, C. NHS Grampian Project: Treating uncomplicated lower urinary tract infection in community pharmacy. Pharm J. 2018. [CrossRef]
- Stewart, F.; Caldwell, G.; Cassells, K.; Burton, J.; Watson, A. Building capacity in primary care: the implementation of a novel ‘Pharmacy First’ scheme for the management of UTI, impetigo and COPD exacerbation. Prim Health Care Res Dev. 2018. 19. 531-541. https://doi:10.1017/S1463423617000925.
- Thornley, T.; Kirkdale, C.L.; Beech, E.; Howard, P.; Wilson, P. Evaluation of a community pharmacy-led test-and-treat service for women with uncomplicated lower urinary tract infection in England. JAC-Antimicrobial Resistance. 2020. 2. [CrossRef]
- Peiffer-Smadja, N.; Allison, R.; Jones, L.F.; Holmes, A.; Patel, P.; Lecky, D.M.; Ahmad, R.; McNulty, C.A.M. Preventing and Managing Urinary Tract Infections: Enhancing the Role of Community Pharmacists-A Mixed Methods Study. Antibiotics (Basel). 2020. 9. 583. [CrossRef]
- Lee, F.; Motta, M.; Wilcock, M. Evaluation of a community pharmacy service for uncomplicated Urinary tract infection. Pharm J. 2021. [CrossRef]
- Budden, M.; Gilbertson, D.; Chung, S.; Benrimoj, S.I.; Mardones, F.; Dineen-Griffin, S. Clinical management protocols for community pharmacist-led management of urinary tract infections: a review of the grey literature and quality appraisal. Int J Clin Pharm. 2024. 46. 1256–1267. [CrossRef]
- Nissen, L.; Lau, E.; Spinks, J. The management of urinary tract infections by community pharmacists: A state-wide trial : Urinary Tract Infection Pharmacy Pilot – Queensland. 2023. Available online: https://eprints.qut.edu.au/239310/8/Approved_UTI_Pilot_Final_Report_April_2023_eprint_FINALv1.1.pdf (accessed 24 September 2025).
- Pharmaceutical Society of New Zealand. Pharmacy Healthcare Services. Urinary Tract Infections. Available online: https://www.psnz.org.nz/healthservices/utis (accessed 22 July 2025).
- Stämpfli, D.; Winkler, B.A.; Vilei, S.B.; Burden, A.M. Assessment of minor health disorders with decision tree-based triage in community pharmacies. Res Social Adm Pharm. 2022. 18. 2867-2873. [CrossRef]
- Virginia Board of Pharmacy. Pharmacist Protocol for Testing and Initiating Treatment for Suspected Acute Uncomplicated Lower Urinary Tract Infection in Women. 2023. Available online : https://www.dhp.virginia.gov/media/dhpweb/docs/pharmacy/protocols/UTICombined.pdf. (accessed 20 March 2024).
- Beahm, N.P.; Smyth, D.J.; Tsuyuki, R.T. Outcomes of urinary tract infection management by pharmacists (RxOUTMAP): A Study of Pharmacist Prescribing and care in patients with uncomplicated urinary tract infections in the community. Canadian Pharmacists Journal/Revue des Pharmaciens du Canada. 151. 305–314. [CrossRef]
- Swart, A.; Benrimoj, S.I.; Dineen-Griffin, S. The clinical and economic evidence of the management of urinary tract infections by community pharmacists in women aged 16 to 65 years: a systematic review. Int J Clin Pharm. 2024. 46. 574-589. [CrossRef]
- Hall, G.; Cork, T.; White, S.; Berry, H.; Smith, L. Evaluation of a new patient consultation initiative in community pharmacy for ear, nose and throat and eye conditions. BMC Health Serv Res. 2019. 3. 285. [CrossRef]
- Hindi, A.M.K.; Schafheutle, E.I.; Jacobs, S. Patient and public perspectives of community pharmacies in the United Kingdom: A systematic review. Health Expect. 2018. 21. 409-428. [CrossRef]
- Seston, E.M.; Magola, E.; Bower, P.; Chen, L.C.; Jacobs, S.; Lewis, P.J.; Steinke, D.; Willis, S.C.; Schafheutle, E.I. Supporting patients with long-term conditions in the community: Evaluation of the Greater Manchester Community Pharmacy Care Plan Service. Health Soc Care Community. 2020. 28. 1671-1687. [CrossRef]
- Chirewa, B.; Wakhisi, A. Emergency hormonal contraceptive service provision via community pharmacies in the UK: a systematic review of pharmacists’ and young women’s views, perspectives and experiences. Perspectives in Public Health. 2019. 140. 108-116. [CrossRef]
- Mantzourani, E.; Cannings-John, R.; Evans, A.; Ahmed, H.; Meudell, A.; Hill, I.; Williams, E.; Way, C.; Hood, K.; Legay, B.; Houldcroft, L.; Deslandes, R. Understanding the impact of a new pharmacy sore throat test and treat service on patient experience: A survey study. Res Social Adm Pharm. 2021. 17. 969-977. [CrossRef]
- Gilmore, K.J.; Corazza, I.; Coletta, L.; Allin, S. The uses of Patient Reported Experience Measures in health systems: A systematic narrative review. Health Policy. 2023. 128. 1-10. [CrossRef]
- NHS Wales. Clinical Community Pharmacy Service. 2025. Available online : https://nwssp.nhs.wales/ourservices/primary-care-services/primary-care-services-documents/ccps-documents/ccps-service-specification-v24-wef-01102025/ (accessed 22 July 2025).
