A total of 11 participants attended the interviews. Most of the participants self-identified as women (N = 9, 81.8%). Almost a third of participants (N = 3, 27.3%) were either less than 30 years old or between 31 to 40 years old. More than a third (N = 4, 36.4%) had either an MPharm or an independent prescriber qualification. More than half (N = 6, 54.5%) worked at BSMHFT. Most participants (N = 8, 72.7%) worked between 25-40 hours on average in a week in the healthcare setting. In addition to the primary setting, participants were asked if they worked in any other healthcare setting, and only 2 (18.2%) worked in another healthcare setting that included a community pharmacy and a mental health hospital. A third of the participants (N = 4, 36.4%) had a work experience of more than 20 years. Many participants (N = 7, 63.6%) had completed formal training and/or continuing education programmes in mental health services and spent more than 60 hours doing so (N = 5, 45.5%).
Qualitative Findings
Qualitative findings revealed four major themes with sub-themes that had several codes. These codes were supported by participants' quotes. These themes are explained as follows:
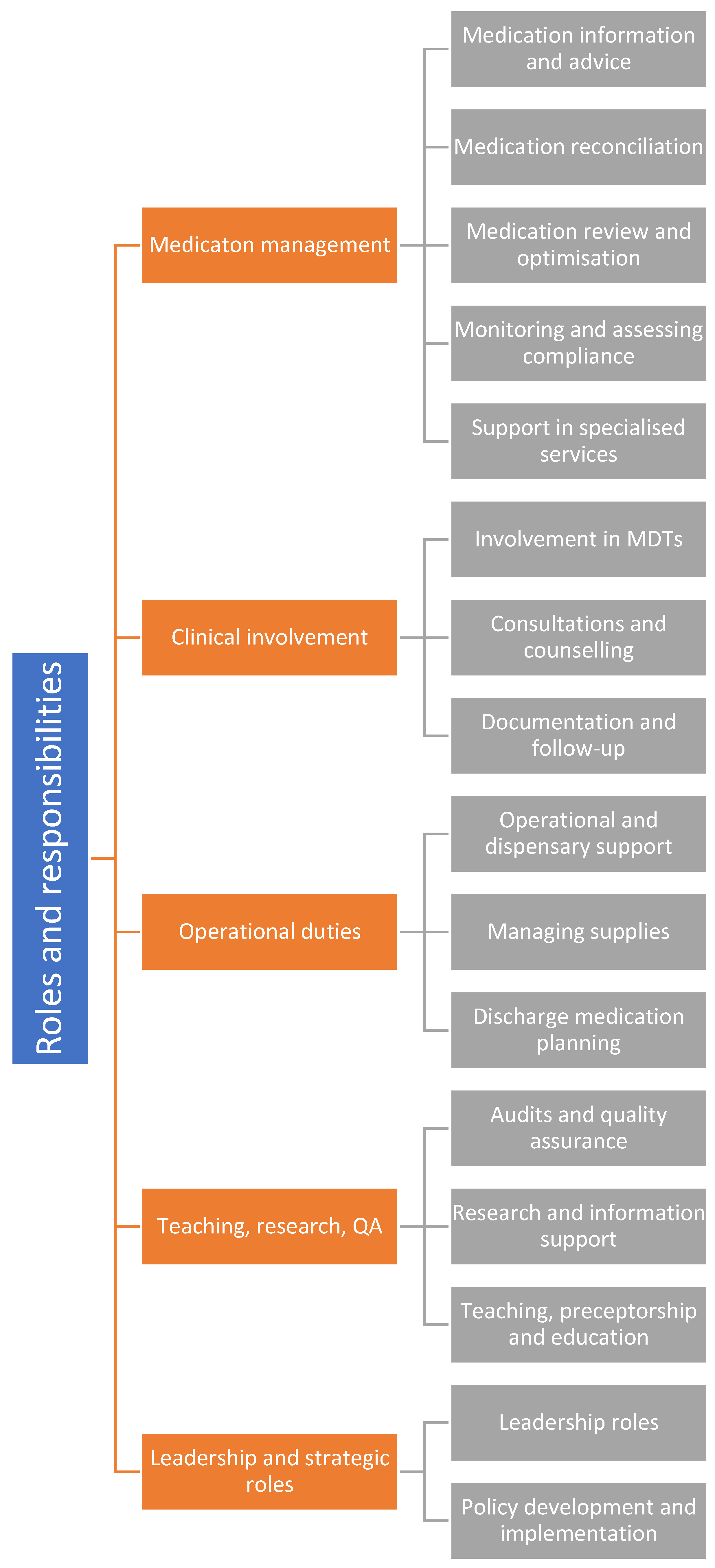
Theme 1: Roles and Responsibilities
The first theme that emerged from the data was about the roles and responsibilities of pharmacists. This included core medication management, involvement in other clinical tasks, operational duties, teaching, research, quality assurance, and leadership and strategic roles (
Figure 1).
