Submitted:
01 October 2025
Posted:
02 October 2025
You are already at the latest version
Abstract
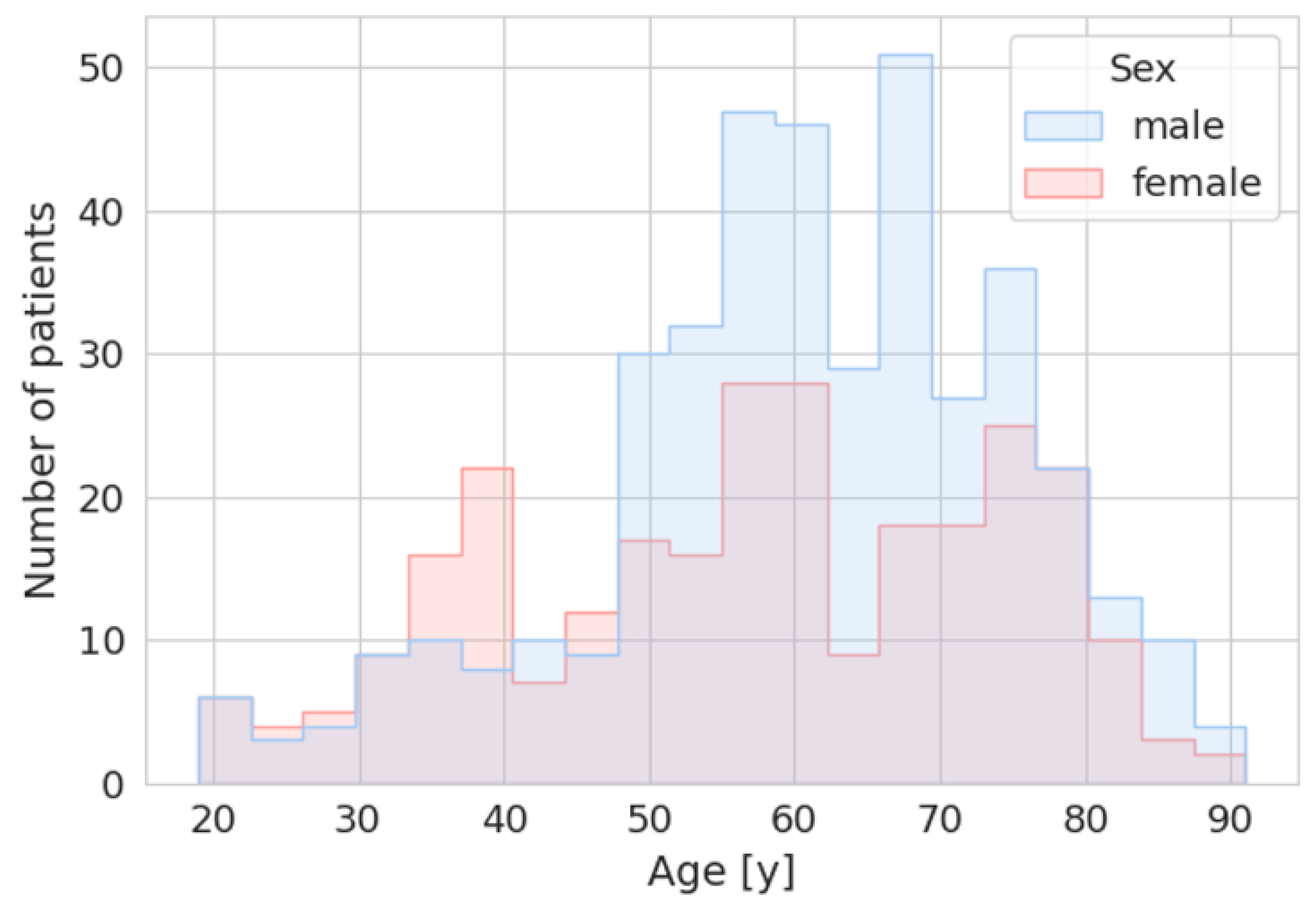
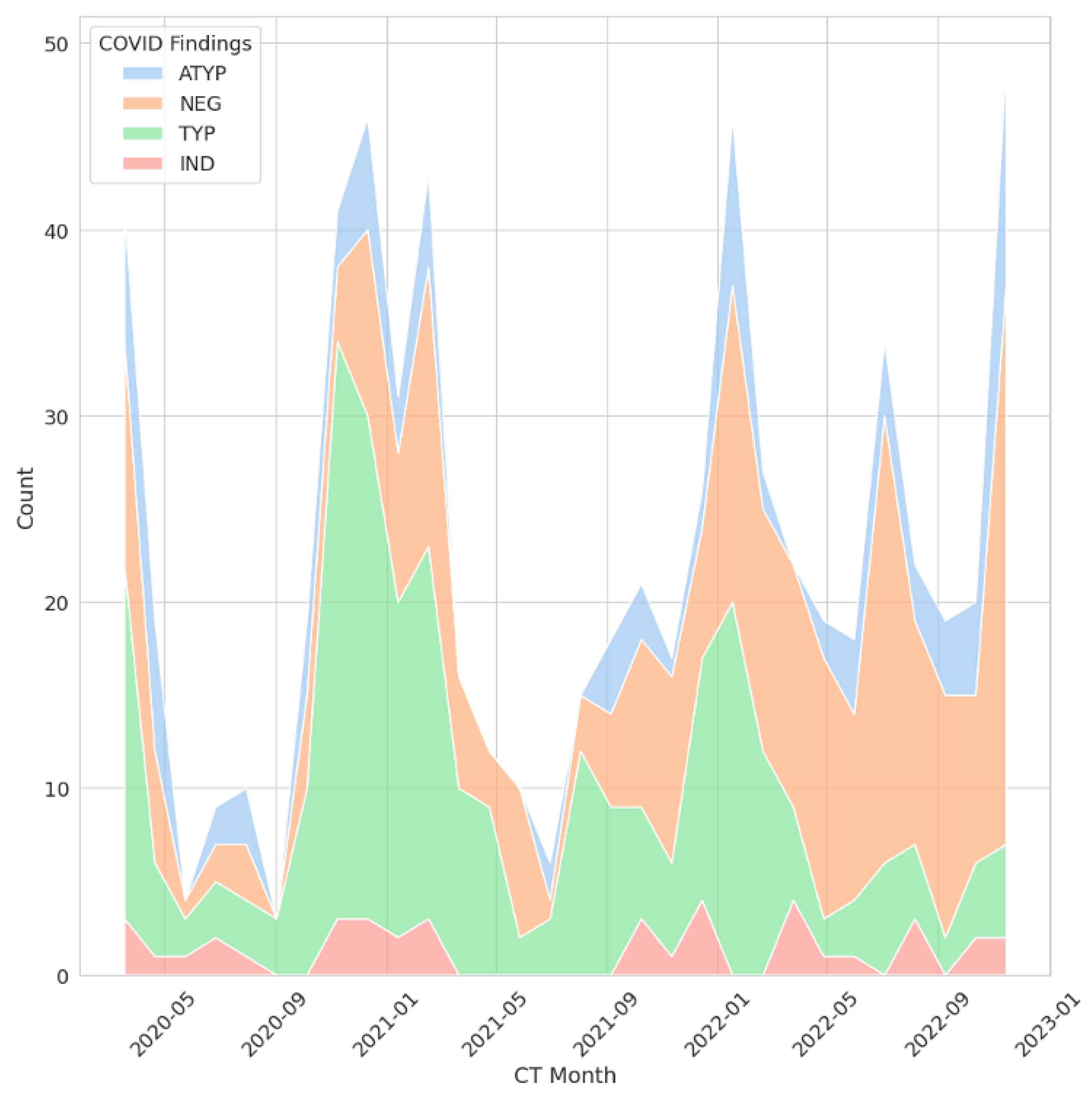
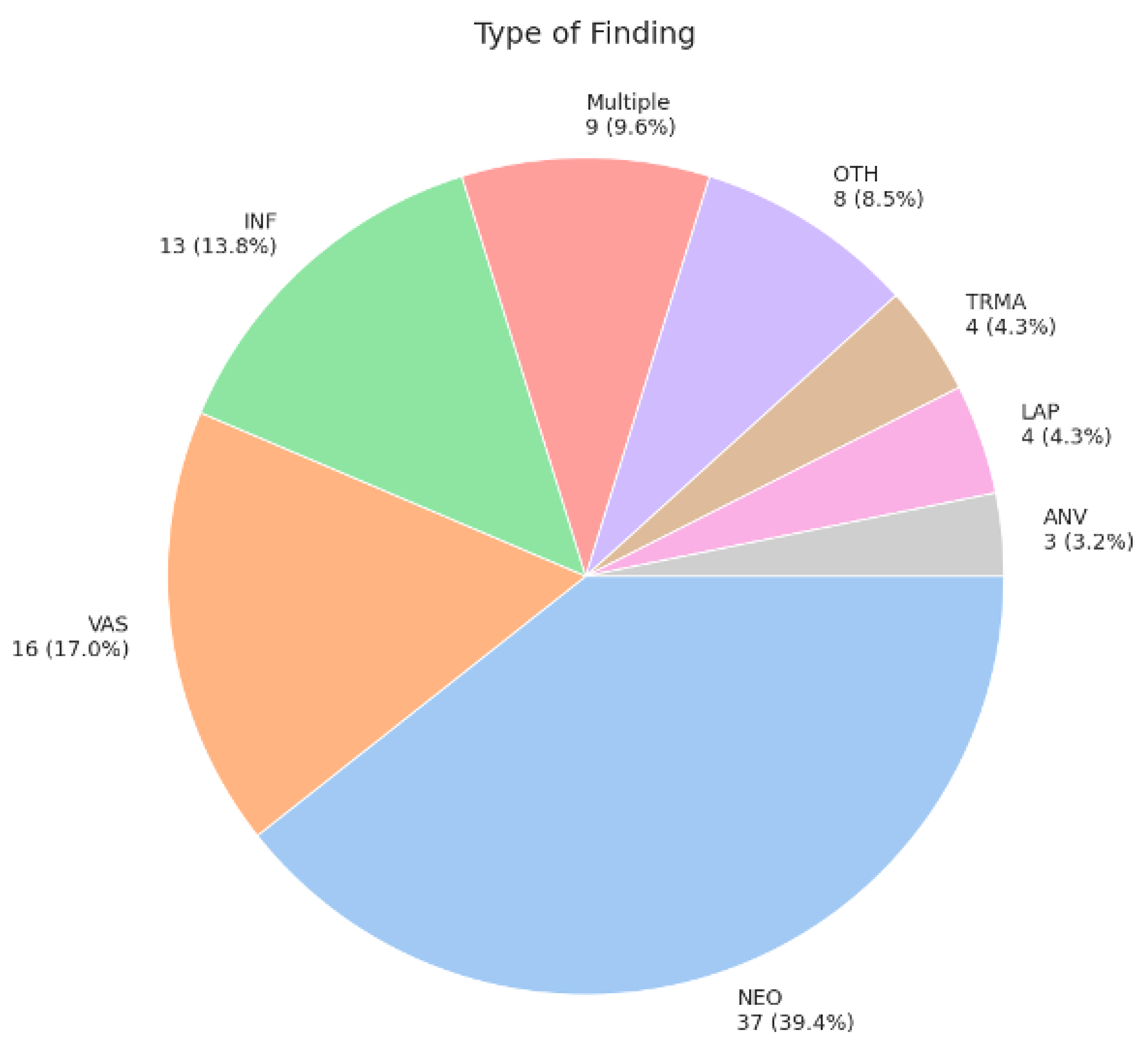
Background/Objectives: To evaluate the prevalence of incidental findings in thoracic computed tomography (CT) performed because of COVID-19 and their potential impact on patient management. Methods: This retrospective analysis included 683 CT scans from 327 patients who underwent CT imaging of the thorax with or without the application of intravenous contrast-agents because of the primary indication of COVID-19. Radiological findings were categorized according to the COVID-19 Pneumonia Imaging Classification by 4 independent readers. Incidental findings were categorized according to a scale ranging from 0 (no patient impairment) to 3b (severe permanent impairment. Results: In the 683 CT-scans, typical COVID-19 findings were present in 273 scans (40.0%), atypical signs in 97 (14.2%), indeterminate findings in 40 (5.9%), and no signs of COVID-19 in 273 (40.0%). Incidental findings were reported in 93 out of 683 cases (13.6%), of which 63 (67.0%) were classified as category 0, 12 (12.8%) as category 1, 9 (9.6%) as category 2a, none (0.0%) as category 2b, 5 (5.3%) as category 3a, and 5 (5.3%) as category 3b. Conclusions: CT scans of the thorax for COVID-19 show a substantial proportion of incidental findings that require further investigation.