- Community Pharmacy Wales. HEIW Re-accreditation for Services. 2025. Available online: https://cpwales.org.uk/training/pharmacy-technician-support/reaccreditation-process-for-services/ (accessed 22 July 2025).
- Guba, E. and Lincoln, Y. 1994. Competing paradigms in qualitative research. 1st ed. California: Sage, pp. 105-113.
- IBM Corp. IBM SPSS Statistics for Windows, Version 29.0. 2023. Armonk, NY: IBM Corp.
- Welsh Government. A Healthier Wales: our Plan for Health and Social Care. 2021. Available online : https://www.gov.wales/sites/default/files/publications/2021-09/a-healthier-wales-our-plan-for-health-and-social-care.pdf (accessed 1 August 2025).
- NHS England. Delivery plan for recovering access to primary care. 2023. Available online : https://www.england.nhs.uk/long-read/delivery-plan-for-recovering-access-to-primary-care-2/ (accessed 22 July 2025).
- Lecky, D.M.; Howdle, J.; Butler, C.C.; McNulty, C.A.M. Optimising management of UTIs in primary care: a qualitative study of patient and GP perspectives to inform the development of an evidence-based, shared decision-making resource. Br J Gen Prac. 2020. 70. e330-e338. [CrossRef]
- Booth JL, Mullen AB, Thomson DAM et al. Antibiotic treatment of urinary tract infection by community pharmacists: a cross-sectional study. Br J Gen Prac 2013;63(609):e244–e249. [CrossRef]
- Jones, L.F.; Owens, R.; Sallis, A.; Ashiru-Oredope, D.; Thornley, T.; Francis, N.; Butler, C.; McNulty, C.A.M. Qualitative study using interviews and focus groups to explore the current and potential for antimicrobial stewardship in community pharmacy informed by the Theoretical Domains Framework. BMJ Open. 2018. 8. e025101. http://dx.doi.org/10.1136/bmjopen-2018-025101.
- UK Parliament. Health and Social Care Committee. Pharmacy. 2024. Available online: https://publications.parliament.uk/pa/cm5804/cmselect/cmhealth/140/report.html#footnote-227 (accessed online 24 September 2025).
- Community Pharmacy England. Pharmacy Pressures Survey. 2024. Available online: https://cpe.org.uk/wp-content/uploads/2024/10/Pharmacy-Pressures-Survey-2024-Staffing-and-Morale-Report-Final-Oct-2024.pdf (accessed 1 August 2025).
- Zied Abozied, E.; Munford, L.A.; Copeland, A.; Kasim, A.; Husband, A.; Bambra, C.; Todd, A. The Positive Pharmacy Care Law revisited: an area-level analysis of the relationship between community pharmacy distribution, urbanicity and deprivation in England. BMJ Open. 2025. 15. e095540. [CrossRef]
- Welsh Government. Written Statement: Community Pharmacy Contractual Framework Agreement 2024-25. 2024. Available online : https://www.gov.wales/written-statement-community-pharmacy-contractual-framework-cpcf-agreement-2024-25 (accessed 24 September 2025).