Pharmacists play a key role in providing medication information and advice to both patients and healthcare professionals. They address medication-related inquiries, ranging from choices of use of medication (such as antidepressants) to complex medication decisions:
I would answer queries from consultants in the public of our outpatient services regarding specific medication choices in patients with complex physical and mental health background. (P2)
Pharmacists also perform medication reconciliation, ensuring patient safety and effective care. They verify the accuracy of medication lists and review drug interactions and appropriateness. They also prioritise timely reconciliation, aiming to complete the process within 24 to 48 hours of patient admission. Thanks to this process, medications are appropriately prescribed and reduce the risk of errors, particularly for patients with complex medication regimens that involve the monitoring of ECGs, blood tests, and vital signs.
The role of medication review and optimisation means an assessment of medication suitability. Pharmacists review patients’ medication charts to assess compliance. They also review psychotropic medications for safety and optimal dosing. They also monitor side effects and collaborate with other healthcare providers to make necessary adjustments. They may suggest switching and reducing medication to ensure patients receive the most appropriate, safe, and effective treatment regimens.
In addition, pharmacists assess medication compliance, particularly for high-risk medications such as sedatives and antipsychotics, and medications requiring specific tests such as lithium (requiring regular blood tests).
I'm responsible for running what we call an insight report which is a basic report which highlights all the high levels above 600 micrograms litre per every week and then we have to report those back to the clinicians directly and also document everything in the patient notes” (P7)
If patient requires switch from a medication to another medication either because patient wishes to change to something else or the side effect profile is not there is not something that patient can tolerate and then we help with the consultant to come with the alternative plan. (P8)
Pharmacists take charge of monitoring and assessing patient compliance. In the words of two participants:
We have to assess their compliance to the medications and sometimes it requires seeing each patient a few times throughout their stay. (P3)
Monitoring for new prescriptions and making sure that new prescriptions are clinically checked, professionally checked and appropriately ordered. (P9)
In critical settings such as psychiatric intensive care units and care homes, pharmacists perform outpatient prescriptions in specialised services such as memory clinics, pain management, and child mental health services. In these services, they manage high-risk medications such as clozapine and lithium.:
Every day we're dealing with clozapine, which is, as you are probably aware of, a very high-risk drug if it's not properly monitored. (P7)
“If somebody is on lithium, there are certain requirements and monitoring is required that we have to prompt our team to do the regular blood test. (P8)
- 2.
Clinical involvement
In multidisciplinary teams, pharmacists engage in ad-hoc and regular meetings to provide team members (doctors, nurses, social workers) with insights into patient care. Their involvement extends to internal pharmacy meetings that address barriers to safety and quality improvement:
We review the guidelines and give recommendations as a team... Discussing treatment plans for patients, monitoring progress, and making recommendations with references. (P4)
Consultations and counselling are key components of a pharmacist's clinical role. They regularly consult with patients to discuss treatment options, side effects, and high-risk medications (clozapine, lithium). They also offer psychoeducation to help patients understand their illness and treatment plans. One-on-one patient counselling sessions focus on medication adherence, side effects, and next steps in the treatment process. Some pharmacists proactively engage with patients to check if they have any concerns or questions.
Sometimes also consultations to speak to patients about any adverse reactions, treatment choice, and explanations of their new medications, especially for high-risk medications like clozapine and lithium. (P2)
Documentation and follow-up are integral to ensuring ongoing patient care and medication adherence. In this regard, pharmacists maintain detailed records for each patient, ensuring continuity in care and patient progress. Pharmacists are involved in verifying that medications are appropriately prescribed and taken as intended. They also contact community mental health teams to make sure plans are followed.
We call and check that medications are ordered and patients are taking them continuously…We contact community mental health teams to make sure plans are followed. (P4)
- 3.
Operational duties
Pharmacists ensure efficient pharmacy operations, thanks to which medication dispensing is smooth and safe. They assist with preparing medication, processing prescriptions, and ensuring accuracy. They also cover dispensary duties. Their responsibilities extend to on-call duties and oversight of medication storage and supply. Additionally, pharmacists lead medication supply logistics, process nurse supply requests, and ensure medication availability across wards. Additionally, pharmacists prepare medication for patients at their hospital discharge and are effectively involved in coordinating discharge plans (medication needs, counselling in advance) with the community mental health team to ensure continuity of care.
I'll be involved in the dispensary and making sure the dispensary is running properly and potentially accuracy checking dispensed medication. (P9)
When I arrive at work, I checked to see if we got any discharges... if it’s a short-term leave, how many days? How many of this tablet do we need? (P1)
- 4.