Keywords:
1. Introduction
2. Materials and Methods
2.1. Study Group
2.2. Imaging
2.3. Radiological Classification of the Imaging Findings
2.3.1. Classification
-
Typical appearance:
- ▪
- Peripheral, bilateral ground-glass opacities (GGO) with or without consolidation or visible intralobular lines ("crazy paving").
-
Indeterminate appearance:
- ▪
- Includes one or more of the following features:
- ▪
- Multifocal GGO with a rounded morphology, with or without consolidation or visible intralobular lines ("crazy paving").
- ▪
- Reverse halo sign or other patterns suggestive of POP.
- ▪
- The absence of typical features, with the presence of multifocal, diffuse, perihilar, or unilateral GGO with or without consolidation lacking a specific distribution. Nonrounded or non-peripheral GGO, or very few small GGO with a non-rounded and non-peripheral distribution, are also included.
- Atypical appearance:
- Negative for pneumonia:
2.3.2. Relevance
2.4. Statistics
3. Results
3.1. Use of a Contrast Agent
3.2. COVID-Typical Findings
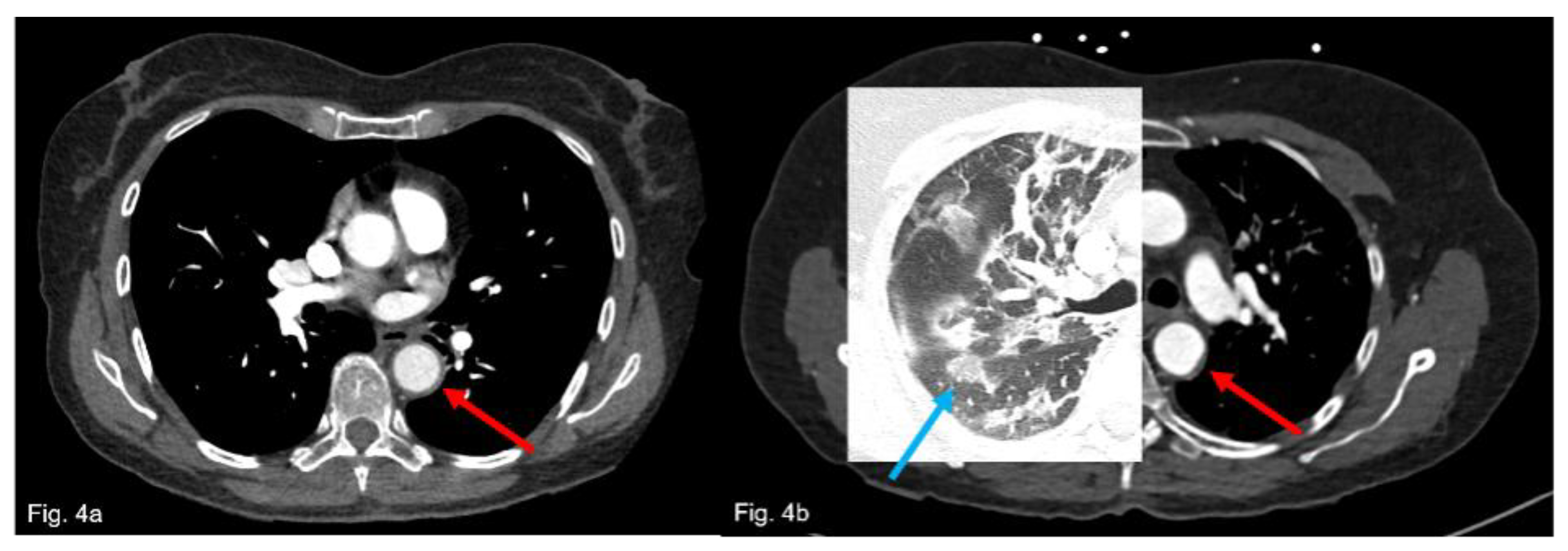
3.3. Incidental Findings
3.4. Follow-Up or Further Clarification Recommendations
3.5. Statistical Evaluation of Imaging Findings Among the Subgroups
4. Discussion
4.1. Limitations
- The absence of direct insight into how clinicians acted upon reported incidental findings, relying solely on subsequent medical documentation. Thus, the extent to which incidental findings were addressed remains uncertain.
- The single-center-design of our study, therefore the applicability of our findings to other institutions or healthcare facilities may be limited.