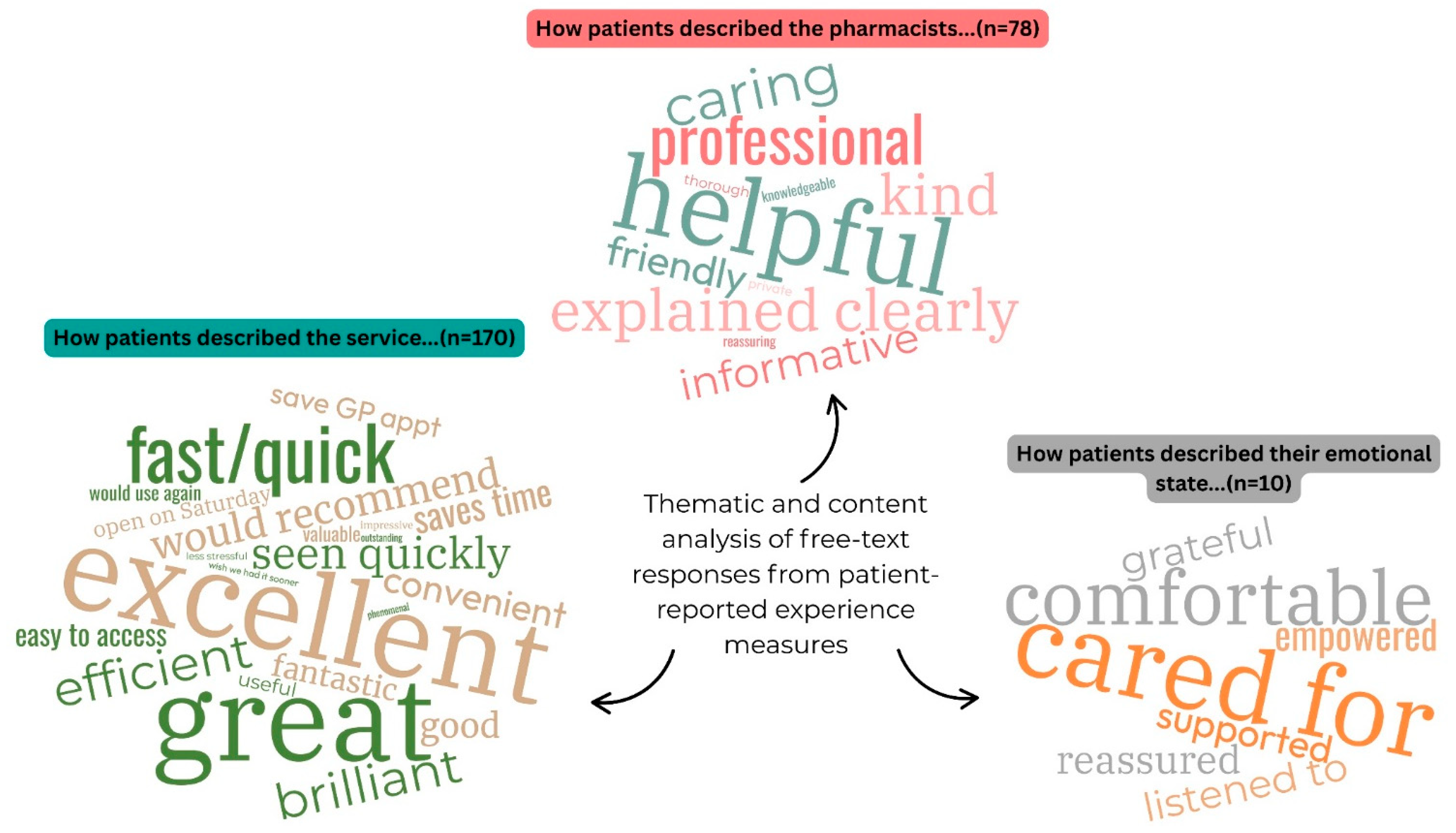
| Theme 1: How patients described the service |
| “Great service provided by the local pharmacist, after two failed attempts to contact my GP from 8am I was told I was on a call back list for 6pm. Due to my worsening symptoms I chose to access support from my nearest pharmacy they were professional and very efficient.” S89 |
| “Efficient service, …… would not hesitate to recommend this service, thank you very much, I would have been waiting 2 days for a doctors [sic] appointment.” S124 |
| “This service is excellent and speeds up the progress of being diagnosed as I normally have to wait weeks to be seen by a doctor. I believe this service to be invaluable to all that use it.” S14 |
| “Excellent & thorough service. Far easier than GP surgery.” S123 |
| “The service I received was phenomenal!” S23 |
| Theme 2: How patients described the pharmacist/staff |
| “The pharmacist at [redacted] pharmacy (I think his name was [redacted]?) went above and beyond and should be commended for his professionalism.” S23 |
| “Staff were very professional. The pharmacist took me to a side room to have privacy to discuss my condition.” S35 |
| “I am so glad my GP told me to go to the pharmacy, I was seen within 10 minutes and the whole thing was super friendly and helpful. Pharmacist was so professional, I did not feel embarrassed to talk about it at all.” S79 |
| “Absolutely amazing service, just called the pharmacy, they gave me a same day appointment and I was dealt with in a private and professional manner, the pharmacist explained everything very clearly and was precise. An excitement [sic] service which I highly recommend.” S142 |
| “Pharmacist explained why I don’t need antibiotics today, thanks for reassuring me” S51 |
| Theme 3: How patients described their feelings |
| “The pharmacist was super friendly and super helpful and I felt really supported.” S26 |
| “This is a wonderful service. I felt empowered. Resolving this problem and receiving advice from Pharmacist on why my symptoms were not a UTI allowed me to get an appointment with my GP to follow up my symptoms. Thank you” S18 |
| “Really grateful for today, thanks!” S43 |
| “I thought the service was excellent. I had taken a urine sample to the doctors [sic] surgery, but it wouldn’t be done until later that day. It was a Friday and I was going away that weekend. I was really uncomfortable and in pain. Seeing the pharmacist helped a lot and having the antibiotics made my weekend a lot more comfortable. When I was given antibiotics and listened to, I cried with relief. I would definitely recommend and would use this service again. Knowing that this is available when the doctors [sic] surgery is closed, is a relief. Thank you for providing this service. Please continue with this service as I will recommend it to others.” S71 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