Involvement in teaching, research, and quality assurance
Pharmacists conduct regular audits of controlled drugs to ensure compliance with safety and quality standards, contributing to the continuous improvement of pharmacy practices and patient safety. Moreover, they research medication-related queries from medical staff and provide evidence-based support, using established guidelines:
We’ll look at like evidence-based situations... NICE guidelines... recommendations from the RPS... Maybe we should try this. (P1)
This research-based approach allows pharmacists to provide recommendations "with pros and cons to support decisions." (P4) Pharmacists also contribute to clinical trials in their institutions:
I work as a teacher practitioner pharmacist and my role is split 50/50 between teaching at (mentions the university) and working in a mental health setting. (P10)
Especially, pharmacists provide educational support (mentorship, role-modelling, instructions) to students and trainees, contributing significantly to their professional development. Their monthly clinical supervision meeting serves as ongoing educational support for colleagues and other healthcare teams.
- 5.
Leadership and strategic roles
Pharmacists play crucial leadership and strategic roles, contributing significantly to team management, coordination, and policy development within healthcare settings. Many pharmacists occupy leadership positions, overseeing teams of other healthcare professionals to ensure effective service delivery, workflows, and optimal function. Pharmacists also introduce new guidelines, medication practices, and new protocols for compliance.
I'm a lead pharmacist, so I'm leading a team of other Band 7 pharmacists and technicians. (P8)
And then I'm involved in a variety of the governance, and operational roles...pharmacological Therapies Committee, approval of policies and new drugs...governance processes within the Secure Care service. (P9)
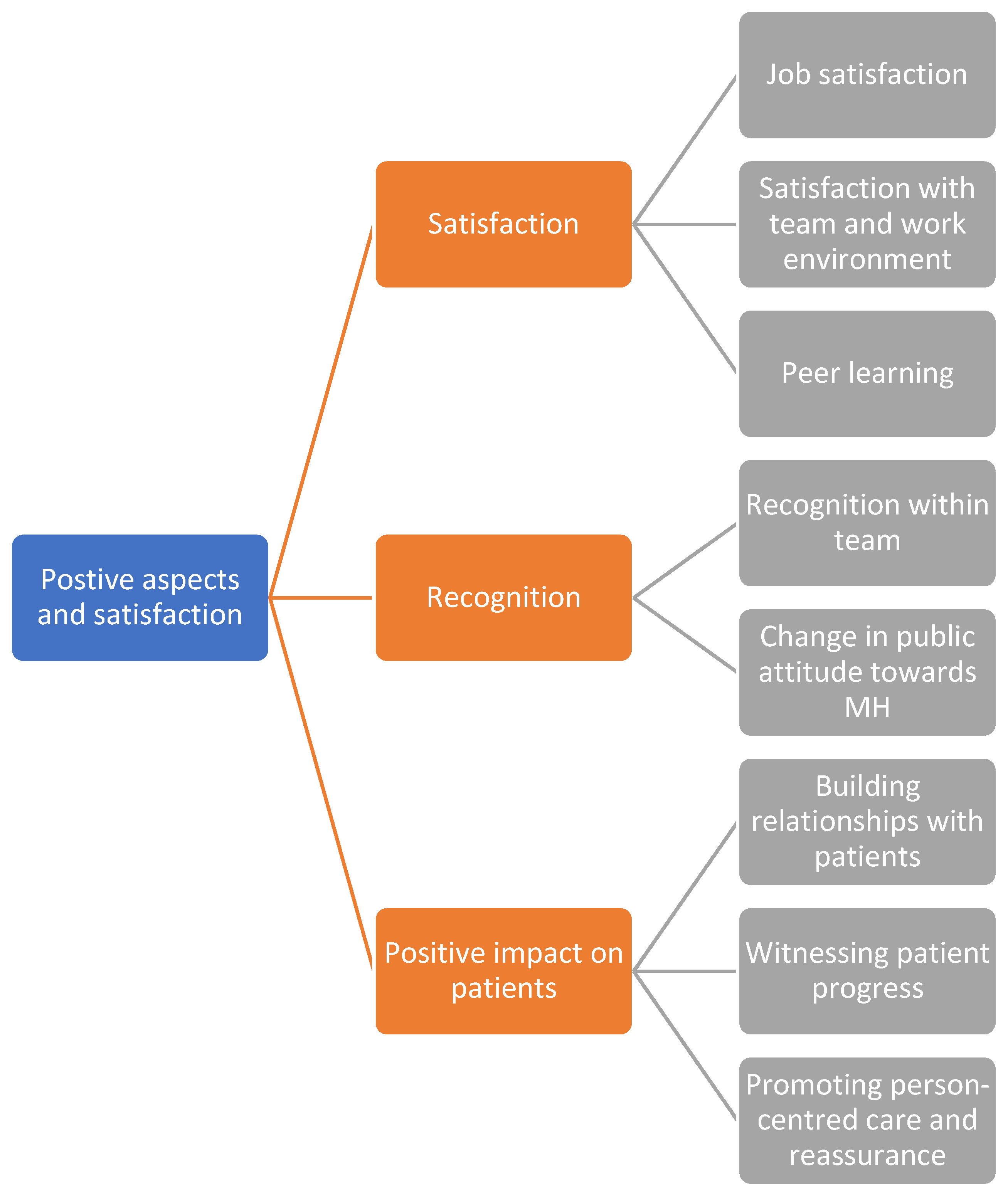
Theme 2: Positive aspects and satisfaction
The second theme that emerged was about the satisfaction of pharmacists with their roles and the positive aspects of the service. This included their personal satisfaction, their feeling of recognition, and the positive impact they bring on patients (
Figure 2).