- Potential reporting bias: Even though the radiologists were unaware of the study participation due to the retrospective design, a potential reporting bias regarding incidental findings cannot be excluded, as the pandemic-related high workload might have affected reporting behavior.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Cucinotta D, Vanelli M. WHO Declares COVID-19 a Pandemic. Acta Biomed. 2020, 91, 157–60. [CrossRef] [PubMed] [PubMed Central]
- Ochani R, Asad A, Yasmin F, Shaikh S, Khalid H, Batra S, et al. COVID-19 pandemic: from origins to outcomes. A comprehensive review of viral pathogenesis, clinical manifestations, diagnostic evaluation, and management. Infez Med. 2021, 29, 20–36. [PubMed]
- Sanidas E, Grassos C, Papadopoulos D, Velliou M, Barbetseas J. Pulmonary Embolism Prophylaxis in Patients With COVID-19: An Emerging Issue. Heart Lung Circ. 2021, 30, 1435–41. [CrossRef] [PubMed] [PubMed Central]
- Mossa-Basha M, Meltzer CC, Kim DC, Tuite MJ, Kolli KP, Tan BS. Radiology Department Preparedness for COVID-19:. Radiology. 2020, 296, E106–E12. [CrossRef] [PubMed] [PubMed Central]
- Darwish HS, Habash MY, Habash WY. Chest computed tomography imaging features in patients with coronavirus disease 2019 (COVID-19). J Int Med Res. 2021, 49, 3000605211010631. [CrossRef] [PubMed] [PubMed Central]
- Alsharif W, Qurashi A. Effectiveness of COVID-19 diagnosis and management tools: A review. Radiography (Lond). 2021, 27, 682–7. [CrossRef] [PubMed] [PubMed Central]
- Battegay, E. Differenzialdiagnose innerer Krankheiten: vom Symptom zur Diagnose. 22., vollständig überarbeitete und erweiterte Auflage. ed. Stuttgart: Georg Thieme Verlag.
- Zhao W, Zhong Z, Xie X, Yu Q, Liu J. Relation Between Chest CT Findings and Clinical Conditions of Coronavirus Disease (COVID-19) Pneumonia: A Multicenter Study. AJR Am J Roentgenol. 2020, 214, 1072–7. [CrossRef] [PubMed]
- Salehi S, Abedi A, Balakrishnan S, Gholamrezanezhad A. Coronavirus Disease 2019 (COVID-19): A Systematic Review of Imaging Findings in 919 Patients. AJR Am J Roentgenol. 2020, 215, 87–93. [CrossRef] [PubMed]
- Caruso D, Zerunian M, Polici M, Pucciarelli F, Polidori T, Rucci C, et al. Chest CT Features of COVID-19 in Rome, Italy. Radiology. 2020, 296, E79–E85. [CrossRef] [PubMed] [PubMed Central]
- Ai T, Yang Z, Hou H, Zhan C, Chen C, Lv W, et al. Correlation of Chest CT and RT-PCR Testing for Coronavirus Disease 2019 (COVID-19) in China: A Report of 1014 Cases. Radiology. 2020, 296, E32–E40. [CrossRef] [PubMed] [PubMed Central]
- Tailor TD, Tong BC, Gao J, Choudhury KR, Rubin GD. A Geospatial Analysis of Factors Affecting Access to CT Facilities: Implications for Lung Cancer Screening. J Am Coll Radiol. 2019, 16, 1663–8. [CrossRef] [PubMed]
- Li Y, Xia L. Coronavirus Disease 2019 (COVID-19): Role of Chest CT in Diagnosis and Management. AJR Am J Roentgenol. 2020, 214, 1280–6. [Google Scholar] [CrossRef] [PubMed]
- ACR. ACR Recommendations for the use of Chest Radiography and Computed Tomography (CT) for Suspected COVID-19 Infection. American College of Radiology. [cited 2025 June 6]. Available online: https://www.acr.org/Advocacy/Position-Statements/Recommendations-for-Chest-Radiography-and-CT-for-Suspected-COVID19-Infection.
- Helms J, Tacquard C, Severac F, Leonard-Lorant I, Ohana M, Delabranche X, et al. High risk of thrombosis in patients with severe SARS-CoV-2 infection: a multicenter prospective cohort study. Intensive Care Med. 2020, 46, 1089–98. [CrossRef] [PubMed] [PubMed Central]
- Klok FA, Kruip MJHA, van der Meer NJM, Arbous MS, Gommers DAMP, Kant KM, et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020, 191, 145–7. [CrossRef] [PubMed] [PubMed Central]
- Llitjos JF, Leclerc M, Chochois C, Monsallier JM, Ramakers M, Auvray M, et al. High incidence of venous thromboembolic events in anticoagulated severe COVID-19 patients. J Thromb Haemost. 2020, 18, 1743–6. [CrossRef] [PubMed] [PubMed Central]
- Trunz LM, Lee P, Lange SM, Pomeranz CL, Needleman L, Ford RW, et al. Imaging approach to COVID-19 associated pulmonary embolism. Int J Clin Pract. 2021, 75, e14340. [CrossRef] [PubMed] [PubMed Central]
- Tugba Akinci D'Antonoli, Marcio A. B. C. Rockenbach, Vera Cruz e Silva, Merel Huisman, Elmar Kotter, Emmanouil Koltsakis, et al. ESR Modern Radiology eBook. European Society of Radiology2023.
- Frank L, Quint LE. Chest CT incidentalomas: thyroid lesions, enlarged mediastinal lymph nodes, and lung nodules. Cancer Imaging. 2012, 12, 41–8. [CrossRef] [PubMed] [PubMed Central]
- Helvacı BC, Ozdemir D, Turan K, Keskin C, İmga NN, Dirikoc A, et al. Incidental thyroid nodules on COVID-19-related thoracic tomography scans: a giant cohort. Hormones (Athens). 2024, 23, 227–33. [CrossRef] [PubMed]
- Valluri S, Lakshmi HN, Sunkavalli C. Incidental Findings in CT Scans on Screening for COVID-19. Indian J Surg Oncol. 2023, 14, 318–23. [CrossRef] [PubMed] [PubMed Central]
- de Magalhães LJT, Rocha VG, de Almeida TC, de Albuquerque Albuquerque EV. Prevalence of reported incidental adrenal findings in chest computerized tomography scans performed during the COVID-19 pandemic in a single center in Northeast Brazil. Arch Endocrinol Metab. 2023, 67, 251–5. [CrossRef] [PubMed] [PubMed Central]
- Simpson S, Kay FU, Abbara S, Bhalla S, Chung JH, Chung M, et al. Radiological Society of North America Expert Consensus Statement on Reporting Chest CT Findings Related to COVID-19. Endorsed by the Society of Thoracic Radiology, the American College of Radiology, and RSNA - Secondary Publication. J Thorac Imaging. 2020, 35, 219–27. [CrossRef] [PubMed] [PubMed Central]
- Remer LF, Lee CI, Picado O, Lew JI. Sex Differences in Papillary Thyroid Cancer. J Surg Res. 2022, 271, 163–70. [CrossRef] [PubMed]
- Wünnemann F, Rehnitz C, Weber MA. [Incidental findings in musculoskeletal radiology]. Radiologe. 2017, 57, 286–95. [CrossRef] [PubMed]
- Leitman, BS. Comment on the Avoidance of Reporting Incidental Findings. J Am Coll Radiol. 2018, 15, 7. [Google Scholar] [CrossRef] [PubMed]
- McCollough CH, Leng S, Yu L, Fletcher JG. Dual- and Multi-Energy CT: Principles, Technical Approaches, and Clinical Applications. Radiology. 2015, 276, 637–53. [CrossRef] [PubMed] [PubMed Central]
- NCI. Age and Cancer Risk. National Cancer Institute. [cited 2025 June 8]. Available online: https://www.cancer.gov/about-cancer/causes-prevention/risk/age#:~:text=Age%20and%20Cancer%20Risk,-Advancing%20age%20is&text=The%20incidence%20rates%20for%20cancer,groups%2060%20years%20and%20older.