- 6.
Satisfaction
Pharmacists' satisfaction results from not only seeing patients’ improvement in mental health. Interviewed pharmacists expressed a sense of accomplishment because their presence on the team results in effective patient intervention:
I get a lot more job satisfaction from working here... it’s really good to be able to sit down... and figure out something that will actually benefit them. (P1)
When we have pharmacists on the team, the patient intervention is there much quicker and more efficiently. (P8)
Team collaboration may result in satisfaction because it fosters a sense of community and strong rapport. The sense of camaraderie extends beyond mere professional interactions. Additionally, peer learning forms a critical aspect of pharmacists’ professional development. Building rapport with colleagues may foster learning, practice insights, and navigation through complex situations. Regular supervision and open dialogue with senior colleagues ensure updates in clinical knowledge and skills.
- 7.
Recognition of mental health and pharmacy services
Pharmacists working in mental health settings receive appreciation for their contributions to teams, of which they are proud. They envision an opportunity for professional growth within a team:
I feel proud of my work because I feel like with mental health, not a lot of people, as pharmacists, want to do it. (P10)
Participants observed a positive shift in public attitudes towards mental health, particularly among younger generations:
The attitudes in a younger generation are a bit changing. (P2)
It’s better than before... 5-10 years ago to now is better. Most people do understand that mental health is like physical health (P4).
Furthermore, the impact of the COVID-19 pandemic on mental health awareness was highlighted, with one participant stating:
Since COVID, I think the whole British population are quite willing to talk about... the troubles that they’re going through. (P6)
- 8.
Positive impacts on patients
Building personal connections with patients can foster trust and understanding. The ability to effectively communicate with patients about their medication contributes to not only therapeutic relationships but also to positive patient outcomes. Helping patients regain their well-being provides a strong sense of purpose and accomplishment. Person-centred treatment engages with patients’ unique needs. Providing patients with information about their treatment can reassure them when they express concerns about medications. Pharmacists may clear up patients’ reservations about medications and offer reassurances about the potential side effects or outcomes:
You've had that consultation with the patient that you know there's a particular medication that they. You want them to try all the team wants them to try, but they've got reservations about it and you can go and clear those reservations up and give them reassurance that what they're thinking might not be the case. (P11)
Figure 2 shows the theme diagram for Positive Aspects and Satisfaction.
Figure 2.
Theme diagram for Positive Aspects and Satisfaction.
Figure 2.
Theme diagram for Positive Aspects and Satisfaction.
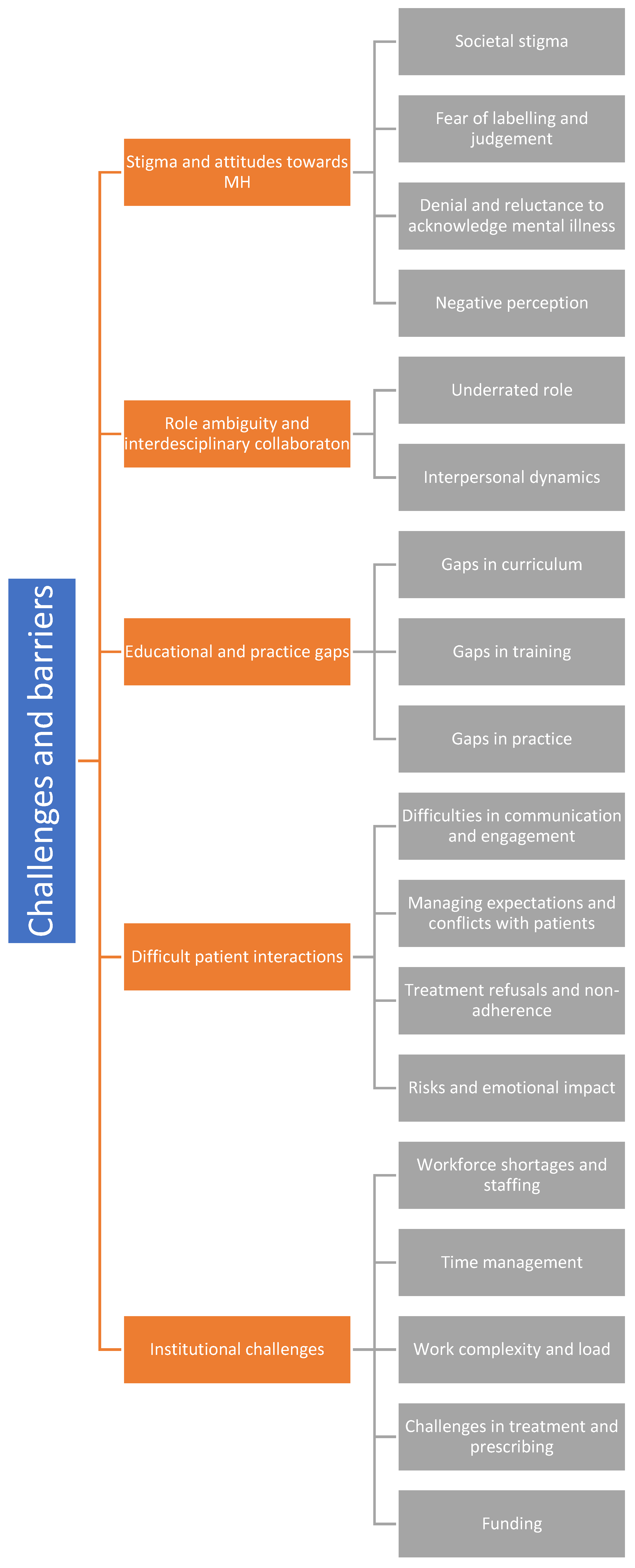
Theme 3: Challenges and Barriers
Mental health pharmacists face several challenges that can hinder the delivery of optimal care. These challenges include stigma and attitudes towards mental health, role ambiguity and interdisciplinary collaboration, educational and practice gaps, difficult patient interactions, and institutional challenges, which can influence continued success and satisfaction in this role.
- 9.
Stigma and attitudes towards mental health