- Erbil D, Onal EM, Demirel C, Sag AA, Dagel T, Afsar B, et al. Can Incidental Vascular Calcifications at Mammography be Used as a Screening Biomarker for Heart and Kidney Disease? Angiology. 2019, 70, 210–9. [CrossRef] [PubMed]
- Hawkins AT, Wise PE, Chan T, Lee JT, Glyn T, Wood V, et al. Diverticulitis: An update from the age old Paradigm. Curr Probl Surg. 2020, 57, 100863. [CrossRef] [PubMed]
- Gareen IF, Gutman R, Sicks J, Tailor TD, Hoffman RM, Trivedi AN, et al. Significant Incidental Findings in the National Lung Screening Trial. JAMA Intern Med. 2023, 183, 677–84. [CrossRef] [PubMed] [PubMed Central]
- Munden RF, Black WC, Hartman TE, MacMahon H, Ko JP, Dyer DS, et al. Managing Incidental Findings on Thoracic CT: Lung Findings. A White Paper of the ACR Incidental Findings Committee. J Am Coll Radiol. 2021, 18, 1267–79. [CrossRef] [PubMed]
- MacMahon H, Naidich DP, Goo JM, Lee KS, Leung ANC, Mayo JR, et al. Guidelines for Management of Incidental Pulmonary Nodules Detected on CT Images: From the Fleischner Society 2017. Radiology. 2017, 284, 228–43. [CrossRef] [PubMed]
- Herts BR, Silverman SG, Hindman NM, Uzzo RG, Hartman RP, Israel GM, et al. Management of the Incidental Renal Mass on CT: A White Paper of the ACR Incidental Findings Committee. J Am Coll Radiol. 2018, 15, 264–73. [CrossRef] [PubMed]
- Berland LL, Silverman SG, Gore RM, Mayo-Smith WW, Megibow AJ, Yee J, et al. Managing incidental findings on abdominal CT: white paper of the ACR incidental findings committee. J Am Coll Radiol. 2010, 7, 754–73. [CrossRef] [PubMed]
- Hillman, BJ. Incidental. J Am Coll Radiol. 2017, 14, 860. [Google Scholar] [CrossRef] [PubMed]
- Mabotuwana T, Hombal V, Dalal S, Hall CS, Gunn M. Determining Adherence to Follow-up Imaging Recommendations. J Am Coll Radiol. 2018, 15, 422–8. [CrossRef] [PubMed]
- Brett, AS. Incidental Findings in Chest CT. NEJM Journal Watch (General Medicine).2024 [cited 2025 July 8]. Available online: https://www.jwatch.org/na57940/2024/09/17/incidental-findings-chest-ct.
- Elhaddad M, Hamam S. AI-Driven Clinical Decision Support Systems: An Ongoing Pursuit of Potential. Cureus 2024, 16, e57728. [CrossRef] [PubMed] [PubMed Central]
- Sutton RT, Pincock D, Baumgart DC, Sadowski DC, Fedorak RN, Kroeker KI. An overview of clinical decision support systems: benefits, risks, and strategies for success. NPJ Digit Med. 2020, 3, 17. [CrossRef] [PubMed] [PubMed Central]
- Langenbach MC, Foldyna B, Hadzic I, Langenbach IL, Raghu VK, Lu MT, et al. Automated anonymization of radiology reports: comparison of publicly available natural language processing and large language models. Eur Radiol. 2025, 35, 2634–41. [CrossRef] [PubMed]
- Sangal RB, Sharifi M, Rhodes D, Melnick ER. Clinical Decision Support: Moving Beyond Interruptive "Pop-up" Alerts. Mayo Clin Proc. 2023, 98, 1275–9. [CrossRef] [PubMed] [PubMed Central]
| Characteristic | Category | Value (n, %) |
|---|---|---|
| Initial and follow-up imaging | Initial imaging Follow-up |
323 (47.3%) 360 (52.7%) |
| The contrast agent used | Yes No |
479 (70.1%) 204 (29.9%) |
| Covid Test Result | Positive Recovered Negative Not tested |
327 (47.9%) 208 (30.5%) 131 (19.2%) 17 (2.5%) |
| Radiological CT findings of COVID-19 | NEG TYP ATYP IND |
273 (40.0%) 273 (40.0%) 97 (14.2%) 40 (5.9%) |
| Incidental findings | No Yes |
589 (86.2%) 94 (13.8%) |
| Recommended Follow-Up Modality | CT NoFC OTH US MRI NUC BIO LAB |
30 (31.9%) 25 (26.6%) 14 (14.9%) 9 (9.6%) 8 (8.5%) 4 (4.3%) 3 (3.2%) 1 (1.1%) |
| Follow-Up Consequence | IGN FI OTH BIO SUR DRU LAB |
45 (47.9%) 23 (24.5%) 16 (17.0%) 4 (4.3%) 3 (3.2%) 2 (2.1%) 1 (1.1%) |
| Relevance of the Incidental Findings | 0 1 2a 3a 3b |
63 (67.0%) 12 (12.8%) 9 (9.6%) 5 (5.3%) 5 (5.3%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