Despite a positive shift in public attitudes, stigma remains a pervasive challenge in mental health care. Mental health is considered "still quite taboo," (P1) and may extend to their families, refusing to acknowledge the reality of their loved one's auditory hallucinations, and attributing the behaviour to moral failings. Also, mental health patients fear being labelled and judged. The fear of judgment extends beyond the individual because the diagnosis of mental health might be seen as a personal failure. However, in one case, patients feel "nothing wrong with them." (P11)
Another challenge is that some patients reflect on their previous experiences and avoid recognising their health conditions. As patients hide themselves “behind shadows," (P6) they might miss access to the support they need.
Society may hold negative perceptions and fear surrounding mental health treatment. People may call mental health facilities by "nasty names." (P1) Individuals with certain mental health diagnoses, such as schizophrenia or bipolar disorder, may be considered “dangerous” (P2). Even students or trainees feel “frightened” (P11) when working in mental health wards.
- 10.
Role ambiguity and interdisciplinary collaboration
Healthcare professionals may "underrate" (P8) mental health pharmacists in patient care
I think as a healthcare provider, pharmacists sometimes are underrated. We don't appreciate how much of an input we can have. (P8)
However, pharmacists may be fully integrated into the team’s decision-making processes and make great contributions to patient care. Moreover, communication and collaboration within multidisciplinary teams may be a challenge due to conflict in approaches to patient care. In some instances, teamwork is challenged by colleagues or by a lack of awareness between professions. Interviewed pharmacists reported that they navigated the challenges by highly valuing team spirit and providing evidence-based recommendations.
- 11.
Educational and practice gaps
Current pharmacy education lacks an emphasis on mental health topics, leaving new pharmacists unprepared for the complexities in practice. Mental health medications are only briefly addressed in the training and take a small component of the general curriculum. Even mental health education was limited to reading case studies or notes, or on-the-job training. Even a few research participants were not aware of the potential for working in mental health until they started in the field. Additionally, unstructured clinical supervision, limited funding, and skill-mix staffing may reduce confidence in knowledge. Patients’ needs may disconnect from pharmacists’ knowledge and skills.
- 12.
Difficult patient interactions
Patients’ mental uncertainty may impede the collection of necessary information for effective medications:
Because obviously mental health patients, depending on their condition, vary very much at their level of engagement and the quality of the interaction. So it's not just straightforward explaining something to somebody. (P7)
Pharmacists then have to determine the right time to engage with them. In cases, patients are in a state of relapse and unable to provide consent or engage in their care, reflecting an ethical dilemma. Managing patient expectations and dealing with conflicts is an aspect of complexity. Conflicts can arise with family members:
You get conflicts with the carers or family and friends of the patients as well about what is the right thing. (P2)
Patients may also resist medications or fail to adhere to prescribed treatments. Relapsed patients may return due to side effects resulting from discontinued treatment. Research participants also reported the risks and emotional impact of working in mental health. From facing personal harassment in the workplace, to working alongside patients with history of violence and aggression, to managing risks, pharmacists face a cumulative, overwhelming emotional burden.
- 13.
Institutional challenges
In the shortage of mental health pharmacists, other healthcare professionals struggle to perform their roles effectively, heavily burdening the existing team. Professional development and operational goals can be compromised, and the capacity to effectively use resources is constrained. A national agenda on mental health services cannot be achieved.
The complexity of systems makes it difficult to effectively manage time. One participant stated, "Systems in place are quite convoluted. It's quite difficult to know who to go to for what specific thing" (P2).
Time pressures become a barrier because professionals struggle to complete tasks within tight timeframes. Additionally, work complexity reflects a lack of guidelines for treatment, and heavy workload challenges meeting high standards.
Prescribing unlicensed medications challenges engagement with mental health treatment. This issue is further complicated when patients or caregivers encounter difficulties in obtaining the appropriate medications, or when patients’ medications are not reviewed after their conditions improve. In some cases, new prescriber pharmacists are not capable of prescribing due to a lack of practice and management of adverse effects. Insufficient funding represents a consistent issue that hampers quality care. Additionally, while students of different disciplines receive low compensation for professional development, pharmacy students do not even receive any:
My son being a physio student gets the £5000 a year learning support and gets travel expenses for placements. Physio, OT, and nursing students get that. Pharmacy doesn’t. (P9)
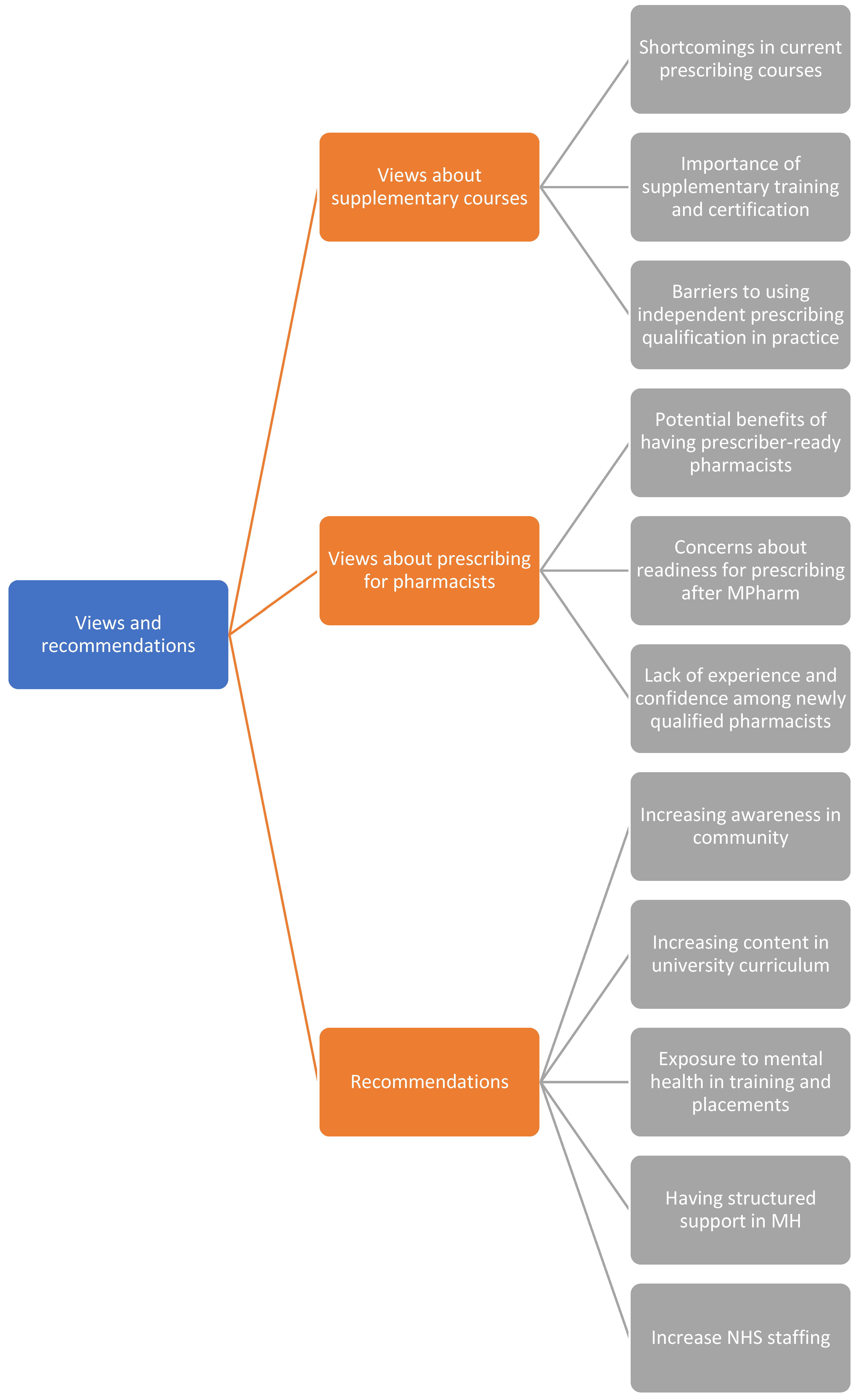
Theme 4: Views and Recommendations
- 14.
Views about supplementary courses
Current training courses do not prepare pharmacists for prescribing in mental health settings. Specialised mental health training (or certification) should be incorporated into prescribing courses to benefit early-career pharmacists, enhancing their competencies. Bespoke training can focus on conditions commonly encountered in mental health settings. Additionally, the healthcare system lacks the capacity to fully integrate pharmacists into prescribing roles, while pharmacists lack confidence and opportunities to take on the prescribing responsibilities. In some cases, pharmacists' tasks are not different from their previous ones (before the qualification), limiting the potential benefits of independent prescribing.
I found that the prescribing course was heavily weighted to physical things, which are important, but there just wasn’t enough in there for me to then go back to my practice and say, ‘OK, well, I learned this. (P10)
When you do that [postgraduate certification], then you kind of get to learn about a lot of different things within mental health. And then you can apply that to the get the resources, you get the knowledge. (P3)
- 15.
Views about prescribing for pharmacists
Prescriber-ready pharmacists alleviate the burden on other healthcare professionals, enhancing healthcare delivery and treatment outcomes. Interviewees expected an increased role of prescribing pharmacists in the future due to healthcare demands. However, many research participants expressed concerns about the readiness and confidence to prescribe after MPharm studies:
Some will not want to prescribe because they're not confident; some are going to be overconfident and wanting to prescribe without any kind of experience in a particular area. (P7)
The expectations placed on newly qualified pharmacists may mismatch their actual experience and readiness for prescribing. Therefore, new graduates should obtain additional qualifications before prescribing. Interviewees also worry about the generalist nature of the MPharm qualification. While other healthcare professionals (generalist junior doctors, trainee GPs) have had an additional two or three years of training before taking on responsibilities, pharmacists have not. Additionally, the transition from university to prescribing was seen as a significant leap in responsibility for many interviewees. Mental health pharmacists need practice and exposure to real-world scenarios to develop their confidence.
- 16.
Recommendations
Interviewees recommend increasing awareness about mental health to promote a more inclusive approach to mental health education and career development for pharmacists. These include (1) raising public and healthcare sector awareness to normalise mental health; (2) promoting community-based mental health initiatives to reduce the burden on hospital admissions; (3) increasing visibility of career opportunities in mental health pharmacy; and (4) enhancing educational exposure through events and job fairs.
Interviewees also recommended improving content in the university pharmacy curriculum, expanding lectures and modules “to give a bit more insight into mental health” (P8), and spanning across multiple years of study. However, a few participants insisted on introducing mental health modules in later years of study. Moreover, bringing in external experts may cultivate interest early on in mental health pharmacy education.
Interviewees requested more direct experience in mental health. Incorporating mental health into the MPharm curriculum could enhance its legitimacy, and workplace placements may foster deeper knowledge and confidence when dealing with mental health patients. In particular, curriculum coverage of mental health topics should be more in-depth and universal for learners, even if they do not intend to specialise in it.
Recommendations for structured support in mental health include (1) establishing clear entryways into the mental health field to make the transition easier for pharmacists; (2) implementing systematic mentorship programs; (3) developing a team-based model on mental health wards; and (4) encouraging early discussions about mental health placements in education programs.
An increase in NHS staffing responds to demands in mental health care. The increased staff-to-patient ratio would improve overall patient care and reduce the workload on individual healthcare professionals. Adding more pharmacists to mental health settings is needed to provide the necessary expertise and support. Newly qualified pharmacists should receive supportive supervision to adequately prepare them for a prescriber role (
Figure 4).
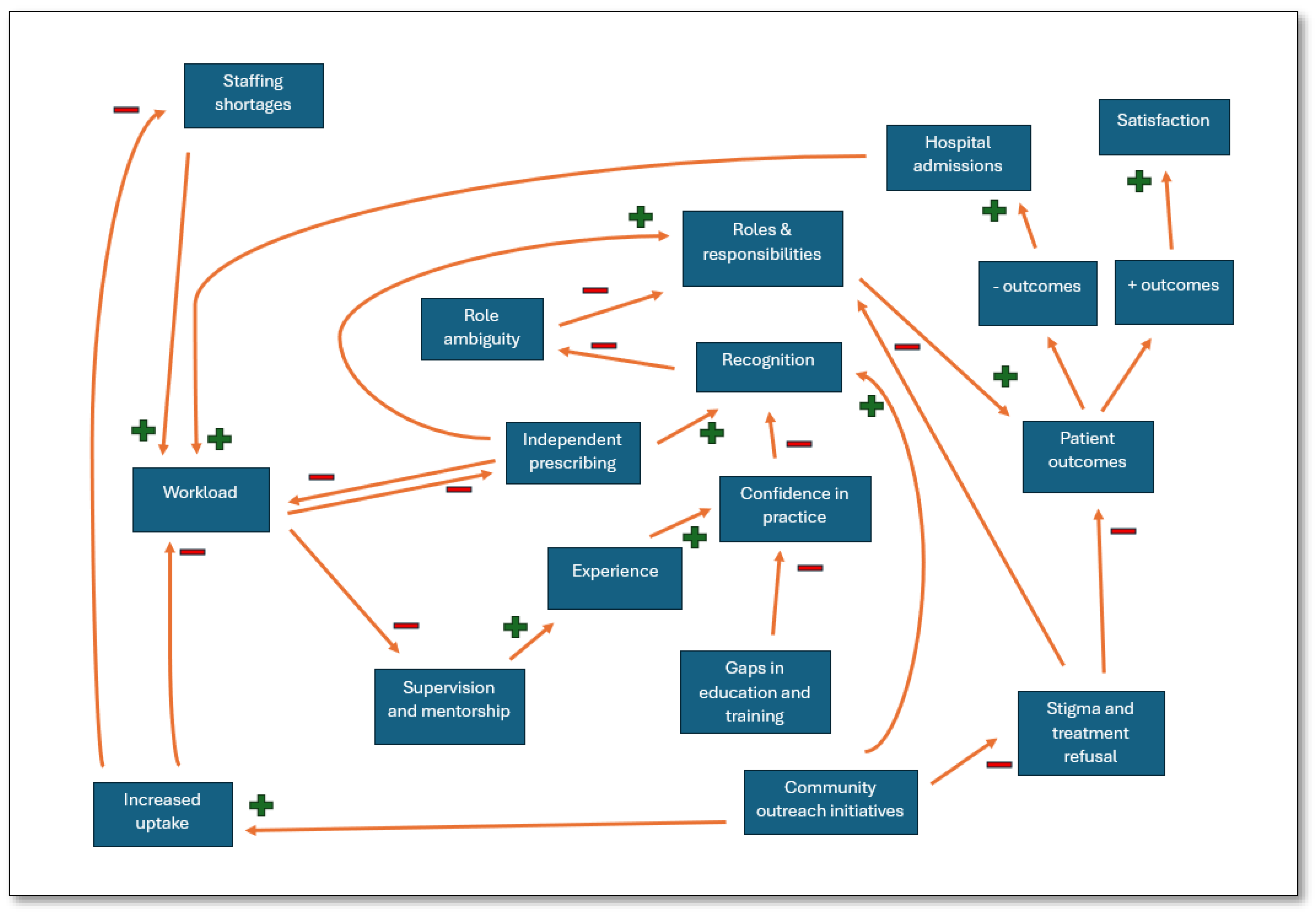
Interpretation and semantic linkages
Semantic linkages were explored across the themes to identify and understand a deeper, structural, and systemic integration of pharmacists' roles, experiences, and viewpoints (
Figure 5).
Pharmacists described the myriad roles and responsibilities they have within the service; however, they felt that their roles are still underrated (P8) and under-evaluated (P9). Despite these concerns, the positive impact on patients can compensate for such limitations, as satisfaction from positive patient outcomes carries an intrinsic value and contributes to the overall satisfaction in the role (P1). For some, it makes all the efforts worthwhile (P7). Stigma and illness denial result in non-adherence to MH treatment therapy by patients, which makes it harder for pharmacists to perform their patient-facing roles. There needs to be more community outreach initiatives and educational interventions that could reduce societal stigma among individuals and increase recognition of pharmacists in mental health. This could promote interest in others to join this field and would contribute to lower hospital admissions in the long run, thereby reducing the workload. This could also reduce hospital admissions (P1, P8-10).
Gaps in the undergraduate curriculum and lack of experience result in low preparedness among newly qualified prescriber pharmacists and consequently, hinder their ability to prescribe confidently (P5, 7-11).
Those who already have an independent prescriber qualification often are unable to utilise it due to staffing shortages and limited capacity to take on this role (P9, P10). Increased promotion of mental health opportunities could improve the uptake (P1, P8). If pharmacists start prescribing independently, it may ease the burden on other healthcare professionals and improve the service (P1). This would also contribute to greater recognition of pharmacists generally and within multidisciplinary teams. Expanding MH contents and placement opportunities in the pharmacy curriculum would improve knowledge and confidence among new graduates (P1, P9). These prescriber-ready graduates could be supported through supervision and mentorship by senior pharmacists. This would give them confidence to prescribe; however, ongoing issues related to staffing, workload, and time constraints prevent them from assuming these roles (P3, P9, P10).